Professional Documents
Culture Documents
AcuteDiarrhoea ICMR
AcuteDiarrhoea ICMR
Uploaded by
Devil DevilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AcuteDiarrhoea ICMR
AcuteDiarrhoea ICMR
Uploaded by
Devil DevilCopyright:
Available Formats
October/ 2019
Department of Health Research
Ministry of Health and Family Welfare, Government of India
Standard Treatment Workflow (STW) for the Management of
ACUTE DIARRHOEA
ICD-10-R19.7
ASK FOR SKIN PINCH TEST REFER TO HOSPITAL
• Duration • Locate the area on the child’s • Severe malnutrition/ HIV
• Blood in stool abdomen halfway between the • Severe dehydration
• Vomiting, fever, cough, recent umbilicus and the side of the • Hypernatremic (Na >145 mmol/L) /
measles, HIV status (if known) abdomen. hyponatremic dehydration (Na
• Immunization status and pre • Use thumb and first finger to pinch <135 mmol/L)
DIARRHOEA IS
illness feeding practices and not finger tips. • Dysentery with age <1 yr/ measles
• >3 loose or watery
• Fluids/ food/ drugs and other • The fold of the skin should be in a line in past 6 weeks/ dehydration/ sick
stools/ day
remedies taken during illness up and down the child’s body. • Dysentery with no improvement
• Acute Diarrhoea
• Firmly pick up all layers of the skin and on antibiotics
<14 days
tissue under them. • Persistent diarrhea with
• Persistent
• Pinch the skin for one second and then dehydration
diarrhoea >14 days EXAMINATION release it. Look to see if the skin pinch • Persistent diarrhea with serious
• Dysentery – blood • General condition of child goes back: systemic infection such as
in stools • Nutritional status (weight/ • Very slowly (longer than 2 seconds) pneumonia, sepsis, infants <4
weight for height / MUAC) • Slowly (skin stays up even for a months of age, or when there is
• Classify malnutrition if any brief instant) no improvement with treatment
• Signs of dehydration & • Immediately (normal) over 5 days
classify dehydration
MANAGEMENT
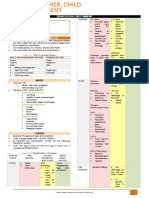
CLASSIFY DEHYDRATION
2 of the following: 2 of the following:
Not enough signs to a) Restless, irritable a) Lethargy/ unconscious
classify some or severe b) Sunken eyes b) Sunken eyes
dehydration c) Drinks eagerly, thirsty c) Not able to drink/ drinking poorly
d) Skin pinch - goes back very slowly d) Skin pinch - goes back slowly
NO DEHYDRATION: PLAN A SOME DEHYDRATION: PLAN B SEVERE DEHYDRATION: PLAN C
• Fluids • Manage in clinic /daycare facility with recommended • Urgent referral to hospital
• Give extra fluids (as much as child amount of ORS (75 ml /kg) over 4 hour period • Mother to continue rehydration by giving
will take) until diarrhoea stops. • If weight is not known frequent sips of ORS during transport or use
• Use WHO ORS after each loose NG tube when possible in patients with
stool (in addition to usual fluid AGE
<4 4 -11 12 -23 2–4 5-14 15 years poor drinking
months months months years years or older
intake) NO
• Upto 2 years → 50 -100 ml 5 – 7.9 8 - 10.9 11 – 16 – 30 kg or
WEIGHT <5kg kg kg 15.9 kg 29.9 kg more CAN YOU GIVE INTRAVENOUS
• 2 years or more → 100 -200 ml (IV) FLUIDS IMMEDIATELY?
200 - 400 - 600 - 800 - 1200 - 2200 -
• On ORS packet check whether IN mL 400 600 800 1200 2200 4000
200ml or 1 litre of clean water is NO
needed • After 4 hours reassess the child, classify dehydration • Start IV fluid immediately
• Frequent small sips with spoon or and select appropriate plan (A /B/C) • Ideal fluid is Ringer lactate solution / Normal
cup. • Give extra fluids, zinc supplement, feeding advise and saline (DNS in malnourished)
• If child vomits, wait 10 minutes counselling regarding danger signs* as in plan A FIRST GIVE THEN GIVE 70
then continue slowly. • Follow up in 5 days if no improvement AGE
30 ML/KG IN ML/KG IN
• Homemade fluids- salted rice
Infant (< 12 1 hour 5 hours
water, salted yogurt drink, months)
vegetable or chicken soup with salt Older 30 minutes 2.5 hours
PATIENT EDUCATION
and clean water, unsweetened fresh
fruit juice and coconut water • Danger signs* • If child can drink, give ORS by mouth while
• Unsuitable fluids - carbonated • Hygiene practices the drip is set up
beverages, commercial fruit juice, • Hand washing , proper disposal of excreta • Assess heart rate/ respiratory rate/ BP/ CFT/
sweetened tea & coffee, other • Safe drinking water consciousness and recognize early shock
medicinal teas / infusions. • Appropriate feeding practices • Refer for hospitalization
• Zinc supplement (Zinc sulphate/ • Vaccination as per IAP guidelines • If prevalance of cholera –
carbonate / acetate) Doxycycline single dose 300mg or
• 2-6 months → 10 mg/day x 2 weeks Tetracycline 12.5mg/kg 4 times a day x 3 days.
• >6 months → 20 mg/day x 2 weeks INVESTIGATIONS For young children Erythromycin 12.5 mg/kg
• Counsel Mother/ Attender • Some dehydration: 4 times a day x 3 days
• Feeding advise Preferable Tests- electrolytes • Associated vomitings –
• Infants on breast feed, to Ondanstetron 0.15 mg/kg/dose IV/oral in
• Severe dehydration:
continue more frequent breast addition to rehydration therapy
Essential tests- CBC, electrolytes
feeding than usual. • Reassess every 15-30 minutes till a strong
Preferable Tests- Renal Function Tests, VBG
• Those not on breast feed to radial pulse is present and then every hour
• In suspected cholera cases:
continue their usual milk feed/ If hydration status is not improving, give IV
Preferable tests- stool for hanging drop and
formula at least once in 3 hours. drip more rapidly
stool culture
• Give age appropriate foods to >6 • After 6 hours (infants) and 3 hours (older
• Dysentery: (no response to antibiotic in 2
months old based on their pre patients) - evaluate for dehydration and
days) Preferable test- stool culture & stool choose the appropriate plan (A, B, or C) to
illness feeding pattern
routine for trophozoites of Amoeba continue treatment
• Persistent diarrhoea: • Give ORS (about 5 ml/kg/hour) as soon as
• Danger signs (return immediately) Preferable test- stool routine microscopy, the child can drink: usually after 3-4 hours
• Passing many watery stools urine routine microscopy, urine culture , (infants) or 1-2 hours (children)
• Repeated vomiting / very thirsty sepsis screen • Observe for 6 hours after the child has been
• Eating / drinking poorly
fully rehydrated.
• Develops fever / blood in stools
• In hypernatremic and hyponatremic
WHEN CONSIDERING ALTERNATIVE DIAGNOSIS OF dehydration child appears relatively less ill /
• Follow up in 5 days if no improvement PERSISTENT DIARRHOEA AND DYSENTRY more ill respectively and needs to be
referred for hospitalization
DISCHARGE CRITERIA
PERSISTENT DIARRHOEA • Suffcient rehydration (indicated by wt gain
• Appropriate fluids to prevent or treat dehydration &/ or clinical status)
• Nutrition: • IV fluids no longer needed
• If breastfeeding, give more frequent, longer breastfeeds, day and night. • Oral intake = / > losses
• Other milk: replace with increased breastfeeding, or with fermented milk • Medical f/u available
products, such as yogurt, or half the milk with nutrient-rich semi-solid food.
• For other foods, follow feeding recommendations for the child’s age: give
small, frequent meals (at least 6 times a day), and avoid very sweet foods or DYSENTERY
drinks.
• Treat dehydration according to assessment.
• Zinc for 14 days
• Supplement vitamins / minerals • Ciprofloxacin 15 mg/kg twice a day and reassess
• Antimicrobial to treat diagnosed infection after 2 days.
A) Intestinal infection: Improvement: 3 days of treatment
• If blood in stool: Treat like dysentery • No improvement → Cefixime 10 mg//kg/d, 2 div
• If stool routine suggestive of Amoebiasis: Treat for it doses. Reassess after 2 days. If better complete
• If stool suggestive of cyst/ Trophozoite of Giardia: Give Metronidazole 5 3 -5 days of treatment.
mg/kg/dose x 8 hourly x 5 -7 days • If stool routine positive for Ameobiasis :
B) Treat Non intestinal such as UTI/ Otitis Media Metronidazole 10mg/kg/dose 8 hourly x 7
• Follow up in 5 days days (10 days in severe cases)
• Refer to hospital (See box) • Refer to hospital (See box)
REFERENCES
1. IMCI (WHO) module on Diarrhea 2014.
2. WHO Treatment for Diarrhea - A manual for physicians and other senior health workers 2005.
3. WHO GLOBAL TASK FORCE ON CHOLERA CONTROL 2010.
KEEP A HIGH THRESHOLD FOR INVASIVE PROCEDURES
This STW has been prepared by national experts of India with feasibility considerations for various levels of healthcare system in the country. These broad guidelines are advisory, and are
based on expert opinions and available scientific evidence. There may be variations in the management of an individual patient based on his/her specific condition, as decided by the
treating physician. There will be no indemnity for direct or indirect consequences. Kindly visit our web portal (stw.icmr.org.in) for more information.
© Indian Council of Medical Research and Department of Health Research, Ministry of Health & Family Welfare, Government of India.
You might also like
- Diagnostic Exam Nov 24Document25 pagesDiagnostic Exam Nov 24genita.keziahandrea100% (1)
- Chapter 1 - Bess GaskellDocument8 pagesChapter 1 - Bess GaskellEunice CortésNo ratings yet
- Argumentative Essay About Anti-VaxxersShould A COVID-19 Vaccine Be MandatoryDocument1 pageArgumentative Essay About Anti-VaxxersShould A COVID-19 Vaccine Be MandatoryAzril owayetNo ratings yet
- Infection Control Competency QuizDocument7 pagesInfection Control Competency QuizLoo DrBrad100% (1)
- Report of Medical Examination and Vaccination RecordDocument14 pagesReport of Medical Examination and Vaccination RecordHrishi WaghNo ratings yet
- LG-14 Important Health Programs CDDDocument20 pagesLG-14 Important Health Programs CDDMazinNo ratings yet
- Summary of IMCI Case ManagementDocument2 pagesSummary of IMCI Case Managementjanesky09100% (1)
- Appendix 11. Flow Chart For Cholera Case ManagementDocument1 pageAppendix 11. Flow Chart For Cholera Case ManagementGerard Pio Wee100% (2)
- Pediatric em 2Document28 pagesPediatric em 2bhupeshwariNo ratings yet
- TRANS - Dehydration & RehydrationDocument3 pagesTRANS - Dehydration & RehydrationRencel Hope BañezNo ratings yet
- Sudan IMCI 2.pptx CCDocument55 pagesSudan IMCI 2.pptx CCabdiqadir ali adanNo ratings yet
- World Health Organization: WHO/CDD/SER/91.15 REV.1Document10 pagesWorld Health Organization: WHO/CDD/SER/91.15 REV.1IjafiyaNo ratings yet
- Diarrhea Is Derived From Greek Word, Meaning 'Flowing Through'. It Is The Second Leading Cause of Death in Children Under 5 Years of AgeDocument12 pagesDiarrhea Is Derived From Greek Word, Meaning 'Flowing Through'. It Is The Second Leading Cause of Death in Children Under 5 Years of AgefitahsinghNo ratings yet
- Case Report Diarrhea: Adviser By: Dr. Alfred, Sp. A Writen By: Meylinda (1261050133)Document18 pagesCase Report Diarrhea: Adviser By: Dr. Alfred, Sp. A Writen By: Meylinda (1261050133)Norma Diona PurbaNo ratings yet
- Conditions of The GITTDocument4 pagesConditions of The GITTPGDME 20192020No ratings yet
- Integrated Management of Childhood Illness: Chart BookletDocument81 pagesIntegrated Management of Childhood Illness: Chart BookletReadcast EFNo ratings yet
- Integrated Management of Childhood IllnessesDocument65 pagesIntegrated Management of Childhood IllnessesJocel LañasNo ratings yet
- Integrated Management of Childhood IllnessesDocument11 pagesIntegrated Management of Childhood IllnessesSophia BarnesNo ratings yet
- CPG Acute Infectious Diarrhea Pocket Guide v2Document21 pagesCPG Acute Infectious Diarrhea Pocket Guide v2Moonyeen Jann Casera BalicNo ratings yet
- د. علي الزيدي Diarrhea-1 (Muhadharaty)Document47 pagesد. علي الزيدي Diarrhea-1 (Muhadharaty)aaaNo ratings yet
- Diarrhea 180822082356Document12 pagesDiarrhea 180822082356Prateek Singh100% (1)
- Dehydration in Peads: Nora Edora Francis PPW 23, Etd Hqe 2Document16 pagesDehydration in Peads: Nora Edora Francis PPW 23, Etd Hqe 2Maman GundohingNo ratings yet
- MalnutritionDocument7 pagesMalnutritionKookia BatoromaioNo ratings yet
- Diarrhea PediaDocument10 pagesDiarrhea PediaSuneeth Kumar MohantyNo ratings yet
- AGE MarchDocument46 pagesAGE MarchJefelson Eu Palaña NahidNo ratings yet
- Case ManagementDocument78 pagesCase ManagementSeyfNo ratings yet
- Diarrheal Diseases in ChildrenDocument16 pagesDiarrheal Diseases in ChildrenNupur SharmaNo ratings yet
- CEM7213 Bronchiolitis Pathway Acute Care West Sussex Oct 2011Document2 pagesCEM7213 Bronchiolitis Pathway Acute Care West Sussex Oct 2011drgrizahNo ratings yet
- Outline: (Trans) Lesson 4: Imci SummaryDocument2 pagesOutline: (Trans) Lesson 4: Imci SummaryAbish Julienne PecundoNo ratings yet
- Sick Young Infants (Referral, Treatment, Oral Drugs) : ImnciDocument46 pagesSick Young Infants (Referral, Treatment, Oral Drugs) : ImnciTanviNo ratings yet
- Care of The Child With Gastrointestinal Dysfunction: Betsy Johnson, MSN, CPNP-PCDocument66 pagesCare of The Child With Gastrointestinal Dysfunction: Betsy Johnson, MSN, CPNP-PCGelsey Gelsinator JianNo ratings yet
- Literature ReviewDocument23 pagesLiterature ReviewSyMaryamHaninaNo ratings yet
- GE in ChildrenDocument23 pagesGE in ChildrensamiNo ratings yet
- DehydrationDocument23 pagesDehydrationEusebius01No ratings yet
- Epidemiology and Control of Acute Diarrheal Diseases: Dr. Anish KhannaDocument21 pagesEpidemiology and Control of Acute Diarrheal Diseases: Dr. Anish KhannaHans Chester Rirao CapindingNo ratings yet
- National Control of Dirrheal Diseases (CDD) Program ObjectivesDocument6 pagesNational Control of Dirrheal Diseases (CDD) Program ObjectivesJoy FucananNo ratings yet
- NCP Leptospirosis - NewDocument5 pagesNCP Leptospirosis - Newglaiza_requintoNo ratings yet
- Nursing Care Plan Cues Diagnosis Justification: Sodium-132 Mmol/l (Low)Document3 pagesNursing Care Plan Cues Diagnosis Justification: Sodium-132 Mmol/l (Low)rei_alina75% (4)
- NCP For Deficient Fluid VolumeDocument2 pagesNCP For Deficient Fluid VolumeRedwing_Dc_854758% (12)
- Acute Diarrheal Diseases: Dr. Priyanka SachdevaDocument45 pagesAcute Diarrheal Diseases: Dr. Priyanka SachdevapriyankaNo ratings yet
- Care of The Child Applying Integrated Management of Childhood Illnesses (Imci)Document22 pagesCare of The Child Applying Integrated Management of Childhood Illnesses (Imci)Jesena SalveNo ratings yet
- CPG On AID PPT PresentationDocument83 pagesCPG On AID PPT Presentationsharmaine peroNo ratings yet
- Diarrhea in ChildrenDocument69 pagesDiarrhea in ChildrenNishita True SpiritNo ratings yet
- MaxineDocument19 pagesMaxinefaithdejamo2No ratings yet
- The Mcmaster Pediatric Curriculum: at NightDocument29 pagesThe Mcmaster Pediatric Curriculum: at NightFrancia ToledanoNo ratings yet
- 104 Theorle Finals PointersDocument7 pages104 Theorle Finals PointersSudaea AgacerNo ratings yet
- DR Mwanzas Pediatric Protocols 2017Document143 pagesDR Mwanzas Pediatric Protocols 2017Mwambazi MathewsNo ratings yet
- Imci Summary Toprank by JadeDocument13 pagesImci Summary Toprank by JadeJade SorongonNo ratings yet
- IMCI SumDocument6 pagesIMCI SumLazo JuleeNo ratings yet
- Approach To A Child With DiarrheaDocument28 pagesApproach To A Child With DiarrheaUmair QasimNo ratings yet
- Nursing Care Plan 1 - DiarrheaDocument7 pagesNursing Care Plan 1 - DiarrheakirbyroohNo ratings yet
- IMCI Management 2m-5yearsDocument35 pagesIMCI Management 2m-5yearsRachanaNo ratings yet
- Diarrhea in ChildrenDocument42 pagesDiarrhea in ChildrenIPNATC NEPALNo ratings yet
- CholeraDocument1 pageCholeraRevan NasirNo ratings yet
- IMCIDocument17 pagesIMCIapi-3707883No ratings yet
- ch2 fs1Document2 pagesch2 fs1ry beNo ratings yet
- General Tonic Monograph and Pharmacology Shi Quan Da Bu WanDocument8 pagesGeneral Tonic Monograph and Pharmacology Shi Quan Da Bu WanrikiNo ratings yet
- Case ReportDocument27 pagesCase ReportRuni ArumndariNo ratings yet
- Diarrhea AnilDocument52 pagesDiarrhea Anilanil sahNo ratings yet
- Dermatitis Herpetiformis: A Concise Guide to Causes, Tests and Treatment OptionsFrom EverandDermatitis Herpetiformis: A Concise Guide to Causes, Tests and Treatment OptionsNo ratings yet
- Soak It In: Hydrotherapy Treatments In 20 Minutes or Less for Health and BeautyFrom EverandSoak It In: Hydrotherapy Treatments In 20 Minutes or Less for Health and BeautyNo ratings yet
- 73. Vaishnavi HospitalDocument17 pages73. Vaishnavi HospitalDevil DevilNo ratings yet
- Patient Registration Form - 1284034 - 27-02-2022Document1 pagePatient Registration Form - 1284034 - 27-02-2022Devil DevilNo ratings yet
- NEET 2023 Solutions Code E2Document55 pagesNEET 2023 Solutions Code E2Devil DevilNo ratings yet
- NEET 2023 Question Paper Code E2Document32 pagesNEET 2023 Question Paper Code E2Devil DevilNo ratings yet
- 01june2019 EEJ IAINDocument17 pages01june2019 EEJ IAINDevil DevilNo ratings yet
- 28-Randomised Controlled Trial-YangBF 09.5.12Document14 pages28-Randomised Controlled Trial-YangBF 09.5.12sanjivdasNo ratings yet
- Cohort Study: Dr. Rahul Netragaonkar Associate ProfessorDocument37 pagesCohort Study: Dr. Rahul Netragaonkar Associate ProfessorRahul NetragaonkarNo ratings yet
- HIV Related LawsDocument7 pagesHIV Related LawsRMNo ratings yet
- REV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GDocument89 pagesREV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GFauziyah AnnisaaNo ratings yet
- eZH Ealth: Dosage Seq. Date (Mm/dd/yyyy) Vaccine Brand Name of Vaccinator Batch No. Lot NoDocument1 pageeZH Ealth: Dosage Seq. Date (Mm/dd/yyyy) Vaccine Brand Name of Vaccinator Batch No. Lot NoRvBombetaNo ratings yet
- Genital Tract InfectionsDocument1 pageGenital Tract InfectionsKatrina TaracatacNo ratings yet
- Bilateral Coperation in Health ManualDocument30 pagesBilateral Coperation in Health ManualHussen AbdulmenanNo ratings yet
- Vaginal Breech Delivery at Term and Neonatal Morbidity and Mortality - A Population-Based Cohort Study in SwedenDocument17 pagesVaginal Breech Delivery at Term and Neonatal Morbidity and Mortality - A Population-Based Cohort Study in SwedenRegina SeptianaNo ratings yet
- G2 Basic Sanitation Action PlanDocument3 pagesG2 Basic Sanitation Action PlanDontogan BarangayNo ratings yet
- Recommendation FormsDocument5 pagesRecommendation FormsRezi Sabutanan AmerilaNo ratings yet
- MCN Questionnaire DraftDocument8 pagesMCN Questionnaire DraftJenny AjocNo ratings yet
- PFAS in Drinking WaterDocument2 pagesPFAS in Drinking WaterWDET 101.9 FMNo ratings yet
- Week 29 - DRRRDocument5 pagesWeek 29 - DRRRMira VeranoNo ratings yet
- 2183 9417 Nas 31 03 206Document6 pages2183 9417 Nas 31 03 206VITOR HUGO PEREZNo ratings yet
- Philippine College of Occupational Medicine, Inc.: Phil M. Pangilinan, MD, Mha, FPSMS, Dpcom, PafpDocument3 pagesPhilippine College of Occupational Medicine, Inc.: Phil M. Pangilinan, MD, Mha, FPSMS, Dpcom, PafpANNLNo ratings yet
- Colorado Road Map For In-Person Learning: Letter To TeachersDocument4 pagesColorado Road Map For In-Person Learning: Letter To TeachersMichael_Roberts2019No ratings yet
- Call To Action For Contraceptive SafetyDocument16 pagesCall To Action For Contraceptive SafetyPopulation & Development Program (PopDev)No ratings yet
- FGBFRHTH Reduce 1 PDFDocument385 pagesFGBFRHTH Reduce 1 PDFAbu Abid Al-FatihNo ratings yet
- Cervicitis Symptoms, Treatment, Causes & TypesDocument1 pageCervicitis Symptoms, Treatment, Causes & Typesramit singlaNo ratings yet
- No Rinse Food Contact Cleaner Sanitizer PDFDocument2 pagesNo Rinse Food Contact Cleaner Sanitizer PDFJaime Lagos BorquezNo ratings yet
- Developing Political CompetenceDocument6 pagesDeveloping Political CompetencernrmmanphdNo ratings yet
- Australia Digital Passenger Declaration (DPD)Document2 pagesAustralia Digital Passenger Declaration (DPD)Anish bhandariNo ratings yet
- Serological Response To Myxomatosis Vaccination by Different Inoculations Systems On Farm RabbitsDocument12 pagesSerological Response To Myxomatosis Vaccination by Different Inoculations Systems On Farm RabbitsCamilaNo ratings yet
- Ovarian Cancer Prevention and Screening.22Document19 pagesOvarian Cancer Prevention and Screening.22tri erdiansyahNo ratings yet
- Sentinel-Event Root Cause Analysis RCADocument11 pagesSentinel-Event Root Cause Analysis RCAavsuNo ratings yet