Professional Documents
Culture Documents
Mosaicism Pamphlet 2023
Mosaicism Pamphlet 2023
Uploaded by
Zhang ZhiyongCopyright:
Available Formats
You might also like
- Wells 2003Document12 pagesWells 2003puspitaNo ratings yet
- Capalbo A Et Al 2023 On The Reproductive Capabilities of Aneuploid Human Preimplantation EmbryosDocument10 pagesCapalbo A Et Al 2023 On The Reproductive Capabilities of Aneuploid Human Preimplantation EmbryosJorge Alberto Salazar CartinNo ratings yet
- Cytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Document5 pagesCytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Mohammed R.HusseinNo ratings yet
- Cytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Document4 pagesCytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Mohammed R.HusseinNo ratings yet
- Illumina PGS Flip BookDocument20 pagesIllumina PGS Flip BookEmily KongNo ratings yet
- What Is Noninvasive Prenatal Screening (NIPS) ?Document5 pagesWhat Is Noninvasive Prenatal Screening (NIPS) ?Le Phuong LyNo ratings yet
- Embryo TransferDocument39 pagesEmbryo TransferMohamed ElhelalyNo ratings yet
- Association of Heteromorphism of Chromosome 9 and Recurrent Abortion (Ultrasound Diagnosed Blighted Ovum) : A Case ReportDocument4 pagesAssociation of Heteromorphism of Chromosome 9 and Recurrent Abortion (Ultrasound Diagnosed Blighted Ovum) : A Case ReportamirahyusnidarNo ratings yet
- PIIS0002937823001564Document2 pagesPIIS0002937823001564Kalaivathanan VathananNo ratings yet
- بیماری تروفوبلستیک بارداریDocument44 pagesبیماری تروفوبلستیک بارداریrazvanNo ratings yet
- Genetics and Fetal DevelopmentDocument16 pagesGenetics and Fetal DevelopmentLikoh TimothyNo ratings yet
- Effect of Oocyte Morphology On Embryo Development and ImplantationDocument8 pagesEffect of Oocyte Morphology On Embryo Development and ImplantationAgung SentosaNo ratings yet
- Vera Rodriguez2017Document6 pagesVera Rodriguez2017Roger BerniniNo ratings yet
- Genetic Screening: Identifying CarriersDocument10 pagesGenetic Screening: Identifying CarriersMohamed MetwalliNo ratings yet
- Embryo Selection in IVFDocument3 pagesEmbryo Selection in IVFFedrik Monte Kristo LimbongNo ratings yet
- Practice Bulletin: Prenatal Diagnostic Testing For Genetic DisordersDocument27 pagesPractice Bulletin: Prenatal Diagnostic Testing For Genetic Disordersmallikharjun medaNo ratings yet
- Chromosomal AbnormalitiesDocument6 pagesChromosomal AbnormalitiesPrashant MundeNo ratings yet
- EMJ Reproductive Health Supplementary Article 2019Document12 pagesEMJ Reproductive Health Supplementary Article 2019alikiyaei82No ratings yet
- Gap 055Document15 pagesGap 05505-OB-HU-DINA MERCEDES CAMPOSANO SALAZARNo ratings yet
- 2024 04 23 - PaperDocument20 pages2024 04 23 - PaperdrmanashreesankheNo ratings yet
- Zygosity: Offspring PregnancyDocument3 pagesZygosity: Offspring PregnancyStanley PangoniloNo ratings yet
- Pi Is 0015028216630704Document2 pagesPi Is 0015028216630704jelenavukoicic75No ratings yet
- 1 s2.0 S2305050014600099 MainDocument5 pages1 s2.0 S2305050014600099 MainMD LarasatiNo ratings yet
- PSTK 2Document6 pagesPSTK 2subhashbhukyaNo ratings yet
- 2022 NavarroDocument12 pages2022 NavarroivanaNo ratings yet
- Cytoplasmic Inheritance Redux (PDFDrive)Document31 pagesCytoplasmic Inheritance Redux (PDFDrive)agusfaturakhman33No ratings yet
- Reliable Detection of Subchromosomal Deletions and Duplications Using Cell Based Noninvasive Prenatal TestingDocument10 pagesReliable Detection of Subchromosomal Deletions and Duplications Using Cell Based Noninvasive Prenatal TestingCavin PengNo ratings yet
- Jurnal Oogenesis InternasionalDocument15 pagesJurnal Oogenesis InternasionalshafiraNo ratings yet
- m857 PDFDocument11 pagesm857 PDFMini PGNo ratings yet
- Topic 2 - Genes and HealthDocument6 pagesTopic 2 - Genes and HealthlamiaNo ratings yet
- 18 01 - 24 00 LeytDocument2 pages18 01 - 24 00 LeytSalo PhilippinesNo ratings yet
- 2024.plancental, Maternal, Fetal, and Techical Origins of False Positive Cell Fre DNA Screening ResultsDocument9 pages2024.plancental, Maternal, Fetal, and Techical Origins of False Positive Cell Fre DNA Screening Resultsrpina.genNo ratings yet
- Inversions - Mosaicism: Autosomal DisordersDocument44 pagesInversions - Mosaicism: Autosomal DisordersZainab Jamal SiddiquiNo ratings yet
- Screening For Fetal Chromosomal AbdnormalitiesDocument22 pagesScreening For Fetal Chromosomal AbdnormalitiesAlejandra MurilloNo ratings yet
- Research Article Placental Expression of NEMO Protein in Normal Pregnancy and PreeclampsiaDocument13 pagesResearch Article Placental Expression of NEMO Protein in Normal Pregnancy and PreeclampsiaAnonymous xEnIDVNo ratings yet
- 1 s2.0 S0015028214025461 MainDocument6 pages1 s2.0 S0015028214025461 MainIsabela LopesNo ratings yet
- tmp647F TMPDocument13 pagestmp647F TMPFrontiersNo ratings yet
- Cloning and Embryonic Stem Cells: A New Era in Human Biology and MedicineDocument10 pagesCloning and Embryonic Stem Cells: A New Era in Human Biology and Medicine7tuihjkhNo ratings yet
- 16multiple GestationsDocument76 pages16multiple Gestationskinfe hailemariamNo ratings yet
- Cytogenetics PDFDocument25 pagesCytogenetics PDFkai dollNo ratings yet
- Pol 030Document6 pagesPol 030Mirabella AstraNo ratings yet
- Pi Is 0015028209011005Document6 pagesPi Is 0015028209011005Meli AnaNo ratings yet
- Genetictesting 140305094745 Phpapp01Document50 pagesGenetictesting 140305094745 Phpapp01Lokeshwari KatreNo ratings yet
- Biology of Polyspermy in IVF and Its Clinical IndicationDocument6 pagesBiology of Polyspermy in IVF and Its Clinical IndicationMD LarasatiNo ratings yet
- Factors Affecting Levels of Circulating Cell-Free Fetal DNA in Maternal Plasma and Their Implications For Noninvasive Prenatal TestingDocument7 pagesFactors Affecting Levels of Circulating Cell-Free Fetal DNA in Maternal Plasma and Their Implications For Noninvasive Prenatal TestingNavidkazemi2056No ratings yet
- 1genetic Testing (L1)Document50 pages1genetic Testing (L1)d.djumanalieva.97No ratings yet
- Glossary of Genetic Terms For PatientsDocument6 pagesGlossary of Genetic Terms For Patientssnowy45.rmNo ratings yet
- In-Vitro Fertilisation: Shruti Samal ROLL NUMBER - 1120096 B.Sc. Life Science Second SemesterDocument20 pagesIn-Vitro Fertilisation: Shruti Samal ROLL NUMBER - 1120096 B.Sc. Life Science Second SemesterSHRUTI SAMALNo ratings yet
- The Genetics of MicrocephalyDocument6 pagesThe Genetics of MicrocephalyErsya MuslihNo ratings yet
- MB & Genetics 1Document17 pagesMB & Genetics 1rayNo ratings yet
- Immature Oocyte Incidence Contributing Factors and Effects OnDocument7 pagesImmature Oocyte Incidence Contributing Factors and Effects OnTrang Nguyễn NhưNo ratings yet
- 2009 TwinsDocument12 pages2009 TwinsHelena Ribeiro SouzaNo ratings yet
- Recurrent MiscarriageDocument6 pagesRecurrent MiscarriageuzmajbnNo ratings yet
- Molecular Support For Heterogonesis Resulting in Sesquizygotic TwinningDocument8 pagesMolecular Support For Heterogonesis Resulting in Sesquizygotic TwinningartNo ratings yet
- Fetal CellDocument5 pagesFetal CellSadia Sharmin NilimaNo ratings yet
- Numerical Aberrations: Meiotic NondisjunctionDocument36 pagesNumerical Aberrations: Meiotic NondisjunctionHemanth_Prasad_2860No ratings yet
- Childhood and Adolescence Voyages in Development 5th Edition Rathus Solutions ManualDocument36 pagesChildhood and Adolescence Voyages in Development 5th Edition Rathus Solutions Manualaudiblycaribbeeuwiq100% (15)
- Ultrasound in The Etiological Assessment of Embryonic Implantation Failures at The Fertilia Medical Clinic in BamakoDocument7 pagesUltrasound in The Etiological Assessment of Embryonic Implantation Failures at The Fertilia Medical Clinic in BamakoIJAR JOURNALNo ratings yet
- Infant Gender Selection & Personalized Medicine: Consumer's GuideFrom EverandInfant Gender Selection & Personalized Medicine: Consumer's GuideNo ratings yet
- Definition of InfertilityDocument6 pagesDefinition of InfertilityRatiram LilhareNo ratings yet
- Gregor Mendel & Quantitative Experimental ApproachDocument16 pagesGregor Mendel & Quantitative Experimental ApproachGerald GuevarraNo ratings yet
- Current Advances in Gestation and Parturition in Cats and DogsDocument12 pagesCurrent Advances in Gestation and Parturition in Cats and DogsVicky Concha AquevequeNo ratings yet
- Bio PracticalDocument5 pagesBio Practical37.Satkrit SamyaanNo ratings yet
- Infertility Lecture (2) - 1Document42 pagesInfertility Lecture (2) - 1Anivasa KabirNo ratings yet
- Comprehensive Evaluation of Contemporary Assisted Reproduction Technology Laboratory Operations To Determine Staffing Levels That Promote Patient Safety and Quality CareDocument7 pagesComprehensive Evaluation of Contemporary Assisted Reproduction Technology Laboratory Operations To Determine Staffing Levels That Promote Patient Safety and Quality CarePaula Manalo-SuliguinNo ratings yet
- Biology: Sexual ReproductionDocument7 pagesBiology: Sexual ReproductionAllan BustamanteNo ratings yet
- Plant CycleDocument6 pagesPlant CycleMinistry of GamersNo ratings yet
- Semen AnalysisDocument77 pagesSemen Analysisismi nurul kartikaNo ratings yet
- Page 2 8 13 19 23 27 42 52 56 61 66 OnlyDocument76 pagesPage 2 8 13 19 23 27 42 52 56 61 66 Onlyキース ジャスニエルNo ratings yet
- Practice Sheet How Do Organisms ReproduceDocument3 pagesPractice Sheet How Do Organisms ReproduceKanishka ChauhanNo ratings yet
- Introduction To PlantsDocument78 pagesIntroduction To PlantsAzizah ManzurNo ratings yet
- Bdol1 1Document2 pagesBdol1 1Olumide FamakindeNo ratings yet
- Analytic Dualisms, Stunted Sexualities, and The 'Horrified Gaze' - Western (Feminist) Dialogues About Female Genital MutilationDocument25 pagesAnalytic Dualisms, Stunted Sexualities, and The 'Horrified Gaze' - Western (Feminist) Dialogues About Female Genital MutilationsssadafNo ratings yet
- Summative Test in Science 7 2Document2 pagesSummative Test in Science 7 2Ana Jalaine Gran-JuezanNo ratings yet
- Reproduction in PlantsDocument17 pagesReproduction in Plantswafa eliasNo ratings yet
- Williams Obstetrics Study Guide - Anatomy - Fetus New Born - Labour & DeliveryDocument290 pagesWilliams Obstetrics Study Guide - Anatomy - Fetus New Born - Labour & DeliveryLoay Emad Abudalu100% (4)
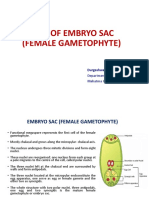
- Types of Embryo SacDocument18 pagesTypes of Embryo SacJemson Khundongbam100% (1)
- Algae Structure and ReproductionDocument18 pagesAlgae Structure and ReproductionPrasanth Kumar S100% (1)
- Frog Reproductive SystemDocument13 pagesFrog Reproductive Systemkaiden.g.lambertNo ratings yet
- Science Quarter 2 Module 5Document13 pagesScience Quarter 2 Module 5Zerreitug Elppa100% (2)
- Plants and Society 7th Edition Levetin Test Bank 1Document19 pagesPlants and Society 7th Edition Levetin Test Bank 1teresa100% (58)
- Minimal Stimulation Using Letrozole in Poor Responders: Original ArticleDocument4 pagesMinimal Stimulation Using Letrozole in Poor Responders: Original ArticleKopeNo ratings yet
- Stages of LaborDocument3 pagesStages of LaborCleo Pabilic100% (1)
- Reproduction DevelopmentDocument52 pagesReproduction DevelopmentYNAH MIA PICONESNo ratings yet
- LESSON 9 GametogenesisDocument20 pagesLESSON 9 GametogenesisMelissa ColosagaNo ratings yet
- Plant Diversity MCQs 1Document6 pagesPlant Diversity MCQs 1gavinliv86% (7)
- 1289 - Andrology Labratory ManualDocument245 pages1289 - Andrology Labratory ManualJuragang PotilNo ratings yet
- Kolfe Keranyo Sub City Educational Office Grade 8 Biology Final Examination 2010Document5 pagesKolfe Keranyo Sub City Educational Office Grade 8 Biology Final Examination 2010Emma Mohamed KhalidNo ratings yet
- Department of Biotechnology N.C.College of Engineering, Israna (Panipat)Document33 pagesDepartment of Biotechnology N.C.College of Engineering, Israna (Panipat)Aashishkatyaal100% (1)
Mosaicism Pamphlet 2023
Mosaicism Pamphlet 2023
Uploaded by
Zhang ZhiyongOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mosaicism Pamphlet 2023
Mosaicism Pamphlet 2023
Uploaded by
Zhang ZhiyongCopyright:
Available Formats
PGT FOR ANEUPLOIDY
SCREENING (PGT-A)
MOSAIC
RESULTS
Of note, reporting preferences may differ between clinics when it comes to
reporting mosaicism. This pamphlet provides information on mosaic
reporting, specifically, and does not pertain to non-mosaic reporting.
Confidential – Not for Redistribution
Version Date 1/6/2023
INTRODUCTION
Why is it important to have an entire pamphlet about mosaic results?
While most PGT-A results are straightforward, the interpretation of mosaic results
is a bit more complicated and can depend on several different subcategories of
mosaic results. Doctors and researchers in reproductive health are continuing to
study the outcomes of mosaic embryo transfers. While we continue to learn, this
pamphlet is intended to provide you an overview of our current knowledge on
mosaic results. Importantly, some mosaic embryos have the potential to grow and
develop into a healthy baby.
If you’ve already had a discussion with your doctor or you have done your own
research on this topic, you’ve probably encountered a lot of new terminology that
may be unfamiliar and confusing. You can read more about related terminology
on page 3 of this pamphlet. This pamphlet will also address questions such as
how mosaicism is detected and reported on pages 6-7.
This pamphlet focuses on mosaic results. Igenomix also offers a more general
Results Guide for PGT-A. Please ask us for a copy!
You are likely wondering what a mosaic result means for the reproductive
potential of an embryo. Whether an embryo transfer will result in a successful
pregnancy is influenced by several factors, including some that are specific to
your clinic and to your reproductive history. For this reason, a conversation about
expected reproductive potential is best addressed with your fertility provider.
Here we share information about the reproductive potential of embryos reported
as mosaic from studies focusing on the outcomes of transferring these embryos.
You can learn more about potential outcomes on pages 4-5 of this pamphlet.
Also check out the section of frequently asked questions (FAQs) found on pages
10-11. We hope you find this pamphlet answers many of your questions. Please
do not hesitate to contact us if you would like to schedule a phone consultation
with a certified genetic counselor for a discussion of your PGT-A results.
Confidential – Not for Redistribution 2|Page
Version Date 1/6/2023
TERMINOLOGY
Typically, human cells contain 23 pairs of chromosomes, for a total of 46.
PGT-A (Pre-implantation Genetic Testing for Aneuploidy): PGT-A refers to
screening a biopsy of an embryo for chromosomal copy number changes.
Testing a preimplantation embryo
PGT-A involves testing a small sample of cells (a biopsy)
from the embryo. Embryo biopsies are taken from the
outer layer of the embryo. These cells are called the
trophectoderm and they will eventually form the
placenta. The part of the embryo that will eventually
form the fetus, the inner cell mass, remains untouched.
If mosaicism is detected in the biopsy, this suggests, but
does not confirm, mosaicism in the rest of the embryo.
There are three main categories of informative PGT-A results:
Euploid refers to embryos with the typical chromosome copy
number. Each of the first 22 chromosomes have a copy
number of 2. The sex chromosomes typically come as a pair,
too, either XX or XY. Euploid embryos are the most likely to
result in a successful pregnancy and birth of a healthy baby.
Aneuploid refers to embryos with extra or missing
chromosomes. One or more chromosomes were observed to
have a copy number change (e.g., 1 or 3 copies instead of the
typical 2 copies). Aneuploid embryos are less likely to implant.
Those that implant are most likely to result in pregnancy loss
or an ongoing pregnancy with a chromosome condition.
Mosaic refers to embryos that have both euploid and
aneuploid cells. When cells in the biopsy are a mix of euploid
and aneuploid, mosaicism can be detected based on
intermediate chromosomal copy number changes. Mosaicism
can be reported as high level or low level.
Confidential – Not for Redistribution 3|Page
Version Date 1/6/2023
OUTCOMES OF MOSAIC EMBRYO TRANSFER
Several studies have examined pregnancy outcomes following transfer of embryos
reported as mosaic.
There are two primary outcomes when an embryo reported as mosaic is
transferred:
1. A seemingly healthy ongoing pregnancy/live birth.
2. Failed implantation or early miscarriage.
If an embryo is mosaic for a chromosome abnormality, it is possible that euploid
cells within the embryo will progress and aneuploid cells will not, resulting in a
healthy child. It is also possible that the aneuploidy will disrupt the development of
the embryo, preventing implantation or causing early miscarriage.
Current studies show that the likelihood of an ongoing pregnancy affected by a
mosaic chromosome abnormality is low (<1%). However, progression of aneuploid
cells in a pregnancy or live birth cannot be ruled out, and there have been rare case
reports of both high and low mosaicism persisting throughout the pregnancy.
There remains limited clinical data regarding the long-term outcomes of children
resulting from mosaic embryo transfers.
Several studies have explored the outcomes of mosaic embryo transfer. Success
rates vary by study. Overall, mosaic embryos have between a 15-45% chance of
resulting in ongoing pregnancy or live birth. Factors that may influence the
reproductive success of a mosaic embryo include:
Confidential – Not for Redistribution 4|Page
Version Date 1/6/2023
THE LEVEL OF MOSAICISM
Studies show that most embryos in the low mosaic range have high reproductive
potential, equal to or only slightly lower than that of euploid embryos. Whereas
some studies suggest slightly lower rates of pregnancy and higher rates of
miscarriage compared to euploid embryos, studies done by Igenomix show that the
reproductive potential of low mosaic embryos is equivalent to that of euploid
embryos. Although we cannot test the entire embryo, studies show that a low
mosaic result is most likely to correspond to an otherwise euploid embryo.
Embryos in the high mosaic range have lower reproductive potential than euploid
or low mosaic embryos but higher than aneuploid embryos. Concordance studies
show that a high mosaic result is more likely to correspond to an embryo where the
majority of the cells, including those of the inner cell mass, are aneuploid.
THE TYPE OF MOSAIC ANEUPLOIDY
Studies suggest that the type of mosaic aneuploidy may be more relevant for
determining the outcome of a mosaic embryo transfer, rather than the specific
chromosome involved in the aneuploidy. For example, embryos reported as mosaic
for a segmental aneuploidy (partial monosomy or partial trisomy) have been shown
to have higher reproductive potential as compared to embryos reported as mosaic
for a whole chromosome aneuploidy.
THE SPECIFIC MOSAIC CHROMOSOME
The specific mosaic chromosome involved has little impact on the chance for a
pregnancy to occur, and the chance for mosaicism to persist throughout the
pregnancy is generally low for all chromosomes. However, there may be some
additional counseling considerations for chromosomes associated with viable
aneuploidy syndromes, including chromosomes 13, 18, 21, and X.
While studies have not thus far demonstrated increased risks for pregnancies or
babies born with an aneuploidy syndrome, the data are very limited. Many
providers remain cautious about transferring embryos mosaic for the
chromosomes associated with viable aneuploidies.
Confidential – Not for Redistribution 5|Page
Version Date 1/6/2023
DETECTION OF MOSAICISM
Cells from the sample are analyzed together as a whole instead of individually.
Therefore, a mosaic result is not actually the direct observation of both euploid and
aneuploid cells in the embryo sample. Rather, PGT-A compares the relative number
of copies of each chromosome in the sample.
A euploid result is reported when the number of sequencing reads, representing
the amount of DNA, from each chromosome falls on the baseline, determined to
be copy number 2.
Chromosome reads that deviate from copy number 2 are an indication of
aneuploidy. An increase to copy number 3 (extra chromosome) or a decrease to
copy number 1 (missing chromosome) suggests that the chromosomal abnormality
is present in every cell of the biopsy. These results are reported as aneuploid.
Mosaicism is reported when an intermediate copy number change (between 1 and
2 or between 2 and 3) is detected. If a chromosome has 2 copies in some cells but
3 copies in other cells, then the content of DNA for that chromosome will fall
between copy number 2 and copy number 3.
Confidential – Not for Redistribution 6|Page
Version Date 1/6/2023
INTERMEDIATE COPY NUMBER VARIATION
When an intermediate copy number variation is detected, the embryo is reported
as mosaic. The level of mosaicism is determined by the degree of copy number
variation.
Low level mosaicism suggests that the majority of
cells are euploid. Chromosomes are reported as low
mosaic if the chromosomal copy number variation in
the biopsy is between 30-50%.
High level mosaicism suggests that the majority of
the cells in the biopsy are aneuploid. Embryos are
reported as high mosaic if the chromosomal copy
number variation in the biopsy is between 50-70%.
The scale below shows another representation of copy number variations.
Intermediate copy number variations between 30% and 70% fall within the
mosaic range and can be either a mosaic monosomy or a mosaic trisomy.
Intermediate copy number variations below 50% would be reported as low
mosaic and above 50% would be reported as high mosaic.
You may have noticed in the graphs on the previous page that the sequencing
reads appear wavy across the chromosomes. Because of this waviness, it is
difficult to provide a more refined percentage of copy number variation beyond
the general categories of euploid, low mosaic, high mosaic, and aneuploid.
Confidential – Not for Redistribution 7|Page
Version Date 1/6/2023
LIMITATIONS
PGT-A is a screening test. Testing is done on a biopsied sample of cells, which
typically represents the status of the whole embryo. False mosaic results are
possible.
True mosaic result False mosaic results
While a mosaic result suggests that the embryo is mosaic, the mosaic result from the
biopsy may not actually represent the embryo. The embryo may be entirely euploid
or entirely aneuploid. There are biological and technical limitations.
It is not possible with PGT-A to determine the chromosomal makeup of each cell
in the embryo. Therefore, even with a euploid result, mosaicism cannot be ruled
out.
Mosaicism cannot be ruled out
If mosaicism is not noted in the biopsy
sample it is unlikely to be present; however,
this possibility cannot be ruled out.
Confidential – Not for Redistribution 8|Page
Version Date 1/6/2023
LIMITATIONS OF COMPLEX MOSAIC RESULTS
When 2-5 chromosomes with intermediate copy number changes (gain or loss) are
detected in an embryo sample, the embryo is reported as complex mosaic
aneuploid.
Given that each cell in an embryo biopsy cannot be analyzed individually, it can be
challenging to interpret complex mosaic results. For example, if intermediate copy
number gains of chromosome 9 and chromosome 16 are reported, this could occur
through different mechanisms:
It is possible that trisomy 9 and It is also possible that trisomy 9
trisomy 16 are occurring and trisomy 16 are occurring
independently in different cells. simultaneously within the same
This may mean that there are no cells and that there are some
normal (euploid) cells in the biopsy. normal (euploid) cells.
If there are no euploid cells in the embryo, the embryo would have low
reproductive potential. Unfortunately, PGT-A cannot confirm that euploid cells are
present in the embryo even when reported as mosaic.
Confidential – Not for Redistribution 9|Page
Version Date 1/6/2023
FREQUENTLY ASKED QUESTIONS
Does mosaicism become more likely with age?
Mosaicism typically occurs after fertilization, with aneuploidy affecting a subset of
an embryo's cells. Chromosome abnormalities that occur after fertilization are
random and occur with similar frequency in all age groups. However, mosaic results
are actually observed a little less frequently for those in older age groups simply
because non-mosaic aneuploidy (pre-fertilization) is more common.
How common are mosaic results?
Based on Igenomix internal data, mosaicism is reported in approximately 8% of
embryos that undergo PGT-A.
What do I do with my mosaic embryos?
Options for embryos reported as mosaic may differ across clinics. These options
may include: transferring the embryo(s), storing the embryo(s) for future
consideration, or discarding the embryo(s). You will need to consult with your
physician to know your clinic’s policies.
Is there the option to do a re-biopsy?
A re-biopsy is not typically recommended, as results of the second biopsy would
not override the results of the first. Differing results between the first and second
biopsy would only confirm that the embryo is mosaic, which is already suspected
based on the initial biopsy. It is not possible to determine whether the results of
the first biopsy or the results of the second biopsy are more representative of the
embryo as a whole.
Does Igenomix recommend transferring an embryo reported as mosaic?
Igenomix recommends euploid and most low mosaic embryos for transfer. Euploid
embryos are the most likely to implant, develop to term, and result in a healthy live
birth. Transfer of an embryo reported as mosaic may be considered following
genetic counseling and discussion with a physician. The reproductive potential of
low mosaic embryos has been shown to be similar to that of euploid embryos with
low risk of persisting mosaicism. Clinics and specialists have varying opinions
regarding embryos reported as mosaic. The decision whether to transfer an
embryo reported as mosaic is ultimately that of the patient and their physician.
Confidential – Not for Redistribution 10 | P a g e
Version Date 1/6/2023
FREQUENTLY ASKED QUESTIONS
Do I need to do prenatal testing after transferring a mosaic embryo?
As for all pregnancies, prenatal evaluation and testing should be offered to you
and discussed with your obstetrician or prenatal genetic counselor. Options
include fetal anatomy scans, non-invasive prenatal testing (NIPT) performed on a
pregnant person’s blood sample, and diagnostic testing performed through
chorionic villus sampling (CVS) or amniocentesis.
Prenatal testing recommendations following transfer of a mosaic embryo are
controversial. Some providers may encourage diagnostic testing while others feel
the risks of prenatal diagnosis, while low, are greater than the risk for mosaicism
to persist through the pregnancy. Be sure to provide a complete copy of your
PGT-A report, which will include information about how to interpret mosaic
results in embryos, to your prenatal provider.
Is there genetic testing available during a pregnancy to assess for mosaicism?
Diagnostic testing is best suited to evaluate prenatal mosaicism. Chromosome
analysis can be performed on samples obtained during pregnancy from an
amniocentesis or chorionic villus sampling (CVS). Amniocentesis is the only
method by which fetal DNA (rather than placental DNA) can be analyzed. NIPT is
considered a screening tool and has limitations in detecting mosaicism.
Although there is no evidence for an increased risk of uniparental disomy (UPD)
following mosaic embryo transfer, additional assessment if diagnostic testing is
elected may be considered following transfer of an embryo with mosaicism of
chromosomes associated with UPD, including chromosomes 6, 7, 11, 14, and 15,
and 20.
Confidential – Not for Redistribution 11 | P a g e
Version Date 1/6/2023
CONCLUSIONS
We understand that mosaic results can be challenging to understand, and we
hope that the information shared in this pamphlet makes the result interpretation
a lot clearer. Igenomix genetic counselors are available to speak with you about
your mosaic results and other PGT-A results. The goal of genetic counseling is not
to tell you what to do or not to do, but rather to provide information to enable
you to make the best decisions about your medical care and embryo transfer
decisions. You may also find it valuable to consult with a genetic counselor
outside of Igenomix and throughout your reproductive journey.
This result guide is intended to provide an overview of your mosaic PGT-A results.
This guide is not intended to replace genetic counseling. If you still have questions
as to what your results mean after reading through this guide and reviewing the
results with your providers, you are welcome to schedule an appointment with a
genetic counselor at Igenomix. Please note that embryos are frozen and kept at the
fertility clinic, and any decisions regarding embryo transfer, discard, or storage are
made with the physician.
Contact us at:
Genetic Counseling department: (786) 485-0014, gc@igenomix.com
Igenomix Customer Support: (305) 501-4948, infousa@igenomix.com
Confidential – Not for Redistribution 12 | P a g e
Version Date 1/6/2023
You might also like
- Wells 2003Document12 pagesWells 2003puspitaNo ratings yet
- Capalbo A Et Al 2023 On The Reproductive Capabilities of Aneuploid Human Preimplantation EmbryosDocument10 pagesCapalbo A Et Al 2023 On The Reproductive Capabilities of Aneuploid Human Preimplantation EmbryosJorge Alberto Salazar CartinNo ratings yet
- Cytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Document5 pagesCytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Mohammed R.HusseinNo ratings yet
- Cytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Document4 pagesCytogenetics: Alkitab University - Collage of Medical Techniques Department of Medical Analysis 3 Rd. Stage - A4Mohammed R.HusseinNo ratings yet
- Illumina PGS Flip BookDocument20 pagesIllumina PGS Flip BookEmily KongNo ratings yet
- What Is Noninvasive Prenatal Screening (NIPS) ?Document5 pagesWhat Is Noninvasive Prenatal Screening (NIPS) ?Le Phuong LyNo ratings yet
- Embryo TransferDocument39 pagesEmbryo TransferMohamed ElhelalyNo ratings yet
- Association of Heteromorphism of Chromosome 9 and Recurrent Abortion (Ultrasound Diagnosed Blighted Ovum) : A Case ReportDocument4 pagesAssociation of Heteromorphism of Chromosome 9 and Recurrent Abortion (Ultrasound Diagnosed Blighted Ovum) : A Case ReportamirahyusnidarNo ratings yet
- PIIS0002937823001564Document2 pagesPIIS0002937823001564Kalaivathanan VathananNo ratings yet
- بیماری تروفوبلستیک بارداریDocument44 pagesبیماری تروفوبلستیک بارداریrazvanNo ratings yet
- Genetics and Fetal DevelopmentDocument16 pagesGenetics and Fetal DevelopmentLikoh TimothyNo ratings yet
- Effect of Oocyte Morphology On Embryo Development and ImplantationDocument8 pagesEffect of Oocyte Morphology On Embryo Development and ImplantationAgung SentosaNo ratings yet
- Vera Rodriguez2017Document6 pagesVera Rodriguez2017Roger BerniniNo ratings yet
- Genetic Screening: Identifying CarriersDocument10 pagesGenetic Screening: Identifying CarriersMohamed MetwalliNo ratings yet
- Embryo Selection in IVFDocument3 pagesEmbryo Selection in IVFFedrik Monte Kristo LimbongNo ratings yet
- Practice Bulletin: Prenatal Diagnostic Testing For Genetic DisordersDocument27 pagesPractice Bulletin: Prenatal Diagnostic Testing For Genetic Disordersmallikharjun medaNo ratings yet
- Chromosomal AbnormalitiesDocument6 pagesChromosomal AbnormalitiesPrashant MundeNo ratings yet
- EMJ Reproductive Health Supplementary Article 2019Document12 pagesEMJ Reproductive Health Supplementary Article 2019alikiyaei82No ratings yet
- Gap 055Document15 pagesGap 05505-OB-HU-DINA MERCEDES CAMPOSANO SALAZARNo ratings yet
- 2024 04 23 - PaperDocument20 pages2024 04 23 - PaperdrmanashreesankheNo ratings yet
- Zygosity: Offspring PregnancyDocument3 pagesZygosity: Offspring PregnancyStanley PangoniloNo ratings yet
- Pi Is 0015028216630704Document2 pagesPi Is 0015028216630704jelenavukoicic75No ratings yet
- 1 s2.0 S2305050014600099 MainDocument5 pages1 s2.0 S2305050014600099 MainMD LarasatiNo ratings yet
- PSTK 2Document6 pagesPSTK 2subhashbhukyaNo ratings yet
- 2022 NavarroDocument12 pages2022 NavarroivanaNo ratings yet
- Cytoplasmic Inheritance Redux (PDFDrive)Document31 pagesCytoplasmic Inheritance Redux (PDFDrive)agusfaturakhman33No ratings yet
- Reliable Detection of Subchromosomal Deletions and Duplications Using Cell Based Noninvasive Prenatal TestingDocument10 pagesReliable Detection of Subchromosomal Deletions and Duplications Using Cell Based Noninvasive Prenatal TestingCavin PengNo ratings yet
- Jurnal Oogenesis InternasionalDocument15 pagesJurnal Oogenesis InternasionalshafiraNo ratings yet
- m857 PDFDocument11 pagesm857 PDFMini PGNo ratings yet
- Topic 2 - Genes and HealthDocument6 pagesTopic 2 - Genes and HealthlamiaNo ratings yet
- 18 01 - 24 00 LeytDocument2 pages18 01 - 24 00 LeytSalo PhilippinesNo ratings yet
- 2024.plancental, Maternal, Fetal, and Techical Origins of False Positive Cell Fre DNA Screening ResultsDocument9 pages2024.plancental, Maternal, Fetal, and Techical Origins of False Positive Cell Fre DNA Screening Resultsrpina.genNo ratings yet
- Inversions - Mosaicism: Autosomal DisordersDocument44 pagesInversions - Mosaicism: Autosomal DisordersZainab Jamal SiddiquiNo ratings yet
- Screening For Fetal Chromosomal AbdnormalitiesDocument22 pagesScreening For Fetal Chromosomal AbdnormalitiesAlejandra MurilloNo ratings yet
- Research Article Placental Expression of NEMO Protein in Normal Pregnancy and PreeclampsiaDocument13 pagesResearch Article Placental Expression of NEMO Protein in Normal Pregnancy and PreeclampsiaAnonymous xEnIDVNo ratings yet
- 1 s2.0 S0015028214025461 MainDocument6 pages1 s2.0 S0015028214025461 MainIsabela LopesNo ratings yet
- tmp647F TMPDocument13 pagestmp647F TMPFrontiersNo ratings yet
- Cloning and Embryonic Stem Cells: A New Era in Human Biology and MedicineDocument10 pagesCloning and Embryonic Stem Cells: A New Era in Human Biology and Medicine7tuihjkhNo ratings yet
- 16multiple GestationsDocument76 pages16multiple Gestationskinfe hailemariamNo ratings yet
- Cytogenetics PDFDocument25 pagesCytogenetics PDFkai dollNo ratings yet
- Pol 030Document6 pagesPol 030Mirabella AstraNo ratings yet
- Pi Is 0015028209011005Document6 pagesPi Is 0015028209011005Meli AnaNo ratings yet
- Genetictesting 140305094745 Phpapp01Document50 pagesGenetictesting 140305094745 Phpapp01Lokeshwari KatreNo ratings yet
- Biology of Polyspermy in IVF and Its Clinical IndicationDocument6 pagesBiology of Polyspermy in IVF and Its Clinical IndicationMD LarasatiNo ratings yet
- Factors Affecting Levels of Circulating Cell-Free Fetal DNA in Maternal Plasma and Their Implications For Noninvasive Prenatal TestingDocument7 pagesFactors Affecting Levels of Circulating Cell-Free Fetal DNA in Maternal Plasma and Their Implications For Noninvasive Prenatal TestingNavidkazemi2056No ratings yet
- 1genetic Testing (L1)Document50 pages1genetic Testing (L1)d.djumanalieva.97No ratings yet
- Glossary of Genetic Terms For PatientsDocument6 pagesGlossary of Genetic Terms For Patientssnowy45.rmNo ratings yet
- In-Vitro Fertilisation: Shruti Samal ROLL NUMBER - 1120096 B.Sc. Life Science Second SemesterDocument20 pagesIn-Vitro Fertilisation: Shruti Samal ROLL NUMBER - 1120096 B.Sc. Life Science Second SemesterSHRUTI SAMALNo ratings yet
- The Genetics of MicrocephalyDocument6 pagesThe Genetics of MicrocephalyErsya MuslihNo ratings yet
- MB & Genetics 1Document17 pagesMB & Genetics 1rayNo ratings yet
- Immature Oocyte Incidence Contributing Factors and Effects OnDocument7 pagesImmature Oocyte Incidence Contributing Factors and Effects OnTrang Nguyễn NhưNo ratings yet
- 2009 TwinsDocument12 pages2009 TwinsHelena Ribeiro SouzaNo ratings yet
- Recurrent MiscarriageDocument6 pagesRecurrent MiscarriageuzmajbnNo ratings yet
- Molecular Support For Heterogonesis Resulting in Sesquizygotic TwinningDocument8 pagesMolecular Support For Heterogonesis Resulting in Sesquizygotic TwinningartNo ratings yet
- Fetal CellDocument5 pagesFetal CellSadia Sharmin NilimaNo ratings yet
- Numerical Aberrations: Meiotic NondisjunctionDocument36 pagesNumerical Aberrations: Meiotic NondisjunctionHemanth_Prasad_2860No ratings yet
- Childhood and Adolescence Voyages in Development 5th Edition Rathus Solutions ManualDocument36 pagesChildhood and Adolescence Voyages in Development 5th Edition Rathus Solutions Manualaudiblycaribbeeuwiq100% (15)
- Ultrasound in The Etiological Assessment of Embryonic Implantation Failures at The Fertilia Medical Clinic in BamakoDocument7 pagesUltrasound in The Etiological Assessment of Embryonic Implantation Failures at The Fertilia Medical Clinic in BamakoIJAR JOURNALNo ratings yet
- Infant Gender Selection & Personalized Medicine: Consumer's GuideFrom EverandInfant Gender Selection & Personalized Medicine: Consumer's GuideNo ratings yet
- Definition of InfertilityDocument6 pagesDefinition of InfertilityRatiram LilhareNo ratings yet
- Gregor Mendel & Quantitative Experimental ApproachDocument16 pagesGregor Mendel & Quantitative Experimental ApproachGerald GuevarraNo ratings yet
- Current Advances in Gestation and Parturition in Cats and DogsDocument12 pagesCurrent Advances in Gestation and Parturition in Cats and DogsVicky Concha AquevequeNo ratings yet
- Bio PracticalDocument5 pagesBio Practical37.Satkrit SamyaanNo ratings yet
- Infertility Lecture (2) - 1Document42 pagesInfertility Lecture (2) - 1Anivasa KabirNo ratings yet
- Comprehensive Evaluation of Contemporary Assisted Reproduction Technology Laboratory Operations To Determine Staffing Levels That Promote Patient Safety and Quality CareDocument7 pagesComprehensive Evaluation of Contemporary Assisted Reproduction Technology Laboratory Operations To Determine Staffing Levels That Promote Patient Safety and Quality CarePaula Manalo-SuliguinNo ratings yet
- Biology: Sexual ReproductionDocument7 pagesBiology: Sexual ReproductionAllan BustamanteNo ratings yet
- Plant CycleDocument6 pagesPlant CycleMinistry of GamersNo ratings yet
- Semen AnalysisDocument77 pagesSemen Analysisismi nurul kartikaNo ratings yet
- Page 2 8 13 19 23 27 42 52 56 61 66 OnlyDocument76 pagesPage 2 8 13 19 23 27 42 52 56 61 66 Onlyキース ジャスニエルNo ratings yet
- Practice Sheet How Do Organisms ReproduceDocument3 pagesPractice Sheet How Do Organisms ReproduceKanishka ChauhanNo ratings yet
- Introduction To PlantsDocument78 pagesIntroduction To PlantsAzizah ManzurNo ratings yet
- Bdol1 1Document2 pagesBdol1 1Olumide FamakindeNo ratings yet
- Analytic Dualisms, Stunted Sexualities, and The 'Horrified Gaze' - Western (Feminist) Dialogues About Female Genital MutilationDocument25 pagesAnalytic Dualisms, Stunted Sexualities, and The 'Horrified Gaze' - Western (Feminist) Dialogues About Female Genital MutilationsssadafNo ratings yet
- Summative Test in Science 7 2Document2 pagesSummative Test in Science 7 2Ana Jalaine Gran-JuezanNo ratings yet
- Reproduction in PlantsDocument17 pagesReproduction in Plantswafa eliasNo ratings yet
- Williams Obstetrics Study Guide - Anatomy - Fetus New Born - Labour & DeliveryDocument290 pagesWilliams Obstetrics Study Guide - Anatomy - Fetus New Born - Labour & DeliveryLoay Emad Abudalu100% (4)
- Types of Embryo SacDocument18 pagesTypes of Embryo SacJemson Khundongbam100% (1)
- Algae Structure and ReproductionDocument18 pagesAlgae Structure and ReproductionPrasanth Kumar S100% (1)
- Frog Reproductive SystemDocument13 pagesFrog Reproductive Systemkaiden.g.lambertNo ratings yet
- Science Quarter 2 Module 5Document13 pagesScience Quarter 2 Module 5Zerreitug Elppa100% (2)
- Plants and Society 7th Edition Levetin Test Bank 1Document19 pagesPlants and Society 7th Edition Levetin Test Bank 1teresa100% (58)
- Minimal Stimulation Using Letrozole in Poor Responders: Original ArticleDocument4 pagesMinimal Stimulation Using Letrozole in Poor Responders: Original ArticleKopeNo ratings yet
- Stages of LaborDocument3 pagesStages of LaborCleo Pabilic100% (1)
- Reproduction DevelopmentDocument52 pagesReproduction DevelopmentYNAH MIA PICONESNo ratings yet
- LESSON 9 GametogenesisDocument20 pagesLESSON 9 GametogenesisMelissa ColosagaNo ratings yet
- Plant Diversity MCQs 1Document6 pagesPlant Diversity MCQs 1gavinliv86% (7)
- 1289 - Andrology Labratory ManualDocument245 pages1289 - Andrology Labratory ManualJuragang PotilNo ratings yet
- Kolfe Keranyo Sub City Educational Office Grade 8 Biology Final Examination 2010Document5 pagesKolfe Keranyo Sub City Educational Office Grade 8 Biology Final Examination 2010Emma Mohamed KhalidNo ratings yet
- Department of Biotechnology N.C.College of Engineering, Israna (Panipat)Document33 pagesDepartment of Biotechnology N.C.College of Engineering, Israna (Panipat)Aashishkatyaal100% (1)