Professional Documents
Culture Documents
Hemostasis
Hemostasis
Uploaded by
sembogga michealOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemostasis
Hemostasis
Uploaded by
sembogga michealCopyright:
Available Formats
Last edited: 10/24/2021
1. HEMOSTASIS: COAGULATION CASCADE
Hemostasis: Coagulation Cascade Medical Editor: Mariel Antoinette L. Perez
OUTLINE
I) INTRODUCTION
II) FIVE STEPS OF HEMOSTASIS
III) APPENDIX
IV) REVIEW QUESTIONS
V) REFRENCES
I) INTRODUCTION
(1) HEMOSTASIS
Word Etiology
o “hemo” – blood; “stasis” – stop
Localized blood stopper
Usually occurs when there’s damage to blood vessels
o E.g., ruptured, lacerated, leaking out
A sequence of five steps
(2) NATURAL ANTI-COAGULATION OF BLOOD
Before studying the process of hemostasis, it’s important
to understand what keeps the blood naturally thin
o Prevents blood from becoming thrombotic,
coagulating on its own, and forming a clot
There are three general layers to take note of:
o Endothelial cells
secrete chemicals
• Nitric Oxide (NO)
• Prostacyclin (PGI2)
o Subendothelial cells
underneath the endothelial layer
made up of connective tissue, specifically collagen
collagen-rich layer
o Smooth muscle cells with specific types of receptors
nociceptors = pain receptors Figure 1 Natural Nanti coagualtion mechanisms
(1) Platelet Inactivation
II) FIVE STEPS OF HEMOSTASIS
There are two things in the blood: plasma and cells
o Cells (or formed elements) such as White Blood Cells
(WBCs), Red Blood Cells (RBCs), and platelets
o Platelets
Microscopic (tiny), cytoplasmic fragments
Derived from megakaryocytes
Naturally inhibited by NO and PGI2
• keeps platelet inactive to prevent it from
binding onto the surface of the endothelial cell
(2) Heparin Sulfate
Glycosaminoglycan present on the membrane
Natural anti-coagulant
Binds and activates protein Anti-Thrombin III (ATIII)
o Degrades and inactivates clotting factors II, IX, X
Clotting factors are naturally just circulating in the
bloodstream
(3) Thrombomodulin
Binds with protein called Thrombin (Factor II/ FII)
o Activates Protein C
Degrades and inactivates factors V and VIII
HEMOSTASIS: COAGULATION CASCADE HEMATOLOGY: Note #7. 1 of 6
(1) VASCULAR SPASM (2) PLATELET PLUG FORMATION
(1) Trigger With the endothelial cells damaged,
o There will be a decreased release of NO and PGI2
injured blood vessel endothelial damage Platelets will not be inactivated
o May also cause damage to the underlying tissue Allow platelets to attach to endothelium
o Blood may leak out and decrease blood volume o Damaged heparin sulfate will not be able to keep
(2) Purpose clotting factors inactivated
o Damaged thrombomodulin will not be able to activate
Prevent blood loss from occurring by contracting or protein C cannot keep FV and FVIII inactivated
constricting blood vessels
(1) Platelet Activation
(3) Mechanism
Platelets are activated when GP1b binds with vWF
(i) Endothelin o GP1b (glycoprotein-1b)
Secreted by injured endothelial cells
Platelet receptor that specifically binds to vWF
binds on to receptor on smooth muscle o von Willebrand Factor (vWF)
activates intracellular PIP2-Calcium mechanism secreted by injured endothelial cells
smooth muscle contracts triggers vessel (2) Platelet chemical release
vasoconstriction decreases blood vessel
diameter prevents blood loss Once activated, will release the following
o Adenosine Diphosphate (ADP)
(ii) Myogenic Mechanism o Thromboxane A2 (TXA2)
o Serotonin (5-hydroxytryptamine or 5-HT)
Direct contact or injury to smooth muscle causes
smooth muscle contraction (3) Platelet Aggregation
(iii) Nociceptor Activation Platelets have receptors on their membrane that
specifically bind with ADP and TXA2
Inflammatory chemicals are released when there’s
ADP & TXA2 stimulates platelets to come and aggregate
inflammation
at area of injured vessel
• E.g., histamine, leukotrienes, prostaglandins, Platelets bind with other platelets via their GP2b/3a, with
These chemicals stimulate the nociceptors fibrinogen bridging them together
Nociceptors (pain receptors) will initiate pain
Pain reflex induces vasoconstriction (4) Vascular Spasm Effect Enhancement
TXA2 and serotonin bind to the smooth muscle
o Cause contraction
o Triggers ↑vasoconstriction of injured blood vessels
o Enhances the vascular spasm effect
(5) Clinical Significance
Aspirin: TXA2 release
Clopidogrel, Prasugrel, Ticagrelor: ADP release
Abciximab: inhibits GP2b/3a inhibitors
Von Willebrand Disease: VWF production
Figure 2 Vascular Spasm
Figure 3 Platelet plug formation
2 of 6 HEMATOLOGY: Note #7 HEMOSTASIS: COAGULATION CASCADE
(3) COAGULATION CASCADE o Activates XIII XIIIa
Requires Ca2+
Intrinsic pathway
o Independent of the extrinsic pathway Factor XIIIa
For example, someone’s blood in a test tube is not o Also known as Fibrin Stabilizing Factor
heparinized (no heparin coating) o Crosslinks fibrin stands together
• Glass has rough, charged surface hence, Crosslinked fibrin
XIIa from the intrinsic pathway gets activated o Creates a fibrin mesh
This shows that the intrinsic pathway can occur in Mesh will hold down the platelet plug in place
a test tube independent of the extrinsic pathway. Mesh prevents platelets from dislodging and going
o Takes 4-6 minutes to different areas to cause an embolism
Extrinsic pathway o Thickens the blood passing through the area to slow
o Dependent on some of the factors and proteins within down the blood flow and prevent blood loss
the intrinsic pathway
(3) Extrinsic Pathway
o Takes 30 seconds
Note: An “a” after the roman numeral indicates an Blood vessel injury triggers release of Tissue factor
activated factor. (Factor III)
Factor III activates Factor VII VIIa
(1) Intrinsic Pathway o requires Ca2+ and PF4
Liver constantly creates clotting proteins that are normally VIIa can activate IX IXa
inactivated while circulating in the blood VIIa can converge into or stimulate the common pathway
Activated platelets express phosphatidyl serine groups on o Requires Ca2+ and PF4
their membrane, causing a negative charge
Negative charge will interact with and activate Factor XII Note: Tip for Remembering the Coagulation Cascade
(Hageman Factor)
o XII XIIa X marks the spot in the middle = Factor X
Left (intrinsic pathway) count downwards
XIIa activates XI FXIa o 12 8 (skip 10)
XIa activates IX IXa
Right (extrinsic pathway)
IXa forms a complex with VIIIa o 3 + 7 = 10
o Complexation requires PF3 and Ca2+
Common Pathway
VIIIa-IXa activates X Xa o 5 x 2 x 1 = 10
(2) Common Pathway (4) Clinical Significance
X Xa is the start of the common pathway Hemophilia A→↓in factor VIII
Xa, Va, and Ca2+ will activate prothrombin activator
Hemophilia B→↓in factor IX
o converts prothrombin (II) to thrombin (IIa)
Hemophilia C→↓in factor XI
Thrombin reacts in two ways:
Heparin, Factor X inhibitors (Rivaroxaban)→↓factor X
o Links together Fibrinogen (I) into Fibrin (Ia)
Fibrinogen is soluble Heparin, Factor II Inhibitors (Dabigatran)→↓thrombin or
Fibrin is insoluble in the plasma also known as Factor II
• Helps turn liquid blood into a jelly-like Warfarin→↓ formation of Thrombin, Factor VII, Factor IX,
substance to slows down blood flow in the Factor X
area and prevent loss of RBCs
HEMOSTASIS: COAGULATION CASCADE HEMATOLOGY: Note #7. 3 of 6
(5) FIBRINOLYSIS
(4) CLOT RETRACTION & REPAIR
(1) Breaking Down Fibrin Mesh
(1) Platelet Contraction
There’s a need to get rid of the clot
Platelet contraction is stimulated once the platelet plug is
o The clot may be big enough that it could occlude
anchored to injured vessel wall by fibrin mesh
blood flow and possibly cause ischemia
Platelets contains contractile proteins
o Actin and myosin7 Endothelium expresses protein Tissue Plasminogen
Activator (TPA)
When platelets contract, they pull the damaged edges of
TPA converts Plasminogen into Plasmin
the injured blood vessel close to each other
o Plasminogen is naturally occurring in the bloodstream
This squeezes some serum out of the injured vessel
(2) Platelet-Derived Growth Factor (PDGF) Secretion Plasmin breaks down Fibrin mesh into Fibrinogen and
If smooth muscle cells are damaged, PDGF triggers Fibrin degradation products like D-Dimer
mitosis or proliferation of smooth muscle cells o This process recanalizes the clotted vessel
Damage to connective tissue, PDGF forms connective (2) Clinical Significance
tissue patches to regenerate collagen fibers
TPA Drugs
(3) Vascular Endothelial Growth Factor (VEGF) o ↑Plasminogen to Plasmin
Secretion Increased rate of blood clot breakdown
Regenerates the new endothelial lining o Given to patient who have stroke or some type of
The blood vessel then starts to go through healing & ischemic attack within hours
remodeling Elevated D-Dimers can be indicative of blood clots and
inflammation
o Specific blood tests can be done to determine if
patient has had some type of clot formation
Antifibrinolytics (TXA)→↓Plasminogen to
plasmin→↓break down of blood clot and stabilizes clot
Figure 4 Clot Retraction
Figure 5 Fibrinolysis
4 of 6 HEMATOLOGY: Note #7 HEMOSTASIS: COAGULATION CASCADE
III) APPENDIX
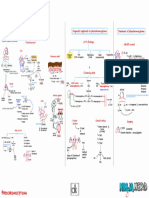
Figure 6. Summary of Hemostasis
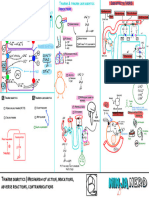
Figure 7. Coagulation Cascade
HEMOSTASIS: COAGULATION CASCADE HEMATOLOGY: Note #7. 5 of 6
IV) REVIEW QUESTIONS
1) Which is not a natural way of the body to prevent
blood from becoming thrombotic?
a) Heparin Sulfate
b) Nitric Oxide
c) Thromboxane
d) Prostacyclin
2) Which of the following is more stable?
a) Fibrinogen
b) Fibrin
c) They are equally stable
3) What is the third step of hemostasis?
a) Platelet Plug Formation
b) Coagulation Cascade
c) Vascular Spasm
d) Fibrinolysis
CHECK YOUR ANSWERS
V) REFRENCES
● Le T, Bhushan V, Sochat M, Chavda Y, Zureick A. First Aid for
the USMLE Step 1 2018. New York, NY: McGraw-Hill Medical; 2017
● Marieb EN, Hoehn K. Anatomy & Physiology. Hoboken, NJ:
Pearson; 2020.
● Boron WF, Boulpaep EL. Medical Physiology.; 2017.
● Urry LA, Cain ML, Wasserman SA, Minorsky PV, Orr RB,
Campbell NA. Campbell Biology. New York, NY: Pearson; 2020.
● Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL,
Loscalzo J. Harrison's Principles of Internal Medicine. New York
etc.: McGraw-Hill Education; 2018.
● Sabatine MS. Pocket Medicine: the Massachusetts General
Hospital Handbook of Internal Medicine. Philadelphia: Wolters
Kluwer; 2020
6 of 6 HEMATOLOGY: Note #7 HEMOSTASIS: COAGULATION CASCADE
You might also like
- Hemostasis, Surgical Bleeding and TransfusionDocument48 pagesHemostasis, Surgical Bleeding and Transfusionaddelins100% (1)
- Blood HemostasisDocument23 pagesBlood HemostasisSummaiya AdnanNo ratings yet
- 13 HemostasisDocument38 pages13 HemostasissiratelNo ratings yet
- Bleeding Disorders1Document81 pagesBleeding Disorders1DrMuskan AroraNo ratings yet
- Hemodynamic Disorders Part 1Document8 pagesHemodynamic Disorders Part 1م.م.زينة عبد الحسينNo ratings yet
- مستند PDF-3C57C64C1675-1Document15 pagesمستند PDF-3C57C64C1675-1lorenoh21No ratings yet
- Hema 2 - Prelim Topic 2 - Additional Notes Primary HemostasisDocument2 pagesHema 2 - Prelim Topic 2 - Additional Notes Primary HemostasisLowenstein JenzenNo ratings yet
- Blood Components and Function - Componentes Sanguíneos y Su FXDocument8 pagesBlood Components and Function - Componentes Sanguíneos y Su FXPaula SaenzNo ratings yet
- Hematology 364 - 371Document8 pagesHematology 364 - 371sami ullahNo ratings yet
- HRM Week 2 - Introduction 2020 - PrintDocument34 pagesHRM Week 2 - Introduction 2020 - PrintShiv SookunNo ratings yet
- 12 - Hemostasis 1Document21 pages12 - Hemostasis 1جووري جووري100% (1)
- HEMOSTASISDocument2 pagesHEMOSTASISVera June RañesesNo ratings yet
- Chapter 35 Part 1Document31 pagesChapter 35 Part 1Gordon JamesonNo ratings yet
- Hemostasis NoteDocument3 pagesHemostasis NoteThanh Hải LâmNo ratings yet
- Thrombosis and Embolism UPR 1Document45 pagesThrombosis and Embolism UPR 1Juan Ortega PutraNo ratings yet
- 1 Blood HemostasisDocument32 pages1 Blood Hemostasisarlinda noviana100% (2)
- Meningitis DifferentialsDocument20 pagesMeningitis DifferentialsJoherNo ratings yet
- Hemostasis and Platelet FunctionDocument17 pagesHemostasis and Platelet FunctionUzama Binu AliNo ratings yet
- Hemostasis and Blood CoagulationDocument9 pagesHemostasis and Blood CoagulationHans De GuzmanNo ratings yet
- Hema OmgDocument82 pagesHema OmgBernadeth BaduaNo ratings yet
- What Are The Components That Play A Role in Hemostatis? - Endhotelial CellsDocument7 pagesWhat Are The Components That Play A Role in Hemostatis? - Endhotelial CellsArmella AzzahraNo ratings yet
- Physio 2.05 Bloodphysiology2 HemostasisDocument9 pagesPhysio 2.05 Bloodphysiology2 HemostasisSimon Peter Familara100% (1)
- PLT & Heamostasis (Autosaved)Document35 pagesPLT & Heamostasis (Autosaved)Лариса ТкачеваNo ratings yet
- Normal Hemostasis: Dr. Ranjita Singh Department of Pathology Chitwan Medical CollegeDocument31 pagesNormal Hemostasis: Dr. Ranjita Singh Department of Pathology Chitwan Medical CollegeMohan Prasad GuptaNo ratings yet
- Lesson 24Document16 pagesLesson 24Anshika BhargavaNo ratings yet
- Hemostasis ThrombosisDocument18 pagesHemostasis ThrombosisHimani JhaNo ratings yet
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Document3 pagesPain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNo ratings yet
- Patho 26Document16 pagesPatho 26saddamixoNo ratings yet
- المحاضرة 5Document10 pagesالمحاضرة 5Shi no Me100% (1)
- Hematologi Pharmacolog: Hemostasis and Blood Coagulation CascadeDocument19 pagesHematologi Pharmacolog: Hemostasis and Blood Coagulation CascadeDivina ArenaNo ratings yet
- Hemostasis and Thrombosis: OutlineDocument11 pagesHemostasis and Thrombosis: OutlineManila MedNo ratings yet
- DIC (Dr. Dimas Bayu)Document48 pagesDIC (Dr. Dimas Bayu)Nur Muhammad KhatimNo ratings yet
- Biology of HemostasisDocument20 pagesBiology of HemostasisVeronica TomaselloNo ratings yet
- Physio - Chapter 37Document4 pagesPhysio - Chapter 37Regina Ysabel SartagudaNo ratings yet
- 716-Article Text-1804-1-10-20221028Document8 pages716-Article Text-1804-1-10-20221028Eka SilvieNo ratings yet
- HaemostasisDocument9 pagesHaemostasisLilyNo ratings yet
- Drugs That Influence CoagulationDocument2 pagesDrugs That Influence CoagulationRy AnneNo ratings yet
- 1.02 Hemostasis and CoagulationDocument4 pages1.02 Hemostasis and CoagulationShiena ArchividoNo ratings yet
- 4 6019258822663605181Document43 pages4 6019258822663605181zeyadmag2004No ratings yet
- Hemostasis Trombosis - Tiara Anggita Q.Document47 pagesHemostasis Trombosis - Tiara Anggita Q.tiara anggitaNo ratings yet
- Physiology of CoagulationDocument16 pagesPhysiology of CoagulationIlyas HalimNo ratings yet
- What Is HemostasisDocument5 pagesWhat Is HemostasissupahvyNo ratings yet
- Lecture - Platelet, Haemostasis - 2Document19 pagesLecture - Platelet, Haemostasis - 2eman el saeedNo ratings yet
- Learning ObjectivesDocument12 pagesLearning ObjectivesjmcvicenteNo ratings yet
- Lo Hemato Onco 3.1Document6 pagesLo Hemato Onco 3.1Sabrina AswanNo ratings yet
- Hematology: Components of The Blood FlowDocument2 pagesHematology: Components of The Blood FlowChristine BadilloNo ratings yet
- Chapter 1 Overview of IsDocument35 pagesChapter 1 Overview of IsNathalie PortugalNo ratings yet
- Clinpath-04.-Disorders of Hemostasis and Blood CoagulationDocument11 pagesClinpath-04.-Disorders of Hemostasis and Blood CoagulationCharisse Angelica MacedaNo ratings yet
- Thrombosis - NewDocument108 pagesThrombosis - NewheruNo ratings yet
- Thrombosis Response - 25 September 2023Document58 pagesThrombosis Response - 25 September 2023Ardian AshadiNo ratings yet
- Hematology AasignmentDocument3 pagesHematology AasignmentBAIGPRONo ratings yet
- Primary HemostasisDocument26 pagesPrimary HemostasisShameena KnNo ratings yet
- Coronary Thrombus: - Development - Classification - Fate - Clinical Presentation Therapeutic StrategiesDocument9 pagesCoronary Thrombus: - Development - Classification - Fate - Clinical Presentation Therapeutic StrategiesGCY56No ratings yet
- Aula Af 2 PDFDocument49 pagesAula Af 2 PDFtobiasmanuel179No ratings yet
- Coagulacion y FibrinolisisDocument22 pagesCoagulacion y FibrinolisisAngy MarsNo ratings yet
- HEMOSTASISDocument4 pagesHEMOSTASISLark CruiseNo ratings yet
- Normal HemostasisDocument34 pagesNormal Hemostasisمصطفي خندقاويNo ratings yet
- ThrombosisDocument13 pagesThrombosisAbigail ChristisnNo ratings yet
- Deep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edFrom EverandDeep Vein Thrombosis and Pulmonary Embolism: A guide for practitioners 2/edRating: 5 out of 5 stars5/5 (1)
- Endocrine Physiology) 15. Adrenal Medulla - Catecholamines - KeyDocument1 pageEndocrine Physiology) 15. Adrenal Medulla - Catecholamines - Keyhasanatiya41No ratings yet
- Neurology LectureDocument48 pagesNeurology Lecturehasanatiya41No ratings yet
- Reumato and EndocrineDocument106 pagesReumato and Endocrinehasanatiya41No ratings yet
- Hematology& Onco LectureDocument66 pagesHematology& Onco Lecturehasanatiya41No ratings yet
- Endocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)Document1 pageEndocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)hasanatiya41No ratings yet
- Endocrinology Pathology - 007) Cushing's Syndrome (Notes)Document7 pagesEndocrinology Pathology - 007) Cushing's Syndrome (Notes)hasanatiya41No ratings yet
- Inflammatory Arthritis Notes - Diagrams & Illustrations - OsmosisDocument15 pagesInflammatory Arthritis Notes - Diagrams & Illustrations - Osmosishasanatiya41No ratings yet
- CardiologyDocument43 pagesCardiologyhasanatiya41No ratings yet
- Orthopedic DisordersDocument15 pagesOrthopedic Disordershasanatiya41No ratings yet
- 010 - Cardiovascular Physiology) Cardiovascular Cardiac CycleDocument3 pages010 - Cardiovascular Physiology) Cardiovascular Cardiac Cyclehasanatiya41No ratings yet
- 057 - Endocrinology Physiology) OvulationDocument4 pages057 - Endocrinology Physiology) Ovulationhasanatiya41No ratings yet
- Development & Growth Nutrition & Behavioral DisordersDocument27 pagesDevelopment & Growth Nutrition & Behavioral Disordershasanatiya41No ratings yet
- Cardiovascular Pharmacology) 07 Calcium Channel Blockers - KeyDocument1 pageCardiovascular Pharmacology) 07 Calcium Channel Blockers - Keyhasanatiya41No ratings yet
- Malabsorption Conditions Notes - Diagrams & Illustrations - OsmosisDocument7 pagesMalabsorption Conditions Notes - Diagrams & Illustrations - Osmosishasanatiya41No ratings yet
- Pharmacology Basics - 016) Drugs For Heart Failure (Notes)Document25 pagesPharmacology Basics - 016) Drugs For Heart Failure (Notes)hasanatiya41No ratings yet
- Cardiovascular Pharmacology) 09 Thiazide Diuretics - KeyDocument1 pageCardiovascular Pharmacology) 09 Thiazide Diuretics - Keyhasanatiya41No ratings yet
- Pharmacology Basics - 016) Drugs For Heart Failure (Notes - Q&A)Document3 pagesPharmacology Basics - 016) Drugs For Heart Failure (Notes - Q&A)hasanatiya41No ratings yet
- Vasculitis PPT NotesDocument14 pagesVasculitis PPT Noteshasanatiya41No ratings yet
- Hematologic Infections Notes - Diagrams & Illustrations - OsmosisDocument6 pagesHematologic Infections Notes - Diagrams & Illustrations - Osmosishasanatiya41No ratings yet
- Cardiovascular Pharmacology) 03 Heparin - KeyDocument1 pageCardiovascular Pharmacology) 03 Heparin - Keyhasanatiya41No ratings yet
- Plasma Cell Dyscrasias Notes - Diagrams & Illustrations - OsmosisDocument6 pagesPlasma Cell Dyscrasias Notes - Diagrams & Illustrations - Osmosishasanatiya41No ratings yet
- Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)Document1 pageHematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)hasanatiya41No ratings yet
- Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)Document11 pagesHematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)hasanatiya41No ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)Document8 pagesHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)hasanatiya41No ratings yet
- Hematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)Document1 pageHematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)hasanatiya41No ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)Document1 pageHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)hasanatiya41No ratings yet
- 342 - Hematology Physiology) Erythropoiesis Red Blood Cell FormationDocument6 pages342 - Hematology Physiology) Erythropoiesis Red Blood Cell Formationhasanatiya41No ratings yet
- Meeting1 Lec1Document73 pagesMeeting1 Lec1hasanatiya41No ratings yet
- Hematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Notes)Document8 pagesHematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Notes)hasanatiya41No ratings yet
- A Comparison Study of Routine Coagulation Screening Tests (PT and APTT) by Three Automated Coagulation AnalyzersDocument6 pagesA Comparison Study of Routine Coagulation Screening Tests (PT and APTT) by Three Automated Coagulation AnalyzersRahadian FaisalNo ratings yet
- Analisis Kuantitatif Fraksi-Fraksi Protein Dalam PlasmaDocument11 pagesAnalisis Kuantitatif Fraksi-Fraksi Protein Dalam PlasmaPuguh 'pugn' NoviarsitoNo ratings yet
- Overview of The Coagulation SystemDocument9 pagesOverview of The Coagulation SystemaksinuNo ratings yet
- HemostasisDocument48 pagesHemostasisBintang Ruth Cecilia FebrinaNo ratings yet
- L2-SURG-Hemostasis, Surgical Bleeding, - Transfusion (Aug2521)Document8 pagesL2-SURG-Hemostasis, Surgical Bleeding, - Transfusion (Aug2521)Marc Lyndon CafinoNo ratings yet
- Hemostasis ReviewerDocument14 pagesHemostasis ReviewerDayledaniel SorvetoNo ratings yet
- Basic Concepts Of: HemophiliaDocument2 pagesBasic Concepts Of: Hemophiliaapi-265604636No ratings yet
- Bleeding Disorders: Drg. Gita Dwi Jiwanda Sovira, M.KesDocument26 pagesBleeding Disorders: Drg. Gita Dwi Jiwanda Sovira, M.KessaskiakonitaNo ratings yet
- Disseminated Intravascular Coagulation Concept MapDocument3 pagesDisseminated Intravascular Coagulation Concept MapphoebjaetanNo ratings yet
- Inserto Fibrinogeno CDocument3 pagesInserto Fibrinogeno CCaro ErazoNo ratings yet
- HaemophiliaDocument38 pagesHaemophiliaAqmal Henderson HamzaNo ratings yet
- HaemophiliaDocument15 pagesHaemophiliaSanmuga VimalanathanNo ratings yet
- Blood CoagulationDocument8 pagesBlood CoagulationJaslir MendozaNo ratings yet
- Pemeriksaan Retraksi Bekuan Dan Pengukuran Masa Lisis BekuanDocument18 pagesPemeriksaan Retraksi Bekuan Dan Pengukuran Masa Lisis BekuanHery StiawanNo ratings yet
- Coagulation and HemostasisDocument72 pagesCoagulation and HemostasisBiniyam AsratNo ratings yet
- CoagulopathyDocument121 pagesCoagulopathyMegat Mohd Azman AdzmiNo ratings yet
- Clot RetractionDocument18 pagesClot RetractionLA ManalangNo ratings yet
- Nilai Normal Laboratorium Patologi KlinikDocument4 pagesNilai Normal Laboratorium Patologi KlinikHarwento Eka putraNo ratings yet
- Erba Protime LSDocument2 pagesErba Protime LSthinh.ho2No ratings yet
- Time RetractionDocument4 pagesTime RetractionVIVA, Trisha Anne L.No ratings yet
- Hemostasis in The NeonateDocument15 pagesHemostasis in The NeonateAdeNo ratings yet
- 3 4Document2 pages3 4cherryNo ratings yet
- 38 - HypofibrinogenaemiaDocument8 pages38 - Hypofibrinogenaemiadr_asalehNo ratings yet
- Hema 2Document35 pagesHema 2Angela ReyesNo ratings yet
- Artikel Jurnal IbnuDocument4 pagesArtikel Jurnal Ibnuibnu rifaldiNo ratings yet
- 3.1 HaemostasisDocument53 pages3.1 HaemostasisFarnida Jamhal100% (1)
- HemophiliaDocument3 pagesHemophiliaMuthoni NdongaNo ratings yet
- PBL BleedingDocument11 pagesPBL BleedingMuhammad FakhriNo ratings yet
- CTBTDocument45 pagesCTBTimpi belindaNo ratings yet