Professional Documents
Culture Documents
PBL Case 1
PBL Case 1
Uploaded by
Saladin AbrahimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PBL Case 1
PBL Case 1
Uploaded by
Saladin AbrahimCopyright:
Available Formats
Patient Information
Patient name ………. Belachew abebaw
Age……………………60 yrs
Sex ……………………male
Address ……………….
Site of visit………….Emergency OPD
Date------------------26/12/2015E.C
Presenting problems:
After arriving at, Emergency OPD, at 6:00 AM, Ato Belachew complains nausea
and vomiting for 3 days duration
Discussion question 1
1. List ato Belachew’s problems
2. Define your hypothesizes
3. Which systems might be involved and describe the mechanisms leading to
the problems
4. What aspects of history would you want to ask that help you to test your
hypothesizes?
History of present illness
After arriving at Hospital, Emergency OPD at 6:00 AM local time, ato BelAchew
said that “ I have been Developing persistent nausea and vomiting since the last
three days.’’
He has also headache, intermittent seizure and loss of appetite.
There was no any management given before he comes to hospital.
Past medical history_ previously, he was treated for UTI two months ago.
Family history- He has no family history of DM, HTN or similar problems.
Personal and social history-he has good interaction with with his families and
neighbours.
ROS:
GIT- No other pertinent data
GUT- small amount of urine
Discussion question 2
1. Summarize the new information you obtained. How does these new
information contribute to your hypothesis or suggest new hypothesis?
2. What pertinent data would you expect on physical examination? How does
it help you to rerank your hypothesis?
Physical examination:
General appearance – Acute sick looking
Vital sign: BP 150/100mmHg, PR 96 bpm, RR 32 bpm, Temp 35.7
HEENT- pink conjunctiva but there is some degree of facial edema
LGS – No any enlarged lymph node.
-No lesion and no palpable mass
RS – Chest is clear and resonant
CVS- s1 and s2 well heard
-No murmur no gallop
Abdomen – No abdominal tenderness and no palpable mass. He has
nausea,vomiting and loss of appetite for days.
MSS: There is some degree of extremity edema.
IGS – There is slow capillary refill time.
GUT – There is CVA tenderness, dysuria and decreased urine output
(approximately 300ml/24hrs).
CNS – Lethargic, seizure
Discussion question 3
1. How does the physical examination help you?
2. Do you want to change the ranking order of the hypothesis based on the
physical examination? How?
3. What investigations would you request to test your hypotheses?
Laboratory Investigations and results:
RFT: Creatinine: 1.4 mg/dl Normal value:0.6_1.02mg/dl
BUN: 27 mg/dl Normal value: 10_20 mg/dl
WBC:10,500/mm3 Normal value:5,000_10,000/mm3
Hgb: 12mg/dl Normal value:10_14m g/dl
Urine analysis: many RBC/HPF, +4 protein
Discussion question 4
1. Interpret test results and re-evaluate your hypotheses.
2. Based on your hypotheses, what medical and nursing interventions do you consider for
Belachew?
3. How would you counsel his family?
You might also like
- Abnormal Psychology An Integrative Approach, 7th EdDocument32 pagesAbnormal Psychology An Integrative Approach, 7th EdSalome GogolauriNo ratings yet
- AMC Clinical Sample QuestionsDocument20 pagesAMC Clinical Sample Questionslaroya_31No ratings yet
- Coronary Artery Diseases Case StudyDocument20 pagesCoronary Artery Diseases Case StudyPyka Izzaty75% (4)
- ENT McqsDocument15 pagesENT McqsSajjad Ahmad93% (14)
- Nursing Care Plan For Cataract Nursing AssessmentDocument2 pagesNursing Care Plan For Cataract Nursing AssessmentMicky Zelia100% (3)
- Family Medicine OSCEDocument195 pagesFamily Medicine OSCEBasmanMarkus93% (14)
- Gi PBLDocument5 pagesGi PBLSaladin AbrahimNo ratings yet
- Adl 2006 Sep 23Document18 pagesAdl 2006 Sep 23ZweNo ratings yet
- A Case of Abdominal PainDocument10 pagesA Case of Abdominal PainJiregna TeshomeNo ratings yet
- Past Paper (No Answer)Document170 pagesPast Paper (No Answer)Hariharan NarendranNo ratings yet
- Health HX Form-Patient KBDocument7 pagesHealth HX Form-Patient KBChandra MuraliNo ratings yet
- OSCE Melb11Nov06Document7 pagesOSCE Melb11Nov06janaka1022No ratings yet
- Pulse: Slightly Thin and Deep On Left, Weak Lung and Spleen. Stronger On Left. Slippery Both Sides. DiagnosisDocument9 pagesPulse: Slightly Thin and Deep On Left, Weak Lung and Spleen. Stronger On Left. Slippery Both Sides. DiagnosisHui YingNo ratings yet
- Case PresentationDocument31 pagesCase PresentationArsalan NadeemNo ratings yet
- Paediatric Gastroenteritis Case StudiesDocument3 pagesPaediatric Gastroenteritis Case StudiesJohnrey DadorNo ratings yet
- AssignmentDocument3 pagesAssignmentracheljennifer540No ratings yet
- Case 1Document3 pagesCase 1איתי עוזרNo ratings yet
- Confused New StationsDocument10 pagesConfused New StationsSomchai PtNo ratings yet
- Morning Report Case: 17th Dec 2013Document22 pagesMorning Report Case: 17th Dec 2013SunardiasihNo ratings yet
- Dengue Case PresDocument49 pagesDengue Case PresDee SarajanNo ratings yet
- Amc Question Bank ClinicalsDocument36 pagesAmc Question Bank ClinicalsSoumen Dutt100% (1)
- Name: Vijayakumar Prabha AnubhaDocument3 pagesName: Vijayakumar Prabha Anubharacheljennifer540No ratings yet
- Surg Week 4Document75 pagesSurg Week 4Casey YanoNo ratings yet
- UGIB CwuDocument2 pagesUGIB CwuTiong NeeNo ratings yet
- Nusing Care Plan 2Document2 pagesNusing Care Plan 2Chona FontanillaNo ratings yet
- CWU - AnaestiologyDocument8 pagesCWU - AnaestiologyAmbhi GanaNo ratings yet
- A Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaDocument34 pagesA Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaJobaer MahmudNo ratings yet
- CFGVDocument28 pagesCFGVmyolie wuNo ratings yet
- Anamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoDocument25 pagesAnamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoTebeNo ratings yet
- ICU (Case 2)Document12 pagesICU (Case 2)arsala.siddiqui305No ratings yet
- GI Case Studies-StudentDocument7 pagesGI Case Studies-StudentRhina FutrellNo ratings yet
- Case PresentationDocument10 pagesCase PresentationnmreaperNo ratings yet
- SGH How To Approach SBAsDocument49 pagesSGH How To Approach SBAsArnav RaiNo ratings yet
- TCM Case Work-Up: Categories (Include A Diagnosis For Each MC/SC)Document9 pagesTCM Case Work-Up: Categories (Include A Diagnosis For Each MC/SC)Hui YingNo ratings yet
- PUD A Case StudyDocument1 pagePUD A Case StudyDonna BellaNo ratings yet
- A-G IbmsDocument4 pagesA-G IbmsAubrey Unique EvangelistaNo ratings yet
- English GaneshaaDocument17 pagesEnglish GaneshaaYudha MaharajNo ratings yet
- Wa0001.Document33 pagesWa0001.kmstt780No ratings yet
- Wa0008.Document14 pagesWa0008.Mahendra NitharwalNo ratings yet
- Bleeding Per Rectum 2: DR - Ahmed AlbasiounyDocument19 pagesBleeding Per Rectum 2: DR - Ahmed AlbasiounyAhmed AfashNo ratings yet
- YL3 GI End of Module Activity Complex Task - StudentsDocument1 pageYL3 GI End of Module Activity Complex Task - StudentsAnonymous Xlpj86laNo ratings yet
- Hypokalemic Periodic ParalysisDocument54 pagesHypokalemic Periodic Paralysislordgoncar100% (1)
- Case Presentation 1Document92 pagesCase Presentation 1Mona MohammadNo ratings yet
- HUEC 2011 Cardio Case StudiesDocument6 pagesHUEC 2011 Cardio Case StudiesShanica Paul-RichardsNo ratings yet
- Nursing DocumentationDocument8 pagesNursing DocumentationRina FSNo ratings yet
- Report Sample I Check Diagnostic SystemDocument11 pagesReport Sample I Check Diagnostic SystemssmaddiNo ratings yet
- PCC CaseDocument9 pagesPCC CaseKaila AbeledaNo ratings yet
- Subjective Data Includes Everything You Patient Tells You!Document4 pagesSubjective Data Includes Everything You Patient Tells You!Tahani AliNo ratings yet
- Recall 145, Sum 6.4.13AMC CLINICALDocument19 pagesRecall 145, Sum 6.4.13AMC CLINICALAMMARANo ratings yet
- Mortality Presentation For Gi Unit Feb 2023Document34 pagesMortality Presentation For Gi Unit Feb 2023nkamiabam2No ratings yet
- Reviewer Board ExamDocument10 pagesReviewer Board ExamKristen Villacarlos86% (7)
- Case Presentation: Abuana Chiong Jagorin Macasa Maruhom Minguito Morata Taneza Tan VillacinDocument53 pagesCase Presentation: Abuana Chiong Jagorin Macasa Maruhom Minguito Morata Taneza Tan VillacinStephanie ChiongNo ratings yet
- Medical Error - Missed MIDocument3 pagesMedical Error - Missed MIDfaid NGNo ratings yet
- Soal Soal WorkshopDocument28 pagesSoal Soal Workshopkes25251No ratings yet
- Soal Soal WorkshopDocument28 pagesSoal Soal WorkshopJuliansyah EfrikoNo ratings yet
- BrisDocument9 pagesBrisYwagar YwagarNo ratings yet
- Morning Report Bedah - 17 November 2017Document18 pagesMorning Report Bedah - 17 November 2017bosstogarNo ratings yet
- Case - IUFDDocument5 pagesCase - IUFDMaris Sarline OpenianoNo ratings yet
- Station 2 and 4 Diet 1 2023 Updated VersionDocument9 pagesStation 2 and 4 Diet 1 2023 Updated VersionThanthanhla94 ThanNo ratings yet
- Summary of Data BaseDocument10 pagesSummary of Data BaseResti Puteri ApriyuslimNo ratings yet
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- No Guts, No Glory: Gut Solution - The Core of Your Total Wellness PlanFrom EverandNo Guts, No Glory: Gut Solution - The Core of Your Total Wellness PlanRating: 3.5 out of 5 stars3.5/5 (2)
- This Is A New Doc Very NewDocument6 pagesThis Is A New Doc Very NewhusseinNo ratings yet
- Compartment SyndromeDocument21 pagesCompartment SyndromeIzaac JdevNo ratings yet
- Chronic Obstructive Pulmonary Disease: A Case Presentation OnDocument95 pagesChronic Obstructive Pulmonary Disease: A Case Presentation OnJunery Bagunas100% (2)
- MEFENAMIC-ACID-mefenamic Acid Caps Ule Sciele Pharma IncDocument14 pagesMEFENAMIC-ACID-mefenamic Acid Caps Ule Sciele Pharma IncIrma DamayantiNo ratings yet
- Open Fracture Tibia Fibula FixDocument42 pagesOpen Fracture Tibia Fibula Fixannisaoktoviani100% (1)
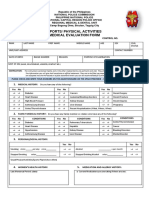
- Pre Medical Evaluatiom Form PFT 1 PDFDocument2 pagesPre Medical Evaluatiom Form PFT 1 PDFAIEN WENDELEIH Q. CAPINPIN100% (2)
- Korsakoff's SyndromeDocument5 pagesKorsakoff's SyndromeburnnotetestNo ratings yet
- Physical Therapy For Cardiopumonary DisordersDocument101 pagesPhysical Therapy For Cardiopumonary Disorderssunita_h100% (5)
- UntitledDocument16 pagesUntitledSucharita RayNo ratings yet
- Bulimia NervosaDocument13 pagesBulimia Nervosaemlyn_lanonNo ratings yet
- Anorectal Anatomy & Surgical ManagementDocument164 pagesAnorectal Anatomy & Surgical Managementsgod34No ratings yet
- PacemakersDocument69 pagesPacemakersdocjeevan89100% (1)
- Targeting TAM Marco To Reprogram Macrophage in Cancer Cell 2016Document13 pagesTargeting TAM Marco To Reprogram Macrophage in Cancer Cell 2016Kudelko MatNo ratings yet
- Types of AnemiaDocument6 pagesTypes of AnemiaSittieNo ratings yet
- Communication Concepts in Administering Intra Cutaneous DrugsDocument2 pagesCommunication Concepts in Administering Intra Cutaneous DrugsNayla FerdianaNo ratings yet
- English Practice 62: I. PronunciationDocument9 pagesEnglish Practice 62: I. PronunciationLe QuocNo ratings yet
- Lumbar Radiculopathy Medback Castillo Mendez EDITEDDocument12 pagesLumbar Radiculopathy Medback Castillo Mendez EDITEDSteve ColbertNo ratings yet
- NDT Lab - Finals (Transes)Document19 pagesNDT Lab - Finals (Transes)Aleah JayaganNo ratings yet
- RBC&WBC AbnormalitiesDocument10 pagesRBC&WBC AbnormalitiesDeomicah SolanoNo ratings yet
- Hiv NotesDocument6 pagesHiv NotesMartin De Haro GarciaNo ratings yet
- Imperforate AnusDocument52 pagesImperforate Anushayssam rashwan100% (6)
- Trichuris TrichiuraDocument3 pagesTrichuris TrichiuraTwish BeraldeNo ratings yet
- Physical Examination of The Critically Injured AthleteDocument25 pagesPhysical Examination of The Critically Injured Athletebrida.bluesNo ratings yet
- Resource-Manual OB WARDDocument3 pagesResource-Manual OB WARDHarvey Lampa SelimNo ratings yet
- Gentner Expo Poster - Leah GentnerDocument1 pageGentner Expo Poster - Leah GentnernurjNo ratings yet
- HPE 113X - First Aid (Choking)Document6 pagesHPE 113X - First Aid (Choking)Doreen MasikaNo ratings yet