Professional Documents
Culture Documents
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Uploaded by
muh.andyjaya.mdCopyright:
Available Formats
You might also like
- 4 Stages of Cirrhosis of The Liver 18 Symptoms, CDocument9 pages4 Stages of Cirrhosis of The Liver 18 Symptoms, CRammy KhanNo ratings yet
- Bowel Elimination Answer - 1Document3 pagesBowel Elimination Answer - 1June Dumdumaya100% (2)
- MCQ in Pediatric SurgeryDocument6 pagesMCQ in Pediatric SurgeryPatrycjaSkierka50% (2)
- Fibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleDocument3 pagesFibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleIKIKIKIKIKI999999No ratings yet
- It Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaDocument5 pagesIt Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaIJAR JOURNALNo ratings yet
- Storch 2007Document3 pagesStorch 2007PNo ratings yet
- Akiyama Case ReportDocument3 pagesAkiyama Case ReportApmc SchwartzNo ratings yet
- 2020 Paper SplenicDocument5 pages2020 Paper SplenicLauburu CrossNo ratings yet
- Aresia de Vias Biliares UltrasonidoDocument14 pagesAresia de Vias Biliares UltrasonidoArturo GarciaNo ratings yet
- Revisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsDocument26 pagesRevisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsArturo García MarquezNo ratings yet
- International Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseDocument4 pagesInternational Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseTegoeh RizkiNo ratings yet
- Literature Review of Liver AbscessDocument4 pagesLiterature Review of Liver Abscessc5ng67v1100% (1)
- Hepatocellular Carcinoma - Diagnosis and TreatmentDocument46 pagesHepatocellular Carcinoma - Diagnosis and TreatmentSigh BalaNo ratings yet
- A Rare Case of Colon Cancer in A Young Patient: A Case Report and Literature ReviewDocument5 pagesA Rare Case of Colon Cancer in A Young Patient: A Case Report and Literature ReviewIJAR JOURNALNo ratings yet
- Recurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureDocument5 pagesRecurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureVika RatuNo ratings yet
- GB Cancer - Radiologic-Pathologic CorrelationDocument20 pagesGB Cancer - Radiologic-Pathologic CorrelationSamuel WidjajaNo ratings yet
- Evaluation of Focal Hepatic Lesions by Using Ultrasound EvaluationDocument2 pagesEvaluation of Focal Hepatic Lesions by Using Ultrasound EvaluationNaufal LutfiNo ratings yet
- Accuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureDocument4 pagesAccuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureAnasriNstNo ratings yet
- 1 s2.0 S2210261222001894 MainDocument5 pages1 s2.0 S2210261222001894 Mainkiki tuanaya1No ratings yet
- Incidental Gallbladder Cancer. Residual Cancer Discovered at Oncologic Extended Resection Determines Outcome. A Report From High - and Low-IncidencDocument10 pagesIncidental Gallbladder Cancer. Residual Cancer Discovered at Oncologic Extended Resection Determines Outcome. A Report From High - and Low-IncidencCarlos SotoNo ratings yet
- Ce 48 291Document6 pagesCe 48 291Siska HarapanNo ratings yet
- Ojped 2024030813565746Document6 pagesOjped 2024030813565746Nicolás Mosso F.No ratings yet
- Unexplained Ascites, A Sign For Neuroendocrine Carcinoma: Case ReportDocument3 pagesUnexplained Ascites, A Sign For Neuroendocrine Carcinoma: Case ReportsandzatNo ratings yet
- Liver Abscess DissertationDocument4 pagesLiver Abscess DissertationPayForAPaperAtlanta100% (1)
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Sonography First-Line Modality in Diagnosis of Acute Colonic Diverticulitis 2013Document6 pagesSonography First-Line Modality in Diagnosis of Acute Colonic Diverticulitis 2013waldemar russellNo ratings yet
- Choledochal CystDocument14 pagesCholedochal CystIndah SolehaNo ratings yet
- Primary Congenital Choledochal Cyst With Squamous Cell Carcinoma: A Case ReportDocument6 pagesPrimary Congenital Choledochal Cyst With Squamous Cell Carcinoma: A Case ReportRais KhairuddinNo ratings yet
- Differentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and ManagementDocument9 pagesDifferentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and ManagementMayerlin CalvacheNo ratings yet
- en Papilla Vaters Tumor in Elderly An InterDocument5 pagesen Papilla Vaters Tumor in Elderly An InterAyip Bahsan AlBantaniNo ratings yet
- Rare Small Bowel Carcinoid Tumor A Case ReportDocument5 pagesRare Small Bowel Carcinoid Tumor A Case ReportAthenaeum Scientific PublishersNo ratings yet
- 1 s2.0 S1015958422013677 MainDocument5 pages1 s2.0 S1015958422013677 MainMohammed S. FoulaNo ratings yet
- Metastatic Spread of Primary Lung Adenocarcino - 2024 - International Journal ofDocument5 pagesMetastatic Spread of Primary Lung Adenocarcino - 2024 - International Journal ofRonald QuezadaNo ratings yet
- Pancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyDocument4 pagesPancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyMolla WariNo ratings yet
- Unusual Presentation of Lung Cancer A Case ReportDocument3 pagesUnusual Presentation of Lung Cancer A Case Reportariza0% (1)
- A Randomized Controlled Trial of Emergency Treatment of Bleeding Esophageal Varices in Cirrhosis For Hepatocellular CarcinomaDocument15 pagesA Randomized Controlled Trial of Emergency Treatment of Bleeding Esophageal Varices in Cirrhosis For Hepatocellular CarcinomaAntonius SimangunsongNo ratings yet
- 260-Article Text-875-1-10-20220728Document4 pages260-Article Text-875-1-10-20220728hasan andrianNo ratings yet
- Diagnostic Imaging Pathways ArticleDocument10 pagesDiagnostic Imaging Pathways ArticleSuhayatra PutraNo ratings yet
- Esophageal Cancer: Diagnosis and Management: Ai Zheng Aizheng Chinese Journal of Cancer October 2010Document13 pagesEsophageal Cancer: Diagnosis and Management: Ai Zheng Aizheng Chinese Journal of Cancer October 2010Al VlaovicNo ratings yet
- 54 Raviswami EtalDocument3 pages54 Raviswami EtaleditorijmrhsNo ratings yet
- Ajol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309Document2 pagesAjol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309alysNo ratings yet
- 5 Advanced Ultrasound TechniquesDocument7 pages5 Advanced Ultrasound Techniquesjefaturaimagenologia Hospital NogalarNo ratings yet
- Gallbladdercancer: Diagnosis, Surgical Management, and Adjuvant TherapiesDocument19 pagesGallbladdercancer: Diagnosis, Surgical Management, and Adjuvant Therapiesmyat252No ratings yet
- Management of Incidentally Detected Gallbladder Polyps Society of Radiologists in Ultrasound Consensus Conference RecommendationsDocument13 pagesManagement of Incidentally Detected Gallbladder Polyps Society of Radiologists in Ultrasound Consensus Conference RecommendationsYasser Farouk Sevilla HernandezNo ratings yet
- 492 568 1 SMnjsjsdjsDocument4 pages492 568 1 SMnjsjsdjsZidna MazayatulNo ratings yet
- International Journal of Infectious Diseases: Anshuman Pandey, Shakeel Masood, Namrata P. AwasthiDocument3 pagesInternational Journal of Infectious Diseases: Anshuman Pandey, Shakeel Masood, Namrata P. Awasthijohanna monsalveNo ratings yet
- Initial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsDocument33 pagesInitial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsClaudia YalanNo ratings yet
- R Azumi Lava 2014Document12 pagesR Azumi Lava 2014limbert manuelNo ratings yet
- Esophageal Composite Tumor With Neuroendocrine Component: A Rare EntityDocument4 pagesEsophageal Composite Tumor With Neuroendocrine Component: A Rare EntityIJAR JOURNALNo ratings yet
- Kanyongo's CardioDocument21 pagesKanyongo's CardioHuram SeremaniNo ratings yet
- SECTION I Inflammatory, Infective, and Congenital: Pyogenic Liver AbscessDocument12 pagesSECTION I Inflammatory, Infective, and Congenital: Pyogenic Liver AbscessandresNo ratings yet
- Neuroendocrine Tumors Dr. WarsinggihDocument20 pagesNeuroendocrine Tumors Dr. WarsinggihAndi Eka Putra PerdanaNo ratings yet
- Kuipersetal CRC NRDP2015Document26 pagesKuipersetal CRC NRDP2015Robert ChristevenNo ratings yet
- Case Report 1676563639Document6 pagesCase Report 1676563639noah jemedafeNo ratings yet
- Primary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportDocument4 pagesPrimary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportGeorge CiorogarNo ratings yet
- Modern Imaging in Obstructive JaundiceDocument4 pagesModern Imaging in Obstructive JaundicedanaogreanuNo ratings yet
- Histopathology of Hepatocellular CarcinomaDocument11 pagesHistopathology of Hepatocellular CarcinomaCindy Sabina FaleandraNo ratings yet
- Aproximación Multidisciplinaria Al Diagnóstico y Tratamiento de La Obs Intestinal 2018Document124 pagesAproximación Multidisciplinaria Al Diagnóstico y Tratamiento de La Obs Intestinal 2018Jorge Nuñez LucicNo ratings yet
- cLINICAL PRACTICE GUIDELINESDocument7 pagescLINICAL PRACTICE GUIDELINESdrmolinammNo ratings yet
- Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy For Pseudomyxoma Peritonei in A Liver-Transplanted Patient: A Case ReportDocument5 pagesCytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy For Pseudomyxoma Peritonei in A Liver-Transplanted Patient: A Case Reportyerich septaNo ratings yet
- An Unusual Cause of Acute Abdomend Gas-Forming Liver Abscess Due To Salmonella EnteritidisDocument4 pagesAn Unusual Cause of Acute Abdomend Gas-Forming Liver Abscess Due To Salmonella EnteritidisMenda JangWooyoung SooyoungsterNo ratings yet
- Imaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesFrom EverandImaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesNo ratings yet
- Fast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesFrom EverandFast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesNo ratings yet
- 5 - Gastrointestinal Bleeding (AMBOSS) ?Document6 pages5 - Gastrointestinal Bleeding (AMBOSS) ?Rawabi rawabi1997No ratings yet
- Swasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurDocument26 pagesSwasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurCyber MagicNo ratings yet
- Digestive SystemDocument7 pagesDigestive SystemKirsten CruzadoNo ratings yet
- Enema Final Lesson Plan PDFDocument17 pagesEnema Final Lesson Plan PDFRahul Damor88% (8)
- Mainz II Surgery IllustratedDocument25 pagesMainz II Surgery IllustratedPurvi Parikh100% (1)
- Acute AbdomenDocument60 pagesAcute AbdomenAnish DhamiNo ratings yet
- ProctopexyDocument6 pagesProctopexydrnareshkumar3281No ratings yet
- Class 7, CH 2 Nutrition in AnimalsDocument4 pagesClass 7, CH 2 Nutrition in AnimalsAkkshara Kashyap 7-HNo ratings yet
- Gastric Fluid Analysis NotesDocument2 pagesGastric Fluid Analysis NotesanonacadsNo ratings yet
- L7 - Gastric - Duodenal SecretionsDocument6 pagesL7 - Gastric - Duodenal SecretionsBig Daddy YoNo ratings yet
- Med Surg: GI - Gastrointestinal: PathophysiologyDocument1 pageMed Surg: GI - Gastrointestinal: PathophysiologyTori RolandNo ratings yet
- Fecal IncontinenceDocument5 pagesFecal IncontinenceDaniel Galindo SotomayorNo ratings yet
- Profil Penderita CBDDocument12 pagesProfil Penderita CBDVandra PrinosaNo ratings yet
- Bio4 4Document14 pagesBio4 4Nomap makNo ratings yet
- Interpretation of Liver Function TestsDocument14 pagesInterpretation of Liver Function TestsNirav SharmaNo ratings yet
- Portal Hypertensive Gastropathy - UpToDateDocument27 pagesPortal Hypertensive Gastropathy - UpToDatebagir_dm10No ratings yet
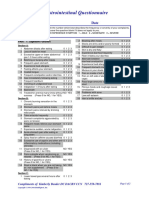
- Gastrointestional QuestionnaireDocument2 pagesGastrointestional QuestionnaireEva SabillaNo ratings yet
- Multiple-Choice Questionnaire: Functional Pelvic Floor ImagingDocument3 pagesMultiple-Choice Questionnaire: Functional Pelvic Floor Imagingtesfaye mekonnenNo ratings yet
- Surgery For Finals 2010Document58 pagesSurgery For Finals 2010Kay Bristol100% (1)
- Human Digestive SystemDocument19 pagesHuman Digestive SystemsyagitaNo ratings yet
- Reflexes in The GutDocument2 pagesReflexes in The GutJeffrey TseNo ratings yet
- Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr Solution ManualDocument9 pagesAdvanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr Solution Manualjames100% (28)
- Management of Obstructive Jaundice Exper PDFDocument3 pagesManagement of Obstructive Jaundice Exper PDFgustianto hutama pNo ratings yet
- Announcement SGU 2021Document10 pagesAnnouncement SGU 2021ceciliaNo ratings yet
- Summary of Digestion: C. Gastrointestinal Hormones 1. GastrinDocument5 pagesSummary of Digestion: C. Gastrointestinal Hormones 1. GastrinIrish Eunice FelixNo ratings yet
- Pancreatic Pseudocyst 2Document37 pagesPancreatic Pseudocyst 2AzharUlHassanQureshi100% (1)
- PancreasDocument11 pagesPancreasCheng XinvennNo ratings yet
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Uploaded by
muh.andyjaya.mdOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Gallbladder Carcinoma, The Difficulty of Early Detection - A Case Report
Uploaded by
muh.andyjaya.mdCopyright:
Available Formats
Open Access Case
Report DOI: 10.7759/cureus.493
Gallbladder Carcinoma, the Difficulty of
Early Detection: A Case Report
Andrew E. Graff 1 , Stephen L. Lewis 1 , Jonathan R. Bear 1 , David C. Van Echo 2 , Hugh M.
Dainer 3
1. Radiation Oncology, Walter Reed National Military Medical Center 2. Hematology/Oncology, Walter
Reed National Military Medical Center 3. Diagnostic Radiology, Walter Reed National Military Medical
Center/Uniformed Services University of Health Sciences
Corresponding author: Andrew E. Graff, zxga@yahoo.com
Disclosures can be found in Additional Information at the end of the article
Abstract
Gallbladder carcinoma (GBC) is an uncommon malignancy with a high mortality rate. Detecting
gallbladder carcinoma in its early stages can be difficult, despite improvements in
ultrasound and computed tomography (CT) imaging. Most diagnoses of GBC are made at
advanced stages, with the majority being found incidentally during surgery for
cholelithiasis. The presented case demonstrates the difficulty of diagnosing GBC preoperatively
in its early stages.
Categories: Medical Education, Oncology, Radiology
Keywords: gallbladder, gallbladder cancer, carcinoma, cancer, cholecystectomy, gallbladder carcinoma
Introduction
Gallbladder carcinoma (GBC) is a rare malignancy, but the most common malignancy of the
biliary tract. The incidence of GBC in the US is 1.2 per 100,000. The majority of gallbladder
carcinomas are diagnosed incidentally, usually when exploring for cholelithiasis [1]. Most
diagnoses of GBC are made at advanced stages and have been associated with poor outcomes
[2]. Several risk factors have been identified for GBC. The leading risk factors include female
gender, cholelithiasis, and advancing age. Gallbladder polyps, porcelain gallbladder, congenital
biliary cysts, abnormal pancreaticobiliary duct junction, and carcinogen exposure have all been
associated with GBC. Additional reported risk factors include smoking, obesity, diabetes,
chronic infections (Salmonella, Helicobacter), and medications (such as methyldopa, OCPs,
isoniazid, and estrogen) [3-5]. Herein, we present a case of locally advanced GBC with node-
positive disease found during laparoscopy for acute cholecystitis.
Received 01/13/2016
Review began 01/22/2016 Case Presentation
Review ended 02/01/2016
Published 02/12/2016 A 65-year-old obese, African-American female with a history of hyperlipidemia presented to
her primary care physician (PCP) in May 2013 for right neck pain radiating to her right shoulder
© Copyright 2016
for several weeks. The patient's initial blood work revealed an elevation in her liver enzymes;
Graff et al. This is an open access
article distributed under the terms of otherwise, all other lab results were normal. Additionally, a right upper quadrant (RUQ)
the Creative Commons Attribution ultrasound was performed which demonstrated probable gallbladder sludge and stones, with
License CC-BY 3.0., which permits a low likelihood of being polyps or gallbladder neoplasm given the absence of discrete
unrestricted use, distribution, and
vascularity (Figures 1, 2).
reproduction in any medium,
provided the original author and
source are credited.
How to cite this article
Graff A E, Lewis S L, Bear J R, et al. (February 12, 2016) Gallbladder Carcinoma, the Difficulty of Early
Detection: A Case Report. Cureus 8(2): e493. DOI 10.7759/cureus.493
FIGURE 1: Initial right upper quadrant ultrasound.
The image demonstrates intraluminal hypoechoic (red arrow) material. Given the appearance
and lack of discrete internal flow, it appears to be most likely due to gallstones or tumefactive
sludge, which is a benign mimic of a neoplasm.
FIGURE 2: Initial right upper quadrant ultrasound.
The image demonstrates no discrete internal flow within the gallbladder with blood flow in
the adjacent vasculature.
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 2 of 9
The patient was followed closely by her PCP until her symptoms resolved and elevated liver
enzymes normalized over the next few months. No additional imaging was performed at that
time, and no surgery was scheduled.
In April 2014, the patient developed RUQ pain that worsened over the next four months,
prompting her to seek medical help. In August 2014, she was reevaluated by her PCP and
subsequently underwent an acute abdominal series (AAS), RUQ ultrasound, and nuclear
medicine hepatobiliary (HIDA) study. The ultrasound demonstrated cholelithiasis and
echogenic sludge within the gallbladder with hypoechoic and hyperemic adjacent liver
parenchyma. A mildly enlarged common duct was also observed. These findings
were concerning for chronic cholecystitis, xanthogranulomatous cholecystitis, or early acute
cholecystitis (Figure 3). The HIDA scan results were also consistent with acute cholecystitis
(Figure 4).
FIGURE 3: Right upper quadrant ultrasound.
The image demonstrates sludge/stone like material within the lumen of the gallbladder (red
arrow) with a rim of hyperemia initially interpreted as outside of the gallbladder given the clinical
appearance of acute cholecystitis.
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 3 of 9
FIGURE 4: HIDA scan.
The image demonstrates excretion through the biliary system into the duodenojejunal junction
(DJJ), but with no uptake within the gallbladder/cystic duct (red arrow).
The patient was taken to surgery for a laparoscopic cholecystectomy for suspected cholecystitis.
The laparoscopic approach was converted to an open procedure after the discovery of a mass
within the lumen of the gallbladder, a second mass near the hepatic flexure of the colon, and
enlarged portal vein lymph nodes. During the operation, the patient underwent a radical
cholecystectomy, right hemicolectomy with primary anastomosis, and a portal vein lymph
node dissection (LND). Pathology of the gallbladder mass demonstrated infiltrating papillary
adenocarcinoma invading the perimuscular connective tissue. The pathology also revealed one
portocaval lymph node that was positive for adenocarcinoma. The patient's stage of disease was
determined to be IVB (pT2N2). After surgery, the patient underwent radiotherapy to 4500 cGy,
targeting the gallbladder fossa and the involved lymph nodes, with concurrent chemotherapy
(capecitabine 625 mg/m2 twice daily). Abdominal CT and MRI scans were performed eight
months after the completion of chemoradiation. At that time, there was no radiologic evidence
of disease recurrence. Currently, the patient is fourteen months post treatment. Overall, she is
doing well and continues to receive close follow-up care.
Discussion
GBC is an infrequent neoplasm that is associated with a high rate of regional lymph node
metastasis and mortality [2,6,9]. Adjuvant chemoradiation is commonly recommended for
node-positive or incompletely resected disease [7-8]. The extent of the resection correlates with
survival. R0 resection is the most important because patients who undergo R2 resections do
poorly in spite of chemoradiation. However, there are some long-term survivors in patients
treated with adjuvant chemoradiation status post R0/R1 resections [6,9-10]. Therefore, early
detection is important because patients found at stage T1N0 would have a greater chance for
surgical cure and spare them the potential toxicity of adjuvant therapy.
Early diagnosis can be difficult because symptoms can mimic or be caused by coexisting
cholecystitis, which is a common condition [5]. Therefore, screening patients who present with
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 4 of 9
these symptoms is essential given the possibility for a coexisting GBC. Symptoms early in
the disease process can also be vague, often leading to a delay in diagnosis. The most common
complaint in the symptomatic patient with GBC is RUQ pain, specifically in the right
hypochondrium. Other warning signs, which our patient did not exhibit, include weight loss,
anorexia, nausea and/or vomiting, jaundice, and pruritus [11-12]. Routine laboratory tests are
generally nondiagnostic and do not significantly improve the identification of GBC
preoperatively, as exemplified by our case [12]. Serum tumor markers, carcinoembryonic
antigen (CEA), and carbohydrate antigen 19-9 (CA 19-9) are frequently elevated in patients
with GBC, but are not useful in its diagnosis because of their lack of sensitivity and specificity
[13-14].
Imaging with ultrasound and CT has improved preoperative diagnosis of GBC. Despite these
advancements, only 50% of gallbladder cancers are recognized before surgery [12]. Ultrasound
is often the initial imaging study of choice for patients presenting with symptoms consistent
with gallstone disease. The RUQ ultrasound is perhaps the single most important test in
helping lead to the diagnosis of GBC preoperatively. Ultrasound images from a group of patients
diagnosed with GBC incidentally were reviewed retrospectively and found to have suspicious
findings on reevaluation [15].
The most common ultrasound findings include calcified and echogenic mucosal masses, which
can be associated with cholelithiasis or porcelain gallbladder [15]. High-risk features on
ultrasonography also include solitary or displaced gallstone, intraluminal mass, gallbladder-
replacing or invasive mass, and discontinuity of the mucosal echo [15]. Other findings that are
suggestive of GBC include the loss of the interface between the gallbladder and liver or direct
liver infiltration [15]. Moreover, ultrasound abnormalities are often more subtle in early stage
disease, making detection more challenging [15]. If abnormalities or suspicious findings are
detected on ultrasound, further evaluation with other non-invasive imaging is warranted.
Consideration of GBC in the differential diagnosis may help to improve detection before surgery
(Figures 5-7), potentially leading to the discovery of the disease in its early stages.
FIGURE 5: Companion case. Right upper quadrant ultrasound
of a patient who presented a few months after the first patient.
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 5 of 9
The image demonstrates a hypoechoic lesion near the expected location of the gallbladder (red
arrow). Given the suspicious ultrasound finding and recent prior GBC case, leading differential
diagnosis was neoplasm. As a result, further evaluation with a CT scan was recommended.
FIGURE 6: CT scan.
The image demonstrates a coronal CT showing a hypodense mass with direct invasion into
the right hepatic lobe (red arrow), with additional small lesion in the left hepatic lobe (yellow
arrow). Not shown is portohepatous and peripancreatic lymphadenopathy. The extent of
disease suggests an element of patient denial of symptoms prior to clinical presentation.
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 6 of 9
FIGURE 7: Preparatory imaging of ultrasound guided biopsy in
the companion case.
The image demonstrates the target lesion and the planned route of the needle (red arrow). The
biopsy results revealed a primary biliary cancer, most likely gallbladder carcinoma.
The most useful, non-invasive imaging studies for evaluating GBC preoperatively include CT,
magnetic resonance imaging (MRI), and/or magnetic resonance cholangiopancreatography
(MRCP) (Figures 5, 6). CT has been shown to be useful in defining the extent of GBC and in
determining the resectability in advanced stages [16-17]. Additionally, CT has a low to
moderate sensitivity for detecting gastrointestinal, omental, and abdominal wall involvement,
but because of its high positive predictive value in detecting liver invasion, lymph node
involvement, and/or distant metastases, it remains a useful imaging study in GBC
preoperatively [16-17]. MRI and MRCP have also been shown to be useful in preoperative
staging of GBC with a high sensitivity in identifying hepatic invasion and lymph node
metastasis [18]. Biopsies of the detected gallbladder masses are often performed via ultrasound
guidance (Figure 7), but can also be performed under CT guidance, endoscopic ultrasound
guidance, endoscopic retrograde cholangiopancreatography (ERCP), or by laparoscopy.
Regarding further procedures and tests for GBC, endoscopic ultrasound (EUS) is a minimally
invasive procedure that has been shown to be more accurate than RUQ ultrasound at imaging
the gallbladder. EUS is also helpful in the differential diagnosis of gallbladder polyps and
excellent in staging tumor depth [19-20]. ERCP and PET are two less commonly used imaging
modalities used for evaluating GBC preoperatively. Generally, PET is not widely used prior to
surgical resection because of its low sensitivity for detecting extrahepatic metastases,
especially in patients with peritoneal carcinomatosis [21]. Although PET/CT is not commonly
used before surgical resection, several studies have shown a potential benefit in detecting
distant metastasis [21-24]. One retrospective study demonstrated that in patients with
potentially resectable tumors based on conventional imaging, PET imaging was able to detect
occult metastatic disease and ultimately changed the management in almost twenty-five
percent of the patients [24].
Conclusions
Our case illustrates the challenge of preoperative, early-stage GBC diagnosis. Despite multiple
imaging studies, GBC was not diagnosed in the described patient until laparoscopy for acute
cholecystitis. In the companion case, GBC was advanced at the time of imaging, which may
have been due to patient denial of symptoms. Given that early detection is important in both
decreasing the morbidity and mortality of GBC, with potential for surgical cure in cases limited
to the gallbladder, patients with RUQ ultrasound findings such as gallstones or polyps should be
offered surgical consultation. Further, consideration of GBC within the differential diagnosis by
primary care clinicians, radiologists, and surgeons may serve to maximize discovery before
the time of surgery.
"The views expressed in this case report are those of the authors and do not reflect the
official policy of the Department of Army/Navy/Air Force, Department of Defense, or
U.S. Government."
Additional Information
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 7 of 9
Disclosures
Conflicts of interest: The authors have declared that no conflicts of interest exist.
References
1. Carriaga MT, Henson DE: Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer.
1995, 75:171–190. 10.1002/1097-0142(19950101)75:1+<171::AID-
CNCR2820751306>3.0.CO;2-2
2. Duffy A, Capanu M, Abou-Alfa GK, et al: Gallbladder cancer (GBC): 10-year experience at
Memorial Sloan-Kettering Cancer Centre (MSKCC). J Surg Oncol. 2008, 98:485–489.
10.1002/jso.21141
3. Zatonski WA, Lowenfels AB, Boyle P, et al: Epidemiologic aspects of gallbladder cancer: a
case-control study of the SEARCH Program of the International Agency for Research on
Cancer. J Natl Cancer Inst. 1997, 89:1132-1138. 10.1093/jnci/89.15.1132
4. Rustagi T, Dasanu CA: Risk factors for gallbladder cancer and cholangiocarcinoma:
similarities, differences and updates. J Gastrointest Cancer. 2012, 43:137-147.
10.1007/s12029-011-9284-y
5. Hsing AW, Gao YT, Han TQ, et al: Gallstones and the risk of biliary tract cancer: a population-
based study in China. Br J Cancer. 2007, 97:1577–1582. 10.1038/sj.bjc.6604047
6. Groot Koerkamp B, Fong Y: Outcomes in biliary malignancy. J Surg Oncol. 2014, 110:585-591.
10.1002/jso.23762
7. Horgan AM, Amir E, Walter T, Knox JJ: Adjuvant therapy in the treatment of biliary tract
cancer: a systematic review and meta-analysis. J Clin Oncol. 2012, 30:1934-1940.
10.1200/jco.2011.40.5381
8. Wang SJ, Lemieux A, Kalpathy-Cramer J, et al: Nomogram for predicting the benefit of
adjuvant chemoradiotherapy for resected gallbladder cancer. J Clin Oncol. 2011, 29:4627-
4632. 10.1200/jco.2010.33.8020
9. Cariati A, Piromalli E, Cetta F: Gallbladder cancers: associated conditions, histological types,
prognosis, and prevention. Eur J Gastroenterol Hepatol. 2014, 26:562–569.
10.1097/meg.0000000000000074
10. Pilgrim CH, Groeschl RT, Turaga KK, Gamblin TC: Key factors influencing prognosis in
relation to gallbladder cancer. Dig Dis Sci. 2013, 58:2455–2462. 10.1007/s10620-013-2713-y
11. Misra S, Chaturvedi A, Misra NC, Sharma ID: Carcinoma of the gallbladder . Lancet Oncol.
2003, 4:167-176. 10.1016/S1470-2045(03)01021-0
12. Löhe F, Meimarakis G, Schauer C, Angele M, Jauch KW, Schauer RJ: The time of diagnosis
impacts surgical management but not the outcome of patients with gallbladder carcinoma.
Eur J Med Res. 2009, 14:345–351.
13. Strom BL, Maislin G, West SL, et al: Serum CEA and CA 19-9: potential future diagnostic or
screening tests for gallbladder cancer. Int J Cancer. 1990, 45:821-824. 10.1002/ijc.2910450505
14. Ritts RE Jr, Nagorney DM, Jacobsen DJ, Talbot RW, Zurawski VR Jr: Comparison of
preoperative serum CA19-9 levels with results of diagnostic imaging modalities in patients
undergoing laparotomy for suspected pancreatic or gallbladder disease. Pancreas. 1994, 9:707-
716.
15. Wibbenmeyer LA, Sharafuddin MJ, Wolverson MK, Heiberg EV, Wade TP, Shields JB:
Sonographic diagnosis of unsuspected gallbladder cancer: imaging findings in comparison
with benign gallbladder conditions. AJR Am J Roentgenol. 1995, 165:1169–1174.
10.2214/ajr.165.5.7572497
16. Kumar A, Aggarwal S: Carcinoma of the gallbladder: CT findings in 50 cases . Abdom Imaging.
1994, 19:304-308. 10.1007/BF00198184
17. Ohtani T, Shirai Y, Tsukada K, Muto T, Hatakeyama K: Spread of gallbladder carcinoma: CT
evaluation with pathologic correlation. Abdom Imaging. 1996, 21:195-201.
10.1007/s002619900045
18. Schwartz LH, Black J, Fong Y, et al: Gallbladder carcinoma: findings at MR imaging with MR
cholangiopancreatography. J Comput Assist Tomogr. 2002, 26:405-410. 10.1097/00004728-
200205000-00015
19. Sugiyama M, Atomi Y, Yamato T: Endoscopic ultrasonography for differential diagnosis of
polypoid gall bladder lesions: analysis in surgical and follow up series. Gut. 2000, 46:250-254.
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 8 of 9
10.1136/gut.46.2.250
20. Sadamoto Y, Kubo H, Harada N, Tanaka M, Eguchi T, Nawata H: Preoperative diagnosis and
staging of gallbladder carcinoma by EUS. Gastrointest Endosc. 2003, 58:536-541.
10.1067/S0016-5107(03)01961-8
21. Anderson CD, Rice MH, Pinson CW, Chapman WC, Chari RS, Delbeke D: Fluorodeoxyglucose
PET imaging in the evaluation of gallbladder carcinoma and cholangiocarcinoma. J
Gastrointest Surg. 2004, 8:90-97. 10.1016/j.gassur.2003.10.003
22. Petrowsky H, Wildbrett P, Husarik DB, et al: Impact of integrated positron emission
tomography and computed tomography on staging and management of gallbladder cancer and
cholangiocarcinoma. J Hepatol. 2006, 45:43-50. 10.1016/j.jhep.2006.03.009
23. Lee SW, Kim HJ, Park JH, et al: Clinical usefulness of 18F-FDG PET-CT for patients with
gallbladder cancer and cholangiocarcinoma. J Gastroenterol. 2010, 45:560-566.
10.1007/s00535-009-0188-6
24. Corvera CU, Blumgart LH, Akhurst T, et al: 18F-fluorodeoxyglucose positron emission
tomography influences management decisions in patients with biliary cancer. J Am Coll Surg.
2008, 206:57-65. 10.1016/j.jamcollsurg.2007.07.002
2016 Graff et al. Cureus 8(2): e493. DOI 10.7759/cureus.493 9 of 9
You might also like
- 4 Stages of Cirrhosis of The Liver 18 Symptoms, CDocument9 pages4 Stages of Cirrhosis of The Liver 18 Symptoms, CRammy KhanNo ratings yet
- Bowel Elimination Answer - 1Document3 pagesBowel Elimination Answer - 1June Dumdumaya100% (2)
- MCQ in Pediatric SurgeryDocument6 pagesMCQ in Pediatric SurgeryPatrycjaSkierka50% (2)
- Fibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleDocument3 pagesFibrolamellar Variant of Hepatocellular Carcinoma in A Young FemaleIKIKIKIKIKI999999No ratings yet
- It Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaDocument5 pagesIt Is Not Always A Cholangiocarcinoma: Unusual Peritoneal Carcinomatosis Revealing Gastric AdenocarcinomaIJAR JOURNALNo ratings yet
- Storch 2007Document3 pagesStorch 2007PNo ratings yet
- Akiyama Case ReportDocument3 pagesAkiyama Case ReportApmc SchwartzNo ratings yet
- 2020 Paper SplenicDocument5 pages2020 Paper SplenicLauburu CrossNo ratings yet
- Aresia de Vias Biliares UltrasonidoDocument14 pagesAresia de Vias Biliares UltrasonidoArturo GarciaNo ratings yet
- Revisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsDocument26 pagesRevisión Del Carcinoma de Vesicula: Poster No.: Congress: Type: AuthorsArturo García MarquezNo ratings yet
- International Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseDocument4 pagesInternational Journal of Surgery Case Reports: Adenocarcinoma in An Ano-Vaginal Fistula in Crohn's DiseaseTegoeh RizkiNo ratings yet
- Literature Review of Liver AbscessDocument4 pagesLiterature Review of Liver Abscessc5ng67v1100% (1)
- Hepatocellular Carcinoma - Diagnosis and TreatmentDocument46 pagesHepatocellular Carcinoma - Diagnosis and TreatmentSigh BalaNo ratings yet
- A Rare Case of Colon Cancer in A Young Patient: A Case Report and Literature ReviewDocument5 pagesA Rare Case of Colon Cancer in A Young Patient: A Case Report and Literature ReviewIJAR JOURNALNo ratings yet
- Recurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureDocument5 pagesRecurrent Adenocarcinoma of Colon Presenting As Duo-Denal Metastasis With Partial Gastric Outlet Obstruction: A Case Report With Review of LiteratureVika RatuNo ratings yet
- GB Cancer - Radiologic-Pathologic CorrelationDocument20 pagesGB Cancer - Radiologic-Pathologic CorrelationSamuel WidjajaNo ratings yet
- Evaluation of Focal Hepatic Lesions by Using Ultrasound EvaluationDocument2 pagesEvaluation of Focal Hepatic Lesions by Using Ultrasound EvaluationNaufal LutfiNo ratings yet
- Accuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureDocument4 pagesAccuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureAnasriNstNo ratings yet
- 1 s2.0 S2210261222001894 MainDocument5 pages1 s2.0 S2210261222001894 Mainkiki tuanaya1No ratings yet
- Incidental Gallbladder Cancer. Residual Cancer Discovered at Oncologic Extended Resection Determines Outcome. A Report From High - and Low-IncidencDocument10 pagesIncidental Gallbladder Cancer. Residual Cancer Discovered at Oncologic Extended Resection Determines Outcome. A Report From High - and Low-IncidencCarlos SotoNo ratings yet
- Ce 48 291Document6 pagesCe 48 291Siska HarapanNo ratings yet
- Ojped 2024030813565746Document6 pagesOjped 2024030813565746Nicolás Mosso F.No ratings yet
- Unexplained Ascites, A Sign For Neuroendocrine Carcinoma: Case ReportDocument3 pagesUnexplained Ascites, A Sign For Neuroendocrine Carcinoma: Case ReportsandzatNo ratings yet
- Liver Abscess DissertationDocument4 pagesLiver Abscess DissertationPayForAPaperAtlanta100% (1)
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Sonography First-Line Modality in Diagnosis of Acute Colonic Diverticulitis 2013Document6 pagesSonography First-Line Modality in Diagnosis of Acute Colonic Diverticulitis 2013waldemar russellNo ratings yet
- Choledochal CystDocument14 pagesCholedochal CystIndah SolehaNo ratings yet
- Primary Congenital Choledochal Cyst With Squamous Cell Carcinoma: A Case ReportDocument6 pagesPrimary Congenital Choledochal Cyst With Squamous Cell Carcinoma: A Case ReportRais KhairuddinNo ratings yet
- Differentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and ManagementDocument9 pagesDifferentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and ManagementMayerlin CalvacheNo ratings yet
- en Papilla Vaters Tumor in Elderly An InterDocument5 pagesen Papilla Vaters Tumor in Elderly An InterAyip Bahsan AlBantaniNo ratings yet
- Rare Small Bowel Carcinoid Tumor A Case ReportDocument5 pagesRare Small Bowel Carcinoid Tumor A Case ReportAthenaeum Scientific PublishersNo ratings yet
- 1 s2.0 S1015958422013677 MainDocument5 pages1 s2.0 S1015958422013677 MainMohammed S. FoulaNo ratings yet
- Metastatic Spread of Primary Lung Adenocarcino - 2024 - International Journal ofDocument5 pagesMetastatic Spread of Primary Lung Adenocarcino - 2024 - International Journal ofRonald QuezadaNo ratings yet
- Pancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyDocument4 pagesPancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyMolla WariNo ratings yet
- Unusual Presentation of Lung Cancer A Case ReportDocument3 pagesUnusual Presentation of Lung Cancer A Case Reportariza0% (1)
- A Randomized Controlled Trial of Emergency Treatment of Bleeding Esophageal Varices in Cirrhosis For Hepatocellular CarcinomaDocument15 pagesA Randomized Controlled Trial of Emergency Treatment of Bleeding Esophageal Varices in Cirrhosis For Hepatocellular CarcinomaAntonius SimangunsongNo ratings yet
- 260-Article Text-875-1-10-20220728Document4 pages260-Article Text-875-1-10-20220728hasan andrianNo ratings yet
- Diagnostic Imaging Pathways ArticleDocument10 pagesDiagnostic Imaging Pathways ArticleSuhayatra PutraNo ratings yet
- Esophageal Cancer: Diagnosis and Management: Ai Zheng Aizheng Chinese Journal of Cancer October 2010Document13 pagesEsophageal Cancer: Diagnosis and Management: Ai Zheng Aizheng Chinese Journal of Cancer October 2010Al VlaovicNo ratings yet
- 54 Raviswami EtalDocument3 pages54 Raviswami EtaleditorijmrhsNo ratings yet
- Ajol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309Document2 pagesAjol File Journals - 76 - Articles - 114038 - Submission - Proof - 114038 901 318286 1 10 20150309alysNo ratings yet
- 5 Advanced Ultrasound TechniquesDocument7 pages5 Advanced Ultrasound Techniquesjefaturaimagenologia Hospital NogalarNo ratings yet
- Gallbladdercancer: Diagnosis, Surgical Management, and Adjuvant TherapiesDocument19 pagesGallbladdercancer: Diagnosis, Surgical Management, and Adjuvant Therapiesmyat252No ratings yet
- Management of Incidentally Detected Gallbladder Polyps Society of Radiologists in Ultrasound Consensus Conference RecommendationsDocument13 pagesManagement of Incidentally Detected Gallbladder Polyps Society of Radiologists in Ultrasound Consensus Conference RecommendationsYasser Farouk Sevilla HernandezNo ratings yet
- 492 568 1 SMnjsjsdjsDocument4 pages492 568 1 SMnjsjsdjsZidna MazayatulNo ratings yet
- International Journal of Infectious Diseases: Anshuman Pandey, Shakeel Masood, Namrata P. AwasthiDocument3 pagesInternational Journal of Infectious Diseases: Anshuman Pandey, Shakeel Masood, Namrata P. Awasthijohanna monsalveNo ratings yet
- Initial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsDocument33 pagesInitial Diagnosis and Staging of Pancreatic Cancer Including Main DifferentialsClaudia YalanNo ratings yet
- R Azumi Lava 2014Document12 pagesR Azumi Lava 2014limbert manuelNo ratings yet
- Esophageal Composite Tumor With Neuroendocrine Component: A Rare EntityDocument4 pagesEsophageal Composite Tumor With Neuroendocrine Component: A Rare EntityIJAR JOURNALNo ratings yet
- Kanyongo's CardioDocument21 pagesKanyongo's CardioHuram SeremaniNo ratings yet
- SECTION I Inflammatory, Infective, and Congenital: Pyogenic Liver AbscessDocument12 pagesSECTION I Inflammatory, Infective, and Congenital: Pyogenic Liver AbscessandresNo ratings yet
- Neuroendocrine Tumors Dr. WarsinggihDocument20 pagesNeuroendocrine Tumors Dr. WarsinggihAndi Eka Putra PerdanaNo ratings yet
- Kuipersetal CRC NRDP2015Document26 pagesKuipersetal CRC NRDP2015Robert ChristevenNo ratings yet
- Case Report 1676563639Document6 pagesCase Report 1676563639noah jemedafeNo ratings yet
- Primary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportDocument4 pagesPrimary Pure Squamous Cell Carcinoma of The Duodenum: A Case ReportGeorge CiorogarNo ratings yet
- Modern Imaging in Obstructive JaundiceDocument4 pagesModern Imaging in Obstructive JaundicedanaogreanuNo ratings yet
- Histopathology of Hepatocellular CarcinomaDocument11 pagesHistopathology of Hepatocellular CarcinomaCindy Sabina FaleandraNo ratings yet
- Aproximación Multidisciplinaria Al Diagnóstico y Tratamiento de La Obs Intestinal 2018Document124 pagesAproximación Multidisciplinaria Al Diagnóstico y Tratamiento de La Obs Intestinal 2018Jorge Nuñez LucicNo ratings yet
- cLINICAL PRACTICE GUIDELINESDocument7 pagescLINICAL PRACTICE GUIDELINESdrmolinammNo ratings yet
- Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy For Pseudomyxoma Peritonei in A Liver-Transplanted Patient: A Case ReportDocument5 pagesCytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy For Pseudomyxoma Peritonei in A Liver-Transplanted Patient: A Case Reportyerich septaNo ratings yet
- An Unusual Cause of Acute Abdomend Gas-Forming Liver Abscess Due To Salmonella EnteritidisDocument4 pagesAn Unusual Cause of Acute Abdomend Gas-Forming Liver Abscess Due To Salmonella EnteritidisMenda JangWooyoung SooyoungsterNo ratings yet
- Imaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesFrom EverandImaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesNo ratings yet
- Fast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesFrom EverandFast Facts: Cholangiocarcinoma: Diagnostic and therapeutic advances are improving outcomesNo ratings yet
- 5 - Gastrointestinal Bleeding (AMBOSS) ?Document6 pages5 - Gastrointestinal Bleeding (AMBOSS) ?Rawabi rawabi1997No ratings yet
- Swasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurDocument26 pagesSwasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurCyber MagicNo ratings yet
- Digestive SystemDocument7 pagesDigestive SystemKirsten CruzadoNo ratings yet
- Enema Final Lesson Plan PDFDocument17 pagesEnema Final Lesson Plan PDFRahul Damor88% (8)
- Mainz II Surgery IllustratedDocument25 pagesMainz II Surgery IllustratedPurvi Parikh100% (1)
- Acute AbdomenDocument60 pagesAcute AbdomenAnish DhamiNo ratings yet
- ProctopexyDocument6 pagesProctopexydrnareshkumar3281No ratings yet
- Class 7, CH 2 Nutrition in AnimalsDocument4 pagesClass 7, CH 2 Nutrition in AnimalsAkkshara Kashyap 7-HNo ratings yet
- Gastric Fluid Analysis NotesDocument2 pagesGastric Fluid Analysis NotesanonacadsNo ratings yet
- L7 - Gastric - Duodenal SecretionsDocument6 pagesL7 - Gastric - Duodenal SecretionsBig Daddy YoNo ratings yet
- Med Surg: GI - Gastrointestinal: PathophysiologyDocument1 pageMed Surg: GI - Gastrointestinal: PathophysiologyTori RolandNo ratings yet
- Fecal IncontinenceDocument5 pagesFecal IncontinenceDaniel Galindo SotomayorNo ratings yet
- Profil Penderita CBDDocument12 pagesProfil Penderita CBDVandra PrinosaNo ratings yet
- Bio4 4Document14 pagesBio4 4Nomap makNo ratings yet
- Interpretation of Liver Function TestsDocument14 pagesInterpretation of Liver Function TestsNirav SharmaNo ratings yet
- Portal Hypertensive Gastropathy - UpToDateDocument27 pagesPortal Hypertensive Gastropathy - UpToDatebagir_dm10No ratings yet
- Gastrointestional QuestionnaireDocument2 pagesGastrointestional QuestionnaireEva SabillaNo ratings yet
- Multiple-Choice Questionnaire: Functional Pelvic Floor ImagingDocument3 pagesMultiple-Choice Questionnaire: Functional Pelvic Floor Imagingtesfaye mekonnenNo ratings yet
- Surgery For Finals 2010Document58 pagesSurgery For Finals 2010Kay Bristol100% (1)
- Human Digestive SystemDocument19 pagesHuman Digestive SystemsyagitaNo ratings yet
- Reflexes in The GutDocument2 pagesReflexes in The GutJeffrey TseNo ratings yet
- Advanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr Solution ManualDocument9 pagesAdvanced Nutrition and Human Metabolism 7th Edition Gropper Smith Carr Solution Manualjames100% (28)
- Management of Obstructive Jaundice Exper PDFDocument3 pagesManagement of Obstructive Jaundice Exper PDFgustianto hutama pNo ratings yet
- Announcement SGU 2021Document10 pagesAnnouncement SGU 2021ceciliaNo ratings yet
- Summary of Digestion: C. Gastrointestinal Hormones 1. GastrinDocument5 pagesSummary of Digestion: C. Gastrointestinal Hormones 1. GastrinIrish Eunice FelixNo ratings yet
- Pancreatic Pseudocyst 2Document37 pagesPancreatic Pseudocyst 2AzharUlHassanQureshi100% (1)
- PancreasDocument11 pagesPancreasCheng XinvennNo ratings yet