Professional Documents
Culture Documents
Ambient Temperature and Seasonal Variation in Inpa
Ambient Temperature and Seasonal Variation in Inpa
Uploaded by
Ibrahima DialloOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ambient Temperature and Seasonal Variation in Inpa
Ambient Temperature and Seasonal Variation in Inpa
Uploaded by
Ibrahima DialloCopyright:
Available Formats
Articles
Ambient temperature and seasonal variation in inpatient
mortality from respiratory diseases: a retrospective
observational study
Hicham Achebak,a,b,∗ Judith Garcia-Aymerich,b,c,d Grégoire Rey,a Zhaoyue Chen,b Raúl Fernando Méndez-Turrubiates,b and Joan Ballesterb
a
Inserm, France Cohortes, Paris, France
b
ISGlobal, Barcelona, Spain
c
Universitat Pompeu Fabra (UPF), Barcelona, Spain
d
CIBER Epidemiología y Salud Pública (CIBERESP), Barcelona, Spain
Summary The Lancet Regional
Health - Europe
Background The seasonal fluctuation in mortality and hospital admissions from respiratory diseases, with a winter
2023;35: 100757
peak and a summer trough, is widely recognized in extratropical countries. However, little is known about the
Published Online 7
seasonality of inpatient mortality and the role of ambient temperature remains uncertain. We aimed to analyse the
November 2023
association between ambient temperature and in-hospital mortality from respiratory diseases in the provinces of https://doi.org/10.
Madrid and Barcelona, Spain. 1016/j.lanepe.2023.
100757
Methods We used data on daily hospitalisations, weather (ie, temperature and relative humidity) and air pollutants (ie,
PM2.5, PM10, NO2 and O3) for the Spanish provinces of Madrid and Barcelona during 2006–2019. We applied a daily
time-series quasi-Poisson regression in combination with distributed lag non-linear models (DLNM) to assess, on the
one hand, the seasonal variation in fatal hospitalisations and the contribution of ambient temperature, and on the
other hand, the day-to-day association between temperature and fatal hospital admissions. The analyses were
stratified by sex, age and primary diagnostic of hospitalisation.
Findings The study analysed 1 710 012 emergency hospital admissions for respiratory diseases (mean [SD] age, 60.4
[31.0] years; 44.2% women), from which 103 845 resulted in in-hospital death (81.4 [12.3] years; 45.1%). We found a
strong seasonal fluctuation in in-hospital mortality from respiratory diseases. While hospital admissions were higher
during the cold season, the maximum incidence of inpatient mortality was during the summer and was strongly
related to high temperatures. When analysing the day-to-day association between temperature and in-hospital
mortality, we only found an effect for high temperatures. The relative risk (RR) of fatal hospitalisation at the 99th
percentile of the distribution of daily temperatures vs the minimum mortality temperature (MMT) was 1.395
(95% eCI: 1.211–1.606) in Madrid and 1.612 (1.379–1.885) in Barcelona. In terms of attributable burden, summer
temperatures (June–September) were responsible for 16.2% (8.8–23.3) and 22.3% (15.4–29.2) of overall fatal
hospitalisations from respiratory diseases in Madrid and Barcelona, respectively. Women were more vulnerable to
heat than men, whereas the results by diagnostic of admission showed heat effects for acute bronchitis and
bronchiolitis, pneumonia and respiratory failure.
Interpretation Unless effective adaptation measures are taken in hospital facilities, climate warming could exacerbate
the burden of inpatient mortality from respiratory diseases during the warm season.
Funding European Research Council Consolidator Grant EARLY-ADAPT, European Research Council Proof-of-
Concept Grants HHS-EWS and FORECAST-AIR.
Copyright © 2023 The Author(s). Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND
license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Keywords: Heat; Respiratory diseases; Hospital mortality
*Corresponding author. Inserm, France Cohortes, Paris 75013, France.
E-mail address: hicham.achebak@inserm.fr (H. Achebak).
www.thelancet.com Vol 35 December, 2023 1
Articles
Research in context
Evidence before this study Added value of this study
We searched PubMed from database inception until June 26, We showed for the first time an inverse seasonal fluctuation
2023, for articles published in English using the search terms between hospital admissions and inpatient mortality from
“seasonality”, “temperature”, “heat”, “cold”, AND respiratory diseases. Contrary to hospital admissions, higher
“hospitalisation”, “in-hospital mortality”, “respiratory during the cold season, the maximum incidence of inpatient
diseases”. We found a reduced number of studies analysing mortality was during the summer. We also showed that the
the seasonal variation in inpatient mortality from respiratory summer peak in in-hospital mortality from respiratory
diseases, and they were focusing solely on a subset of conditions was largely driven by high temperatures.
respiratory conditions accounting for a small fraction of all Moreover, when analysing the day-to-day association
respiratory hospitalisations. Meanwhile, the contribution of between ambient temperature and hospital admissions
ambient temperature to the seasonality of in-hospital resulting in death, we only found an effect for heat, thus
mortality remained unexplored. On the other hand, although confirming the results obtained in the seasonal analysis (ie,
the day-to-day association between heat/cold and hospital higher incidence of inpatient mortality in summer).
admissions form a range of respiratory diseases (such as
Implications of all the available evidence
pneumonia, chronic obstructive pulmonary disease [COPD]
Unless effective adaptation measures are taken in hospital
and asthma) was extensively described, so far no study has
facilities, climate warming could exacerbate the burden of
focused on the fraction of hospitalisations resulting in death,
inpatient mortality from respiratory diseases during the warm
and therefore, in the more severe cases of morbidity.
season.
Introduction inpatient mortality in winter season.23–25 Meanwhile, the
Ambient temperature is a major environmental role of ambient temperature in the seasonal fluctuation
contributor to adverse respiratory health.1,2 Short-term of in-hospital mortality remains unexplored. On the
exposure to heat and cold, as well as temperature vari- other hand, although it has been extensively described
ability, increases morbidity and mortality from respira- that the daily exposure to heat and cold are associated
tory diseases, especially among vulnerable individuals with a greater risk of hospital admission from a range of
with pre-existing conditions.3–12 As a result of the pro- respiratory diseases (such as pneumonia, chronic
jected increase in the exposure to extreme heat due to obstructive pulmonary disease [COPD] and
climate change,13 as well as its interaction with the rising asthma),6,8,26–28 so far no study has focused on the frac-
prevalence of chronic respiratory diseases,14 population tion of hospitalisations resulting in death, and therefore,
ageing15 and urbanisation,16 the heat-related respiratory in the more severe cases of morbidity.
adverse health outcomes are expected to worsen in the In this study we assessed the seasonal variation in in-
future, unless strong adaptation measures are put in hospital mortality from respiratory diseases, the contri-
place.1,17 By contrast, the negative effects of cold, which bution of temperature to this seasonal variation, and the
are nowadays far more common in extratropical coun- daily association between temperature and respiratory
tries,3,7 could be substantially reduced because of inpatient mortality in the provinces of Madrid and
warming temperatures. These opposing trends in the Barcelona, Spain. These research questions are of
impacts of heat and cold could in turn lead in the very especial relevance because in-hospital deaths from res-
long-term to a redefinition of the seasonality of respi- piratory conditions, which account for a large proportion
ratory morbidity and mortality.18,19 Moreover, climate of total respiratory mortality in Spain (64.4% during
change will also lead to more variability in temperature, 2016–2018),29 could be more preventable than outpatient
which could translate into a substantial respiratory deaths, and therefore, being able to predict them could
health burden.9,10,20 help to take preventive measures (eg, patient moni-
The seasonal fluctuation in mortality and hospital toring). Our results could inform climate change adap-
admissions from respiratory diseases, with a winter tation in healthcare facilities in a country that emerges
peak (mainly driven by respiratory infections) and a as a major hotspot in terms of both the impact of global
summer trough, is widely recognized in extratropical warming30 and human longevity rise.31
countries.21,22 However, to date, little is known about the
seasonal variation in inpatient mortality, a surrogate for
hospital performance in relation to severe respiratory Methods
events.23–25 Previous studies only focused on very specific Data sources
respiratory diseases accounting for a very small fraction This cross-sectional multicentre retrospective observa-
of all respiratory hospitalisations and found higher tional study used data on hospitalisations, weather (ie,
2 www.thelancet.com Vol 35 December, 2023
Articles
temperature and relative humidity) and air pollution (ie, Seasonality of in-hospital mortality
PM2.5, PM10, O3 and NO2) for the Spanish provinces of We first calculated the monthly case-fatality ratio (CFR)
Madrid and Barcelona during 2006–2019, representing as the proportion of the number of hospital admissions
an average population of approximately 12 million resulting in death (regardless of the month when the
people (26% of total population in Spain). death occurred) compared to the total number of hos-
On the one side, the Spanish National Institute of pital admissions in a given month:
Statistics (INE) provided individual-level records of
hospital admissions both from public and private hos- CFR (%) = (number of fatal hospital admissions
pitals, which included the following variables for the
/ total number of hospital admissions) × 100
patients: sex, age, date of admission and discharge,
province of residence, type of admission (ie, ordinary or (1)
urgent), primary diagnostic of admission, type of
discharge (ie, recovery, death, transfer, other) and length and did a graphical representation of the CFR in order
of hospital stay (in days). The dataset did not include to have a first picture of the seasonal distribution of this
unique identifier of patient, and therefore, readmissions variable (see Fig. 1). We then applied a daily time-series
or admissions belonging to the same subject could not quasi-Poisson regression model41 to estimate the sea-
be identified. The present study was restricted to sonality of hospital admissions resulting in death (μ):
emergency (ie, non-planned) hospital admissions due to
respiratory disease (see ICD codes in the Appendix, p 3). log(μ) = offset(log(admissions)) + α + ns(age)
Individual hospital records were aggregated by date of + int(year, dow) + cs(doy)
admission in order to conduct the statistical analyses (2)
described below.
Gridded (0.10◦ × 0.10◦ ) observations of daily mean 2- This model included the log-transformed total number
m temperature (◦ C) and daily mean relative humidity of hospital admissions as an offset; an intercept (α); a
(%) were derived from E-OBS (version 24.0e) of the natural cubic B-spline with 3 degrees of freedom (df) for
European Climate Assessment and Dataset (ECA&D).32 the average age of the fatal admissions because it showed a
Daily mean concentrations of PM2.5, PM10, NO2 and seasonal fluctuation (see Appendix, p 4); a stratum defined
daily maximum 8-hour averages of O3 across Spain were by a two-way interaction term of year and day-of-the-week
estimated using a Quantile Machine Learning (QML) (dow) to control for the long-term trends and the weekly
model framework at a spatial resolution of 10 km × 10 cycle of fatal hospital admissions; and a cyclic spline (cs)
km. The model’s development involved integrating with four 4 df for day-of-the-year (doy, taking values from 1
various data sources, including ground monitoring to 366) to quantify the number of fatal hospitalisations on
measurements,33 fine-mode and course-mode Aerosol each calendar day. The seasonality, here referring to the
Optical Depth (AOD),34 climate and air quality reanalysis association between the day-of-year and hospitalisations
data,35–37 and geographical features (eg, land-use, resulting in death, was reported as the relative risk (RR) of
topography, road traffic).38,39 The model was trained us- fatal hospital admission estimation at each calendar day
ing data from across Europe, covering the period from with 95% empirical confidence interval (eCI) (see Fig. 2).
Jan 1, 2003, to Dec 31, 2020. To assess the accuracy of Moreover, the ratio of the maximum fatal hospitalisation
the model, we conducted a 10-fold validation. The re- estimation at peak calendar day relative to the trough cal-
sults showed good performance, with correlation co- endar day, ie, the peak-to-trough ratio (PTR), was used as a
efficients of 0.80, 0.79, 0.79, and 0.90 for PM2.5, PM10, measure of seasonal amplitude.
NO2 and O3, respectively, when compared with site
observations in Europe. The Normalized Root Mean Role of temperature in the seasonality of in-hospital
Square Error (NRMSE) for PM2.5, PM10, NO2 and O3 mortality
predictions in Europe were found to be 1.84%, 2.07%, We introduced daily mean temperature into the model
8.99%, and 3.35%, respectively, in comparison to site described above (equation (2)) in order to obtain the
observations. Both meteorological and air pollution data temperature-adjusted seasonality (see again Fig. 2):
were transformed into provincial estimates by weighting
the values with 1 km × 1 km gridded population counts log(μ) = offset(log(admissions)) + α + ns(age)
for the year 2011 from INE.40 + int(year, dow) + cs(doy) + cb(temperature)
(3)
Statistical analysis
The statistical analyses were stratified by sex, age and Specifically, the short-term effects of temperature
diagnostic of hospitalisation and were done with R were modelled with a cross-basis function (cb) produced
software (version 4.3.1) using the packages pbs (for cyclic by DLNM,42 using a natural cubic B-spline both for the
splines), splines (for natural cubic splines) and dlnm (for exposure-response and lag-response functions. The
distributed lag non-linear models). spline representing the exposure-response function in
www.thelancet.com Vol 35 December, 2023 3
Articles
a Madrid b Barcelona
28 Temperature 90 26 80
26 Relative humidity 85 24 78
24 80 22 76
22 75 20
Relative humidity (%)
Relative humidity (%)
74
20 70
Temperature (°C)
Temperature (°C)
18
18 65 72
16
16 60 70
14
14 55 68
12
12 50
10
66
10 45
8 64
8 40
6 35 6 62
4 30 4 60
Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec
c Madrid d Barcelona
14 12 14 12
Hospital admissions Case−fatality ratio
12 11 12 11
Hospital admissions (per 10 000)
10 Hospital admissions (per 10 000) 10
Case−fatality ratio (%)
Case−fatality ratio (%)
10 10
9 9
8 8
8 8
6 6
7 7
4 4
6 6
2 5 2 5
0 4 0 4
Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec
e Madrid f Barcelona
14 Hospital admissions 14 14 12
Case−fatality ratio
12 12 12
Hospital admissions (per 1 000)
Hospital admissions (per 1 000)
10
10
Case−fatality ratio (%)
Case−fatality ratio (%)
10
10
8
8 8
8
6 6 6
6
4 4
4
4
2 2
0 2 0 2
2006 2008 2010 2012 2014 2016 2018 2020 2006 2008 2010 2012 2014 2016 2018 2020
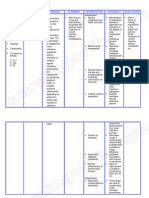
Fig. 1: Monthly distribution of meteorological variables, hospital admissions and case-fatality ratio.
the cb was modelled with one internal knot placed at the PM2.5, PM10, O3 and NO2) and summer holidays on the
75th percentile of the daily mean temperature distribu- role of temperature in the seasonality of in-hospital
tion. The lag period was extended up to 7 days, with an mortality by including separately the following terms
intercept and one internal knot placed at equally spaced in equation (3): a natural cubic B-spline with 2 df for
values in the log scale to account for the delayed effects relative humidity, a linear term for air pollutants, and a
of temperature. Moreover, we also explored the potential dummy or binary variable with value equal to 1 for July–
confounding effect of relative humidity, air pollution (ie, August days.
4 www.thelancet.com Vol 35 December, 2023
Articles
a Madrid b Barcelona
2.0 Temperature unadjusted 2.0
Temperature adjusted
1.9 1.9
1.8 1.8
1.7 1.7
1.6 1.6
1.5 1.5
RR
RR
1.4 1.4
1.3 1.3
1.2 1.2
1.1 1.1
1.0 1.0
0.9 0.9
01
01
01
01
01
01
31
01
01
01
01
31
01
01
01
01
1
01
01
01
01
01
01
01
01
0
0
May
May
Sep
Aug
Nov
Dec
Dec
Aug
Sep
Nov
Dec
Dec
Feb
Mar
Feb
Mar
Jan
Jun
Jan
Jun
Apr
Oct
Apr
Oct
Jul
Jul
Fig. 2: Seasonality of in-hospital mortality. RR = relative risk.
Day-to-day association between temperature and in-hospital residual confounding. The temperature-hospitalisation
mortality associations captured by the cb were summarised as
We performed a time-series quasi-Poisson regression in the RR of fatal hospital admission across the whole
combination with DLNM to estimate the day-to-day as- range of temperatures vs the minimum mortality tem-
sociation between temperature and in-hospital mortality perature (MMT) with 95% eCI (see Fig. 3). We then
counts. This model included the log-transformed total used the RRs to compute monthly attributable fatal
number of hospital admissions as an offset; an inter- hospital admissions (ie, numbers and fractions of hos-
cept; a natural cubic B-spline with 3 degrees of freedom pitalisations) following a methodology described else-
(df) for the average age of fatal admissions; a categorical where43 (see Fig. 4). In short, the RR corresponding to
variable of day of the week to account for the weekly each day of the series was used to calculate the attrib-
cycle in fatal hospital admissions; a natural cubic B- utable fraction (AF) of fatal hospital admissions on that
spline of time with 9 df per year to adjust for seasonal day and the next 7 days. Then, the daily attributable
and long-term trends; a natural cubic B-spline with 2 df number (AN) of fatal hospital admissions was computed
for relative humidity; and a cb of temperature with the by multiplying the daily AF by the daily number of fatal
same configuration as described above. Algebraically, hospitalisations. The number of AN in each month was
the model can be written as: separately aggregated from the daily series, and its ratio
with the corresponding total number of hospital ad-
log(μ) = offset(log(admissions)) + α + ns(age) + dow missions provided the monthly AF. We calculated 95%
+ ns(time) + ns(humidity) + cb(temperature) eCI of attributable mortality using Monte Carlo
simulations.
(4)
where μ denotes the expected number of hospital ad- Sensitivity analyses
missions resulting in death; and ns the natural cubic These abovementioned modelling choices were based
spline. To test the potential confounding effect of air on a quasi-likelihood version of the Akaike information
pollution on temperature-mortality association, we criterion (Q-AIC) and thoroughly tested in sensitivity
introduced separately in equation (4) a linear term for analyses. Specifically, we used different configuration
air pollutants (ie, PM2.5, PM10, NO2 and O3). We also for the cb function of temperature and different func-
analysed the effect modification of temperature by tions (linear and non-linear) for average age of the fatal
relative humidity and air pollutants by including in admissions.
equation (4) an interaction between the cb function of
temperature and dummy variables representing hu- Role of the funding source
midity and air pollution categories (low [below the me- The funders of the study had no role in study design,
dian] and high [above the median]), and a linear term for data collection, data analysis, data interpretation, or
the air pollutants in order to account for potential writing of the report. Multiple authors had full access to
www.thelancet.com Vol 35 December, 2023 5
Articles
a Madrid b Barcelona
2.4 2.4
2.2 2.2
2.0 2.0
1.8 1.8
RR
RR
1.6 1.6
1.4 1.4
1.2 1.2
1.0 1.0
0.8 0.8
−4 0 4 8 12 16 20 24 28 32 0 2 4 6 8 12 16 20 24 28 32
Temperature (°C) Temperature (°C)
Fig. 3: Day-to-day association between temperature and hospital admissions resulting in death. RR = relative risk.
all of the data and the corresponding author had final diagnostics of respiratory hospitalisations (48.8% of the
responsibility to submit for publication. total; see Appendix, p 5), although the highest case-
fatality ratio was by far among lung diseases due to
external agents (24.2%; see Appendix, p 5). The average
Results value (interquartile range) of non-population-weighted
The study analysed 1 710 012 non-planned hospital daily mean temperature and relative humidity was,
admissions for respiratory diseases (mean [SD] age, respectively, 14.3 ◦ C (13.1) and 60.4% (31.9) in Madrid,
60.4 [31.0] years; 44.2% women), from which 103 845 and 13.8 ◦ C (11.1) and 70.6% (14.7) in Barcelona. As
resulted in death (81.4 [12.3] years; 45.1%). This expected, there was an inverse correlation between the
number of hospitalisations accounted for 16.9% of all- daily mean temperature and daily mean relative hu-
cause non-planned admissions. Chronic lower respi- midity (Pearson correlation of −0.76 in Madrid
ratory diseases and pneumonia were the leading and −0.24 in Barcelona).
a Madrid b Barcelona
40 40
30 30
Attributable fraction (%)
Attributable fraction (%)
20 20
10 10
0 0
−10 −10
Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec
Fig. 4: Temperature attributable fraction of hospital admissions resulting in death.
6 www.thelancet.com Vol 35 December, 2023
Articles
Fig. 1 shows the monthly distribution of the number of fatal hospitalisation, especially in Barcelona, whereas
of hospital admissions and the CFR in the provinces of low temperatures were not associated with this health
Madrid and Barcelona during 2006–2019. In both loca- variable (Fig. 3). Note that the effect of heat was im-
tions, the number of hospital admissions (including mediate, as most of the impact took place in the first 3
those resulting in death [see Appendix, p 6]) was higher days since the exposure (Appendix, p 15). The RR of
in the cold season and lower in the warm season, with a fatal hospitalisation (accumulated across the lags) at the
peak in the month of January (the coldest one) and a 99th (1st) percentile of the distribution of daily tem-
minimum in the month of August (the hottest one after peratures vs the MMT was 1.395 (95% eCI: 1.211–1.606)
July). By contrast, the CFR drew the opposite seasonal (1.017 [0.963–1.073]) in Madrid and 1.612 (1.379–1.885)
pattern (see also age-standardised CFR in the Appendix, (1.057 [0.990–1.129]) in Barcelona. Note that in Madrid
p 7), with maximum monthly incidence in summer (Barcelona) the 99th temperature percentile, 1st tem-
(peak in August) and the minimum monthly incidence perature percentile and the MMT corresponded to
in autumn (minimum in November). When stratifying 30.0 ◦ C (27.6 ◦ C), 1.9 ◦ C (4.0 ◦ C) and 8.9 ◦ C (11.4 ◦ C),
CFR by cause-specific respiratory disease (see Appendix, respectively. Risks by age group were similar, but
p 8), we saw that the higher CFR in the warm season women were more vulnerable to heat than men, espe-
was mainly driven by pneumonia, acute bronchitis and cially in Madrid. Moreover, results by diagnostic of
bronchiolitis, COPD and, especially, respiratory failure. admission showed heat effects for acute bronchitis and
Fig. 2 depicts the estimation of the seasonality of bronchiolitis and pneumonia in Madrid and respiratory
hospital admissions resulting in death from the time- failure in Barcelona (see Appendix, p 16). Interestingly,
series regression model. Prior to the adjustment for neither relative humidity nor air pollutants (ie, PM2.5,
ambient temperature (equation (2) in Methods section), PM10, NO2 and O3) played a statistically significant role
a marked seasonal pattern with low fatal hospital in the association of heat with inpatient mortality (see
admission in winter and a high fatal hospital admission Appendix, pp 17–18). Moreover, the reported estimates
in summer was observed, as already shown in Fig. 1. hardly changed after adjustment for air pollutants (see
The shape of seasonality was similar between Madrid Appendix, p 19). Finally, in terms of mortality burden,
and Barcelona, but the amplitude of the seasonal vari- summer temperatures (June–September) were respon-
ation was greater in Madrid. The temperature- sible for 16.2% (8.8–23.3) and 22.3% (15.4–29.2) of
unadjusted PTR was 1.554 (95% eCI: 1.499–1.610) and overall fatal hospitalisations from respiratory diseases in
1.779 (1.720–1.840) for Barcelona and Madrid, respec- Madrid and Barcelona, respectively (Fig. 4).
tively. When accounting for temperature (equation (3) in All sensitivity analyses suggested that the results re-
Methods section), the shape of the seasonality was ported were not dependent on modelling assumptions
similar, but the amplitude showed a large decrease. The (see Appendix, pp 20–21).
PTR was reduced to 1.433 (1.311–1.565) in Madrid and
1.211 (1.098–1.335) in Barcelona. It is important to note
that the summer peak persisted after the adjustment for Discussion
temperature, especially in Madrid, which underlines the Our study showed for the first time a strong seasonal
presence of other factors contributing to higher fatal fluctuation in in-hospital mortality from respiratory
hospital admission during the summer, particularly in diseases and demonstrated that temperature is an
August. However, when accounting for the potential important driver of this phenomena. Contrary to hospital
confounding effect of humidity, air pollution (ie, PM2.5, admissions, higher during the cold season, the
PM10, O3 and NO2) and summer holidays, the yielded maximum incidence of inpatient mortality was during
estimates hardly changed (see Appendix, pp 9–10). Re- the summer and was strongly related to high tempera-
sults by age group (ie, ≥60 years, ≥70 years and ≥80 tures. Moreover, when analysing the day-to-day associa-
years) were quite similar, while women displayed higher tion between temperature and in-hospital mortality, we
seasonal amplitude than men, both before and after only found an effect for heat, thus confirming the results
adjustment for temperature (see Appendix, pp 11–12). obtained in the seasonal analysis (ie, higher incidence of
All diagnostics of hospitalisation exhibited a seasonal inpatient mortality in summer). These results have
peak during the summer season, except the lung dis- important implications for climate change health adap-
eases due to external agents, and high temperatures tation policies, and for the projections of climate change
contributed importantly to this peak in the case of acute impacts on human health. Unless effective adaptation
bronchitis and bronchiolitis, pneumonia and respiratory measures are taken in hospital facilities, climate warm-
failure in Madrid and respiratory failure in Barcelona ing might exacerbate the burden of inpatient mortality
(see, Appendix, pp 13–14). from respiratory diseases during the warm season.
Fig. 3 reports the day-to-day association between In the present study, we described a maximum
daily mean temperature and hospital admissions incidence of inpatient mortality in summer and a min-
resulting in death (equation (4) in Methods section). imum in winter, which contrast with the seasonal
High temperatures contributed to an increase in the risk pattern in hospital admissions. We also found that
www.thelancet.com Vol 35 December, 2023 7
Articles
ambient temperature had an important contribution to complete reversal of the seasonality of temperature-
the summer peak in in-hospital mortality, which might attributable mortality, with a shift of the maximum
be related to increased severity of respiratory morbidity. monthly incidence from winter to summer, and the
However, although it is true that the adjustment for minimum monthly incidence from early and late sum-
temperature reduced considerably the higher incidence mer to winter. However, it is important to note that our
of inpatient deaths during the summer, the August peak findings for cold cannot be extrapolated to previous
persisted, especially in Madrid, coinciding in time with periods and other countries, which are characterised by
the summer holidays and the eventual reorganisation of different healthcare contexts.
the healthcare services in many hospitals (eg, reduction The underlying physiological mechanisms by which
in physicians), which could affect negatively the quality heat trigger adverse health outcomes remain unclear,
of medical care. Nonetheless, this hypothesis does not but they seem to be largely mediated by a thermoregu-
seem to be supported by the results of our study, which latory pathway.17,45 Under conditions of heat stress, the
show no significant change in the seasonal pattern of in- body activates heat loss responses of cutaneous vasodi-
hospital mortality after the adjustment for the July– lation and sweat production (which subsequently evap-
August days in the time-series regression model (see orates and removes body heat) to limit elevations in core
Appendix, p 10), and therefore, further research is temperature, which can affect people differently based
warranted to clarify this issue. On the other hand, when on, for example, age, pre-existing health conditions (eg,
comparing the monthly CFR for respiratory diseases chronic cardiovascular-respiratory-kidney diseases,
with the CFR for cardiovascular conditions (note that obesity, diabetes, etc) or even the use of certain medi-
current research does not support that heat may cation.46 Vasodilation increases blood flow from the core
contribute to cardiovascular hospitalisations5,44), we saw to the skin and this allows more heat to be dissipated to
that cardiovascular CFR is at its lowest values during the the environment. Consequently, central blood volume is
summer months (see Appendix, p 22), though with a decreased and can be further reduced if sweating is not
small peak in August, which reinforce the idea of a compensated by appropriate fluid intake (ie, dehydra-
causal association between high temperatures and tion). In response to this, heart rate and contractility
increased inpatient mortality from respiratory diseases. increase, leading to a higher cardiac oxygen demand,
It has been extensively described that the short-term which predisposes individuals with limited coronary
(daily) exposure to heat and cold, as well as temperature flow reserve to ischaemia (ie, inadequate blood flow to
variability, are associated with a greater risk of hospital other organs). Compounding factors of ischaemia and
admission from a range of respiratory diseases such as severe hyperthermia can cause cell damage (ie, necro-
pneumonia, COPD and asthma.6,8,26–28 But so far no sis), affecting critically the functioning of several vital
study has focused on the fraction of hospitalisations organs, with the brain, heart, kidneys, intestines, liver,
resulting in death, and therefore, in the more severe pancreas and lungs at greatest risk. Hyperthermia and
cases of morbidity. Here we assessed the day-to-day ischaemia can also break down (i) cell membranes
association between ambient temperature and hospital rendering the organs more permeable to pathogens and
admissions resulting in death and we only found an toxins, which induce a systemic inflammatory response
effect for heat, thus confirming the results obtained in that can activate a hypercoagulable state, potentially
the seasonal analysis (ie, higher incidence of inpatient resulting in thrombosis; and (ii) skeletal muscle cells (ie,
mortality in summer). In addition, it is also important to rhabdomyolysis), thereby releasing myoglobin that can
note that the impact of heat was immediate, in the first 3 cause acute renal failure by obstructing kidney tubules.
days since the exposure, which suggest that the increase Nevertheless, although adverse effects related to
in acute respiratory outcomes during heat is more impaired thermoregulation may play an important role
related to the aggravation of chronic and infectious in heat-related respiratory diseases, a direct effect of
respiratory diseases than the spread of new respiratory breathing hot air is also plausible.6 For example, a study
infections through indoor crowding to avoid heat, as found that the inhalation of hot air triggered broncho-
respiratory infections usually take several days to cause constriction in patients with asthma.47
symptoms. Consistently with the majority of previous studies on
In this study we found no association between low total mortality (ie, hospital and non-hospital mortal-
temperatures and the risk of fatal outcome in patients ity),48,49 we found that women have a much higher
hospitalised for respiratory diseases. This might have to inpatient mortality from heat than men. This is very
do with the fact that health services are increasingly likely linked to sex-specific physiological differences in
prepared to deal with winter peaks in respiratory dis- thermoregulation. Women have been reported to have a
eases, which might in turn help explain the results of a higher temperature threshold above which sweating
previous study4 in which we found a very large reduction mechanisms are activated, and a lower sweat output
in the effects of cold on overall respiratory mortality than men, which results in less evaporative heat loss,
(hospital [about 65% in 2016–2018] and non-hospital and therefore a larger susceptibility to the effects of
deaths) in the most recent years in Spain, leading to a heat.50 Another biological factor (perhaps less
8 www.thelancet.com Vol 35 December, 2023
Articles
determinant) might have to do with the cardiovascular Appendix A. Supplementary data
system; women are more likely to have high blood Supplementary data related to this article can be found at https://doi.
org/10.1016/j.lanepe.2023.100757.
pressure after menopause.51
Last but not least, this study had strengths and lim-
itations. On the one hand, we analysed high-quality References
morbidity and environmental data spanning 14 years, 1 D’Amato G, Cecchi L, D’Amato M, Annesi-Maesano I. Climate
which allowed us to accurately characterise the seasonal change and respiratory diseases. Eur Respir Rev. 2014;23:161–169.
2 Collaco JM, Appel LJ, McGready J, Cutting GR. The relationship of
variation in-patient mortality from respiratory diseases lung function with ambient temperature. PLoS One. 2018;13:
and its association with ambient temperature. Addi- e0191409.
3 Chen R, Yin P, Wang L, et al. Association between ambient tem-
tionally, we used the most advanced modelling ap- perature and mortality risk and burden: time series study in 272
proaches, based on state-of-the-art methodologies in main Chinese cities. BMJ. 2018;363:k4306. https://doi.org/10.
environmental epidemiology, which allowed us to 1136/bmj.k4306.
4 Achebak H, Devolder D, Ingole V, Ballester J. Reversal of the sea-
obtain robust estimations while accounting for complex sonality of temperature-attributable mortality from respiratory dis-
temporal patterns in the data. On the other hand, our eases in Spain. Nat Commun. 2020;11:2457.
5 Michelozzi P, Accetta G, De Sario M, et al. High temperature and
findings might be affected by a selection bias if the hospitalizations for cardiovascular and respiratory causes in 12
characteristics of patients admitted to the hospital differ european cities. Am J Respir Crit Care Med. 2009;179:383–389.
systematically by season, and therefore, they should be 6 Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML,
Peng RD. Heat-related emergency hospitalizations for respiratory
interpreted with caution. Although we controlled for age diseases in the medicare population. Am J Respir Crit Care Med.
of the patients in the regression models, a variable 2013;187:1098–1103.
showing a clear seasonal fluctuation (see Appendix, p 4), 7 Martínez-Solanas È, Basagaña X. Temporal changes in the effects
of ambient temperatures on hospital admissions in Spain. PLoS
other patient characteristics (eg, comorbidities) were not One. 2019;14:e0218262.
taken into account because they were not available. 8 Xu R, Zhao Q, Coelho MSZS, et al. Socioeconomic level and as-
Moreover, the study is limited to two Spanish provinces, sociations between heat exposure and all-cause and cause-specific
hospitalization in 1,814 Brazilian cities: a nationwide case-
and therefore, the generalizability our findings might be crossover study. PLoS Med. 2020;17:1–18.
limited. 9 Lim Y-H, Hong Y-C, Kim H. Effects of diurnal temperature range
on cardiovascular and respiratory hospital admissions in Korea. Sci
Contributors Total Environ. 2012;417–418:55–60.
10 Zhan Z, Zhao Y, Pang S, Zhong X, Wu C, Ding Z. Temperature
HA designed the study, did the statistical analysis and drafted the
change between neighboring days and mortality in United
manuscript. JGA, GR and JB contributed to the study design and edited States: a nationwide study. Sci Total Environ. 2017;584–585:
the manuscript. ZC generated the air pollution data and edited the 1152–1161.
manuscript. RFMT processed the meteorological data. All authors 11 Xu R, Zhao Q, Coelho MSZS, et al. Socioeconomic inequality in
revised the manuscript and approved the final version. vulnerability to all-cause and cause-specific hospitalisation associ-
ated with temperature variability: a time-series study in 1814 Bra-
Data sharing statement zilian cities. Lancet Planet Health. 2020;4:e566–e576.
Health data can be obtained from the Spanish National Institute 12 Arsad FS, Hod R, Ahmad N, et al. The impact of heatwaves on
mortality and morbidity and the associated vulnerability factors:
of Statistics (INE) under request (https://www.ine.es/infoine/?L=1).
a systematic review. Int J Environ Res Public Health. 2022;19:
Meteorological data can be freely obtained from E-OBS gridded dataset 16356.
(https://doi.org/10.24381/cds.151d3ec6). Air pollution data are available 13 IPCC. Climate change 2021: the physical science basis. In: Working
from the corresponding author upon reasonable request. group I contribution to the IPCC sixth assessment report. 2021. https://
doi.org/10.1017/9781009157896.
Declaration of interests 14 Soriano JB, Kendrick PJ, Paulson KR, et al. Prevalence and attrib-
We declare no competing interests. utable health burden of chronic respiratory diseases, 1990–2017: a
systematic analysis for the Global Burden of Disease Study 2017.
Lancet Respir Med. 2020;8:585–596.
Acknowledgements 15 Lutz W, Sanderson W, Scherbov S. The coming acceleration of
HA gratefully acknowledges funding from the European Union’s Ho- global population ageing. Nature. 2008;451:716–719.
rizon Europe research and innovation programme under grant agree- 16 Huang K, Li X, Liu X, Seto KC. Projecting global urban land
ment No 101065876 (MSCA Postdoctoral Fellowship TEMP-MOMO). expansion and heat island intensification through 2050. Environ Res
HA, ZC, RFMT, and JB acknowledge funding from the European Lett. 2019;14:114037.
Union’s Horizon 2020 research and innovation programme under grant 17 Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes:
agreement No 865564 (European Research Council Consolidator Grant health risks. Lancet. 2021;398:698–708.
18 Martínez-Solanas È, Quijal-Zamorano M, Achebak H, et al. Pro-
EARLY-ADAPT, https://www.early-adapt.eu/). JB acknowledges fund-
jections of temperature-attributable mortality in Europe: a time
ing from the European Union’s Horizon Europe Research and Inno-
series analysis of 147 contiguous regions in 16 countries. Lancet
vation Programme under grant agreements No 101069213 (European Planet Health. 2021;5:e446–e454.
Research Council Proof-of-Concept HHS-EWS) and 101123382 (Euro- 19 Quijal-Zamorano M, Martínez-Solanas È, Achebak H, et al. Sea-
pean Research Council Proof-of-Concept FORECAST-AIR), and from sonality reversal of temperature attributable mortality projections
the Spanish Ministry of Science and Innovation under grant agreement due to previously unobserved extreme heat in Europe. Lancet Planet
No RYC2018-025446-I (programme Ramón y Cajal). ISGlobal authors Health. 2021;5:e573–e575.
acknowledge support from the grant CEX2018-000806-S funded by 20 Lee W, Kim Y, Sera F, et al. Projections of excess mortality related
MCIN/AEI/10.13039/501100011033, and support from the Generalitat to diurnal temperature range under climate change scenarios: a
multi-country modelling study. Lancet Planet Health. 2020;4:e512–
de Catalunya through the CERCA Program. We acknowledge the E-OBS
e521.
dataset from the EU-FP6 project UERRA (http://www.uerra.eu) and the 21 Madaniyazi L, Armstrong B, Chung Y, et al. Seasonal variation in
Copernicus Climate Change Service, and the data providers in the mortality and the role of temperature: a multi-country multi-city
ECA&D project (https://www.ecad.eu). study. Int J Epidemiol. 2022;51:122–133.
www.thelancet.com Vol 35 December, 2023 9
Articles
22 Upshur RE, Moineddin R, Crighton E, Kiefer L, Mamdani M. 36 Gelaro R, McCarty W, Suárez MJ, et al. The modern-era retro-
Simplicity within complexity: seasonality and predictability of hos- spective analysis for research and applications, version 2 (MERRA-
pital admissions in the province of Ontario 1988–2001, a 2). J Clim. 2017;30:5419–5454.
population-based analysis. BMC Health Serv Res. 2005;5:13. 37 Muñoz-Sabater J. ERA5-land hourly data from 1981 to present.
23 Wise RA, Calverley PM, Carter K, Clerisme-Beaty E, Metzdorf N, Copernicus Climate Change Service (C3S) Climate Data Store
Anzueto A. Seasonal variations in exacerbations and deaths in pa- (CDS); 2019. https://doi.org/10.24381/cds.e2161bac.
tients with COPD during the TIOSPIR® trial. Int J Chron Obstruct 38 Meijer JR, Huijbregts MAJ, Schotten KCGJ, Schipper AM. Global
Pulmon Dis. 2018;13:605–616. patterns of current and future road infrastructure. Environ Res Lett.
24 Keller K, Hobohm L, Münzel T, Konstantinides SV, Lankeit M. Sex- 2018;13:064006.
specific and age-related seasonal variations regarding incidence and 39 Ching J, Mills G, Bechtel B, et al. WUDAPT: an urban weather,
in-hospital mortality of pulmonary embolism in Germany. ERJ climate, and environmental modeling infrastructure for the
Open Res. 2020;6:00181-2020. https://doi.org/10.1183/23120541. Anthropocene. Bull Am Meteorol Soc. 2018;99:1907–1924.
00181-2020. 40 INE. Population and housing censuses. https://www.ine.es/dyngs/
25 Ho ATN, Shmelev A, Charbek E. Trends and seasonal variation of INEbase/en/operacion.htm?c=Estadistica_C&cid=1254736176992&
hospitalization and mortality of interstitial lung disease in the menu=resultados&idp=1254735572981. Accessed October 25, 2022.
United States from 2006 to 2016. Respir Res. 2020;21:152. 41 Madaniyazi L, Tobias A, Kim Y, Chung Y, Armstrong B,
26 Lam HCY, Li AM, Chan EYY, Goggins WB. The short-term asso- Hashizume M. Assessing seasonality and the role of its potential
ciation between asthma hospitalisations, ambient temperature, drivers in environmental epidemiology: a tutorial. Int J Epidemiol.
other meteorological factors and air pollutants in Hong Kong: a 2022;51:1677–1686.
time-series study. Thorax. 2016;71:1097–1109. 42 Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-
27 Konstantinoudis G, Minelli C, Vicedo-Cabrera AM, Ballester J, linear models. Stat Med. 2010;29:2224–2234.
Gasparrini A, Blangiardo M. Ambient heat exposure and COPD 43 Gasparrini A, Leone M. Attributable risk from distributed lag
hospitalisations in England: a nationwide case-crossover study models. BMC Med Res Methodol. 2014;14:1–8.
during 2007–2018. Thorax. 2022;77:1098–1104. 44 Martínez-Solanas È, Basagaña X. Temporal changes in
28 Qiu H, Sun S, Tang R, Chan K-P, Tian L. Pneumonia hospitali- temperature-related mortality in Spain and effect of the imple-
zation risk in the elderly attributable to cold and hot temperatures mentation of a Heat Health Prevention Plan. Environ Res. 2019;
in Hong Kong, China. Am J Epidemiol. 2016;184:570–578. 169:102–113.
29 INE. Death statistics according to cause of death. https://ine.es/ 45 Mora C, Counsell CWW, Bielecki CR, Louis LV. Twenty-seven ways
dyngs/INEbase/en/operacion.htm?c=Estadistica_C&cid=12547361 a heat wave can kill you. Circ Cardiovasc Qual Outcomes. 2017;10:
76780&menu=ultiDatos&idp=1254735573175. Accessed December e004233. https://doi.org/10.1161/CIRCOUTCOMES.117.004233.
12, 2022. 46 Chen K, Dubrow R, Breitner S, et al. Triggering of myocardial
30 Giorgi F. Climate change hot-spots. Geophys Res Lett. 2006;33:1–4. infarction by heat exposure is modified by medication intake. Nat
31 Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expec- Cardiovasc Res. 2022;1:727–731.
tancy, years of life lost, and all-cause and cause-specific mortality for 47 Hayes D, Collins PB, Khosravi M, Lin R-L, Lee L-Y. Bronchocon-
250 causes of death: reference and alternative scenarios for 2016–40 striction triggered by breathing hot humid air in patients with
for 195 countries and territories. Lancet. 2018;392:2052–2090. asthma. Am J Respir Crit Care Med. 2012;185:1190–1196.
32 Cornes RC, van der Schrier G, van den Besselaar EJM, Jones PD. 48 Hajat S, Kovats RS, Lachowycz K. Heat-related and cold-related
An ensemble version of the E-OBS temperature and precipitation deaths in England and Wales: who is at risk? Occup Environ Med.
data sets. J Geophys Res Atmos. 2018;123:9391–9409. 2007;64:93–100.
33 European Environment Agency (EEA). European Environment In- 49 Achebak H, Devolder D, Ballester J. Heat-related mortality trends
formation and Observation Network (Eionet). https://www.eionet. under recent climate warming in Spain: a 36-year observational
europa.eu/. study. PLoS Med. 2018;15:e1002617.
34 Aerosol NASA. Robotic Network (AERONET). https://aeronet.gsfc. 50 Yanovich R, Ketko I, Charkoudian N. Sex differences in human
nasa.gov/. thermoregulation: relevance for 2020 and beyond. Physiology.
35 Copernicus Atmosphere Monitoring Service (CAMS). CAMS global 2020;35:177–184.
reanalysis (EAC4). https://ads.atmosphere.copernicus.eu/cdsa 51 Rosano GMC, Vitale C, Marazzi G, Volterrani M. Menopause and
pp#!/dataset/cams-global-reanalysis-eac4?tab=overview. cardiovascular disease: the evidence. Climacteric. 2007;10:19–24.
10 www.thelancet.com Vol 35 December, 2023
You might also like
- American Board of Family MedicineDocument71 pagesAmerican Board of Family MedicineMohamed Elmasry100% (4)
- КРОК-1 (microbiology 2009-2020) -перетвореноDocument57 pagesКРОК-1 (microbiology 2009-2020) -перетвореноMA1910o nii odoi patterson100% (1)
- Mosco's Clerking Guide..Document88 pagesMosco's Clerking Guide..temitopeNo ratings yet
- Case Study PN Pcap C FinalDocument50 pagesCase Study PN Pcap C FinalKimberly Milaran33% (3)
- Pulmonology Step2 CKDocument22 pagesPulmonology Step2 CKsarwat86% (7)
- Chapter 19Document29 pagesChapter 19Carmela Laraya Alayon100% (3)
- 1 s2.0 S0013935122018163 MainDocument12 pages1 s2.0 S0013935122018163 MainEducation serviceNo ratings yet
- Unhealthy Effects of Atmospheric Temperature and Pressure On The Occurrence of Myocardial Infarction and Coronary DeathsDocument7 pagesUnhealthy Effects of Atmospheric Temperature and Pressure On The Occurrence of Myocardial Infarction and Coronary DeathsrobsonwiNo ratings yet
- Seasonal StudyDocument9 pagesSeasonal StudyumerspkNo ratings yet
- Journal Pre-Proof: Environmental ResearchDocument31 pagesJournal Pre-Proof: Environmental ResearchMohammed Shuaib AhmedNo ratings yet
- Lungs in A Warming WorldDocument5 pagesLungs in A Warming WorldEnamul HaqueNo ratings yet
- Indiv Crit FelicianoDocument3 pagesIndiv Crit FelicianoNathaniel FelicianoNo ratings yet
- Aen Kelompok 1Document10 pagesAen Kelompok 1mahkda anjaniNo ratings yet
- Pneumonia 3Document8 pagesPneumonia 3furqan92No ratings yet
- Complicatii PneumonieDocument9 pagesComplicatii PneumonieTatiana JalbaNo ratings yet
- Geographical Variation in Relative Risks Associated With C - 2016 - EnvironmentDocument9 pagesGeographical Variation in Relative Risks Associated With C - 2016 - Environmentkunyang1983No ratings yet
- The Effect of Air Temperature On Hospital AdmissioDocument8 pagesThe Effect of Air Temperature On Hospital AdmissioK173730 Eisha Tir RaaziaNo ratings yet
- Journal Pone 0224563Document13 pagesJournal Pone 0224563Jhony FloresNo ratings yet
- Geriatric Medicine and Gerontology: Association Between Extreme Cold Weather Temperatures and Mortality in GreeceDocument4 pagesGeriatric Medicine and Gerontology: Association Between Extreme Cold Weather Temperatures and Mortality in GreeceLeonidas IoannouNo ratings yet
- Astma Impact IncovidDocument9 pagesAstma Impact IncovidRosintchi MirsalNo ratings yet
- The Pathophysiology and Dangers of Silent Hypoxemia in COVID-19 Lung InjuryDocument24 pagesThe Pathophysiology and Dangers of Silent Hypoxemia in COVID-19 Lung Injurypulmo unandNo ratings yet
- Science of The Total Environment: Elisavet Tsekeri Dionysia Kolokotsa Mat SantamourisDocument10 pagesScience of The Total Environment: Elisavet Tsekeri Dionysia Kolokotsa Mat SantamouriskikyflNo ratings yet
- A Comparative Analysis of The Outcomes of PatientsDocument5 pagesA Comparative Analysis of The Outcomes of PatientsCerveza La GacetaNo ratings yet
- 2020 Thoraxjnl 2020 216549.fullDocument17 pages2020 Thoraxjnl 2020 216549.fullMichelleNo ratings yet
- Neumonía Artículo 2Document48 pagesNeumonía Artículo 2alejmendoza63No ratings yet
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of LiteratureDocument5 pagesPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of Literatureamelya asryNo ratings yet
- Pi Is 0749070421000397Document14 pagesPi Is 0749070421000397Vlady78No ratings yet
- Asma Exacerbacioes EpidemiologiaDocument7 pagesAsma Exacerbacioes Epidemiologiahebert ramosNo ratings yet
- Jogh 09 020421Document12 pagesJogh 09 020421LindaNo ratings yet
- Environmental Risk Factors For Pneumocystis Pneumonia Hospitalizations in HIV PatientsDocument8 pagesEnvironmental Risk Factors For Pneumocystis Pneumonia Hospitalizations in HIV PatientsKartika LuthfianaNo ratings yet
- Profiling of Lung SARS-CoV-2 and Influenza Virus Infection Dissects Virus-Specific Host Responses and Gene SignaturesDocument19 pagesProfiling of Lung SARS-CoV-2 and Influenza Virus Infection Dissects Virus-Specific Host Responses and Gene Signaturesbrhpcn2rrfNo ratings yet
- Tuberculosis and Lung Damage: From Epidemiology To PathophysiologyDocument20 pagesTuberculosis and Lung Damage: From Epidemiology To PathophysiologyDyan TonyNo ratings yet
- 10.1016@j.yjmcc.2020.04.031 Hipertensi Dan Covid 19Document22 pages10.1016@j.yjmcc.2020.04.031 Hipertensi Dan Covid 19Sulis TioNo ratings yet
- Temporal Variation of The Temperature-Mortality Association in Spain: A Nationwide AnalysisDocument10 pagesTemporal Variation of The Temperature-Mortality Association in Spain: A Nationwide AnalysisPatricio GonzálezNo ratings yet
- Asthma in COVID-19 Hospitalizations: An Overestimated Risk Factor?Document13 pagesAsthma in COVID-19 Hospitalizations: An Overestimated Risk Factor?Analia De LucaNo ratings yet
- Jurnal Cohort Stroke 3Document6 pagesJurnal Cohort Stroke 3afifah.nurfaidahNo ratings yet
- Hub TBC DG CopdDocument7 pagesHub TBC DG CopdAmalNo ratings yet
- Relación Entre Bronquiolitis Aguda Con Factores Climáticos y Contaminación AmbientalDocument6 pagesRelación Entre Bronquiolitis Aguda Con Factores Climáticos y Contaminación AmbientalCarla Miranda AracenaNo ratings yet
- Patgen Covid 19 Induced ArdsDocument31 pagesPatgen Covid 19 Induced ArdssefinafinaNo ratings yet
- MainDocument14 pagesMainCarlos MejiaNo ratings yet
- American Thoracic Society DocumentsDocument11 pagesAmerican Thoracic Society DocumentsNicolaeDincaNo ratings yet
- Cap AsmaDocument10 pagesCap AsmaAuliaNo ratings yet
- Plural ArticleDocument16 pagesPlural ArticleAlirio Angulo QuinteroNo ratings yet
- Soler Cataluna2005Document7 pagesSoler Cataluna2005Yara PereiraNo ratings yet
- Winter Air Pollution and Infant Bronchiolitis in ParisDocument5 pagesWinter Air Pollution and Infant Bronchiolitis in ParisrobsonwiNo ratings yet
- All-Cause Mortality During COVID-19: No Plague and A Likely Signature of Mass Homicide by Government ResponseDocument27 pagesAll-Cause Mortality During COVID-19: No Plague and A Likely Signature of Mass Homicide by Government ResponsejuanNo ratings yet
- CDC 33213 DS1Document11 pagesCDC 33213 DS1vn003411No ratings yet
- HHS Public Access: The Effects of Air Pollution and Temperature On COPDDocument15 pagesHHS Public Access: The Effects of Air Pollution and Temperature On COPDWahyuNo ratings yet
- Effect of Heat and Humidity On The Incidence and Mortality Due To COVID-19 Pandemic in European CountriesDocument10 pagesEffect of Heat and Humidity On The Incidence and Mortality Due To COVID-19 Pandemic in European Countriesriffat.asifaNo ratings yet
- All causemortalityduringCOVID 19 - 3Document27 pagesAll causemortalityduringCOVID 19 - 3maria eugenia maya marinNo ratings yet
- Written by Yamin Khan, PHD and Sarah Tilly: NtroductionDocument10 pagesWritten by Yamin Khan, PHD and Sarah Tilly: NtroductionChikezie OnwukweNo ratings yet
- Ambient Temperature and Outpatient Visits For Acute Ex 2015 Biomedical and EDocument4 pagesAmbient Temperature and Outpatient Visits For Acute Ex 2015 Biomedical and Eluis11256No ratings yet
- The Effect of High Temperatures On Cause-Specific Mortality in England and WalesDocument7 pagesThe Effect of High Temperatures On Cause-Specific Mortality in England and WalesRei Akai YagamiNo ratings yet
- Cambio Climático y AsmaDocument3 pagesCambio Climático y Asmaagonzal1974No ratings yet
- Projek 2Document17 pagesProjek 2sweetykalaNo ratings yet
- Review Analysis WHO-URTIDocument18 pagesReview Analysis WHO-URTIrizkaNo ratings yet
- Sars-Cov-2: A Storm Is Raging: Savannah F. Pedersen, Ya-Chi HoDocument10 pagesSars-Cov-2: A Storm Is Raging: Savannah F. Pedersen, Ya-Chi HoLucia Estevez CobelaNo ratings yet
- Current Incidence and Outcome of The Acute Respiratory Distress SyndromeDocument6 pagesCurrent Incidence and Outcome of The Acute Respiratory Distress Syndromedarius2311No ratings yet
- Comparison Between Patients Hospitalized With Influenza and COVID-19 at A Tertiary Care CenterDocument7 pagesComparison Between Patients Hospitalized With Influenza and COVID-19 at A Tertiary Care CenterSofiaNo ratings yet
- Acute Respiratory Distress Syndrome: Etiology, Pathogenesis, and Summary On ManagementDocument15 pagesAcute Respiratory Distress Syndrome: Etiology, Pathogenesis, and Summary On ManagementLiri AndiyaniNo ratings yet
- Relationship Between Extravascular Lung Water and Severity Categories of Acute Respiratory Distress Syndrome by The Berlin DefinitionDocument9 pagesRelationship Between Extravascular Lung Water and Severity Categories of Acute Respiratory Distress Syndrome by The Berlin DefinitionVictor Euclides Briones MoralesNo ratings yet
- 97 102 Pintaric I Sur PDFDocument6 pages97 102 Pintaric I Sur PDFpedaedrNo ratings yet
- (2247059X - Pneumologia) Asthma-COPD-Bronchiectasis Combination - An Unstudied TripletDocument3 pages(2247059X - Pneumologia) Asthma-COPD-Bronchiectasis Combination - An Unstudied TripletConstantin PopescuNo ratings yet
- Impact of Immunoglobulin E and Airway Obstruction On BronchiectasisDocument7 pagesImpact of Immunoglobulin E and Airway Obstruction On BronchiectasisRichie Irvanto CiandraNo ratings yet
- Science of The Total EnvironmentDocument7 pagesScience of The Total EnvironmentFabio Galvan GilNo ratings yet
- FILM177 Lesson Plan 1Document3 pagesFILM177 Lesson Plan 1Jayvee FerrerNo ratings yet
- WHO IMAI Acute - Care PDFDocument138 pagesWHO IMAI Acute - Care PDFJohn Philip TiongcoNo ratings yet
- 30 Facts You NEED To Know Your Covid Cribsheet - OffGuardianDocument5 pages30 Facts You NEED To Know Your Covid Cribsheet - OffGuardianjohnsmithdosNo ratings yet
- Nosocomial InfectionDocument16 pagesNosocomial Infectionmarissa ulkhairNo ratings yet
- Disnea - Rosen - 230526 - 125351Document10 pagesDisnea - Rosen - 230526 - 125351Pablo BetancourtNo ratings yet
- Broncho PneumoniaDocument23 pagesBroncho Pneumoniaanon-84769398% (43)
- State Senator Darryl Rouson Aug. 27 LetterDocument1 pageState Senator Darryl Rouson Aug. 27 LetterWTSP 10No ratings yet
- Textbook Atlas of Infectious Disease Pathology 1St Edition Bryan H Schmitt Eds Ebook All Chapter PDFDocument53 pagesTextbook Atlas of Infectious Disease Pathology 1St Edition Bryan H Schmitt Eds Ebook All Chapter PDFdonna.riebel227100% (20)
- Step 2 CK QuestionsDocument8 pagesStep 2 CK QuestionsIrfan Majeed50% (2)
- Noninvasive Ventilation HandbookDocument88 pagesNoninvasive Ventilation HandbookPablo100% (1)
- The Vaccine Book 2nd EditionDocument61 pagesThe Vaccine Book 2nd Editiontom.dimaggio515100% (41)
- Model Paper 4Document22 pagesModel Paper 4Mobin Ur Rehman KhanNo ratings yet
- BronchiolitisDocument7 pagesBronchiolitisNader SmadiNo ratings yet
- 1 Daftar PustakaDocument9 pages1 Daftar PustakaGalihCandraKusumaNo ratings yet
- Bronchopneumonia - MedscapeDocument7 pagesBronchopneumonia - MedscapecleoaerNo ratings yet
- Chest Physiotherapy For Pneumonia in Children.9Document1 pageChest Physiotherapy For Pneumonia in Children.9Julenda CintarinovaNo ratings yet
- VivaChek Bio Products Catalog (En) 092421Document14 pagesVivaChek Bio Products Catalog (En) 092421Emmanuel BonillaNo ratings yet
- Quizlet (4) MMMMMMDocument30 pagesQuizlet (4) MMMMMMnaimNo ratings yet
- COPARDocument48 pagesCOPARJasmin Jacob100% (2)
- Administrative Order 2022-0010: Guidelines On TB-HIV Services Integration For Universal Health Care (UHC) ImplementationDocument22 pagesAdministrative Order 2022-0010: Guidelines On TB-HIV Services Integration For Universal Health Care (UHC) ImplementationJovania B.No ratings yet
- Nursing Care Plan Neonatal PneumoniaDocument2 pagesNursing Care Plan Neonatal Pneumoniaderic93% (42)
- Acute Viral Encephalitis in ChildrenDocument16 pagesAcute Viral Encephalitis in ChildrenCF PonceNo ratings yet
- Introduction To Critical Care Nursing 7th EditionDocument61 pagesIntroduction To Critical Care Nursing 7th Editiondana.nelson19598% (63)
- Profile of PoblacionDocument38 pagesProfile of PoblacionmpdoNo ratings yet