Professional Documents
Culture Documents
MGH Housestaff Manual 2023-2024 Page 146
MGH Housestaff Manual 2023-2024 Page 146
Uploaded by
sr652dmx9tCopyright:
Available Formats
You might also like
- Fast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesFrom EverandFast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesNo ratings yet
- LeukemiaDocument12 pagesLeukemiaDingdong-didiNo ratings yet
- 1 - Hodgkin's LymphomaDocument12 pages1 - Hodgkin's LymphomaDiana MitreaNo ratings yet
- P ' R O R N 2008: Etiology/EpidemiologyDocument10 pagesP ' R O R N 2008: Etiology/EpidemiologyDiana MitreaNo ratings yet
- 13 Recent Advances in Management of Hodhkin's LymphomaDocument63 pages13 Recent Advances in Management of Hodhkin's LymphomaVipul BansalNo ratings yet
- Advances in LymphomaDocument20 pagesAdvances in LymphomaSaiKrishnaReddySeemalaNo ratings yet
- P ' R O R N 2008: Etiology/EpidemiologyDocument11 pagesP ' R O R N 2008: Etiology/EpidemiologyDiana MitreaNo ratings yet
- ASH Hematology Review Series - Hodgkin Lymphoma - HerreraDocument69 pagesASH Hematology Review Series - Hodgkin Lymphoma - HerreraИван НегарэNo ratings yet
- Clasificacion de Linfomas BDocument25 pagesClasificacion de Linfomas BFiorella SalvatNo ratings yet
- MiscDocument29 pagesMiscsam2000samNo ratings yet
- Applied Therapeutic Koda Kimble 10e 2012 - 1Document6 pagesApplied Therapeutic Koda Kimble 10e 2012 - 1Tinsy ClaudiaNo ratings yet
- Hodgkins Icp Final Slide DeckDocument7 pagesHodgkins Icp Final Slide DeckNutan JoshiNo ratings yet
- THORAKXDocument59 pagesTHORAKXwihelminaNo ratings yet
- Linfoma Hodgkin SigloxxiDocument27 pagesLinfoma Hodgkin SigloxxiLucas OchoaNo ratings yet
- WhddidsorhkDocument50 pagesWhddidsorhkestherin909No ratings yet
- 18c. Lymphoma EditedDocument36 pages18c. Lymphoma EditedMUHAMMAD BAGIR ALJUFRINo ratings yet
- Boala HodgkinDocument44 pagesBoala HodgkinAlice Monica BeşaNo ratings yet
- Lymphoproliferative DisordersDocument29 pagesLymphoproliferative DisordersShaza ElkourashyNo ratings yet
- Boala Hodgkin Curs 2016Document68 pagesBoala Hodgkin Curs 2016LittleThingsInside100% (1)
- 11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaDocument74 pages11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaMita AdrianiNo ratings yet
- Hodgkin'S Disease AND Non-Hodgkin'S LymphomaDocument42 pagesHodgkin'S Disease AND Non-Hodgkin'S LymphomaRayya TriandaNo ratings yet
- Bone Pain, Lymphadenopathy,: CD34, CD33Document2 pagesBone Pain, Lymphadenopathy,: CD34, CD33Gabriella Santa LuciaNo ratings yet
- Alperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFDocument2 pagesAlperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFflashjetNo ratings yet
- Lymphoma NotesDocument3 pagesLymphoma Notesmichael karpNo ratings yet
- Non-Hodgkin's LymphomaDocument45 pagesNon-Hodgkin's LymphomaIvy Dane BalanayNo ratings yet
- GCT in Males by Dr. Musaib MushtaqDocument44 pagesGCT in Males by Dr. Musaib MushtaqDr. Musaib MushtaqNo ratings yet
- Gastric CancerDocument5 pagesGastric Cancerahmed.ali33266No ratings yet
- Hodgkin Lymphoma KlapperDocument17 pagesHodgkin Lymphoma KlapperAthika RodhyaNo ratings yet
- Hepatology MRCP1Document87 pagesHepatology MRCP1Raouf Ra'fat SolimanNo ratings yet
- 2021 How I Treat Adult T-Cell Leukemia-LymphomaDocument12 pages2021 How I Treat Adult T-Cell Leukemia-Lymphomamateusmalacarne96No ratings yet
- Uci Protocol Brighman BostonDocument43 pagesUci Protocol Brighman BostonAnonymous ZUaUz1wwNo ratings yet
- 14 HF-Limfoma GI TractDocument27 pages14 HF-Limfoma GI TractNur akilaNo ratings yet
- 18c. Lymphoma 1editedDocument36 pages18c. Lymphoma 1editedMuhammad DaviqNo ratings yet
- Virus ChartDocument18 pagesVirus Chartezaz000No ratings yet
- Armand Et Al. - 2013 - Detection of Circulating Tumour DNA in Patients With Aggressive B-Cell Non-Hodgkin Lymphoma PDFDocument4 pagesArmand Et Al. - 2013 - Detection of Circulating Tumour DNA in Patients With Aggressive B-Cell Non-Hodgkin Lymphoma PDFflashjetNo ratings yet
- Hodgkins Lymphoma by Dr. Anum UsmanDocument48 pagesHodgkins Lymphoma by Dr. Anum UsmanHumar Haider100% (1)
- Lymphoma NewDocument36 pagesLymphoma Newmedo2002alfadaliNo ratings yet
- Lymphomas of The Head and Neck - Practice Essentials, Background, PathophysiologyDocument6 pagesLymphomas of The Head and Neck - Practice Essentials, Background, Pathophysiologymiranddaelvira02No ratings yet
- Castillo 2018Document3 pagesCastillo 201890STRATOVARIUS90No ratings yet
- Lymphoma B CellDocument47 pagesLymphoma B CellJessica SantillanNo ratings yet
- Lymphoma: Cells/ul 5,000 Cells/ul Is CLL and Should Be Staged As Such 1.5 CMDocument10 pagesLymphoma: Cells/ul 5,000 Cells/ul Is CLL and Should Be Staged As Such 1.5 CMJohn Robert AcostaNo ratings yet
- Hodgkin's DiseaseDocument58 pagesHodgkin's Diseasealibayaty1No ratings yet
- DD HematologyDocument43 pagesDD HematologyDemianaNo ratings yet
- LymphomaDocument34 pagesLymphomaSaiKrishnaReddySeemala0% (1)
- EAHP With Corrections (V2) - Changes by GCC (On 10-4-19)Document2 pagesEAHP With Corrections (V2) - Changes by GCC (On 10-4-19)Christopher JulienNo ratings yet
- Leucemia Linfoide CrónicaDocument17 pagesLeucemia Linfoide CrónicaJose AbadiaNo ratings yet
- ENT CPC - Tonsil ProblemsDocument3 pagesENT CPC - Tonsil ProblemsrieuxNo ratings yet
- 2017 08 15 ConsensusGuidelinesHSCTinMDSandJMML v1-3Document19 pages2017 08 15 ConsensusGuidelinesHSCTinMDSandJMML v1-3cristina_zaharia865440No ratings yet
- ImmunologyDocument38 pagesImmunologygautam harshNo ratings yet
- Can We Use Epigenetics To Prime Chemoresistant Lymphomas?Document10 pagesCan We Use Epigenetics To Prime Chemoresistant Lymphomas?nutnut29No ratings yet
- Lab Values Hema: All Values Varies With Age or Sex, or Ethnic SubgroupDocument9 pagesLab Values Hema: All Values Varies With Age or Sex, or Ethnic SubgroupXerxyllXyreaneLinaoNo ratings yet
- April RecallsDocument4 pagesApril Recallsfritzie dara f adjilaniNo ratings yet
- Malignant Lymphoma: Nur MuallimaDocument34 pagesMalignant Lymphoma: Nur MuallimaSRi RamadhaniNo ratings yet
- ENDODocument3 pagesENDOOmar Picado RoqueNo ratings yet
- Riska Tugas DR - JusfeniDocument19 pagesRiska Tugas DR - Jusfeniriska oktarinda utamiNo ratings yet
- Burkitts Lymphoma 2015 PDFDocument9 pagesBurkitts Lymphoma 2015 PDFAffra CahyoNo ratings yet
- 2022 HRS - Aggressive B-Cell Lymphomas FINALDocument80 pages2022 HRS - Aggressive B-Cell Lymphomas FINALИван НегарэNo ratings yet
- Abbreviation Key: Abbrev Full Spell-OutDocument9 pagesAbbreviation Key: Abbrev Full Spell-Outkairton6648No ratings yet
- Diagnostic Tests PDFDocument2 pagesDiagnostic Tests PDFBenedict AlvarezNo ratings yet
- S.N IM2 SOAP P3 Week 3Document28 pagesS.N IM2 SOAP P3 Week 3Rayane MahmoudNo ratings yet
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseFrom EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseNo ratings yet
- KP 2.2.5.1 - LimfadenopatiDocument38 pagesKP 2.2.5.1 - LimfadenopatiArie160No ratings yet
- Cancers of The Blood: Leukemia and LymphomaDocument46 pagesCancers of The Blood: Leukemia and LymphomaMaica LectanaNo ratings yet
- Imunohistochimie LNHDocument4 pagesImunohistochimie LNHHaralambie SarbuNo ratings yet
- Hematology Oncology - LymphomaDocument1 pageHematology Oncology - LymphomaEugen MNo ratings yet
- Malignant LymphomaDocument29 pagesMalignant LymphomaSurya BudikusumaNo ratings yet
- Malignant Disorders of Leukocytes: Supachai A. Basit, RMT, PHDDocument109 pagesMalignant Disorders of Leukocytes: Supachai A. Basit, RMT, PHDChatie PipitNo ratings yet
- Hodgkin's DiseaseDocument4 pagesHodgkin's DiseaseLillabinNo ratings yet
- OcuandAdnexalLymphom PDFDocument126 pagesOcuandAdnexalLymphom PDFJovan PopovićNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Leukemia What Is Leukemia?Document2 pagesLeukemia What Is Leukemia?Ctn ZQNo ratings yet
- Leukemia Cutis in Childhood Acute Myeloid.6Document3 pagesLeukemia Cutis in Childhood Acute Myeloid.6fikriafisNo ratings yet
- Highlights What Is Minimal Residual Disease (MRD) ?Document6 pagesHighlights What Is Minimal Residual Disease (MRD) ?ANo ratings yet
- Laporan IKM KSM PK FEBRUARI 2022Document27 pagesLaporan IKM KSM PK FEBRUARI 2022Nur iffahNo ratings yet
- Pathology Revision E6.5Document129 pagesPathology Revision E6.5massprithiv58No ratings yet
- 18 Lymphoma - Libre PathologyDocument13 pages18 Lymphoma - Libre PathologyfadoNo ratings yet
- Hematology Oncology - LeukemiaDocument2 pagesHematology Oncology - LeukemiaEugen MNo ratings yet
- DapusDocument2 pagesDapusrahmadNo ratings yet
- Pediatric LeukemiasDocument42 pagesPediatric LeukemiasslyfoxkittyNo ratings yet
- Acute LeukemiaDocument4 pagesAcute LeukemiaazayrhusseinNo ratings yet
- Phatophysiology of Acute Lymphoblastic LeukemiaDocument1 pagePhatophysiology of Acute Lymphoblastic LeukemiaHardiyanti RahayuNo ratings yet
- Laporan Kasus LeukemiaDocument2 pagesLaporan Kasus LeukemiaYtyNo ratings yet
- Understanding Leukemia From A Lab PerspectiveDocument48 pagesUnderstanding Leukemia From A Lab PerspectiveGlorya NathasiaNo ratings yet
- 702-Book Chapter-6692-2-10-20221018Document22 pages702-Book Chapter-6692-2-10-20221018AbinayaBNo ratings yet
- Hodgkins and Non Hodgkins LymphomaDocument5 pagesHodgkins and Non Hodgkins LymphomakakuNo ratings yet
- Non Hodgkin's LymphomaDocument31 pagesNon Hodgkin's LymphomaJeo Thomas100% (1)
- DapusDocument1 pageDapusJihadNo ratings yet
- Limfoproliferari Cronice MaligneDocument18 pagesLimfoproliferari Cronice MaligneAlice MuscaNo ratings yet
- Acute Leukemia: Thirunavukkarasu MurugappanDocument22 pagesAcute Leukemia: Thirunavukkarasu MurugappanFelix Allen100% (1)
- قلق الموت من السرطانDocument212 pagesقلق الموت من السرطانBouchareb AhmedNo ratings yet
MGH Housestaff Manual 2023-2024 Page 146
MGH Housestaff Manual 2023-2024 Page 146
Uploaded by
sr652dmx9tOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MGH Housestaff Manual 2023-2024 Page 146
MGH Housestaff Manual 2023-2024 Page 146
Uploaded by
sr652dmx9tCopyright:
Available Formats
TOC
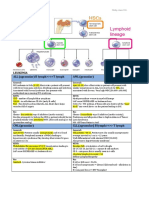
Oncology Lymphadenopathy & Lymphoma
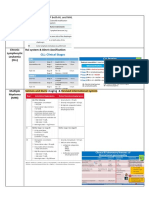
E V A L U A T I O N O F L Y M P H A D E N O P A T H Y (AFP 2016;94:896)
• Generalized LAD: HIV, EBV/CMV/toxo, mycobacteria, SLE, meds (e.g. phenytoin), sarcoid, lymphoma, Castleman’s, Kikuchi dz, IgG4
• Localized LAD: cervical (EBV/CMV/toxo, mycobacteria, lymphoma), supraclav. (malignancy), axillary (infection, breast), inguinal (STI)
• Hx: exposures, travel, meds, B Sx (fever, drenching night sweats, >10% unintentional wt loss in 6mo), other s/sx of infxn/malignancy
• Exam: localization (think about area of nodal drainage), size (abnormal >1cm), consistency, fixation, tenderness (inflammation)
• Labs: CBC/diff, LDH, HIV (PCR if acute), HBV, HCV. Depending on pre-test probability: T-spot, RPR, ANA, EBV/CMV/toxo serologies
• Imaging: CT C/A/P w/ contrast, PET/CT can define node size, distribution, monitoring of response/progression (w/ Deauville scoring)
• Biopsy: consider if large (>2cm), persistent 4-6w, or increased size, w/ immunophenotyping & cytogenetics. Empiric steroids may
decrease yield of biopsy. Excisional (cells & nodal architecture) > core needle (tissue for molecular studies) > FNA (high false neg.)
LYMPHOMA GENERAL PRINCIPLES
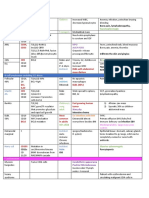
Lymphoma Staging: if Hodgkin lymphoma (HL), add “B” if B Sx. PET Deauville score (1-5): 1 = no FDG uptake; 5 = markedly FDG-avid
Stage I: 1 LN region, or single extralymphatic organ Stage III: LN groups above and below diaphragm
Stage II: ≥2 LN groups on same side of diaphragm Stage IV: disseminated ≥1 extralymphatic organs
LN region: cervical (R/L), axillary (R/L), subpectoral (R/L), mediastinal, hilar (R/L), celiac, paraaortic, mesenteric, iliac (R/L), inguinal (R/L)
Workup: PET/CT, HBV/HCV/HIV serology, G6PD, quantitative bHCG (if applicable), PFTs (+DLCO), TTE (prior to anticipated chemo)
Fertility Preservation: semen, oocyte or ovarian tissue cryopreservation. Menstrual suppression: GnRH agonists if ↓platelet expected
H O D G K I N L Y M P H O M A (NCCN; 2023)
Bimodal age distribution (Lancet 2012;380:836). Reed-Sternberg cells (CD15+ CD30+ CD20- CD45- PAX5+ PD-L1+) in inflammatory milieu
S/Sx: neck LAD, mediastinal mass, pruritis, constitutional sx, ↑Eos. Rare: burning pain w/
alcohol, nephrotic syndrome (i.e. minimal change disease), liver dysfunction, skin lesions HL International Prognostic Score (IPS)
WHO classification: nodular sclerosis (70%), mixed cellularity (25%), lymphocyte rich 1 point/factor (JCO 2012;30:3383)
Age >45 Points 5y PFS
(5%), lymphocyte depleted (<1%). Nodular lymphocyte-predominant HL is distinct entity.
Male 0 88%
Treatment: note long-term risk of cardio- and pulm-toxicity, 2° malignancy (t-AML) Stage IV 1 84%
o Stage I-II: ABVD ± XRT. Stage III-IV: ABVD vs. BV-AVD (NEJM 2018;378:331) Albumin <4 2 80%
vs. BEACOPP ± XRT. Interim PET/CT helpful for escalating vs. de-escalating tx Hb <10.5 3 74%
o Relapsed/refractory: salvage chemo + auto-HCT; brentuximab vedotin (BV); WBC ≥15,000 4 67%
PD1 inhibition (pembrolizumab or nivolumab), bendamustine, allo-HCT Lymphocytes <600 <8% ≥5 62%
NON-HODGKIN LYMPHOMA
Most common blood cancer, a/w immunosupp., autoimmunity, infection (EBV, H. pylori, HCV, HIV, HHV8, HTLV1) (Lancet 2012;380:848)
Indolent (e.g. FL): incurable, but better prognosis vs. Aggressive (e.g. DLBCL): higher chance of cure, but worse prognosis overall
Diagnosis Prevalence Clinical Features Treatment
- Stage I-II: R-CHOP + RT; Stage III-IV: R-CHOP; if DHL, consider
Aggressive, rapid growth, nodal/extranodal
more aggressive Tx (i.e. R-EPOCH); if old/frail, R-mini-CHOP
Diffuse BCL2, BCL6, or MYC translocations common
- CNS ppx controversial; some give high CNS-IPI IT MTX
Large Prognosis: IPI, cell-of-origin (GCB > ABC)
~35% - Relapsed/refractory: CD19 CAR T-cells preferred (Lancet
B-cell Double-hit lymphoma (DHL): more
2022;399:2294, NEJM 2022;386:640) vs. salvage chemo + auto-HCT
(DLBCL) aggressive subtype w/ MYC + either BCL2 or
- Trials adding drugs to R-CHOP failed in most phase III RCT so far,
BCL6 translocations. Triple-hit = ultra-HR.
except polatuzumab (NEJM 2022;386:351)
Generally indolent; occasionally aggressive - Stage I/contiguous II: RT preferred; Stage II-IV: observation, anti-
Follicular
~25% t(14:18) BCL2+. High grade = more CD20 ± bendamustine (BR), lenalidomide (LR), CHOP, or CVP
(FL)
centroblasts. FLIPI score prognostic - Monitor for transformation (rapid LN growth, ↑LDH, B symptoms)
Often indolent, painless LAD, IgM M-protein - Only treat when “active” (Blood 2018;131:2745), i.e. cytopenia, bulky
Small or chronic No risk of leukostasis unless WBC >400k disease, progressive lymphocytosis w/ increase >50% over 2mo,
lymphocytic ~5% Prognosis: Rai/Binet, IGHV unmutated (HR), autoimmune dz (AIHA, ITP), significant constitutional symptoms
(SLL/CLL) ZAP70+ (HR), CD38+ (HR), FISH (del17p = - Evolving combinations with BTKi (zanubrutinib, acalabrutinib,
HR), genetics (TP53 mut. = HR) ibrutinib), anti-CD20 (obinituzumab, rituximab), and venetoclax
Wide clinical spectrum, can involve spleen, - Stage I/non-bulk II: BR, VR-CAP, R-CHOP, or LR + R maintenance
Mantle Cell
~5% GI, BM. Leukemic (SOX11-) often indolent - Stage II-IV: RDHA + platinum, R-CHOP, NORDIC or HyperCVAD +
(MCL)
t(11;14), cyclin D1+. MIPI score prognostic auto-HCT w/ R maint. Relapsed/refractory: BTKi, CD19 CAR T-cells
Extranodal MZL (MALT): a/w sites with - Gastric MALT: if H. Pylori+, quad Tx can cure; if H. Pylori-, RT
chronic inflammation, e.g. stomach w/ H. - Nongastric extranodal localized: RT, observation
Marginal Zone pylori+ t(11;18), salivary glands (Sjogren’s), - Advanced nodal: observe, rituximab + chlorambucil/bendamustine
~10%
(MZL) thyroid (Hashimoto’s), small intestine, etc. - Splenic MZL: if HCV+, HCV Tx can lead to regression. If HCV-,
Splenic MZL: often HCV+, cryoglobulinemia Rituxumab (preferred) or splenectomy (definitive for diagnosis to
Nodal MZL: generally indolent, similar to FL differentiate from splenic diffuse red pulp small B-cell lymphoma)
Burkitt Aggressive, extranodal sites (jaw if African). - More aggressive than DLBCL treatment: R-EPOCH, R-CODOX-
~1%
(BL) ↑spont. TLS. t(8:14), cMYC+, EBV/HIV M/IVAC, R-HyperCVAD. Relapsed: chemo + auto- or allo-HCT
Diverse varieties. Peripheral T-cell (PTCL) NOS most common. Cutaneous T-cell (CTCL) i.e. Mycosis fungoides,
T-cell lymphoma ~15% Sezary syndrome (disseminated). Anaplastic large cell (ALCL) a/w ALK, breast implants. Adult T-cell leukemia/
lymphoma (ATL) a/w HTLV-1, geography (e.g. Caribbean). Enteropathy-associated T-cell (EATL) a/w celiac disease
ABVD = Doxorubicin, Bleomycin, Vinblastine, Dacarbazine CVP = Cyclophosphamide, Vincristine, Prednisolone
BEACOPP = Bleomycin, Etoposide, Doxorubicin, Cyclophosphamide, Vincristine, DHA + platinum = Rituximab, Dex, Cytarabine and Carbo-, -Cis- or Oxali-platin
Procarbazine, Prednisone EPOCH = Etoposide, Prednisone, Vincristine, Cyclophosphamide, Doxorubicin
CHOP = Cyclophosphamide, Doxorubicin, Vincristine, Prednisone HyperCVAD = Hyper-fractionated Cyclophosphamide, Vincristine, Doxorubicin,
CODOX-M/IVAC = Cyclophosphamide, Vincristine, Doxorubicin, Methotrexate, Ifosfamide, Dexamethasone, alternated w/ methotrexate & cytarabine, followed by maintenance POMP
Etoposide, Cytarabine VR-CAP = Bortezomib, Rituximab, Cyclophosphamide, Doxorubicin, Prednisone
Priyanka Pullarkat
143
You might also like
- Fast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesFrom EverandFast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesNo ratings yet
- LeukemiaDocument12 pagesLeukemiaDingdong-didiNo ratings yet
- 1 - Hodgkin's LymphomaDocument12 pages1 - Hodgkin's LymphomaDiana MitreaNo ratings yet
- P ' R O R N 2008: Etiology/EpidemiologyDocument10 pagesP ' R O R N 2008: Etiology/EpidemiologyDiana MitreaNo ratings yet
- 13 Recent Advances in Management of Hodhkin's LymphomaDocument63 pages13 Recent Advances in Management of Hodhkin's LymphomaVipul BansalNo ratings yet
- Advances in LymphomaDocument20 pagesAdvances in LymphomaSaiKrishnaReddySeemalaNo ratings yet
- P ' R O R N 2008: Etiology/EpidemiologyDocument11 pagesP ' R O R N 2008: Etiology/EpidemiologyDiana MitreaNo ratings yet
- ASH Hematology Review Series - Hodgkin Lymphoma - HerreraDocument69 pagesASH Hematology Review Series - Hodgkin Lymphoma - HerreraИван НегарэNo ratings yet
- Clasificacion de Linfomas BDocument25 pagesClasificacion de Linfomas BFiorella SalvatNo ratings yet
- MiscDocument29 pagesMiscsam2000samNo ratings yet
- Applied Therapeutic Koda Kimble 10e 2012 - 1Document6 pagesApplied Therapeutic Koda Kimble 10e 2012 - 1Tinsy ClaudiaNo ratings yet
- Hodgkins Icp Final Slide DeckDocument7 pagesHodgkins Icp Final Slide DeckNutan JoshiNo ratings yet
- THORAKXDocument59 pagesTHORAKXwihelminaNo ratings yet
- Linfoma Hodgkin SigloxxiDocument27 pagesLinfoma Hodgkin SigloxxiLucas OchoaNo ratings yet
- WhddidsorhkDocument50 pagesWhddidsorhkestherin909No ratings yet
- 18c. Lymphoma EditedDocument36 pages18c. Lymphoma EditedMUHAMMAD BAGIR ALJUFRINo ratings yet
- Boala HodgkinDocument44 pagesBoala HodgkinAlice Monica BeşaNo ratings yet
- Lymphoproliferative DisordersDocument29 pagesLymphoproliferative DisordersShaza ElkourashyNo ratings yet
- Boala Hodgkin Curs 2016Document68 pagesBoala Hodgkin Curs 2016LittleThingsInside100% (1)
- 11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaDocument74 pages11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaMita AdrianiNo ratings yet
- Hodgkin'S Disease AND Non-Hodgkin'S LymphomaDocument42 pagesHodgkin'S Disease AND Non-Hodgkin'S LymphomaRayya TriandaNo ratings yet
- Bone Pain, Lymphadenopathy,: CD34, CD33Document2 pagesBone Pain, Lymphadenopathy,: CD34, CD33Gabriella Santa LuciaNo ratings yet
- Alperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFDocument2 pagesAlperovich Et Al. - 2015 - Composite Angioimmunoblastic T-Cell and Diffuse Large B-Cell Lymphoma PDFflashjetNo ratings yet
- Lymphoma NotesDocument3 pagesLymphoma Notesmichael karpNo ratings yet
- Non-Hodgkin's LymphomaDocument45 pagesNon-Hodgkin's LymphomaIvy Dane BalanayNo ratings yet
- GCT in Males by Dr. Musaib MushtaqDocument44 pagesGCT in Males by Dr. Musaib MushtaqDr. Musaib MushtaqNo ratings yet
- Gastric CancerDocument5 pagesGastric Cancerahmed.ali33266No ratings yet
- Hodgkin Lymphoma KlapperDocument17 pagesHodgkin Lymphoma KlapperAthika RodhyaNo ratings yet
- Hepatology MRCP1Document87 pagesHepatology MRCP1Raouf Ra'fat SolimanNo ratings yet
- 2021 How I Treat Adult T-Cell Leukemia-LymphomaDocument12 pages2021 How I Treat Adult T-Cell Leukemia-Lymphomamateusmalacarne96No ratings yet
- Uci Protocol Brighman BostonDocument43 pagesUci Protocol Brighman BostonAnonymous ZUaUz1wwNo ratings yet
- 14 HF-Limfoma GI TractDocument27 pages14 HF-Limfoma GI TractNur akilaNo ratings yet
- 18c. Lymphoma 1editedDocument36 pages18c. Lymphoma 1editedMuhammad DaviqNo ratings yet
- Virus ChartDocument18 pagesVirus Chartezaz000No ratings yet
- Armand Et Al. - 2013 - Detection of Circulating Tumour DNA in Patients With Aggressive B-Cell Non-Hodgkin Lymphoma PDFDocument4 pagesArmand Et Al. - 2013 - Detection of Circulating Tumour DNA in Patients With Aggressive B-Cell Non-Hodgkin Lymphoma PDFflashjetNo ratings yet
- Hodgkins Lymphoma by Dr. Anum UsmanDocument48 pagesHodgkins Lymphoma by Dr. Anum UsmanHumar Haider100% (1)
- Lymphoma NewDocument36 pagesLymphoma Newmedo2002alfadaliNo ratings yet
- Lymphomas of The Head and Neck - Practice Essentials, Background, PathophysiologyDocument6 pagesLymphomas of The Head and Neck - Practice Essentials, Background, Pathophysiologymiranddaelvira02No ratings yet
- Castillo 2018Document3 pagesCastillo 201890STRATOVARIUS90No ratings yet
- Lymphoma B CellDocument47 pagesLymphoma B CellJessica SantillanNo ratings yet
- Lymphoma: Cells/ul 5,000 Cells/ul Is CLL and Should Be Staged As Such 1.5 CMDocument10 pagesLymphoma: Cells/ul 5,000 Cells/ul Is CLL and Should Be Staged As Such 1.5 CMJohn Robert AcostaNo ratings yet
- Hodgkin's DiseaseDocument58 pagesHodgkin's Diseasealibayaty1No ratings yet
- DD HematologyDocument43 pagesDD HematologyDemianaNo ratings yet
- LymphomaDocument34 pagesLymphomaSaiKrishnaReddySeemala0% (1)
- EAHP With Corrections (V2) - Changes by GCC (On 10-4-19)Document2 pagesEAHP With Corrections (V2) - Changes by GCC (On 10-4-19)Christopher JulienNo ratings yet
- Leucemia Linfoide CrónicaDocument17 pagesLeucemia Linfoide CrónicaJose AbadiaNo ratings yet
- ENT CPC - Tonsil ProblemsDocument3 pagesENT CPC - Tonsil ProblemsrieuxNo ratings yet
- 2017 08 15 ConsensusGuidelinesHSCTinMDSandJMML v1-3Document19 pages2017 08 15 ConsensusGuidelinesHSCTinMDSandJMML v1-3cristina_zaharia865440No ratings yet
- ImmunologyDocument38 pagesImmunologygautam harshNo ratings yet
- Can We Use Epigenetics To Prime Chemoresistant Lymphomas?Document10 pagesCan We Use Epigenetics To Prime Chemoresistant Lymphomas?nutnut29No ratings yet
- Lab Values Hema: All Values Varies With Age or Sex, or Ethnic SubgroupDocument9 pagesLab Values Hema: All Values Varies With Age or Sex, or Ethnic SubgroupXerxyllXyreaneLinaoNo ratings yet
- April RecallsDocument4 pagesApril Recallsfritzie dara f adjilaniNo ratings yet
- Malignant Lymphoma: Nur MuallimaDocument34 pagesMalignant Lymphoma: Nur MuallimaSRi RamadhaniNo ratings yet
- ENDODocument3 pagesENDOOmar Picado RoqueNo ratings yet
- Riska Tugas DR - JusfeniDocument19 pagesRiska Tugas DR - Jusfeniriska oktarinda utamiNo ratings yet
- Burkitts Lymphoma 2015 PDFDocument9 pagesBurkitts Lymphoma 2015 PDFAffra CahyoNo ratings yet
- 2022 HRS - Aggressive B-Cell Lymphomas FINALDocument80 pages2022 HRS - Aggressive B-Cell Lymphomas FINALИван НегарэNo ratings yet
- Abbreviation Key: Abbrev Full Spell-OutDocument9 pagesAbbreviation Key: Abbrev Full Spell-Outkairton6648No ratings yet
- Diagnostic Tests PDFDocument2 pagesDiagnostic Tests PDFBenedict AlvarezNo ratings yet
- S.N IM2 SOAP P3 Week 3Document28 pagesS.N IM2 SOAP P3 Week 3Rayane MahmoudNo ratings yet
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseFrom EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseNo ratings yet
- KP 2.2.5.1 - LimfadenopatiDocument38 pagesKP 2.2.5.1 - LimfadenopatiArie160No ratings yet
- Cancers of The Blood: Leukemia and LymphomaDocument46 pagesCancers of The Blood: Leukemia and LymphomaMaica LectanaNo ratings yet
- Imunohistochimie LNHDocument4 pagesImunohistochimie LNHHaralambie SarbuNo ratings yet
- Hematology Oncology - LymphomaDocument1 pageHematology Oncology - LymphomaEugen MNo ratings yet
- Malignant LymphomaDocument29 pagesMalignant LymphomaSurya BudikusumaNo ratings yet
- Malignant Disorders of Leukocytes: Supachai A. Basit, RMT, PHDDocument109 pagesMalignant Disorders of Leukocytes: Supachai A. Basit, RMT, PHDChatie PipitNo ratings yet
- Hodgkin's DiseaseDocument4 pagesHodgkin's DiseaseLillabinNo ratings yet
- OcuandAdnexalLymphom PDFDocument126 pagesOcuandAdnexalLymphom PDFJovan PopovićNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Leukemia What Is Leukemia?Document2 pagesLeukemia What Is Leukemia?Ctn ZQNo ratings yet
- Leukemia Cutis in Childhood Acute Myeloid.6Document3 pagesLeukemia Cutis in Childhood Acute Myeloid.6fikriafisNo ratings yet
- Highlights What Is Minimal Residual Disease (MRD) ?Document6 pagesHighlights What Is Minimal Residual Disease (MRD) ?ANo ratings yet
- Laporan IKM KSM PK FEBRUARI 2022Document27 pagesLaporan IKM KSM PK FEBRUARI 2022Nur iffahNo ratings yet
- Pathology Revision E6.5Document129 pagesPathology Revision E6.5massprithiv58No ratings yet
- 18 Lymphoma - Libre PathologyDocument13 pages18 Lymphoma - Libre PathologyfadoNo ratings yet
- Hematology Oncology - LeukemiaDocument2 pagesHematology Oncology - LeukemiaEugen MNo ratings yet
- DapusDocument2 pagesDapusrahmadNo ratings yet
- Pediatric LeukemiasDocument42 pagesPediatric LeukemiasslyfoxkittyNo ratings yet
- Acute LeukemiaDocument4 pagesAcute LeukemiaazayrhusseinNo ratings yet
- Phatophysiology of Acute Lymphoblastic LeukemiaDocument1 pagePhatophysiology of Acute Lymphoblastic LeukemiaHardiyanti RahayuNo ratings yet
- Laporan Kasus LeukemiaDocument2 pagesLaporan Kasus LeukemiaYtyNo ratings yet
- Understanding Leukemia From A Lab PerspectiveDocument48 pagesUnderstanding Leukemia From A Lab PerspectiveGlorya NathasiaNo ratings yet
- 702-Book Chapter-6692-2-10-20221018Document22 pages702-Book Chapter-6692-2-10-20221018AbinayaBNo ratings yet
- Hodgkins and Non Hodgkins LymphomaDocument5 pagesHodgkins and Non Hodgkins LymphomakakuNo ratings yet
- Non Hodgkin's LymphomaDocument31 pagesNon Hodgkin's LymphomaJeo Thomas100% (1)
- DapusDocument1 pageDapusJihadNo ratings yet
- Limfoproliferari Cronice MaligneDocument18 pagesLimfoproliferari Cronice MaligneAlice MuscaNo ratings yet
- Acute Leukemia: Thirunavukkarasu MurugappanDocument22 pagesAcute Leukemia: Thirunavukkarasu MurugappanFelix Allen100% (1)
- قلق الموت من السرطانDocument212 pagesقلق الموت من السرطانBouchareb AhmedNo ratings yet