Professional Documents
Culture Documents
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Uploaded by
minacristalCopyright:
Available Formats
You might also like
- 04 FS Package InsertDocument6 pages04 FS Package InsertImas NurhayatiNo ratings yet
- Coagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704Document7 pagesCoagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704minacristalNo ratings yet
- Hyphen Fviii Fix Fxi Fxii DP v3 2021 01Document2 pagesHyphen Fviii Fix Fxi Fxii DP v3 2021 01minacristalNo ratings yet
- FXII RocheDocument3 pagesFXII RocheminacristalNo ratings yet
- FXI RocheDocument3 pagesFXI RocheminacristalNo ratings yet
- Dade Thrombin ReagentDocument8 pagesDade Thrombin ReagentchaiNo ratings yet
- Use of Protein TetsDocument5 pagesUse of Protein TetsNutsa ToduaNo ratings yet
- Dade Actin FSL Activated PTT Reagent - Rev 10 DXDCM 09017fe9804eb3b9-1605649828217Document7 pagesDade Actin FSL Activated PTT Reagent - Rev 10 DXDCM 09017fe9804eb3b9-1605649828217Dany BatistaNo ratings yet
- Hema Ii Laboratory Week 6Document65 pagesHema Ii Laboratory Week 6Al-hadad AndromacheNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- At 13704Document2 pagesAt 13704dr_joe23No ratings yet
- ALTL 0020764957322COIN V7 enDocument4 pagesALTL 0020764957322COIN V7 enMMCSTORENo ratings yet
- Immulite/Immulite 1000 Acth 2005-04-26 Pilkac - 11: Changes in This EditionDocument11 pagesImmulite/Immulite 1000 Acth 2005-04-26 Pilkac - 11: Changes in This EditionDeborah GongoraNo ratings yet
- LDHI2 enDocument3 pagesLDHI2 enArnaz AdisaputraNo ratings yet
- Kit InsertDocument2 pagesKit InsertfaujraneNo ratings yet
- Biolabo PTDocument2 pagesBiolabo PTSendy Fadilla OktoraNo ratings yet
- Dade InnovinDocument8 pagesDade InnovinSheyk SagoNo ratings yet
- Ftna-Assl4 1Document2 pagesFtna-Assl4 1Matthew KingNo ratings yet
- PLAC Test For Lp-PLA2 Activity Package InsertDocument12 pagesPLAC Test For Lp-PLA2 Activity Package InsertSmithesh TpNo ratings yet
- At 13660Document2 pagesAt 13660dr_joe23No ratings yet
- Insert PREA 0108252645190c503 V4 enDocument3 pagesInsert PREA 0108252645190c503 V4 enVegha NedyaNo ratings yet
- ACL TOP Family SOP Manual 2016-10-19 enDocument238 pagesACL TOP Family SOP Manual 2016-10-19 enAndra Radulescu100% (1)
- Tugas Pak AzharDocument9 pagesTugas Pak Azhardedi gunawanNo ratings yet
- 02 571-572-575 FIBRIPHEN v4 2021-01Document2 pages02 571-572-575 FIBRIPHEN v4 2021-01dr_joe23No ratings yet
- Cholinesterase - ADVIA Chemistry - Rev D DXDCM 09008b838062478c-1369138193191Document11 pagesCholinesterase - ADVIA Chemistry - Rev D DXDCM 09008b838062478c-1369138193191Lee-Ya AchmadNo ratings yet
- Clonatest Alt/Gpt OptDocument4 pagesClonatest Alt/Gpt OptSuprovet LabotatorioNo ratings yet
- Limulus Amebocyte Lysate (LAL) Pyrogent™ and Pyrogent™ Plus: Pharma&BiotechDocument13 pagesLimulus Amebocyte Lysate (LAL) Pyrogent™ and Pyrogent™ Plus: Pharma&BiotechABDO ELJANo ratings yet
- ApttDocument2 pagesApttNonameNo ratings yet
- ALTL enDocument3 pagesALTL enyolanda0811No ratings yet
- Sgot Roche c111Document4 pagesSgot Roche c111Harditya FirdhausNo ratings yet
- #C-310-5 Lot.89740 EinsertDocument3 pages#C-310-5 Lot.89740 Einsertjnyng222100% (3)
- Lyphochek Assayed Chemistry Control Levels 1 and 2Document4 pagesLyphochek Assayed Chemistry Control Levels 1 and 2Gaurav MauryaNo ratings yet
- Alat (GPT) Fs : Order Information Warnings and PrecautionsDocument3 pagesAlat (GPT) Fs : Order Information Warnings and Precautionssovi haswindhaNo ratings yet
- 732 CT10052Document2 pages732 CT10052thureinwinnNo ratings yet
- Inserto TP Thromborel S SIEMENSDocument6 pagesInserto TP Thromborel S SIEMENSedson flores100% (2)
- LIPASEDocument4 pagesLIPASEsyufriyadiNo ratings yet
- PI e ALT 1 PDFDocument3 pagesPI e ALT 1 PDFMuhammad DaffaNo ratings yet
- FolateDocument15 pagesFolatecarineNo ratings yet
- IFU - R910 e ALT 2Document4 pagesIFU - R910 e ALT 2Osama Ben DawNo ratings yet
- At 80027Document2 pagesAt 80027Yesha Bio ValenciaNo ratings yet
- Kalsitonin PDFDocument12 pagesKalsitonin PDFFariz KasyidiNo ratings yet
- 107 - Uk51081 Ifu 25oh-Direct ElisaDocument8 pages107 - Uk51081 Ifu 25oh-Direct Elisad208dgNo ratings yet
- Multifibren UDocument6 pagesMultifibren UMari Fere100% (1)
- APTT MispaClogDocument1 pageAPTT MispaClogDharmesh PatelNo ratings yet
- Prolactin - IMMULITE and IMMULITE 1000 - Rev 13 DXDCM 09017fe9802977c5-1538194815088Document32 pagesProlactin - IMMULITE and IMMULITE 1000 - Rev 13 DXDCM 09017fe9802977c5-1538194815088Guneyden GuneydenNo ratings yet
- Lab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535Document20 pagesLab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535tomNo ratings yet
- Alat (GPT) Fs : Order Information Warnings and PrecautionsDocument4 pagesAlat (GPT) Fs : Order Information Warnings and Precautionssovi haswindhaNo ratings yet
- Apolipoprotein BDocument13 pagesApolipoprotein BcarineNo ratings yet
- PI e AST 2Document3 pagesPI e AST 2Cindy Mae A. PogoyNo ratings yet
- ACTHDocument6 pagesACTHşaban günerNo ratings yet
- Blood Grouping ReagentsDocument7 pagesBlood Grouping ReagentsDominic EmerencianaNo ratings yet
- LAL Kinetic-QCLDocument32 pagesLAL Kinetic-QCLSykat ZamanNo ratings yet
- A46221DDocument15 pagesA46221DQuoctytranNo ratings yet
- HemosIL APTT Brochure Rev2 May 07 PDFDocument4 pagesHemosIL APTT Brochure Rev2 May 07 PDFKath ONo ratings yet
- At 82560Document2 pagesAt 82560nidhal amamiNo ratings yet
- Package Insert - PYROGENT™-5000 (English) - Original - 29682Document17 pagesPackage Insert - PYROGENT™-5000 (English) - Original - 29682Putri DozanNo ratings yet
- PreciControl ClinChem Multi 2.05117224001.V4.EnDocument2 pagesPreciControl ClinChem Multi 2.05117224001.V4.EnARIF AHAMMED P29% (7)
- Syndecan1 (CD138) RGP009R Biovendor-3Document20 pagesSyndecan1 (CD138) RGP009R Biovendor-3YogiHadityaNo ratings yet
- Protéines Totales Biuret - ENDocument2 pagesProtéines Totales Biuret - ENYousra NanoNo ratings yet
- FXI RocheDocument3 pagesFXI RocheminacristalNo ratings yet
- FXII RocheDocument3 pagesFXII RocheminacristalNo ratings yet
- HemosIL Factor XI Deficient Plasma 0020011300Document3 pagesHemosIL Factor XI Deficient Plasma 0020011300minacristalNo ratings yet
- Hyphen Fviii Fix Fxi Fxii DP v3 2021 01Document2 pagesHyphen Fviii Fix Fxi Fxii DP v3 2021 01minacristalNo ratings yet
- HemosIL SynthASil - En, FR, ES, De, IT, PT Insert Sheet v2017-06Document3 pagesHemosIL SynthASil - En, FR, ES, De, IT, PT Insert Sheet v2017-06minacristalNo ratings yet
- Coagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704Document7 pagesCoagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704minacristalNo ratings yet
- Complement Fixation TestDocument2 pagesComplement Fixation TestGIST (Gujarat Institute of Science & Technology)100% (1)
- Summer Training Report 2022Document85 pagesSummer Training Report 2022Rakesh InnovationsAnd SolutionsInstituteNo ratings yet
- Reticulocyte CountDocument5 pagesReticulocyte CountAdiel CalsaNo ratings yet
- Blood Cell PathologyDocument12 pagesBlood Cell PathologyRoman CoNo ratings yet
- Paida Lajin Self-Healing EnglishDocument69 pagesPaida Lajin Self-Healing EnglishKarma Arnab100% (2)
- Practice QuestionsDocument130 pagesPractice Questionsshirin kayNo ratings yet
- Problems and Remedies For MarsDocument4 pagesProblems and Remedies For MarsSunil RupaniNo ratings yet
- (Reliable Diagnostic Laboratory Nepal Pvt. LTD.) Samakhushi-26, Kathmandu, Nepal, Phone: 014366073 9801612348Document1 page(Reliable Diagnostic Laboratory Nepal Pvt. LTD.) Samakhushi-26, Kathmandu, Nepal, Phone: 014366073 9801612348Abinash MandalNo ratings yet
- Blood Banking: Clinical ChemistryDocument8 pagesBlood Banking: Clinical ChemistryAirah Angela Oben ArnigoNo ratings yet
- General Surgery Two-1Document3 pagesGeneral Surgery Two-1Abhishek NaikNo ratings yet
- Chapter 8 Blood DonationDocument55 pagesChapter 8 Blood DonationCHALIE MEQUNo ratings yet
- Pathophysiology of Acute Kidney InjuryDocument4 pagesPathophysiology of Acute Kidney InjuryJane Arian Berzabal0% (1)
- First Grading VIDocument82 pagesFirst Grading VIIvy Villanueva Divino100% (1)
- Development of VeinsDocument37 pagesDevelopment of Veinsokolodivine334No ratings yet
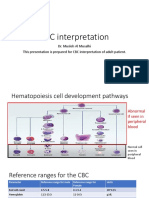
- CBC Interpetation Dr. MuslehDocument37 pagesCBC Interpetation Dr. MuslehMusleh Al MusalhiNo ratings yet
- Fang and Fury - Guidebook To Vampires PDFDocument83 pagesFang and Fury - Guidebook To Vampires PDFalexis gerrick100% (2)
- The Gel Test, A New Way To Detect Red Cell PDFDocument5 pagesThe Gel Test, A New Way To Detect Red Cell PDFTaufan LutfiNo ratings yet
- Megaloblastic AnemiaDocument5 pagesMegaloblastic AnemiaNTA UGC-NETNo ratings yet
- 2018 Year 11 Human Biology ATAR Course OutlineDocument21 pages2018 Year 11 Human Biology ATAR Course OutlineNessrynNo ratings yet
- Reaksi Transfusi, TRALI Vs TACODocument12 pagesReaksi Transfusi, TRALI Vs TACOifadhrohayatNo ratings yet
- Notes in Forensic ChemistryDocument10 pagesNotes in Forensic ChemistryRivera Aezyl JoyNo ratings yet
- Case Study - Reading and Writing Skill - WorksheetDocument3 pagesCase Study - Reading and Writing Skill - WorksheetDevinNo ratings yet
- Elso Anticoagulation Guideline 8-2014-Table-Contents 1Document17 pagesElso Anticoagulation Guideline 8-2014-Table-Contents 1api-302708069No ratings yet
- Neonatal Polycythemia and HyperviscosityDocument8 pagesNeonatal Polycythemia and HyperviscosityToto HandayonoNo ratings yet
- Caber 2021 Oape TP NTP Template 1Document3 pagesCaber 2021 Oape TP NTP Template 1Ma Corazon Sagun CaberNo ratings yet
- Presentation For Saksham Training - Basic Life SupportDocument51 pagesPresentation For Saksham Training - Basic Life SupportPotluri SunilNo ratings yet
- Aplastic AnemiaDocument3 pagesAplastic AnemiaFrancis JuneNo ratings yet
- Minuman Coklat Eritrosit AnemiaDocument6 pagesMinuman Coklat Eritrosit AnemiaMatthew NathanielNo ratings yet
- Overcoming Cancer With Food and Nutrition Liz LipskiDocument2 pagesOvercoming Cancer With Food and Nutrition Liz LipskivaleriabostanNo ratings yet
- Approach To Hematologic DisordersDocument8 pagesApproach To Hematologic DisorderstyasNo ratings yet
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Uploaded by
minacristalCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Coagulation Factor XI Deficient Plasma - Rev 08 DXDCM 090234ed8210b3e4-1713201418519
Uploaded by
minacristalCopyright:
Available Formats
Coagulation Factor XI Deficient Plasma
FACTOR XI DEFICIENT
Revision bar indicates update to previous version.
Intended Use
FACTOR XI DEFICIENT is an in vitro diagnostic reagent for the quantitative, WHO-standardized
determination of coagulation factor XI (FXI) activity as aid to diagnosis of congenital or acquired FXI
deficiencies in patients with bleeding disorders or at risk for FXI deficiency in human sodium citrated
plasma by means of automated, semi-automated and/or manual coagulometric methods.
Summary and Explanation
Coagulation factor XI (FXI) is involved in the early phase of the contact activation pathway of the
coagulation system. Some patients with FXI deficiency experience mild bleeding. On the other hand
FXI levels have been shown to play a significant, dose dependent role in the development of
thrombosis; FXI deficiency patients were reported to exhibit a lower incidence of thrombotic and
ischemic events1–3.
Detection of an activation of the contact phase of blood coagulation can be achieved by measuring the
activity of FXI and FXII. FXI is involved in the intrinsic coagulation pathway; hence a prolongation of
activated partial thromboplastin time APTT is seen in case of a FXI deficiency. The APTT-based one-
stage clotting assay using FACTOR XI DEFICIENT is applied for determination of FXI activity2.
The determination of FXI in plasma is indicated in the following cases:
• clarifying the cause of a prolonged APTT,
• diagnosing congenital or acquired factor deficiency states,
• distinguishing between dysproteinemias and protein synthesis disorders (in conjunction with
immunochemical methods).
Principles of the Procedure
A plasma deficient in any of the factors comprising the intrinsic pathway will result in a prolonged
partial thromboplastin time (APTT). Coagulation factor deficient plasma can be used to confirm a factor
deficiency, in general, and to identify and quantify coagulation factor deficiency in patient plasma. A
mixture of the respective factor deficient plasma and the patient plasma is tested in the APTT assay,
and the result is interpreted using a reference curve obtained with dilutions of STANDARD PLASMA or a
normal plasma pool mixed with the deficient plasma. A patient plasma deficient in a specific factor will
not be able to compensate for the absence of the factor in the corresponding coagulation factor
deficient plasma and therefore result in a prolonged APTT.
Reagents
Note: FACTOR XI DEFICIENT can be used manually or on automated coagulation analyzers.
Siemens Healthineers provides Reference Guides (Application Sheets) for several coagulation
analyzers. The Reference Guides (Application Sheets) contain analyzer/assay specific handling and
performance information which may differ from that provided in these Instructions for Use. In this
case, the information contained in the Reference Guides (Application Sheets) supersedes the
11541625_en Rev. 08 – Outside USA 2024-04 1/7
Coagulation Factor XI Deficient Plasma
information in these Instructions for Use. Please also consult the instruction manual of the instrument
manufacturer!
Reagent Description Storage Stability
Coagulation Factor XI Deficient Lyophilized reagent containing: 2–8 °C 15–25 °C:
Plasma • human plasmaa, FXI activity May be used up to the reconstituted,
FACTOR XI DEFICIENT ≤1 % expiry date indicated on the 8 hoursb;
• Stabilizer: label if stored unopened. −20 °C:
• D-Mannitol (reconstituted: reconstituted,
20 g/L) 4 weeksb
a
from pooled plasma collected from selected healthy blood donor
b
closed original vial
FACTOR XI DEFICIENT is manufactured by immunoadsorption from normal plasma and is free from
antigen of the respective factor. Fibrinogen is present in a quantity of ≥ 1 g/L, and the remaining
coagulation factor is present in an activity > 40 % of Norm.
FACTOR XI DEFICIENT can be frozen and thawed once after reconstitution without a loss of coagulation
activity. The plasma must be well sealed and frozen as quickly as possible. Thawing should be
accomplished at 37 °C within 10 minutes. Thawed plasma should be used within 2 hours when held at
15 to 25 °C.
On-board stability
Information regarding on-board stability is specified in the Reference Guides (Application Sheets) for
the different coagulation analyzers.
Warnings and Precautions
For in-vitro diagnostic use only.
For laboratory professional use.
According to EU regulation 2017/746, any serious incident that has occurred in relation to the device
shall be reported to the manufacturer and the competent authority of the EU Member State through
your local distribution representative in which the user and/or patient is established.
Safety data sheets (MSDS/SDS) available on siemens-healthineers.com/sds.
CAUTION! POTENTIAL BIOHAZARD
Each donor or donor unit was tested and found to be negative for human immunodeficiency virus
(HIV) 1 and 2, hepatitis B virus (HBV) and hepatitis C virus (HCV) using either tests that are CE marked
or FDA approved for this purpose. Because no known test can offer complete assurance of the absence
of infectious agents, all human derived products should be handled with appropriate caution.
Caution
This device contains material of animal origin and should be handled as a potential carrier and
transmitter of disease.
Dispose of hazardous or biologically contaminated materials according to the practices of your
institution. Discard all materials in a safe and acceptable manner and in compliance with all
government requirements.
Preparing Reagents
FACTOR XI DEFICIENT : Dissolve the contents of a vial with 1 mL of distilled or deionized water. Before
use, let stand at least 15 minutes at 15 to 25 °C, then swivel carefully to mix (without foam formation).
Mix carefully once more before using.
APTT reagent: Use according to the respective Instructions for Use.
CaCl2 SOLUTION 0.025 mol/L: warm to 37 °C (not required for automated coagulation systems with
heated reagent probes).
2/7 2024-04 11541625_en Rev. 08 – Outside USA
Coagulation Factor XI Deficient Plasma
Specimen Collection and Handling
Collecting the Specimen
To obtain the plasma, carefully mix one part of 0.11 or 0.13 mol/L (3.2 % or 3.8 %) sodium citrate
solution with nine parts of freshly collected patient blood, avoiding the formation of foam. Centrifuge
the blood specimen at 1 500 × g at least 15 minutes at 15 to 25 °C4.
Storing the Specimen
Stability of the samples:
15 to 25 °C 3 hours
−20 °C 4 weeks
Plasma stored at −20 °C is to be thawed in a water bath within 10 minutes at 37 °C, mixed gently and
then tested immediately. If testing cannot be performed immediately after thawing, the specimen may
be held for a maximum of 2 hours at 4 °C until tested (H21–A5)4.
Procedure
Materials Provided
REF Contents
OSDF13 Coagulation Factor XI Deficient Plasma 3× 1 mL
FACTOR XI DEFICIENT
Materials Required but not Provided
Item Description
REF OQGS29, OQGS35 Pathromtin® SL, or
REF B4218-1, B4218-2 ACTIN , Dade® Actin® Activated Cephaloplastin Reagent, or
REF B4218-20, B4218-100 ACTIN FS , Dade® Actin® FS Activated PTT Reagent, or
REF B4219-1, B4219-2 ACTIN FSL , Dade® Actin® FSL Activated PTT Reagent
REF ORHO37 CaCl2 SOLUTION , Calcium Chloride Solution
REF OQAA33 IMIDAZOLE BUFFER , Imidazole Buffer Solution, or
REF B4234-25 OV BUFFER , Dade® Owren’s Veronal Buffer, or
REF B4265-35, B4265-37 CA SYSTEM BUFFER , Dade® CA System Buffer, or
– Physiological Saline Solution
REF ORKL17 STANDARD PLASMA , Standard Human Plasma
REF ORKE41 CONTROL N , Control Plasma N
REF OUPZ17 CONTROL P , Control Plasma P
Coagulation analyzersc, such as: • BCS® XP System
• BFT II Analyzer
• AUTOMATED BLOOD COAGULATION ANALYZER CA-1500 (CA-1500 System)
• AUTOMATED BLOOD COAGULATION ANALYZER CS-2500 (CS‑2500 System)
• AUTOMATED BLOOD COAGULATION ANALYZER CS-5100 (CS‑5100 System)
• Automated Blood Coagulation Analyzer CN‑3000/CN‑6000 (CN‑3000/
CN‑6000 System)
c
Availability of analyzers may vary by country.
Please note that the applications on other analyzers can be validated by the instrument manufacturer
in accordance with the requirements of the REGULATION (EU) 2017/746 under their responsibility as
long as the intended purpose and performance are not modified.
11541625_en Rev. 08 – Outside USA 2024-04 3/7
Coagulation Factor XI Deficient Plasma
Manual Testing
Pre-warm CaCl2 SOLUTION at 37 °C
Immediately before the measurement:
Dilute plasma sample 1:5 in IMIDAZOLE BUFFER (equilibrated at
15–25 °C).
Pipette into a test tube pre-warmed to 37 °C:
FACTOR XI DEFICIENT 100 µL
Plasma (diluted) 100 µL
APTT reagent 100 µL
Mix well. Incubate at 37 °C for 2 minutes.
CaCl2 SOLUTION (pre-warmed) 100 µL
On addition of CaCl2 SOLUTION start stop-
watch or timer on the coagulation analyzer
and determine the coagulation time.
Establishment of the Reference Curve
Use either STANDARD PLASMAor fresh citrated pooled plasma of at least 10 healthy donors. Using
IMIDAZOLE BUFFER , prepare dilutions as shown in the following scheme and determine the coagulation
times as described under "Manual Testing", page 4. A new reference curve must be generated if there
is a change in the instrument or in the lot of reagent used, or if there is any change in the experimental
conditions.
Dilution
Imidazole Buffer Solution µL
Standard Human Plasma µL
% of the norm
Additional dilutions can be prepared if necessary. Plot the measured coagulation times (ordinate) on
log graph paper against the corresponding percentage factor activities (abscissa). The coagulation
times are dependent on the measurement principle and thus also on the coagulation analyzer used.
Therefore, each laboratory must establish its own reference curve.
Internal Quality Control
Normal range: CONTROL N
Pathological range: CONTROL P
Two levels of quality control material (normal and pathologic range) have to be measured at start of
the test run, with each calibration, upon reagent vial changes and at least every eight hours on each
day of testing.The controls should be processed like the samples. Each laboratory should establish its
own quality control range, either by means of the target values and ranges provided by the
manufacturer of the controls or by means of its own confidence ranges established in the laboratory. If
the control values lie outside the range the reagent, calibration curve and coagulation analyzer should
be checked. Patient results must not be released until the cause of the deviation is identified and
corrected.
4/7 2024-04 11541625_en Rev. 08 – Outside USA
Coagulation Factor XI Deficient Plasma
Results
Read the coagulation factor content from the reference curve in % of Norm. If the given nominal value
of the STANDARD PLASMA is not 100 % of Norm, but e.g. only 95 % of Norm, multiply the result read
from the curve by 0.95. In the case of coagulation times which correspond to a coagulation factor
content of more than 100 % of Norm, further determination will be required using higher dilutions of
specimen (e.g. 1:10). The percentage of norm value read from the reference curve for such a higher
dilution must be multiplied by a correction factor corresponding to the dilution; e.g. for a dilution of
1:10 by a correction factor of 2.
Limitations
Therapeutic doses of hirudin or other direct thrombin inhibitors lead to an erroneously lower factor
activity5,6.
Specific inhibitors against plasmatic coagulation factors may also modify the real factor activity7. Partial
activation of the coagulation factors due to incorrect sample handling can lead to falsely elevated
single factor results. In single factor determination, lupus anticoagulant can affect the apparent factor
activity. Non-parallelism upon dilution may occur when a lupus anticoagulant is present in the test
sample8.
Siemens Healthineers has validated use of these reagents on various analyzers to optimize product
performance and meet product specifications. Please note that the applications on other analyzers can
be validated by the instrument manufacturer in accordance with the requirements of the REGULATION
(EU) 2017/746 under their responsibility as long as the intended purpose and performance are not
modified. User defined modifications are not supported by Siemens Healthineers as they may affect
performance of the system and assay results. It is the responsibility of the user to validate modifications
to these instructions or use of the reagents on analyzers other than those included in
Siemens Healthineers Application Sheets or these Instructions for Use.
Results of this test should always be interpreted in conjunction with the patient's medical history,
clinical presentation and other findings.
Expected Values9
Factor XI 70 to 120 % of Norm
Reference intervals vary from laboratory to laboratory depending on the population served and the
technique, method, equipment and reagent lot used. Therefore, each laboratory must establish its own
reference intervals or verify them whenever one or more of the aforementioned variables are changed.
Performance Characteristics
Measuring Range
The measuring range depends on the individual application of the assay due to instrument related
conditions. Application specific performance data is listed in the respective Reference Guide of the
instrument.
Precision
The results of all precision studies with applications of the assay Factor XI showed a precision
(repeatability and within-device/lab precision) in the range of 2 to 14 % across the measuring range.
Other system specific results are given in the respective Reference Guides (Application Sheets).
The reproducibility was assessed by Siemens Healthineers for Factor XI Deficient Plasma based on
publicly available proficiency testing information in 2019. The overall reproducibility median CV% was
found to be < 10 % including APTT reagent used, lot, instrument, laboratory and operator variability
factors.
11541625_en Rev. 08 – Outside USA 2024-04 5/7
Coagulation Factor XI Deficient Plasma
Method Comparison
In a study, the determination of FXI on the Atellica® COAG 360 System was compared to the CS-2000i
System.
The correlation resulted in the following:
n Slope Intercept Correlation Coefficient
[% of Norm]
Factor XI 104 . 1.02 + 4.08 0.990
Technical Assistance
For customer support, contact your local technical support provider or distributor.
siemens-healthineers.com
Current Version of Application Sheets
FACTOR XI DEFICIENT can be used in combination with various automated coagulation analyzers.
Siemens Healthineers provides Reference Guides/Application Sheets for the coagulation analyzers
listed in section "Materials Required but not Provided", page 3 under the dedicated link below:
siemens-healthineers.com/rg
As Siemens Healthineers continuously monitors the product performance and safety, the users are
required to ensure that they work with the correct revision of the instructions for the product lots in
use. Please periodically review the availability of new electronic labeling revisions to ensure safe use of
the product.
The IFU version number is visible on each product box label. Siemens Healthineers ensures that all
products lots bearing the same IFU version number are compatible with the electronic labeling
provided via siemens-healthineers.com/eIFU.
References
1. Peyvandi F, Menegatti M. Treatment of rare factor deficiency in 2016. Hematology.
2016;2016:663-9.
2. James P, Salomon O, Mikovic D, et al. Rare bleeding disorders - bleeding assessment tools,
laboratory aspects and phenotype and therapy of FXI deficiency. Haemophilia 2014; 20 Suppl
4:71-5.
3. Puy C, Rigg RA, McCarty OJ. The hemostatic role of factor XI. Thromb Res. 2016; 141 Suppl 2:S8-
S11.
4. CLSI. Collection, Transport, and Processing of Blood Specimens for Testing Plasma-Based
Coagulation Assays and Molecular Hemostasis Assays. Approved Guideline – Fifth Edition. CLSI
document H21-A5 [ISBN 1-56238-657-3]. CLSI, 940 West Valley Road, Suite 1400, Wayne, PA
19087-1898 USA, 2008.
5. Boogen C, Niederau C, Reinauer H. Assessment of the influence of r-hirudin on coagulometric
factor assays [Abstract]. Ann Hematol. 1999;78 Suppl:73.
6. Walenga JM, Drenth A, Mayuga M, et al. Effects of Argatroban alone and combined with oral
anticoagulation on coagulation parameters [Abstract]. Blood 2002;100:4006.
7. Feinstein, DI. Immune coagulation disorders. In: Colman, RW, et al., editors. Hemostasis and
Thrombosis. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 1003-20
8. Brandt JT, Triplett DA, Rock WA, et al. Effect of lupus anticoagulants on the activated partial
thromboplastin time. Arch Pathol Lab Med. 1991;115:109-14
9. Fickenscher K. Analysis of individual coagulation factors. In: Thomas L, editor. Clinical Laboratory
Diagnostics. Frankfurt: TH-Books Verlagsgesellschaft; 1998: 607-9.
6/7 2024-04 11541625_en Rev. 08 – Outside USA
Coagulation Factor XI Deficient Plasma
Definition of Symbols
The following symbols may appear on the product labeling:
Do not reuse Use By
LOT Batch Code REF Catalogue Number
Caution Manufacturer
Authorized representative in the Authorized representative in
EC REP CH REP
European Community Switzerland
Contains sufficient for <n> tests Biological Risks
IVD In Vitro Diagnostic Medical Device Temperature Limitation
Consult instruction for Use Non-sterile
CE marking of conformity with
CE marking of conformity notified body ID number.
Notified body ID number can vary.
CONTENTS Contents Reconstitution volume
LEVEL Level Keep away from sunlight and heat
WARNING Warning DANGER Danger
RxOnly Prescription device (US only) UDI Device Identification (UDI) barcode
REACH xx/xx/xx REACH Authorization Number
Legal Information
Actin, Atellica, BCS, Dade and Pathromtin are trademarks of Siemens Healthineers.
All other trademarks are the property of their respective owners.
© Siemens Healthineers, 2008–2024. All rights reserved.
Siemens Healthineers Headquarters Siemens Healthcare Diagnostics Products GmbH
Siemens Healthcare GmbH Emil-von-Behring-Str. 76
Henkestraße 127 35041 Marburg
91052 Erlangen Germany
Germany siemens-healthineers.com
Phone: +49 9131 84-0
siemens-healthineers.com
11541625_en Rev. 08 – Outside USA 2024-04 7/7
You might also like
- 04 FS Package InsertDocument6 pages04 FS Package InsertImas NurhayatiNo ratings yet
- Coagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704Document7 pagesCoagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704minacristalNo ratings yet
- Hyphen Fviii Fix Fxi Fxii DP v3 2021 01Document2 pagesHyphen Fviii Fix Fxi Fxii DP v3 2021 01minacristalNo ratings yet
- FXII RocheDocument3 pagesFXII RocheminacristalNo ratings yet
- FXI RocheDocument3 pagesFXI RocheminacristalNo ratings yet
- Dade Thrombin ReagentDocument8 pagesDade Thrombin ReagentchaiNo ratings yet
- Use of Protein TetsDocument5 pagesUse of Protein TetsNutsa ToduaNo ratings yet
- Dade Actin FSL Activated PTT Reagent - Rev 10 DXDCM 09017fe9804eb3b9-1605649828217Document7 pagesDade Actin FSL Activated PTT Reagent - Rev 10 DXDCM 09017fe9804eb3b9-1605649828217Dany BatistaNo ratings yet
- Hema Ii Laboratory Week 6Document65 pagesHema Ii Laboratory Week 6Al-hadad AndromacheNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- At 13704Document2 pagesAt 13704dr_joe23No ratings yet
- ALTL 0020764957322COIN V7 enDocument4 pagesALTL 0020764957322COIN V7 enMMCSTORENo ratings yet
- Immulite/Immulite 1000 Acth 2005-04-26 Pilkac - 11: Changes in This EditionDocument11 pagesImmulite/Immulite 1000 Acth 2005-04-26 Pilkac - 11: Changes in This EditionDeborah GongoraNo ratings yet
- LDHI2 enDocument3 pagesLDHI2 enArnaz AdisaputraNo ratings yet
- Kit InsertDocument2 pagesKit InsertfaujraneNo ratings yet
- Biolabo PTDocument2 pagesBiolabo PTSendy Fadilla OktoraNo ratings yet
- Dade InnovinDocument8 pagesDade InnovinSheyk SagoNo ratings yet
- Ftna-Assl4 1Document2 pagesFtna-Assl4 1Matthew KingNo ratings yet
- PLAC Test For Lp-PLA2 Activity Package InsertDocument12 pagesPLAC Test For Lp-PLA2 Activity Package InsertSmithesh TpNo ratings yet
- At 13660Document2 pagesAt 13660dr_joe23No ratings yet
- Insert PREA 0108252645190c503 V4 enDocument3 pagesInsert PREA 0108252645190c503 V4 enVegha NedyaNo ratings yet
- ACL TOP Family SOP Manual 2016-10-19 enDocument238 pagesACL TOP Family SOP Manual 2016-10-19 enAndra Radulescu100% (1)
- Tugas Pak AzharDocument9 pagesTugas Pak Azhardedi gunawanNo ratings yet
- 02 571-572-575 FIBRIPHEN v4 2021-01Document2 pages02 571-572-575 FIBRIPHEN v4 2021-01dr_joe23No ratings yet
- Cholinesterase - ADVIA Chemistry - Rev D DXDCM 09008b838062478c-1369138193191Document11 pagesCholinesterase - ADVIA Chemistry - Rev D DXDCM 09008b838062478c-1369138193191Lee-Ya AchmadNo ratings yet
- Clonatest Alt/Gpt OptDocument4 pagesClonatest Alt/Gpt OptSuprovet LabotatorioNo ratings yet
- Limulus Amebocyte Lysate (LAL) Pyrogent™ and Pyrogent™ Plus: Pharma&BiotechDocument13 pagesLimulus Amebocyte Lysate (LAL) Pyrogent™ and Pyrogent™ Plus: Pharma&BiotechABDO ELJANo ratings yet
- ApttDocument2 pagesApttNonameNo ratings yet
- ALTL enDocument3 pagesALTL enyolanda0811No ratings yet
- Sgot Roche c111Document4 pagesSgot Roche c111Harditya FirdhausNo ratings yet
- #C-310-5 Lot.89740 EinsertDocument3 pages#C-310-5 Lot.89740 Einsertjnyng222100% (3)
- Lyphochek Assayed Chemistry Control Levels 1 and 2Document4 pagesLyphochek Assayed Chemistry Control Levels 1 and 2Gaurav MauryaNo ratings yet
- Alat (GPT) Fs : Order Information Warnings and PrecautionsDocument3 pagesAlat (GPT) Fs : Order Information Warnings and Precautionssovi haswindhaNo ratings yet
- 732 CT10052Document2 pages732 CT10052thureinwinnNo ratings yet
- Inserto TP Thromborel S SIEMENSDocument6 pagesInserto TP Thromborel S SIEMENSedson flores100% (2)
- LIPASEDocument4 pagesLIPASEsyufriyadiNo ratings yet
- PI e ALT 1 PDFDocument3 pagesPI e ALT 1 PDFMuhammad DaffaNo ratings yet
- FolateDocument15 pagesFolatecarineNo ratings yet
- IFU - R910 e ALT 2Document4 pagesIFU - R910 e ALT 2Osama Ben DawNo ratings yet
- At 80027Document2 pagesAt 80027Yesha Bio ValenciaNo ratings yet
- Kalsitonin PDFDocument12 pagesKalsitonin PDFFariz KasyidiNo ratings yet
- 107 - Uk51081 Ifu 25oh-Direct ElisaDocument8 pages107 - Uk51081 Ifu 25oh-Direct Elisad208dgNo ratings yet
- Multifibren UDocument6 pagesMultifibren UMari Fere100% (1)
- APTT MispaClogDocument1 pageAPTT MispaClogDharmesh PatelNo ratings yet
- Prolactin - IMMULITE and IMMULITE 1000 - Rev 13 DXDCM 09017fe9802977c5-1538194815088Document32 pagesProlactin - IMMULITE and IMMULITE 1000 - Rev 13 DXDCM 09017fe9802977c5-1538194815088Guneyden GuneydenNo ratings yet
- Lab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535Document20 pagesLab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535tomNo ratings yet
- Alat (GPT) Fs : Order Information Warnings and PrecautionsDocument4 pagesAlat (GPT) Fs : Order Information Warnings and Precautionssovi haswindhaNo ratings yet
- Apolipoprotein BDocument13 pagesApolipoprotein BcarineNo ratings yet
- PI e AST 2Document3 pagesPI e AST 2Cindy Mae A. PogoyNo ratings yet
- ACTHDocument6 pagesACTHşaban günerNo ratings yet
- Blood Grouping ReagentsDocument7 pagesBlood Grouping ReagentsDominic EmerencianaNo ratings yet
- LAL Kinetic-QCLDocument32 pagesLAL Kinetic-QCLSykat ZamanNo ratings yet
- A46221DDocument15 pagesA46221DQuoctytranNo ratings yet
- HemosIL APTT Brochure Rev2 May 07 PDFDocument4 pagesHemosIL APTT Brochure Rev2 May 07 PDFKath ONo ratings yet
- At 82560Document2 pagesAt 82560nidhal amamiNo ratings yet
- Package Insert - PYROGENT™-5000 (English) - Original - 29682Document17 pagesPackage Insert - PYROGENT™-5000 (English) - Original - 29682Putri DozanNo ratings yet
- PreciControl ClinChem Multi 2.05117224001.V4.EnDocument2 pagesPreciControl ClinChem Multi 2.05117224001.V4.EnARIF AHAMMED P29% (7)
- Syndecan1 (CD138) RGP009R Biovendor-3Document20 pagesSyndecan1 (CD138) RGP009R Biovendor-3YogiHadityaNo ratings yet
- Protéines Totales Biuret - ENDocument2 pagesProtéines Totales Biuret - ENYousra NanoNo ratings yet
- FXI RocheDocument3 pagesFXI RocheminacristalNo ratings yet
- FXII RocheDocument3 pagesFXII RocheminacristalNo ratings yet
- HemosIL Factor XI Deficient Plasma 0020011300Document3 pagesHemosIL Factor XI Deficient Plasma 0020011300minacristalNo ratings yet
- Hyphen Fviii Fix Fxi Fxii DP v3 2021 01Document2 pagesHyphen Fviii Fix Fxi Fxii DP v3 2021 01minacristalNo ratings yet
- HemosIL SynthASil - En, FR, ES, De, IT, PT Insert Sheet v2017-06Document3 pagesHemosIL SynthASil - En, FR, ES, De, IT, PT Insert Sheet v2017-06minacristalNo ratings yet
- Coagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704Document7 pagesCoagulation Factor XII Deficient Plasma - Rev 08 DXDCM 090234ed81f683d0-1713371554704minacristalNo ratings yet
- Complement Fixation TestDocument2 pagesComplement Fixation TestGIST (Gujarat Institute of Science & Technology)100% (1)
- Summer Training Report 2022Document85 pagesSummer Training Report 2022Rakesh InnovationsAnd SolutionsInstituteNo ratings yet
- Reticulocyte CountDocument5 pagesReticulocyte CountAdiel CalsaNo ratings yet
- Blood Cell PathologyDocument12 pagesBlood Cell PathologyRoman CoNo ratings yet
- Paida Lajin Self-Healing EnglishDocument69 pagesPaida Lajin Self-Healing EnglishKarma Arnab100% (2)
- Practice QuestionsDocument130 pagesPractice Questionsshirin kayNo ratings yet
- Problems and Remedies For MarsDocument4 pagesProblems and Remedies For MarsSunil RupaniNo ratings yet
- (Reliable Diagnostic Laboratory Nepal Pvt. LTD.) Samakhushi-26, Kathmandu, Nepal, Phone: 014366073 9801612348Document1 page(Reliable Diagnostic Laboratory Nepal Pvt. LTD.) Samakhushi-26, Kathmandu, Nepal, Phone: 014366073 9801612348Abinash MandalNo ratings yet
- Blood Banking: Clinical ChemistryDocument8 pagesBlood Banking: Clinical ChemistryAirah Angela Oben ArnigoNo ratings yet
- General Surgery Two-1Document3 pagesGeneral Surgery Two-1Abhishek NaikNo ratings yet
- Chapter 8 Blood DonationDocument55 pagesChapter 8 Blood DonationCHALIE MEQUNo ratings yet
- Pathophysiology of Acute Kidney InjuryDocument4 pagesPathophysiology of Acute Kidney InjuryJane Arian Berzabal0% (1)
- First Grading VIDocument82 pagesFirst Grading VIIvy Villanueva Divino100% (1)
- Development of VeinsDocument37 pagesDevelopment of Veinsokolodivine334No ratings yet
- CBC Interpetation Dr. MuslehDocument37 pagesCBC Interpetation Dr. MuslehMusleh Al MusalhiNo ratings yet
- Fang and Fury - Guidebook To Vampires PDFDocument83 pagesFang and Fury - Guidebook To Vampires PDFalexis gerrick100% (2)
- The Gel Test, A New Way To Detect Red Cell PDFDocument5 pagesThe Gel Test, A New Way To Detect Red Cell PDFTaufan LutfiNo ratings yet
- Megaloblastic AnemiaDocument5 pagesMegaloblastic AnemiaNTA UGC-NETNo ratings yet
- 2018 Year 11 Human Biology ATAR Course OutlineDocument21 pages2018 Year 11 Human Biology ATAR Course OutlineNessrynNo ratings yet
- Reaksi Transfusi, TRALI Vs TACODocument12 pagesReaksi Transfusi, TRALI Vs TACOifadhrohayatNo ratings yet
- Notes in Forensic ChemistryDocument10 pagesNotes in Forensic ChemistryRivera Aezyl JoyNo ratings yet
- Case Study - Reading and Writing Skill - WorksheetDocument3 pagesCase Study - Reading and Writing Skill - WorksheetDevinNo ratings yet
- Elso Anticoagulation Guideline 8-2014-Table-Contents 1Document17 pagesElso Anticoagulation Guideline 8-2014-Table-Contents 1api-302708069No ratings yet
- Neonatal Polycythemia and HyperviscosityDocument8 pagesNeonatal Polycythemia and HyperviscosityToto HandayonoNo ratings yet
- Caber 2021 Oape TP NTP Template 1Document3 pagesCaber 2021 Oape TP NTP Template 1Ma Corazon Sagun CaberNo ratings yet
- Presentation For Saksham Training - Basic Life SupportDocument51 pagesPresentation For Saksham Training - Basic Life SupportPotluri SunilNo ratings yet
- Aplastic AnemiaDocument3 pagesAplastic AnemiaFrancis JuneNo ratings yet
- Minuman Coklat Eritrosit AnemiaDocument6 pagesMinuman Coklat Eritrosit AnemiaMatthew NathanielNo ratings yet
- Overcoming Cancer With Food and Nutrition Liz LipskiDocument2 pagesOvercoming Cancer With Food and Nutrition Liz LipskivaleriabostanNo ratings yet
- Approach To Hematologic DisordersDocument8 pagesApproach To Hematologic DisorderstyasNo ratings yet