Professional Documents
Culture Documents
Woc Empiema
Woc Empiema
Uploaded by
Rizka Yuliasih KussantyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Woc Empiema
Woc Empiema
Uploaded by
Rizka Yuliasih KussantyCopyright:
Available Formats
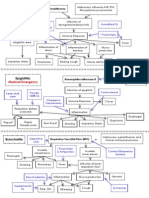
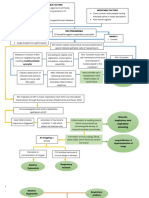
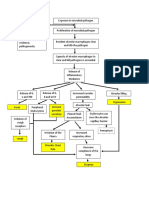
WOC
Invasion of pilogenic bacilli into pleura Infection from the Lungs Infection from outside lungs Perietal-visceral pleural
vibrous attachment
CATEGORY
Acute Inflammation
Thoracocentasis Antibiotic
DS :
administration Fibrothorax
Hyperther PMN Increased Serous Exudate Increased Protein Levels
Pleurodesis Bed rest
mia
Biopsi dan aspirasi pleura Mechanical drag
(D0130)
Drainage/ Cloudy and thick fluid (Pus) in the pleural cavum
Fever occurs Invasive Friction on pleura during breathing
procedure Emphyema
Elevated body temperature Pleuritis pain
DS : Infection Increased intrapleural pressure
Histamine and pyrogenic substances Risk (D0143) DS : Acute Pain
Pleural Effusion (D0077)
Fluid collection in the pleural cavity
Inflammatory
response
Increased intrapleural pressure Limited lung expansion
Increased capillary permeability
Pulmonary collapse Impaired lung
Purulent exudate on bronchi
Decreased lung surface area Disturbed ventilation
Increased secretion production Irritation/ulceration of bronchi
Lactic acid increases Hypoxia PO2 decreased, PCO2 increased Hypercapnic
Productive cough Hemoptysis
Decreased blood pH Kusmaul Dyspnea/ Asidosis respiratoric
breathing breathlessn
DS: Airway clearance ineffectiveness (D0001)
Asidosis metabolic
DS : Activity DS : Ineffective breath pattern
intolerance (D0056) (D0005)
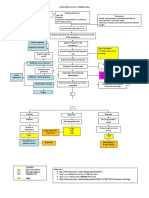
Ineffective airway clearance (D.0001) Airway Hyperthermia (D.0130) Ineffective breathing pattern (D.0005)
Management (I. 01011) Hyperthermia management (I.15506) Respiration monitoring (I.01014)
Observation Observation Observation
1) Monitor breath patterns (frequency, 1) Identify the cause of hyperthermia (e.g. 1) Monitor breath frequency, rhythm,
depth, breath effort) dehydration exposed to hot environment depth, and effort
2) Monitor for additional breath sounds incubator use) 2) Monitor breathing pattern (such as
3) Monitor sputum 2) Monitor body temperature bradypnea, tachypnea, hyperventilation,
Therapeutic 3) Monitor electrolyte levels Kussmaul, Cheyne Stokes, Biot, ataxic0
1) Maintain airway patency with head-tilt 4) Monitor urine output 3) Monitor the ability to cough effectively
and chin-lift (jaw thrust if cervical trauma Therapeutic 4) Monitor for sputum production
is suspected) 1) Provide a cool environment 5) Monitor for airway obstruction
2) Position semi fowler or fowler 2) Loosen or remove clothing 6) Palpate for symmetry of lung expansion
3) Perform chest physiotherapy, if necessary 3) Wet and fan the body surface 7) Auscultate breath sounds
4) Perform lung suction for less than 15 4) Give oral fluids 8) Monitor oxygen saturation
seconds 5) Change linen daily or more frequently if 9) Monitor AGD value
5) Give oxygen, if necessary experiencing hyperhidrosis (excessive 10) Monitor thoracic x-ray results
Education sweating) Therapeutic
1) Teach fluid intake 2000 ml/day, if not 6) Apply external cooling (e.g. hypothermic 1) Set the respiration monitoring time
contraindicated blanket or cold compresses on forehead, interval according to the patient's
2) Teach effective coughing techniques neck, chest, abdomen, axilla) condition.
Collaboration 7) Avoid giving antipyretics or aspirin 2) Document the monitoring results
1) Collaborative administration of 8) Limit oxygen, if necessary Education
bronchodilators, expectorants, Education 1) Explain the purpose and procedure of
mucolytics, if necessary 1) Encourage bed rest monitoring
Collaboration 2) Inform the results of monitoring, if
1) Collaborate intravenous fluids and necessary
electrolytes, if necessary
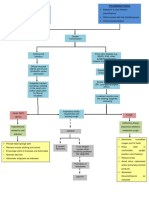
Acute Pain (D.0077) Risk of Infection (D.0143)
Pain Management (I. 08238) Infection Prevention (I.14539)
Observation Observation
1) Monitor the success of the coping therapy that has been 1) Monitor signs and symptoms of local and schizemic infection
given Therapeutic
2) Monitor side effects of analgesic use 1) Limit the number of visitors
Therapeutic 2) Provide skin care to areas of edema
1) Control the environment that exacerbates pain (room 3) Wash hands before and after contact with the patient and the patient's
temperature, lighting, noise) environment
2) Facilitate rest and sleep 4) Maintain aseptic technique in high-risk patients
3) Consider the type and source of pain in choosing pain relief Education
strategies 4) 1) Explain the signs and symptoms of infection
Education 2) Encourage increased nutritional intake
1) Encourage appropriate use of analgesics 3) Encourage increased fluid intake
2) Teach non-pharmacological techniques to reduce pain 2) Collaboration
Collaboration 1) Immunization collaboration, if necessary
1) Collaboration on analgesic administration
You might also like
- Heart Rate and Breathing Lab 1 - AgsaldaDocument4 pagesHeart Rate and Breathing Lab 1 - AgsaldaEj AgsaldaNo ratings yet
- Concept Map - OxygenationDocument3 pagesConcept Map - Oxygenationannie lalangNo ratings yet
- Pneumonia Concept Map - KPoindexterDocument1 pagePneumonia Concept Map - KPoindexterKatie_Poindext_5154100% (2)
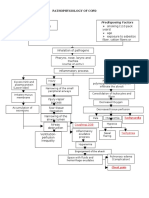
- COPD PathoDocument1 pageCOPD PathoGlenn_Ancheta_2074100% (2)
- Ineffective Airway Clearance Related To BronchospasmDocument2 pagesIneffective Airway Clearance Related To BronchospasmReylan Garcia100% (4)
- A&P Cardiovascular System PowerPoint (Nursing)Document34 pagesA&P Cardiovascular System PowerPoint (Nursing)Linsey Bowen67% (6)
- Pathophysiology of Chronic Obstructive Pulmonary DisorderDocument2 pagesPathophysiology of Chronic Obstructive Pulmonary DisorderBlessyl Mae EstenzoNo ratings yet
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaMaria Cristina100% (1)
- Woc Asma BronkialDocument4 pagesWoc Asma Bronkialyedida susanaNo ratings yet
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJuneNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJesselle LasernaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJeffrey Ramos100% (1)
- Respiratory SystemDocument55 pagesRespiratory SystemEndla SriniNo ratings yet
- Predisposing Factors: Precipitating Factors: Contributing FactorsDocument6 pagesPredisposing Factors: Precipitating Factors: Contributing FactorsKen SimonNo ratings yet
- The Patient and His Illness A. Pathophysiology (Book Based)Document5 pagesThe Patient and His Illness A. Pathophysiology (Book Based)Edmar Francis SabileNo ratings yet
- COPD PathoDocument1 pageCOPD PathoLeah May AnchetaNo ratings yet
- Pneumonia PathoDocument2 pagesPneumonia PathoDerick Nyl PascualNo ratings yet
- Textbook Discussion On Acute Community-Acquired Pneumonia (BSN 3A-Group 6)Document9 pagesTextbook Discussion On Acute Community-Acquired Pneumonia (BSN 3A-Group 6)Jica Marie Bandiola GicaroNo ratings yet
- ARDS (Acute Respiratory Distress Syndrome) : EarlyDocument1 pageARDS (Acute Respiratory Distress Syndrome) : EarlyDora Elena HurtadoNo ratings yet
- Thorax MedDocument3 pagesThorax Medangela mamauagNo ratings yet
- MS LEC Reviewer Oxygenation Problems 1Document4 pagesMS LEC Reviewer Oxygenation Problems 1Shekinah GeriosaNo ratings yet
- Pneumonia Parient BasedDocument2 pagesPneumonia Parient BasedKismet SummonsNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaAzria John DemetriNo ratings yet
- 2023 UsDocument10 pages2023 UswisgeorgekwokNo ratings yet
- Broncho 2Document4 pagesBroncho 2hotteenstar_23No ratings yet
- Pedia RespiDocument2 pagesPedia RespiKerby RosasNo ratings yet
- LEQ PaedsDocument5 pagesLEQ PaedsAtiqah ShahNo ratings yet
- P ATHODocument2 pagesP ATHOValentino Andres Y AntonioNo ratings yet
- NCM 112 Medical SurgicalDocument25 pagesNCM 112 Medical Surgicalstephaniecaronan15No ratings yet
- NCP Difficulty of Breathing R/T SecretionDocument3 pagesNCP Difficulty of Breathing R/T Secretionherscentasiascribd50% (8)
- Culture and Sensitivity: InhalationDocument3 pagesCulture and Sensitivity: Inhalationjamie carpioNo ratings yet
- Laporan Pendahuluan Asuahan Keperawatan Pada Klien Dengan PneumoniaDocument15 pagesLaporan Pendahuluan Asuahan Keperawatan Pada Klien Dengan PneumoniaIka Ulya Cahyani PutriNo ratings yet
- Pathophysiology of PneumoniaDocument1 pagePathophysiology of PneumoniaJeffrey RamosNo ratings yet
- CROUP Concept MapDocument3 pagesCROUP Concept Mapingrid50% (2)
- Non-Modifiable Factors Modifiable Factors: (Causative Agent: Respiratory Syncytia Virus)Document3 pagesNon-Modifiable Factors Modifiable Factors: (Causative Agent: Respiratory Syncytia Virus)Venice Joy CelociaNo ratings yet
- Case Study: Submitted By: Jane Arian Berzabal Nbb2Document14 pagesCase Study: Submitted By: Jane Arian Berzabal Nbb2Jane Arian BerzabalNo ratings yet
- Parapneumonic EffusionDocument1 pageParapneumonic EffusionValerie Anne BebitaNo ratings yet
- COPDDocument15 pagesCOPDMary Grace AgataNo ratings yet
- Patho of COPD and CorP NewDocument5 pagesPatho of COPD and CorP NewInchan Montesines100% (1)
- Wk4 Restrictive Lung DisordersDocument38 pagesWk4 Restrictive Lung DisordersPotato PceeNo ratings yet
- Pneumonia Cheat Sheet: by ViaDocument3 pagesPneumonia Cheat Sheet: by ViaGayle MarieNo ratings yet
- Acute TracheobronchitisDocument15 pagesAcute Tracheobronchitisp.apples634No ratings yet
- Streptococcus Pneumonae: Pathophysiology of CopdDocument1 pageStreptococcus Pneumonae: Pathophysiology of CopdDimpal ChoudharyNo ratings yet
- Respiratory Pedia Activity - Gomez, Griselle Ann J.Document1 pageRespiratory Pedia Activity - Gomez, Griselle Ann J.Griselle GomezNo ratings yet
- Nursing CS CroupDocument1 pageNursing CS Croupreuben kadarajaNo ratings yet
- Pathophysiology: Entry of Microorganism To Nasal PassagesDocument1 pagePathophysiology: Entry of Microorganism To Nasal PassagesBrian John DugayNo ratings yet
- Ventilatory Assistance Study GuideDocument9 pagesVentilatory Assistance Study GuideBrianna RorickNo ratings yet
- Respiratory Conditions ChartDocument1 pageRespiratory Conditions ChartAmanda MuchaNo ratings yet
- Unit 1 5ADocument7 pagesUnit 1 5AArvin O-CaféNo ratings yet
- Med SurgDocument3 pagesMed SurgShaira Mae GordoraNo ratings yet
- Clinical Pictures of AATDDocument2 pagesClinical Pictures of AATDHamed AhmedNo ratings yet
- Impaired Gas Exchange NCPDocument4 pagesImpaired Gas Exchange NCPkimglaidyl bontuyanNo ratings yet
- Bronchiolitis 44Document7 pagesBronchiolitis 44Fati NurNo ratings yet
- Pathophysiology & Concept Map: Precipitating FactorsDocument2 pagesPathophysiology & Concept Map: Precipitating FactorsVanessa Rose Vargas0% (1)
- 4.1 PEDIA-Pneumonia, Tuberculosis, Interstitial Lung Diseases (Dr. Bermejo)Document6 pages4.1 PEDIA-Pneumonia, Tuberculosis, Interstitial Lung Diseases (Dr. Bermejo)Monique BorresNo ratings yet
- Pa Tho Physiology of MumpsDocument1 pagePa Tho Physiology of MumpslilchecksNo ratings yet
- Respiratory FailureDocument5 pagesRespiratory Failureta CNo ratings yet
- Pleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- The Thoracic CavityDocument43 pagesThe Thoracic Cavitybayenn100% (2)
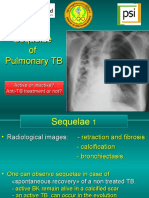
- 15c TB SequelaeDocument49 pages15c TB SequelaeWin Sein Myint100% (1)
- Name - Date - Score - TesDocument2 pagesName - Date - Score - TesSHEILA MAE PERTIMOSNo ratings yet
- Group 4 Gas Exchange BioDocument29 pagesGroup 4 Gas Exchange BioLJ Princess Mary MontenegroNo ratings yet
- Therapeutic Gases 9.3.17 and CoughDocument29 pagesTherapeutic Gases 9.3.17 and CoughThor O100% (1)
- Mediastinal MassesDocument110 pagesMediastinal Massesosep77100% (1)
- Student Support Material X EnglishDocument103 pagesStudent Support Material X EnglishMaydhansh KadgeNo ratings yet
- Tlm4all@10th Bs Imp MatchingDocument9 pagesTlm4all@10th Bs Imp MatchingThirupathaiahNo ratings yet
- C O P D: Hronic Bstructive Ulmonary IseaseDocument53 pagesC O P D: Hronic Bstructive Ulmonary IseaseLe KhoaNo ratings yet
- Chavis Davis Autopsy ReportDocument7 pagesChavis Davis Autopsy ReportwendyistaNo ratings yet
- Alteration in Respiratory SystemDocument138 pagesAlteration in Respiratory Systemcute_gurljhoanNo ratings yet
- 12 Respiratory System - ATFDocument43 pages12 Respiratory System - ATFLucas BarbosaNo ratings yet
- Congenital Cystic Adenomatoid Malformation (CCAM)Document7 pagesCongenital Cystic Adenomatoid Malformation (CCAM)sarguss14No ratings yet
- Overhead Transparency Human AtlasDocument34 pagesOverhead Transparency Human Atlasdr tamerNo ratings yet
- Midterm Mathayom 2Document8 pagesMidterm Mathayom 2AbdullohNo ratings yet
- Penetration of Anti Infective Agents Into.3Document28 pagesPenetration of Anti Infective Agents Into.3Thawatchai NakkaratniyomNo ratings yet
- Anatomy of LungDocument47 pagesAnatomy of Lungadelina.jianu9991No ratings yet
- DIB - Week 01 - 02 - Anatomy & Physiology PDFDocument99 pagesDIB - Week 01 - 02 - Anatomy & Physiology PDFFaisal MujibNo ratings yet
- NCM 112 Lec 1 Sir Arnel Respiratory System: Basic Gas-Exchange Unit of The RespiratoryDocument5 pagesNCM 112 Lec 1 Sir Arnel Respiratory System: Basic Gas-Exchange Unit of The RespiratoryJane BautistaNo ratings yet
- Yamada Et Al 2024 Pictorial Review of Pleural Disease Multimodality Imaging and Differential DiagnosisDocument17 pagesYamada Et Al 2024 Pictorial Review of Pleural Disease Multimodality Imaging and Differential Diagnosisgabrielajimena202No ratings yet
- Beige and Brown Vintage Risograph Illustration Cutout Scrapbook Animated PresentationDocument38 pagesBeige and Brown Vintage Risograph Illustration Cutout Scrapbook Animated PresentationKyla Macauba VHNo ratings yet
- Breathing AND Exchange of Gases MCQs PDFDocument78 pagesBreathing AND Exchange of Gases MCQs PDFJatin SinglaNo ratings yet
- Lung Capacity LabDocument3 pagesLung Capacity LabMasato KimuraNo ratings yet
- Msds K2cro4 PDFDocument6 pagesMsds K2cro4 PDFAnonymous U0RczPNo ratings yet
- Metastatic TumorsDocument43 pagesMetastatic TumorsRadio ResidentNo ratings yet
- Chest Injury and Its TypesDocument14 pagesChest Injury and Its TypesKoochi PoojithaNo ratings yet
- The Physical Benefits of SalatDocument7 pagesThe Physical Benefits of SalateLrynaNo ratings yet
- Chapter 40-OxygenationDocument14 pagesChapter 40-OxygenationHaji RajiNo ratings yet