Professional Documents
Culture Documents
Protozoan Parasites
Protozoan Parasites
Uploaded by
francelourdiette25Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Protozoan Parasites
Protozoan Parasites
Uploaded by
francelourdiette25Copyright:
Available Formats
MLS 108 LECTURE 1
- Microsporidia are a group of spore-forming
PROTOZOAN PARASITES unicellular parasites. These spores contain an
extrusion apparatus that has a coiled polar tube
PROTOZOA
ending in an anchoring disc at the apical part of
• Provided with nucleus/nuclei, cytoplasm, outer the spore. They were once considered protozoans
limiting membrane, and cellular elaborations called or protists, but are now known to be fungi, or a
organelles. sister group to fungi.
• Locomotory apparatus: cilia, flagella and
pseudopodia.
• Require a wet environment for feeding, locomotion,
osmoregulation, and reproduction.
Stages:
• Cyst – infective stage
• Trophozoite – vegetative stage CLASSIFICATION OF PROTOZOAN PARASITES
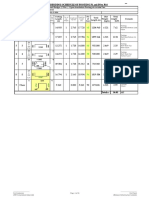
Sarcomastigophora Entamoeba histolytica
Entaamoeba coli
Sarcodina Entamoeba dispar
Entamoeba hartmanni
Entamoeba polecki
Entamoeba gingivalis
Iodamoeba butschlii
Endolimax nana
Naegleria fowleri
Acanthamoeba spp.
Mastigophora Chilomastix mesnili
KINGDOM: PROTISTA Dientamoeba fragilis
Giardia lamblia
PHYLA: Pentatrichomonas hominis
(formerly Trichomonas hominis)
• Sarcomastigophora
• Ciliophora Trichomonas tenax
• Apicomplexa Trichomonas vaginalis
- They have a unique organelle called an apicoplast, Leishmania braziliensis
which is a non-photosynthetic plastid that helps them
penetrate host cells. Leishmania donovani
- They also have an apical complex structure that Leishmania tropica
contains several rings, including a conoid in some Trypanosoma brucei complex
species. They are spore-producing and lack
Trypanosoma cruzi
contractile vacuoles and locomotor processes.
Ciliophora Balantidium coli
• Microspora Apicomplexa Babesia spp.
Francine Lourdiette Castro 1
MLS 108 LECTURE 2
- apical complex at the anterior Cryptosporidium hominis The resulting trophozoites proliferate by binary fission in the
end which consists of polar lumen of the colon.
Cyclospora cayatanensis
rings, subpellicular tubules,
conoid, rhoptries, and Isospora belli Both cysts and trophozoites may be passed in feces, but only
micronemes. mature cysts are infective.
Plasmodium spp.
Toxoplasma gondii Note:
Microspora Enterocytozoon bineusi
E. histolytica is the only amebic species capable of invading
consists of spore-forming Encephalitozoon spp. tissues and causing disease.
parasites of both vertebrates
Vittaforma cornea
and invertebrates.
Trachipleistophora homimis
Pleistophora spp.
Brachiola vesicularum
Microsporidium spp.
INTESTINAL AMOEBA
7 species of amoebae that are commonly found in human fecal
specimens:
1) Entamoeba histolytica
2) Entamoeba dispar
3) Entamoeba hartmanni
4) Entamoeba coli
5) Entamoeba polecki
6) Endolimax nana
7) Iodamoeba butschlii
ENTAMOEBA HISTOLYTICA
• Subphylum: Sarcodina
3 genera of amebae may inhabit the intestinal tract: • Superclass: Rhizopoda
• Class: Lobosea
1) Entamoeba • Order: Amoebida
2) Endolimax • Family: Entamoebidae
3) Iodamoeba • Genus: Entamoeba
• Specie: Histolytica
Cysts are ingested and excyst in the small intestine
Francine Lourdiette Castro 2
MLS 108 LECTURE 3
TAKE NOTE:
The scientific names of species are italicized. The genus name
is always capitalized and is written first; the specific epithet
follows the genus name and is not capitalized.
There is no exception to this!
Example:
• Entamoeba histolytica
• Entamoeba histolytica
CONT. ENTAMOEBA HISTOLYTICA
• Pseudopod-forming nonflagellated parasite
• Most invasive of the parasites in the Entamoeba family MODES OF TRANSMISSION
• The only member of the family to cause colitis and
liver abscess a) fecal-oral contact
b) direct colonic inoculation through contaminated
enema equipment.
LIFE CYCLE OF E. HISTOLYTICA
• Infection by Entamoeba histolytica occurs
by ingestion of mature cysts in fecally contaminated
food, water, or hands.
• Excystation occurs in the small intestine and
trophozoites are released, which migrate to the large
2 STAGES IN THE LIFE CYLE: intestine.
• Cyst
- The quadrinucleate cyst is resistant to gastric
acidity and desiccation and can survive in a moist
environment for several weeks.
• Trophozoite
PATHOGENESIS AND CLINICAL MANIFESTATIONS
• may cause various clinical diseases:
- amebic dysentery
- amebic colitis
- liver abscess
STAGES OF DEVELOPMENT: AMEBIC DYSENTERY
Francine Lourdiette Castro 3
MLS 108 LECTURE 4
• Acute disease characterized by bloody diarrhea with b) right upper quadrant pain (diagnosed by radiographic
abdominal cramping. scans, ultrasound, and serologic tests).
• Invasion of the intestinal mucosa occurs, producing c) Rarely appear in other organs, such as the lung, brain,
ulceration that may lead to perforation and peritonitis. or skin, either by hematogenous spread from the
intestine or by contiguous spread from a liver abscess.
AMEBIC COLITIS
• mimic ulcerative colitis.
• Less severe than amoebic dysentery (may include
non-bloody diarrhea, constipation, abdominal
cramping, and weight loss).
• Develops small, pinpoint mucosal ulcerations and
expand within the submucosa to form flask-shaped
ulcers.
PATHOLOGY
Invasiveness of the trophozoites is facilitated by:
a) Gal/Gal Nac lectin which mediates adherence to the
host cells
b) Amebapores which forms pores in host cell
membranes
c) cysteine proteinases which are cytopathic for host
tissues
AMEBIC LIVER ABSCESS
most common form of extraintestinal amebiasis (5% of patients IMMUNITY
with a history of intestinal amebiasis)
• Natural immunity (intestines) – mucin inhibition of
Symptoms: amebic attachment to mucosal cells.
• Systemic circulation – complement-mediated killing
a) fever of trophozoites
Francine Lourdiette Castro 4
MLS 108 LECTURE 5
• Activated T-cells kill E.histo by: • Minimum of 3 stool specimens collected in different
a) directly lysing trophozoites in a contact- days should be examined.
dependent process • Fresh stool examination should be examined within 30
b) producing cytokines which activate macrophages mins. (troph identification)
c) providing helper effect for B cell Ab production • DFS with saline – observe troph motility (unidirectional
movement)
EFFECTS OF AMEBIC MODULATION OF HOST IMMUNE • Saline and MB – differentiating Entamoeba from WBCs
RESPONSES: • Saline and iodine – nucleus and karyosome can be
observed
Infected subjects have been shown to be in a state of
- Karyosome – in the center of the nucleus
immunosuppression during acute stage:
- Centrally locally (E. histolytica), ara sa kilid ang
a) T cell hyporesponsiveness nucleus (E. coli)
b) suppressed proliferation and cytokine production • E.histo troph with ingested RBC – diagnostic of
c) depressed delayed type hypersensitivity amebiasis
d) macrophage suppression
DIFFERENTIAL DIAGNOSIS:
BACILLARY DYSENTERY AMEBIC DYSENTERY
Maybe epidemic Seldom epidemic
Acute oneset Gradual oneset
Prodromal fever and malaise No prodromal features
common
Vomiting common No vomiting CONCENTRATION METHOD
Patient prostrate Patient usually ambulant
• Formalin ether concentration test (FECT)
Watery, bloody diarrhea Bloody diarrhea • Merthiolate iodine formalin concentration test (MIFC)
Odorless stool Fishy odor stool
Morphological structures are noted:
Stool microscopy: numerous Stool microscopy: few bacilli,
bacilli, pus cells, macrophages, red cells, trophozoites with - size of the cyst
red cells, no Charcot-Leyden ingested RBCs, Charcot-Leyden - number nuclei
crystals crystals
- location and appearance of karyosome
Abdominal cramps common Mild abdominal cramps - characteristic appearance of chromatoid bodies
and severe - presence of cytoplasmic structures such as glycogen
Tenesmus common Tenesmus uncommon vacuole.
Natural history: spontaneous Natural history: lasts for weeks,
recovery in few days, weeks, or dysentery returns after
more: no relapse remission, infection persists for
years
Side notes:
• Prostrate – sever exhaustion
• Ambulant – nagalakat lakat pa kuno ang patient
• Charcot-Layden Crystals – just the product of
integrated eosinophils
• Tenesmus – abi mo ma poop ka pero ubos na
DIAGNOSIS
Microscopic Diagnosis:
Francine Lourdiette Castro 5
MLS 108 LECTURE 6
NOTE:
Laboratories who do not use one of the immunologic or
molecular methods to differentiate E. histolytica from E. dispar,
and rely exclusively on morphologic analysis, must use a
reporting format – “E. histolytica/E. dispar” would be most
appropriate.
SEROLOGY
• Serum Abs – key in the dx of ALA (amoebic liver
abscess)
Able to detect Abs of past infection
- indirect hemagglutination (IHAT)
Short duration Abs detection
- counter immunoelectrophoresis (CIE)
- agar gel diffusion (AGD)
- indirect fluorescent antibody test (IFAT)
- enzyme-linked immunosorbent assay (ELISA)
TREATMENT AND PROGNOSIS
2 objectives:
• To cure invasive disease at both intestinal and extra-
intestinal sites
• To eliminate the passage of cysts from the intestinal
lumen
- Metronidazole (drug of choice)
- Nitroimidazole (tinidazole secnidazole)
- Diloxanide furoate (asymptomatic cyst
passers)
Francine Lourdiette Castro 6
You might also like
- Siemens Siremobil Compact Error CodesDocument160 pagesSiemens Siremobil Compact Error CodesHabib93% (30)
- Designmate 3024/3036 Top AssemblyDocument11 pagesDesignmate 3024/3036 Top AssemblySerge MaciaNo ratings yet
- New Sialkot International AirportDocument7 pagesNew Sialkot International Airportm.suleman Khushi100% (1)
- LV5-1510-20-UL-SLR 1MW/ GFDI/6input/Insul - Monitor: Verdrahtungshinweise Wiring InstructionsDocument113 pagesLV5-1510-20-UL-SLR 1MW/ GFDI/6input/Insul - Monitor: Verdrahtungshinweise Wiring Instructionsedvaldo alves pintoNo ratings yet
- Species Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesDocument2 pagesSpecies Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesautumntreesNo ratings yet
- List of Parasites and Their Common Names: Compiled Topics in Parasitology By: BNKLDocument47 pagesList of Parasites and Their Common Names: Compiled Topics in Parasitology By: BNKLDIVINE GRACE FLORITA PEPITONo ratings yet
- Sistematika ParasitDocument30 pagesSistematika ParasitFatmawati NadhyaNo ratings yet
- 1MicrobioTrans - EukaryotesDocument9 pages1MicrobioTrans - EukaryotesJeztin Faye Del RosarioNo ratings yet
- Week14 Protozoa1 Transcript PDFDocument23 pagesWeek14 Protozoa1 Transcript PDFrabiaNo ratings yet
- Protists: BiologyDocument56 pagesProtists: BiologyAgnesia NcihoNo ratings yet
- Classification of Veterinary ProtozoansDocument10 pagesClassification of Veterinary ProtozoansihtishamulhaqNo ratings yet
- 7.stool Examination - Morphology of Eggs, Cysts, LarvaeDocument9 pages7.stool Examination - Morphology of Eggs, Cysts, LarvaeKowshik AvulaNo ratings yet
- Fungi Classification MapDocument3 pagesFungi Classification MapShoaibNo ratings yet
- Parasitology Post TestDocument6 pagesParasitology Post TestLaiza Janelle AtendidoNo ratings yet
- Parasitology ClassificationDocument4 pagesParasitology Classificationaparna viswanbNo ratings yet
- Intestinal and Luminal ProtozoaDocument27 pagesIntestinal and Luminal ProtozoashafariyahNo ratings yet
- BotanyDocument25 pagesBotanynaagin12300No ratings yet
- PARA NematodesDocument23 pagesPARA Nematodes12 Newton - Cayetano, Arafe Nicole A.No ratings yet
- Mycology Must KnowDocument5 pagesMycology Must Knowblueandblack2417No ratings yet
- Introduction To para For Med.Document73 pagesIntroduction To para For Med.amare kumlachewNo ratings yet
- Parasite TaxonomyDocument2 pagesParasite TaxonomyJoanne Mary RomoNo ratings yet
- ED Na STR FUNGIDocument46 pagesED Na STR FUNGIdw21541No ratings yet
- Helminths 12Document34 pagesHelminths 12malakaiad212No ratings yet
- AlveolateDocument8 pagesAlveolatex456456456xNo ratings yet
- Supplemental Readings On ProtozoansDocument18 pagesSupplemental Readings On Protozoansferrerjericho300No ratings yet
- Asal Mula Keragaman EukariotDocument16 pagesAsal Mula Keragaman EukariotRofiqoNo ratings yet
- Caracter Is Tica Delos Hong OsDocument59 pagesCaracter Is Tica Delos Hong OsCaysahuana Seguil Jose NilsonNo ratings yet
- Introduction To Parasitology - B28Document23 pagesIntroduction To Parasitology - B28Heswer RajNo ratings yet
- Merge AbDocument17 pagesMerge AbEricsson CarabbacanNo ratings yet
- P A R T: NematodesDocument21 pagesP A R T: NematodesGrazielle Almazan100% (2)
- Kingdoms Shortlisting PDFDocument28 pagesKingdoms Shortlisting PDFNoman KhanNo ratings yet
- Tabelase ParazitologieDocument10 pagesTabelase ParazitologieAlexandraCrauNo ratings yet
- Lesson 8 - Nematodes IDocument7 pagesLesson 8 - Nematodes IAnya IgnacioNo ratings yet
- Week 4 Medical and Public Health ParasitologyDocument36 pagesWeek 4 Medical and Public Health Parasitologylewistulio004No ratings yet
- Mode of Reproduction: Invertebrate Animals: October 2018Document11 pagesMode of Reproduction: Invertebrate Animals: October 2018Sophia Pauline HernandezNo ratings yet
- Plant Taxonomy NotesDocument13 pagesPlant Taxonomy NotesMikaela MendozaNo ratings yet
- Parasite Cheat SheetDocument4 pagesParasite Cheat SheetSeyahNo ratings yet
- MUST To KNOW in ParasitologyDocument22 pagesMUST To KNOW in ParasitologyTristan Jay CalabiaNo ratings yet
- Clinical Parasitology PrelimsDocument25 pagesClinical Parasitology PrelimsErilyn MarinduqueNo ratings yet
- General Characteristics of AlveolataDocument25 pagesGeneral Characteristics of AlveolataNada AmrNo ratings yet
- MycologyDocument68 pagesMycologyANCHELANo ratings yet
- MUST To KNOW in Parasitology PDFDocument22 pagesMUST To KNOW in Parasitology PDFvillajanellaNo ratings yet
- HSSRPTR - Botany Focus Area NotesDocument27 pagesHSSRPTR - Botany Focus Area Notesfiredrops122No ratings yet
- Day 2 Additional Lecture Notes For Genetics Cell Bio Microbio and AnaphyDocument91 pagesDay 2 Additional Lecture Notes For Genetics Cell Bio Microbio and AnaphyJeffrey PolisticoNo ratings yet
- Protozoa Summary TableDocument1 pageProtozoa Summary TablejustNo ratings yet
- Rule of ThumbDocument2 pagesRule of ThumbChandy TaralaNo ratings yet
- ParasitologyDocument27 pagesParasitologyDreyden HaloNo ratings yet
- Microbiology T-02 (2nd Edition)Document261 pagesMicrobiology T-02 (2nd Edition)baratniloy1No ratings yet
- Blood and Tissue Protozoan Blood and Tissue Protozoan Blood and Tissue Protozoan Urogenital Protozoa - Pear Shaped-FlagellatedDocument1 pageBlood and Tissue Protozoan Blood and Tissue Protozoan Blood and Tissue Protozoan Urogenital Protozoa - Pear Shaped-FlagellatedMohamed ElserwyNo ratings yet
- protozoaDocument48 pagesprotozoaleoreynon19No ratings yet
- Sarcodina Amoebae (Amoebas) (False Feet)Document4 pagesSarcodina Amoebae (Amoebas) (False Feet)Lyka ReyesNo ratings yet
- BACTERIOLOGYDocument9 pagesBACTERIOLOGYJe GregorioNo ratings yet
- ParasiteDocument27 pagesParasiteAbdullah AlkharsNo ratings yet
- Species Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesDocument2 pagesSpecies Common/Other Name Pathogenesis Mot/Infective Stage Diagnostic Stage I. NematodesArenNo ratings yet
- My CologyDocument15 pagesMy Cologydeytonu63No ratings yet
- Parasit OlogyDocument20 pagesParasit OlogysherwinbuluranNo ratings yet
- Arthropoda: BIO2135 Animal Form & FunctionDocument18 pagesArthropoda: BIO2135 Animal Form & FunctionGabrielle ForgetNo ratings yet
- Parasitology: An IntroductionDocument8 pagesParasitology: An IntroductionRuthenie RedobleNo ratings yet
- BMY4301 - MollicutesDocument7 pagesBMY4301 - MollicutesMUHAMMAD FIKQRAN SHAH BIN SHAHRIZAD / UPMNo ratings yet
- ChinilinDocument37 pagesChinilinyepNo ratings yet
- Merged PDF 2021 11 16T12 - 01 - 01Document15 pagesMerged PDF 2021 11 16T12 - 01 - 01Ericsson CarabbacanNo ratings yet
- EntamoebaDocument94 pagesEntamoebaAtlas AstreaNo ratings yet
- Mushroom Spotter's Deck: A Field Guide to Fungi & Their Age-Old WisdomFrom EverandMushroom Spotter's Deck: A Field Guide to Fungi & Their Age-Old WisdomNo ratings yet
- Tagburos FinalDocument46 pagesTagburos FinalZiedwrick Ayson DicarNo ratings yet
- Advanced Monolithic Systems: 800ma Low Dropout Voltage RegulatorDocument8 pagesAdvanced Monolithic Systems: 800ma Low Dropout Voltage RegulatorTahar BenacherineNo ratings yet
- Department of Education: Daily Lesson PlanDocument14 pagesDepartment of Education: Daily Lesson PlanSharlene Jane Roque AporboNo ratings yet
- Providing Food Stations For Stray Animals: National Service Training ProgramDocument8 pagesProviding Food Stations For Stray Animals: National Service Training ProgramLeane ZapantaNo ratings yet
- Structure AhmedabadDocument87 pagesStructure AhmedabadNandpal Prashant100% (1)
- Hmma 865-03Document24 pagesHmma 865-03eugenio.gutenbertNo ratings yet
- Analysis of Diaphragm WallDocument6 pagesAnalysis of Diaphragm WallSanthosh BabuNo ratings yet
- Third Space Learning - Nov 2022 Foundation Paper 2 Mark Scheme - EdexcelDocument8 pagesThird Space Learning - Nov 2022 Foundation Paper 2 Mark Scheme - EdexcelArzhel BoissinotNo ratings yet
- AA SL Test 1Document3 pagesAA SL Test 1Ejaz Ahmad100% (1)
- Sohbi Kohgei - Solar Power System Proposal (Toshiba325W)Document4 pagesSohbi Kohgei - Solar Power System Proposal (Toshiba325W)Jeffcaster ComelNo ratings yet
- K 512472Document2 pagesK 512472Daniel ManoleNo ratings yet
- BBS of All Pier Foundations of MAYARDocument16 pagesBBS of All Pier Foundations of MAYARAmanjot Singh0% (1)
- Danfoss Product Overview WebDocument4 pagesDanfoss Product Overview WebOlivera MilenkovicNo ratings yet
- Semester Scheme Odd21Document90 pagesSemester Scheme Odd21Rahul SinghNo ratings yet
- Terex Jaques - ST JawDocument12 pagesTerex Jaques - ST Jawjonathandyson100% (2)
- AsDocument777 pagesAsCristhian QuimizNo ratings yet
- Factsheet - REPowerEU PDFDocument2 pagesFactsheet - REPowerEU PDFconor farrellNo ratings yet
- Timing Calibration Harness AssemblyDocument5 pagesTiming Calibration Harness Assemblyflordeliz jimenez rodriguezNo ratings yet
- A Narrative Report On Informing The Barangay 1 and Barangay 9Document3 pagesA Narrative Report On Informing The Barangay 1 and Barangay 9Heugh Gerard Rizo33% (3)
- Ir. H. Isnugroho, CES: Faculty of Engineering Civil Engineering Program Study Muhammadiyah University of SurakartaDocument21 pagesIr. H. Isnugroho, CES: Faculty of Engineering Civil Engineering Program Study Muhammadiyah University of SurakartaRhezader AgNo ratings yet
- Anti-Inflammatory and Analgesic Activities of Flavonoid and Saponin Fractions From Zizyphus Lotus (L.) LamDocument5 pagesAnti-Inflammatory and Analgesic Activities of Flavonoid and Saponin Fractions From Zizyphus Lotus (L.) LamDaris UntoroNo ratings yet
- Modeling and Simulation of A Distillation Column Using MatlabDocument15 pagesModeling and Simulation of A Distillation Column Using Matlabrajtharun48No ratings yet
- ASTM C 566 Kadar AirDocument2 pagesASTM C 566 Kadar AirBengkulu BetonNo ratings yet
- ZX450 ZX650Document109 pagesZX450 ZX650mohanNo ratings yet
- Cradles of Early Science Development of Science in Asia IndiaDocument4 pagesCradles of Early Science Development of Science in Asia IndiaAvox EverdeenNo ratings yet
- Beating The Bonk QuestionsDocument1 pageBeating The Bonk Questionst3xxaNo ratings yet