Professional Documents
Culture Documents
aerly appropiated care
aerly appropiated care
Uploaded by
Surlanys LezamaCopyright:
Available Formats
You might also like
- The Eucharistic Miracles of The WorldDocument2 pagesThe Eucharistic Miracles of The WorldFrancisco MartinezNo ratings yet
- Anterior Cervical Discectomy and FusionDocument7 pagesAnterior Cervical Discectomy and FusionGeraldine Alvarez ANo ratings yet
- Vesta 1000 01 PDFDocument53 pagesVesta 1000 01 PDFDuta NarendratamaNo ratings yet
- David 2003Document4 pagesDavid 2003Sung Soon ChangNo ratings yet
- Fraktur FemurDocument11 pagesFraktur FemurYusuf BrilliantNo ratings yet
- The World Society of Emergency Surgery WSES SpleenDocument10 pagesThe World Society of Emergency Surgery WSES SpleenLily GaribaldyNo ratings yet
- Polytrauma Management - What Is New and What Is True in 2020?Document8 pagesPolytrauma Management - What Is New and What Is True in 2020?JJCONo ratings yet
- Benefit of Multidisciplinary Wound Care Center On The Volume and Outcomes of A Vascular Surgery PracticeDocument8 pagesBenefit of Multidisciplinary Wound Care Center On The Volume and Outcomes of A Vascular Surgery PracticeCandace LongNo ratings yet
- Artículos OrtopediaDocument8 pagesArtículos OrtopediaTania salais obregonNo ratings yet
- Coccolini2019 Article TheWorldSocietyOfEmergencySurgDocument9 pagesCoccolini2019 Article TheWorldSocietyOfEmergencySurgfaisaldanyaniNo ratings yet
- The 2019 ESSKA Meniscus ConsensusDocument18 pagesThe 2019 ESSKA Meniscus ConsensusQuiroprácticaParaTodosNo ratings yet
- Art:10.1186/1471 2474 15 188Document8 pagesArt:10.1186/1471 2474 15 188indriNo ratings yet
- Journal of Clinical Orthopaedics and TraumaDocument8 pagesJournal of Clinical Orthopaedics and TraumaandiNo ratings yet
- 2018 Article 211Document4 pages2018 Article 211Cinthya Añazco RomeroNo ratings yet
- Medi 97 E0523Document9 pagesMedi 97 E0523Andrea OsborneNo ratings yet
- Pi Is 0976566220304872Document11 pagesPi Is 0976566220304872rivanNo ratings yet
- Using Risk Models To Improve Patient Selection For High-Risk Vascular SurgeryDocument14 pagesUsing Risk Models To Improve Patient Selection For High-Risk Vascular Surgerylino.delabarreraNo ratings yet
- Moore 2019Document5 pagesMoore 2019Tania salais obregonNo ratings yet
- 2014 Article 3495Document7 pages2014 Article 3495cogajoNo ratings yet
- The Current Relationship Between Surgeon ReimburseDocument4 pagesThe Current Relationship Between Surgeon ReimburseRenan Scalon MachadoNo ratings yet
- Length of Stay Total Knee ArthroplastyDocument9 pagesLength of Stay Total Knee ArthroplastyRista MarginaNo ratings yet
- Dco 5 PDFDocument10 pagesDco 5 PDFGauda GranthanaNo ratings yet
- Comparison of Treatment Outcomes Associated With Early Versus Late Treatment of Mandible Fractures - A Retrospective Chart Review and AnalysisDocument5 pagesComparison of Treatment Outcomes Associated With Early Versus Late Treatment of Mandible Fractures - A Retrospective Chart Review and AnalysisMichaella LimNo ratings yet
- Indications and Interventions of Damage Control Orthopedic SurgeriesDocument12 pagesIndications and Interventions of Damage Control Orthopedic SurgeriesSacha SalasNo ratings yet
- Anaesthetic Considerations in Polytrauma PatientsDocument8 pagesAnaesthetic Considerations in Polytrauma PatientsMileidys LopezNo ratings yet
- Modern and Classic Wound Dressing Comparison in WoDocument6 pagesModern and Classic Wound Dressing Comparison in WoJuan LuckyNo ratings yet
- What Adverse Events and Injuries Are Cited in Anesthesia Malpractice Claims For NonspineDocument11 pagesWhat Adverse Events and Injuries Are Cited in Anesthesia Malpractice Claims For NonspineManolin KinNo ratings yet
- Computer-Assisted Preoperative Planning Improves TDocument12 pagesComputer-Assisted Preoperative Planning Improves TAlishaNo ratings yet
- Comparison of Functional Outcome Between Early and Usual CPM Physiotherapy in Healing Tibia Plateau FractureDocument14 pagesComparison of Functional Outcome Between Early and Usual CPM Physiotherapy in Healing Tibia Plateau FractureAthenaeum Scientific PublishersNo ratings yet
- Critical Care Considerations in Trauma - Overview, Trauma Systems, Initial Assessment PDFDocument19 pagesCritical Care Considerations in Trauma - Overview, Trauma Systems, Initial Assessment PDFPaulina Jiménez JáureguiNo ratings yet
- Three-Dimensional Printed Models Can Reduce Costs and Surgical Time For ComplexDocument11 pagesThree-Dimensional Printed Models Can Reduce Costs and Surgical Time For ComplextaylortNo ratings yet
- DiniDocument10 pagesDiniMuhammad Yasdar BahriNo ratings yet
- Application of Trauma Time Axis Management in The Treatment of Severe Trauma PatientsDocument6 pagesApplication of Trauma Time Axis Management in The Treatment of Severe Trauma PatientsFelix NainggolanNo ratings yet
- Analysis of Risk Factors in Thoracic Trauma Patients With A Comparison of A Modern Trauma Centre: A Mono-Centre StudyDocument10 pagesAnalysis of Risk Factors in Thoracic Trauma Patients With A Comparison of A Modern Trauma Centre: A Mono-Centre StudyWahyu SholekhuddinNo ratings yet
- Bessire 2014Document7 pagesBessire 2014andrei3cucuNo ratings yet
- Comparison of Closed Femur Fracture: Skeletal Traction and Intramedullary Nailing Cost-EffectivenessDocument6 pagesComparison of Closed Femur Fracture: Skeletal Traction and Intramedullary Nailing Cost-EffectivenessS3V4_9154No ratings yet
- WSES Splenic TraumaDocument26 pagesWSES Splenic TraumaAndreas RendraNo ratings yet
- Rodgers Lucio Et Al Risk MGMT HCPolicy 2012 Economics Less Invasive SpineSxDocument10 pagesRodgers Lucio Et Al Risk MGMT HCPolicy 2012 Economics Less Invasive SpineSxAmanda MatthewsNo ratings yet
- Enfermeras y Camas en UciDocument10 pagesEnfermeras y Camas en UciÁlvaro Raúl Conto MorenoNo ratings yet
- Current Concepts in Orthopedic Management of Multiple TraumaDocument8 pagesCurrent Concepts in Orthopedic Management of Multiple TraumanellieauthorNo ratings yet
- International Wound Journal - 2023 - Zhai - Impact of Fast Track Rehabilitation Nursing On Pressure Ulcers andDocument9 pagesInternational Wound Journal - 2023 - Zhai - Impact of Fast Track Rehabilitation Nursing On Pressure Ulcers andMaya LessyNo ratings yet
- Surgical Preferences of Patients at Risk of Hip Fractures: Hemiarthroplasty Versus Total Hip ArthroplastyDocument9 pagesSurgical Preferences of Patients at Risk of Hip Fractures: Hemiarthroplasty Versus Total Hip ArthroplastyCraciun Ana-MariaNo ratings yet
- Trauma Surgery and Acute Care Surgery: Evolution in The Eye of The StormDocument3 pagesTrauma Surgery and Acute Care Surgery: Evolution in The Eye of The StormDeddy WidjajaNo ratings yet
- Critical Biomechanical and Clinical Insights Concerning Tissue Protection When Positioning Patients in The Operating Room: A Scoping ReviewDocument19 pagesCritical Biomechanical and Clinical Insights Concerning Tissue Protection When Positioning Patients in The Operating Room: A Scoping ReviewDiana Pacheco BriceñoNo ratings yet
- Design and Implementation of A Trauma Care BundleDocument7 pagesDesign and Implementation of A Trauma Care BundleNi Nyoman AstriningsihNo ratings yet
- Eichinger2021 Article ChallengesInThePREHOSPITALEmerDocument12 pagesEichinger2021 Article ChallengesInThePREHOSPITALEmerBarry TraceyNo ratings yet
- Anaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative ReviewDocument7 pagesAnaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative Reviewomar gonzalezNo ratings yet
- Diagnostics 12 01289Document15 pagesDiagnostics 12 01289Sushmica BaquiranNo ratings yet
- A Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesDocument11 pagesA Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesJeremyNo ratings yet
- Art 1Document7 pagesArt 1Hajji AhmedNo ratings yet
- To Identify The Spectrum of Post Operative Complications and Appropriate Management in Polytraumatised Patients With Musculoskeletal InjuriesDocument4 pagesTo Identify The Spectrum of Post Operative Complications and Appropriate Management in Polytraumatised Patients With Musculoskeletal InjuriesShaneed KpNo ratings yet
- Systematic Review and Meta-Analysis of Endovascular Therapy Versus Open Surgical Repair For The Traumatic Lower Extremity Arterial InjuryDocument10 pagesSystematic Review and Meta-Analysis of Endovascular Therapy Versus Open Surgical Repair For The Traumatic Lower Extremity Arterial InjuryRamiro Manzano NúñezNo ratings yet
- Swart 2016Document7 pagesSwart 2016TommysNo ratings yet
- 1 s2.0 S0737614618300017 MainDocument22 pages1 s2.0 S0737614618300017 MainJEFFERSON MUÑOZNo ratings yet
- Splenic Trauma WSES Classification and GuidelinesDocument27 pagesSplenic Trauma WSES Classification and GuidelinespgmzNo ratings yet
- ContohDocument9 pagesContohVino DoangNo ratings yet
- Meniscus Root Repair Vs Meniscectomy orDocument8 pagesMeniscus Root Repair Vs Meniscectomy orJulio Cesar Guillen MoralesNo ratings yet
- Burns v7 1 151Document10 pagesBurns v7 1 151Beatriz BeckerNo ratings yet
- Optimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchDocument18 pagesOptimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchEva GarciaNo ratings yet
- 1 s2.0 S002013832030632XDocument6 pages1 s2.0 S002013832030632XKar RodriguezNo ratings yet
- Term PolytraumaDocument13 pagesTerm PolytraumaElmer NarvaezNo ratings yet
- Acetabular Fractures in Older Patients: Assessment and ManagementFrom EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonNo ratings yet
- DevynsresumeDocument2 pagesDevynsresumeapi-272399469No ratings yet
- RPD Daily Incident Report 2/3/21Document7 pagesRPD Daily Incident Report 2/3/21inforumdocsNo ratings yet
- (Limpin, Shakti Dev) Mil Q4W1Document3 pages(Limpin, Shakti Dev) Mil Q4W1Shakti Dev LimpinNo ratings yet
- Test Bank For Biology The Unity and Diversity of Life 14Th Edition by Starr Taggart and Evers Isbn 1305073959 978130507395 Full Chapter PDFDocument36 pagesTest Bank For Biology The Unity and Diversity of Life 14Th Edition by Starr Taggart and Evers Isbn 1305073959 978130507395 Full Chapter PDFjoan.derrick732100% (10)
- 03 Preliminary PagesDocument12 pages03 Preliminary PagesBillie Jan Louie JardinNo ratings yet
- Escovilla 4qmath3aa2 - Patterns in The World I Live inDocument7 pagesEscovilla 4qmath3aa2 - Patterns in The World I Live inapi-743665882No ratings yet
- Ajit ResumeDocument3 pagesAjit ResumeSreeluNo ratings yet
- ENG 10 Q2 Lesson 8 Techniques in Public SpeakingDocument29 pagesENG 10 Q2 Lesson 8 Techniques in Public SpeakingronsairoathenadugayNo ratings yet
- An Overview of Monopolistic CompetitionDocument9 pagesAn Overview of Monopolistic CompetitionsaifNo ratings yet
- Ecofeminism Perspective - A Gendered Approach in Reducing Poverty by Implementing Sustainable Development Practices in IndonesiaDocument20 pagesEcofeminism Perspective - A Gendered Approach in Reducing Poverty by Implementing Sustainable Development Practices in IndonesiaM. NaQviNo ratings yet
- Self Affirmation ScaleDocument19 pagesSelf Affirmation ScaleQonitah Arya SulthanahNo ratings yet
- Literature Review of Water Level SensorDocument4 pagesLiterature Review of Water Level Sensorc5mr3mxf100% (1)
- A. H. M. Jones - Studies in Roman Government and Law-Basil Blackwell (1960)Document260 pagesA. H. M. Jones - Studies in Roman Government and Law-Basil Blackwell (1960)L V100% (1)
- Avinash Mourya TYBMSDocument66 pagesAvinash Mourya TYBMSAbhi KengaleNo ratings yet
- Engr. Frederick B. Garcia: Proposed 3-Storey ResidenceDocument1 pageEngr. Frederick B. Garcia: Proposed 3-Storey Residencesam nacionNo ratings yet
- Conjugarea Verbului Manifesta: Indicativ PrezentDocument4 pagesConjugarea Verbului Manifesta: Indicativ PrezentAndrei PleșaNo ratings yet
- Social Media and Political Communication in India: An Analysis of 2017 Legislative Assembly Elections in Himachal PradeshDocument7 pagesSocial Media and Political Communication in India: An Analysis of 2017 Legislative Assembly Elections in Himachal PradeshEditor IJTSRDNo ratings yet
- Admission Form Eleven Class Mar 2016Document3 pagesAdmission Form Eleven Class Mar 2016Aaqib AliNo ratings yet
- Toym and TofilDocument19 pagesToym and TofilJohn Rey CempronNo ratings yet
- The Emotional Tone Scale - Read "The Hubbard Chart of Human EvaluationDocument1 pageThe Emotional Tone Scale - Read "The Hubbard Chart of Human EvaluationErnesto Salomon Jaldín MendezNo ratings yet
- Schematic Diagram of Relay & Tcms Panel T: REV Revised by Checked by Approved byDocument1 pageSchematic Diagram of Relay & Tcms Panel T: REV Revised by Checked by Approved byTaufiq HidayatNo ratings yet
- Hematology: Mohamad H Qari, MD, FRCPADocument49 pagesHematology: Mohamad H Qari, MD, FRCPASantoz ArieNo ratings yet
- Bago CityDocument8 pagesBago CityTricia Marvi P. NavarroNo ratings yet
- Christian Worldview - PostmodernismDocument6 pagesChristian Worldview - PostmodernismLuke Wilson100% (2)
- 3 Year - V - Sem - FinalDocument208 pages3 Year - V - Sem - FinalKARTHIK ANo ratings yet
- A Project Report-1 - 231020 - 204422Document59 pagesA Project Report-1 - 231020 - 204422Ankit Sharma 028No ratings yet
- Argala: Illustration: Define Primary Argala and Virodha Argala On Lagna For A Standard BirthDocument4 pagesArgala: Illustration: Define Primary Argala and Virodha Argala On Lagna For A Standard Birthsurinder sangarNo ratings yet
- Banners of The Insurgent Army of N. Makhno 1918-1921Document10 pagesBanners of The Insurgent Army of N. Makhno 1918-1921Malcolm ArchibaldNo ratings yet
aerly appropiated care
aerly appropiated care
Uploaded by
Surlanys LezamaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
aerly appropiated care
aerly appropiated care
Uploaded by
Surlanys LezamaCopyright:
Available Formats
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
Authors: Abstract
Early appropriate care (EAC) is a treatment
Nickolas J Nahm MD1 protocol for trauma patients with unstable fractures of
Heather A Vallier MD2 the thoracolumbar spine, pelvis, acetabulum, and/or
femur. The protocol was designed to expedite treatment
Authors note: based on patient physiologic readiness for definitive
fracture surgery. In the EAC protocol, patients are
1
Department of aggressively resuscitated and managed by a
Orthopaedic Surgery, multidisciplinary team. Upon achieving predefined
Henry Ford Hospital, thresholds for adequate resuscitation, patients undergo
Detroit, MI. Email: definitive stabilization of their fractures with the goal of
nnahm1@hfhs.org performing surgery within 36 hours of injury. As an
integrated care pathway, the EAC protocol defines a time
2
Department of dependent strategy to trauma care and minimizes
Orthopaedic Surgery, complications and reduces cost through a
MetroHealth Medical multidisciplinary approach. Adoption of the EAC
Center, Case Western protocol was achieved through buy-in from all involved
Reserve University, parties in the development phase and contributed to
Cleveland, OH. subsequent adherence to the protocol. As such, lessons
learned from the development, institution and study of
Email: the EAC protocol may be applied to other clinical
hvallier@metrohealth.org challenges in orthopaedic trauma, including fracture
management in high-energy geriatric injuries as well as
head injury.
Keywords: pathway, early appropriate care, timing
fixation, multiply-injured
Copyright 2017 KEI Journals. All Rights Reserved. Page | 1
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
1. Introduction Prolonged bed rest is associated with
Trauma care is provided in a poor pulmonary compromise and
multidisciplinary fashion and is most thromboembolic disease (12). For these
effective and efficient in regionalized reasons, many authors advocate early
trauma centers (1). In particular, the definitive fracture fixation in order to
multiply-injured patient requires promote mobility, reducing
immediate care from several specialists complications and length of stay (LOS)
and availability of intensive care units (13-15). However, the balance between
and operating rooms. As a result, the early fracture fixation and patient’s
care of the trauma patient is resource ability to tolerate surgery has been
intensive but cost effective due to debated within the literature (16, 17).
improved clinical outcomes achieved in The EAC protocol addresses these issues
trauma centers (2). Nevertheless, trauma by defining specific resuscitation
centers face challenges in financial thresholds for fracture fixation with the
viability, and continuous efforts are goal of definitive fracture surgery within
required to establish practice patterns 36 hours of injury. In this review, we
that result in optimal patient outcomes provide an overview of the factors
and are also cost-efficient (3, 4). leading to the development of the EAC
One avenue for achieving protocol, discuss outcomes associated
excellent clinical outcomes in a cost- with the EAC protocol, and define the
efficient manner in trauma care is the use of and opportunities available for
integrated care pathway (ICP) (5). ICPs ICPs in orthopaedic trauma.
are time-dependent treatment protocols
utilizing a multidisciplinary approach. 2. Regionalization of trauma care:
With respect to orthopaedic practice, background for Early Appropriate
ICPs have been studied extensively in Care
the total joint arthroplasty literature and The trauma patient is frequently
are associated with decreased associated with injuries that span the
complications and cost in this population domain of many specialties and
(6, 7). They have also been utilized with therefore requires a multidisciplinary
success in geriatric patients with hip approach for treatment (18). Substantial
fracture (8, 9). However, their use is not investment in resources is required to
as well-established in the management maintain readiness for trauma care, and,
of the multiply-injured patient requiring as a result, the care of the trauma patient
fracture care. is regionalized (19). The American
The Early Appropriate Care College of Surgeons (ACS) formalized
(EAC) protocol is a type of ICP this regionalization in 1976 by
developed to address the timing of categorizing hospitals based on
definitive surgery in unstable fractures resources needed to provide different
of the spine, pelvis, acetabulum, and levels of care for trauma (20).
femur (10). In the trauma patient, these Subsequent to the development
fractures are similar injuries because of trauma center status, multiple studies
they predispose to systemic demonstrated the benefit of Level I
inflammation and require patients to trauma centers on clinical outcomes and
maintain bed rest prior to fixation (11). cost. Nathens et al showed that states
Copyright 2017 KEI Journals. All Rights Reserved. Page | 2
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
with trauma system implementation had (26.3%), and cardiac care (15.6%) (24).
an 8% reduction in motor vehicle crash The authors concluded that the
mortality compared to states without an investment necessary to maintain trauma
organized system of trauma care, after center status is sustained by favorable
adjusting for restraint laws, laws that contributions to hospital net revenue.
deter drunk driving, and laws that allow Despite improved and cost-
for highway speeds greater than 55 mph effective care provided by trauma
(21). The findings of this study were centers, trauma centers face significant
verified in the National Study on the challenges to financial viability,
Costs and Outcomes of Trauma particularly due to issues surrounding
(NSCOT), a large multi-center study patient transfer. In an analysis of the
examining mortality from all National Trauma Data Bank, Koval et al
mechanisms of injury. In this study, studied patients with low Injury Severity
MacKenzie et al showed that both in- Scores (ISS ≤ 9) (26). They found that
hospital mortality (relative risk of 0.80) 21% of patients with low severity
as well as one year mortality (relative injuries were transferred to a Level I
risk of 0.75) were significantly lower in trauma center. Compared to patients who
level I trauma centers compared to were not transferred, transferred patients
hospitals without trauma center with low severity injuries were more
designation (22). likely to have Medicaid insurance versus
In addition to improved clinical other types of insurance (OR 2.02, 99%
outcomes, care provided by trauma CI 1.89-2.15), were more likely to
centers has been shown to be cost- present during evenings or nights
effective. In an analysis of the NSCOT compared to mornings or afternoons
data, Mackenzie et al showed that the (OR 2.25, 99% CI 2.15-2.35), and be
added cost of treatment at a trauma African American versus Caucasian race
center was $36,319 per life year gained (OR 1.28, 99% CI 1.21-1.36), after
compared to hospitals without trauma controlling for confounding factors. The
center designation (2). Although the authors concluded that transfer of
economic value of a statistical year of injured patients occurs for reasons other
life has been debated, a commonly cited than medical necessity, as outlined by
benchmark is $50,000 to $200,000 (23). the Emergency Medical Treatment and
Based on this estimate, the authors Active Labor Act. In another study of
concluded that the more expensive care patients treated at a Level I trauma
provided at trauma centers is more cost- center, transfer patients were found to
effective. Furthermore, trauma care has have lower ISS compared to patients
been shown to positively impact the who were not transferred (27).
financial characteristics of a trauma Furthermore, the authors found that a
center (24, 25). In a retrospective study higher proportion of patients with low
of a single Level I trauma center, severity injury (ISS < 18) had no
Breedlove et al showed that Level I insurance versus patients with ISS ≥ 18.
trauma care had favorable contribution Transferred patients were also more
margins (40.2%) relative to other service likely to undergo delayed definitive
lines at their hospital, including fixation of their fractures, which is
orthopaedics (29.8%), oncology associated with higher complications in
Copyright 2017 KEI Journals. All Rights Reserved. Page | 3
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
medically stable patients. These studies study evaluating early (≤ 24 hours after
suggest that initial triage and transfer injury) versus delayed (> 48 hours after
processes require optimization so that injury) treatment of femoral shaft
trauma centers can continue to maintain fractures (28). They reported more
financial viability and provide pulmonary complications (acute
expeditious fracture care. In this setting respiratory distress syndrome (ARDS),
of financial challenges, trauma centers pneumonia, and fat embolism), greater
must seek patient care strategies that hospital costs, and longer LOS in
produce excellent clinical outcomes but multiply-injured patients treated on a
are also cost-effective. delayed basis. This study was
foundational for the philosophy of early
3. Development of the Early total care in which all fractures are
Appropriate Care protocol treated on an early basis. The authors
Trauma centers are able to suggested that early total care allows
provide better patient outcomes in part patients to avoid bed rest and recumbent
due to patient care algorithms that positioning, which are associated with
continuously evolve based on research poor pulmonary toilet and
efforts. The management of unstable thromboembolic complications (12).
axial fractures (spine, pelvis, The paradigm of early total care
acetabulum, and femur) in the multiply- shifted with the introduction of damage
injured patients remains an area of active control orthopaedics (DCO) (29). In this
investigation. Based on this treatment approach, the initial injury
investigation, fracture care in these event is described as a “first hit,” which
patients has changed dramatically with primes an inflammatory response (30).
respect to timing of definitive surgery. Fracture surgery is the “second hit” that
Early Appropriate Care (EAC) is a aggravates the inflammatory response
protocol driven pathway for fracture care and predisposes the trauma patient to
in multiply-injured patients that emerged immune-mediated complications,
from this investigation (10). Based on including systemic inflammatory
measures of resuscitation, including response syndrome, ARDS, and multiple
lactate, arterial pH, and base excess, organ dysfunction syndrome. In order to
patients with unstable fractures of the minimize the “second hit,” many authors
axial skeleton undergo definitive suggested that definitive fracture surgery
treatment of their fractures within 36 should be delayed in favor of
hours of injury. Efforts are made in temporizing stabilization, such as
patients who do not meet these external fixation (31-33). In particular,
thresholds to continue resuscitation so subgroups of “borderline” and unstable
that fracture care may be undertaken in patients were thought to be vulnerable to
an expeditious manner. the “second hit” phenomenon, and DCO
The EAC protocol was was recommended in these patients (34).
developed in the background of a In a randomized controlled trial, the
significant volume of work in the area of European Polytrauma Study on the
fracture care in multiply-injured patients. Management of Femur Fractures study
In a landmark paper, Bone et al group compared DCO to early definitive
performed a prospective, randomized treatment of femoral shaft fractures (16).
Copyright 2017 KEI Journals. All Rights Reserved. Page | 4
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
Among stable patients, DCO was undertaken in a large cohort of patients
associated with increased time on (n=1,443) with unstable injuries of the
ventilation but no differences in thoracolumbar spine, pelvis, acetabulum,
pulmonary complications. However, in and/or femur in order to identify injuries,
borderline patients, early definitive physiology, or laboratory parameters
treatment was associated with higher associated with complications (10). This
rate of acute lung injury, with no set of injuries was selected for review
difference in other pulmonary due to bed rest and recumbent
complications. positioning required prior to fixation, as
The DCO strategy set the stage these activity restrictions portend a
for EAC. DCO studies emphasized that common pathway of poor pulmonary
subgroups of patients require further toilet and thromboembolic disorders
resuscitation prior to definitive fracture (12). Definitive fracture fixation within
surgery. The main question was which 36 hours of injury was recommended in
patients require further resuscitation or patients with lactate < 4.0 mmol/L, pH ≥
should be delayed for other reasons. In 7.25, or base excess ≥ -5.5 mmol/L
developing the EAC protocol, (Table 1).
multivariable regression analysis was
Table 1. Early Appropriate Care protocol
Timing of fracture fixation
Parameter* ≤36 hours >36 hours
pH ≥7.25 <7.25
Base excess (mmol/L) ≥-5.5 <-5.5
Lactate (mmol/L) <4.0 ≥4.0
*Definitive fracture fixation recommended when a patient has
responded to resuscitation and any one parameter is met
In the EAC protocol, findings are similar to the results of
resuscitation is ongoing and other investigators who found that
continuously monitored in order to diligent resuscitation after injury
expedite definitive fracture surgery. In a promotes early fracture care and limits
prospective evaluation of the EAC the use of DCO (35), preventing
protocol, Vallier et al found that all additional hospital stay and costs
patients (n=335) achieved adequate associated with a secondary surgery.
resuscitation within 36 hours of injury
(11). Definitive fracture fixation was 4. Cost and outcomes associated with
delayed most commonly due to surgeon Early Appropriate Care
preference. Patients treated on an early The EAC protocol was
basis experienced fewer complications developed in the context of increasing
and shorter length of stay. These challenges to the viability of trauma
Copyright 2017 KEI Journals. All Rights Reserved. Page | 5
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
care. Specifically, disproportionately fractures and US $4,304 for patients
frequent care for the underinsured, with pelvis or acetabulum fractures (38).
declining reimbursement from payers, The authors estimated that the reduction
and fewer available subspecialists, in complications associated with
represent threats to high quality care implementation of the EAC protocol
provided by Level I trauma centers (4, resulted in annual cost savings of US
27, 36). The EAC protocol not only $2,227,151 to their trauma center. In
addresses clinical outcomes but also sum, these data represent compelling
optimizes efficiency and cost associated support for the use of the EAC protocol,
with trauma care. both with regard to improved patient
Because the EAC protocol outcomes as well as systems based
emphasizes the resuscitation process, processes and cost savings.
patients are continuously monitored for
adequacy of resuscitation and undergo 5. Integrated care pathways in
fracture fixation in an expeditious orthopaedic trauma
manner when thresholds for surgery are The EAC protocol represents one
met. As a result, patients recover and example of the increasing trend toward
participate with physical therapy after the use of integrated care pathways
surgery and are on their way to hospital (ICPs) in orthopaedics and medicine as a
discharge in a time-efficient manner. whole (5). An ICP standardizes care at
Indeed, prospective review of the EAC specific time points during a treatment
protocol at a Level I trauma center course (39). ICPs are dependent on a
demonstrated that patients undergoing multidisciplinary approach to achieve
early fixation (≤ 36 hours after injury) predefined outcomes (40). ICPs in
had shorter mean intensive care unit trauma, as well as other subspecialties,
(ICU) stays (4.5 vs 9.4 days, p < 0.0001) including total joint arthroplasty and
and hospital LOS (9.4 vs 15.3 days, p < pediatric orthopaedics, have also
0.0001) compared to delayed fixation demonstrated success by reducing
(>36 hours after injury) (37). The complications, hospital LOS, and cost
increased LOS for patients treated on a (6, 41-43). As an ICP, the EAC protocol
delayed basis translated to a mean loss has an established track record for fewer
of revenue of US $6,380 per patient. complications, shorter hospital LOS, and
Furthermore, the authors estimated that lower costs of care (11, 37, 38, 44).
the facility revenue loss associated with Because multidisciplinary care is
a hospital bed that could not be used for necessary for the care of the orthopaedic
an additional trauma patient was US trauma patient, the opportunities for
$35,330. ICPs in orthopaedic trauma are
Furthermore, the reduction in substantial. Geriatric fracture cares for
complications associated with the EAC both low-energy and a high-energy
protocol translates to more cost-effective injury is an area of particular interest,
care. In another study analyzing the given the aging population (45). ICPs
financial impact of the EAC protocol, have been studied extensively in
Childs and Vallier found that a geriatric hip fracture literature. In a
complication increased the cost of care study evaluating co-management of
by US $4,368 for patients with femur geriatric patients with hip fracture by
Copyright 2017 KEI Journals. All Rights Reserved. Page | 6
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
orthopaedic surgeons and geriatricians, with normal vital signs (50). The authors
Friedman et al found lower complication found that mortality associated with a
rates (30.6% versus 46.3%), shorter LOS heart rate greater than 90 in elderly
(4.6 versus 8.3 days), and shorter time to patients did not equal mortality in a
surgery (24.1 versus 37.4 hours) for co- younger cohort until heart rate was
managed patients compared to standard greater than 130. The authors concluded
care (46). In another study, the authors that increased caution is required in
found that this co-managed protocol geriatric trauma patients and new triage
driven program resulted in significant set points of HR > 90 and SBP < 110
cost savings, 66.7% of the expected mmHg should be considered. Another
costs nationally (47). Co-management study examined the impact of increased
services and treatment protocols vigilance in geriatric trauma patients by
optimize the treatment of this fragile initiating trauma team activation for all
population and reduce expenses. patients age 70 years or more with early
The study of ICPs in high-energy aggressive monitoring and resuscitation
geriatric trauma is more limited. The (51). The authors found significantly
high-energy geriatric trauma patient reduced mortality after the initiation of
represents unique challenges. Due to the this ICP (34.2% versus 53.8%, p=0.003).
physiology and comorbidities specific to The importance of recognizing occult
the geriatric population (48), this shock was emphasized by another study
subgroup of trauma patients may benefit examining the impact of aggressive
significantly from a multidisciplinary monitoring and resuscitation in the
approach available through an ICP. Of geriatric population who presented with
note, trauma centers that provide pedestrian versus motor vehicle
effective care for younger adult trauma mechanism of injury, having multiple
patients do not necessarily provide the fractures, head injury, initial blood
same level of care for geriatric patients. pressure less than 150 mmHg, or
In a retrospective review of the Quebec acidosis (52). In this study, Scalea et al
Trauma Registry, Moore et al showed found that early invasive monitoring
that risk-adjusted mortality rate for improved survival in patients older than
younger adult trauma patients did not 65 years-old from 7% to 53%. These
necessarily correlate with risk-adjusted studies suggest that recognizing occult
mortality rate for geriatric patients (49). shock with early invasive monitoring
These findings suggest that trauma and providing aggressive resuscitation
principles utilized for young adult are key elements of an ICP for high-
patients may not necessarily apply to energy geriatric trauma.
geriatric patients. In an example of applying these
Furthermore, geriatric trauma principles to practice, Bradburn et al
patients often present with normal vital established an ICP for geriatric trauma
signs but are under-resuscitated. In a patients (53). Their ICP consisted of
retrospective study, elderly patients (≥ identifying high-risk geriatric patients
65 years old) presenting with normal based on injury profile, medical history
vital signs were found to have a higher indicators, and physiologic parameters.
mortality rate compared to other adult After identifying a high-risk patient,
patients (17 to 35 years old) presenting markers of resuscitation, including ABG
Copyright 2017 KEI Journals. All Rights Reserved. Page | 7
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
and base excess, as well as ICU another study examining early femur
admission and geriatric consultation fracture fixation in patients with head
were obtained. Compared to a time injury, Scalea et al found no difference
period prior to the initiation of this high- in discharge GCS, mortality, and CNS
risk geriatric protocol, the authors found complications between patients treated
a significant decrease in mortality after on an early basis (≤ 24 hours) and
adjusting for confounding variables (OR patients treated on a delayed basis (> 24
0.63, p=0.046). In another study hours) (58). To our knowledge, high
examining the use of the EAC protocol quality prospective evaluation has not
in elderly trauma patients, Reich et al been performed.
found no difference in complications for An ICP in this subgroup of
patients ≤ 30 years-old (16%) compared patients with head injury requiring
to patients ≥ 60 years-old (16%, p=0.84). fracture fixation would necessarily
The authors concluded that the EAC involve a multidisciplinary team of
protocol was a viable treatment neurosurgeons, intensivists,
algorithm for elderly patients but that anesthesiologists, and orthopaedic
further study was required to evaluate surgeons to determine preoperative
pre-existing medical conditions. Future monitoring and resuscitation as well as
study examining the impact of these appropriate anesthesia and intraoperative
measures on hospital course and costs of monitoring. Intracranial pressure
care will further delineate the effect of monitoring in these patients appears
an ICP in elderly high-energy trauma warranted in many situations (58).
patients. Furthermore, fluid resuscitation
The presence of a head injury in supplemented by vasopressors as
the patient requiring fracture fixation necessary is required to avoid central
presents a unique challenge for which nervous system hypoperfusion (59).
ICPs could play an important role. Future study examining thresholds for
Specifically, the timing of definitive surgery and the impact of these
fracture fixation in the setting of head thresholds on complications and costs is
injury has been evaluated multiple times required for the development of an ICP.
in prior literature, but evidence regarding Despite improved clinical
timing of fracture surgery is still unclear outcomes and cost of care associated
(54). The primary concern for early with ICP, the adoption and use of ICPs
fracture fixation in this cohort of patients may represent a significant barrier (5).
is intra-operative hypotension and Manning et al suggested that adoption of
hypoxia with the potential to cause ICP may be limited by a culture of
secondary brain injury (55, 56). Jaicks et physician autonomy, scarce resources,
al found a trend toward increased and conflicting financial incentives
hypotension and hypoxia in patients with between physicians and hospital
head injury receiving early fracture management. Specifically, in the culture
fixation (< 24 hours) versus patients of orthopaedics, independence is highly-
receiving delayed fixation (> 24 hours) valued so with the implementation of an
(57). The implications of these findings ICP, the surgeon may be reluctant to
were unclear as the study found no participate (60). Furthermore,
difference in mortality or LOS. In implementing an ICP represents a major
Copyright 2017 KEI Journals. All Rights Reserved. Page | 8
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
undertaking requiring substantial ICP (63). This process ensures
investments of time and money. The ownership and buy-in from the
lack of resources and time was identified orthopaedic surgeon. Furthermore,
as one of the greatest barriers to incentives for participation in the ICP,
collaboration among providers (61). including financial bonuses and better
Finally, cooperation between hospital operative room availability, may also
management and physicians required for improve physician adoption of an ICP
instituting an ICP may be limited by (64). Finally, penalties for non-
reimbursement. Hospitals often receive adherence are viewed as a final resort
one predefined payment for a patient’s and may have implications on hospital
hospital stay based on a diagnosis, but credentialing and financial
the physician may be reimbursed on a reimbursement (65).
per procedure basis, which creates a Implementation of the EAC
conflicting financial reimbursement protocol was noted to be successful
structure (62). These barriers to ICP almost at the start and adherence
adoption can be addressed by involving improved steadily over a two-year
the orthopaedic surgeon in the period (Figure 1) (66).
development and implementation of the
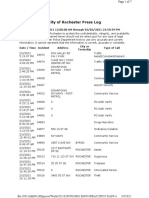
Figure 1. Delayed fixation by fracture type (66). Comparison of percentage (y axis) of
patients treated on a delayed basis depending on the type of fracture: spine, pelvis,
acetabulum, or femur. Comparisons are made with a historical group of patients treated
for 3 years prior to the EAC protocol implementation and with the first and second years
after the implementation of EAC.
90
80
70
60
50 historical
EAC year 1
40
EAC year 2
30
20
10
0
spine acetabulum pelvis femur
Copyright 2017 KEI Journals. All Rights Reserved. Page | 9
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
In the first three months after compared to 76% of similar fractures
implanting the EAC protocol, 22% of treated historically (Table 2).
fractures were treated on a delayed basis
Table 2. Fractures treated more than 36 hours after injury in the Early
Appropriate Care protocol. 59 fractures in 54 patients were treated on a delayed
basis.
Fractures treated with Surgeon choice to treat
definitive fixation more than 36 fractures more than 36
Quarter* hours after injury (%) hours after injury (%)
1 22.0 16.2
2 27.0 16.2
3 23.0 8.8
4 17.0 11.3
5 10.2 10.2
6 11.8 8.8
7 15.3 5.1
8 10.0 10.0
*Each quarter is defined by a sequential 3 month period
Data are used with permission from the work of Vallier et al (66)
Furthermore, in the last three implementation. This process ensured
months of the study period, <10% of ownership from all involved physicians.
fractures were treated on a delayed basis. Finally, the authors noted that the EAC
Of note, all patients met thresholds for protocol contains a simple set of
resuscitation within 36 hours of injury, parameters, which assisted in adherence.
but 54 patients were treated on a delayed Although implementation of the EAC
basis. The most common reason for protocol was found to be successful,
delayed treatment was surgeon continued study of processes relevant to
preference (67%). The authors ICP implementation is needed to
concluded that teamwork from providers optimize care and reduce cost.
as well as institutional support in the 6. Conclusion
form of operating room and equipment The regionalization of trauma
accessibility contributed to the rapid care centralizes specialists and resources
adoption of the EAC protocol. The necessary for the optimal care of the
authors also reported that protocol trauma patient. In the setting of trauma
development involved subspecialists centers, ICPs show promise in
from general surgery, critical care, optimizing patient outcomes and
anesthesiology, neurosurgery, and improving the efficiency and cost of
orthopaedic trauma. All involved parties care. As an example of an ICP, the EAC
took part in developing details of the protocol decreases complications and
protocol and timeline for reduces costs among patients with
Copyright 2017 KEI Journals. All Rights Reserved. Page | 10
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
unstable fractures of the thoracolumbar pathways in geriatric trauma and head
spine, pelvis, acetabulum, and femur. injury. Further examination of methods
Certainly, ICPs have been used with for instituting and adopting ICPs
success for patient populations within represents another avenue for
orthopaedics with opportunities investigation.
available for optimization of these
Copyright 2017 KEI Journals. All Rights Reserved. Page | 11
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
References
1. Jurkovich GJ, Mock C. 9. Adunsky A, Arad M, Levi R,
Systematic review of trauma system Blankstein A, Zeilig G, Mizrachi E.
effectiveness based on registry Five-year experience with the 'Sheba'
comparisons. J Trauma. 1999;47(3 model of comprehensive orthogeriatric
Suppl):S46-55. care for elderly hip fracture patients.
2. MacKenzie EJ, Weir S, Rivara Disabil Rehabil. 2005;27(18-19):1123-7.
FP, Jurkovich GJ, Nathens AB, Wang 10. Vallier HA, Wang X, Moore TA,
W, et al. The value of trauma center Wilber JH, Como JJ. Timing of
care. J Trauma. 2010;69(1):1-10. orthopaedic surgery in multiple trauma
3. Crichlow RJ, Zeni A, Reveal G, patients: development of a protocol for
Kuhl M, Heisler J, Kaehr D, et al. early appropriate care. J Orthop Trauma.
Appropriateness of patient transfer with 2013;27(10):543-51.
associated orthopaedic injuries to a 11. Vallier HA, Moore TA, Como JJ,
Level I trauma center. J Orthop Trauma. Wilczewski PA, Steinmetz MP, Wagner
2010;24(6):331-5. KG, et al. Complications are reduced
4. Nathens AB, Maier RV, Copass with a protocol to standardize timing of
MK, Jurkovich GJ. Payer status: the fixation based on response to
unspoken triage criterion. J Trauma. resuscitation. J Orthop Surg Res.
2001;50(5):776-83. 2015;10:155.
5. Manning BT, Callahan CD, 12. Seibel R, LaDuca J, Hassett JM,
Robinson BS, Adair D, Saleh KJ. Babikian G, Mills B, Border DO, et al.
Overcoming resistance to Blunt multiple trauma (ISS 36), femur
implementation of integrated care traction, and the pulmonary failure-
pathways in orthopaedics. J Bone Joint septic state. Ann Surg. 1985;202(3):283-
Surg Am. 2013;95(14):e100 1-6. 95.
6. Jimenez Munoz AB, Duran 13. Bosse MJ, MacKenzie EJ,
Garcia ME, Rodriguez Perez MP, Riemer BL, Brumback RJ, McCarthy
Sanjurjo M, Vigil MD, Vaquero J. ML, Burgess AR, et al. Adult respiratory
Clinical pathway for hip arthroplasty six distress syndrome, pneumonia, and
years after introduction. Int J Health mortality following thoracic injury and a
Care Qual Assur Inc Leadersh Health femoral fracture treated either with
Serv. 2006;19(2-3):237-45. intramedullary nailing with reaming or
7. Pearson S, Moraw I, Maddern with a plate. A comparative study. J
GJ. Clinical pathway management of Bone Joint Surg Am. 1997;79(6):799-
total knee arthroplasty: a retrospective 809.
comparative study. Aust N Z J Surg. 14. Vallier HA, Cureton BA, Ekstein
2000;70(5):351-4. C, Oldenburg FP, Wilber JH. Early
8. Leung AH, Lam TP, Cheung definitive stabilization of unstable pelvis
WH, Chan T, Sze PC, Lau T, et al. An and acetabulum fractures reduces
orthogeriatric collaborative intervention morbidity. J Trauma. 2010;69(3):677-84.
program for fragility fractures: a 15. Bellabarba C, Fisher C, Chapman
retrospective cohort study. J Trauma. JR, Dettori JR, Norvell DC. Does early
2011;71(5):1390-4. fracture fixation of thoracolumbar spine
fractures decrease morbidity or
Copyright 2017 KEI Journals. All Rights Reserved. Page | 12
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
mortality? Spine (Phila Pa 1976). 24. Breedlove LL, Fallon WF, Jr.,
2010;35(9 Suppl):S138-45. Cullado M, Dalton A, Donthi R,
16. Pape HC, Rixen D, Morley J, Donovan DL. Dollars and sense:
Husebye EE, Mueller M, Dumont C, et attributing value to a level I trauma
al. Impact of the method of initial center in economic terms. J Trauma.
stabilization for femoral shaft fractures 2005;58(4):668-73; discussion 73-4.
in patients with multiple injuries at risk 25. Vallier HA, Patterson BM,
for complications (borderline patients). Meehan CJ, Lombardo T. Orthopaedic
Ann Surg. 2007;246(3):491-9; traumatology: the hospital side of the
discussion 9-501. ledger, defining the financial
17. Morshed S, Miclau T, 3rd, relationship between physicians and
Bembom O, Cohen M, Knudson MM, hospitals. J Orthop Trauma.
Colford JM, Jr. Delayed internal fixation 2008;22(4):221-6.
of femoral shaft fracture reduces 26. Koval KJ, Tingey CW, Spratt
mortality among patients with KF. Are patients being transferred to
multisystem trauma. J Bone Joint Surg level-I trauma centers for reasons other
Am. 2009;91(1):3-13. than medical necessity? J Bone Joint
18. MacKenzie EJ, Hoyt DB, Sacra Surg Am. 2006;88(10):2124-32.
JC, Jurkovich GJ, Carlini AR, 27. Vallier HA, Parker NA, Beddow
Teitelbaum SD, et al. National inventory ME. Reasons for transfer to a level 1
of hospital trauma centers. JAMA. trauma center and barriers to timely
2003;289(12):1515-22. definitive fracture fixation. J Orthop
19. Taheri PA, Butz DA, Lottenberg Trauma. 2014;28(12):e284-9.
L, Clawson A, Flint LM. The cost of 28. Bone LB, Johnson KD, Weigelt
trauma center readiness. Am J Surg. J, Scheinberg R. Early versus delayed
2004;187(1):7-13. stabilization of femoral fractures. A
20. Resources for Optimal Care of prospective randomized study. J Bone
the Injured Patient, 6th ed. Rotondo MF, Joint Surg Am. 1989;71(3):336-40.
Cribari C, Smith RS, editors. Am Coll 29. Scalea TM, Boswell SA, Scott
Surg. Chicago, IL, 2014. JD, Mitchell KA, Kramer ME, Pollak
21. Nathens AB, Jurkovich GJ, AN. External fixation as a bridge to
Cummings P, Rivara FP, Maier RV. The intramedullary nailing for patients with
effect of organized systems of trauma multiple injuries and with femur
care on motor vehicle crash mortality. fractures: damage control orthopedics. J
JAMA. 2000;283(15):1990-4. Trauma. 2000;48(4):613-21; discussion
22. MacKenzie EJ, Rivara FP, 21-3.
Jurkovich GJ, Nathens AB, Frey KP, 30. Giannoudis PV, Smith RM,
Egleston BL, et al. A national evaluation Bellamy MC, Morrison JF, Dickson RA,
of the effect of trauma-center care on Guillou PJ. Stimulation of the
mortality. N Engl J Med. inflammatory system by reamed and
2006;354(4):366-78. unreamed nailing of femoral fractures.
23. Cutler DM, Rosen AB, Vijan S. An analysis of the second hit. J Bone
The value of medical spending in the Joint Surg Br. 1999;81(2):356-61.
United States, 1960-2000. N Engl J 31. Pape HC, Giannoudis P, Krettek
Med. 2006;355(9):920-7. C. The timing of fracture treatment in
Copyright 2017 KEI Journals. All Rights Reserved. Page | 13
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
polytrauma patients: relevance of multidisciplinary protocol that expedites
damage control orthopedic surgery. Am definitive fracture care. Am J Orthop
J Surg. 2002;183(6):622-9. (Belle Mead NJ). 2014;43(7):309-15.
32. Pape HC, Hildebrand F, Pertschy 39. Sladek ML, Swenson KK, Ritz
S, Zelle B, Garapati R, Grimme K, et al. LJ, Schroeder LM. A critical pathway
Changes in the management of femoral for patients undergoing one-day breast
shaft fractures in polytrauma patients: cancer surgery. Clin J Oncol Nurs.
from early total care to damage control 1999;3(3):99-106.
orthopedic surgery. J Trauma. 40. Fuss MA, Pasquale MD. Clinical
2002;53(3):452-61; discussion 61-2. management protocols: the bedside
33. Pape HC, Tornetta P, 3rd, Tarkin answer to clinical practice guidelines. J
I, Tzioupis C, Sabeson V, Olson SA. Trauma Nurs. 1998;5(1):4-11; quiz 27-8.
Timing of fracture fixation in 41. Barbieri A, Vanhaecht K, Van
multitrauma patients: the role of early Herck P, Sermeus W, Faggiano F,
total care and damage control surgery. J Marchisio S, et al. Effects of clinical
Am Acad Orthop Surg. 2009;17(9):541- pathways in the joint replacement: a
9. meta-analysis. BMC Med. 2009;7:32.
34. Pape HC, Giannoudis PV, 42. Shan LQ, Skaggs DL, Lee C,
Krettek C, Trentz O. Timing of fixation Kissinger C, Myung KS. Intensive care
of major fractures in blunt polytrauma: unit versus hospital floor: a comparative
role of conventional indicators in clinical study of postoperative management of
decision making. J Orthop Trauma. patients with adolescent idiopathic
2005;19(8):551-62. scoliosis. J Bone Joint Surg Am.
35. O'Toole RV, O'Brien M, Scalea 2013;95(7):e40.
TM, Habashi N, Pollak AN, Turen CH. 43. Sesperez J, Wilson S, Jalaludin
Resuscitation before stabilization of B, Seger M, Sugrue M. Trauma case
femoral fractures limits acute respiratory management and clinical pathways:
distress syndrome in patients with prospective evaluation of their effect on
multiple traumatic injuries despite low selected patient outcomes in five key
use of damage control orthopedics. J trauma conditions. J Trauma.
Trauma. 2009;67(5):1013-21. 2001;50(4):643-9.
36. McConnell KJ, Johnson LA, 44. Weinberg DS, Narayanan AS,
Arab N, Richards CF, Newgard CD, Moore TA, Vallier HA. Assessment of
Edlund T. The on-call crisis: a statewide resuscitation as measured by markers of
assessment of the costs of providing on- metabolic acidosis and features of injury.
call specialist coverage. Ann Emerg Bone Joint J. 2017;99-B(1):122-7.
Med. 2007;49(6):727-33, 33 e1-18. 45. Switzer JA, Gammon SR. High-
37. Vallier HA, Dolenc AJ, Moore energy skeletal trauma in the elderly. J
TA. Early Appropriate Care: A Protocol Bone Joint Surg Am. 2012;94(23):2195-
to Standardize Resuscitation Assessment 204.
and to Expedite Fracture Care Reduces 46. Friedman SM, Mendelson DA,
Hospital Stay and Enhances Revenue. J Bingham KW, Kates SL. Impact of a
Orthop Trauma. 2016;30(6):306-11. comanaged Geriatric Fracture Center on
38. Childs BR, Vallier HA. Cost short-term hip fracture outcomes. Arch
savings associated with a Intern Med. 2009;169(18):1712-7.
Copyright 2017 KEI Journals. All Rights Reserved. Page | 14
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
47. Kates SL, Mendelson DA, Trauma Acute Care Surg.
Friedman SM. The value of an organized 2012;73(5):1046-63.
fracture program for the elderly: early 55. Chesnut RM, Marshall LF,
results. J Orthop Trauma. Klauber MR, Blunt BA, Baldwin N,
2011;25(4):233-7. Eisenberg HM, et al. The role of
48. Bergeron E, Clement J, Lavoie secondary brain injury in determining
A, Ratte S, Bamvita JM, Aumont F, et outcome from severe head injury. J
al. A simple fall in the elderly: not so Trauma. 1993;34(2):216-22.
simple. J Trauma. 2006;60(2):268-73. 56. Pietropaoli JA, Rogers FB,
49. Moore L, Turgeon AF, Sirois Shackford SR, Wald SL, Schmoker JD,
MJ, Lavoie A. Trauma centre outcome Zhuang J. The deleterious effects of
performance: a comparison of young intraoperative hypotension on outcome
adults and geriatric patients in an in patients with severe head injuries. J
inclusive trauma system. Injury. Trauma. 1992;33(3):403-7.
2012;43(9):1580-5. 57. Jaicks RR, Cohn SM, Moller
50. Heffernan DS, Thakkar RK, BA. Early fracture fixation may be
Monaghan SF, Ravindran R, Adams CA, deleterious after head injury. J Trauma.
Jr., Kozloff MS, et al. Normal presenting 1997;42(1):1-5; discussion -6.
vital signs are unreliable in geriatric 58. Scalea TM, Scott JD, Brumback
blunt trauma victims. J Trauma. RJ, Burgess AR, Mitchell KA, Kufera
2010;69(4):813-20. JA, et al. Early fracture fixation may be
51. Demetriades D, Karaiskakis M, "just fine" after head injury: no
Velmahos G, Alo K, Newton E, Murray difference in central nervous system
J, et al. Effect on outcome of early outcomes. J Trauma. 1999;46(5):839-46.
intensive management of geriatric 59. Scalea TM, Maltz S, Yelon J,
trauma patients. Br J Surg. Trooskin SZ, Duncan AO, Sclafani SJ.
2002;89(10):1319-22. Resuscitation of multiple trauma and
52. Scalea TM, Simon HM, Duncan head injury: role of crystalloid fluids and
AO, Atweh NA, Sclafani SJ, Phillips TF, inotropes. Crit Care Med.
et al. Geriatric blunt multiple trauma: 1994;22(10):1610-5.
improved survival with early invasive 60. Davies C. Getting health
monitoring. J Trauma. 1990;30(2):129- professionals to work together. BMJ.
34; discussion 34-6. 2000;320(7241):1021-2.
53. Bradburn E, Rogers FB, Krasne 61. Gandhi TK, Puopolo AL, Dasse
M, Rogers A, Horst MA, Beelen MJ, et P, Haas JS, Burstin HR, Cook EF, et al.
al. High-risk geriatric protocol: Obstacles to collaborative quality
improving mortality in the elderly. J improvement: the case of ambulatory
Trauma Acute Care Surg. general medical care. Int J Qual Health
2012;73(2):435-40. Care. 2000;12(2):115-23.
54. Nahm NJ, Vallier HA. Timing of 62. Lee TH. Turning doctors into
definitive treatment of femoral shaft leaders. Harv Bus Rev. 2010;88(4):50-8.
fractures in patients with multiple 63. Keen J, Moore J, West R.
injuries: a systematic review of Pathways, networks and choice in health
randomized and nonrandomized trials. J care. Int J Health Care Qual Assur Inc
Copyright 2017 KEI Journals. All Rights Reserved. Page | 15
Medical Research Archives. Volume 5 Issue 5.May 2017.
Early appropriate care and opportunities for integrated care pathways in orthopaedic
trauma
Leadersh Health Serv. 2006;19(4- guidelines for clinical practice. Med
5):316-27. Care. 2001;39(8 Suppl 2):II46-54.
64. Chaix-Couturier C, Durand- 66. Vallier HA, Moore TA, Como JJ,
Zaleski I, Jolly D, Durieux P. Effects of Dolenc AJ, Steinmetz MP, Wagner KG,
financial incentives on medical practice: et al. Teamwork in Trauma: System
results from a systematic review of the Adjustment to a Protocol for the
literature and methodological issues. Int Management of Multiply Injured
J Qual Health Care. 2000;12(2):133-42. Patients. J Orthop Trauma.
65. Grol R. Successes and failures in 2015;29(11):e446-50.
the implementation of evidence-based
Copyright 2017 KEI Journals. All Rights Reserved. Page | 16
You might also like
- The Eucharistic Miracles of The WorldDocument2 pagesThe Eucharistic Miracles of The WorldFrancisco MartinezNo ratings yet
- Anterior Cervical Discectomy and FusionDocument7 pagesAnterior Cervical Discectomy and FusionGeraldine Alvarez ANo ratings yet
- Vesta 1000 01 PDFDocument53 pagesVesta 1000 01 PDFDuta NarendratamaNo ratings yet
- David 2003Document4 pagesDavid 2003Sung Soon ChangNo ratings yet
- Fraktur FemurDocument11 pagesFraktur FemurYusuf BrilliantNo ratings yet
- The World Society of Emergency Surgery WSES SpleenDocument10 pagesThe World Society of Emergency Surgery WSES SpleenLily GaribaldyNo ratings yet
- Polytrauma Management - What Is New and What Is True in 2020?Document8 pagesPolytrauma Management - What Is New and What Is True in 2020?JJCONo ratings yet
- Benefit of Multidisciplinary Wound Care Center On The Volume and Outcomes of A Vascular Surgery PracticeDocument8 pagesBenefit of Multidisciplinary Wound Care Center On The Volume and Outcomes of A Vascular Surgery PracticeCandace LongNo ratings yet
- Artículos OrtopediaDocument8 pagesArtículos OrtopediaTania salais obregonNo ratings yet
- Coccolini2019 Article TheWorldSocietyOfEmergencySurgDocument9 pagesCoccolini2019 Article TheWorldSocietyOfEmergencySurgfaisaldanyaniNo ratings yet
- The 2019 ESSKA Meniscus ConsensusDocument18 pagesThe 2019 ESSKA Meniscus ConsensusQuiroprácticaParaTodosNo ratings yet
- Art:10.1186/1471 2474 15 188Document8 pagesArt:10.1186/1471 2474 15 188indriNo ratings yet
- Journal of Clinical Orthopaedics and TraumaDocument8 pagesJournal of Clinical Orthopaedics and TraumaandiNo ratings yet
- 2018 Article 211Document4 pages2018 Article 211Cinthya Añazco RomeroNo ratings yet
- Medi 97 E0523Document9 pagesMedi 97 E0523Andrea OsborneNo ratings yet
- Pi Is 0976566220304872Document11 pagesPi Is 0976566220304872rivanNo ratings yet
- Using Risk Models To Improve Patient Selection For High-Risk Vascular SurgeryDocument14 pagesUsing Risk Models To Improve Patient Selection For High-Risk Vascular Surgerylino.delabarreraNo ratings yet
- Moore 2019Document5 pagesMoore 2019Tania salais obregonNo ratings yet
- 2014 Article 3495Document7 pages2014 Article 3495cogajoNo ratings yet
- The Current Relationship Between Surgeon ReimburseDocument4 pagesThe Current Relationship Between Surgeon ReimburseRenan Scalon MachadoNo ratings yet
- Length of Stay Total Knee ArthroplastyDocument9 pagesLength of Stay Total Knee ArthroplastyRista MarginaNo ratings yet
- Dco 5 PDFDocument10 pagesDco 5 PDFGauda GranthanaNo ratings yet
- Comparison of Treatment Outcomes Associated With Early Versus Late Treatment of Mandible Fractures - A Retrospective Chart Review and AnalysisDocument5 pagesComparison of Treatment Outcomes Associated With Early Versus Late Treatment of Mandible Fractures - A Retrospective Chart Review and AnalysisMichaella LimNo ratings yet
- Indications and Interventions of Damage Control Orthopedic SurgeriesDocument12 pagesIndications and Interventions of Damage Control Orthopedic SurgeriesSacha SalasNo ratings yet
- Anaesthetic Considerations in Polytrauma PatientsDocument8 pagesAnaesthetic Considerations in Polytrauma PatientsMileidys LopezNo ratings yet
- Modern and Classic Wound Dressing Comparison in WoDocument6 pagesModern and Classic Wound Dressing Comparison in WoJuan LuckyNo ratings yet
- What Adverse Events and Injuries Are Cited in Anesthesia Malpractice Claims For NonspineDocument11 pagesWhat Adverse Events and Injuries Are Cited in Anesthesia Malpractice Claims For NonspineManolin KinNo ratings yet
- Computer-Assisted Preoperative Planning Improves TDocument12 pagesComputer-Assisted Preoperative Planning Improves TAlishaNo ratings yet
- Comparison of Functional Outcome Between Early and Usual CPM Physiotherapy in Healing Tibia Plateau FractureDocument14 pagesComparison of Functional Outcome Between Early and Usual CPM Physiotherapy in Healing Tibia Plateau FractureAthenaeum Scientific PublishersNo ratings yet
- Critical Care Considerations in Trauma - Overview, Trauma Systems, Initial Assessment PDFDocument19 pagesCritical Care Considerations in Trauma - Overview, Trauma Systems, Initial Assessment PDFPaulina Jiménez JáureguiNo ratings yet
- Three-Dimensional Printed Models Can Reduce Costs and Surgical Time For ComplexDocument11 pagesThree-Dimensional Printed Models Can Reduce Costs and Surgical Time For ComplextaylortNo ratings yet
- DiniDocument10 pagesDiniMuhammad Yasdar BahriNo ratings yet
- Application of Trauma Time Axis Management in The Treatment of Severe Trauma PatientsDocument6 pagesApplication of Trauma Time Axis Management in The Treatment of Severe Trauma PatientsFelix NainggolanNo ratings yet
- Analysis of Risk Factors in Thoracic Trauma Patients With A Comparison of A Modern Trauma Centre: A Mono-Centre StudyDocument10 pagesAnalysis of Risk Factors in Thoracic Trauma Patients With A Comparison of A Modern Trauma Centre: A Mono-Centre StudyWahyu SholekhuddinNo ratings yet
- Bessire 2014Document7 pagesBessire 2014andrei3cucuNo ratings yet
- Comparison of Closed Femur Fracture: Skeletal Traction and Intramedullary Nailing Cost-EffectivenessDocument6 pagesComparison of Closed Femur Fracture: Skeletal Traction and Intramedullary Nailing Cost-EffectivenessS3V4_9154No ratings yet
- WSES Splenic TraumaDocument26 pagesWSES Splenic TraumaAndreas RendraNo ratings yet
- Rodgers Lucio Et Al Risk MGMT HCPolicy 2012 Economics Less Invasive SpineSxDocument10 pagesRodgers Lucio Et Al Risk MGMT HCPolicy 2012 Economics Less Invasive SpineSxAmanda MatthewsNo ratings yet
- Enfermeras y Camas en UciDocument10 pagesEnfermeras y Camas en UciÁlvaro Raúl Conto MorenoNo ratings yet
- Current Concepts in Orthopedic Management of Multiple TraumaDocument8 pagesCurrent Concepts in Orthopedic Management of Multiple TraumanellieauthorNo ratings yet
- International Wound Journal - 2023 - Zhai - Impact of Fast Track Rehabilitation Nursing On Pressure Ulcers andDocument9 pagesInternational Wound Journal - 2023 - Zhai - Impact of Fast Track Rehabilitation Nursing On Pressure Ulcers andMaya LessyNo ratings yet
- Surgical Preferences of Patients at Risk of Hip Fractures: Hemiarthroplasty Versus Total Hip ArthroplastyDocument9 pagesSurgical Preferences of Patients at Risk of Hip Fractures: Hemiarthroplasty Versus Total Hip ArthroplastyCraciun Ana-MariaNo ratings yet
- Trauma Surgery and Acute Care Surgery: Evolution in The Eye of The StormDocument3 pagesTrauma Surgery and Acute Care Surgery: Evolution in The Eye of The StormDeddy WidjajaNo ratings yet
- Critical Biomechanical and Clinical Insights Concerning Tissue Protection When Positioning Patients in The Operating Room: A Scoping ReviewDocument19 pagesCritical Biomechanical and Clinical Insights Concerning Tissue Protection When Positioning Patients in The Operating Room: A Scoping ReviewDiana Pacheco BriceñoNo ratings yet
- Design and Implementation of A Trauma Care BundleDocument7 pagesDesign and Implementation of A Trauma Care BundleNi Nyoman AstriningsihNo ratings yet
- Eichinger2021 Article ChallengesInThePREHOSPITALEmerDocument12 pagesEichinger2021 Article ChallengesInThePREHOSPITALEmerBarry TraceyNo ratings yet
- Anaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative ReviewDocument7 pagesAnaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative Reviewomar gonzalezNo ratings yet
- Diagnostics 12 01289Document15 pagesDiagnostics 12 01289Sushmica BaquiranNo ratings yet
- A Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesDocument11 pagesA Systematic Review and Meta Analysis of Arthroscopic Meniscus Repair in Young Patients: Comparison of All Inside and Inside Out Suture TechniquesJeremyNo ratings yet
- Art 1Document7 pagesArt 1Hajji AhmedNo ratings yet
- To Identify The Spectrum of Post Operative Complications and Appropriate Management in Polytraumatised Patients With Musculoskeletal InjuriesDocument4 pagesTo Identify The Spectrum of Post Operative Complications and Appropriate Management in Polytraumatised Patients With Musculoskeletal InjuriesShaneed KpNo ratings yet
- Systematic Review and Meta-Analysis of Endovascular Therapy Versus Open Surgical Repair For The Traumatic Lower Extremity Arterial InjuryDocument10 pagesSystematic Review and Meta-Analysis of Endovascular Therapy Versus Open Surgical Repair For The Traumatic Lower Extremity Arterial InjuryRamiro Manzano NúñezNo ratings yet
- Swart 2016Document7 pagesSwart 2016TommysNo ratings yet
- 1 s2.0 S0737614618300017 MainDocument22 pages1 s2.0 S0737614618300017 MainJEFFERSON MUÑOZNo ratings yet
- Splenic Trauma WSES Classification and GuidelinesDocument27 pagesSplenic Trauma WSES Classification and GuidelinespgmzNo ratings yet
- ContohDocument9 pagesContohVino DoangNo ratings yet
- Meniscus Root Repair Vs Meniscectomy orDocument8 pagesMeniscus Root Repair Vs Meniscectomy orJulio Cesar Guillen MoralesNo ratings yet
- Burns v7 1 151Document10 pagesBurns v7 1 151Beatriz BeckerNo ratings yet
- Optimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchDocument18 pagesOptimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchEva GarciaNo ratings yet
- 1 s2.0 S002013832030632XDocument6 pages1 s2.0 S002013832030632XKar RodriguezNo ratings yet
- Term PolytraumaDocument13 pagesTerm PolytraumaElmer NarvaezNo ratings yet
- Acetabular Fractures in Older Patients: Assessment and ManagementFrom EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonNo ratings yet
- DevynsresumeDocument2 pagesDevynsresumeapi-272399469No ratings yet
- RPD Daily Incident Report 2/3/21Document7 pagesRPD Daily Incident Report 2/3/21inforumdocsNo ratings yet
- (Limpin, Shakti Dev) Mil Q4W1Document3 pages(Limpin, Shakti Dev) Mil Q4W1Shakti Dev LimpinNo ratings yet
- Test Bank For Biology The Unity and Diversity of Life 14Th Edition by Starr Taggart and Evers Isbn 1305073959 978130507395 Full Chapter PDFDocument36 pagesTest Bank For Biology The Unity and Diversity of Life 14Th Edition by Starr Taggart and Evers Isbn 1305073959 978130507395 Full Chapter PDFjoan.derrick732100% (10)
- 03 Preliminary PagesDocument12 pages03 Preliminary PagesBillie Jan Louie JardinNo ratings yet
- Escovilla 4qmath3aa2 - Patterns in The World I Live inDocument7 pagesEscovilla 4qmath3aa2 - Patterns in The World I Live inapi-743665882No ratings yet
- Ajit ResumeDocument3 pagesAjit ResumeSreeluNo ratings yet
- ENG 10 Q2 Lesson 8 Techniques in Public SpeakingDocument29 pagesENG 10 Q2 Lesson 8 Techniques in Public SpeakingronsairoathenadugayNo ratings yet
- An Overview of Monopolistic CompetitionDocument9 pagesAn Overview of Monopolistic CompetitionsaifNo ratings yet
- Ecofeminism Perspective - A Gendered Approach in Reducing Poverty by Implementing Sustainable Development Practices in IndonesiaDocument20 pagesEcofeminism Perspective - A Gendered Approach in Reducing Poverty by Implementing Sustainable Development Practices in IndonesiaM. NaQviNo ratings yet
- Self Affirmation ScaleDocument19 pagesSelf Affirmation ScaleQonitah Arya SulthanahNo ratings yet
- Literature Review of Water Level SensorDocument4 pagesLiterature Review of Water Level Sensorc5mr3mxf100% (1)
- A. H. M. Jones - Studies in Roman Government and Law-Basil Blackwell (1960)Document260 pagesA. H. M. Jones - Studies in Roman Government and Law-Basil Blackwell (1960)L V100% (1)
- Avinash Mourya TYBMSDocument66 pagesAvinash Mourya TYBMSAbhi KengaleNo ratings yet
- Engr. Frederick B. Garcia: Proposed 3-Storey ResidenceDocument1 pageEngr. Frederick B. Garcia: Proposed 3-Storey Residencesam nacionNo ratings yet
- Conjugarea Verbului Manifesta: Indicativ PrezentDocument4 pagesConjugarea Verbului Manifesta: Indicativ PrezentAndrei PleșaNo ratings yet
- Social Media and Political Communication in India: An Analysis of 2017 Legislative Assembly Elections in Himachal PradeshDocument7 pagesSocial Media and Political Communication in India: An Analysis of 2017 Legislative Assembly Elections in Himachal PradeshEditor IJTSRDNo ratings yet
- Admission Form Eleven Class Mar 2016Document3 pagesAdmission Form Eleven Class Mar 2016Aaqib AliNo ratings yet
- Toym and TofilDocument19 pagesToym and TofilJohn Rey CempronNo ratings yet
- The Emotional Tone Scale - Read "The Hubbard Chart of Human EvaluationDocument1 pageThe Emotional Tone Scale - Read "The Hubbard Chart of Human EvaluationErnesto Salomon Jaldín MendezNo ratings yet
- Schematic Diagram of Relay & Tcms Panel T: REV Revised by Checked by Approved byDocument1 pageSchematic Diagram of Relay & Tcms Panel T: REV Revised by Checked by Approved byTaufiq HidayatNo ratings yet
- Hematology: Mohamad H Qari, MD, FRCPADocument49 pagesHematology: Mohamad H Qari, MD, FRCPASantoz ArieNo ratings yet
- Bago CityDocument8 pagesBago CityTricia Marvi P. NavarroNo ratings yet
- Christian Worldview - PostmodernismDocument6 pagesChristian Worldview - PostmodernismLuke Wilson100% (2)
- 3 Year - V - Sem - FinalDocument208 pages3 Year - V - Sem - FinalKARTHIK ANo ratings yet
- A Project Report-1 - 231020 - 204422Document59 pagesA Project Report-1 - 231020 - 204422Ankit Sharma 028No ratings yet
- Argala: Illustration: Define Primary Argala and Virodha Argala On Lagna For A Standard BirthDocument4 pagesArgala: Illustration: Define Primary Argala and Virodha Argala On Lagna For A Standard Birthsurinder sangarNo ratings yet
- Banners of The Insurgent Army of N. Makhno 1918-1921Document10 pagesBanners of The Insurgent Army of N. Makhno 1918-1921Malcolm ArchibaldNo ratings yet