Professional Documents
Culture Documents
j-neurosurg-pediatr-article-p35
j-neurosurg-pediatr-article-p35
Uploaded by
mikonugrihiCopyright:
Available Formats
You might also like
- Create 24 - 7 - The Blueprint To Build A 6-Figure Twitter BusinessDocument7 pagesCreate 24 - 7 - The Blueprint To Build A 6-Figure Twitter BusinessEmmanuel0% (2)
- Ace Strategy InfoDocument1 pageAce Strategy Infoapi-292206241No ratings yet
- 1 Novacron S OverviewDocument3 pages1 Novacron S OverviewsaskoNo ratings yet
- THINK L4 Unit 6 Grammar BasicDocument2 pagesTHINK L4 Unit 6 Grammar Basicniyazi polatNo ratings yet
- Compression of The Fourth Ventricle Using A Craniosacral Osteopathic ...Document9 pagesCompression of The Fourth Ventricle Using A Craniosacral Osteopathic ...AlexNo ratings yet
- The Cartography of Crete in The 17thDocument28 pagesThe Cartography of Crete in The 17thΕυτύχης ΤζιρτζιλάκηςNo ratings yet
- Art. 1474 - PRICEDocument4 pagesArt. 1474 - PRICEjamaica_maglinteNo ratings yet
- 2014 7 Peds14324Document5 pages2014 7 Peds14324dewiNo ratings yet
- Pediatric Hydrocephalus: Systematic Literature Review and Evidence-Based Guidelines. Part 1: Introduction and MethodologyDocument5 pagesPediatric Hydrocephalus: Systematic Literature Review and Evidence-Based Guidelines. Part 1: Introduction and MethodologyagusNo ratings yet
- HydrocephalusDocument9 pagesHydrocephalusDeby AnditaNo ratings yet
- Intraoperative Evaluation of Urinary Tract Injuries at The Time of Pelvic Surgery A Systematic ReviewDocument9 pagesIntraoperative Evaluation of Urinary Tract Injuries at The Time of Pelvic Surgery A Systematic ReviewdlmejiapNo ratings yet
- Dural RepairDocument8 pagesDural RepairNolan James BrownNo ratings yet
- Van Midden Dorp 2013Document14 pagesVan Midden Dorp 2013Raveli KalvinNo ratings yet
- Treatment of Idiopathic A Chal Asia in The Ped PopulationDocument7 pagesTreatment of Idiopathic A Chal Asia in The Ped Populationcesar sanchez sanchezNo ratings yet
- BR J Sports Med-2008-Hegedus-80-92 PDFDocument14 pagesBR J Sports Med-2008-Hegedus-80-92 PDFAnonymous Jx2UvBeteNo ratings yet
- Can Neonatal Pull-Through Replace Staged Pull-ThrDocument26 pagesCan Neonatal Pull-Through Replace Staged Pull-Thrrahulrooney49No ratings yet
- Sedation Guidelines, Protocols, and Algorithms In.13Document8 pagesSedation Guidelines, Protocols, and Algorithms In.13Juan Pedro Alconada MaglianoNo ratings yet
- A Study To Assess The Effectiveness of Structured Teaching Programme On Knowledge Regarding Kidney Transplantation Among ESRD Patients at Selected Hospitals at Mandya (Dist.)Document8 pagesA Study To Assess The Effectiveness of Structured Teaching Programme On Knowledge Regarding Kidney Transplantation Among ESRD Patients at Selected Hospitals at Mandya (Dist.)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Article 2Document14 pagesArticle 2fatmazahrabahrounNo ratings yet
- Reflection PaperDocument8 pagesReflection Paperapi-240352465No ratings yet
- Neonatal Heart Rate Variability - A Contemporary Scoping Review of Analysis Methods and Clinical ApplicationsDocument23 pagesNeonatal Heart Rate Variability - A Contemporary Scoping Review of Analysis Methods and Clinical ApplicationsLucas SalgadoNo ratings yet
- Jurnal 2Document9 pagesJurnal 2Syanindita MaharaniNo ratings yet
- ICCS Standardization Report On Urodynamic StudiesDocument8 pagesICCS Standardization Report On Urodynamic StudiesAndy WijayaNo ratings yet
- SR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryDocument10 pagesSR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryPaul MarjiNo ratings yet
- Ultrasound Imaging Reduces Failure Rates of Percutaneous Central Venous Catheterization in ChildrenDocument8 pagesUltrasound Imaging Reduces Failure Rates of Percutaneous Central Venous Catheterization in Childrenangelama1783riosNo ratings yet
- Incidencia de La Reabsorcion Espontanea de HNPDocument8 pagesIncidencia de La Reabsorcion Espontanea de HNPNicolas ParejaNo ratings yet
- Suresh 2015Document6 pagesSuresh 2015ade_liaNo ratings yet
- 10 1016@j Ctim 2012 07 009Document10 pages10 1016@j Ctim 2012 07 009Alexandra GeomaraNo ratings yet
- BR J Sports Med-2008-Hegedus-80-92Document14 pagesBR J Sports Med-2008-Hegedus-80-92api-263772125No ratings yet
- 10 1111@ans 15125Document7 pages10 1111@ans 15125Sahily MoralesNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- ERAS HigadoDocument24 pagesERAS HigadoGeraldNo ratings yet
- Epilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-AnalysisDocument9 pagesEpilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-Analysisbaba ababNo ratings yet
- 2013 RC THB 2160.fullDocument27 pages2013 RC THB 2160.fullNoelia CalderónNo ratings yet
- Group Lit Rev PaperDocument15 pagesGroup Lit Rev PaperChelsea RuthrauffNo ratings yet
- [19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedDocument7 pages[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedBruno MañonNo ratings yet
- Epidural Space Identification A Meta Analysis Of.45Document10 pagesEpidural Space Identification A Meta Analysis Of.45Palliative MedicineNo ratings yet
- Effectiveness ESWT in Lower Limb Tendinopathy Syst. Rev. Mani-Babu 2014Document10 pagesEffectiveness ESWT in Lower Limb Tendinopathy Syst. Rev. Mani-Babu 2014Javier MartinNo ratings yet
- PROCESSDocument11 pagesPROCESSandrea vargasNo ratings yet
- 2017 Paravertebral Block en Pediatrics BJADocument8 pages2017 Paravertebral Block en Pediatrics BJAAlejandra SanchezNo ratings yet
- HHS Public Access: Developing A New Definition and Assessing New Clinical Criteria For Septic ShockDocument28 pagesHHS Public Access: Developing A New Definition and Assessing New Clinical Criteria For Septic ShockDulCee Cano SanzNo ratings yet
- Management of The Undescended Testis in ChildrenDocument16 pagesManagement of The Undescended Testis in ChildrenRashmeeta ThadhaniNo ratings yet
- Loop Vs DividedDocument8 pagesLoop Vs DividedNatalindah Jokiem Woecandra T. D.No ratings yet
- Kohn 2013Document20 pagesKohn 2013Georgiana BuneaNo ratings yet
- Wrist Ganglion Treatment - 2015 (Tema 4)Document16 pagesWrist Ganglion Treatment - 2015 (Tema 4)Carlos NoronaNo ratings yet
- Educationandadministration: Development of A Validated Exam To Assess Physician Transfusion Medicine KnowledgeDocument6 pagesEducationandadministration: Development of A Validated Exam To Assess Physician Transfusion Medicine KnowledgeFOURAT OUERGHEMMI100% (1)
- A Nonrigorous and Incorrect Evaluation Of  TheDocument2 pagesA Nonrigorous and Incorrect Evaluation Of  Thelincolnbasilio1No ratings yet
- Heart & Lung: Care of Critically Ill AdultsDocument13 pagesHeart & Lung: Care of Critically Ill AdultsRabiyatul AwaliyahNo ratings yet
- Withholding Feeds and Transfusion-Associated Necrotizing Enterocolitis in Preterm Infants: A Systematic ReviewDocument6 pagesWithholding Feeds and Transfusion-Associated Necrotizing Enterocolitis in Preterm Infants: A Systematic ReviewrezkyfikriNo ratings yet
- AlqahtaniDocument8 pagesAlqahtaniGanda SilitongaNo ratings yet
- Meta 2 - Sofi AA - 2018Document9 pagesMeta 2 - Sofi AA - 2018matheus.verasNo ratings yet
- Children 10 01862Document11 pagesChildren 10 01862Sinan Adnan Al-AbayechiNo ratings yet
- Appendix 21Document18 pagesAppendix 21Nailatul Hifdziyati CuhibnahNo ratings yet
- 1678-4227-anp-80-01-084Document13 pages1678-4227-anp-80-01-084anaclarapuzzellaNo ratings yet
- Lumbar PIDDocument6 pagesLumbar PIDdesai_erNo ratings yet
- Effect of Desflurane Versus Sevoflurane in Pediatric Anesthesia: A Meta-AnalysisDocument8 pagesEffect of Desflurane Versus Sevoflurane in Pediatric Anesthesia: A Meta-AnalysisdennyramdhanNo ratings yet
- Cefalea PospuncionDocument31 pagesCefalea Pospuncionmanolo.mendozavNo ratings yet
- Integrative Review 1Document17 pagesIntegrative Review 1api-442558242No ratings yet
- Academic Emergency Medicine - 2022 - Jessen - Restrictive Fluids Versus Standard Care in Adults With Sepsis in TheDocument32 pagesAcademic Emergency Medicine - 2022 - Jessen - Restrictive Fluids Versus Standard Care in Adults With Sepsis in TheLenin BlancasNo ratings yet
- E014478 FullDocument6 pagesE014478 FullГанбат М.No ratings yet
- Performing The Embryo Transfer - A GuidelineDocument15 pagesPerforming The Embryo Transfer - A GuidelineАнатолий КомогорцевNo ratings yet
- 1-s2.0-S0104001421000609-mainDocument9 pages1-s2.0-S0104001421000609-mainsyukronchalimNo ratings yet
- Surgery For Degenerative Lumbar Spondylosis: Updated Cochrane ReviewDocument9 pagesSurgery For Degenerative Lumbar Spondylosis: Updated Cochrane Reviewchartreuse avonleaNo ratings yet
- Research ArticleDocument10 pagesResearch Articlerazaqhussain00No ratings yet
- Cuff-Leak Test For Predicting Postextubation Airway Complications: A Systematic ReviewDocument13 pagesCuff-Leak Test For Predicting Postextubation Airway Complications: A Systematic ReviewMau MillanNo ratings yet
- Evidence-Based LaryngologyFrom EverandEvidence-Based LaryngologyDavid E. RosowNo ratings yet
- Tide Times and Tide Chart For Dammam PDFDocument8 pagesTide Times and Tide Chart For Dammam PDFAnonymous g5nMjONo ratings yet
- Land Titles and DeedsDocument1 pageLand Titles and DeedsIanLightPajaroNo ratings yet
- Prince Ganai NuclearDocument30 pagesPrince Ganai Nuclearprince_ganaiNo ratings yet
- Buy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlineDocument5 pagesBuy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlinelorendesuzaNo ratings yet
- The Titans Curse - Robert VendittiDocument134 pagesThe Titans Curse - Robert VendittimarianaqueirosluzNo ratings yet
- Portfolio Output No. 17: Reflections On Personal RelationshipsDocument3 pagesPortfolio Output No. 17: Reflections On Personal RelationshipsKatrina De VeraNo ratings yet
- Routing CodesDocument4 pagesRouting CodesScribdTranslationsNo ratings yet
- Adetunji CVDocument5 pagesAdetunji CVAdetunji AdegbiteNo ratings yet
- Testable Concepts in MCQDocument188 pagesTestable Concepts in MCQrami100% (1)
- Lesson A Worksheets. Print or Copy in Your Notebook-1Document3 pagesLesson A Worksheets. Print or Copy in Your Notebook-1Martha Lucia Arcila HenaoNo ratings yet
- Manual Therapy in The Treatment of Facial WrinklesDocument4 pagesManual Therapy in The Treatment of Facial WrinklesKarolina MirosNo ratings yet
- Perlengkapan Bayi Ellena and FamilyDocument9 pagesPerlengkapan Bayi Ellena and FamilyintanchairranyNo ratings yet
- Pre-Feasibility of Tunnel Farming in BahawalpurDocument10 pagesPre-Feasibility of Tunnel Farming in Bahawalpurshahidameen2100% (1)
- Architecture in EthDocument4 pagesArchitecture in Ethmelakumikias2No ratings yet
- Herbert Morrison BooklistDocument2 pagesHerbert Morrison BooklistGillian HallNo ratings yet
- Examen Blanc Et Corrige 3ASLLE Anglais 2e Sujet 2017Document4 pagesExamen Blanc Et Corrige 3ASLLE Anglais 2e Sujet 2017dila sailNo ratings yet
- HP Scanjet Pro 2500 F1 Flatbed Scanner: DatasheetDocument2 pagesHP Scanjet Pro 2500 F1 Flatbed Scanner: DatasheetKarkittykatNo ratings yet
- What A Body Can DoDocument26 pagesWhat A Body Can DoMariana Romero Bello100% (1)
- Bio-Valley Day Spa (Final Proposal To Submit) MDocument85 pagesBio-Valley Day Spa (Final Proposal To Submit) MAtiqah Hasan100% (4)
- Solid Edge Mold ToolingDocument3 pagesSolid Edge Mold ToolingVetrivendhan SathiyamoorthyNo ratings yet
- Hispanic Tradition in Philippine ArtsDocument14 pagesHispanic Tradition in Philippine ArtsRoger Pascual Cuaresma100% (1)
- Nemesis - TipsDocument2 pagesNemesis - TipsZoran StrajinNo ratings yet
- Form PDF 870914450231220Document8 pagesForm PDF 870914450231220Sachin KumarNo ratings yet
- Distress Tolerance Handout 5 - Pros and Cons PDFDocument1 pageDistress Tolerance Handout 5 - Pros and Cons PDFRobinNo ratings yet
j-neurosurg-pediatr-article-p35
j-neurosurg-pediatr-article-p35
Uploaded by
mikonugrihiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
j-neurosurg-pediatr-article-p35
j-neurosurg-pediatr-article-p35
Uploaded by
mikonugrihiCopyright:
Available Formats
J Neurosurg Pediatrics (Suppl) 14:35–43, 2014
©AANS, 2014
Pediatric hydrocephalus: systematic literature review and
evidence-based guidelines. Part 5: Effect of valve type on
cerebrospinal fluid shunt efficacy
Lissa C. Baird, M.D.,1 Catherine A. Mazzola, M.D., 2 Kurtis I. Auguste, M.D., 3
Paul Klimo Jr., M.D., M.P.H., 4–6 and Ann Marie Flannery, M.D.7
1
Department of Neurological Surgery, Oregon Health & Science University, Portland, Oregon; 2Division
of Pediatric Neurological Surgery, Goryeb Children’s Hospital, Morristown, New Jersey; 3Department of
Neurosurgery, University of California, San Francisco, California; 4Semmes-Murphey Neurologic & Spine
Institute; 5Department of Neurosurgery, University of Tennessee Health Science Center; and 6Le Bonheur
Children’s Hospital, Memphis, Tennessee; and 7Department of Neurological Surgery, Saint Louis University,
St. Louis, Missouri
Object. The objective of this systematic review was to examine the existing literature to compare differing shunt
components used to treat hydrocephalus in children, find whether there is a superior shunt design for the treatment
of pediatric hydrocephalus, and make evidence-based recommendations for the selection of shunt implants when
placing shunts.
Methods. Both the US National Library of Medicine PubMed/MEDLINE database and the Cochrane Database
of Systematic Reviews were queried using MeSH headings and key words chosen to identify publications comparing
the use of shunt implant components. Abstracts of these publications were reviewed, after which studies meeting the
inclusion criteria were selected. An evidentiary table was compiled summarizing the selected articles and quality of
evidence. These data were then analyzed by the Pediatric Hydrocephalus Systematic Review and Evidence-Based
Guidelines Task Force to consider evidence-based treatment recommendations.
Results. Two hundred sixty-nine articles were identified using the search parameters, and 43 articles were re-
called for full-text review. Of these, 22 papers met the study criteria for a comparison of shunt components and were
included in the evidentiary table. The included studies consisted of 1 Class I study, 11 Class II studies, and 10 Class
III studies. The remaining 21 articles were excluded.
Conclusions. An analysis of the evidence did not demonstrate a clear advantage for any specific shunt compo-
nent, mechanism, or valve design over another.
Recommendation: There is insufficient evidence to demonstrate an advantage for one shunt hardware design
over another in the treatment of pediatric hydrocephalus. Current designs described in the evidentiary tables are all
treatment options. Strength of Recommendation: Level I, high degree of clinical certainty.
Recommendation: There is insufficient evidence to recommend the use of a programmable valve versus a
nonprogrammable valve. Programmable and nonprogrammable valves are both options for the treatment of pediatric
hydrocephalus. Strength of Recommendation: Level II, moderate degree of clinical certainty.
(http://thejns.org/doi/abs/10.3171/2014.7.PEDS14325)
Key Words • hydrocephalus • cerebrospinal fluid shunt • practice guidelines •
programmable valve • antisiphon device
H
ydrocephalus is the most common condition ically. Simple differential pressure valves were initially
treated by pediatric neurosurgeons. Successful engineered followed by a second generation of valves
management with cerebrospinal fluid shunt sys- that included autoregulating, adjustable, antisiphon, and
tems began after Nulsen and Spitz placed the first im- gravitational components.
plantable shunt in 1949, using a stainless steel ball-valve The objective of this systematic review is to exam-
system.34 Over the next 2 decades, shunt systems evolved ine literature in which differing shunt components used
to include distal slit valves, proximal slit valves, and dia- to treat hydrocephalus in children are compared to find
phragm valves. The subsequent development of artificial whether there is a superior shunt design for the treatment
valves and silicone tubing advanced shunt design dramat- of pediatric hydrocephalus and to make evidence-based
recommendations regarding the selection of shunt im-
Abbreviations used in this paper: AANS = American Association plants when placing shunts. Currently, many shunt system
of Neurological Surgeons; CNS = Congress of Neurological components are available to the pediatric neurosurgeon,
Surgeons. and they function with a variety of pressure, flow, and
J Neurosurg: Pediatrics / Volume 14 / November 2014 35
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
L. C. Baird et al.
siphon control characteristics. Shunt system design has were recalled for full-text review. Predetermined inclu-
evolved along with attempts to minimize failure rates. sion and exclusion criteria were used to review each of
The initial use of simple differential pressure valves led these articles in detail. Twenty-two articles were included
to concerns about the disadvantages of siphoning and as- in the final evidentiary table. Reasons for exclusion of full-
sociated shunt obstruction, subdural hematoma, slit ven- text articles included the absence of a valid comparison
tricle syndrome, overdrainage, and craniosynostosis. In group (n = 14),1–3,7–10,12,13,20,25,26,28,35 the absence of a valid
an attempt to minimize these complications, antisiphon outcome variable (n = 4),14,18,22,32 invalid study design (n =
devices have been developed and integrated into shunt 2),30,31 and redundant patient population (n = 1) (Fig. 1). 5
systems as intrinsic to the valve mechanism or as sepa- For each article included in the evidentiary table, the
rate devices. The antisiphon device is designed to provide study type, summary findings, and major conclusions
progressive resistance to flow to counteract the siphoning were recorded, and a preliminary data class was assigned.
that occurs when negative pressure is exerted with verti- The Pediatric Hydrocephalus Systematic Review and Ev-
cal positioning. The later development of programmable idence-Based Guidelines Task Force met to discuss the
valves allowed for purposeful alterations in valve func- ranking of the evidence and the classification of data.
tion to be made without a surgical procedure. Recommendations were then made based on the strength
The purpose of this evidence-based review is to criti- of the data in the evidentiary table (Table 1). In these dis-
cally evaluate available data on the efficacy of comparable cussions, if disagreement was encountered among Task
shunt components to determine if one shunt component Force members, a blinded vote was held and a consensus
is superior to another. Additionally, we created evidence- or majority opinion was reached.
based recommendations on the selection of shunt com-
ponents based on the strength of the available data. Most
of the available evidence focuses on the comparison of Results
shunt valve designs. Study outcome variables accepted for The review process identified 1 Class I study, 11
the purposes of this review included shunt survival, shunt Class II studies, and 10 Class III studies.
complications, development of slit ventricle syndrome, Only one included article was rated as a Class I study,
and development of signs or symptoms of overdrainage. Kestle et al. (2000),19 in which the investigators performed
a randomized controlled trial comparing 3 kinds of
Methods valves: all types of standard differential pressure valves,
a Delta valve (Medtronic) with an antisiphon mechanism,
Search Criteria and an Orbis-Sigma valve (Cordis) with a variable-resis-
The US National Library of Medicine (PubMed/ tance and flow-limiting mechanism. Three hundred forty-
MEDLINE) and the Cochrane Database of System- four patients were randomly assigned to a valve type and
atic Reviews were queried for the period January 1966 followed up until the time of first shunt failure. Assessed
through March 2012 using MeSH headings and key words outcome variables included shunt obstruction, overdrain-
relevant to shunt system components as detailed below. age, ventricular loculations, and infection. The investiga-
tors did not find a significant difference in shunt survival
Search Terms between the 3 valve types in either the short-term (Drake
19985) or extended19 follow-up.
PubMed/MEDLINE Eleven Class II studies4,11,15,21,23,24,27,33,36,41,44 in which
1. (“Cerebrospinal Fluid Shunts”[MeSH]) “Hydro differing valve types were compared also failed to dem-
cephalus”[MeSH:noexp] onstrate a superior valve when shunt survival was as-
2. 1 AND (programmable OR nonprogrammable OR sessed. Jain et al.15 (2000) conducted a prospective cohort
non-programmable OR siphon OR antisiphon* OR anti- study in which they compared shunts using a standard
siphon* OR (“differential pressure” OR “fixed pressure”) differential pressure valve with a Delta (Medtronic) flow-
OR valve*) regulating valve. The authors found no significant differ-
3. Limit 2 to Child (0–18 years) ence in overall shunt survival (p = 0.72), with a 5-year
4. Limit to English and Humans survival rate of 58.6% for the differential pressure valves
and 58.7% for the Delta valves. The authors did note a
Cochrane Database relative difference between the 2 groups in the incidence
1. MeSH descriptor Child of overdrainage and infection. The differential pressure
2. MeSH descriptor Infant valve was associated with 4 cases of post-shunt subdural
3. 1 or 2 and (MeSH descriptor Cerebrospinal Fluid effusion or slit ventricle syndrome, while the Delta valve
Shunts) was associated with only 1 case of subdural effusion. The
4. 3 and (MeSH descriptor Hydrocephalus) Delta valve group had 3 infections, whereas the differen-
5. (programmable OR nonprogrammable) tial pressure valve group had no infections. Warf et al.44
6. 4 and 5 (2005) conducted a prospective randomized trial in which
they compared the Codman-Hakim microprecision valve
Search Results with the more affordable Chhabra valve. Ninety children
The search yielded 269 abstracts, which were then were evaluated after randomization for shunt malfunc-
reviewed for relevance to the demonstration of superiority tion, shunt migration, and wound complication. No sig-
of 1 shunt component over another. Forty-three articles nificant differences in outcome variables were demon-
36 J Neurosurg: Pediatrics / Volume 14 / November 2014
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
Part 5: Effect of valve type on CSF shunt efficacy
Fig. 1. Flowchart showing the process involved in identifying relevant literature.
strated between the 2 groups. Smely and Van Velthoven group (6.25%) than in the flow-controlled valve group
(1997) conducted a retrospective cohort review in which (9%); however this finding did not reach statistical sig-
they compared 66 infants who underwent placement of nificance (p > 0.99). The incidence of shunt revision was
a ventriculoperitoneal Cordis Orbis-Sigma valve system also lower in the Delta group (0.12 revisions/patient/year)
with 53 patients who underwent placement of a ventricu- than in the flow-controlled valve group (0.19 revisions/
loatrial Codman Holter Valve shunt system.41 Forty-eight patient/year), a finding that also failed to reach statistical
percent of patients with the Orbis-Sigma valve required significance (p = 0.75). Khan et al.21 (2010) studied the
one or more revisions while 98.1% of patients with the role of the antisiphon mechanism in a randomized con-
Holter Valve required 1 or more revisions (p < 0.001). trolled trial. Forty patients undergoing shunt placement
The difference in distal placement of the shunt system were randomized to receive a differential pressure valve
is a confounding factor when comparing valve types in with an antisiphon device (Vygon shunt) or a differential
this study. valve without an antisiphon device (Chhabra or Ceredrain
shunts). Shunt blockage, shunt infection, overdrainage,
Antisiphon Mechanism loculated ventricles, and occipitofrontal circumference
Three Class II studies evaluating the antisiphon were assessed in the 2 groups. No end point variables
mechanism were included in our review. Liniger et al.23 demonstrated a statistically significant difference. Over-
(2003) studied 27 infants in a prospective cohort study drainage complications occurred in 10% of the patients
in which a PS Medical medium pressure, flow-controlled in the group without an antisiphon device as opposed to
valve was compared with a PS Medical 1.0 Delta valve 0% in the group with an antisiphon device (p = 0.48). A
with an antisiphon mechanism. The authors found a low- slightly higher infection and obstruction rate was noted
er incidence of slit ventricle syndrome in the Delta valve in the antisiphon group. In a retrospective cohort study of
J Neurosurg: Pediatrics / Volume 14 / November 2014 37
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
38
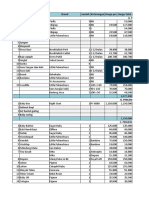
TABLE 1: Valve type: summary of evidence*
Authors & Year Study Description Data Class, Quality, & Reasons Results & Conclusions
Kestle et al., Multicenter randomized trial comparing differential pressure Class I No clear advantage of 1 valve over another.
2000 valve, Delta valve, & an Orbis-Sigma valve. Randomized controlled trial.
344 pts w/ time to shunt failure as end point.
Khan et al., Role of ASD. Class II No overdrainage in ASD group, 2 pts w/ overdrainage in non-
2010 40 pts randomly assigned to shunt w/ ASD or differential valve. Prospective, randomized comparative trial. antisiphon group; higher occlusion & infection in ASD group.
Small study w/ short follow-up (<6 mos). No end point variables reached statistical significance.
Jain et al., 2000 Prospective data from 50 consecutive 1st-time shunt insertions. Class II No significant difference in shunt survival between 2 groups: 5-yr
Comparison of shunt survival between differential pressure & Prospective cohort study. survival = 58.6% in DPV group & 58.7% in Delta valve group.
flow-regulating (Delta) valves. Higher incidence of overdrainage in DPV group & higher rate of
infection in Delta valve group, although neither was statisti-
cally significant.
Liniger et al., 27 infants w/ flow-control vs antisiphon valves followed for Class II No significant difference in development of slit ventricles or slit
2003 development of slit ventricles & slit ventricle syndrome. Prospective cohort study. ventricle syndrome between 2 groups. Slit ventricle syndrome
developed in 6.25% of pts in the antisiphon group & 9% of pts
in the flow-controlled valve group (p > 0.99).
Pollack et al., 377 pts randomized to receive the Codman Hakim program- Class II Comparable efficacy & safety w/ no statistically significant differ-
1999 mable shunt vs a conventional valve of surgeon’s choice & Multicenter randomized controlled trial. ence in shunt survival.
followed for valve explant & shunt failure. Control group not uniform in valve type.
Davis et al., Retrospective cohort study of 475 pts who underwent VP Class II No significant difference in shunt survival at 2-yr follow-up:
2000 shunt placement w/ Delta valve w/ antisiphon function or 2 Single-institution retrospective cohort 65% in Delta group, 66% in Holter-Hasner group, & 64% in
differential pressure valves w/o antisiphon function (Holter- study. Heyer-Schulte valve group. No significant difference in rate of
Hausner & Heyer-Schulte). End points included shunt survival subdural fluid collection between groups.
& symptomatic subdural fluid collections.
Hatlen et al., Retrospective review of 523 pts who underwent 616 shunt Class II 5-yr survival for nonprogrammable valves (45.8%) was signifi-
2012 surgeries w/ 2-yr min follow-up. Pts w/ programmable valve Retrospective cohort study. Data obtained cantly higher than that for programmable valves (19.8%), p =
placement (Strata & Codman Hakim valves) compared w/ from prospectively collected shunt 0.0001.
nonprogrammable valves (Heyer-Schulte, Spetzer, Delta, & database.
Medtronic).
Valve survival was primary end point.
McGirt et al., 279 pts who underwent shunt placement procedures w/ either a Class II Programmable valves associated w/ reduced risk of both overall
2007 programmable (Strata or Codman Hakim) or a nonprogram- Retrospective cohort review. shunt revision (35% vs 54%, p = 0.016) & proximal obstruction
mable valve (PS Medical Delta) were retrospectively as- (12% vs 28%, p = 0.006).
sessed & their cases analyzed for time to shunt malfunction
& type of malfunction.
Notarianni et 253 pts who underwent shunting procedures w/ either a Class II Failure rates (p = 0.11) were not significantly different btwn
al., 2009 programmable (Medtronic Strata or Codman Hakim) or a Retrospective review. shunts w/ programmable valve (76.1%), shunts w/ nonpro-
nonprogrammable (pressure-controlled or not specified) grammable valve (80.0%), & shunts w/ nonspecified valve
valve were retrospectively assessed & their cases analyzed (65.0%).
for time to shunt malfunction.
(continued)
J Neurosurg: Pediatrics / Volume 14 / November 2014
L. C. Baird et al.
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
TABLE 1: Valve type: summary of evidence* (continued)
Authors & Year Study Description Data Class, Quality, & Reasons Results & Conclusions
Warf, 2005 90 pts randomized to receive the Chhabra or Codman Hakim Class II No difference btwn 2 groups in incidence of shunt malfunction,
shunt as primary treatment for hydrocephalus & 105 pts Prospective, randomized study. shunt migration, wound complication, or death.
treated w/ Chhabra shunt after unsuccessful ETV. This study was downgraded from a Class
I to a Class II study due to nonblinded
outcome assessors.
Mangano et al., 189 children who underwent shunt placement w/ either a Class II Programmable valves had higher rate of malfunction (11.1%
2005 programmable valve (Strata or Codman-Medos w/ ASD) or Retrospective cohort review, short follow- compared to 0%), but the difference did not reach statistical
a nonprogrammable valve (PS Medical) were retrospectively up (mean 9 mos). significance.
assessed & their cases analyzed for time to shunt malfunc-
tion & CSF protein levels.
Smely & Van Retrospective review of 66 infants treated w/ Cordis Orbis-Sig- Class II Codman Holter Valve group demonstrated a greater than double
Velthoven, ma Valve compared to 53 children treated w/ Codman Holter Retrospective cohort review. risk of shunt complications in comparison to the ventricu-
1997 Valve ventriculoatrial system. loperitoneal Orbis-Sigma valve system. 48.5% of pts w/
Orbis-Sigma valve required 1 or more revisions; 98.1% of pts
w/ Holter Valve required 1 or more revisions (p < 0.001).
Gruber et al., Retrospective review of 41 pts in whom there was primary or Class III Fewer shunt malfunctions after ASD placement. Complication
J Neurosurg: Pediatrics / Volume 14 / November 2014
1984 secondary placement of an ASD to their shunt system. Retrospective case series. rate per pt was 4 times less frequent & the annual ventricular
Comparison of clinical course before & after placement of ASD. catheter obstruction rate per pt improved 12 times. No statisti-
cal analysis to determine significance.
Part 5: Effect of valve type on CSF shunt efficacy
Kan et al., 2007 244 children who underwent shunt placement w/ either a dif- Class III 23 pts developed slitlike ventricles: 10.8% of pts w/ differential
ferential pressure valve, Delta valve, or Orbis-Sigma valve Retrospective review. pressure valves, 10.5% of pts w/ Delta valves, & 3.6% of pts
& had 1-yr follow-up data were assessed for development of w/ Orbis-Sigma valves, p = 0.007.
slitlike ventricles. Children w/ differential pressure or Delta valves were 1.67 times
more likely to develop slitlike ventricles than those w/ Orbis-
Sigma valves.
Miranda et al., Retrospective review of shunt survival in 103 pts treated for Class III 42 episodes of obstruction. Fixed medium pressure valves were
2011 preterm-related posthemorrhagic hydrocephalus. Retrospective review. associated w/ a higher rate of obstruction than low pressure
valves; only statistically significant in those pts weighing >
2000 g, p = 0.040.
Ramadwar et 28 pts underwent retrospective comparison of the efficacy of the Class III 69% of pts w/ Delta valve & 53% of pts w/ Multi-Purpose valve
al., 1997 Delta valve vs the Heyer-Shulte Multi-Purpose valve. Retrospective review. Small sample. required revision. Did not reach statistical significance.
Robinson et al., 158 pts whose cases were retrospectively analyzed for signifi- Class III Revision rate per yr was 4 times higher for pts w/ no valve or low
2002 cant factors associated w/ shunt malfunction. Retrospective case series. pressure valve (72% 5-yr failure rate) than for pts w/ medium
or high pressure valve (47% 5-yr failure rate), p = 0.0005.
Sainte-Rose et Retrospective review of the mechanical complications leading to Class III A higher risk of proximal occlusion is associated w/ flanged
al., 1991– shunt malfunction in 1719 pts w/ shunted hydrocephalus. Pts Retrospective case series. ventricular catheters (p < 0.04); shunts w/ proximal medium
1992 were treated w/ distal slit valves or medium pressure proximal pressure valves are less likely to malfunction than shunts w/
valves. distal slit valves (p < 0.000002); open-ended distal catheters
associated w/ fewer distal obstructions (p < 0.0003).
(continued)
39
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
L. C. Baird et al.
475 patients, Davis et al.4 (2000) assessed shunt survival
No significant differences in efficacy. Tendency toward increased
No evidence of an association between shunt malfunction & type
and the development of subdural collection in patients
increased rate of slit ventricles in pts w/ Cordis Hakim valve.
No difference in number of revisions. Fewer proximal revisions
in Delta Valve group. No determination of significance from
treated with a Delta valve shunt with antisiphon function
valve & Delta w/ ASD groups in number of revisions, infec-
No significant differences were found between the distal slit
The higher patency rate of the Pudenz-Heyer valve was
and in patients treated with one of 2 differential pressure
rate of catheter rupture in pts w/ Pudenz-Heyer valve &
valves without antisiphon control. In a comparison of the
3 groups, no significant difference was found.
The Class III studies that assessed the antisiphon
mechanism include a retrospective review by Gruber et
Results & Conclusions
al.6 (1984), in which the authors evaluated 41 patients be-
fore and after primary or secondary placement of an an-
statistically significant (p < 0.001).
tisiphon device. In the secondary placement group fewer
complications and proximal catheter obstructions were
noted after placement of such a device. However, no sta-
tions, or overdrainage.
tistical analysis was provided by the authors to demon-
strate the significance of their findings. In a retrospective
of shunt hardware.
cohort review of 101 patients who underwent shunt place-
described data.
ment, Virella et al.43 (2002) reported no significant dif-
ferences between patients who underwent placement of a
* ASD = antisiphon device; DPV = differential pressure valve; ETV = endoscopic third ventriculostomy; pt = patient; VP = ventriculoperitoneal.
distal slit valve and patients who underwent placement of
a Delta valve with an antisiphon component. The authors
assessed the number of revisions, infections, and evidence
of overdrainage, and reported that 31% of patients in the
distal slit valve group required a single shunt revision and
Poor description of study design & data.
8% required a second revision, whereas 30% of patients
Data Class, Quality, & Reasons
Prospective cohort study, post hoc
in the Delta valve group required a single revision and
20% required a second. Kaiser et al.16 (1997) reported a
prospective but incompletely described comparison study
Retrospective case series.
Prospective randomized.
between a conventional medium pressure valve and the
Retrospective review.
Delta valve. The authors found no difference in the num-
ber of shunt revisions.
analysis.
Slit Ventricles
Class III
Class III
Class III
Class III
Kan et al.17 (2007) conducted a retrospective review
of 244 patients with at least 1 year of follow-up after pri-
mary shunt placement with a differential pressure valve,
Retrospective review of 101 pts who underwent shunt placement
a Delta valve, or an Orbis-Sigma valve. Variables associ-
Data prospectively collected on 839 pts who underwent primary
treated w/ shunt placement procedures w/ either the Pudenz-
w/ a distal slit valve or a Delta level 1 valve w/ an antisiphon
Valve types included flow regulated & differential pressure.
ated with the development of slitlike ventricles included
Prospective study comparing conventional medium valve w/
shunt insertion. 1183 episodes of shunt failure occurred.
Retrospective review of consecutive series of 148 children
patient age (younger age at insertion was associated with
Delta level 1 valve in 25 infants younger than 6 mos.
a higher incidence of slitlike ventricles; p = 0.09), etiology
(trauma, infection, and aqueductal stenosis were associ-
ated with a higher incidence of slitlike ventricles), and
valve type (10.8% of patients with differential pressure
Heyer valve or the Cordis Hakim valve.
Study Description
valves, 10.5% with Delta valves, and 3.6% with Orbis-
TABLE 1: Valve type: summary of evidence* (continued)
Sigma valves developed slitlike ventricles; p = 0.007).
This article suggests that a slower reduction in ventricle
size and slower flow may lead to larger ventricles after
shunt placement. Slit ventricle syndrome was not directly
assessed; rather, the radiographic appearance of slitlike
ventricles was used as a surrogate outcome.
Programmable Valves
component.
Five Class II studies11,24,27,33,36 evaluated programma-
ble valves. Pollack et al.36 (1999) conducted a multicenter
randomized controlled trial in which they compared the
programmable Codman Hakim valve to the surgeon’s
choice of any conventional valve. The authors demon-
Tuli et al., 2000
Authors & Year
Kaiser et al.,
strated comparable efficacy and safety with no statisti-
Virella et al.,
Serlo et al.,
cally significant difference in shunt survival between the
2002
1986
1997
experimental and control groups.
Hatlen et al. (2012) published an analysis of program-
40 J Neurosurg: Pediatrics / Volume 14 / November 2014
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
Part 5: Effect of valve type on CSF shunt efficacy
mable and nonprogrammable valve survival.11 The pro- the efficacy of the Delta valve with the Heyer-Shulte
grammable Strata and Codman Hakim valves were com- Multi-Purpose valve in 28 patients. Sixty-nine percent of
pared with multiple nonprogrammable valves and found patients with the Delta valve required revision, compared
to have significantly lower survival rates (19.8% vs. 45.8%, with 53% of patients with the Multi-Purpose valve. The
p = 0.0001). Another retrospective comparison between sample size in that study was small, and the data did not
programmable valves (Strata or Codman-Medos) and non- reach statistical significance. In an older paper by Serlo
programmable valves (Medtronic PS Medical) was under- et al.40 (1986), a retrospective review of 148 children was
taken by Mangano et al.24 (2005). In that study 11% of the conducted to compare the Pudenz-Heyer valve with the
programmable valves malfunctioned compared with 0% Cordis Hakim valve. No significant difference was found
of the nonprogrammable valves. The authors demonstrat- in overall shunt efficacy, although significance was dem-
ed a trend toward longer valve survival and shunt survival onstrated in a higher rate of valve patency on the part of
in the nonprogrammable group; however, neither reached the Pudenz-Heyer valve (p < 0.001).
statistical significance. McGirt et al. (2007) retrospective-
ly reviewed 279 patients who had undergone shunt place- Excluded Studies
ment procedures involving either a programmable (Strata The Task Force excluded 21 articles recalled for full-
or Codman Hakim) or nonprogrammable (PS Medical text review from the final evidentiary table. The majority
Delta) valve.27 The authors found that programmable valve of excluded papers did not include a comparison group
placement was associated with a reduced risk of both over- or control group.1–3,7–10,12,13,20,25,26,28,35 Other reasons for
all shunt revision (35% vs 54% in the nonprogrammable exclusion included invalid study design (questionnaire
group; p = 0.016) and proximal shunt obstruction (12% survey),30,31 redundant patient population5 (only the paper
vs 28% in the nonprogrammable group; p = 0.006). No- with the longest reported follow-up was included), and
tarianni et al.33 (2009) found no significant difference in a absence of a valid outcome variable (change in ventricle
retrospective review of 253 patients who underwent shunt size, development of spinal canal stenosis, historical de-
placement with either a programmable (Strata or Codman scription, and frequency of hospital visits).14,18,22,32
Hakim) or nonprogrammable (pressure-controlled or not
specified) valve. The failure rate among the programma-
ble valve group was 76.1%, and that among the differential Conclusions
pressure valve group was 80.0% (p = 0.11). Recommendation: There is insufficient evidence to
Other Comparison Groups demonstrate an advantage of one shunt hardware design
over another for the treatment of pediatric hydrocephalus.
Several Class III studies comparing variable shunt Current designs described in the evidentiary tables are all
valves were included in the review. Miranda et al.29 (2011) treatment options. Strength of Recommendation: Level
describe a retrospective review of 103 patients who re- I, high degree of clinical certainty.
ceived shunts for preterm-related posthemorrhagic hydro- Recommendation: There is insufficient evidence
cephalus. The authors reported a significantly higher rate to recommend the use of a programmable valve versus
of obstruction in patients weighing more than 2000 g who a nonprogrammable valve. Programmable and nonpro-
were treated with a fixed medium pressure valve (6 of 8 grammable valves are both options for the treatment of
patients) than in those who were treated with a fixed low pediatric hydrocephalus. Strength of Recommendation:
pressure valve (12 of 39 patients) (p = 0.040). Contrary Level II, moderate degree of clinical certainty.
findings were reported by Robinson et al. (2002) in a ret- The available literature in which one shunt com-
rospective analysis of shunt malfunction variables in 158 ponent is compared with another does not demonstrate
patients.38 Valve opening pressure was the only signifi- a clear superiority of one over another. Higher rates of
cant controllable factor found to be associated with shunt overdrainage were seen with standard differential pres-
malfunction. The 5-year shunt failure rate was 72% in the sure valves; however, the outcome variables studied in
no valve or low pressure valve group and 47% in the me- the comparisons of these groups with other shunt mecha-
dium or high pressure valve group (p = 0.0005). nisms failed to demonstrate statistical significance. While
Sainte-Rose et al.39 (1991) reviewed the charts of 1719 valves with antisiphon mechanisms may be superior in
patients with shunted hydrocephalus to assess mechani- preventing overdrainage complications, no statistically
cal complications. These authors found that the flanged significant data exist in the current medical literature to
ventricular catheter was associated with a higher risk of support this trend.
proximal occlusion (p < 0.04), open-ended distal catheters The studies assessing programmable versus nonpro-
were associated with fewer distal obstructions (log-rank grammable valves demonstrated either no statistically
p < 0.0003), and shunts with proximal medium pressure significant differences or contrary outcomes, pointing to
valves were less likely to malfunction than shunts with the need for long-term prospective controlled analysis of
distal slit valves (p < 0.000002). Tuli et al.42 (2000) did this issue. Class III data demonstrating poorer function
not find valve type to be associated with shunt malfunc- of distal slit valves in comparison with a proximal valve
tion in a post hoc analysis of a prospective cohort of 839 are described and are consistent with the contemporary
patients who underwent primary shunt insertions. No as- decrease in utilization of the former type of shunt system.
sociation between shunt malfunction and any component Many contemporary valve designs exist despite ma-
of the shunt hardware was reported in that study. jor deficiencies in long-term clinical evaluation. Well-de-
Ramadwar et al.37 (1997) retrospectively compared signed comparison studies with clearly defined outcome
J Neurosurg: Pediatrics / Volume 14 / November 2014 41
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
L. C. Baird et al.
variables and appropriate stratification of patient variables 10. Hanlo PW, Cinalli G, Vandertop WP, Faber JA, Bøgeskov L,
are needed to further investigate the appropriate clinical Børgesen SE, et al: Treatment of hydrocephalus determined
utilization of these valves. Accessing the necessary pa- by the European Orbis Sigma Valve II survey: a multicenter
prospective 5-year shunt survival study in children and adults
tient volume required to reach significance and balancing in whom a flow-regulating shunt was used. J Neurosurg
industry interests with trial integrity may be significant 99:52–57, 2003
barriers to pursuing needed studies; however, as increas- 11. Hatlen TJ, Shurtleff DB, Loeser JD, Ojemann JG, Avellino
ingly expensive and complex valves become available for AM, Ellenbogen RG: Nonprogrammable and programmable
clinical use, these studies will become imperative. cerebrospinal fluid shunt valves: a 5-year study. Clinical ar-
ticle. J Neurosurg Pediatr 9:462–467, 2012
Acknowledgments 12. Hertle DN, Tilgner J, Fruh K, Keinert T, Hagenston AM,
Unterberg AW, et al: Reversible occlusion (on-off) valves in
We acknowledge the American Association of Neurological shunted tumor patients. Neurosurg Rev 34:235–242, 2010
Surgeons (AANS)/Congress of Neurological Surgeons (CNS) Joint 13. Hoekstra A: Artificial shunting of cerebrospinal fluid. Int J
Guidelines Committee for the members’ reviews, comments, and Artif Organs 17:107–111, 1994
suggestions; Laura Mitchell, Guidelines Project Manager for the 14. Jain H, Natarajan K, Sgouros S: Influence of the shunt type in
CNS, for her contributions; Pamela Shaw, research librarian, for her the difference in reduction of volume between the two lateral
assistance with the literature searches; Kevin Boyer for his assistance ventricles in shunted hydrocephalic children. Childs Nerv
with data analysis; and Sue Ann Kawecki for her assistance with Syst 21:552–558, 2005
editing. 15. Jain H, Sgouros S, Walsh AR, Hockley AD: The treatment
of infantile hydrocephalus: “differential-pressure” or “flow-
Disclosure control” valves. A pilot study. Childs Nerv Syst 16:242–246,
The systematic review and evidence-based guidelines were 2000
funded exclusively by the CNS and AANS Pediatric Section, which 16. Kaiser GL, Horner E, Marchand S, Jost A: Conventional ver-
received no funding from outside commercial sources to support the sus Delta valve in the treatment of hydrocephalus in early in-
development of this document. fancy. Eur J Pediatr Surg 7 (Suppl 1):45–46, 1997
Conflict(s) of Interest: None. All Task Force members declared 17. Kan P, Walker ML, Drake JM, Kestle JR: Predicting slitlike
any potential conflicts of interest prior to beginning work on this ventricles in children on the basis of baseline characteristics
evidence review. at the time of shunt insertion. J Neurosurg 106 (5 Suppl):
Author contributions to the study and manuscript preparation 347–349, 2007
include the following. Conception and design: AANS/CNS Joint 18. Keen J: Casey Holter and the Spitz-Holter valve. Eur J Pedi-
Section on Pediatrics. Acquisition of data: all authors. Analysis and atr Surg 2 (Suppl 1):5–6, 1992
interpretation of data: all authors. Drafting the article: Baird. Criti- 19. Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F,
cally revising the article: all authors. Reviewed submitted version of et al: Long-term follow-up data from the Shunt Design Trial.
manuscript: all authors. Approved the final version of the manuscript Pediatr Neurosurg 33:230–236, 2000
on behalf of all authors: Flannery. Administrative/technical/material 20. Kestle JR, Walker ML: A multicenter prospective cohort study
support: all authors. Study supervision: Flannery. of the Strata valve for the management of hydrocephalus in
pediatric patients. J Neurosurg 102 (2 Suppl):141–145, 2005
21. Khan RA, Narasimhan KL, Tewari MK, Saxena AK: Role of
References
shunts with antisiphon device in treatment of pediatric hydro-
1. Ahn ES, Bookland M, Carson BS, Weingart JD, Jallo GI: The cephalus. Clin Neurol Neurosurg 112:687–690, 2010
Strata programmable valve for shunt-dependent hydrocepha- 22. Kondageski C, Thompson D, Reynolds M, Hayward RD: Ex-
lus: the pediatric experience at a single institution. Childs perience with the Strata valve in the management of shunt
Nerv Syst 23:297–303, 2007 overdrainage. J Neurosurg 106 (2 Suppl):95–102, 2007
2. Arnell K, Eriksson E, Olsen L: The programmable adult Cod- 23. Liniger P, Marchand S, Kaiser GL: Flow control versus anti-
man Hakim valve is useful even in very small children with siphon valves: late results concerning slit ventricles and slit-
hydrocephalus. A 7-year retrospective study with special fo- ventricle syndrome. Eur J Pediatr Surg 13 (Suppl 1):S3–S6,
cus on cost/benefit analysis. Eur J Pediatr Surg 16:1–7, 2006 2003
3. Breimer GE, Sival DA, Hoving EW: Low-pressure valves in 24. Mangano FT, Menendez JA, Habrock T, Narayan P, Leonard
hydrocephalic children: a retrospective analysis. Childs Nerv JR, Park TS, et al: Early programmable valve malfunctions
Syst 28:469–473, 2012 in pediatric hydrocephalus. J Neurosurg 103 (6 Suppl):
4. Davis SE, Levy ML, McComb JG, Sposto R: The delta valve: 501–507, 2005
how does its clinical performance compare with two other 25. Martínez-Lage JF, Almagro MJ, Del Rincón IS, Pérez-Espejo
pressure differential valves without antisiphon control? Pedi- MA, Piqueras C, Alfaro R, et al: Management of neonatal hy-
atr Neurosurg 33:58–63, 2000 drocephalus: feasibility of use and safety of two programma-
5. Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J Jr, et ble (Sophy and Polaris) valves. Childs Nerv Syst 24:549–556,
al: Randomized trial of cerebrospinal fluid shunt valve design 2008
in pediatric hydrocephalus. Neurosurgery 43:294–305, 1998 26. Mauer UM, Kunz U: More malfunctioning Medos Hakim
6. Gruber R, Jenny P, Herzog B: Experiences with the anti-si- programmable valves: cause for concern? Clinical article. J
phon device (ASD) in shunt therapy of pediatric hydrocepha- Neurosurg 115:1047–1052, 2011
lus. J Neurosurg 61:156–162, 1984 27. McGirt MJ, Buck DW II, Sciubba D, Woodworth GF, Carson
7. Guthkelch AN: The treatment of infantile hydrocephalus by B, Weingart J, et al: Adjustable vs set-pressure valves decrease
the Holter valve. Br J Surg 54:665–673, 1967 the risk of proximal shunt obstruction in the treatment of pe-
8. Haberl EJ, Messing-Juenger M, Schuhmann M, Eymann R, diatric hydrocephalus. Childs Nerv Syst 23:289–295, 2007
Cedzich C, Fritsch MJ, et al: Experiences with a gravity-as- 28. Meling TR, Egge A, Due-Tønnessen B: The gravity-assisted
sisted valve in hydrocephalic children. Clinical article. J Neu- Paedi-Gav valve in the treatment of pediatric hydrocephalus.
rosurg Pediatr 4:289–294, 2009 Pediatr Neurosurg 41:8–14, 2005
9. Hahn YS: Use of the distal double-slit valve system in children 29. Miranda P, Simal JA, Menor F, Plaza E, Conde R, Botella C:
with hydrocephalus. Childs Nerv Syst 10:99–103, 1994 Initial proximal obstruction of ventriculoperitoneal shunt in
42 J Neurosurg: Pediatrics / Volume 14 / November 2014
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
Part 5: Effect of valve type on CSF shunt efficacy
patients with preterm-related posthaemorrhagic hydrocepha- 38. Robinson S, Kaufman BA, Park TS: Outcome analysis of ini-
lus. Pediatr Neurosurg 47:88–92, 2011 tial neonatal shunts: does the valve make a difference? Pedi-
30. Miyake H, Ohta T, Kajimoto Y, Ogawa D: A clinical survey of atr Neurosurg 37:287–294, 2002
hydrocephalus and current treatment for hydrocephalus in Ja- 39. Sainte-Rose C, Piatt JH, Renier D, Pierre-Kahn A, Hirsch JF,
pan: analysis by nationwide questionnaire. Childs Nerv Syst Hoffman HJ, et al: Mechanical complications in shunts. Pedi-
15:363–368, 1999 atr Neurosurg 17:2–9, 1991–1992
31. Moritake K, Nagai H, Miyazaki T, Nagasako N, Yamasaki M, 40. Serlo W, von Wendt L, Heikkinen ES, Heikkinen ER: Ball and
Sakamoto H, et al: Analysis of a nationwide survey on treat- spring or slit and core valve for hydrocephalus shunting? Ann
ment and outcomes of congenital hydrocephalus in Japan. Clin Res 18 (Suppl 47):103–106, 1986
Neurol Med Chir (Tokyo) 47:453–461, 2007 41. Smely C, Van Velthoven V: Comparative study of two custom-
32. Nomura S, Fujii M, Kajiwara K, Ishihara H, Suehiro E, Goto ary cerebrospinal fluid shunting systems in early childhood
H, et al: Factors influencing spinal canal stenosis in patients hydrocephalus. Acta Neurochir (Wien) 139:875–882, 1997
with long-term controlled hydrocephalus treated with cere- 42. Tuli S, Drake J, Lawless J, Wigg M, Lamberti-Pasculli M:
brospinal fluid shunt. Childs Nerv Syst 26:931–935, 2010 Risk factors for repeated cerebrospinal shunt failures in pe-
33. Notarianni C, Vannemreddy P, Caldito G, Bollam P, Wylen diatric patients with hydrocephalus. J Neurosurg 92:31–38,
E, Willis B, et al: Congenital hydrocephalus and ventriculo- 2000
peritoneal shunts: influence of etiology and programmable 43. Virella AA, Galarza M, Masterman-Smith M, Lemus R, Laz-
shunts on revisions. Clinical article. J Neurosurg Pediatr areff JA: Distal slit valve and clinically relevant CSF over-
4:547–552, 2009 drainage in children with hydrocephalus. Childs Nerv Syst
34. Nulsen FE, Spitz EB: Treatment of hydrocephalus by direct 18:15–18, 2002
shunt from ventricle to jugular vein. Surg Forum:399–403, 44. Warf BC: Comparison of 1-year outcomes for the Chhabra
1951 and Codman-Hakim Micro Precision shunt systems in Ugan-
35. Piatt JH Jr, Carlson CV: A search for determinants of cerebro- da: a prospective study in 195 children. J Neurosurg 102 (4
spinal fluid shunt survival: retrospective analysis of a 14-year Suppl):358–362, 2005
institutional experience. Pediatr Neurosurg 19:233–242,
1993
36. Pollack IF, Albright AL, Adelson PD: A randomized, con- Manuscript submitted June 25, 2014.
trolled study of a programmable shunt valve versus a conven- Accepted July 7, 2014.
tional valve for patients with hydrocephalus. Neurosurgery Please include this information when citing this paper: DOI:
45:1399–1411, 1999 10.3171/2014.7.PEDS14325.
37. Ramadwar RH, Carachi R, Young DG: Infantile hydrocepha- Address correspondence to: Ann Marie Flannery, M.D., Depart-
lus: a comparison of the Delta valve and multipurpose valve. ment of Neurological Surgery, Saint Louis University, 3565 Vista
Eur J Pediatr Surg 7 (Suppl 1):44–45, 1997 Ave., St. Louis, MO 63110. email: flanneam@slu.edu.
J Neurosurg: Pediatrics / Volume 14 / November 2014 43
Unauthenticated | Downloaded 04/16/24 12:09 PM UTC
You might also like
- Create 24 - 7 - The Blueprint To Build A 6-Figure Twitter BusinessDocument7 pagesCreate 24 - 7 - The Blueprint To Build A 6-Figure Twitter BusinessEmmanuel0% (2)
- Ace Strategy InfoDocument1 pageAce Strategy Infoapi-292206241No ratings yet
- 1 Novacron S OverviewDocument3 pages1 Novacron S OverviewsaskoNo ratings yet
- THINK L4 Unit 6 Grammar BasicDocument2 pagesTHINK L4 Unit 6 Grammar Basicniyazi polatNo ratings yet
- Compression of The Fourth Ventricle Using A Craniosacral Osteopathic ...Document9 pagesCompression of The Fourth Ventricle Using A Craniosacral Osteopathic ...AlexNo ratings yet
- The Cartography of Crete in The 17thDocument28 pagesThe Cartography of Crete in The 17thΕυτύχης ΤζιρτζιλάκηςNo ratings yet
- Art. 1474 - PRICEDocument4 pagesArt. 1474 - PRICEjamaica_maglinteNo ratings yet
- 2014 7 Peds14324Document5 pages2014 7 Peds14324dewiNo ratings yet
- Pediatric Hydrocephalus: Systematic Literature Review and Evidence-Based Guidelines. Part 1: Introduction and MethodologyDocument5 pagesPediatric Hydrocephalus: Systematic Literature Review and Evidence-Based Guidelines. Part 1: Introduction and MethodologyagusNo ratings yet
- HydrocephalusDocument9 pagesHydrocephalusDeby AnditaNo ratings yet
- Intraoperative Evaluation of Urinary Tract Injuries at The Time of Pelvic Surgery A Systematic ReviewDocument9 pagesIntraoperative Evaluation of Urinary Tract Injuries at The Time of Pelvic Surgery A Systematic ReviewdlmejiapNo ratings yet
- Dural RepairDocument8 pagesDural RepairNolan James BrownNo ratings yet
- Van Midden Dorp 2013Document14 pagesVan Midden Dorp 2013Raveli KalvinNo ratings yet
- Treatment of Idiopathic A Chal Asia in The Ped PopulationDocument7 pagesTreatment of Idiopathic A Chal Asia in The Ped Populationcesar sanchez sanchezNo ratings yet
- BR J Sports Med-2008-Hegedus-80-92 PDFDocument14 pagesBR J Sports Med-2008-Hegedus-80-92 PDFAnonymous Jx2UvBeteNo ratings yet
- Can Neonatal Pull-Through Replace Staged Pull-ThrDocument26 pagesCan Neonatal Pull-Through Replace Staged Pull-Thrrahulrooney49No ratings yet
- Sedation Guidelines, Protocols, and Algorithms In.13Document8 pagesSedation Guidelines, Protocols, and Algorithms In.13Juan Pedro Alconada MaglianoNo ratings yet
- A Study To Assess The Effectiveness of Structured Teaching Programme On Knowledge Regarding Kidney Transplantation Among ESRD Patients at Selected Hospitals at Mandya (Dist.)Document8 pagesA Study To Assess The Effectiveness of Structured Teaching Programme On Knowledge Regarding Kidney Transplantation Among ESRD Patients at Selected Hospitals at Mandya (Dist.)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Article 2Document14 pagesArticle 2fatmazahrabahrounNo ratings yet
- Reflection PaperDocument8 pagesReflection Paperapi-240352465No ratings yet
- Neonatal Heart Rate Variability - A Contemporary Scoping Review of Analysis Methods and Clinical ApplicationsDocument23 pagesNeonatal Heart Rate Variability - A Contemporary Scoping Review of Analysis Methods and Clinical ApplicationsLucas SalgadoNo ratings yet
- Jurnal 2Document9 pagesJurnal 2Syanindita MaharaniNo ratings yet
- ICCS Standardization Report On Urodynamic StudiesDocument8 pagesICCS Standardization Report On Urodynamic StudiesAndy WijayaNo ratings yet
- SR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryDocument10 pagesSR and Guidelines For Periop MGMT of Peds Patients Undergoing Major Plastic SurgeryPaul MarjiNo ratings yet
- Ultrasound Imaging Reduces Failure Rates of Percutaneous Central Venous Catheterization in ChildrenDocument8 pagesUltrasound Imaging Reduces Failure Rates of Percutaneous Central Venous Catheterization in Childrenangelama1783riosNo ratings yet
- Incidencia de La Reabsorcion Espontanea de HNPDocument8 pagesIncidencia de La Reabsorcion Espontanea de HNPNicolas ParejaNo ratings yet
- Suresh 2015Document6 pagesSuresh 2015ade_liaNo ratings yet
- 10 1016@j Ctim 2012 07 009Document10 pages10 1016@j Ctim 2012 07 009Alexandra GeomaraNo ratings yet
- BR J Sports Med-2008-Hegedus-80-92Document14 pagesBR J Sports Med-2008-Hegedus-80-92api-263772125No ratings yet
- 10 1111@ans 15125Document7 pages10 1111@ans 15125Sahily MoralesNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- ERAS HigadoDocument24 pagesERAS HigadoGeraldNo ratings yet
- Epilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-AnalysisDocument9 pagesEpilepsy Duration and Seizure Outcome in Epilepsy Surgery: A Systematic Review and Meta-Analysisbaba ababNo ratings yet
- 2013 RC THB 2160.fullDocument27 pages2013 RC THB 2160.fullNoelia CalderónNo ratings yet
- Group Lit Rev PaperDocument15 pagesGroup Lit Rev PaperChelsea RuthrauffNo ratings yet
- [19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedDocument7 pages[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedBruno MañonNo ratings yet
- Epidural Space Identification A Meta Analysis Of.45Document10 pagesEpidural Space Identification A Meta Analysis Of.45Palliative MedicineNo ratings yet
- Effectiveness ESWT in Lower Limb Tendinopathy Syst. Rev. Mani-Babu 2014Document10 pagesEffectiveness ESWT in Lower Limb Tendinopathy Syst. Rev. Mani-Babu 2014Javier MartinNo ratings yet
- PROCESSDocument11 pagesPROCESSandrea vargasNo ratings yet
- 2017 Paravertebral Block en Pediatrics BJADocument8 pages2017 Paravertebral Block en Pediatrics BJAAlejandra SanchezNo ratings yet
- HHS Public Access: Developing A New Definition and Assessing New Clinical Criteria For Septic ShockDocument28 pagesHHS Public Access: Developing A New Definition and Assessing New Clinical Criteria For Septic ShockDulCee Cano SanzNo ratings yet
- Management of The Undescended Testis in ChildrenDocument16 pagesManagement of The Undescended Testis in ChildrenRashmeeta ThadhaniNo ratings yet
- Loop Vs DividedDocument8 pagesLoop Vs DividedNatalindah Jokiem Woecandra T. D.No ratings yet
- Kohn 2013Document20 pagesKohn 2013Georgiana BuneaNo ratings yet
- Wrist Ganglion Treatment - 2015 (Tema 4)Document16 pagesWrist Ganglion Treatment - 2015 (Tema 4)Carlos NoronaNo ratings yet
- Educationandadministration: Development of A Validated Exam To Assess Physician Transfusion Medicine KnowledgeDocument6 pagesEducationandadministration: Development of A Validated Exam To Assess Physician Transfusion Medicine KnowledgeFOURAT OUERGHEMMI100% (1)
- A Nonrigorous and Incorrect Evaluation Of  TheDocument2 pagesA Nonrigorous and Incorrect Evaluation Of  Thelincolnbasilio1No ratings yet
- Heart & Lung: Care of Critically Ill AdultsDocument13 pagesHeart & Lung: Care of Critically Ill AdultsRabiyatul AwaliyahNo ratings yet
- Withholding Feeds and Transfusion-Associated Necrotizing Enterocolitis in Preterm Infants: A Systematic ReviewDocument6 pagesWithholding Feeds and Transfusion-Associated Necrotizing Enterocolitis in Preterm Infants: A Systematic ReviewrezkyfikriNo ratings yet
- AlqahtaniDocument8 pagesAlqahtaniGanda SilitongaNo ratings yet
- Meta 2 - Sofi AA - 2018Document9 pagesMeta 2 - Sofi AA - 2018matheus.verasNo ratings yet
- Children 10 01862Document11 pagesChildren 10 01862Sinan Adnan Al-AbayechiNo ratings yet
- Appendix 21Document18 pagesAppendix 21Nailatul Hifdziyati CuhibnahNo ratings yet
- 1678-4227-anp-80-01-084Document13 pages1678-4227-anp-80-01-084anaclarapuzzellaNo ratings yet
- Lumbar PIDDocument6 pagesLumbar PIDdesai_erNo ratings yet
- Effect of Desflurane Versus Sevoflurane in Pediatric Anesthesia: A Meta-AnalysisDocument8 pagesEffect of Desflurane Versus Sevoflurane in Pediatric Anesthesia: A Meta-AnalysisdennyramdhanNo ratings yet
- Cefalea PospuncionDocument31 pagesCefalea Pospuncionmanolo.mendozavNo ratings yet
- Integrative Review 1Document17 pagesIntegrative Review 1api-442558242No ratings yet
- Academic Emergency Medicine - 2022 - Jessen - Restrictive Fluids Versus Standard Care in Adults With Sepsis in TheDocument32 pagesAcademic Emergency Medicine - 2022 - Jessen - Restrictive Fluids Versus Standard Care in Adults With Sepsis in TheLenin BlancasNo ratings yet
- E014478 FullDocument6 pagesE014478 FullГанбат М.No ratings yet
- Performing The Embryo Transfer - A GuidelineDocument15 pagesPerforming The Embryo Transfer - A GuidelineАнатолий КомогорцевNo ratings yet
- 1-s2.0-S0104001421000609-mainDocument9 pages1-s2.0-S0104001421000609-mainsyukronchalimNo ratings yet
- Surgery For Degenerative Lumbar Spondylosis: Updated Cochrane ReviewDocument9 pagesSurgery For Degenerative Lumbar Spondylosis: Updated Cochrane Reviewchartreuse avonleaNo ratings yet
- Research ArticleDocument10 pagesResearch Articlerazaqhussain00No ratings yet
- Cuff-Leak Test For Predicting Postextubation Airway Complications: A Systematic ReviewDocument13 pagesCuff-Leak Test For Predicting Postextubation Airway Complications: A Systematic ReviewMau MillanNo ratings yet
- Evidence-Based LaryngologyFrom EverandEvidence-Based LaryngologyDavid E. RosowNo ratings yet
- Tide Times and Tide Chart For Dammam PDFDocument8 pagesTide Times and Tide Chart For Dammam PDFAnonymous g5nMjONo ratings yet
- Land Titles and DeedsDocument1 pageLand Titles and DeedsIanLightPajaroNo ratings yet
- Prince Ganai NuclearDocument30 pagesPrince Ganai Nuclearprince_ganaiNo ratings yet
- Buy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlineDocument5 pagesBuy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlinelorendesuzaNo ratings yet
- The Titans Curse - Robert VendittiDocument134 pagesThe Titans Curse - Robert VendittimarianaqueirosluzNo ratings yet
- Portfolio Output No. 17: Reflections On Personal RelationshipsDocument3 pagesPortfolio Output No. 17: Reflections On Personal RelationshipsKatrina De VeraNo ratings yet
- Routing CodesDocument4 pagesRouting CodesScribdTranslationsNo ratings yet
- Adetunji CVDocument5 pagesAdetunji CVAdetunji AdegbiteNo ratings yet
- Testable Concepts in MCQDocument188 pagesTestable Concepts in MCQrami100% (1)
- Lesson A Worksheets. Print or Copy in Your Notebook-1Document3 pagesLesson A Worksheets. Print or Copy in Your Notebook-1Martha Lucia Arcila HenaoNo ratings yet
- Manual Therapy in The Treatment of Facial WrinklesDocument4 pagesManual Therapy in The Treatment of Facial WrinklesKarolina MirosNo ratings yet
- Perlengkapan Bayi Ellena and FamilyDocument9 pagesPerlengkapan Bayi Ellena and FamilyintanchairranyNo ratings yet
- Pre-Feasibility of Tunnel Farming in BahawalpurDocument10 pagesPre-Feasibility of Tunnel Farming in Bahawalpurshahidameen2100% (1)
- Architecture in EthDocument4 pagesArchitecture in Ethmelakumikias2No ratings yet
- Herbert Morrison BooklistDocument2 pagesHerbert Morrison BooklistGillian HallNo ratings yet
- Examen Blanc Et Corrige 3ASLLE Anglais 2e Sujet 2017Document4 pagesExamen Blanc Et Corrige 3ASLLE Anglais 2e Sujet 2017dila sailNo ratings yet
- HP Scanjet Pro 2500 F1 Flatbed Scanner: DatasheetDocument2 pagesHP Scanjet Pro 2500 F1 Flatbed Scanner: DatasheetKarkittykatNo ratings yet
- What A Body Can DoDocument26 pagesWhat A Body Can DoMariana Romero Bello100% (1)
- Bio-Valley Day Spa (Final Proposal To Submit) MDocument85 pagesBio-Valley Day Spa (Final Proposal To Submit) MAtiqah Hasan100% (4)
- Solid Edge Mold ToolingDocument3 pagesSolid Edge Mold ToolingVetrivendhan SathiyamoorthyNo ratings yet
- Hispanic Tradition in Philippine ArtsDocument14 pagesHispanic Tradition in Philippine ArtsRoger Pascual Cuaresma100% (1)
- Nemesis - TipsDocument2 pagesNemesis - TipsZoran StrajinNo ratings yet
- Form PDF 870914450231220Document8 pagesForm PDF 870914450231220Sachin KumarNo ratings yet
- Distress Tolerance Handout 5 - Pros and Cons PDFDocument1 pageDistress Tolerance Handout 5 - Pros and Cons PDFRobinNo ratings yet



































![[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matched](https://imgv2-1-f.scribdassets.com/img/document/722525723/149x198/0c84be9862/1712965550?v=1)