Professional Documents
Culture Documents
Enuresis Evaluation High Yield Notes
Enuresis Evaluation High Yield Notes
Uploaded by
hassan.m.55555Copyright:
Available Formats
You might also like
- Infusion Pumps Training-Converted1Document79 pagesInfusion Pumps Training-Converted1Trương DuyNo ratings yet
- HRM - Group 7 FinalDocument15 pagesHRM - Group 7 FinalsoumyaNo ratings yet
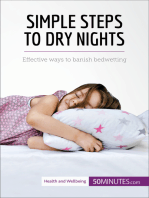
- Bedwetting in ChildrenDocument41 pagesBedwetting in ChildrenAnkit Mangla100% (1)
- Enuresis. 2Document50 pagesEnuresis. 2q55xkm5n47No ratings yet
- EnuresisDocument5 pagesEnuresisCristy BarriosNo ratings yet
- DR - Yacobda - ENURESIS AND GPDocument26 pagesDR - Yacobda - ENURESIS AND GPNikko Caesario Mauldy SusiloNo ratings yet
- Febrile SeizuresDocument1 pageFebrile SeizuresDiana AlexandraNo ratings yet
- Enuresis FinalDocument21 pagesEnuresis FinalNac OsceNo ratings yet
- Bedwetting and Toileting Problems in ChildrenDocument6 pagesBedwetting and Toileting Problems in ChildrenBogdan NeamtuNo ratings yet
- Final Bed WettingDocument40 pagesFinal Bed Wettingdrmurad321No ratings yet
- Childhood Seizures and Meningitis Part-1Document28 pagesChildhood Seizures and Meningitis Part-1younas63No ratings yet
- LEC-Psych2 - Enuresis - Epidemiology 0 EtiologyDocument2 pagesLEC-Psych2 - Enuresis - Epidemiology 0 EtiologyGriselle GomezNo ratings yet
- IntussusceptionDocument2 pagesIntussusceptionqalbiNo ratings yet
- Nocturnal EnuresisDocument1 pageNocturnal EnuresisGerardLumNo ratings yet
- Pediatric Surg TransDocument4 pagesPediatric Surg TransSven OrdanzaNo ratings yet
- Enuresis in Children - A Case - Based ApproachDocument9 pagesEnuresis in Children - A Case - Based ApproachBogdan NeamtuNo ratings yet
- EnuresisDocument31 pagesEnuresisZubair Mahmood KamalNo ratings yet
- Caldwell2013review Nocturnal EnuresisDocument6 pagesCaldwell2013review Nocturnal EnuresisBogdan Neamtu100% (1)
- 21.2 Seizure in ChildhoodDocument4 pages21.2 Seizure in Childhoodhusenbrz4No ratings yet
- Children Part I Continuation TABLEDocument5 pagesChildren Part I Continuation TABLEMaikka IlaganNo ratings yet
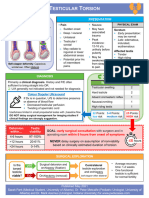
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- Elimination Disorder - A Psychiatric Paediatric DisorderDocument22 pagesElimination Disorder - A Psychiatric Paediatric DisorderMeghana PatilNo ratings yet
- Clinical Management of Nocturnal EnuresisDocument11 pagesClinical Management of Nocturnal EnuresisDaniela Rodríguez MartínezNo ratings yet
- LECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)Document57 pagesLECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)CristinaGheorgheNo ratings yet
- Enuresis PDFDocument7 pagesEnuresis PDFmist73No ratings yet
- Diagnostic and Statistical Manual DSM Elimination DisorderDocument6 pagesDiagnostic and Statistical Manual DSM Elimination DisorderMihai Mirel RusuNo ratings yet
- Exam 3 Blueprint UpdateDocument63 pagesExam 3 Blueprint Updatewedad jumaNo ratings yet
- Diare Dehidrasi BeratDocument40 pagesDiare Dehidrasi BeratcutietimothyNo ratings yet
- Elimination DisordersDocument7 pagesElimination DisordersGladysh Jera QuinagonNo ratings yet
- Practical Algorithms in Pediatric GastroenterologyDocument4 pagesPractical Algorithms in Pediatric GastroenterologyHitesh Deora0% (1)
- Enuresis Aafp PDFDocument8 pagesEnuresis Aafp PDFyusditaoNo ratings yet
- Pediatric EpilepsyDocument6 pagesPediatric EpilepsyJosh RoshalNo ratings yet
- Screenshot 2024-03-07 at 11.13.52 AMDocument88 pagesScreenshot 2024-03-07 at 11.13.52 AMmarlyaasri2No ratings yet
- Physical Examination of The NewbornDocument39 pagesPhysical Examination of The NewbornSabita Jana100% (1)
- PediatricDocument10 pagesPediatrictalarashad2002No ratings yet
- (Surgery) Midterms PediatricsDocument5 pages(Surgery) Midterms Pediatricsalmira.s.mercadoNo ratings yet
- Pages From PEM - 5 Minute Pediatric Emergency Medicine Consult-2Document2 pagesPages From PEM - 5 Minute Pediatric Emergency Medicine Consult-2Dmitri KaramazovNo ratings yet
- Care of The Mother, Child at Risk or With Problems (Acute and Chronic)Document5 pagesCare of The Mother, Child at Risk or With Problems (Acute and Chronic)Elizabeth ZamoraNo ratings yet
- Apnea OyODocument22 pagesApnea OyOLaura BulaNo ratings yet
- Asfixia Perinatal, CompendiumDocument7 pagesAsfixia Perinatal, CompendiumClaudia LópezNo ratings yet
- NCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Document55 pagesNCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Joseph DusichNo ratings yet
- UTI in ChildrenDocument94 pagesUTI in ChildrenSarfraz AnsariNo ratings yet
- Management of PX With Neurologic DysfunctionDocument12 pagesManagement of PX With Neurologic Dysfunctiongabrielle magdaraogNo ratings yet
- Pediatric Neurology - Pediatric Epilepsy SyndromeDocument6 pagesPediatric Neurology - Pediatric Epilepsy Syndromemkct111100% (1)
- Nocturnal Enuresis:: Current ConceptsDocument9 pagesNocturnal Enuresis:: Current Conceptsdstu20No ratings yet
- Pediatric Nursing HandoutDocument17 pagesPediatric Nursing HandoutJem TupazNo ratings yet
- NCM 109 Midterms - Infertility L2Document7 pagesNCM 109 Midterms - Infertility L2Leigh Angelika Dela CruzNo ratings yet
- Pregnancy LossDocument32 pagesPregnancy LossDaniel GalitzineNo ratings yet
- PEDIATRIC NURSING HandoutDocument17 pagesPEDIATRIC NURSING HandoutJen Ezel100% (1)
- Acute Scrotal Pain or SwellingDocument6 pagesAcute Scrotal Pain or SwellingAnna N WachidahNo ratings yet
- Seizures in Childhood: John Bradford Ingram M.D. Assistant Professor of Pediatrics Division of Child NeurologyDocument50 pagesSeizures in Childhood: John Bradford Ingram M.D. Assistant Professor of Pediatrics Division of Child NeurologyTaylor ChristianNo ratings yet
- BedwettingDocument3 pagesBedwettingaanya khajuriaNo ratings yet
- Pregnancy Induced HypertensionDocument4 pagesPregnancy Induced HypertensionNibraz ChNo ratings yet
- Gynaecological Issues in PubertyDocument56 pagesGynaecological Issues in PubertyAnil DasNo ratings yet
- DysphagiaDocument2 pagesDysphagiaKimberlyLaw95No ratings yet
- Febrile Seizure and Epilepsy PDFDocument36 pagesFebrile Seizure and Epilepsy PDFMuhammad Amiro RasheeqNo ratings yet
- Alvarez, Synthesis 5Document6 pagesAlvarez, Synthesis 5Arianne AlvarezNo ratings yet
- Pedia - Seizure Final PDFDocument8 pagesPedia - Seizure Final PDFPrakkash SJNo ratings yet
- NeonatologyDocument8 pagesNeonatologyPixel MlbbNo ratings yet
- EnuresisDocument7 pagesEnuresisMohammed HarisNo ratings yet
- Nocturnal Enuresis, (Night Urination) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNocturnal Enuresis, (Night Urination) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 1 out of 5 stars1/5 (1)
- Treatment Plan FormDocument10 pagesTreatment Plan Formba pettycrewNo ratings yet
- Research Latest Final Kian Okay NaDocument57 pagesResearch Latest Final Kian Okay NaKian NotarioNo ratings yet
- World Malaria Report: Years of Global Progress & ChallengesDocument300 pagesWorld Malaria Report: Years of Global Progress & ChallengesMOBA LQNo ratings yet
- Beauty Therapy Thesis SampleDocument8 pagesBeauty Therapy Thesis Samplerachelvalenzuelaglendale100% (2)
- Resume Ahmad AkbariDocument3 pagesResume Ahmad AkbariSepideh MirzaeiNo ratings yet
- Outcomes of Surgical Management of Floating Knee Injuries: Original ResearchDocument4 pagesOutcomes of Surgical Management of Floating Knee Injuries: Original ResearchManiDeep ReddyNo ratings yet
- Prabhat KhabarDocument64 pagesPrabhat KhabarShree CyberiaNo ratings yet
- Salinan ISO 14155 - 2020Document31 pagesSalinan ISO 14155 - 2020regulatory ransNo ratings yet
- Treatment Plan Sample PDFDocument4 pagesTreatment Plan Sample PDFRM April AlonNo ratings yet
- Lecture 01 Introduction - Part 2 BackgroundDocument32 pagesLecture 01 Introduction - Part 2 BackgroundZahraa student2No ratings yet
- XTX PDFDocument338 pagesXTX PDFAndrei MihaiNo ratings yet
- Foundations of EpidemiologyDocument106 pagesFoundations of EpidemiologySudaysi AbdisalamNo ratings yet
- 102 - SCO8048A-Alert - Fixings-FinalDocument3 pages102 - SCO8048A-Alert - Fixings-FinalO SNo ratings yet
- Individual Performance Commitment and Review Formlatest2016blankDocument5 pagesIndividual Performance Commitment and Review Formlatest2016blankJohn AmbasNo ratings yet
- SOS Children'S Villages: Case Study IiiDocument13 pagesSOS Children'S Villages: Case Study IiiSalahuddin HusseinNo ratings yet
- AIIMS NORCET Syllabus 2021Document3 pagesAIIMS NORCET Syllabus 2021BhavnaNo ratings yet
- Recommendation: Osteoporosis To Prevent Fractures: Screening - United States Preventive Services TaskforceDocument22 pagesRecommendation: Osteoporosis To Prevent Fractures: Screening - United States Preventive Services TaskforceNonoy JoyaNo ratings yet
- Prospectus - 2022 Admission: M. Phil Course in Clinical Epidemiology (Part-Time) CourseDocument5 pagesProspectus - 2022 Admission: M. Phil Course in Clinical Epidemiology (Part-Time) CourseDr.Minu C MathewsNo ratings yet
- Debitul de Sânge CerebralDocument4 pagesDebitul de Sânge CerebralAurelia AlexandraNo ratings yet
- Voucher VaticanDocument4 pagesVoucher VaticanSpirosGongasNo ratings yet
- Good Governance FormatDocument16 pagesGood Governance FormatMarjonNo ratings yet
- Hba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Document1 pageHba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Michamiel SerratoNo ratings yet
- Lifespan Development Lives in Context 1st Edition Kuther Solutions Manual DownloadDocument5 pagesLifespan Development Lives in Context 1st Edition Kuther Solutions Manual DownloadSean Hamlin100% (25)
- Enteral and ParenteralDocument64 pagesEnteral and ParenteralHeba IyadNo ratings yet
- Proposal Business PlanDocument13 pagesProposal Business PlanM Yusuf MaulanaNo ratings yet
- Pakistan Floods SitRep 28 September 2022Document8 pagesPakistan Floods SitRep 28 September 2022Shuja NoorNo ratings yet
- BIOQUELL PRODUCT SHEET - Pod - HC001-MKT-034Document2 pagesBIOQUELL PRODUCT SHEET - Pod - HC001-MKT-034Andrei SanduNo ratings yet
- Ls10 Reaching The Age of Adolescence WSDocument2 pagesLs10 Reaching The Age of Adolescence WSAshwika AgarwalNo ratings yet
Enuresis Evaluation High Yield Notes
Enuresis Evaluation High Yield Notes
Uploaded by
hassan.m.55555Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Enuresis Evaluation High Yield Notes
Enuresis Evaluation High Yield Notes
Uploaded by
hassan.m.55555Copyright:
Available Formats
ENURESIS: EVALUATION
EPIDEMIOLOGY &
Enuresis = persistent nocturnal incontinence
NATURAL HISTORY
>2 episodes/week Occurs during sleep Uncontrolled
urinary voiding Daytime Nighttime
• In children ≥5 years old. Also known as “bedwetting” bladder bladder control
• Occurs when child does not wake up from sleep to void control achieved
• Results from a combination of: genetic factors, maturational delay, expected months-years
1°
excessively deep sleep, reduced bladder capacity, nocturnal polyuria ~age 4 after daytime
2°
~age 5 – 7
Primary Enuresis Secondary Enuresis
Never previously achieved Enuresis developed after ≥6 consecutive Age Prevalence
period of nighttime dryness. months of nighttime continence. Often 5 15% • Common!
~80% of nocturnal enuresis triggered by stressors (divorce, birth of
cases, high rate of sibling, school), sleep disordered breathing, 6 13% • Resolves
spontaneous resolution constipation, suboptimal voiding habits. spontaneously
7 10% ~15%/year
8 7% • Longer
Goal: rule out presence of underlying medical problem
10 5% persistence
Such as urinary tract infection, constipation, obstructive sleep
= lower
apnea, and diabetes insipidus. 12-14 2-3% probability of
spontaneous
≥15 1-2%
resolution
PRESENTATION
HISTORY PHYSICAL EXAM
2:1
? Frequency (# /night, # /week, timing of episodes) o Genital exam Male : Female
? Trend (improving vs. worsening) usually normal in
? Daytime symptoms and/or LUTS* primary enuresis 20% also have
? Constipation or fecal incontinence o Fever may daytime
? Previous period of dryness (>6mths?) indicate UTI symptoms
o Abdominal
? Volume voided (large volumes are indicative of 15% also
palpation for stool
nocturnal polyuria) have fecal
o Lower back for
? Fluid intake (majority in evening?) stigmata of spinal incontinence
? Previous interventions? Were they successful? dysraphism
? PMHx (sleep apnea, diabetes, UTIs, sickle cell, (midline hair tufts,
?
neurologic abnormalities, ADHD, ASD)
Neurodevelopmental delays? Behavioural or
sacral dimple)
o Lower limb
* Lower Urinary Tract
Symptoms (LUTS)
psychologic concerns? strength, tone,
? FHx of nocturnal enuresis (what age reflexes, Voiding Storage
did parent resolve enuresis? sensation for § Hesitancy § Urgency
evidence of § Weak stream § Frequency
? SHx (recent stressors?)
neurogenic § Intermittent ≥8 or ≤3
? Impact on child and family stream times/day
bladder
? Review voiding diary if available § Straining
§ Genital or lower
§ Incomplete
urinary tract pain
emptying
§ Holding
INVESTIGATIONS § Dribbling
maneuvers
If reassuring presentation… If concerning history and physical exam…
Presence of daytime symptoms
Urinalysis & Culture Renal/Bladder and/or LUTS is suggestive of
No routine Ultrasound dysfunctional voiding or
tests are To rule out
anatomical abnormalities, thus
required UTI, DM, Only if otherwise should be referred to Urology
DKA, DI indicated
Published January 2022
Sarah Park (Medical Student C2022, University of Alberta), Dr. Peter Metcalfe (Pediatric Urologist,
University of Alberta) for www.pedscases.com
ENURESIS: COUNSELLING & MANAGEMENT
INITIAL MANAGEMENT
1. Determine if… Personalized Calendar § Helps to follow
q Both child and parent see enuresis as problematic, progress
and are motivated to participate in treatment Record: § Parents should
q The child is mature enough to engage in and • Daytime incontinence be cautious of
assume responsibility for treatment implementing a
• Enuresis events
2. Treat co-existing conditions: reward system
q Constipation, sleep disordered breathing, ADHD,
• Encopresis
• Frequency & timing § AVOID
underlying stressors, poor self-concept, psychologic
3. Educate, emphasizing… of bowel movements punishment
q High prevalence and generally self-resolving and humiliation
natural history
q Child should NOT be punished for bedwetting
q Usefulness of bed protection, absorbent BEHAVIOURAL THERAPY
undergarments, room deodorizers
q Avoiding sugary and caffeinated beverages Goal: achieve good bladder and bowel habits
4. Establish goals and expectations: ü Encourage frequent voids
q Determine family priorities (Reassurance? Staying o Introduce timed voiding every 2 hours,
dry for sleepovers? Decreasing # wet nights?) regardless of if child feels the need to void
q May involve several methods, be prolonged, fail in o Avoid holding urine, urgency, and incontinence
short term, often relapses o Ensure easy access to toilets at school & home
q Slow, steady improvement is more realistic o Always have child void immediately before sleep
ü Encourage daily bowel movements
o Establish a schedule at specific time of day such
as after breakfast before leaving for school
§ Time of void
Voiding § Volume voided
o PEG 3350 for constipation
Should ü Consume majority of fluids in morning
Diary § Relationship to events and afternoon, minimize after dinner
record: (meals, school recess, ü Encourage physical activity and
play activities, stress) discourage prolonged sitting
§ Episodes of urgency ü Requires supportive environment, child
or incontinence motivation, patience, and time (average 6 months)
ACTIVE THERAPY
Similar outcomes, choose based on patient preference and fit with family
Pharmacologic Therapy Bed Alarms
• Desmopressin: Goal: teach child to awaken from sensation of a full bladder.
Goal: optimize oral medication to reduce Sensors attached to child’s undergarments are connected to an
production of urine overnight (ADH analogue). alarm that awakens the child at the moment of bed wetting.
Ø Take medication 60 minutes before bedtime Ø Should be using every night
Ø No fluid intake 1 hour prior to and Ø Initially, child may not awaken from alarm,
8 hours after taking medication requiring parent to awaken child instead
Ø WATCH FOR: signs of symptomatic Ø Child should then void in the washroom
hyponatremia with water intoxication: Ø Return to sleep
discontinue if developing headache, • Most effective in children >7 years old
nausea, vomiting. • Generally see initial response in 1 – 2 months
Can be used intermittently, thus a good option for • 3 – 4 month trial of continuous therapy is recommended
special occasions such as sleepovers and camps. • Discontinue when dry for 14 consecutive nights,
or if no improvement at one month
• Anticholinergics and tricyclic agents • Effective long term in < 50% of children
(second and third line): may be considered if • Recommend for older, motivated children
other therapeutic options have failed. from cooperative families
Published December 2021
Sarah Park (Medical Student C2022, University of Alberta), Dr. Peter Metcalfe (Pediatric Urologist,
University of Alberta) for www.pedscases.com
You might also like
- Infusion Pumps Training-Converted1Document79 pagesInfusion Pumps Training-Converted1Trương DuyNo ratings yet
- HRM - Group 7 FinalDocument15 pagesHRM - Group 7 FinalsoumyaNo ratings yet
- Bedwetting in ChildrenDocument41 pagesBedwetting in ChildrenAnkit Mangla100% (1)
- Enuresis. 2Document50 pagesEnuresis. 2q55xkm5n47No ratings yet
- EnuresisDocument5 pagesEnuresisCristy BarriosNo ratings yet
- DR - Yacobda - ENURESIS AND GPDocument26 pagesDR - Yacobda - ENURESIS AND GPNikko Caesario Mauldy SusiloNo ratings yet
- Febrile SeizuresDocument1 pageFebrile SeizuresDiana AlexandraNo ratings yet
- Enuresis FinalDocument21 pagesEnuresis FinalNac OsceNo ratings yet
- Bedwetting and Toileting Problems in ChildrenDocument6 pagesBedwetting and Toileting Problems in ChildrenBogdan NeamtuNo ratings yet
- Final Bed WettingDocument40 pagesFinal Bed Wettingdrmurad321No ratings yet
- Childhood Seizures and Meningitis Part-1Document28 pagesChildhood Seizures and Meningitis Part-1younas63No ratings yet
- LEC-Psych2 - Enuresis - Epidemiology 0 EtiologyDocument2 pagesLEC-Psych2 - Enuresis - Epidemiology 0 EtiologyGriselle GomezNo ratings yet
- IntussusceptionDocument2 pagesIntussusceptionqalbiNo ratings yet
- Nocturnal EnuresisDocument1 pageNocturnal EnuresisGerardLumNo ratings yet
- Pediatric Surg TransDocument4 pagesPediatric Surg TransSven OrdanzaNo ratings yet
- Enuresis in Children - A Case - Based ApproachDocument9 pagesEnuresis in Children - A Case - Based ApproachBogdan NeamtuNo ratings yet
- EnuresisDocument31 pagesEnuresisZubair Mahmood KamalNo ratings yet
- Caldwell2013review Nocturnal EnuresisDocument6 pagesCaldwell2013review Nocturnal EnuresisBogdan Neamtu100% (1)
- 21.2 Seizure in ChildhoodDocument4 pages21.2 Seizure in Childhoodhusenbrz4No ratings yet
- Children Part I Continuation TABLEDocument5 pagesChildren Part I Continuation TABLEMaikka IlaganNo ratings yet
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- Elimination Disorder - A Psychiatric Paediatric DisorderDocument22 pagesElimination Disorder - A Psychiatric Paediatric DisorderMeghana PatilNo ratings yet
- Clinical Management of Nocturnal EnuresisDocument11 pagesClinical Management of Nocturnal EnuresisDaniela Rodríguez MartínezNo ratings yet
- LECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)Document57 pagesLECTURE 3 - NONEPILEPTIC Events (Held in 14.2.19)CristinaGheorgheNo ratings yet
- Enuresis PDFDocument7 pagesEnuresis PDFmist73No ratings yet
- Diagnostic and Statistical Manual DSM Elimination DisorderDocument6 pagesDiagnostic and Statistical Manual DSM Elimination DisorderMihai Mirel RusuNo ratings yet
- Exam 3 Blueprint UpdateDocument63 pagesExam 3 Blueprint Updatewedad jumaNo ratings yet
- Diare Dehidrasi BeratDocument40 pagesDiare Dehidrasi BeratcutietimothyNo ratings yet
- Elimination DisordersDocument7 pagesElimination DisordersGladysh Jera QuinagonNo ratings yet
- Practical Algorithms in Pediatric GastroenterologyDocument4 pagesPractical Algorithms in Pediatric GastroenterologyHitesh Deora0% (1)
- Enuresis Aafp PDFDocument8 pagesEnuresis Aafp PDFyusditaoNo ratings yet
- Pediatric EpilepsyDocument6 pagesPediatric EpilepsyJosh RoshalNo ratings yet
- Screenshot 2024-03-07 at 11.13.52 AMDocument88 pagesScreenshot 2024-03-07 at 11.13.52 AMmarlyaasri2No ratings yet
- Physical Examination of The NewbornDocument39 pagesPhysical Examination of The NewbornSabita Jana100% (1)
- PediatricDocument10 pagesPediatrictalarashad2002No ratings yet
- (Surgery) Midterms PediatricsDocument5 pages(Surgery) Midterms Pediatricsalmira.s.mercadoNo ratings yet
- Pages From PEM - 5 Minute Pediatric Emergency Medicine Consult-2Document2 pagesPages From PEM - 5 Minute Pediatric Emergency Medicine Consult-2Dmitri KaramazovNo ratings yet
- Care of The Mother, Child at Risk or With Problems (Acute and Chronic)Document5 pagesCare of The Mother, Child at Risk or With Problems (Acute and Chronic)Elizabeth ZamoraNo ratings yet
- Apnea OyODocument22 pagesApnea OyOLaura BulaNo ratings yet
- Asfixia Perinatal, CompendiumDocument7 pagesAsfixia Perinatal, CompendiumClaudia LópezNo ratings yet
- NCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Document55 pagesNCM 109 SKILLS LAB DAY 1 Laboratory and Diagnostics22Joseph DusichNo ratings yet
- UTI in ChildrenDocument94 pagesUTI in ChildrenSarfraz AnsariNo ratings yet
- Management of PX With Neurologic DysfunctionDocument12 pagesManagement of PX With Neurologic Dysfunctiongabrielle magdaraogNo ratings yet
- Pediatric Neurology - Pediatric Epilepsy SyndromeDocument6 pagesPediatric Neurology - Pediatric Epilepsy Syndromemkct111100% (1)
- Nocturnal Enuresis:: Current ConceptsDocument9 pagesNocturnal Enuresis:: Current Conceptsdstu20No ratings yet
- Pediatric Nursing HandoutDocument17 pagesPediatric Nursing HandoutJem TupazNo ratings yet
- NCM 109 Midterms - Infertility L2Document7 pagesNCM 109 Midterms - Infertility L2Leigh Angelika Dela CruzNo ratings yet
- Pregnancy LossDocument32 pagesPregnancy LossDaniel GalitzineNo ratings yet
- PEDIATRIC NURSING HandoutDocument17 pagesPEDIATRIC NURSING HandoutJen Ezel100% (1)
- Acute Scrotal Pain or SwellingDocument6 pagesAcute Scrotal Pain or SwellingAnna N WachidahNo ratings yet
- Seizures in Childhood: John Bradford Ingram M.D. Assistant Professor of Pediatrics Division of Child NeurologyDocument50 pagesSeizures in Childhood: John Bradford Ingram M.D. Assistant Professor of Pediatrics Division of Child NeurologyTaylor ChristianNo ratings yet
- BedwettingDocument3 pagesBedwettingaanya khajuriaNo ratings yet
- Pregnancy Induced HypertensionDocument4 pagesPregnancy Induced HypertensionNibraz ChNo ratings yet
- Gynaecological Issues in PubertyDocument56 pagesGynaecological Issues in PubertyAnil DasNo ratings yet
- DysphagiaDocument2 pagesDysphagiaKimberlyLaw95No ratings yet
- Febrile Seizure and Epilepsy PDFDocument36 pagesFebrile Seizure and Epilepsy PDFMuhammad Amiro RasheeqNo ratings yet
- Alvarez, Synthesis 5Document6 pagesAlvarez, Synthesis 5Arianne AlvarezNo ratings yet
- Pedia - Seizure Final PDFDocument8 pagesPedia - Seizure Final PDFPrakkash SJNo ratings yet
- NeonatologyDocument8 pagesNeonatologyPixel MlbbNo ratings yet
- EnuresisDocument7 pagesEnuresisMohammed HarisNo ratings yet
- Nocturnal Enuresis, (Night Urination) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNocturnal Enuresis, (Night Urination) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 1 out of 5 stars1/5 (1)
- Treatment Plan FormDocument10 pagesTreatment Plan Formba pettycrewNo ratings yet
- Research Latest Final Kian Okay NaDocument57 pagesResearch Latest Final Kian Okay NaKian NotarioNo ratings yet
- World Malaria Report: Years of Global Progress & ChallengesDocument300 pagesWorld Malaria Report: Years of Global Progress & ChallengesMOBA LQNo ratings yet
- Beauty Therapy Thesis SampleDocument8 pagesBeauty Therapy Thesis Samplerachelvalenzuelaglendale100% (2)
- Resume Ahmad AkbariDocument3 pagesResume Ahmad AkbariSepideh MirzaeiNo ratings yet
- Outcomes of Surgical Management of Floating Knee Injuries: Original ResearchDocument4 pagesOutcomes of Surgical Management of Floating Knee Injuries: Original ResearchManiDeep ReddyNo ratings yet
- Prabhat KhabarDocument64 pagesPrabhat KhabarShree CyberiaNo ratings yet
- Salinan ISO 14155 - 2020Document31 pagesSalinan ISO 14155 - 2020regulatory ransNo ratings yet
- Treatment Plan Sample PDFDocument4 pagesTreatment Plan Sample PDFRM April AlonNo ratings yet
- Lecture 01 Introduction - Part 2 BackgroundDocument32 pagesLecture 01 Introduction - Part 2 BackgroundZahraa student2No ratings yet
- XTX PDFDocument338 pagesXTX PDFAndrei MihaiNo ratings yet
- Foundations of EpidemiologyDocument106 pagesFoundations of EpidemiologySudaysi AbdisalamNo ratings yet
- 102 - SCO8048A-Alert - Fixings-FinalDocument3 pages102 - SCO8048A-Alert - Fixings-FinalO SNo ratings yet
- Individual Performance Commitment and Review Formlatest2016blankDocument5 pagesIndividual Performance Commitment and Review Formlatest2016blankJohn AmbasNo ratings yet
- SOS Children'S Villages: Case Study IiiDocument13 pagesSOS Children'S Villages: Case Study IiiSalahuddin HusseinNo ratings yet
- AIIMS NORCET Syllabus 2021Document3 pagesAIIMS NORCET Syllabus 2021BhavnaNo ratings yet
- Recommendation: Osteoporosis To Prevent Fractures: Screening - United States Preventive Services TaskforceDocument22 pagesRecommendation: Osteoporosis To Prevent Fractures: Screening - United States Preventive Services TaskforceNonoy JoyaNo ratings yet
- Prospectus - 2022 Admission: M. Phil Course in Clinical Epidemiology (Part-Time) CourseDocument5 pagesProspectus - 2022 Admission: M. Phil Course in Clinical Epidemiology (Part-Time) CourseDr.Minu C MathewsNo ratings yet
- Debitul de Sânge CerebralDocument4 pagesDebitul de Sânge CerebralAurelia AlexandraNo ratings yet
- Voucher VaticanDocument4 pagesVoucher VaticanSpirosGongasNo ratings yet
- Good Governance FormatDocument16 pagesGood Governance FormatMarjonNo ratings yet
- Hba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Document1 pageHba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Michamiel SerratoNo ratings yet
- Lifespan Development Lives in Context 1st Edition Kuther Solutions Manual DownloadDocument5 pagesLifespan Development Lives in Context 1st Edition Kuther Solutions Manual DownloadSean Hamlin100% (25)
- Enteral and ParenteralDocument64 pagesEnteral and ParenteralHeba IyadNo ratings yet
- Proposal Business PlanDocument13 pagesProposal Business PlanM Yusuf MaulanaNo ratings yet
- Pakistan Floods SitRep 28 September 2022Document8 pagesPakistan Floods SitRep 28 September 2022Shuja NoorNo ratings yet
- BIOQUELL PRODUCT SHEET - Pod - HC001-MKT-034Document2 pagesBIOQUELL PRODUCT SHEET - Pod - HC001-MKT-034Andrei SanduNo ratings yet
- Ls10 Reaching The Age of Adolescence WSDocument2 pagesLs10 Reaching The Age of Adolescence WSAshwika AgarwalNo ratings yet