Professional Documents
Culture Documents
Vendaje Compresivo Para Ulceras Venosas en Pierna
Vendaje Compresivo Para Ulceras Venosas en Pierna
Uploaded by
Belen mtzCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vendaje Compresivo Para Ulceras Venosas en Pierna
Vendaje Compresivo Para Ulceras Venosas en Pierna
Uploaded by
Belen mtzCopyright:
Available Formats
Therapeutic Guidelines
Compression therapy for venous leg ulcers
Brijesh Nair
Consultant INTRODUCTION elastic (long stretch bandages [LSB]). The
Dermatologist, differences between the two groups of bandages
Department of are elucidated in Table 2.
Compression therapy is the mainstay of treatment
Dermatology and
Venereology, INHS of venous leg ulcers (VLU). Good wound care
Sanjivani, Kochi, India and compression therapy will heal majority of COMPRESSION BANDAGES
small venous ulcers of short duration.[1] Goals
of compression therapy are ulcer healing, All bandages used in compression must be
reduction of pain and edema, and prevention of applied on top of padding (subcompression
recurrence.[2] Compression is used for VLU and wadding bandage) to prevent friction and
narrows veins and restores valve competence pressure damage over bony prominences by
and reduces ambulatory venous pressure, spreading pressure across a greater area.
thus reducing venous reflux (VR). It also helps Bandages should generally be applied toe to
decrease inflammatory cytokines, accelerates knee at 50% stretch and with 50% overlap but
capillary flow, and lowers capillary fluid leakage specific manufacturer’s instructions should be
thereby alleviating limb edema. It also softens followed for each bandage. Interface pressure
peaks on the leg during walking exceeding
lipodermatosclerosis, improves lymphatic flow
50-60 mm Hg reduce VR and increase venous
and function, and enhances fibrinolysis.[3]
pumping function. This may be achieved by
stiff compression textiles like multicomponent
Indications
bandages, especially when containing cohesive
The aim of compression therapy is to improve the
material or by zinc paste bandages. These
venous function without compromising arterial
compression types exert high stiffness which is
function.
characterized by a tolerable resting pressure and
high pressure peaks during walking (“working
Contraindications pressure”), but need to be applied by well trained
The contraindications of compression therapy and experienced staff. Short stretch adjustable
are the following[4,5] Velcro-wraps and (double) compression
Access this article online • Advanced peripheral obstructive arterial stockings may be promising alternatives allowing
Website: www.idoj.in disease (ankle brachial pressure index self-management.
DOI: 10.4103/2229-5178.137822 [ABPI] <0.8) (Evidence level A)
Quick Response Code: • Systemic arterial pressure <80 mm Hg at INTERMITTENT PNEUMATIC
ankle
COMPRESSION
• Phlegmasia cerulea dolens
• Uncontrolled congestive heart failure Intermittent pneumatic compression constitutes
• Abscesses inflating and deflating an airtight bag worn around
• Septic phlebitis leg. IPC controls edema in case compression
• Advanced peripheral neuropathy. bandage and stocking has failed. IPC upon
compression therapy may accelerate ulcer
Address for
correspondence:
CLASSIFICATION healing.[8] It is particularly useful in patients with
Dr. Brijesh Nair, restricted mobility and when concomitant arterial
Dermatologist, INHS Compression can be broadly divided into disease is detected, where it helps reduce edema
Sanjivani, bandages and compression stockings. The and enhance arterial blood flow.[9,10] IPC may
Kochi - 682 004, India. details are mentioned in Table 1. [6,7] The improvement in hematologic, hemodynamic
E-mail: meshugah12@ compression bandages can be classified as and endothelial effects which explains its role in
rediffmail.com
inelastic (short stretch bandages [SSB]) and healing of VLU.[11]
378 Indian Dermatology Online Journal - July-September 2014 - Volume 5 - Issue 3
Nair: Compression therapy for venous leg ulcers
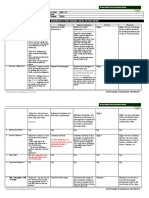
Table 1: Types of compression therapy
Compression system Advantages Disadvantages
Single component bandage Has only one layer/aspect. Since padding
layer is present in most systems, they
cannot be described as single component
Elastic wraps Inexpensive, can be re-used Applied incorrectly by patients, tends
E.g.: Elastocrepe to unravel, no sustained compression
delivered, lose elasticity on washing
Light support (crepe) For holding dressings in place, as a layer Pressures are too low for affectivity in
within multilayer bandage treating VLU. 40-60% pressure lost in first
20 min of application
Cohesive compression bandages Self-adherent but non adherent to Expensive, cannot be reused
E.g.: Tensoplus forte, coban skin, prevents slippage; provides light
support; useful over non adhesive
bandages like elastocrepe and paste
bandages, compression well sustained
Inelastic bandages (SSB) Bandages with minimal or no elastomers. Needs to be applied at full stretch
E.g.: Comprilan These bandages have low extensibility
and high stiffness. Low resting pressures
and high working pressures are delivered.
Patient comfort ensured
Inelastic paste bandages (Unnas boot) Cost effective. Comfortable. Protects Pressure changes over time, needs to be
against trauma, full ambulation status applied by trained physicians and nurses,
possible, minimal activity interference does not accommodate highly exudative
wounds, no leeway for fluctuating edema
Multilayered (four layered) bandaging Comfortable, can be left in place Needs to be applied by well trained
E.g.: Velfour for 7 days, protects against trauma, nurses/physicians
maintains constant pressure for 7 days,
High compression bandage system (SBP of used for highly exudative wounds,
35-40 mm Hg at the ankle) that incorporates pressure distribution is even, adequate
elastic layers to achieve sustained compression balance between resting/working
Layer 1 is orthopedic wool pressures, useful for bigger legs and
active patients
Layer 2 is a cotton crepe bandage
Layer 3 is a light weight elastic compression
bandage maintains SBP of 20 mm Hg at ankle
Layer 4 is a cohesive compression bandage
and it retains the bandage in position,
maintains a pressure of 30 mm Hg at the ankle
High elastic compression bandages (LSB) Sustained compression, can be worn up
E.g.: Tensopress, setopress, surepress to 1 week, can be washed and reused
Graduated compression stockings Reduces ambulatory venous pressure, Often cannot monitor patient compliance,
3 classes are available depending on the increases venous refilling time, improves difficult to put on, particularly arthritics;
desired degree of ankle pressure in mm of Hg calf pump function, different stocking lack of consensus on compression scales
types accommodate different legs,
Class I (18-21 mm Hg) dressings underneath can be changed
Indicated in mild varicosis, early varicosis in frequently, offers mid-level compression
pregnancy and heaviness of legs between elastic and inelastic bandage
systems
Class II (23-32 mm Hg)
Indicated in severe varicose veins, moderate
edema, pronounced varicosis in pregnancy,
post healing minor ulcerations, superficial
thrombophlebitis and post sclerotherapy
Class III (34-46 mm Hg)
For severe chronic venous insufficiency,
marked edema and induration of skin
IPC Useful as a solo and adjuvant, good Expensive, requires immobility for a few
Used in those who do not respond to tolerability in mixed arteriovenous hours/day; contraindicated in congestive
stockings or compression bandages ulcers, augments venous return, improve heart failure, inflammatory phlebitis
hemodynamics, microvascular functions,
Pressure is applied via a boot inflated by a enhances fibrinolysis, useful when other
machine either continuously, intermittently or modalities of compression fail, stiff
in sequential cycles ankle, edema and immobile patient
VLU: Venous leg ulcers, SBP: Sub bandage pressure, LSB: Long stretch bandages, IPC: Intermittent pneumatic compression, SSB: Short stretch bandages
Indian Dermatology Online Journal - July-September 2014 - Volume 5 - Issue 3 379
Nair: Compression therapy for venous leg ulcers
Table 2: Comparison between elastic (LSB) and Multicomponent multilayered compression is superior to a
inelastic compression bandages (SSB) single component, single layer compression bandage systems.
Elastic/active (long stretch) Inelastic/passive (short stretch)
Stretch provides pressure Movement of calf muscles
Inelastic versus elastic bandages (long stretch
provide pressure bandages vs. short stretch bandages)
Low stiffness High stiffness Two studies[17,18] demonstrated superiority of inelastic bandages
Self-applied Trained staff required in healing venous ulcers and reducing VR over elastic
Daytime use only Day and night use bandages. Short stretch compression (inelastic) and Unna’s
Pressures are less on walking Intermittent pressure peaks of boot was found to support the pump function better than a long
and low tolerability in resting 60-80 mm Hg during walking and stretch compression (elastic)[19,20] (evidence level A).
pressures tolerable resting pressure
Bandage pressure maintained Bandage pressure reduces by
for longer time 25% in first hour after application
Compression stockings
Use of a Class I or II stocking in patients with chronic venous
Standing increases pressure by 8 Standing increases pressure by 22
mm Hg, less working pressures, mm Hg; high working pressures, insufficiency (CVI) led to reduction in the lower leg volume of
more resting pressures no resting pressures 55-70 ml[14] (evidence level C).
Materials applied at lower Material applied at higher
tension tensions
Stockings (single layer/two-layer) versus bandages
Technique easy Technique determines success
A Cochrane review[4] identified two trials of compression
Contraindicated in arterial Can be used in moderate
bandages versus single layer compression stocking. No
insufficiency arterial insufficiency
difference was detected among single layer stocking when
LSB: Long stretch bandages, SSB: Short stretch bandages
compared to paste based bandages (Evidence level A). However
healing outcome was better when a two layered stocking was
HEAD-TO-HEAD COMPARISON BETWEEN
compared to SSB (evidence level A). A meta-analysis of eight
VARIOUS MODALITIES OF COMPRESSION heterogenous randomized-controlled clinical trials (RCTs)
concluded that stockings are better than compression
Compression versus no compression/usual care/simple bandages. There was better impact on pain, quicker healing
dressings by 3 weeks and increased ease of use with stockings[21]
Various guidelines have recommended that some compression (level of evidence B). Pain scores were better for compression
is better than no compression [12,13] (evidence level A). stockings than compression bandages[4,22] (level of evidence A).
A Cochrane review in 2009[4] (evidence level A) compared A well-chosen and correctly calibrated compression stocking
compression with either primary dressing, noncompressive exerting a pressure of 35 mm Hg or more is a good alternative
bandages and usual care that always did not include to bandages in healing VLU[23,24] (level of evidence B).
compression and concluded that venous ulcers healed faster
with compression and some form of compression is better than Compression and surgery
no compression in healing VLU. Multiple sources and studies have shown that selective
c o m p r e s s i o n e n h a n c e s s c l e r o t h e r a p y r e s u l t s [25,26]
High compression versus low compression (level of evidence B). A RCT compared subfascial endoscopic
High compression bandages provide and maintain high levels perforator surgery with ambulatory compression and concluded
of compression pressures in the range 25-35 mm Hg at the that healing rates and recurrence rates in both modalities of
ankle. High compression is useful for bigger legs or more active treatment were same. However, the study recommended a
patients. They can be used over padding on their own or as combination of both for optimal results[27] (level of evidence B).
part of a layered system, and should be applied in a spiral
according to manufacturer’s instructions. Evidence exists that Intermittent pneumatic compression with or without
high compression is better than low compression in managing compression versus compression alone
VLU[4,12-15] (evidence level A). Berliner et al.[28] (evidence level A) reviewed eight studies,
three of which showed that compression pumps could alleviate
Single component versus multicomponent bandage symptoms of CVI and assist with the healing of longstanding
systems and single layer versus multilayer chronic ulcerations. A systematic Cochrane review identified
Studies have emphasized the fact that multi-layering four trials of IPC + Compression versus compression alone
increases stiffness of bandages and increases sub bandage (Unnas boot/four layer dressing/stockings)[29] (evidence level A).
pressure (SBP), thereby being inelastic practically. It ensures Only one trial showed lesser time to heal and increased rate
even distribution of SBP[4,12,16] (evidence level A). SBP of 30-40 of reduction in ulcer area, although it could not identify any
mm Hg is recommended for healing of VLU (level of evidence A). difference in ulcer healing between the two groups. Further
380 Indian Dermatology Online Journal - July-September 2014 - Volume 5 - Issue 3
Nair: Compression therapy for venous leg ulcers
studies are required to assess the status of IPC as alternative/ vascular disease with intermittent pneumatic foot compression:
adjuvant to compression and to optimize cycle times and IPC A prospective controlled study with 1-year follow-up. J Vasc Surg
2000;31:650-61.
duration per day to effectively heal VLU.
11. Comerota AJ. Intermittent pneumatic compression: Physiologic and
clinical basis to improve management of venous leg ulcers. J Vasc Surg
Compression therapy modification in peripheral 2011;53:1121-9.
12. Fletcher A, Cullum N, Sheldon TA. A systematic review of compression
arterial disease
treatment for venous leg ulcers. BMJ 1997;315:576-80.
In patients with arterial occlusive disease (ABPI 0.6-0.8) 13. Cullum N, Nelson EA, Fletcher AW, Sheldon TA. Compression bandages
modified compression using stiff material applied with reduced and stockings for venous leg ulcers. Cochrane Database Syst Rev
pressure (<40 mm Hg) under careful control may increase 2000:CD000265.
both arterial flow and venous pumping function. Compression 14. Strolin A, Volkert B, Hafner HM, Junger M. Medical compression
decreases the elevated pressure within the venous system and stockings in CVI-Patients. Phlebologie 2005;34:34-41.
15. Amsler F, Blättler W. Compression therapy for occupational leg
may also increase arterial blood flow according to recent data symptoms and chronic venous disorders-a meta-analysis of randomised
in patients with mixed ulcers[30-35], (evidence level B). controlled trials. Eur J Vasc Endovasc Surg 2008;35:366-72.
16. Moffatt CJ, Franks PJ, Oldroyd M, Bosanquet N, Brown P,
Drawbacks of compression therapy Greenhalgh RM, et al. Community clinics for leg ulcers and impact on
healing. BMJ 1992;305:1389-92.
• Correct application of compression bandages need
17. Partsch H, Menzinger G, Mostbeck A. Inelastic leg compression is more
expertise effective to reduce deep venous refluxes than elastic bandages. Dermatol
• Older debilitated patients with comorbidities find it difficult Surg 1999;25:695-700.
to use compression stockings 18. Moody M. Comparison of Rosidal K and SurePress in the treatment of
• Peripheral vascular compromise in patients with venous leg ulcers. Br J Nurs 1999;8:345-55.
19. Partsch H. The static stiffness index: A simple method to assess the elastic
mixed-arterial venous ulcers with low ABPI
property of compression material in vivo. Dermatol Surg 2005;31:625-30.
• Reduced compliance due to wearer discomfort. 20. Polignano R, Bonadeo P, Gasbarro S, Allegra C. A randomised controlled
study of four-layer compression versus Unna’s Boot for venous ulcers.
CONCLUSION J Wound Care 2004;13:21-4.
21. Amsler F, Willenberg T, Blättler W. In search of optimal compression
therapy for venous leg ulcers: A meta-analysis of studies comparing
Compression therapy is a highly effective treatment for VLU. diverse [corrected] bandages with specifically designed stockings. J Vasc
Care should be taken while administering this therapeutic Surg 2009;50:668-74.
modality in case of mixed-arteriovenous ulcers. The minimum 22. Scriven JM, Taylor LE, Wood AJ, Bell PR, Naylor AR, London NJ.
tolerable compression pressure tailored to the patient’s A prospective randomised trial of four-layer versus short stretch
compression bandages for the treatment of venous leg ulcers. Ann R
requirement should be ensured so as to maximize compliance.
Coll Surg Engl 1998;80:215-20.
23. Kurz X, Kahn SR, Abenhaim L, Clement D, Norgren L, Baccaglini U,
REFERENCES et al. Chronic venous disorders of the leg: Epidemiology, outcomes,
diagnosis and management. Summary of an evidence-based report of the
1. Phillips TJ. Current approaches to venous ulcers and compression. VEINES task force. Venous insufficiency epidemiologic and economic
Dermatol Surg 2001;27:611-21. studies. Int Angiol 1999;18:83-102.
2. Abu-Own A, Scurr JH, Coleridge Smith PD. Effect of leg elevation on 24. Partsch H, Horakova MA. Compression stockings in treatment of lower
the skin microcirculation in chronic venous insufficiency. J Vasc Surg leg venous ulcer. Wien Med Wochenschr 1994;144:242-9.
1994;20:705-10. 25. Weiss RA, Sadick NS, Goldman MP, Weiss MA. Post-sclerotherapy
3. Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment compression: Controlled comparative study of duration of compression
of venous ulcers. Am J Surg 2004;188:1-8. and its effects on clinical outcome. Dermatol Surg 1999;25:105-8.
4. O’Meara S, Cullum NA, Nelson EA. Compression for venous leg ulcers. 26. Tazelaar DJ, Neumann HA, De Roos KP. Long cotton wool rolls as
Cochrane Database Syst Rev 2009:CD000265. compression enhancers in macrosclerotherapy for varicose veins.
5. Nelson EA, Harper DR, Prescott RJ, Gibson B, Brown D, Ruckley CV. Dermatol Surg 1999;25:38-40.
Prevention of recurrence of venous ulceration: Randomized controlled 27. van Gent WB, Hop WC, van Praag MC, Mackaay AJ, de Boer EM,
trial of class 2 and class 3 elastic compression. J Vasc Surg 2006;44:803-8. Wittens CH. Conservative versus surgical treatment of venous leg ulcers:
6. Choucair M, Phillips TJ. Compression therapy. Dermatol Surg A prospective, randomized, multicenter trial. J Vasc Surg 2006;44:563-71.
1998;24:141-8. 28. Berliner E, Ozbilgin B, Zarin DA. A systematic review of pneumatic
7. Morison MJ. A Colour Guide to the Nursing Management of Wounds. compression for treatment of chronic venous insufficiency and venous
London: Wolfe; 1992. ulcers. J Vasc Surg 2003;37:539-44.
8. Smith PC, Sarin S, Hasty J, Scurr JH. Sequential gradient pneumatic 29. Nelson EA, Mani R, Thomas K, Vowden K. Intermittent pneumatic
compression enhances venous ulcer healing: A randomized trial. Surgery compression for treating venous leg ulcers. Cochrane Database Syst
1990;108:871-5. Rev 2011:CD001899.
9. Eze AR, Comerota AJ, Cisek PL, Holland BS, Kerr RP, Veeramasuneni R, 30. Mosti G, Iabichella ML, Partsch H. Compression therapy in mixed ulcers
et al. Intermittent calf and foot compression increases lower extremity increases venous output and arterial perfusion. J Vasc Surg 2012;55:122-8.
blood flow. Am J Surg 1996;172:130-4. 31. Humphreys ML, Stewart AH, Gohel MS, Taylor M, Whyman MR,
10. Delis KT, Nicolaides AN, Wolfe JH, Stansby G. Improving walking Poskitt KR. Management of mixed arterial and venous leg ulcers. Br J
ability and ankle brachial pressure indices in symptomatic peripheral Surg 2007;94:1104-7.
Indian Dermatology Online Journal - July-September 2014 - Volume 5 - Issue 3 381
Nair: Compression therapy for venous leg ulcers
32. Grey JE, Harding KG, Enoch S. Venous and arterial leg ulcers. BMJ 35. Obermayer A, Göstl K, Partsch H, Benesch T. Venous reflux surgery
2006;332:347-50. promotes venous leg ulcer healing despite reduced ankle brachial
33. World Union of Wound Healing Societies Initiative (WUWHS) pressure index. Int Angiol 2008;27:239-46.
compression in venous leg ulcers. A consensus document. London: MEP
Ltd.; 2008.
34. Hopf HW, Ueno C, Aslam R, Burnand K, Fife C, Grant L, et al. Cite this article as: Nair B. Compression therapy for venous leg ulcers. Indian
Dermatol Online J 2014;5:378-82.
Guidelines for the treatment of arterial insufficiency ulcers. Wound
Source of Support: Nil, Conflict of Interest: Nil.
Repair Regen 2006;14:693-710.
382 Indian Dermatology Online Journal - July-September 2014 - Volume 5 - Issue 3
You might also like
- Fluid and Electrolyte ImbalancesDocument35 pagesFluid and Electrolyte Imbalancesmardsz95% (22)
- Protein Case SummaryDocument2 pagesProtein Case SummaryGlydenne Glaire Poncardas Gayam100% (2)
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Document12 pagesPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesNo ratings yet
- Ultrasound and clinically guided Injection techniques on the musculoskeletal systemFrom EverandUltrasound and clinically guided Injection techniques on the musculoskeletal systemNo ratings yet
- Water LoseDocument29 pagesWater LoseJAKLIN EMPOLNo ratings yet
- Intermittent Compression HandoutDocument42 pagesIntermittent Compression HandoutPaula ColeenNo ratings yet
- Advanced Textiles For Wound Compression 1Document24 pagesAdvanced Textiles For Wound Compression 1Ahsan NazirNo ratings yet
- Bandages and Bandaging Techniques For Compression Therapy: FocusDocument6 pagesBandages and Bandaging Techniques For Compression Therapy: FocuspakemainmainNo ratings yet
- Nursing Diagnosis (Ineffective Tissue Perfusion)Document1 pageNursing Diagnosis (Ineffective Tissue Perfusion)Therese Melchie SantuyoNo ratings yet
- B. Caso Clinico. Turchin, I., & Barankin, B. 2006. Dermacase. Chronic Venous Insufficiency.Document3 pagesB. Caso Clinico. Turchin, I., & Barankin, B. 2006. Dermacase. Chronic Venous Insufficiency.Alex Andrés Cuevas UrriolaNo ratings yet
- NCPDocument5 pagesNCPMcmc Ryan Ferdinand GutierrezNo ratings yet
- Physical Agents Pentru Modificare 9.pintea 407-431Document23 pagesPhysical Agents Pentru Modificare 9.pintea 407-431PAE PAENo ratings yet
- Mahogany St. Rabe Subdivision, Tagum City Bachelor of Science in NursingDocument4 pagesMahogany St. Rabe Subdivision, Tagum City Bachelor of Science in NursingRoel John Atamosa CasilacNo ratings yet
- Cryotherapy: When, Why and HowDocument2 pagesCryotherapy: When, Why and HowRestu AryaNo ratings yet
- Nursing Care Plan: Priority No. 2Document2 pagesNursing Care Plan: Priority No. 2Pantaleon PacisNo ratings yet
- NL Handout 2013-03-05 PDFDocument21 pagesNL Handout 2013-03-05 PDFsilkofosNo ratings yet
- NMT Lymphatic Introduction English 2024Document64 pagesNMT Lymphatic Introduction English 2024Wahyu Hidayat Bin SidijantoNo ratings yet
- Principles and Techniques of Tendon and Ligament Repair: Jay D. Ryan, DPMDocument5 pagesPrinciples and Techniques of Tendon and Ligament Repair: Jay D. Ryan, DPMWadezigNo ratings yet
- Exercises MYTH 1 To 4Document6 pagesExercises MYTH 1 To 4alejandra sandovalNo ratings yet
- 675 FullDocument3 pages675 FullzoreNo ratings yet
- A Study On Effectiveness of Low Level Laser Therapy and Mcconnell Taping in Subjects With Infrapatellar BursistisDocument4 pagesA Study On Effectiveness of Low Level Laser Therapy and Mcconnell Taping in Subjects With Infrapatellar BursistisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Rosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NerveDocument4 pagesRosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NervedanielpohlmanNo ratings yet
- Compartment Syndrome: It Occurs When Excessive Pressure Builds Up Inside An Enclosed Muscle Space in The BodyDocument1 pageCompartment Syndrome: It Occurs When Excessive Pressure Builds Up Inside An Enclosed Muscle Space in The BodyRachelle Ann CarilloNo ratings yet
- 1 BASIC CARE AND COMFORT BCC 21-Day Course 2023 - ExpiresDocument31 pages1 BASIC CARE AND COMFORT BCC 21-Day Course 2023 - ExpiresCALEB K. SAMBAINo ratings yet
- Bases de La MasoterapiaDocument4 pagesBases de La MasoterapiaSergio Andres ZeitgeistNo ratings yet
- Fascial Distortion Model - Vol.2Document62 pagesFascial Distortion Model - Vol.2Magno FilhoNo ratings yet
- Practical Guide To Joint and Soft Tissue Injection TechniquesDocument5 pagesPractical Guide To Joint and Soft Tissue Injection TechniquesHerry HendrayadiNo ratings yet
- The Pneumatic Tourniquet Mechanical,.5Document8 pagesThe Pneumatic Tourniquet Mechanical,.5Alejandro Pesqueira BojorquezNo ratings yet
- Volkmann's Ischaemic Contracture: January 2015Document21 pagesVolkmann's Ischaemic Contracture: January 2015Siti novizahNo ratings yet
- Compression Textiles 6018Document12 pagesCompression Textiles 6018aqsa imranNo ratings yet
- Skeletal and Skin TractionDocument38 pagesSkeletal and Skin TractionCORROS JASMIN MARIE100% (1)
- Bandaging: Respect For Living TissuesDocument5 pagesBandaging: Respect For Living Tissuesim. EliasNo ratings yet
- Fractures and Compartment SyndromeDocument4 pagesFractures and Compartment SyndromeTom MallinsonNo ratings yet
- Transverse Friction MassageDocument4 pagesTransverse Friction MassageNotCarlos TheJeda100% (1)
- Small Incision Total Hip Replacement by The Lateral Approach Using Standard InstrumentsDocument5 pagesSmall Incision Total Hip Replacement by The Lateral Approach Using Standard InstrumentsApolinar González HernándezNo ratings yet
- Kinesio TapeDocument1 pageKinesio Tapeapi-435929154No ratings yet
- Qindeel Fatima Ankle Sprain TreatmentDocument19 pagesQindeel Fatima Ankle Sprain TreatmentQindeel FatimaNo ratings yet
- Use Only: Pressure Therapy For Post-Burn Scars: Does It Work?Document2 pagesUse Only: Pressure Therapy For Post-Burn Scars: Does It Work?Anonymous 2ETFXiNo ratings yet
- Template Review Paper - XLSX - IVTDocument1 pageTemplate Review Paper - XLSX - IVTputriikurniawati23No ratings yet
- NCP604Document2 pagesNCP604Dorice AchiengNo ratings yet
- Knee Exam v01Document4 pagesKnee Exam v01Achmad Harun MuchsinNo ratings yet
- Cyriax's Friction MassageDocument23 pagesCyriax's Friction MassageKrinal ShahNo ratings yet
- Pitting and Non-Pitting Oedema: Clinical SkillsDocument3 pagesPitting and Non-Pitting Oedema: Clinical SkillsDinnar Ulya FauziahNo ratings yet
- Al-Quds University: Students NameDocument75 pagesAl-Quds University: Students Namebayan salahNo ratings yet
- Kinesio GoldDocument9 pagesKinesio GoldHenrique AthadeuNo ratings yet
- Traction : LumbarDocument10 pagesTraction : LumbarAkshaya MistryNo ratings yet
- J S T A I (A) : Oint and Oft Issue Spiration and Njection RthrocentesisDocument19 pagesJ S T A I (A) : Oint and Oft Issue Spiration and Njection RthrocentesisSgantzos MarkosNo ratings yet
- Nursing Care Plans For Cruris Fracture: Case 1Document9 pagesNursing Care Plans For Cruris Fracture: Case 1susanti santaliaNo ratings yet
- Nursing Care Plan and FdarDocument6 pagesNursing Care Plan and FdarCheska YsabelleNo ratings yet
- Lymphedema 2Document13 pagesLymphedema 2Anurag ThakurNo ratings yet
- 9 Intrinsic Contracture of The HandDocument6 pages9 Intrinsic Contracture of The HandjcNo ratings yet
- Toorthj 8 185Document10 pagesToorthj 8 185fatimah putriNo ratings yet
- Artrocenseis - Libro de Reumato en InglesDocument15 pagesArtrocenseis - Libro de Reumato en InglesPabloNo ratings yet
- Pressure Ulcer 2Document26 pagesPressure Ulcer 2birkbrunNo ratings yet
- Multi Layer Compression System Brochure CarolonDocument2 pagesMulti Layer Compression System Brochure Carolonkemaw20100No ratings yet
- TheraDocument2 pagesTheraolliston.ellieNo ratings yet
- Brainstorming Pasos Instrucciones Corporativo Profesional Rojo Amarillo AzulDocument1 pageBrainstorming Pasos Instrucciones Corporativo Profesional Rojo Amarillo AzulNoris GonzálezNo ratings yet
- Prepration, Assisting and After Care of PatientsDocument24 pagesPrepration, Assisting and After Care of PatientsLaxmi SinghNo ratings yet
- Mar2012 CC NoyesDocument17 pagesMar2012 CC NoyesJavierLarenasNo ratings yet
- Pt in ReconstructiveDocument14 pagesPt in Reconstructiveprd7vkbqsbNo ratings yet
- Mod. 4 (Part 2) - Sports MedicineDocument17 pagesMod. 4 (Part 2) - Sports Medicineadrian kristopher dela cruzNo ratings yet
- Ncp-Case Pre Impaired Tissue Integrity-1Document2 pagesNcp-Case Pre Impaired Tissue Integrity-1Jade HemmingsNo ratings yet
- Annsurg00058 0041Document3 pagesAnnsurg00058 0041tvxtvq2f6wNo ratings yet
- Compartment Syndrome: Citra Ahdi Prasetya, Dr. SpotDocument33 pagesCompartment Syndrome: Citra Ahdi Prasetya, Dr. SpotTeye OntiNo ratings yet
- MTC 1 Basic Course 2014 PDFDocument96 pagesMTC 1 Basic Course 2014 PDFАнна ПуховаNo ratings yet
- Comparative Assessment of Flap-Advancing TechniquesDocument9 pagesComparative Assessment of Flap-Advancing Techniques李潮忠No ratings yet
- Gordon'S Functional Health PatternDocument10 pagesGordon'S Functional Health PatternDave SapladNo ratings yet
- CHF Patient Education Booklet English WebDocument20 pagesCHF Patient Education Booklet English WebBelete NigusieNo ratings yet
- Calvin Damanik, DR, SPPD: Departement Penyakit Dalam Fak Kedokteran Umi MedDocument37 pagesCalvin Damanik, DR, SPPD: Departement Penyakit Dalam Fak Kedokteran Umi MedMaria lestari harianjaNo ratings yet
- Nimesil PDFDocument5 pagesNimesil PDFTemur LegendaryNo ratings yet
- NCP For Nephrotic SyndromeDocument2 pagesNCP For Nephrotic SyndromeLee Jenny100% (5)
- PH Protocol For Nephrotic SyndromeDocument4 pagesPH Protocol For Nephrotic Syndromeprachi100% (1)
- Kati Sriwiyati, Dr. Bagian Fisiologi FK UnswagatiDocument52 pagesKati Sriwiyati, Dr. Bagian Fisiologi FK UnswagatiMelia100% (1)
- Rosenberg, Disease in HistoryDocument16 pagesRosenberg, Disease in Historyhector3nu3ezNo ratings yet
- Hydrocollator, Whirlpool Tank + Parrafin 1st Lecture PPT 2Document47 pagesHydrocollator, Whirlpool Tank + Parrafin 1st Lecture PPT 2Mustafa MabroukNo ratings yet
- Pedal EdemaDocument45 pagesPedal Edemafirdaushassan2112No ratings yet
- Note of Clinical Surgery - Dr-HassebDocument92 pagesNote of Clinical Surgery - Dr-HassebruchikaNo ratings yet
- Medicine All DIagnosis by AVI SeriesDocument8 pagesMedicine All DIagnosis by AVI SeriesMuhammad Awais Hassan AwaanNo ratings yet
- Venosmil Technical NformationDocument6 pagesVenosmil Technical NformationTheo HemagiriNo ratings yet
- Orthopedic Case Proformas-1Document19 pagesOrthopedic Case Proformas-1md maaz100% (1)
- Medical Nutrition Therapy A Case Study Approach 5Th Edition Nelms Solutions Manual Full Chapter PDFDocument29 pagesMedical Nutrition Therapy A Case Study Approach 5Th Edition Nelms Solutions Manual Full Chapter PDFStephanieMckayeqwr100% (10)
- Exam Ticket Number Wise CaseDocument37 pagesExam Ticket Number Wise CaseVikrantNo ratings yet
- Marasmus Kwashiorkor 12022009Document62 pagesMarasmus Kwashiorkor 12022009Ardie Ceme ThedoctorNo ratings yet
- Nephrotic Syndrome HistoryDocument7 pagesNephrotic Syndrome HistorySouvori ChandaNo ratings yet
- HC Compression DeviceDocument2 pagesHC Compression DeviceTahir YousafNo ratings yet
- Liver Pathophysiology and Schematic DiagramDocument1 pageLiver Pathophysiology and Schematic DiagramCyrus De Asis100% (4)
- Test Bank For Business and Society Stakeholders Ethics Public Policy 14Th Edition by Lawrence Weber Isbn 9780078029479 0078029473 Full Chapter PDFDocument30 pagesTest Bank For Business and Society Stakeholders Ethics Public Policy 14Th Edition by Lawrence Weber Isbn 9780078029479 0078029473 Full Chapter PDFmary.meyer123100% (12)
- 216 Miracle Acupunture Points: ShavoshangDocument12 pages216 Miracle Acupunture Points: Shavoshangடைகர் தேவாNo ratings yet
- THIAZIDES and Thiazide Like MedicationsDocument5 pagesTHIAZIDES and Thiazide Like MedicationsIrene Grace BalcuevaNo ratings yet
- Anthonela - Terán SebastiánDocument5 pagesAnthonela - Terán SebastiánJuleyssiNo ratings yet