Professional Documents
Culture Documents
fimmu-12-800029
fimmu-12-800029
Uploaded by
anaclarapuzzellaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
fimmu-12-800029
fimmu-12-800029
Uploaded by
anaclarapuzzellaCopyright:
Available Formats
ORIGINAL RESEARCH
published: 02 February 2022
doi: 10.3389/fimmu.2021.800029
Evaluation of Oropharyngeal
Dysphagia in Older Patients for
Risk Stratification of Pneumonia
Tai-Han Lin 1, Chih-Wei Yang 2 and Wei-Kuo Chang 2*
1Department of Pathology and Graduate Institute of Pathology and Parasitology, Tri-Service General Hospital, National
Defense Medical Center, Taipei, Taiwan, 2 Division of Gastroenterology, Department of Internal Medicine, Tri-Service General
Hospital, National Defense Medical Center, Taipei, Taiwan
Objective: Nasogastric tube (NGT) and percutaneous endoscopic gastrostomy (PEG)
are widely used techniques to feed older patients with oropharyngeal dysphagia.
Aspiration pneumonia is the most common cause of death in these patients. This study
aimed to evaluate the role of oropharyngeal dysphagia in older patients on long-term
enteral feeding for risk stratification of pneumonia requiring hospitalization.
Methods: We performed modified flexible endoscopic evaluation of swallowing to
evaluate oropharyngeal dysphagia in older patients and conducted prospective follow-
up for pneumonia requiring hospitalization. A total of 664 oral-feeding patients and 155
tube-feeding patients were enrolled. Multivariate Cox analysis was performed to identify
Edited by:
Jianhua Wu, risk factors of pneumonia requiring hospitalization.
University of Leeds, United Kingdom
Results: Multivariate analyses showed that the risk of pneumonia requiring hospitalization
Reviewed by:
Peng Li,
significantly increased in older patients and in patients with neurological disorders, tube
Guangzhou Institutes of Biomedicine feeding, and oropharyngeal dysphagia. Subgroup analysis revealed that the risk of
and Health (CAS), China
pneumonia requiring hospitalization was significantly lower in patients with PEG than in
Robert Sawyer,
Western Michigan University, those with NGT among the patients with oropharyngeal dysphagia (adjusted hazard ratio
United States 0.26, 95% confidence interval: 0.11–0.63, P = 0.003).
*Correspondence:
Wei-Kuo Chang
Conclusions: For older patients with oropharyngeal dysphagia requiring long-term
weikuohome@hotmail.com enteral tube feeding, PEG is a better choice than NGT. Further research is needed to
elucidate the role of oropharyngeal dysphagia in enteral feeding in older patients.
Specialty section:
This article was submitted to Keywords: older patients, oropharyngeal dysphagia, aspiration pneumonia, percutaneous endoscopic
Nutritional Immunology, gastrostomy, nasogastric tube, tube feeding, enteral feeding
a section of the journal
Frontiers in Immunology
Received: 22 October 2021
Accepted: 27 December 2021
INTRODUCTION
Published: 02 February 2022
Population aging is a global issue, and it is estimated that the older population will reach approximately
Citation: 1.5 billion in 2050 (1). Degeneration and multiple comorbidities accompany as people age, and
Lin T-H, Yang C-W and Chang W-K
approximately 13%–81% of older patients are affected by oropharyngeal dysphagia (1–4). This
(2022) Evaluation of Oropharyngeal
Dysphagia in Older Patients for Risk
condition is common particularly in patients with neurological disorders (3, 4). Patients with
Stratification of Pneumonia. oropharyngeal dysphagia may require enteral tube feeding if they cannot meet their nutritional needs
Front. Immunol. 12:800029. orally (5). Such patients may face greater socioeconomic issues as the prevalence rates of stroke,
doi: 10.3389/fimmu.2021.800029 dementia, and esophageal motility disorder increase with older age (4, 6, 7).
Frontiers in Immunology | www.frontiersin.org 1 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
The two commonly used methods of enteral tube feeding are stratification of pneumonia requiring hospitalization in older
nasogastric tube (NGT) and percutaneous endoscopic gastrostomy patients on long-term enteral feeding.
(PEG) (8). Aspiration pneumonia is the most common cause of
death in these patients with enteral tube feeding (9, 10), with
estimated incidence rates of 12%–87% for NGT (11–15) and 9%–
52% for PEG (12–15). At present, NGT is recommended for
MATERIALS AND METHODS
temporary enteral nutrition lasting less than 4 weeks, whereas Patients
PEG is recommended for cases longer than 4 weeks (16). We performed modified FEES in older patients who received
However, in Asian counties, NGT is more frequently selected enteral feeding between January 2015 and July 2020.
than PEG for long-term enteral feeding. Possible explanations for Additionally, we conducted a prospective follow-up of those
this choice include refusal of interventional surgical procedures by requiring hospital admission due to pneumonia. The study was
the patient’s family due to considering patients has already been approved by the institutional review board of the Tri-Service
tortured by long-term morbidity or disability, desire to follow the General Hospital, No: 2-108-05-136. The participants provided
custom of maintaining the “whole corpse” for burial purposes, and written informed consent.
concerns related to complications after the PEG procedure (17–19).
The risks of aspiration pneumonia in older patients rise
significantly with oropharyngeal dysphagia (20, 21). Meta-analyses
Study Design
Of the 2,923 patients who underwent modified FEES to evaluate
have not conclusively determined whether oropharyngeal dysphagia
oropharyngeal dysphagia (Figure 1), 2,031 were excluded
is a risk for aspiration pneumonia in older patients on enteral
because they were below 65 years of age, 39 were excluded
feeding and whether PEG is better than NGT (15, 22). However, this
because modified FEES provided a poor pharyngolaryngeal view,
may be due to the high level of statistical heterogeneity among
and 34 were excluded for missing demographic profile data. Of
analyzed studies. Therefore, oropharyngeal dysphagia should be
the remaining 819 older patients who required enteral feeding for
evaluated and subgroup analysis regarding the risk of pneumonia in
more than 4 weeks, 664 were enrolled in the oral-feeding group
older patients on long-term enteral feeding, especially in regions in
and 155 in the tube-feeding group.
favor or NGT over PEG, should be performed.
Flexible endoscopic evaluation of swallowing (FEES) is a well-
documented standard method for evaluating oropharyngeal Demographic and Clinical Data
dysphagia (23, 24). This method allows assessment of aspiration We recorded the demographic and clinical profiles, such as age,
risk by direct visualization of test material accumulating in the gender, body mass index, reasons for enteral feeding, and
pharyngolaryngeal region or entering the vocal cords (23–26); pneumonia requiring admission. Reasons for enteral feeding
however, adverse events such as epistaxis, vasovagal response, and were categorized into two groups according to whether the
laryngospasm can develop during the procedure (27). Furthermore, patient had any neurological disorder, such as Alzheimer’s
this method can only be performed if the patient has adequate disease, dementia, Parkinson’s disease, or stroke.
physical and cognitive function to cooperate with degulgitation, and
thus cannot be properly applied in patients with advanced Modified Flexible Endoscopic Evaluation
neurological diseases such as dementia, Parkinson’s disease, or of Swallowing
stroke (24–26). In contrast, a modified version of FEES that Patients fasted for at least 4 hours before UGI endoscopic
involves additional pharyngolaryngeal examination during upper examination and were placed in the left lateral decubitus
gastrointestinal (UGI) endoscopy is easy and bearable to patients, position (24, 33). The endoscope tip was inserted through a
and may thus help in stratifying the severity of oropharyngeal mouthpiece with its axis aligned with that of the patient’s
dysphagia according to the pooling of secretions in the esophagus. The endoscope was advanced along the palate
pharyngolaryngeal region (24). midline, rotated slightly, and gently advanced past the uvula
Aspiration pneumonia could develop if aspiration of potential with anterior flexion to visualize the pyriform sinus, laryngeal
pathogenic gastric contents or oropharyngeal secretions into the vestibule, vocal cords, and upper part of the trachea (Figure 2A).
larynx or respiratory tract, which is common in older adults with The examination result was recorded using a digital video
dysphagia (28). As more residues in the pharyngolaryngeal region recorder (HVO-550MD; Sony, Tokyo, Japan) for later analysis
were reported in those with NGT due to NGT passes through the and was reviewed frame by frame in slow motion by two
upper esophageal sphincter (29–32), we hypothesized that endoscopists (WKC and CWY).
oropharyngeal dysphagia significantly increased the risk of
pneumonia requiring hospitalization in older patients with NGT, Evaluation of Oropharyngeal Dysphagia
and that PEG is recommended in preference to NGT for patients When patients are placed in the left lateral decubitus position
with oropharyngeal dysphagia requiring long-term tube feeding. during examination, the accumulated secretions may fill the
Previous studies primarily focused on the utility of FEES in lowest area of the right side of the pyriform sinus, leak into the
evaluating the risk of aspiration pneumonia in patients with oral left side of the pyriform sinus, or flow into the laryngeal vestibule
feeding, whereas studies examining the utility of FEES in evaluating or vocal cords (24). Swallowing frequency is estimated to be
the risks in NGT- and PEG-feeding patients remain limited. This about 600 times per day under normal physiological conditions
study aimed to evaluate the role of oropharyngeal dysphagia for risk (34). In most patients, no pooling or minimal pooling of
Frontiers in Immunology | www.frontiersin.org 2 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
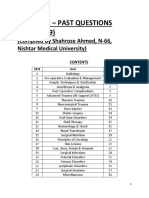
FIGURE 1 | Patient selection flow chart.
secretions in the pharyngolaryngeal region was observed under (24, 35). The pooling of secretions in the pyriform sinus was
endoscopy; occasionally, thin, watery secretions or clear bubbles quantified as follows: minimal, < 25%; moderate, 25%–50%; and
were observed in the pharyngolaryngeal region (24, 25). large, > 50% secretions filling the pyriform sinuses. Endoscopic
Oropharyngeal dysphagia was evaluated according to the evidence of oropharyngeal dysphagia was divided into two
amount and location of accumulated secretions observed categories: (1) absence of oropharyngeal dysphagia (< 25%
endoscopically in the pharyngolaryngeal region (Figure 2) pooled secretions filling the pyriform sinus, Figure 2A) and (2)
FIGURE 2 | Endoscopic views of pooled secretions (arrow) in the pharyngolaryngeal region. Absence of secretions filling the pharyngolaryngeal region (A). A large
amount of pooled secretions in the right side of the pyriform sinus but not entering the laryngeal vestibule (B), and pooled secretions leaking into the laryngeal vestibule (C).
Frontiers in Immunology | www.frontiersin.org 3 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
presence of oropharyngeal dysphagia (> 25% pooled secretions with older ages (with each year of age increase, adjusted HR 1.03,
filling the pyriform sinus, Figure 2B; or pooled secretions 95% CI 1.01–1.06, p = 0.004), neurological disorders (adjusted
entering the laryngeal vestibule, Figure 2C) (24, 35). HR 2.39, 95% CI: 1.49–3.84, P < 0.001), tube feeding (adjusted
HR 2.57, 95% CI: 1.61–4.12, P < 0.001), and oropharyngeal
Diagnosis of Pneumonia dysphagia (adjusted HR 1.59, 95% CI: 1.02–2.47, P =
Pneumonia was diagnosed based on radiological evidence of 0.041) (Table 2).
pulmonary consolidation, shortness of breath, body temperature
above 38°C, serum white blood cell count > 10,000/mm3, and the Subgroup Analysis: Presence Versus
requirement for hospitalization within 2 years after the patient Absence of Oropharyngeal Dysphagia
was enrolled (36). Subgroup analysis was conducted for patients on enteral feeding
based on whether the patients had oropharyngeal dysphagia
Statistical Analysis (Figure 3A). Presence of oropharyngeal dysphagia significantly
Statistical analyses were performed using SPSS Statistics 22.0 increased the risk of pneumonia in patients with enteral
(IBM Inc., Armonk, NY, USA) with a two-sided significance feeding (adjusted HR 1.59, 95% CI: 1.02–2.47, P = 0.041).
level of 5%. Parametric continuous data were compared using the However, it did not increase the risk in patients with oral
independent t-test. Categorical data were compared using the feeding (adjusted HR 1.63, 95% CI: 0.68–3.88, P = 0.274) and
Chi-square test or Fisher’s exact test. A univariate and in patients with tube feeding (adjusted HR 1.54, 95% CI: 0.91–
multivariate Cox regression model was applied to determine 2.62, P = 0.109).
the association between the clinical-demographic profile and
developing pneumonia. The hazard ratio (HR) for pneumonia Subgroup Analysis: PEG Versus NGT
development was estimated via multivariate analysis using the The risk of pneumonia showed no significant difference between
Cox proportional hazards model after adjusting the statistically PEG and NGT in all tube-feeding patients (adjusted HR 0.58,
significant variables in the univariate analysis as potential 95% CI: 0.32–1.04, P = 0.070). We conducted subgroup analysis
confounding factors. Survival curves were plotted with the for all enteral feeding patients with tube feeding based on the
Kaplan–Meier method. presence of NGT or PEG long-term feeding (Figure 3B). The
risk of pneumonia was not significantly different between PEG
and NGT (adjusted HR 1.57, 95% CI: 0.71–3.45, P = 0.261) in
RESULTS patients with absence of oropharyngeal dysphagia; however, the
risk of pneumonia was significantly lower in PEG than NGT in
Patient Characteristics patients with presence of oropharyngeal dysphagia (adjusted HR
A total of 819 older patients were enrolled in this study, with 664 0.26, 95% CI: 0.11–0.63, P = 0.003).
in the oral-feeding group and 155 in the tube-feeding group.
Patient characteristics are shown in Table 1. The mean age was Cumulative Proportion of Pneumonia
76.4 ± 7.5 years in the oral-feeding group and 78.5 ± 8.9 years in Requiring Admission
the tube-feeding group. Significant differences in age, sex, body Kaplan–Meier analysis indicated that the cumulative proportion
mass index, reasons for enteral feeding, and oropharyngeal of pneumonia was significantly increased in patients with tube
dysphagia were observed between the two groups. feeding compared with oral feeding (P < 0.001) (Figure 4A).
When subgroup analysis patients had absence of oropharyngeal
Risk Factors for Pneumonia Requiring dysphagia, the cumulative proportion of pneumonia was not
Hospitalization significantly different between PEG and NGT (P = 0.425)
Multivariate analyses showed that the risk of pneumonia (Figure 4B). However, when subgroup analysis patients had
requiring hospitalization was significantly increased in patients presence of oropharyngeal dysphagia, the cumulative proportion
TABLE 1 | Patients characteristics.
Variable Oral feeding (n = 664) Tube feeding (n = 155) P Value
Age (years) 76.4 ± 7.5 78.5 ± 8.9 0.006
Sex 0.001
Female 349 (52.6%) 58 (37.4%)
Male 315 (47.4%) 97 (62.6%)
Body mass index (kg/m2) 23.6 ± 3.8 21.9 ± 3.6 <0.001
Reasons for enteral feeding, no. (%) <0.001
Neurological disorders 135 (20.3%) 118 (76.1%)
Non-neurological disorders 529 (79.7%) 37 (23.9%)
Oropharyngeal dysphagia, no. (%) <0.001
Absence 613 (92.3%) 96 (61.9%)
Presence 51 (7.7%) 59 (38.1%)
Frontiers in Immunology | www.frontiersin.org 4 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
TABLE 2 | Multivariable analysis of the factors associated with pneumonia.
Variable With pneumonia (n = 113) Without pneumonia (n = 706) Crude HR (95% CI) P value Adjusted HR (95% CI) P value
Age (years) 79.8 ± 8.7 76.3 ± 7.6 1.06 (1.03–1.08) <0.001 1.03 (1.01–1.06) 0.004
Sex, no. (%)
Female 45 (39.8%) 362 (51.3%) Reference Reference
Male 68 (60.2%) 344 (48.7%) 1.57 (1.08–2.29) 0.018 1.22 (0.83–1.79) 0.302
Body mass index (kg/m2) 22.5 ± 3.9 23.4 ± 3.8 0.95 (0.90–0.99) 0.03 0.99 (0.94–1.05) 0.842
Reasons for enteral feeding, no. (%)
Non-neurological disorders 38 (33.6%) 528 (74.8%) Reference Reference
Neurological disorders 75 (66.4%) 178 (25.2%) 4.92 (3.33–7.27) <0.001 2.39 (1.49–3.84) <0.001
Enteral feeding, no. (%)
Oral feeding 53 (46.9%) 611 (86.5%) Reference Reference
Tube feeding 60 (53.1%) 95 (13.5%) 5.53 (3.82–8.01) <0.001 2.57 (1.61–4.12) <0.001
Oropharyngeal dysphagia, no. (%)
Absence 77 (68.1%) 632 (89.5%) Reference Reference
Presence 36 (31.9%) 74 (10.5%) 3.61 (2.43–5.37) <0.001 1.59 (1.02–2.47) 0.041
HR, hazard ratio; CI, confidence interval.
of pneumonia was significantly decreased in patients with PEG disorders, tube feeding, and oropharyngeal dysphagia were
compared with NGT (P = 0.001) (Figure 4C). associated with an increased risk of pneumonia requiring
hospitalization; (2) oropharyngeal dysphagia significantly
increased the risk of pneumonia in patients on long-term
DISCUSSION enteral feeding; (3) pneumonia significantly decreased in
patients with PEG compared to those with NGT among the
This was a prospective study of older patients requiring long- patients with oropharyngeal dysphagia. The implication of this
term enteral tube feeding in a tertiary care center. We found that study is that the evaluation of oropharyngeal dysphagia is crucial
(1) multivariate analyses showed that older ages, neurological for older patients on long-term enteral feeding. In older patients
FIGURE 3 | Subgroup analysis of risk of pneumonia requiring admission in older patients with enteral feeding. (A) Based on whether the patients had oropharyngeal
dysphagia, the risk of pneumonia requiring hospitalization increased significantly in overall enteral feeding patients, but not in oral-feeding and tube-feeding patients.
(B) Based on the type of tube feeding, PEG did not decrease the risk of pneumonia requiring hospitalization in the overall tube-feeding patients and patients without
oropharyngeal dysphagia, but the risk was reduced significantly in patients with oropharyngeal dysphagia.
Frontiers in Immunology | www.frontiersin.org 5 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
B C
FIGURE 4 | Kaplan–Meier curves for the cumulative proportion of pneumonia requiring hospital admission in older patients. (A) Cumulative proportion of pneumonia
in older patients for tube-feeding and oral-feeding group. (B) Cumulative proportion of pneumonia in older patients without oropharyngeal dysphagia for nasogastric
tube (NGT) and percutaneous endoscopic gastrostomy (PEG) groups. (C) Cumulative proportion of pneumonia in older patients with oropharyngeal dysphagia for
NGT and PEG groups.
with oropharyngeal dysphagia, PEG is a better choice than NGT of pneumonia requiring hospitalization was significantly higher
for long-term enteral tube feeding. in older patients (with each year of age increase, adjusted HR
1.03, 95% CI 1.01–1.06, P = 0.004) and in patients with
Evaluation of Oropharyngeal Dysphagia neurological disorders (adjusted HR 2.39, 95% CI: 1.49–3.84,
Detailed history-taking, physical examination, and FEES are P < 0.001). Oropharyngeal dysphagia is associated with increased
important for evaluating oropharyngeal dysphagia (37), risk of aspiration pneumonia or death (42, 43). The risk of
and evaluation of oropharyngeal dysphagia is recommended in pneumonia requiring hospitalization also increased significantly
patients requiring long-term enteral feeding (33, 38, 39). Digital in patients with oropharyngeal dysphagia (adjusted HR 1.59,
video recording systems can aid in overcoming the limitations of 95% CI: 1.02–2.47, P = 0.041) in the multivariate analyses in the
conventional UGI endoscopy for pharyngolaryngeal examination current study. If oropharyngeal dysphagia is suspected in older
due to limited photographic recording within a short observation patients, referral to a physician or speech therapist is warranted
period (24, 40). Furthermore, the recorded video can facilitate the (44). A multidisciplinary team should develop a management
evaluation of oropharyngeal dysphagia by recording protective plan to monitor, assess, and prevent aspiration pneumonia in
cough reflex, vocal cord adduction, and movements for clearing patients receiving long-term enteral feeding who are at risk of
secretions during the process (24, 40). Although a swallowing test oropharyngeal aspiration (5, 45). The development of
was not conducted as a part of the traditional methodology of malnutrition might be related to reduced swallowing function
FESS due to the patient characteristics (23–26), we were able to due to oropharyngeal dysphagia (20, 46), and further
stratify the groups with higher pneumonia risk using modified deterioration of laryngeal muscle might lead to a vicious cycle
FESS with UGI endoscopy through the direct visualization of the (20, 46). Effective swallowing function and salivary flow are
pharyngolaryngeal region. crucial for the clearance of most oropharyngeal pathogens in
healthy individuals (47), whereas reduced mechanical clearance
Older Patients With Oropharyngeal might be associated with oropharyngeal residue or bacterial
Dysphagia colonization (46, 47). Aspiration pneumonia could develop due
Deterioration in neural control and structural alteration of the to pulmonary aspiration induced by impaired swallowing
pharyngeal region can lead to swallowing difficulties (41), which function, particularly if the aspirated material contains an
can gradually worsen with increasing age of people (3, 4, 6, 7). In abundant bacterial load or in the presence of impaired
the current study, the multivariate analyses revealed that the risk mechanical or immune defense mechanism (48).
Frontiers in Immunology | www.frontiersin.org 6 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
Tube Feeding in Older Patients With possible confounders (58). However, to the best of our
Oropharyngeal Dysphagia knowledge, the present study is the first prospective study
Tube feeding is associated with a higher risk of aspiration designed to evaluate the optimal choice of long-term tube
pneumonia compared to oral feeding (32, 49), and our study feeding in older patients with oropharyngeal dysphagia.
showed similar results (adjusted HR 2.57, 95% CI: 1.61–4.12, P <
0.001) under multivariate analysis. Although PEG has not shown
more favorable outcomes compared to NGT in meta-analyses CONCLUSIONS
(15, 22), subgroup analysis in this study demonstrates that the
risk of pneumonia was significantly reduced in PEG compared to Despite the limitations, this study shows that oropharyngeal
NGT in older patients with oropharyngeal dysphagia (adjusted dysphagia significantly increased the risk of pneumonia
HR 0.26, 95% CI: 0.11–0.63, P = 0.003), but not in patients requiring hospitalization in older patients with NGT. PEG is
without oropharyngeal dysphagia (adjusted HR 1.57, 95% recommended in preference to NGT for patients with
CI: 0.71–3.45, P = 0.261). Bacterial colonization and oropharyngeal dysphagia requiring long-term tube feeding.
gastroesophageal reflux might increase due to interference with Further study will be needed to elucidate the role of
protective cough reflexes in patients with NGT (29–32). The oropharyngeal dysphagia in enteral feeding in older patients.
NGT passes through the upper esophageal sphincter, and studies
have reported more residues in the pharyngolaryngeal region
(29–32), and aspiration of pathogenic bacterial colonization DATA AVAILABILITY STATEMENT
from oropharyngeal secretions could lead to aspiration
pneumonia (48). Therefore, in older patients requiring long- The datasets presented in this article are not readily available
term enteral tube feeding with oropharyngeal dysphagia, PEG is because legal restrictions imposed by the government of Taiwan
a better choice than NGT. in relation to the “Personal Information Protection Act”.
Requests to access the datasets should be directed to Tri-
Management of Oropharyngeal Dysphagia Service General Hospital.
in Older Patients
The management of oropharyngeal dysphagia should include
familial support and a multidisciplinary team (45). Strategies for
reducing the rate of aspiration pneumonia in patients with
ETHICS STATEMENT
oropharyngeal dysphagia include (1) maintaining a semi- The studies involving human participants were reviewed and
recumbent position and turning the patient’s head to one side approved by institutional review board of the Tri-Service General
with the chin down during feeding to reduce the risk of gastric Hospital. The patients/participants provided their written
aspiration (50); (2) maintenance of oral hygiene by proper tooth informed consent to participate in this study.
brushing, mechanical oral cleaning, and oral rinsing with
chlorhexidine (50–52); (3) dental examination to remove
debris, plaque or treat tooth decay (50–52); (4) suctioning of
subglottic and oropharyngeal secretions (33, 53); (5) avoidance AUTHOR CONTRIBUTIONS
of oversedation, antipsychotics, and cough suppressants that
T-HL and W-KC contributed to conception and design of the
weaken the cough reflex (50); (6) regular swallowing
study. T-HL organized the database, performed statistical
rehabilitation (54); (7) feeding with PEG rather than NGT in
analysis, and wrote the first draft of the manuscript. C-WY
patients requiring long-term tube feeding (24, 33).
and W-KC wrote sections of the manuscript. All authors
contributed to manuscript revision, reading, and approval of
Limitations
the submitted version.
Several limitations should be considered when interpreting our
results. First, the study was a prospective single-center non-
randomized design, and due to the limited sample size, the
statistical power is limited. Second, although direct FUNDING
visualization of the pharyngolaryngeal region was feasible with
FEES, we could not assess the contents or amounts aspirated We are grateful for the financial support provided by the
during follow-up and determine their relationship to the Ministry of National Defense-Medical Affairs Bureau, Tri-
development of pneumonia. In addition, swallowing trial was Service General Hospital (TSGH-C108-070 and TSGH-D-
not conducted since a significant proportion of enrolled patients 111080), Taiwan for this study.
had advanced neurological diseases who could not follow
instructions during the examination and penetration-aspiration
scale was not assessed (55–57). Third, information on body ACKNOWLEDGMENTS
weight variation, feeding intolerance, and gastric residual
volume was not available; thus, we could not adjust for these We thank Enago for English language editing service.
Frontiers in Immunology | www.frontiersin.org 7 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
REFERENCES 19. Metheny NA, Schallom L, Oliver DA, Clouse RE. Gastric Residual Volume
and Aspiration in Critically Ill Patients Receiving Gastric Feedings. Am J Crit
1. Cheng X, Yang Y, Schwebel DC, Liu Z, Li L, Cheng P, et al. Population Ageing Care (2008) 17(6):512–9; quiz 520. doi: 10.4037/ajcc2008.17.6.512
and Mortality During 1990-2017: A Global Decomposition Analysis. PloS 20. Almirall J, Rofes L, Serra-Prat M, Icart R, Palomera E, Arreola V, et al.
Med (2020) 17(6):e1003138. doi: 10.1371/journal.pmed.1003138 Oropharyngeal Dysphagia Is a Risk Factor for Community-Acquired
2. Carrion S, Cabre M, Monteis R, Roca M, Palomera E, Serra-Prat M, et al. Pneumonia in the Elderly. Eur Respir J (2013) 41(4):923–8. doi: 10.1183/
Oropharyngeal Dysphagia Is a Prevalent Risk Factor for Malnutrition in a 09031936.00019012
Cohort of Older Patients Admitted With an Acute Disease to a General 21. van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de
Hospital. Clin Nutr (2015) 34(3):436–42. doi: 10.1016/j.clnu.2014.04.014 Baat C. Meta-Analysis of Dysphagia and Aspiration Pneumonia in Frail
3. Alagiakrishnan K, Bhanji RA, Kurian M. Evaluation and Management of Elders. J Dent Res (2011) 90(12):1398–404. doi: 10.1177/0022034511422909
Oropharyngeal Dysphagia in Different Types of Dementia: A Systematic 22. Gomes CA Jr, Andriolo RB, Bennett C, Lustosa SA, Matos D, Waisberg DR,
Review. Arch Gerontol Geriatr (2013) 56(1):1–9. doi: 10.1016/j.archger.2012. et al. Percutaneous Endoscopic Gastrostomy Versus Nasogastric Tube
04.011 Feeding for Adults With Swallowing Disturbances. Cochrane Database Syst
4. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Rev (2015) 5):CD008096. doi: 10.1002/14651858.CD008096.pub4
et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the 23. Baijens LW, Clave P, Cras P, Ekberg O, Forster A, Kolb GF, et al. European
American Heart Association. Circulation (2020) 141(9):e139–596. Society for Swallowing Disorders - European Union Geriatric Medicine
doi: 10.1161/CIR.0000000000000757 Society White Paper: Oropharyngeal Dysphagia as a Geriatric Syndrome.
5. Kozeniecki M, Fritzshall R. Enteral Nutrition for Adults in the Hospital Clin Interv Aging (2016) 11:1403–28. doi: 10.2147/CIA.S107750
Setting. Nutr Clin Pract (2015) 30(5):634–51. doi: 10.1177/08845336155 24. Chang WK, Huang HH, Lin HH, Tsai CL. Evaluation of Oropharyngeal
94012 Dysphagia in Patients Who Underwent Percutaneous Endoscopic
6. Shim YK, Kim N, Park YH, Lee JC, Sung J, Choi YJ, et al. Effects of Age on Gastrostomy: Stratification Risk of Pneumonia. JPEN J Parenter Enteral
Esophageal Motility: Use of High-Resolution Esophageal Impedance Nutr (2020) 44(2):239–45. doi: 10.1002/jpen.1592
Manometry. J Neurogastroenterol Motil (2017) 23(2):229–36. doi: 10.5056/ 25. Srivanitchapoom P, Pandey S, Hallett M. Drooling in Parkinson’s Disease: A
jnm16104 Review. Parkinsonism Relat Disord (2014) 20(11):1109–18. doi: 10.1016/
7. van der Flier WM, Scheltens P. Epidemiology and Risk Factors of Dementia. j.parkreldis.2014.08.013
J Neurol Neurosurg Psychiatry (2005) 76(suppl 5):v2–7. doi: 10.1136/ 26. Granell J, Garrido L, Millas T, Gutierrez-Fonseca R. Management of
jnnp.2005.082867 Oropharyngeal Dysphagia in Laryngeal and Hypopharyngeal Cancer. Int J
8. Rowat A. Enteral Tube Feeding for Dysphagic Stroke Patients. Br J Nurs Otolaryngol (2012) 2012:157630. doi: 10.1155/2012/157630
(2015) 24(3):138, 140, 142–5. doi: 10.12968/bjon.2015.24.3.138 27. Langmore SE. History of Fiberoptic Endoscopic Evaluation of Swallowing for
9. Tokunaga T, Kubo T, Ryan S, Tomizawa M, Yoshida S, Takagi K, et al. Long- Evaluation and Management of Pharyngeal Dysphagia: Changes Over the
Term Outcome After Placement of a Percutaneous Endoscopic Gastrostomy Years. Dysphagia (2017) 32(1):27–38. doi: 10.1007/s00455-016-9775-x
Tube. Geriatr Gerontol Int (2008) 8(1):19–23. doi: 10.1111/j.1447-0594.2008. 28. Pace CC, McCullough GH. The Association Between Oral Microorgansims
00442.x and Aspiration Pneumonia in the Institutionalized Elderly: Review and
10. Nordin N, Kamaruzzaman SB, Chin AV, Poi PJ, Tan MP. A Descriptive Study Recommendations. Dysphagia (2010) 25(4):307–22. doi: 10.1007/s00455-
of Nasogastric Tube Feeding Among Geriatric Inpatients in Malaysia: 010-9298-9
Utilization, Complications, and Caregiver Opinions. J Nutr Gerontol Geriatr 29. Dziewas R, Warnecke T, Hamacher C, Oelenberg S, Teismann I, Kraemer C,
(2015) 34(1):34–49. doi: 10.1080/21551197.2014.998326 et al. Do Nasogastric Tubes Worsen Dysphagia in Patients With Acute Stroke?
11. Cintra MT, de Rezende NA, de Moraes EN, Cunha LC, da Gama Torres HO. BMC Neurol (2008) 8:28. doi: 10.1186/1471-2377-8-28
A Comparison of Survival, Pneumonia, and Hospitalization in Patients With 30. Satou Y, Oguro H, Murakami Y, Onoda K, Mitaki S, Hamada C, et al.
Advanced Dementia and Dysphagia Receiving Either Oral or Enteral Gastroesophageal Reflux During Enteral Feeding in Stroke Patients: A 24-
Nutrition. J Nutr Health Aging (2014) 18(10):894–9. doi: 10.1007/s12603- Hour Esophageal pH-Monitoring Study. J Stroke Cerebrovasc Dis (2013) 22
014-0487-3 (3):185–9. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.008
12. Kumagai R, Kubokura M, Sano A, Shinomiya M, Ohta S, Ishibiki Y, et al. 31. Wang ZY, Chen JM, Ni GX. Effect of an Indwelling Nasogastric Tube on
Clinical Evaluation of Percutaneous Endoscopic Gastrostomy Tube Feeding in Swallowing Function in Elderly Post-Stroke Dysphagia Patients With Long-
Japanese Patients With Dementia. Psychiatry Clin Neurosci (2012) 66(5):418– Term Nasal Feeding. BMC Neurol (2019) 19(1):83. doi: 10.1186/s12883-019-
22. doi: 10.1111/j.1440-1819.2012.02378.x 1314-6
13. Hayashi T, Matsushima M, Wakabayashi H, Bito S. Association Between 32. Gomes GF, Pisani JC, Macedo ED, Campos AC. The Nasogastric Feeding
Delivery Methods for Enteral Nutrition and Physical Status Among Older Tube as a Risk Factor for Aspiration and Aspiration Pneumonia. Curr Opin
Adults. BMC Nutr (2020) 6:2. doi: 10.1186/s40795-019-0318-3 Clin Nutr Metab Care (2003) 6(3):327–33. doi: 10.1097/01.mco.
14. Kano S, Tsushima N, Suzuki T, Hamada S, Yokokawa T, Idogawa H, et al. 0000068970.34812.8b
Predictors of the Need for Prophylactic Percutaneous Endoscopic 33. Wu CC, Huang HH, Lin HH, Chang WK. Oropharyngeal Dysphagia
Gastrostomy in Head and Neck Cancer Patients Treated With Concurrent Increased the Risk of Pneumonia in Patients Undergoing Nasogastric Tube
Chemoradiotherapy. Int J Clin Oncol (2021) 26(7):1179–87. doi: 10.1007/ Feeding. Asia Pac J Clin Nutr (2020) 29(2):266–73. doi: 10.6133/
s10147-021-01889-w apjcn.202007_29(2).0009
15. Jaafar MH, Mahadeva S, Morgan K, Tan MP. Percutaneous Endoscopic 34. Pedersen A, Sorensen CE, Proctor GB, Carpenter GH. Salivary Functions in
Gastrostomy Versus Nasogastric Feeding in Older Individuals With Non- Mastication, Taste and Textural Perception, Swallowing and Initial Digestion.
Stroke Dysphagia: A Systematic Review. J Nutr Health Aging (2015) 19 Oral Dis (2018) 24(8):1399–416. doi: 10.1111/odi.12867
(2):190–7. doi: 10.1007/s12603-014-0527-z 35. Neubauer PD, Rademaker AW, Leder SB. The Yale Pharyngeal Residue
16. Volkert D, Beck AM, Cederholm T, Cruz-Jentoft A, Goisser S, Hooper L, et al. Severity Rating Scale: An Anatomically Defined and Image-Based Tool.
ESPEN Guideline on Clinical Nutrition and Hydration in Geriatrics. Clin Nutr Dysphagia (2015) 30(5):521–8. doi: 10.1007/s00455-015-9631-4
(2019) 38(1):10–47. doi: 10.1016/j.clnu.2018.05.024 36. Teasell RW, McRae M, Marchuk Y, Finestone HM. Pneumonia Associated
17. Lin L-C, Li M-H, Watson R. A Survey of the Reasons Patients do Not Chose With Aspiration Following Stroke. Arch Phys Med Rehabil (1996) 77(7):707–
Percutaneous Endoscopic Gastrostomy/Jejunostomy (PEG/PEJ) as a Route 9. doi: 10.1016/s0003-9993(96)90012-x
for Long-Term Feeding. J Clin Nurs (2011) 20(5-6):802–10. doi: 10.1111/ 37. Cook IJ. Diagnostic Evaluation of Dysphagia. Nat Clin Pract Gastroenterol
j.1365-2702.2010.03541.x Hepatol (2008) 5(7):393–403. doi: 10.1038/ncpgasthep1153
18. Mamun K, Lim J. Role of Nasogastric Tube in Preventing Aspiration 38. Nyabanga C, Khan A, Knotts RM. Oropharyngeal Dysphagia. In: Geriatric
Pneumonia in Patients With Dysphagia. Singapore Med J (2005) 46 Gastroenterology. USA: Springer, Cham (2020). doi: 10.1007/978-3-319-
(11):627–31. 90761-1_40-1
Frontiers in Immunology | www.frontiersin.org 8 February 2022 | Volume 12 | Article 800029
Lin et al. Oropharyngeal Dysphagia in Older Patients
39. Forster A, Samaras N, Gold G, Samaras D. Oropharyngeal Dysphagia in Older 52. Hong C, Aung MM, Kanagasabai K, Lim CA, Liang S, Tan KS. The
Adults: A Review. Eur Geriatric Med (2011) 2(6):356–62. doi: 10.1016/ Association Between Oral Health Status and Respiratory Pathogen
j.eurger.2011.08.007 Colonization With Pneumonia Risk in Institutionalized Adults. Int J Dent
40. Kamarunas EE, McCullough GH, Guidry TJ, Mennemeier M, Schluterman K. Hyg (2018) 16(2):e96–e102. doi: 10.1111/idh.12321
Effects of Topical Nasal Anesthetic on Fiberoptic Endoscopic Examination of 53. Mahmoodpoor A, Hamishehkar H, Hamidi M, Shadvar K, Sanaie S, Golzari
Swallowing With Sensory Testing (FEESST). Dysphagia (2014) 29(1):33–43. SE, et al. A Prospective Randomized Trial of Tapered-Cuff Endotracheal
doi: 10.1007/s00455-013-9473-x Tubes With Intermittent Subglottic Suctioning in Preventing Ventilator-
41. Berner YN. Enteral Nutrition in Geriatric Patients. Mediterranean J Nutr Associated Pneumonia in Critically Ill Patients. J Crit Care (2017) 38:152–6.
Metab (2009) 1(3):141–4. doi: 10.1007/s12349-008-0021-4 doi: 10.1016/j.jcrc.2016.11.007
42. Carucci LR, Turner MA. Dysphagia Revisited: Common and Unusual Causes. 54. Burgos R, Bretó n I, Cereda E, Desport JC, Dziewas R, Genton L, et al. ESPEN
Radiographics (2015) 35(1):105–22. doi: 10.1148/rg.351130150 Guideline Clinical Nutrition in Neurology. Clin Nutr (2018) 37(1):354–96.
43. Roden DF, Altman KW. Causes of Dysphagia Among Different Age Groups: doi: 10.1016/j.clnu.2017.09.003
A Systematic Review of the Literature. Otolaryngol Clin North Am (2013) 46 55. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A Penetration-
(6):965–87. doi: 10.1016/j.otc.2013.08.008 Aspiration Scale. Dysphagia (1996) 11(2):93–8. doi: 10.1007/BF00417897
44. Wilkinson JM, Codipilly DC, Wilfahrt RP. Dysphagia: Evaluation and 56. Lee JS, Collard HR, Raghu G, Sweet MP, Hays SR, Campos GM, et al. Does
Collaborative Management. Am Fam Physician (2021) 103(2):97–106. Chronic Microaspiration Cause Idiopathic Pulmonary Fibrosis? Am J Med
45. Rofes L, Arreola V, Almirall J, Cabre M, Campins L, Garcia-Peris P, et al. (2010) 123(4):304–11. doi: 10.1016/j.amjmed.2009.07.033
Diagnosis and Management of Oropharyngeal Dysphagia and Its Nutritional 57. Weir KA, McMahon S, Taylor S, Chang AB. Oropharyngeal Aspiration and
and Respiratory Complications in the Elderly. Gastroenterol Res Pract (2011) Silent Aspiration in Children. Chest (2011) 140(3):589–97. doi: 10.1378/
2011:818979. doi: 10.1155/2011/818979 chest.10-1618
46. Serra-Prat M, Palomera M, Gomez C, Sar-Shalom D, Saiz A, Montoya JG, 58. Clouse RE, Oliver DA, Schallom L, Metheny NA. Gastric Residual Volume
et al. Oropharyngeal Dysphagia as a Risk Factor for Malnutrition and Lower and Aspiration in Critically Ill Patients Receiving Gastric Feedings. Am J Crit
Respiratory Tract Infection in Independently Living Older Persons: A Care (2008) 17(6):512–9. doi: 10.4037/ajcc2008.17.6.512
Population-Based Prospective Study. Age Ageing (2012) 41(3):376–81.
doi: 10.1093/ageing/afs006
47. Palmer LB, Albulak K, Fields S, Filkin AM, Simon S, Smaldone GC. Oral Conflict of Interest: The authors declare that the research was conducted in the
Clearance and Pathogenic Oropharyngeal Colonization in the Elderly. Am J absence of any commercial or financial relationships that could be construed as a
Respir Crit Care Med (2001) 164(3):464–8. doi: 10.1164/ajrccm.164.3.2008149 potential conflict of interest.
48. Marik PE. Aspiration Pneumonitis and Aspiration Pneumonia. N Engl J Med
(2001) 344(9):665–71. doi: 10.1056/NEJM200103013440908 Publisher’s Note: All claims expressed in this article are solely those of the authors
49. Sakashita R, Takami M, Ono H, Nishihira T, Sato T, Hamada M. Preventing and do not necessarily represent those of their affiliated organizations, or those of
Aspiration Pneumonia Among the Elderly: A Review Focused on the Impact of the publisher, the editors and the reviewers. Any product that may be evaluated in
the Consistency of Food Substances. In: K Sasaki, O Suzuki and N Takahashi, this article, or claim that may be made by its manufacturer, is not guaranteed or
editors. Interface Oral Health Science 2014. Tokyo: Springer Japan (2015). endorsed by the publisher.
50. Mandell LA, Niederman MS. Aspiration Pneumonia. N Engl J Med (2019) 380
(7):651–63. doi: 10.1056/NEJMra1714562 Copyright © 2022 Lin, Yang and Chang. This is an open-access article distributed
51. Hollaar VRY, van der Putten GJ, van der Maarel-Wierink CD, Bronkhorst under the terms of the Creative Commons Attribution License (CC BY). The
EM, de Swart BJM, Creugers NHJ. The Effect of a Daily Application of a 0.05% use, distribution or reproduction in other forums is permitted, provided the original
Chlorhexidine Oral Rinse Solution on the Incidence of Aspiration Pneumonia author(s) and the copyright owner(s) are credited and that the original publication in
in Nursing Home Residents: A Multicenter Study. BMC Geriatr (2017) 17 this journal is cited, in accordance with accepted academic practice. No use,
(1):128. doi: 10.1186/s12877-017-0519-z distribution or reproduction is permitted which does not comply with these terms.
Frontiers in Immunology | www.frontiersin.org 9 February 2022 | Volume 12 | Article 800029
You might also like
- PLAB 1700 MCQs Dr. Khalid - S Explanation of 1700 MCQDocument680 pagesPLAB 1700 MCQs Dr. Khalid - S Explanation of 1700 MCQguzelnor100% (35)
- Surgery I - Topical Past Papers (2007-2019)Document41 pagesSurgery I - Topical Past Papers (2007-2019)AnmahNo ratings yet
- Oropharyngeal Dysphagia in Head and Neck Cancer - How To Reduce Aspiration PneumoniaDocument6 pagesOropharyngeal Dysphagia in Head and Neck Cancer - How To Reduce Aspiration PneumoniaAlvina RusliNo ratings yet
- Pediatric Gastroesophageal Reflux DiseaseDocument5 pagesPediatric Gastroesophageal Reflux Diseasegemala wahabNo ratings yet
- Snijders 2007Document6 pagesSnijders 2007carlaNo ratings yet
- Eiamkulbutr 2023Document12 pagesEiamkulbutr 2023eliza.chiperiNo ratings yet
- VFC 2021Document9 pagesVFC 2021cinthya zambranoNo ratings yet
- Axelsson 2017Document8 pagesAxelsson 2017Yondi Piter PapulungNo ratings yet
- Rigid BronchosDocument6 pagesRigid BronchosVania Dwi AndhaniNo ratings yet
- Ventilator-Associated PneumoniDocument15 pagesVentilator-Associated PneumoniYasminNo ratings yet
- International Journal of Pediatric Otorhinolaryngology: F. Glynn, D. Fitzgerald, M.J. Earley, H. RowleyDocument4 pagesInternational Journal of Pediatric Otorhinolaryngology: F. Glynn, D. Fitzgerald, M.J. Earley, H. RowleyJaavyeraa' BelenNo ratings yet
- Pediatric Critical Care MedicineDocument107 pagesPediatric Critical Care Medicinerahmawatusayu100% (1)
- 1 s2.0 S0022347617301452 MainDocument3 pages1 s2.0 S0022347617301452 MainCindy Julia AmandaNo ratings yet
- 2014 Maeda Neumonia y Higiene AncianosDocument6 pages2014 Maeda Neumonia y Higiene AncianosIvan Ramos GutarraNo ratings yet
- WJG 18 4335Document7 pagesWJG 18 4335aalmadasalazarNo ratings yet
- Dysphagia in Older AdultsDocument10 pagesDysphagia in Older Adultsconstanza duran cordovaNo ratings yet
- Clinical Outcomes and Patient Safety of Nasogastric Tube in Acute Stroke PatientsDocument8 pagesClinical Outcomes and Patient Safety of Nasogastric Tube in Acute Stroke Patientssilviainii0104No ratings yet
- Respiratory Problems in Children With Esophageal Atresia and Tracheoesophageal FistulaDocument9 pagesRespiratory Problems in Children With Esophageal Atresia and Tracheoesophageal FistulaAshley2993No ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- Gastroesophageal Reflux Disease, A Cause For Eustachian Tube Dysfunction in Obstructive Sleep ApneaDocument6 pagesGastroesophageal Reflux Disease, A Cause For Eustachian Tube Dysfunction in Obstructive Sleep ApneaIlham RahmanNo ratings yet
- Cap AdultDocument11 pagesCap AdultashikNo ratings yet
- EsofagusDocument7 pagesEsofagusWillie VanegasNo ratings yet
- 473 1255 1 PBDocument13 pages473 1255 1 PBPeter SalimNo ratings yet
- Diagnosis of Pneumonia in Children With Dehydrating DiarrhoeaDocument6 pagesDiagnosis of Pneumonia in Children With Dehydrating DiarrhoeaEmaa AmooraNo ratings yet
- Pi Is 1078817422002152Document7 pagesPi Is 1078817422002152fernanda contrerasNo ratings yet
- Subglottic Stenosis 2018 PDFDocument7 pagesSubglottic Stenosis 2018 PDFAlexi Chávez EchevarríaNo ratings yet
- RetrieveDocument11 pagesRetrieveSantiago PortillaNo ratings yet
- Researcharticle Open Access: BackgroundDocument4 pagesResearcharticle Open Access: BackgroundMagfira Al HabsyiNo ratings yet
- 1 IiomainDocument6 pages1 IiomainyandaputriNo ratings yet
- Laryngomalacia and Swallowing Function in ChildrenDocument7 pagesLaryngomalacia and Swallowing Function in ChildrenmelaniaNo ratings yet
- Pediatric Pulmonology 2021, Dell'ortoDocument8 pagesPediatric Pulmonology 2021, Dell'ortoRadu CiprianNo ratings yet
- Jurnal 3Document6 pagesJurnal 3Dheana IsmaniarNo ratings yet
- Using Tube Feeding and Levodopa-Carbidopa Intestinal Gel Application in Advanced Parkinson's DiseaseDocument4 pagesUsing Tube Feeding and Levodopa-Carbidopa Intestinal Gel Application in Advanced Parkinson's DiseaseLorenaNo ratings yet
- Bacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General HospitalDocument7 pagesBacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General Hospitalfirda rosyidaNo ratings yet
- Effect of Aspiration On The Lungs in Children: A Comparison Using Chest Computed Tomography FindingsDocument7 pagesEffect of Aspiration On The Lungs in Children: A Comparison Using Chest Computed Tomography FindingsYuliaAntolisNo ratings yet
- Predictors of Aspiration Pneumonia How Important Is DysphagiaDocument13 pagesPredictors of Aspiration Pneumonia How Important Is DysphagiasmilaircNo ratings yet
- H Fistule BronchosDocument10 pagesH Fistule BronchosCirugia Pediatrica La RazaNo ratings yet
- Original Articles: Proton Pump Inhibitor Therapy For Chronic Laryngo-Pharyngitis: A Randomized Placebo-Control TrialDocument9 pagesOriginal Articles: Proton Pump Inhibitor Therapy For Chronic Laryngo-Pharyngitis: A Randomized Placebo-Control TrialAnonymous iM2totBrNo ratings yet
- Estenosis Sub 5Document7 pagesEstenosis Sub 5Nicolás HenaoNo ratings yet
- 10 1080@02770903 2020 1805750Document19 pages10 1080@02770903 2020 1805750locolocomedicinaNo ratings yet
- 10.1007@s00455 018 9894 7 PDFDocument8 pages10.1007@s00455 018 9894 7 PDFCristina Vargas RamosNo ratings yet
- Efficacy of Bronchoalveolar Lavage As Adjunct Therapy in The Treatment of Neonatal Severe PneumoniaDocument6 pagesEfficacy of Bronchoalveolar Lavage As Adjunct Therapy in The Treatment of Neonatal Severe Pneumoniaanita awNo ratings yet
- Paediatrica IndonesianaDocument9 pagesPaediatrica IndonesianaAudina PutriNo ratings yet
- TMP 18829-E354.full91399039Document7 pagesTMP 18829-E354.full91399039Cordova ArridhoNo ratings yet
- J Voice 2019 33 5 708-711Document4 pagesJ Voice 2019 33 5 708-711baltazarottonelloNo ratings yet
- Journal Pone 0193913Document10 pagesJournal Pone 0193913tiara nadya putriandaNo ratings yet
- Incidencia de Disfagia Post Extubación en Pacientes Criticos Revisión SistemáticaDocument9 pagesIncidencia de Disfagia Post Extubación en Pacientes Criticos Revisión SistemáticaKatherine Lepe AbarcaNo ratings yet
- CDC 119845 DS1Document2 pagesCDC 119845 DS1ZarNo ratings yet
- PBD in Pediatric AchalasiaDocument6 pagesPBD in Pediatric AchalasiamuhammadfahmanNo ratings yet
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoNo ratings yet
- Fibrinolytic Treatment of Complicated Pediatric TDocument2 pagesFibrinolytic Treatment of Complicated Pediatric TDR GURDEEP SINGHNo ratings yet
- Endoscopic Examination of The Nasal Cavity and Nasopharynx in Patients With Otitis MediaDocument8 pagesEndoscopic Examination of The Nasal Cavity and Nasopharynx in Patients With Otitis Mediagemala wahabNo ratings yet
- A Therapeutic Maneuver For Oropharyngeal Dysphagia in Patients With PDDocument6 pagesA Therapeutic Maneuver For Oropharyngeal Dysphagia in Patients With PDmajid mirzaeeNo ratings yet
- Wang 2015Document7 pagesWang 2015api-307002076No ratings yet
- Effects of Rapid Palatal Expansion On The Upper Airway SpaceDocument11 pagesEffects of Rapid Palatal Expansion On The Upper Airway SpacevenancioNo ratings yet
- Complications in Children With Percutaneous Endoscopic Gastrostomy (PEG) PlacementDocument5 pagesComplications in Children With Percutaneous Endoscopic Gastrostomy (PEG) PlacementHenry BarberenaNo ratings yet
- Laryngeal Complications of COVID-19Document8 pagesLaryngeal Complications of COVID-19Mariana BarrosNo ratings yet
- Association Between Breathing Route, Oxygen Desaturation, and Upper Airway MorphologyDocument6 pagesAssociation Between Breathing Route, Oxygen Desaturation, and Upper Airway MorphologyMark Burhenne DDSNo ratings yet
- Coordes 2017Document21 pagesCoordes 2017nunisulastri1998No ratings yet
- Dupilumab Improves Upper and Lower Airway Disease Control in Chronic Rhinosinusitis With Nasal Polyps and AsthmaDocument10 pagesDupilumab Improves Upper and Lower Airway Disease Control in Chronic Rhinosinusitis With Nasal Polyps and AsthmaMeylinda RizkyNo ratings yet
- Diagnostic Utility of Bronchoalveolar Lavage in Children With Complicated Intrathoracic TuberculosisDocument9 pagesDiagnostic Utility of Bronchoalveolar Lavage in Children With Complicated Intrathoracic TuberculosisFitri Amelia RizkiNo ratings yet
- Diagnosis and Treatment of Chronic CoughFrom EverandDiagnosis and Treatment of Chronic CoughSang Heon ChoNo ratings yet
- Smile Care FoodDocument18 pagesSmile Care FoodmccasreqNo ratings yet
- Clinical Utility of The 3-Ounce Water Swallow TestDocument7 pagesClinical Utility of The 3-Ounce Water Swallow Testmaria fernanda hurtadoNo ratings yet
- Positioning Improves The Oral and Pharyngeal Swallowing Function in Children With Cerebral PalsyDocument4 pagesPositioning Improves The Oral and Pharyngeal Swallowing Function in Children With Cerebral PalsySwathi GeethaNo ratings yet
- Word Ncp.......... TetanusDocument6 pagesWord Ncp.......... TetanusaianrNo ratings yet
- NCP NeuroDocument20 pagesNCP NeuroNica Gaborne Navarro100% (3)
- Mann-Assessment-Of-Swallowing-Ability - Scoring SheetDocument1 pageMann-Assessment-Of-Swallowing-Ability - Scoring SheetThu TranNo ratings yet
- Okuno 2014Document4 pagesOkuno 2014mujtabaNo ratings yet
- 11 Digestion and Bowel Elimination 2019 (Nursing) Geriatric NursingDocument44 pages11 Digestion and Bowel Elimination 2019 (Nursing) Geriatric NursingDarla SaulerNo ratings yet
- Module 3 Tools: Pressure Ulcer Prevention ToolkitDocument16 pagesModule 3 Tools: Pressure Ulcer Prevention ToolkitIntanAgustiFernandesNo ratings yet
- Premotor, NonmotorDocument12 pagesPremotor, Nonmotormicaelporto.internationalNo ratings yet
- Size Shape and Other Physical Attributes of Generic Tablets and CapsulesDocument10 pagesSize Shape and Other Physical Attributes of Generic Tablets and CapsulesrajeebNo ratings yet
- Assessing The Breastfeeding Dyad - A Guide For Speech-Language PathologistsDocument5 pagesAssessing The Breastfeeding Dyad - A Guide For Speech-Language PathologistsPaloma LópezNo ratings yet
- LATADA, Christiane Kyla G.Document11 pagesLATADA, Christiane Kyla G.Kyla LatadaNo ratings yet
- A Study of Psycho-Pathology and Treatment ofDocument9 pagesA Study of Psycho-Pathology and Treatment ofUlysses PinheiroNo ratings yet
- A Case Report On - A Rare Case of Laryngocele in A Young Male MenDocument4 pagesA Case Report On - A Rare Case of Laryngocele in A Young Male MenIOSRjournalNo ratings yet
- DysphagiaDocument4 pagesDysphagiaMicaNo ratings yet
- Esophageal Disorders Types, Risks, Symptoms and TDocument14 pagesEsophageal Disorders Types, Risks, Symptoms and TKolade YousuffNo ratings yet
- The Transition To Work of Newly Qualified Speech and Language Therapists: Implications For The CurriculumDocument15 pagesThe Transition To Work of Newly Qualified Speech and Language Therapists: Implications For The CurriculumLaura RodriguezNo ratings yet
- Esophageal Disorder Part IIDocument27 pagesEsophageal Disorder Part IIJuma AwarNo ratings yet
- FINAL - 15062012 - Dysphagia - Clinical - Guidelines - Web 5Document51 pagesFINAL - 15062012 - Dysphagia - Clinical - Guidelines - Web 5Nathalia Dos ReisNo ratings yet
- Malformations of OesophagusDocument24 pagesMalformations of OesophagusOwoupele Ak-Gabriel100% (1)
- Eating Assessment Tool EAT 10 PDFDocument70 pagesEating Assessment Tool EAT 10 PDFCarol Artigas GómezNo ratings yet
- Dysphagia DissertationDocument4 pagesDysphagia DissertationOrderAPaperSingapore100% (1)
- Tests and DisordersDocument21 pagesTests and DisordersNoor KhalilNo ratings yet
- Cricopharyngeal DysphagiaDocument8 pagesCricopharyngeal Dysphagiataner_soysurenNo ratings yet
- Roth 10e Nclex Chapter 23Document2 pagesRoth 10e Nclex Chapter 23jennaaahhhNo ratings yet
- Pemicu 1 DessyDocument184 pagesPemicu 1 DessyDessy DsyNo ratings yet
- NCMA 215 Course Task 15 - Lecture Module Week 9: Andrea B. Autor BSN 2YC-2Document2 pagesNCMA 215 Course Task 15 - Lecture Module Week 9: Andrea B. Autor BSN 2YC-2Gina PrancelisoNo ratings yet