Professional Documents
Culture Documents
Download
Download
Uploaded by
srozi1367Copyright:
Available Formats
You might also like
- Summary - Granovetter (1985) Economic Action and Social StructureDocument2 pagesSummary - Granovetter (1985) Economic Action and Social StructureSimon Fiala100% (12)
- Bio Eoc Review Session 1 Questions 11-12Document6 pagesBio Eoc Review Session 1 Questions 11-12api-269873615No ratings yet
- Format PengkajianDocument8 pagesFormat PengkajianHandiniNo ratings yet
- Metabolic Syndrome and Psoriatic Arthritis Among Patients With Psoriasis Vulgaris: Quality of Life and PrevalenceDocument8 pagesMetabolic Syndrome and Psoriatic Arthritis Among Patients With Psoriasis Vulgaris: Quality of Life and PrevalenceVictor CastilloNo ratings yet
- KAP Towards DMDocument10 pagesKAP Towards DMHabtamu Wondifraw100% (1)
- Alencar 2010Document6 pagesAlencar 2010Tín NguyễnNo ratings yet
- Prevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateDocument7 pagesPrevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateIJAERS JOURNALNo ratings yet
- Added Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataDocument6 pagesAdded Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataNavaneethan GnanadesiganNo ratings yet
- 8 Mansour - Factors - Associated - With - Glycemic - Control - in - Type - 2 - Diabetic - Patients - in - Saudi - ArabiaDocument5 pages8 Mansour - Factors - Associated - With - Glycemic - Control - in - Type - 2 - Diabetic - Patients - in - Saudi - Arabiabangd1f4nNo ratings yet
- Prediction of Type 2 Diabetes Mellitus Using Hematological Factors Based On Machine Learning Approaches: A Cohort Study AnalysisDocument11 pagesPrediction of Type 2 Diabetes Mellitus Using Hematological Factors Based On Machine Learning Approaches: A Cohort Study Analysis21bit20No ratings yet
- Artículo Redalyc 32751053016Document25 pagesArtículo Redalyc 32751053016Angélica Oyola FernándezNo ratings yet
- Adua Et Al-2017-Clinical and Translational MedicineDocument11 pagesAdua Et Al-2017-Clinical and Translational MedicineSam Asamoah SakyiNo ratings yet
- Jurnal LepraDocument7 pagesJurnal LepraDipa Zoda HelfandoNo ratings yet
- Literature Review DiabetesDocument5 pagesLiterature Review Diabetesukefbfvkg100% (1)
- 2017 Subinical DiabetesDocument24 pages2017 Subinical DiabetesLuís Mauricio LimaNo ratings yet
- JUrnal AurinaDocument8 pagesJUrnal AurinaRahmiyantiNo ratings yet
- Presentation and Character For Adult Patients With Diabetes in LibyaDocument8 pagesPresentation and Character For Adult Patients With Diabetes in LibyaMediterr J Pharm Pharm SciNo ratings yet
- 0104 1169 Rlae 28 E3369Document10 pages0104 1169 Rlae 28 E3369surya rakhmat hidayatNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleRicardo Joshua RojasNo ratings yet
- 2181 2407 3 PBDocument18 pages2181 2407 3 PBFahrika Luthfi AfiqohNo ratings yet
- Content ServerDocument11 pagesContent ServerRachma FadillahNo ratings yet
- Pi Is 2589537019301877Document2 pagesPi Is 2589537019301877prince BoadiNo ratings yet
- Research Proposal IntroductionDocument8 pagesResearch Proposal IntroductionIsaac OmwengaNo ratings yet
- Burden of Cardiovascular Diseases Attributable ToDocument11 pagesBurden of Cardiovascular Diseases Attributable ToAnindya Anjas PutriaviNo ratings yet
- Associations of Diabesity With All Cause and Cardiovascular Disease MortalityDocument10 pagesAssociations of Diabesity With All Cause and Cardiovascular Disease Mortalityluis sanchezNo ratings yet
- Prevalence of Undiagnosed and Uncontrolled Diabetes Mellitus Among Adults in South ChennaiDocument5 pagesPrevalence of Undiagnosed and Uncontrolled Diabetes Mellitus Among Adults in South ChennaiVishakha BhosaleNo ratings yet
- Shenes Thompson Final Draft For Ethical ApprovalDocument36 pagesShenes Thompson Final Draft For Ethical ApprovalKaif AliNo ratings yet
- Variability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.Document12 pagesVariability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.franciscoNo ratings yet
- Final Pint ResearchDocument90 pagesFinal Pint ResearchNhelia Santos BañagaNo ratings yet
- Prevalence of Diabetes Mellitus in Patients Seeking Medical Care at Morogoro Regional Referral Hospital in TanzaniaDocument8 pagesPrevalence of Diabetes Mellitus in Patients Seeking Medical Care at Morogoro Regional Referral Hospital in TanzaniaEmmanuel MpaliyeNo ratings yet
- Afsana Afroz, Khurshid Alam, Mohammed J Alramadan, MD Nassif Hossain, Hasina Akhter Chowdhury, Liaquat Ali, Dianna J Magliano, Baki BillahDocument7 pagesAfsana Afroz, Khurshid Alam, Mohammed J Alramadan, MD Nassif Hossain, Hasina Akhter Chowdhury, Liaquat Ali, Dianna J Magliano, Baki BillahS1 FARMASI STIKESNAS ANGKATAN 2 2017No ratings yet
- Article 233554Document11 pagesArticle 233554رقية ياسينNo ratings yet
- 1. Utama nutrients-15-00430Document15 pages1. Utama nutrients-15-00430besti verawatiNo ratings yet
- 30IJAERS 06202035 Perceptionsof PDFDocument8 pages30IJAERS 06202035 Perceptionsof PDFIJAERS JOURNALNo ratings yet
- Evaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyDocument7 pagesEvaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyMirna Liliana Carmona GarciaNo ratings yet
- Changes in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyDocument6 pagesChanges in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyReny NapitupuluNo ratings yet
- BMJ Open 2013 MorganDocument8 pagesBMJ Open 2013 Morganjft842No ratings yet
- 2024 APRU Case Comp Challenge Final2Document10 pages2024 APRU Case Comp Challenge Final2AnneAyushaNo ratings yet
- Health Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesDocument9 pagesHealth Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesgamzeNo ratings yet
- Burden of DiabetesDocument7 pagesBurden of DiabetesNaga LakshmiNo ratings yet
- Retinopatía DiabéticaDocument7 pagesRetinopatía DiabéticaDIANE EDITH LUNA TOPETENo ratings yet
- Prevalencia de Diabetes e Hiperglucemia Intermedia en Adultos. Centroamerica. Diabetescare2012Document3 pagesPrevalencia de Diabetes e Hiperglucemia Intermedia en Adultos. Centroamerica. Diabetescare2012Kevin CastilloNo ratings yet
- Spatio-Temporal Trend in Detections of Diabetes Mellitus and Systematic Arterial Hypertension in IMSS Users, 2004-2019Document11 pagesSpatio-Temporal Trend in Detections of Diabetes Mellitus and Systematic Arterial Hypertension in IMSS Users, 2004-2019MIGUEL ERNESTO GONZALEZ CASTANEDANo ratings yet
- DNHE4 Project Proposal 2201393222Document17 pagesDNHE4 Project Proposal 2201393222Surya Dharshni HomoeoNo ratings yet
- Diabetes Mellitus in Brazil: Risk Factors, Classification and ComplicationsDocument4 pagesDiabetes Mellitus in Brazil: Risk Factors, Classification and Complicationsjoy parimalaNo ratings yet
- TransleteDocument85 pagesTransleteFeliany BiroNo ratings yet
- A Study Assess The Level of Stress Among Patients With Type II Diabetes Mellitus in Relation To Level of Blood Sugar at Nerkundrum I UPHCDocument4 pagesA Study Assess The Level of Stress Among Patients With Type II Diabetes Mellitus in Relation To Level of Blood Sugar at Nerkundrum I UPHCEditor IJTSRDNo ratings yet
- Prediabetes Education To Prevent The Progression To Type 2 DiabetDocument20 pagesPrediabetes Education To Prevent The Progression To Type 2 DiabetEndah WulandariNo ratings yet
- Pengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas HidupDocument8 pagesPengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas Hidupilma adilla syahidaNo ratings yet
- Pengaruh Hipoglikemia Pada Pasien Diabetes MelitusDocument8 pagesPengaruh Hipoglikemia Pada Pasien Diabetes Melitusmail junkNo ratings yet
- Anemia in Patients With Type 2 Diabetes MellitusDocument9 pagesAnemia in Patients With Type 2 Diabetes MellitusmitchelNo ratings yet
- 349 FullDocument3 pages349 FullsenkonenNo ratings yet
- Diabetes Mellitus: A Review On Pathophysiology, Current Status of Oral Medications and Future PerspectivesDocument23 pagesDiabetes Mellitus: A Review On Pathophysiology, Current Status of Oral Medications and Future PerspectivesGhede DhayatNo ratings yet
- Nutritional Assessment of Older Adults With Diabetes MellitusDocument8 pagesNutritional Assessment of Older Adults With Diabetes MellitusCarlo EspadinNo ratings yet
- Anesthesia Management On Perioperative With DM Patients - A Literature ReviewDocument9 pagesAnesthesia Management On Perioperative With DM Patients - A Literature ReviewvienvienkkNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument14 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaAnna StimNo ratings yet
- Risk Factors of Type 2 DiabetesDocument13 pagesRisk Factors of Type 2 DiabetesLalu Angling PatayaNo ratings yet
- Jurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. . No 20 . E-Issn: 2087-0035Document9 pagesJurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. . No 20 . E-Issn: 2087-0035nurfitriaNo ratings yet
- Low Extremity AmputationDocument5 pagesLow Extremity AmputationMuhammad RizqiNo ratings yet
- Effect of Diet On Type 2 Diabetes Mellitus: A ReviewDocument7 pagesEffect of Diet On Type 2 Diabetes Mellitus: A ReviewTowo RottenNo ratings yet
- Healthcare 09 00832Document9 pagesHealthcare 09 00832cheatingw995No ratings yet
- Ampalaya: Nature's Remedy for Type 1 & Type 2 DiabetesFrom EverandAmpalaya: Nature's Remedy for Type 1 & Type 2 DiabetesRating: 5 out of 5 stars5/5 (1)
- Danfoss Vane Tip LUG SylaxDocument18 pagesDanfoss Vane Tip LUG SylaxmaggamNo ratings yet
- (The Logic of Political Survival) .Bruce Bueno de Mesquita, Alastair Smith, Randolph M. Siverson, James D. Morrow PDFDocument551 pages(The Logic of Political Survival) .Bruce Bueno de Mesquita, Alastair Smith, Randolph M. Siverson, James D. Morrow PDFjasonnijmh100% (1)
- Appendix-1 Piping Isometric With Node Numbers: Saudi Arabian Oil CompanyDocument1 pageAppendix-1 Piping Isometric With Node Numbers: Saudi Arabian Oil CompanyJohn BuntalesNo ratings yet
- Propylene (Asia-Pacific) 31 Jan 2020Document5 pagesPropylene (Asia-Pacific) 31 Jan 2020Wira Nata S SinuhajiNo ratings yet
- Cema Belt Conveyors For Bulk Materials Vol 1: Traducir Esta PáginaDocument6 pagesCema Belt Conveyors For Bulk Materials Vol 1: Traducir Esta PáginaDIEGO FERNANDO CADENA ARANGONo ratings yet
- Nisbet Idea of Progress PDFDocument31 pagesNisbet Idea of Progress PDFHernan Cuevas ValenzuelaNo ratings yet
- English A Status ReportDocument3 pagesEnglish A Status ReportNataliasol07No ratings yet
- Logix SERCOS Tuning Tips v1.02 1Document6 pagesLogix SERCOS Tuning Tips v1.02 1José AlanizNo ratings yet
- Tube ClampDocument113 pagesTube ClampAmitava SilNo ratings yet
- Engineering Mathematics Questions and Answers - Laplace Transform by Properties - 1Document9 pagesEngineering Mathematics Questions and Answers - Laplace Transform by Properties - 1RAHUL SOLANKENo ratings yet
- The Handmaid's Tale ContextDocument2 pagesThe Handmaid's Tale ContextBeheshtaNo ratings yet
- Artificial Retina: Presented byDocument6 pagesArtificial Retina: Presented bySai KrishnaNo ratings yet
- Customer Service AssignmentDocument2 pagesCustomer Service AssignmentJoe Kau Zi YaoNo ratings yet
- Social Dimensions in Education Part 1Document4 pagesSocial Dimensions in Education Part 1Laurice Marie GabianaNo ratings yet
- A Project Proposal of Online Enrollment in WmsuDocument9 pagesA Project Proposal of Online Enrollment in WmsuClairole Marie Quilantang100% (2)
- CPRG - V4 - Advanced Issues in Contract PricingDocument304 pagesCPRG - V4 - Advanced Issues in Contract Pricingjarod437No ratings yet
- List of Figures: Inter State Bus Terminal, DwarkaDocument4 pagesList of Figures: Inter State Bus Terminal, Dwarkamalay SRIVASTAVANo ratings yet
- KTM ContentsDocument4 pagesKTM Contentstahaqureshi123No ratings yet
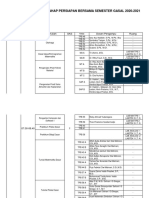
- JADWAL KULIAH TPB SMT GASAL TA 2020 2021 Rev 5Document49 pagesJADWAL KULIAH TPB SMT GASAL TA 2020 2021 Rev 5shin yongriNo ratings yet
- DETAILED LESSON PLAN SubatomicparticlesDocument16 pagesDETAILED LESSON PLAN SubatomicparticlesMary Rose Ramos100% (3)
- fmamsmlmflmlmlllmmlDUK DOSEN UNTAD AGUSTUS 2013bhvffyfDocument117 pagesfmamsmlmflmlmlllmmlDUK DOSEN UNTAD AGUSTUS 2013bhvffyfIsmail Sholeh Bahrun MakkaratteNo ratings yet
- Reading Comprehension Power ToolsDocument6 pagesReading Comprehension Power ToolsCarlos Alberto Lopez MartinezNo ratings yet
- 3374 PDFDocument10 pages3374 PDFCornel DumitruNo ratings yet
- Why Critical Thinking Is ImportantDocument3 pagesWhy Critical Thinking Is ImportantMehreen KandaanNo ratings yet
- GCC Lab Manual Mahesh Kumar PDFDocument130 pagesGCC Lab Manual Mahesh Kumar PDFMohan ReddyNo ratings yet
- Msi MPG b550 Gaming PlusDocument68 pagesMsi MPG b550 Gaming PlusMarvelous WololoNo ratings yet
- Pathway To English Peminatan 3 Bab 3Document9 pagesPathway To English Peminatan 3 Bab 3Agung PrasetyoNo ratings yet
- Petroleum & Petrochemicals Test Method Capabilities: Intertek Caleb Brett 1Document18 pagesPetroleum & Petrochemicals Test Method Capabilities: Intertek Caleb Brett 1Eng-sadeq HesseinNo ratings yet
Download
Download
Uploaded by
srozi1367Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Download
Download
Uploaded by
srozi1367Copyright:
Available Formats
e20497
Brazilian Journal of
Article
Pharmaceutical Sciences
http://dx.doi.org/10.1590/s2175-97902022e20497
Prevalence of hypertension and obesity in
patients with type 2 Diabetes Mellitus
Misma Silva Cruz1, Ingrid Cristina Ferreira da Silva1,
Jéssica Silva Gonçalves Miguez1, Mariana Pirani Rocha Machado1,2*
¹Araguaia Valley University Center (UNIVAR), Barra do Garças, MT, Brazil, 2Postgraduate Program
in Pharmacology and Biotechnology, Institute of Biosciences (UNESP), Botucatu, SP, Brazil
Faced with the increase of type 2 Diabetes mellitus (DM2) and the failure in treatment, questions
have been raised about the clinical situation of these patients. The present study analyzes the
prevalence of hypertension and obesity in DM2 patients. Data were collected through interviews
and anamnesis of 16 participants. After the meetings, in which capillary glycemia and blood
pressure were measured, the participants received guidance about glycemic monitoring, blood
pressure control and changes in lifestyle. Approximately 75% of the participants were women with
average age of 65 years, 87.5% were sedentary, 18.75% smoked and/or used alcoholic beverages and
none performed regular blood glucose monitoring. The initial blood glucose average was 148 mg/
dL and finally decreased to 133 mg/dL. There was no significant difference in blood pressure levels.
Regarding the body mass index, 89.4% of the patients were above normal standards and 100%
had altered waist circumference values. There is a need for studies like this in order to promote
educational practices for health and disease control, highlighting the importance of multidisciplinary
teams and the pharmaceutical professional, since non-adherence to blood glucose monitoring, also
associated with hypertension and obesity, can interfere with the individual’s clinical condition.
KEYWORDS: Chronic noncommunicable disease. Hyperglycemia. Hypertensive. Overweight.
Educational practices.
INTRODUCTION number has reached about 14.3 million adults (20 to 79
years old) (International Diabetes Federation - IDF, 2017).
Chronic noncommunicable diseases (NCD) have The classification of DM, characterized by
increased significantly in the world population with hyperglycemia, is based on the etiology and not on the
the appearance of circulatory system diseases, chronic type of treatment, thus the World Health Organization
respiratory diseases, neoplasms and diabetes. Most of (WHO) and the American Diabetes Association (ADA)
the factors are related to the population’s lifestyle habits proposed four clinical classes: type 1 DM (DM1), Type
according to Diretrizes da Sociedade Brasileira de 2 DM (DM2), gestational DM, and also specific types of
Diabetes (SBD, 2019-2020). diabetes due to other causes (ADA, 2020).
Diabetes mellitus (DM) and Systemic Arterial Among the clinical classes mentioned, DM2 appears
Hypertension (SAH) are part of NCDs, which are related in 90% to 95% of cases, characterized by defects in
to the main causes of morbidity and mortality across the action and secretion of insulin. This is characterized
country (Malfatti, Assunção, 2011; Schmidt et al., 2011). by the progressive loss of insulin secretion through β
It is estimated that if current trends persist, the number of cells, contextualized as insulin resistance (Kahn, Cooper,
diabetics may reach 642 million by 2040; in Brazil, this Del Prato, 2014; Diretrizes da Sociedade Brasileira de
Diabetes - SBD, 2014-2015). The following are the main
*Correspondence: M. P. R. Machado. Centro Universitário do Vale do
Araguaia (UNIVAR). Rua Moreira Cabral, número 1000 – Barra do Garças.
risk factors: age over 45 years, family history, overweight
CEP: 78600-000, Mato Grosso, Brasil. Phone: +55 66 99986-6530. E-mail: (Body Mass Index – BMI> 25 kg / m²), physical inactivity,
mariana.pirani@hotmail.com. ORCID: https://orcid.org/0000-0001-8412-
2483
Braz. J. Pharm. Sci. 2022;58: e20497 Page 1/9
Misma Silva Cruz, Ingrid Cristina Ferreira da Silva, Jéssica Silva Gonçalves Miguez, Mariana Pirani Rocha Machado
low HDL-C, high total cholesterol and triglycerides, and Considering the growing number of patients with
the presence of SAH (Marinho et al., 2013). DM2, SAH and obesity, also due to the significant
SAH is a multifactorial disease, frequently associated number of therapeutic failures, there are questions about
with metabolic, hormonal changes and trophic phenomena, the epidemiological profile and about the possible changes
which consist of cardiac and vascular hypertrophy, its in the glycemic profile, blood pressure and BMI of type 2
main characteristic is elevated blood pressure (Duarte et diabetic patients registered in Basic Health Units (UBS)
al., 2019; Laar et al., 2019). In Brazil, SAH affects 32.5% in Barra do Garças-MT. Thus, this study examines the
(36 million) of adult individuals, more than 60% of the prevalence of hypertension and obesity in type 2 diabetic
elderly, contributing directly or indirectly to 50% of deaths patients.
from cardiovascular disease (Santos, 2016; Diretrizes da
Sociedade Brasileira de Cardiologia - SBC, 2017). MATERIAL AND METHODS
The emergence of SAH is closely related to the
economic, social and cultural environment (Malta et al., Study design and population
2016). And in Brazil it is also related to unemployment,
low wages, sedentary lifestyles, age, sex, family history, This is an observational analytical cross-sectional
stress, smoking, excessive consumption of salt, fat, study with a quantitative approach, characterized as a
carbohydrates, alcoholism and lack of information data collection survey, considering the description of
(Duarte et al., 2019). These factors have resulted in factors related to the population.
increased numbers of hypertensive patients, leading The data were collected through interviews,
to unfavorable consequences such as heart attacks, subsequently measuring the blood pressure and capillary
kidney diseases and neurological diseases, increasing glycemia and anthropometric variables during previously
the population’s morbidity (Porto et al., 2020). scheduled home visits to the participants. The participants
Obesity is classified as a multifactorial disease and were attended at two Basic Health Units (UBS): UBS
has become a global pandemic. Over 650 million people São Sebastião and UBS Fundação Rotariana, in the city
face a complex interaction between biological, epigenetic, of Barra do Garças-MT, together with the health agents
psychosocial, and environmental factors, as well as of the region.
industrial factors (Ralston et al., 2018; Upadhyay et al.,
2018). Thus, it is now argued that a variety of environmental Inclusion/exclusion criteria
factors can be superimposed on diet and exercise to
influence the development of obesity (Lee, Blumberg, 2019). In our study, the participants included must be
Chronic and microvascular complications of DM, regularly registered in the Family Health Program (PSF),
such as diabetic nephropathy, diabetic retinopathy, be of legal age and diagnosed with diabetes or diabetes
diabetic neuropathy and macrovascular diseases, can and hypertension. We excluded the participants with
lead to acute myocardial infarction, stroke and peripheral related kidney disease or who did not follow the above-
vascular disease resulting mainly from inadequate mentioned restrictions.
control, time of evolution and disease factors (Tschiedel,
2014). In turn, SAH is one of the most important risk Sample Characterization / Ethical aspects
factors for the development of cardiovascular diseases,
which are characterized by high and sustained blood 16 participants who were regularly registered in
pressure levels (Petrie, Guzik, Touyz, 2018). Furthermore, the Family Health Program (PSF) were selected, of
obesity is often associated with complications that these, 2 were diagnosed as diabetic and 14 as diabetic
affect cardiovascular, endocrine, and gastrointestinal and hypertensive. The interview was conducted through
(GI) systems (Lee, Blumberg, 2019), leading to severe a questionnaire with objective and specific questions
comorbidities when associated with other NCDs. and only with participants who had signed the Free and
Page 2/9 Braz. J. Pharm. Sci. 2022;58: e20497
Prevalence of hypertension and obesity in patients with type 2 Diabetes Mellitus
Informed Consent Term and in accordance with the test strips. In one of the meetings, the participants were
approval of the Research Ethics Committee of the Federal also assessed for anthropometric variables.
University of Mato Grosso, by protocol number: 3.356.510 In addition, during this period, participants
(CAAE: 14294319.4.0000.5587). received guidance in all visits, with educational
practices via information leaf lets and dialogs, to
Data collection maintain health, including glycemic / blood pressure
monitoring and guidelines for lifestyle changes. Figure
For 5 months, patients were followed up, guided 1 shows the study design and data collection of all home
and evaluated for blood pressure measurement using a visits as a timeline.
stethoscope and sphygmomanometer, capillary blood
glucose using the Accu-Chek Performa® glucometer and
FIGURE 1 – Study design and data collection of all home visits.
Data Collection Instrument reading taken at expiration time. Weight was measured
using a portable scale, with the subject standing and
The anthropometric variables used in this study barefoot; and height was measured by a stadiometer,
were BMI and waist circumference (WC). BMI was with the individual standing, barefoot, heels together,
obtained using the BMI formula = weight (kg) / height2 back straight and arms extended at the side of the body.
(m), which classifies individuals according to the cutoff The classification of cardiovascular risk used the
points: low weight <18.5 kg/m 2; eutrophic 18.5-24.9 cutoff points proposed by the National Cholesterol
kg/m2; overweight 25.0-29.9 kg/m2; obesity I 30.0-34.9 Education Program (NCEP, 2001), which indicate high
kg/m2; obesity II 35.0-39.9 kg/m 2; and obesity III ≥ 40 cardiovascular risk for WC values ≥94 cm for men and
kg/m 2, according to the World Health Organization ≥ 80 cm for women and very high values ≥102 cm for
(WHO, 1995). men and ≥88 cm for women.
WC was obtained using a flexible measuring tape, The recommendations of the Brazilian Diabetes
positioned immediately above the umbilical scar and the Society (SBD, 2019-2020) for blood glucose levels were
Braz. J. Pharm. Sci. 2022;58: e20497 Page 3/9
Misma Silva Cruz, Ingrid Cristina Ferreira da Silva, Jéssica Silva Gonçalves Miguez, Mariana Pirani Rocha Machado
used as a parameter, as metabolic control goals, which TABLE I - Clinical and lifestyle characterization of the 16
advocate pre-prandial glycemic values from 80 to 130mg/ diabetics treated at two Basic Health Units in Barra do
Garças-MT
dL for established type 2 diabetic patients, according to
the American Diabetes Association (ADA, 2020).
VARIABLES N %
For a classification / diagnosis of SAH according
to the Ministério da Saúde (2017), there’s a standard set Gender
of measurements determined according to the systolic Women 12 75.00
and diastolic pressure, respectively: normal readings are Men 4 25.00
below 120 mmHg/80 mmHg; prehypertension of 120-129
Age
mmHg and <80 mmHg; mild hypertension (stage 1) of
130-139 mmHg and 80-89 mmHg; severe hypertension < 50 2 12.50
(stage 2) with readings above 140 mmHg and 90 mmHg; ≥ 50 14 87.50
hypertensive crisis above 180 mmHg and 110 mmHg; Polypharmacy
diabetic and chronic renal patients below 130 mmHg
<5 14 87.50
and 80 mmHg.
≥5 2 12.50
Data analysis / Statistical analysis Hypertensive
Yes 14 87.50
Descriptive analyses were performed to assess the No 2 12.50
patients’ characteristics. As quantitative variables, the
Diagnostic time of DM
Kolmogorov-Smirnov and Shapiro-Wilk tests were used
to assess normality. The figures, tables and statistical < 5 years 5 31.25
analyzes between four collections/home visits were > 5 years 11 68.75
performed using the GraphPad Prism5 software, using the Laboratory analyzes per year
Student’s T test. It was considered statistically significant Once 9 56.25
when the p value is less than or equal to 0.05.
More than one time 7 43.75
RESULTS AND DISCUSSION Daily glycemic control 0 0.00
Practice of physical activity
This work included the 16 participants, evaluating Yes 2 12.50
diabetic or diabetic and hypertensive individuals, 75% (n
No 14 87.50
= 12) of the female gender and 25% (n = 4) of the male
gender (Table I). These data corroborate the findings in Use of alcoholic beverages
the study by Silva et al. (2018), in which about 64% of the Yes 3 18.75
patients attended were women and 36% were men. This can No 13 81.25
be explained by the fact that women are more concerned Smoker
with their own health, thus increasing the number of women
Yes 3 18.75
diagnosed with diabetes in relation to men (Schlichthorst
et al., 2016; Silva, Araújo, Campos, 2018). No 13 81.25
N= number of participants; % = percentage of responses
about clinical situation and lifestyle.
Regarding the use of medications, about 87.5% of
the participants used less than 5 medications and 12.5%
Page 4/9 Braz. J. Pharm. Sci. 2022;58: e20497
Prevalence of hypertension and obesity in patients with type 2 Diabetes Mellitus
used more than 5 medications (Table I), which in this The alarming data found in our research was that none
case characterizes a polypharmacy (Veronin, 2022). In of these participants underwent daily glycemic control, this
the study by Lima et al. (2015), most diabetic patients data corroborates the work of Rocha et al. (2017). In part,
used less than five medications, with an average of 4.6 many patients stated they are afraid of self-applying the
medications. These data are quite worrying, given that test, or are unable to buy a device, while others said that
the use of several medications, although sometimes not they look for it in the public service (UBS) and complain
classified as polypharmacy, can present adverse drug about the lack of materials (Rocha et al., 2017).
reaction (ADR) risks and drug interactions (Munger, In addition, regarding to physical activity, only
2010; Lima et al., 2015; Noale et al., 2016; Rocha et al., 12.5% practiced some activity, about 18.75% used
2017), mainly causing impacts on the health of the elderly alcoholic beverages and the same percentage were
(Munger, 2010; Secoli, 2010; Noale et al., 2016). smoking patients (Table I). These data agreed with
In our study, 87.5% of all evaluated participants Silva et al. (2018), who reported that 19.4% of the study
were hypertensive (Table I). Pinho et al. (2015) presented participants did physical activity, 19.6% used alcohol,
similar data, that indicated that the majority of diabetic and 16.5% smoked, aspects that can negatively influence
patients were also hypertensive, a fact that can be the patient’s health.
explained by a higher prevalence of diabetic individuals In the first evaluation of pre-prandial capillary blood
presenting characteristics such as obesity, physical glucose, the average was 148.88 mg/dL, in the second
inactivity, high triglycerides and total cholesterol levels, evaluation it was 140.00 mg/dL, in the third it was 147.44
stimulation of hyperinsulinemia on the sympathetic mg/dL and in the fourth and last evaluation the average
nervous system, sodium retention and the excitatory was about 133.56 mg/dL (Figure 2), considering both
activity of hyperglycemia in the renin-angiotensin- genders. The study by Lima, Menezes and Peixoto (2018)
aldosterone system (Ormazabal et al., 2018). found an average initial capillary glycemia of 213.9 mg
It is important to keep in mind that DM is / dL, shifting to 138.6 mg / dL at the final evaluation.
characterized as a heterogeneous group of metabolic
disorders that presents hyperglycemia, due to defects
in the action of insulin or in the secretion of insulin.
This chronic disorder in glucose metabolism, with
persistent increase in glycemia, can trigger acute or
chronic complications in the cardiovascular, renal and
neurological system (Kahn, Cooper, Del Prato, 2014;
Francisco et al., 2018).
As for the time of diagnosis of DM2, 68.75% were
diagnosed more than 5 years ago and 31.75% less than
five years ago. Bernini et al. (2017) showed that 30.5% of
patients had less than five years of diagnosis, while those
FIGURE 2 - Mean and standard deviation of glycemia of
diagnosed more than five years ago were around 69.5%. patients between the 1st to 4th collection (n=16).
This prevalence has increased substantially over the last
decades due to several factors such as sedentary lifestyle,
higher rate of urbanism, obesity, inadequate diet (diets Regarding our results, although there was no
rich in simple carbohydrates), population aging (Bernini statistical difference between the collections performed,
et al., 2017). When asked about performing laboratory glycemic averages show that better knowledge regarding
tests, approximately 56.25% said they performed routine DM, whether through educational pamphlets, lectures,
tests at least once a year and 43.75% more than once a home monitoring, can bring positive results to the
year (Table I). patient’s health (Lima, Menezes, Peixoto, 2018; Salinero-
Braz. J. Pharm. Sci. 2022;58: e20497 Page 5/9
Misma Silva Cruz, Ingrid Cristina Ferreira da Silva, Jéssica Silva Gonçalves Miguez, Mariana Pirani Rocha Machado
Fort et al., 2011), since glycemic levels decreased in the four assessments of systolic and diastolic pressure
last collection. at different times, with mean and standard deviation
It is emphasized that in the diagnosis, the normal shown in Table II.
glycemia value is <100 mg/dL fasting for non-diabetic Despite all monitoring related to blood pressure
patients. As a metabolic control goal for the patients with levels, there was no statistical difference between the
already established DM, ADA et al. (2020) recommends different measurements. However, a noticeable tendency
pre-prandial glycemia between 80 to 130mg/dL and that these parameters decreased was observed during the
postprandial less than 180 mg/dL, showing that the meetings held. Because patients do not exert control and
participants did not have adequate control of glucose levels. care over blood pressure maintenance the levels tend
to be
Diabetic and concomitantly hypertensive patients out of control. Therefore, if there was regular monitoring,
represented 87.5% (n=14), 92.85% were women (n = 13) the number of comorbidities and complications would
and only 7.15% were men (n = 1) (Figure 3). Regarding drastically be reduced.
the prevalence being higher in the female audience, also
found by Fagundes, Corso and González-Chica (2017), TABLE II - Mean and standard deviation of blood pressure
that showed a total of 68.6% of women, this data can (BP) of patients performed during collections and home visits
also be explained by these patients’ greater demand for
health services (Schlichthorst et al., 2016). Measurement Systolic pressure Diastolic pressure
(BP) (mmHg) (mmHg)
1 134.00 ± 17.11 83.00 ± 9.46
2 133.00 ± 15.37 84.00 ± 12.63
3 135.00 ± 15.04 89.00 ± 12.37
4 131.00 ± 11.47 83.00 ± 6.19
Costa (2013), presented in his work the importance
of monitoring, guidance, attention to these patients,
in which educational practices were carried out by
lectures, guidelines and questionnaires about diets,
FIGURE 3 – Percentage (%) of hypertensive and diabetic
medications, among other procedures. It was observed
patients by gender (n=14), related to the total number of study that over the course of 5 months of our study, there
participants, n=16. was an increase in the number of patients who were
interested in participating in the project, which showed
In addition, it is known that the number of their greater concern in relation to health. Thus, blood
hypertensive patients in Brazil has increased 14.2% in ten glucose and blood pressure levels, when accompanied
years, from 22.5% in 2006 to 25.7% in 2016, with a higher by the pharmacist, in addition to supporting adherence
number of diagnoses in women (Ministério da Saúde, to therapy, represent an important tool in the prevention
2017). From 1990 to 2018 the diagnoses of hypertension of diabetic complications. The importance of health
cases increased from 50% to 75%, showing the health education for improving the quality of life of the
teams’ greater performance and the population looking diabetic patient is highlighted, thus avoiding, biological
for these services (Jardim et al., 2018). complications (Salinero-Fort et al., 2011). Thus, this
As previously mentioned, there was a high professional can perform pharmacotherapeutic follow-up,
prevalence of SAH (87.5%) in the study participants, with self-care instruction for the prevention and treatment
in addition to being diagnosed with DM. As for blood of the disease, performing the capillary blood glucose
pressure measurements, these patients underwent test (Alayoub et al., 2018).
Page 6/9 Braz. J. Pharm. Sci. 2022;58: e20497
Prevalence of hypertension and obesity in patients with type 2 Diabetes Mellitus
The anthropometric parameters (Table III) showed patients are twice as likely to have hypertension. In
that the patients’ BMI of 89.4% was above normal addition, hypertensive patients usually have insulin
standards, with the male mean of 34.1±4.6 representing resistance and are at greater risk of acquiring diabetes
grade I obesity and the female mean of 29.3±3.6 indicating than normotensive people. The main problem of
the classification as overweight. In addition, 100% of this association is morbidity and mortality due to
the sample had high waist circumference values, the cardiovascular disease, which share similar risk factors
male average was 127.0±4.6 and the female average of such as atherosclerosis, endothelial dysfunction,
104.0±11.3 indicating a very high risk for cardiovascular inflammation and vascular remodeling, dyslipidemia
diseases, which clearly shows the risks of metabolic (Jardim et al., 2018; Petrie, Guzik, Touyz, 2018). And,
complications associated with obesity. it has been estimated that approximately 90% of type
2 diabetic patients are overweight or obese (Daousi et
TABLE III - Anthropometric parameters of diabetic al., 2006), though certainly, not all obese individuals
individuals, according to gender develop type 2 diabetes and not all individuals with type
2 diabetes are obese (Maggio, Pi-Sunyer, 2003).
Anthropometric Men Women
parameters M ± SD M ± SD CONCLUSION
Body Weight (Kg) 101.0 ± 13.0 68.5 ± 9.8**
We know the importance of adhering to monitoring
BMI (Kg/m2) 34.1 ± 4.6 29.3 ± 3.6*
blood glucose and blood pressure, and controlling body
WC (cm) 127.0 ± 4.6 104.0 ± 11.3** weight, so as to not negatively interfere in the control
BMI = Body Mass Index; WC = Waist Circumference. of these chronic diseases and develop associated
Values expressed as mean (M) ± standard deviation (SD). health problems. Hence, multidisciplinary treatment
* p <0.05; ** p <0.0001 - compared to the male group
combined with monitoring can increase adherence to
(Student t test).
pharmacological and non-pharmacological treatment,
considered essential measures for clinical and laboratory
Statistically analyzing body weight, BMI and control.
WC, showed significant differences between men and This kind of research is necessary, as the goal is to
women, where all parameters decreased in women when promote health through the influence of the educational
compared to men. A study by Da Vitória and Guandalini process on disease control, which also highlights the
(2017), with type 2 diabetic patients treated in primary importance of multidisciplinary teams, including the
care, found that 74% of individuals were classified as pharmacist. Thereby, educational practices combined
obese through the BMI and WC assessment. Another with the primary care team can improve the prevention
study by Silveira et al. (2016), detected 49% of obesity of chronic diseases, solving and/or avoiding biological
in the evaluated sample, and it was observed that the complications, costly for the healthcare system.
prevalence of obesity was significantly higher in the
elderly who had previous DM diagnoses. These results ACKNOWLEDGMENTS
are associated with our found data, and shows obesity
as a fundamental factor in the pathogenesis of type 2 We would like to thank the health agents of the Basic
DM, reinforcing the importance of combating excess Health Units: São Sebastião and Fundação Rotariana, in
weight in the control of the disease, since excess weight the city of Barra do Garças-MT and all the participants.
is a trigger for comorbidities in diabetes and premature The Araguaia Valley University Center which was our
death of these patients (Wilding, 2014). structural support for laboratory and data analysis, and
Type 2 Diabetes mellitus and arterial hypertension the coordinators of the pharmacy and nutrition course
are commonly associated syndromes, since diabetic who supported us in carrying out this work.
Braz. J. Pharm. Sci. 2022;58: e20497 Page 7/9
Misma Silva Cruz, Ingrid Cristina Ferreira da Silva, Jéssica Silva Gonçalves Miguez, Mariana Pirani Rocha Machado
Laar AK, Adler AJ, Kotoh AM, Legido-Quigley H, LangeI
REFERENCES
L, Perel P, et al. Health system challenges to hypertension
and related non-communicable diseases prevention and
ADA, American Diabetes Association. 6. Glycemic Targets: treatment: perspectives from Ghanaian stakeholders. BMC
Standards of Medical Care in Diabetes—2020. Diabet Care. Health Serv Res. 2019;19(693):1-13.
2020;43(1):S66-S76.
Lee MK, Blumberg B. Transgenerational effects of
Alayoub, H, Curran S, Coffey M, Hatunic M, Higgins M. obesogens. Basic Clin Pharmacol Toxicol. 2019;125(3):44-57.
Assessment of the effectiveness of group education on
knowledge for women with newly diagnosed gestational Lima RF, Machado AV, Rebelo FM, Naves JDOS, Lavich TR,
diabetes. Ir J Med Sci (1971-). 2018;187(1):65-68. Dullius J. Interações medicamentosas potenciais em diabéticos
tipo 2 participantes de um programa de educação em saúde.
Bernini LS, Barrile SR, Mangili AF, Arca EA, Correr R, Infarma Ciências Farmacêuticas. 2015; 27(3):160-167.
Ximenes MA, et al. O impacto do Diabetes Mellitus na
qualidade de vida de pacientes da Unidade Básica de Saúde. Lima CR, Menezes IHCF, Peixoto MRG. Educação em
Cad Bras Ter Ocup. 2017;25(3):533-541. saúde: avaliação de intervenção educativa com pacientes
diabéticos, baseada na teoria social cognitiva. Ciênc Educ.
Costa MM. A baixa adesão de pacientes hipertensos no 2018;24(1):141-156.
programa hiperdia, um problema na unidade de saúde
da família Lagoa das Flores, Vitória da Conquista-BA. Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes.
[dissertation]. Campo Grande: Universidade Federal de Mato Endocrinol Metab Clin North Am. 2003;32(1):805–822.
Grosso do Sul, Atenção Básica em Saúde da Família; 2013.
Malfatti CRM, Assunção AN. Hipertensão arterial e
Daousi C, Casson IF, Gill GV, MacFarlane IA, Wilding JP, diabetes na estratégia de Saúde da Família: uma análise da
Pinkney JH. Prevalence of obesity in type 2 diabetes in frequência de acompanhamento pelas equipes de Saúde da
secondary care: association with cardiovascular risk factors. Família. Ciênc Saúde Colet. 2011;16(1):1383-1388.
Postgrad Med J. 2006;82(1):280–84.
Malta DC, Bernal RTI, Souza MFM, Szwarcwald CL, Lima
Duarte APP, Rodrigues PRM, Ferreira MG, Cunha MG, Barros MBA. Social inequalities in the prevalence
DB, Moreira NF, Sichieri R, et al. Socio-economic and of self-reported chronic non-communicable diseases in
demographic characteristics associated with risk behaviour Brazil: national health survey 2013. Int J Equity Health.
patterns for chronic non-communicable diseases in Brazil: 2016;15(153): 1-11.
data from the National Health Survey, 2013. Public Health
Marinho NBP, Vasconcelos HCA, Alencar AMPG, Almeida
Nutr. 2019;22(11):2083-2091.
PC, Damasceno MMC. Risk for type 2 diabetes mellitus and
Fagundes CN, Corso ACT, González-Chica DA. Perfil associated factors. Acta Paul Enferm. 2013;26(6):569-574.
Epidemiológico De Hipertensos E Diabéticos Cadastrados
Ministério da Saúde - Brasil [homepage on the internet].
Na Atenção Básica Em Saúde, Florianópolis-Sc/
Saúde: Hábitos dos brasileiros impactam no crescimento da
Epidemiological Profile Of Hypertensive And Diabetics
obesidade e aumenta a prevalência de diabetes e hipertensão.
Registered In Basic Health Care, Florianópolis-SC. Rev Pesq
2017. [acess in 23 Mar 2020]. Avaiable link: http://portalms.
Saúde. 2017;18(1):28-34.
saude.gov.br.
Francisco PMSB, Segri NJ, Borim FSA, Malta DC.
Munger MA. Polypharmacy and Combination Therapy
Prevalência simultânea de hipertensão e diabetes em idosos
in the Management of Hypertension in Elderly Patients
brasileiros: desigualdades individuais e contextuais. Ciênc
with Co-Morbid Diabetes Mellitus. Drugs Aging.
Saúde Colet. 2018; 23(11):3829-3840.
2010;27(1):871–883.
IDF, International Diabetes Federation. Diabetes Atlas - 8th
NCEP, National Cholesterol Education Program. Expert
Edition. Brussels: International Diabetes Federation; 2017.
Panel on Detection, Evaluation, and Treatment of High
Jardim TV, Inuzuka S, Galvão L, Negretto LAF, Oliveira Blood Cholesterol in Adults (Adult Treatment Panel III).
RO, Sá WF, et al. Multidisciplinary treatment of patients JAMA. 2001;285(19):2486–2497.
with diabetes and hypertension: experience of a Brazilian
Noale M, Veronese N, Cavallo Perin P, Pilotto A, Tiengo A,
center. Diabetol Metab Syndr. 2018;10(3):1-8.
Crepaldi G, Maggi S. Polypharmacy in elderly patients with
Kahn SE, Cooper ME, Del Prato S. Pathophysiology and type 2 diabetes receiving oral antidiabetic treatment. Acta
treatment of type 2 diabetes: perspectives on the past, Diabetol. 2016;53(1):323–330.
present, and future. The Lancet. 2014;383(9922):1068-1083.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C,
Zuñiga FA. Association between insulin resistance and the
Page 8/9 Braz. J. Pharm. Sci. 2022;58: e20497
This is an open-access article distributed under the terms of the Creative Commons Attribution License.
Prevalence of hypertension and obesity in patients with type 2 Diabetes Mellitus
development of cardiovascular disease. Cardiovasc Diabetol. diseases in Brazil: burden and current challenges. Lancet.
2018;17(122):1-14. 2011;377(9781):1949-1961.
Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, Secoli SR. Polifarmácia: interações e reações adversas
and Cardiovascular Disease: Clinical Insights and Vascular no uso de medicamentos por idosos. Rev Bras Enferm.,
Mechanisms. Can J Cardiol. 2018;34(5):575-584. 2010;63(1):136-140.
Pinho L, AguiarAPS, Oliveira MR, Barreto NAP, Silva DF, Araújo NCS, Campos EAD. Perfil dos pacientes
Ferreira CMM. Hipertensão e dislipidemia em pacientes hipertensos e diabéticos atendidos na Atenção Básica.
diabetes mellitus tipo 2: uma revisão integrativa. Renome. REFACI. 2018;2(2):1-11.
2015;4(1):87-101.
Silva MDCC, de Araújo Soares K, Leal CS, da Silva DV, da
Porto EF, Souza JDS, Marques NDM. Frequency of Stroke and Rocha Filho DR. Avaliação epidemiológica dos pacientes
Cardiovascular Events in Diabetic and Hypertensive Patients diabetes mellitus e hipertensão arterial. JIBI. 2018;3(1):25-30.
- Follow up 15 years. J Diab Obes Metab. 2020;3(1):116.
Silveira EA, Vieira LL, Jardim TV, Souza JD. Obesidade em
Ralston J, Brinsden H, Buse K, Candeias V, Caterson I, Idosos e sua Associação com Consumo Alimentar, Diabetes
Hassell T, et al. Time for a new obesity narrative. Lancet. Mellitus e Infarto Agudo do Miocárdio. Arq. Bras Cardiol.
2018;392(10156):1384-1386. 2016;107(6):509-517.
Rocha NS, Souza MP, de Oliveira Paegle ACR, dos Santos Tschiedel B. Complicações Crônicas do Diabetes. JMB.
ACO. Avaliação do controle glicêmico pela glicemia capilar 2014;102(5):7-11.
de usuários diabéticos tipo 2, em um serviço de atenção
básica no município de Recife. Ciênc Biol Saúd Unit. 2017; Upadhyay J, Farr O, Perakakis N, Ghaly W, Mantzoros C.
3(1): 75-86. Obesity as a Disease. Med Clin North Am. 2018;102(1):13-33.
Salinero-Fort MA, Pau ECS, Arrieta-Blanco FJ, Abanades- Vitória AG, Guandalini VR. Qualidade da dieta e estado
Herranz JC, Martín-Madrazo C, Rodés-Soldevila B, et al. nutricional de diabéticos tipo 2 atendidos na atenção primária
Effectiveness of PRECEDE model for health education do município de Vitória, Espírito Santo. Rev Baiana Saúde
on changes and level of control of HbA1c, blood pressure, Pública. 2016;40(4):909-923.
lipids, and body mass index in patients with type 2 Diabetes Veronin MA. An atypical case of extreme polypharmacy.
Mellitus. BMC Public Health. 2011;11(267):1-9. Drug Healthc Patient Saf. 2022;14:19-26.
Santos PCJL. Atenção farmacêutica: contexto atual, exames WHO, World Health Organization [homepage on the
laboratoriais e acompanhamento farmacoterapêutico. 1 internet] Physical status: the use of and interpretation of
Edition. São Paulo: Atheneu; 2016. anthropometry, report of a WHO expert committee. World
SBC Diretrizes, Sociedade Brasileira de Cardiologia Health Organization. 1995. [Acess in 10 feb 2020]. Link:
[homepage on the internet]. Conceituação, epidemiologia e avaiable https://apps.who.int/iris/handle/10665/37003.
prevenção primária. 2017. [acess in 15 apr 2020]. Avaiable Wilding JPH. The importance of weight management in type
link: http://www.departamentos.cardiol.br. 2 diabetes mellitus. Int J Clin Pract. 2014;68(6):682-691.
SBD Diretrizes, Sociedade Brasileira de Diabetes [homepage Received for publication on 23th June 2020
on the internet]. 2019-2020. [acess in 27 May 2020]. Avaiable Accepted for publication on 17th October 2020
link: https://www.diabetes.org.br/
SBD Diretrizes, Sociedade Brasileira de Diabetes [homepage
on the internet]. Classificação etiológica do Diabetes Mellitus.
2014-2015. [acess in 13 feb 2020]. Avaiable link: http://www.
diabetes.org.br.
Schlichthorst M, Sanci LA, Pirkis J, Spittal MJ, Hocking
JS. Why do men go to the doctor? Socio-demographic
and lifestyle factors associated with healthcare utilisation
among a cohort of Australian men. BMC Public Health.
2016;16(1028):81-90.
Schmidt MI, Duncan BB, Silva GA, Menezes AM, Monteiro
CA, Barreto SM, et al. Chronic non-communicable
Braz. J. Pharm. Sci. 2022;58: e20497 Page 9/9
You might also like
- Summary - Granovetter (1985) Economic Action and Social StructureDocument2 pagesSummary - Granovetter (1985) Economic Action and Social StructureSimon Fiala100% (12)
- Bio Eoc Review Session 1 Questions 11-12Document6 pagesBio Eoc Review Session 1 Questions 11-12api-269873615No ratings yet
- Format PengkajianDocument8 pagesFormat PengkajianHandiniNo ratings yet
- Metabolic Syndrome and Psoriatic Arthritis Among Patients With Psoriasis Vulgaris: Quality of Life and PrevalenceDocument8 pagesMetabolic Syndrome and Psoriatic Arthritis Among Patients With Psoriasis Vulgaris: Quality of Life and PrevalenceVictor CastilloNo ratings yet
- KAP Towards DMDocument10 pagesKAP Towards DMHabtamu Wondifraw100% (1)
- Alencar 2010Document6 pagesAlencar 2010Tín NguyễnNo ratings yet
- Prevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateDocument7 pagesPrevalence of Cardiovascular Risk Factors in Two Brazilian Quilombola Communities in Southwest Bahia StateIJAERS JOURNALNo ratings yet
- Added Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataDocument6 pagesAdded Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataNavaneethan GnanadesiganNo ratings yet
- 8 Mansour - Factors - Associated - With - Glycemic - Control - in - Type - 2 - Diabetic - Patients - in - Saudi - ArabiaDocument5 pages8 Mansour - Factors - Associated - With - Glycemic - Control - in - Type - 2 - Diabetic - Patients - in - Saudi - Arabiabangd1f4nNo ratings yet
- Prediction of Type 2 Diabetes Mellitus Using Hematological Factors Based On Machine Learning Approaches: A Cohort Study AnalysisDocument11 pagesPrediction of Type 2 Diabetes Mellitus Using Hematological Factors Based On Machine Learning Approaches: A Cohort Study Analysis21bit20No ratings yet
- Artículo Redalyc 32751053016Document25 pagesArtículo Redalyc 32751053016Angélica Oyola FernándezNo ratings yet
- Adua Et Al-2017-Clinical and Translational MedicineDocument11 pagesAdua Et Al-2017-Clinical and Translational MedicineSam Asamoah SakyiNo ratings yet
- Jurnal LepraDocument7 pagesJurnal LepraDipa Zoda HelfandoNo ratings yet
- Literature Review DiabetesDocument5 pagesLiterature Review Diabetesukefbfvkg100% (1)
- 2017 Subinical DiabetesDocument24 pages2017 Subinical DiabetesLuís Mauricio LimaNo ratings yet
- JUrnal AurinaDocument8 pagesJUrnal AurinaRahmiyantiNo ratings yet
- Presentation and Character For Adult Patients With Diabetes in LibyaDocument8 pagesPresentation and Character For Adult Patients With Diabetes in LibyaMediterr J Pharm Pharm SciNo ratings yet
- 0104 1169 Rlae 28 E3369Document10 pages0104 1169 Rlae 28 E3369surya rakhmat hidayatNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleRicardo Joshua RojasNo ratings yet
- 2181 2407 3 PBDocument18 pages2181 2407 3 PBFahrika Luthfi AfiqohNo ratings yet
- Content ServerDocument11 pagesContent ServerRachma FadillahNo ratings yet
- Pi Is 2589537019301877Document2 pagesPi Is 2589537019301877prince BoadiNo ratings yet
- Research Proposal IntroductionDocument8 pagesResearch Proposal IntroductionIsaac OmwengaNo ratings yet
- Burden of Cardiovascular Diseases Attributable ToDocument11 pagesBurden of Cardiovascular Diseases Attributable ToAnindya Anjas PutriaviNo ratings yet
- Associations of Diabesity With All Cause and Cardiovascular Disease MortalityDocument10 pagesAssociations of Diabesity With All Cause and Cardiovascular Disease Mortalityluis sanchezNo ratings yet
- Prevalence of Undiagnosed and Uncontrolled Diabetes Mellitus Among Adults in South ChennaiDocument5 pagesPrevalence of Undiagnosed and Uncontrolled Diabetes Mellitus Among Adults in South ChennaiVishakha BhosaleNo ratings yet
- Shenes Thompson Final Draft For Ethical ApprovalDocument36 pagesShenes Thompson Final Draft For Ethical ApprovalKaif AliNo ratings yet
- Variability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.Document12 pagesVariability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.franciscoNo ratings yet
- Final Pint ResearchDocument90 pagesFinal Pint ResearchNhelia Santos BañagaNo ratings yet
- Prevalence of Diabetes Mellitus in Patients Seeking Medical Care at Morogoro Regional Referral Hospital in TanzaniaDocument8 pagesPrevalence of Diabetes Mellitus in Patients Seeking Medical Care at Morogoro Regional Referral Hospital in TanzaniaEmmanuel MpaliyeNo ratings yet
- Afsana Afroz, Khurshid Alam, Mohammed J Alramadan, MD Nassif Hossain, Hasina Akhter Chowdhury, Liaquat Ali, Dianna J Magliano, Baki BillahDocument7 pagesAfsana Afroz, Khurshid Alam, Mohammed J Alramadan, MD Nassif Hossain, Hasina Akhter Chowdhury, Liaquat Ali, Dianna J Magliano, Baki BillahS1 FARMASI STIKESNAS ANGKATAN 2 2017No ratings yet
- Article 233554Document11 pagesArticle 233554رقية ياسينNo ratings yet
- 1. Utama nutrients-15-00430Document15 pages1. Utama nutrients-15-00430besti verawatiNo ratings yet
- 30IJAERS 06202035 Perceptionsof PDFDocument8 pages30IJAERS 06202035 Perceptionsof PDFIJAERS JOURNALNo ratings yet
- Evaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyDocument7 pagesEvaluation of Medical Care For Diabetic and Hypertensive Patients in Primary Care in Mexico: Observational Retrospective StudyMirna Liliana Carmona GarciaNo ratings yet
- Changes in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyDocument6 pagesChanges in Glycemic Control From 1996 To 2006 Among Adults With Type 2 Diabetes: A Longitudinal Cohort StudyReny NapitupuluNo ratings yet
- BMJ Open 2013 MorganDocument8 pagesBMJ Open 2013 Morganjft842No ratings yet
- 2024 APRU Case Comp Challenge Final2Document10 pages2024 APRU Case Comp Challenge Final2AnneAyushaNo ratings yet
- Health Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesDocument9 pagesHealth Beliefs, Self-Care Behaviors and Quality of Life in Adults With Type 2 DiabetesgamzeNo ratings yet
- Burden of DiabetesDocument7 pagesBurden of DiabetesNaga LakshmiNo ratings yet
- Retinopatía DiabéticaDocument7 pagesRetinopatía DiabéticaDIANE EDITH LUNA TOPETENo ratings yet
- Prevalencia de Diabetes e Hiperglucemia Intermedia en Adultos. Centroamerica. Diabetescare2012Document3 pagesPrevalencia de Diabetes e Hiperglucemia Intermedia en Adultos. Centroamerica. Diabetescare2012Kevin CastilloNo ratings yet
- Spatio-Temporal Trend in Detections of Diabetes Mellitus and Systematic Arterial Hypertension in IMSS Users, 2004-2019Document11 pagesSpatio-Temporal Trend in Detections of Diabetes Mellitus and Systematic Arterial Hypertension in IMSS Users, 2004-2019MIGUEL ERNESTO GONZALEZ CASTANEDANo ratings yet
- DNHE4 Project Proposal 2201393222Document17 pagesDNHE4 Project Proposal 2201393222Surya Dharshni HomoeoNo ratings yet
- Diabetes Mellitus in Brazil: Risk Factors, Classification and ComplicationsDocument4 pagesDiabetes Mellitus in Brazil: Risk Factors, Classification and Complicationsjoy parimalaNo ratings yet
- TransleteDocument85 pagesTransleteFeliany BiroNo ratings yet
- A Study Assess The Level of Stress Among Patients With Type II Diabetes Mellitus in Relation To Level of Blood Sugar at Nerkundrum I UPHCDocument4 pagesA Study Assess The Level of Stress Among Patients With Type II Diabetes Mellitus in Relation To Level of Blood Sugar at Nerkundrum I UPHCEditor IJTSRDNo ratings yet
- Prediabetes Education To Prevent The Progression To Type 2 DiabetDocument20 pagesPrediabetes Education To Prevent The Progression To Type 2 DiabetEndah WulandariNo ratings yet
- Pengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas HidupDocument8 pagesPengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas Hidupilma adilla syahidaNo ratings yet
- Pengaruh Hipoglikemia Pada Pasien Diabetes MelitusDocument8 pagesPengaruh Hipoglikemia Pada Pasien Diabetes Melitusmail junkNo ratings yet
- Anemia in Patients With Type 2 Diabetes MellitusDocument9 pagesAnemia in Patients With Type 2 Diabetes MellitusmitchelNo ratings yet
- 349 FullDocument3 pages349 FullsenkonenNo ratings yet
- Diabetes Mellitus: A Review On Pathophysiology, Current Status of Oral Medications and Future PerspectivesDocument23 pagesDiabetes Mellitus: A Review On Pathophysiology, Current Status of Oral Medications and Future PerspectivesGhede DhayatNo ratings yet
- Nutritional Assessment of Older Adults With Diabetes MellitusDocument8 pagesNutritional Assessment of Older Adults With Diabetes MellitusCarlo EspadinNo ratings yet
- Anesthesia Management On Perioperative With DM Patients - A Literature ReviewDocument9 pagesAnesthesia Management On Perioperative With DM Patients - A Literature ReviewvienvienkkNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument14 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaAnna StimNo ratings yet
- Risk Factors of Type 2 DiabetesDocument13 pagesRisk Factors of Type 2 DiabetesLalu Angling PatayaNo ratings yet
- Jurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. . No 20 . E-Issn: 2087-0035Document9 pagesJurnal Media Keperawatan: Politeknik Kesehatan Makassar Vol. . No 20 . E-Issn: 2087-0035nurfitriaNo ratings yet
- Low Extremity AmputationDocument5 pagesLow Extremity AmputationMuhammad RizqiNo ratings yet
- Effect of Diet On Type 2 Diabetes Mellitus: A ReviewDocument7 pagesEffect of Diet On Type 2 Diabetes Mellitus: A ReviewTowo RottenNo ratings yet
- Healthcare 09 00832Document9 pagesHealthcare 09 00832cheatingw995No ratings yet
- Ampalaya: Nature's Remedy for Type 1 & Type 2 DiabetesFrom EverandAmpalaya: Nature's Remedy for Type 1 & Type 2 DiabetesRating: 5 out of 5 stars5/5 (1)
- Danfoss Vane Tip LUG SylaxDocument18 pagesDanfoss Vane Tip LUG SylaxmaggamNo ratings yet
- (The Logic of Political Survival) .Bruce Bueno de Mesquita, Alastair Smith, Randolph M. Siverson, James D. Morrow PDFDocument551 pages(The Logic of Political Survival) .Bruce Bueno de Mesquita, Alastair Smith, Randolph M. Siverson, James D. Morrow PDFjasonnijmh100% (1)
- Appendix-1 Piping Isometric With Node Numbers: Saudi Arabian Oil CompanyDocument1 pageAppendix-1 Piping Isometric With Node Numbers: Saudi Arabian Oil CompanyJohn BuntalesNo ratings yet
- Propylene (Asia-Pacific) 31 Jan 2020Document5 pagesPropylene (Asia-Pacific) 31 Jan 2020Wira Nata S SinuhajiNo ratings yet
- Cema Belt Conveyors For Bulk Materials Vol 1: Traducir Esta PáginaDocument6 pagesCema Belt Conveyors For Bulk Materials Vol 1: Traducir Esta PáginaDIEGO FERNANDO CADENA ARANGONo ratings yet
- Nisbet Idea of Progress PDFDocument31 pagesNisbet Idea of Progress PDFHernan Cuevas ValenzuelaNo ratings yet
- English A Status ReportDocument3 pagesEnglish A Status ReportNataliasol07No ratings yet
- Logix SERCOS Tuning Tips v1.02 1Document6 pagesLogix SERCOS Tuning Tips v1.02 1José AlanizNo ratings yet
- Tube ClampDocument113 pagesTube ClampAmitava SilNo ratings yet
- Engineering Mathematics Questions and Answers - Laplace Transform by Properties - 1Document9 pagesEngineering Mathematics Questions and Answers - Laplace Transform by Properties - 1RAHUL SOLANKENo ratings yet
- The Handmaid's Tale ContextDocument2 pagesThe Handmaid's Tale ContextBeheshtaNo ratings yet
- Artificial Retina: Presented byDocument6 pagesArtificial Retina: Presented bySai KrishnaNo ratings yet
- Customer Service AssignmentDocument2 pagesCustomer Service AssignmentJoe Kau Zi YaoNo ratings yet
- Social Dimensions in Education Part 1Document4 pagesSocial Dimensions in Education Part 1Laurice Marie GabianaNo ratings yet
- A Project Proposal of Online Enrollment in WmsuDocument9 pagesA Project Proposal of Online Enrollment in WmsuClairole Marie Quilantang100% (2)
- CPRG - V4 - Advanced Issues in Contract PricingDocument304 pagesCPRG - V4 - Advanced Issues in Contract Pricingjarod437No ratings yet
- List of Figures: Inter State Bus Terminal, DwarkaDocument4 pagesList of Figures: Inter State Bus Terminal, Dwarkamalay SRIVASTAVANo ratings yet
- KTM ContentsDocument4 pagesKTM Contentstahaqureshi123No ratings yet
- JADWAL KULIAH TPB SMT GASAL TA 2020 2021 Rev 5Document49 pagesJADWAL KULIAH TPB SMT GASAL TA 2020 2021 Rev 5shin yongriNo ratings yet
- DETAILED LESSON PLAN SubatomicparticlesDocument16 pagesDETAILED LESSON PLAN SubatomicparticlesMary Rose Ramos100% (3)
- fmamsmlmflmlmlllmmlDUK DOSEN UNTAD AGUSTUS 2013bhvffyfDocument117 pagesfmamsmlmflmlmlllmmlDUK DOSEN UNTAD AGUSTUS 2013bhvffyfIsmail Sholeh Bahrun MakkaratteNo ratings yet
- Reading Comprehension Power ToolsDocument6 pagesReading Comprehension Power ToolsCarlos Alberto Lopez MartinezNo ratings yet
- 3374 PDFDocument10 pages3374 PDFCornel DumitruNo ratings yet
- Why Critical Thinking Is ImportantDocument3 pagesWhy Critical Thinking Is ImportantMehreen KandaanNo ratings yet
- GCC Lab Manual Mahesh Kumar PDFDocument130 pagesGCC Lab Manual Mahesh Kumar PDFMohan ReddyNo ratings yet
- Msi MPG b550 Gaming PlusDocument68 pagesMsi MPG b550 Gaming PlusMarvelous WololoNo ratings yet
- Pathway To English Peminatan 3 Bab 3Document9 pagesPathway To English Peminatan 3 Bab 3Agung PrasetyoNo ratings yet
- Petroleum & Petrochemicals Test Method Capabilities: Intertek Caleb Brett 1Document18 pagesPetroleum & Petrochemicals Test Method Capabilities: Intertek Caleb Brett 1Eng-sadeq HesseinNo ratings yet