Professional Documents
Culture Documents
Arachnoid Cysts Review
Arachnoid Cysts Review
Uploaded by
helbertpalmieroCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arachnoid Cysts Review
Arachnoid Cysts Review
Uploaded by
helbertpalmieroCopyright:
Available Formats
Neurosurg Focus 22 (2):E7, 2007
Arachnoid cysts: case series and review of the literature
GUSTAVO PRADILLA, M.D.,1 AND GEORGE JALLO, M.D.1,2
Departments of 1Neurosurgery and 2Pediatrics, The Johns Hopkins School of Medicine,
Baltimore, Maryland
Object. Arachnoid cysts are commonly encountered fluid collections in the central nervous system. Recent
advances in neuroimaging have translated into an increased detection of these cysts; that is, diagnoses can be made
more frequently at earlier stages. Significant advances have also been made in the surgical management of these
lesions. The authors report on a case series that illustrates the diverse forms of presentation and the treatment modal-
ities commonly used for arachnoid cysts.
Methods. Between January 2002 and December 2006, 20 patients with arachnoid cysts underwent surgery per-
formed by the senior author at The Johns Hopkins Hospital. Seventy percent of the cysts were supratentorial, 5%
infratentorial, and 25% spinal. All diagnoses were confirmed on neuroimaging, surgery, and histological examina-
tion. Included in the study were 12 male (60%) and eight female (40%) patients, ranging in age from 2 weeks to 39
years (mean age 10.9 years) at the time of surgery.
Symptoms at presentation included headache (41%), weakness (23%), seizure (14%), hydrocephalus (9%), scolio-
sis (4%), cognitive decline (4%), and visual loss (4%). Twenty-five percent of the cysts were sylvian, 20% intraven-
tricular, and 20% suprasellar. Supratentorial cysts were treated endoscopically in 73% of patients and with open resec-
tion in the remaining 27%. Complications included spasticity, hemiparesis, cerebrospinal fluid leak, hydrocephalus,
and subdural hygroma. On follow-up evaluation, 60% of patients had stable cysts and improved symptoms, 13% com-
plete symptom resolution, and 13% stable symptoms.
All patients with spinal cysts underwent laminectomies and fenestration, and one cystosubarachnoid (CS) shunt was
placed. Cyst reaccumulation occurred in three patients; two patients required cystoperitoneal (CP) and CS shunts. No
deaths occurred.
Conclusions. Most arachnoid cysts are found incidentally and can be managed conservatively. Symptomatic
patients are surgical candidates. Treatments include CP shunt placement, craniotomy, or endoscopic fenestration,
and stereotactic aspiration. Recent advances in neurosurgical techniques and neuroendoscopy continue to favor fen-
estration over shunt insertion as the method of choice for initial cyst decompression.
KEY WORDS • arachnoid cystd • surgery • craniotomy • outcome
RACHNOID CYSTS are congenital collections of CSF The overall male/female predominance is approximately
A contained within the arachnoidal membrane and
subarachnoid space19 of the cisterns and major
cerebral fissures. Although some cysts remain stable, oth-
2:1. Multiple or bilateral arachnoid cysts are unusual, and
familial occurrence has been reported in only a few cases.9
An association between bilateral sylvian fissure arachnoid
ers can expand and compress surrounding structures, cysts and glutaric aciduria Type I has been demonstrated.14
prompting evaluation.3,19,24 Most of these lesions become Arachnoid cysts may result from either developmental
symptomatic in early childhood; hence, 60 to 90% of all defects or trauma. Congenital cysts appear to originate
patients with arachnoid cysts are children.8,11,12 from alterations in CSF flow in the early phase of sub-
In 1831 Bright4 first defined intracranial arachnoid arachnoid space formation.15 In some cases, these cysts are
cysts, describing them as “serous cysts forming in con- seen in patients with corpus callosum agenesis and mal-
nection with the arachnoid and apparently lying between formations of the cerebral venous systems, which suggest
its layers.” Overall, arachnoid cysts account for approxi- a more pronounced developmental defect. Traumatic
mately 1% of all intracranial mass lesions.1 Data from arachnoid cysts appear to occur following minor closed-
autopsy studies have shown a low incidence ranging from head injuries in infancy and can result from arachnoid
0.l to 0.7%, a rate that correlates with that in studies of cra- splitting within incomplete cisterns during infancy.
nial MR images, which show an incidence of 0.75%. Most Pathological examination usually reveals a cyst wall that
cysts are incidentally diagnosed during neuroimaging resembles normal arachnoid; however, the cyst location
after head trauma. Prenatal ultrasonography as well as in- seems to determine its pathological appearance. Whereas
creased access to computed tomography and MR imaging posterior fossa cysts display choroid plexus remnants,
has allowed cyst detection at earlier ages; hence, most suprasellar and prepontine cysts exhibit neuroglial ele-
cysts are recognized during the first two decades of life. ments that resemble those found on the floor of the third
ventricle.
Abbreviations used in this paper: CP = cystoperitoneal; CSF = Although most arachnoid cysts remain stable through-
cerebrospinal fluid; MR = magnetic resonance. out life, some can enlarge due to various mechanisms such
Neurosurg. Focus / Volume 22 / February, 2007 1
G. Pradilla and G. Jallo
as active CSF secretion from the cyst membrane,19 osmot- TABLE 2
ic gradients caused by a higher protein concentration in Locations of arachnoid cysts in 20 patients
the cyst fluid, or cyst contents communicating with the
subarachnoid space via ball-valve mechanisms that entrap Location No. (%)
CSF during Valsalva maneuvers.5,21,22 Cysts can rupture supratentorial
following minor trauma, resulting in subdural hygromas suprasellar region 4 (20)
and intracranial hypertension,1 and can occur in associa- lat ventricle 3 (15)
tion with traumatic subdural hematomas.16 Supratentorial 3rd ventricle 1 (5)
cysts are more frequently encountered, with nearly half of sylvian fissure 5 (25)
temporal lobe 1 (5)
all cysts occurring within the sylvian fissure.19 Less fre- infratentorial
quent locations include the interhemispheric fissure and midline region 1 (5)
the periclival region. Cysts of the suprasellar region are spinal
more commonly encountered in children than in adults.20 cervical region 2 (10)
We retrospectively report on a consecutive series of pa- thoracic region 2 (10)
tients with arachnoid cysts that were surgically treated by cervical-thoracic region 1 (5)
the senior author. Our data illustrate the common clinical
features encountered, available surgical options, compli-
cations, and patient outcomes after surgical treatment of underwent endoscopic fenestration. There were no post-
arachnoid cysts. operative complications directly related to the surgeries in
nine patients (60%) with intracranial cysts. Among the
Clinical Material and Methods remaining patients, one had persistent spasticity, one suf-
fered mild hemiparesis, one had a CSF leak, two had
Between January 2002 and December 2006, 20 patients hydrocephalus (one was treated with a second successful
with arachnoid cysts underwent surgery performed by the fenestration and the other with ventriculoperitoneal shunt
senior author at The Johns Hopkins Hospital. Fourteen of placement), and one patient had a subdural hygroma re-
the cysts were supratentorial (70%), one was infratentori- quiring bur hole drainage. On follow-up evaluation, two
al (5%), and five were spinal (25%). All diagnoses were patients (13.3%) demonstrated cyst reduction and com-
confirmed on neuroimaging, surgery, and histological plete symptom resolution, two patients (13.3%) had de-
examination. Tables 1 to 4 summarize cyst location, pre- creased cyst sizes and improved symptoms, nine patients
operative clinical symptoms, complications, and outcome. (60%) had stable cyst sizes with improvement in their
The study included 12 male (60%) and eight female symptoms, one patient (7%) had hydrocephalus due to
(40%) patients, ranging in age from 2 weeks to 39 years cyst increase and required placement of a ventriculoperi-
(mean age 10.9 years) at the time of surgery. toneal shunt, and one patient (7%) was lost to follow up.
Results Spinal Cysts
Symptoms at presentation included headache (41%), Spinal arachnoid cysts were present in five patients:
weakness (23%), seizures (14%), hydrocephalus (9%), sco- cervical and thoracic cysts in two patients each and a cer-
liosis (4%), cognitive decline (4%), and visual loss (4%). vical-thoracic cyst in one patient. All of these patients un-
No deaths occurred among patients in the study. derwent laminectomies and fenestration, and in one patient
Intracranial Cysts a cystosubarachnoid shunt was placed. Postoperatively,
reaccumulation of the cyst occurred in three patients, two
Fifteen patients presented with intracranial cysts: five in of whom required CP and cystosubarachnoid shunts and
the sylvian fissure (25%), four in the intraventricular re- one of whom had mild postoperative hemiparesis that
gion (20%), four (20%) in the suprasellar area, one in the improved. On follow-up evaluation, one patient had a de-
temporal lobe, and one in the infratentorial region. Where- creased cyst and improved symptoms, two had cysts that
as endoscopic fenestration was performed in 11 patients remained stable and controlled symptoms, one had cyst
(involving 73% of the supratentorial cysts), a direct ap- reaccumulation and stable symptoms, and one demon-
proach with marsupialization and fenestration of the cyst strated cyst expansion that required shunting.
was used in only four patients (involving 27% of the
supratentorial cysts). All patients with suprasellar lesions
Discussion
TABLE 1 Our data illustrate the diverse spectrum of presentations
Preoperative symptoms in 20 patients with arachnoid cysts
Symptom No. (%) TABLE 3
Treatments according to cyst location
headache 9 (41)
weakness 5 (23) Cyst Location Treatment No.
seizure 3 (14)
visual loss 1 (4) supratentorial craniotomy 4
cognitive decline 1 (4) endoscopic fenestration 11
hydrocephalus 2 (9) infratentorial craniotomy 1
scoliosis 1 (4) spinal laminectomy 5
2 Neurosurg. Focus / Volume 22 / February, 2007
Arachnoid cysts: case series and literature review
sels,8 and pathological diagnosis confirmation with a tis-
sue biopsy procedure. Fenestration tends to be especially
favored over shunting for cyst locations in which vital
structures may be injured during shunt placement or fol-
lowing cyst wall collapse.
Advantages of open cyst fenestration via craniotomy
include excision of the cyst wall, possible fenestration of
multiloculated cysts, and, in certain locations, fenestration
of the cyst into neighboring cisterns.10,17 Despite the ab-
sence of the immediate reexpansion of displaced struc-
tures on postoperative imaging, patients report rapid reso-
lution of symptoms such as headache. However, headaches
may return in 5 to 25% of patients because of cyst reaccu-
mulation.10,17,25
Upfront CP shunt insertion has been proposed in pa-
tients with concomitant or resultant hydrocephalus2,6–8,26
(based on reports of high reaccumulation rates following
fenestration6) as well as in those with arachnoid cyst–
related ventriculomegaly that fails to resolve after cyst
fenestration. Cystoperitoneal shunt placement remains an
appealing option given the simplicity of the surgical tech-
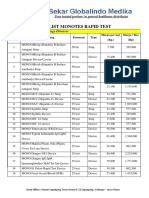
FIG. 1. Axial (A, C, and D) and sagittal (B) T1-weighted MR nique involved and the availability of intraoperative guid-
images showing arachnoid cysts. Left porencephalic arachnoid ance via ultrasonography or neuronavigation, but compli-
cyst in a 2-week-old patient (A and B). Suprasellar arachnoid cyst cations inherent to all CSF drainage systems must be
in an 11-month-old patient (C). Left sylvian arachnoid cyst in a six- considered. The development of slit-cyst syndrome (a
year-old patient (D). condition similar to slit-ventricle syndrome) is also possi-
ble following CP shunt placement and should be consid-
in patients with arachnoid cysts, available surgical op- ered on neurological deterioration in the patient. Reported
tions, and the complications and surgical outcomes in a rates of shunt revision in this patient population are
selected population treated by a single surgeon. Although approximately 30%.10,25
all patients underwent surgical treatment, not all arach- Endoscopic cyst fenestration has gained popularity with
noid cysts require surgical intervention.5 On patient pre- excellent reported outcomes.22,23 Magnetic resonance
sentation, clinical decision-making is based on sympto- imaging– or computed tomography–guided endoscope tra-
matology and neuroimaging findings. Patients with jectories are used, access to the cyst is gained via coagu-
asymptomatic or incidental cysts should be monitored lation of the outer cyst membrane, and generous cystocis-
clinically and with serial MR imaging. Surgical manage- ternostomies are performed.23 Neuroendoscopic access
ment should be considered only for increasing cysts caus- has also been used as a complement to open microsurgical
ing neural compression, hydrocephalus, or refractory fenestration.13 As this technique gains exposure, minimal-
symptoms attributable to mass effect. Postoperative cyst ly invasive fenestration may become the preferred surgi-
reaccumulation has been reported to occur in approxi- cal technique for accessible cysts.
mately 25% of patients (Fig. 1).17,25
Surgical treatment options remain controversial and
most commonly include either craniotomy, open fenestra- Conclusions
tion of the cyst, stereotactic cyst aspiration, endoscopic In summary, recent advances in, and greater access to,
cyst fenestration, or shunt placement. Fenestration through neuroimaging have increased the detection of arachnoid
either approach is often preferred to upfront shunt place- cysts. Most cysts are found incidentally and can be man-
ment to avoid shunt-related complications.2,17,18 Cra- aged conservatively with periodic imaging. Symptomatic
niotomy and endoscopic fenestration allow inspection of patients are candidates for surgical intervention via sever-
the cyst wall,2,12,18 coagulation of arachnoidal blood ves- al methods, including CP shunt placement, craniotomy,
endoscopic fenestration, and stereotactic aspiration. Re-
cent advances in neurosurgical techniques and neuroen-
TABLE 4 doscopy continue to favor fenestration over shunting as
Complications following surgery for arachnoid cysts
the method of choice for initial cyst decompression.
Complication No. of Cases References
none 11 1. Albuquerque FC, Giannotta SL: Arachnoid cyst rupture pro-
weakness 3 ducing subdural hygroma and intracranial hypertension: case
reaccumulation 5 reports. Neurosurgery 41:951–956, 1997
required shunt placement 3 2. Anderson FM, Segall HD, Caton WL: Use of computerized
CSF leak 1 tomography scanning in supratentorial arachnoid cysts. A
seizure 1 report on 20 children and four adults. J Neurosurg 50:
subural hygroma 1 333–338, 1979
Neurosurg. Focus / Volume 22 / February, 2007 3
G. Pradilla and G. Jallo
3. Becker T, Wagner M, Hofmann E, Warmuth-Metz M, Nadjmi 16. Prabhu VC, Bailes JE: Chronic subdural hematoma complicat-
M: Do arachnoid cysts grow? A retrospective CT volumetric ing arachnoid cyst secondary to soccer-related head injury: case
study. Neuroradiology 33:341–345, 1991 report. Neurosurgery 50: 195–198, 2002.
4. Bright R: Serous cysts in the arachnoid, in Rees, Orme, Brown, 17. Raffel C, McComb JG: To shunt or to fenestrate: which is the
Green (eds): Diseases of the Brain and Nervous System. Part best surgical treatment for arachnoid cysts in pediatric patients?
I. London: Longman Group Ltd, 1831, pp 437–439 Neurosurgery 23:338–342, 1988
5. Caemaert J, Abdullah J, Calliauw L, Carton D, Dhooge C, van 18. Raimondi AJ, Shimoji T, Gutierrez FA: Suprasellar cysts: sur-
Coster R: Endoscopic treatment of suprasellar arachnoid cysts. gical treatment and results. Childs Brain 7:57–72, 1980
Acta Neurochir (Wien) 119:68–73, 1992 19. Rengachary SS, Watanabe I: Ultrastructure and pathogenesis of
6. Ciricillo SF, Cogen PH, Harsh GR, Edwards MS: Intracranial intracranial arachnoid cysts. J Neuropathol Exp Neurol 40:
arachnoid cysts in children. A comparison of the effects of fen- 61–83, 1981
estration and shunting. J Neurosurg 74:230–235, 1991 20. Rengachary SS, Watanabe I, Brackett CE: Pathogenesis of in-
7. di Rocco C, Caldarelli M, di Trapani G: Infratentorial arachnoid tracranial arachnoid cysts. Surg Neurol 9:139–144, 1978
cysts in children. Childs Brain 8:119–133, 1981 21. Santamarta D, Aguas J, Ferrer E: The natural history of arach-
8. Galassi E, Tognetti F, Frank F, Fagioli L, Nasi MT, Gaist G: In- noid cysts: endoscopic and cine-mode MRI evidence of a slit-
fratentorial arachnoid cysts. J Neurosurg 63:210–217, 1985 valve mechanism. Minim Invasive Neurosurg 38:133–137,
9. Handa J, Okamoto K, Sato M: Arachnoid cyst of the middle cra- 1995
nial fossa: report of bilateral cysts in siblings. Surg Neurol 22. Schroeder HW, Gaab MR: Endoscopic observation of a slit-
16:127–130, 1981 valve mechanism in a suprasellar prepontine arachnoid cyst:
10. Harsh GR IV, Edwards MS, Wilson CB: Intracranial arachnoid case report. Neurosurgery 40:198–200, 1997
cysts in children. J Neurosurg 64:835–842, 1986 23. Schroeder HW, Gaab MR, Niendorf WR: Neuroendoscopic
11. Higashi S, Yamashita J, Yamamoto Y, Izumi K: Hemifacial approach to arachnoid cysts. J Neurosurg 85:293–298, 1996
spasm associated with a cerebellopontine angle arachnoid cyst 24. Smith RA, Smith WA: Arachnoid cysts of the middle cranial
in a young adult. Surg Neurol 37:289–292, 1992 fossa. Surg Neurol 5:246–252, 1976
12. Hoffman HJ, Hendrick EB, Humphreys RP, Armstrong EA: 25. Stein SC: Intracranial developmental cysts in children: treat-
Investigation and management of suprasellar arachnoid cysts. J ment by cystoperitoneal shunting. Neurosurgery 8:647–650,
Neurosurg 57:597–602, 1982 1981
13. Hopf NJ, Perneczky A: Endoscopic neurosurgery and endo- 26. Vaquero J, Carrillo R, Cabezudo JM, Nombela L, Bravo G:
scope-assisted microneurosurgery for the treatment of intracra- Arachnoid cysts of the posterior fossa. Surg Neurol
nial cysts. Neurosurgery 43:1330–1337, 1998 16:117–121, 1981
14. Jamjoom ZA, Okamoto E, Jamjoom AH, al-Hajery O, Abu-
Melha A: Bilateral arachnoid cysts of the sylvian region in Manuscript submitted January 15, 2007.
female siblings with glutaric aciduria type I. Report of two Accepted January 23, 2007.
cases. J Neurosurg 82:1078–1081, 1995 Address reprint requests to: George Jallo, M.D., Department of
15. Lemire R, Loeser J, Leech R, Alvord EJ: Normal and Neurosurgery, The Johns Hopkins University, School of Medicine,
Abnormal Development of the Human Nervous System. Harvey 811, 600 North Wolfe Street, Baltimore, Maryland 21287.
New York: Harper & Row, 1975 email: gjallo1@jhmi.edu.
4 Neurosurg. Focus / Volume 22 / February, 2007
You might also like
- (10920684 - Neurosurgical Focus) Endoscopic Management of Intracranial CystsDocument9 pages(10920684 - Neurosurgical Focus) Endoscopic Management of Intracranial Cystsrifki irsyadNo ratings yet
- Large Cerebral Arachnoid CystDocument2 pagesLarge Cerebral Arachnoid CystAtiquzzaman RinkuNo ratings yet
- (10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionDocument7 pages(10920684 - Neurosurgical Focus) Endovascular Management of Fusiform Aneurysms in The Posterior Circulation - The Era of Flow DiversionCharles MorrisonNo ratings yet
- Neurosurg-Focus-2010 5 Focus10149Document7 pagesNeurosurg-Focus-2010 5 Focus10149antonioskrasoudakisNo ratings yet
- Ajns 11 183Document11 pagesAjns 11 183Salomo MahaputraNo ratings yet
- Complications of Posterior Cranial Fossa PDFDocument7 pagesComplications of Posterior Cranial Fossa PDFemilio9fernandez9gatNo ratings yet
- Miyajima2000 PDFDocument6 pagesMiyajima2000 PDFFlorencia RubioNo ratings yet
- Possible Origin of Suprasellar Arachnoid Cysts: Neuroimaging and Neurosurgical Observations in Nine CasesDocument6 pagesPossible Origin of Suprasellar Arachnoid Cysts: Neuroimaging and Neurosurgical Observations in Nine CasesFlorencia RubioNo ratings yet
- Neuroendoscopic Management of Suprasellar Arachnoid Cysts, 2013Document12 pagesNeuroendoscopic Management of Suprasellar Arachnoid Cysts, 2013CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- Persistent Posttraumatic Cerebrospinal Fluid Leakage: J A. F, M.D., M J. E, M.D., L M. Q, R.NDocument5 pagesPersistent Posttraumatic Cerebrospinal Fluid Leakage: J A. F, M.D., M J. E, M.D., L M. Q, R.NAlexanderCahyadiNo ratings yet
- CSF LeaksDocument11 pagesCSF Leakssudheer joelNo ratings yet
- Large Arachnoid Cyst: T. Mondal K. Jagdish Kumar R. Anand N.K. Dubey D. SharmaDocument3 pagesLarge Arachnoid Cyst: T. Mondal K. Jagdish Kumar R. Anand N.K. Dubey D. SharmaJaya PrabhaNo ratings yet
- Agarwal 2016Document51 pagesAgarwal 2016Daniel Alfredo Tenorio GonzálezNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Craniopharyngiomas: Clinic Al PearlsDocument18 pagesCraniopharyngiomas: Clinic Al PearlsRanintha SurbaktiNo ratings yet
- William Ignace Wei Daniel Chua: Factol8Document21 pagesWilliam Ignace Wei Daniel Chua: Factol8Aldy BimaNo ratings yet
- Pi Is 0003497505012002Document5 pagesPi Is 0003497505012002Tri RachmadijantoNo ratings yet
- Leclerc 2020Document10 pagesLeclerc 2020Mella WarizkaNo ratings yet
- Medip, IJRMS-7729 ODocument7 pagesMedip, IJRMS-7729 ORagupathi MNo ratings yet
- Traumatic CSF LeaksDocument17 pagesTraumatic CSF LeaksNada AhmedNo ratings yet
- Surgical Outcome of Primary Intradural Surgical Outcome of Primary IntraduralDocument6 pagesSurgical Outcome of Primary Intradural Surgical Outcome of Primary Intraduralmazen alkarrasNo ratings yet
- Cornell A 2003Document13 pagesCornell A 2003dnazaryNo ratings yet
- 264 2011 Article 1480Document6 pages264 2011 Article 1480Paul Mendez AguilarNo ratings yet
- Surgical Treatment and Outcome of Cerebral CavernomaDocument12 pagesSurgical Treatment and Outcome of Cerebral CavernomaYovanka Naryai ManuhutuNo ratings yet
- Arachnoid Cyst Burst in Presence of Contralateral Nomura IV Subdural Hematoma After Effects of Traumatic Kickback and Intracranial PressureDocument6 pagesArachnoid Cyst Burst in Presence of Contralateral Nomura IV Subdural Hematoma After Effects of Traumatic Kickback and Intracranial PressureAthenaeum Scientific PublishersNo ratings yet
- A Systematic Review of Sinonasal Oncocytomas and Oncocytic Carcinomas: Diagnosis, Management, and Technical ConsiderationsDocument11 pagesA Systematic Review of Sinonasal Oncocytomas and Oncocytic Carcinomas: Diagnosis, Management, and Technical ConsiderationsInes Camilla PutriNo ratings yet
- Retinoblastoma: An Overview: Review ArticleDocument6 pagesRetinoblastoma: An Overview: Review ArticledechastraNo ratings yet
- Arachnoidal Diverticula of Sacral Extradural Meningeal CysDocument7 pagesArachnoidal Diverticula of Sacral Extradural Meningeal Cysjabarin.hNo ratings yet
- 701 2022 Article 5445Document9 pages701 2022 Article 5445PeyepeyeNo ratings yet
- ContentsDocument3 pagesContentsNaim CalilNo ratings yet
- Thick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageDocument9 pagesThick and Diffuse Cisternal Clot Independently Predicts Vasospasm-Related Morbidity and Poor Outcome After Aneurysmal Subarachnoid HemorrhageVanessa LandaNo ratings yet
- Hydro Cep Hal UsDocument7 pagesHydro Cep Hal Usalex soaresNo ratings yet
- Ocular Histoplasmosis SyndromeDocument17 pagesOcular Histoplasmosis SyndromeDiana PSNo ratings yet
- Surgical Education: Neck Dissection: Shaheel Chummun, N.R. Mclean, Maniram RagbirDocument14 pagesSurgical Education: Neck Dissection: Shaheel Chummun, N.R. Mclean, Maniram RagbirpaulineNo ratings yet
- (26941902 - Journal of Neurosurgery: Case Lessons) Calcifying Pseudoneoplasm of The Neuraxis Within The Sellar Region: Illustrative CaseDocument3 pages(26941902 - Journal of Neurosurgery: Case Lessons) Calcifying Pseudoneoplasm of The Neuraxis Within The Sellar Region: Illustrative CaseJUAN GUAPO MENDOZANo ratings yet
- Sinus Pericranii: Diagnosis and Management in 21 Pediatric PatientsDocument11 pagesSinus Pericranii: Diagnosis and Management in 21 Pediatric Patients相壮壮No ratings yet
- Craniopharyngioma and Other Cystic Epithelial Lesions of The Sellar Region A Review of Clinical, Imaging, and Histopathological Relationships, 2010Document12 pagesCraniopharyngioma and Other Cystic Epithelial Lesions of The Sellar Region A Review of Clinical, Imaging, and Histopathological Relationships, 2010CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- 2-9 Reda KamelDocument8 pages2-9 Reda KamelMoustafa Amin AlyNo ratings yet
- Trauma Toracico - Natalia GarciaDocument4 pagesTrauma Toracico - Natalia GarciaNatalia GarcíaNo ratings yet
- Controversies in The Pathophysiology and Management of HyphemaDocument12 pagesControversies in The Pathophysiology and Management of HyphemaJoseph Chipana GutierrezNo ratings yet
- 2014 1 Focus13569 PDFDocument7 pages2014 1 Focus13569 PDFNovia AyuNo ratings yet
- Intracranial Aneurysms in Childhood: 27-Year Single-Institution ExperienceDocument10 pagesIntracranial Aneurysms in Childhood: 27-Year Single-Institution Experiencezrated786No ratings yet
- Lower Extremity Artery Aneurysms and Their Management-An Institutional ExperienceDocument8 pagesLower Extremity Artery Aneurysms and Their Management-An Institutional ExperienceIJAR JOURNALNo ratings yet
- 10 FullDocument17 pages10 FulldraamqaderNo ratings yet
- Cerebrospinal Fluid Rhinorrhea: Diagnosis and Management: Julie T. Kerr, MD, Felix W.K. Chu, MD, Stephen W. Bayles, MDDocument15 pagesCerebrospinal Fluid Rhinorrhea: Diagnosis and Management: Julie T. Kerr, MD, Felix W.K. Chu, MD, Stephen W. Bayles, MDapasic9833No ratings yet
- Management of Suprasellar Arachnoid Cysts in Children A Systematic Literature Review Highlighting Modern Endoscopic Approaches, 2020Document15 pagesManagement of Suprasellar Arachnoid Cysts in Children A Systematic Literature Review Highlighting Modern Endoscopic Approaches, 2020CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- The Management of Intracranial AbscessesDocument3 pagesThe Management of Intracranial AbscessesDio AlexanderNo ratings yet
- Case Anemia Thalasemia FixDocument4 pagesCase Anemia Thalasemia FixmasranraisaNo ratings yet
- Search This SiteDocument20 pagesSearch This SiteDika Putra YudaNo ratings yet
- Bahan Ajar 9 SiringomieliaDocument5 pagesBahan Ajar 9 SiringomieliaMuhammadKadafiNo ratings yet
- 01 Cne 0000361504 25020 73Document8 pages01 Cne 0000361504 25020 73Alexandra E.No ratings yet
- Journal Pre-Proof: Journal of Stomatology Oral and Maxillofacial SurgeryDocument26 pagesJournal Pre-Proof: Journal of Stomatology Oral and Maxillofacial SurgeryGastón SalasNo ratings yet
- Otogenic Complications of Otitis Media Experience at Tertiary Care HospitalDocument5 pagesOtogenic Complications of Otitis Media Experience at Tertiary Care HospitalAjeng Ratna HaryantiNo ratings yet
- Ecr2013 C-1259Document25 pagesEcr2013 C-1259Nazir KhanNo ratings yet
- (Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsDocument10 pages(Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsAniaNo ratings yet
- Diagnosis and Treatment of Pericallosal Artery Aneurysms: SciencedirectDocument4 pagesDiagnosis and Treatment of Pericallosal Artery Aneurysms: SciencedirectRais RyuzakiNo ratings yet
- Complications Associated With Ivanissevich PDFDocument3 pagesComplications Associated With Ivanissevich PDFTahir TahirNo ratings yet
- Nasopharyngeal Carcinoma: Imaging Features of Unusual Cancer in ChildrenDocument5 pagesNasopharyngeal Carcinoma: Imaging Features of Unusual Cancer in ChildrenDevanti EkaNo ratings yet
- Posterior Fossa Arachnoid Cysts As Findings in An Ataxia ClinicDocument8 pagesPosterior Fossa Arachnoid Cysts As Findings in An Ataxia ClinicPedroNo ratings yet
- ATLS 10th Edition RESUMEDocument7 pagesATLS 10th Edition RESUMEhelbertpalmieroNo ratings yet
- A History of Pituitary SurgeryDocument10 pagesA History of Pituitary SurgeryhelbertpalmieroNo ratings yet
- DICTIONDocument7 pagesDICTIONhelbertpalmieroNo ratings yet
- ANATO - Campos VisuaisDocument11 pagesANATO - Campos VisuaishelbertpalmieroNo ratings yet
- Pituitary Apoplexy - Image of NEJMDocument1 pagePituitary Apoplexy - Image of NEJMhelbertpalmieroNo ratings yet
- 12 Angry Men (1957) DvDrip (Eng) - StealthmasterDocument103 pages12 Angry Men (1957) DvDrip (Eng) - StealthmasterhelbertpalmieroNo ratings yet
- Fundamentals of Nursing TestDocument78 pagesFundamentals of Nursing TestNicomille T. Caliging80% (5)
- Template Soap NeuroDocument2 pagesTemplate Soap NeuroJohan SitepuanNo ratings yet
- Oral GenodermatosesDocument4 pagesOral GenodermatosesAkshatNo ratings yet
- Introduction To The Astm E3219 Standard Guide For Derivation of Health Based Exposure Limits (Hbels)Document10 pagesIntroduction To The Astm E3219 Standard Guide For Derivation of Health Based Exposure Limits (Hbels)nsk79inNo ratings yet
- CFR - Code of Federal Regulations Title 21Document5 pagesCFR - Code of Federal Regulations Title 21Bhargav krishnaNo ratings yet
- Pricelist MonotestDocument3 pagesPricelist MonotestMimi AnugrahNo ratings yet
- PEH 11 Q1 Week9 MELC05 MODDocument17 pagesPEH 11 Q1 Week9 MELC05 MODRheane Joyce CastroNo ratings yet
- Pharmacology 1 Exam 1 Study GuideDocument5 pagesPharmacology 1 Exam 1 Study GuideHeroNo ratings yet
- Blood Banking and SerologyDocument9 pagesBlood Banking and SerologyMiaNo ratings yet
- Renal PathologyDocument2 pagesRenal PathologySiddhant KotaNo ratings yet
- Health Flow ChartDocument1 pageHealth Flow ChartAlex Cainoy JrNo ratings yet
- 503 659 1 SMDocument10 pages503 659 1 SMAnggie SilalahiNo ratings yet
- Tumours of The Central Nervous System: FM Brett MD., FrcpathDocument57 pagesTumours of The Central Nervous System: FM Brett MD., FrcpathRerendhutNo ratings yet
- NRP 2015 7th Ed Update 04 2017 Claudia ReedDocument53 pagesNRP 2015 7th Ed Update 04 2017 Claudia Reeddistya.npNo ratings yet
- MCQ in General Surgery For UndergraduatesDocument259 pagesMCQ in General Surgery For UndergraduatesBadri Kobalava100% (5)
- ICU AlgorithmsDocument45 pagesICU AlgorithmsHashimIdreesNo ratings yet
- Who Pneu Im Pgi ProtocolDocument2 pagesWho Pneu Im Pgi ProtocolRoxanneGailBigcasGoleroNo ratings yet
- Treating Addiction With TunesDocument10 pagesTreating Addiction With TunesHajrudinNo ratings yet
- Biochemical Assessment Is An Essential Component of The Assessment andDocument2 pagesBiochemical Assessment Is An Essential Component of The Assessment andSophia Kaye AguinaldoNo ratings yet
- Art Therapy PlanDocument12 pagesArt Therapy Planapi-549933917No ratings yet
- Preventing Prescription Error - KKM Guideline 2020Document48 pagesPreventing Prescription Error - KKM Guideline 2020ABDULLAH BIN OTHMAN (HKULIM)No ratings yet
- Indications For Common Rlung Formulas in Tibetan MedicineDocument8 pagesIndications For Common Rlung Formulas in Tibetan MedicineErikjampaNo ratings yet
- Diabetic NephropathyDocument38 pagesDiabetic NephropathyMade Widiastika100% (1)
- Sas 8Document5 pagesSas 8Rodesa MigarNo ratings yet
- Approach To Renal BiopsyDocument77 pagesApproach To Renal BiopsySandeep Kumar VushikamallaNo ratings yet
- Session #37 SAS - AnaPhy (Lab)Document5 pagesSession #37 SAS - AnaPhy (Lab)Cristina SottoNo ratings yet
- Health Benefits of CoffeeDocument9 pagesHealth Benefits of CoffeeMaru PabloNo ratings yet
- Actual NCPDocument10 pagesActual NCPRouie Björn ABrianNo ratings yet
- NIH Guidelines For Zoning of Hospitals 0701Document3 pagesNIH Guidelines For Zoning of Hospitals 0701SalehaQasimNo ratings yet
- RDS HvacDocument1 pageRDS HvacQNBNo ratings yet