Professional Documents
Culture Documents
913
913
Uploaded by
firda rosyidaCopyright:
Available Formats
You might also like
- BookofRaziel PDFDocument74 pagesBookofRaziel PDFLoli Darriba Perez100% (1)
- Sezer Et Al. - 2018 - Comparison of The Efficacy of Parenteral and OralDocument6 pagesSezer Et Al. - 2018 - Comparison of The Efficacy of Parenteral and OralVictor MendozaNo ratings yet
- Determinants of Nutritional Anaemia in Children Less Than Five Years AgeDocument6 pagesDeterminants of Nutritional Anaemia in Children Less Than Five Years AgeBaiiqDelaYulianingtyasNo ratings yet
- Demir 2013Document5 pagesDemir 2013박가영No ratings yet
- Vitamin B Deficiency in Children With Infantile Spasms: A Case-Control StudyDocument5 pagesVitamin B Deficiency in Children With Infantile Spasms: A Case-Control StudyireneaureliaNo ratings yet
- Prevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's HospitalDocument4 pagesPrevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's Hospitalindahsarizahab 28No ratings yet
- Pengaruh Pemberian Suplemen Vitamin B12 Terhadap Serum Vitamin B12 Dan Hemoglobin Anak PrasekolahDocument9 pagesPengaruh Pemberian Suplemen Vitamin B12 Terhadap Serum Vitamin B12 Dan Hemoglobin Anak PrasekolahAnonymous hTRCQgNo ratings yet
- Iron Def IJPDocument5 pagesIron Def IJPPrahbhjot MalhiNo ratings yet
- Profile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDocument8 pagesProfile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDr. Krishna N. SharmaNo ratings yet
- Risk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpDocument12 pagesRisk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpSari MustikaNo ratings yet
- 782Document20 pages782Aarathi raoNo ratings yet
- Saudi Med J 2011 32 6 589 592Document4 pagesSaudi Med J 2011 32 6 589 592Shivpartap SinghNo ratings yet
- How Prevalent Is Vitamin B 12 Deficiency Among Vegetarians? - Pawlak 2013Document8 pagesHow Prevalent Is Vitamin B 12 Deficiency Among Vegetarians? - Pawlak 2013acolpoNo ratings yet
- Apem 20 198Document8 pagesApem 20 198Sari MustikaNo ratings yet
- Jurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDocument8 pagesJurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDyah FiharjatinNo ratings yet
- Valproic Acid Therapy Decreases Serum 25-Hydroxyvitamin D Level in Female Infants and Toddlers With Epilepsy - A Pilot Longitudinal StudyDocument7 pagesValproic Acid Therapy Decreases Serum 25-Hydroxyvitamin D Level in Female Infants and Toddlers With Epilepsy - A Pilot Longitudinal StudyAnna FlorentinaNo ratings yet
- Vitamin D Levels in Indian Children With Intrathoracic TuberculosisDocument7 pagesVitamin D Levels in Indian Children With Intrathoracic TuberculosisLawrence NapitupuluNo ratings yet
- AlbuminaDocument8 pagesAlbuminaOctavia RaicaNo ratings yet
- Nutrients: Dietary Determinants of Anemia in Children Aged 6-36 Months: A Cross-Sectional Study in IndonesiaDocument10 pagesNutrients: Dietary Determinants of Anemia in Children Aged 6-36 Months: A Cross-Sectional Study in IndonesiaAriqah GinaNo ratings yet
- B 12Document11 pagesB 12Vijay MgNo ratings yet
- Oral Vitamin B12 For Patients Suspected of Subtle Cobalamin Deficiency: A Multicentre Pragmatic Randomised Controlled TrialDocument8 pagesOral Vitamin B12 For Patients Suspected of Subtle Cobalamin Deficiency: A Multicentre Pragmatic Randomised Controlled TrialJhon Alexander OrmazaNo ratings yet
- Jaundice 1Document4 pagesJaundice 1Ie DochieNo ratings yet
- CnsoapsDocument8 pagesCnsoapsNabilah ShafiraNo ratings yet
- Bhat Et Al., 2009Document5 pagesBhat Et Al., 2009Caoimhe O'BrienNo ratings yet
- Vitamin B12 Pancytopneia RecorrectedDocument8 pagesVitamin B12 Pancytopneia RecorrectedSafdar Shabir AwanNo ratings yet
- Jurnal BayiDocument7 pagesJurnal BayiAnonymous AKr7hWjBiNo ratings yet
- Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency AnemiaDocument4 pagesCeliac Disease in Children With Moderate-to-Severe Iron-Deficiency AnemiaAnda PostovaruNo ratings yet
- The Pathophysiology of Elevated Vitamin B12 in Clinical PracticeDocument11 pagesThe Pathophysiology of Elevated Vitamin B12 in Clinical PracticePanagiotis-Sokratis LoumakisNo ratings yet
- Pi Is 1059131119301219Document6 pagesPi Is 1059131119301219cindyNo ratings yet
- Cow Milk AllergyDocument12 pagesCow Milk AllergyAbi ArifiNo ratings yet
- Maternal Gene Polymorphisms of Vitamin B12 Metabolic Pathway and Their Association With Congenital Heart DiseasesDocument6 pagesMaternal Gene Polymorphisms of Vitamin B12 Metabolic Pathway and Their Association With Congenital Heart DiseasesIJAR JOURNALNo ratings yet
- Severe Vitamin B12 Deficiency in An Exclusively Breastfed 5-Month-Old Italian Infant Born To A Mother Receiving Multivitamin Supplementation During PregnancyDocument5 pagesSevere Vitamin B12 Deficiency in An Exclusively Breastfed 5-Month-Old Italian Infant Born To A Mother Receiving Multivitamin Supplementation During PregnancyRamesh lal ShahNo ratings yet
- Jurnal KFDocument4 pagesJurnal KFSandi Rizki ArdiantoNo ratings yet
- Prevalence of Iron-Deficiency Anaemia Among University Students in Noakhali Region, BangladeshDocument8 pagesPrevalence of Iron-Deficiency Anaemia Among University Students in Noakhali Region, BangladeshFitrah RahmadhaniNo ratings yet
- Netherlands Vitamin B12 Deficiency and The Lack of Its Consequences in Type 2 Diabetes Patients Using MetforminDocument5 pagesNetherlands Vitamin B12 Deficiency and The Lack of Its Consequences in Type 2 Diabetes Patients Using Metforminmachoka.peninaNo ratings yet
- Extended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - EcliniDocument16 pagesExtended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - Eclinironaldquezada038No ratings yet
- Original Research Paper Clinical Research: Anemia in Pregnancy and Its Consequences, and Effect of Maternal EducationDocument2 pagesOriginal Research Paper Clinical Research: Anemia in Pregnancy and Its Consequences, and Effect of Maternal EducationfadilahNo ratings yet
- Risk Factors of Vitamin B12 DeficiencyDocument5 pagesRisk Factors of Vitamin B12 DeficiencySamia LatifNo ratings yet
- Changes of Vitamin D Levels in Parkinson's Disease in LibyaDocument1 pageChanges of Vitamin D Levels in Parkinson's Disease in LibyaJagannadh peelaNo ratings yet
- Effect of Lipid Based Nutrient Supplements On Micronutrie 2024 The AmericanDocument9 pagesEffect of Lipid Based Nutrient Supplements On Micronutrie 2024 The AmericanridhoNo ratings yet
- (20493614 - Endocrine Connections) Vitamin B12 Deficiency and Diabetic Neuropathy in Patients Taking Metformin - A Cross-Sectional StudyDocument6 pages(20493614 - Endocrine Connections) Vitamin B12 Deficiency and Diabetic Neuropathy in Patients Taking Metformin - A Cross-Sectional StudySergio MauricioNo ratings yet
- Pharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminDocument5 pagesPharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminMuhammad ZubairNo ratings yet
- Late Vitamin K Deficiency Bleeding in Infants: Five-Year Prospective StudyDocument6 pagesLate Vitamin K Deficiency Bleeding in Infants: Five-Year Prospective StudyzuliaahmadNo ratings yet
- Article: Vitamin B12 Deficiency: Case Report and Review of LiteratureDocument6 pagesArticle: Vitamin B12 Deficiency: Case Report and Review of LiteratureSilvia Emy RarasNo ratings yet
- Vitamina B12Document5 pagesVitamina B12luisNo ratings yet
- Association of Biochemical B12Document7 pagesAssociation of Biochemical B12Samia LatifNo ratings yet
- Efficacy of Vitamin D Supplementation in Asthmatic Children With Vit9amin D Deficiency A Randomized Controlled Trial (ESDAC Trial)Document11 pagesEfficacy of Vitamin D Supplementation in Asthmatic Children With Vit9amin D Deficiency A Randomized Controlled Trial (ESDAC Trial)mirr daaNo ratings yet
- Vitamine ADocument9 pagesVitamine AAzharuddin AkhtarNo ratings yet
- Association Between Metformin Dose and VitaminDocument8 pagesAssociation Between Metformin Dose and VitaminMaria Bernardino CorrêaNo ratings yet
- Model-Informed Precision Dosing of Antibiotics in Pediatric Patients: A Narrative ReviewDocument11 pagesModel-Informed Precision Dosing of Antibiotics in Pediatric Patients: A Narrative ReviewTatiana MarquesNo ratings yet
- Jamapediatrics Ganmaa 2022 Oi 220071 1672265214.39726Document10 pagesJamapediatrics Ganmaa 2022 Oi 220071 1672265214.39726muradchy321No ratings yet
- Original ArticleDocument8 pagesOriginal ArticleadityaNo ratings yet
- RA Iron Deficiency AnemiaDocument6 pagesRA Iron Deficiency Anemiainggrit06No ratings yet
- 8725-Article Text-16096-1-10-20200713Document9 pages8725-Article Text-16096-1-10-20200713Silvie WidyaNo ratings yet
- S 1368980016000409 ADocument11 pagesS 1368980016000409 Atihemex618No ratings yet
- Iron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripDocument17 pagesIron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripMohammedAAl-HaddadAbo-alaaNo ratings yet
- Study of Prevalence of Vitamin D Deficiency in Nephrotic SyndromeDocument7 pagesStudy of Prevalence of Vitamin D Deficiency in Nephrotic SyndromeDrShibsankar PalNo ratings yet
- Indeks MentzerDocument5 pagesIndeks MentzerRINNY ARDINA S.ST., M.SiNo ratings yet
- Laboratory Report Bahasa InggrisDocument11 pagesLaboratory Report Bahasa Inggrisfx8hmxfmc4No ratings yet
- Serum Vitamin B12 and Folic Acid in Vitiligo Patients: A Case Control StudyDocument3 pagesSerum Vitamin B12 and Folic Acid in Vitiligo Patients: A Case Control StudyvaiyenNo ratings yet
- A Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaFrom EverandA Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaNo ratings yet
- JMedSoc35247-5007162 135431Document1 pageJMedSoc35247-5007162 135431firda rosyidaNo ratings yet
- Epidemic Covid19Document5 pagesEpidemic Covid19firda rosyidaNo ratings yet
- Pembagian Kel. PPDS Periode Jan. 2023 BaruDocument88 pagesPembagian Kel. PPDS Periode Jan. 2023 Barufirda rosyidaNo ratings yet
- Bacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General HospitalDocument7 pagesBacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General Hospitalfirda rosyidaNo ratings yet
- Peripartum Cardiomyopathy: A Systematic Literature ReviewDocument15 pagesPeripartum Cardiomyopathy: A Systematic Literature Reviewfirda rosyidaNo ratings yet
- Jadwal Poli Feb MeiDocument5 pagesJadwal Poli Feb Meifirda rosyidaNo ratings yet
- Weight Vel Birth To 60 Days BoysDocument1 pageWeight Vel Birth To 60 Days Boysfirda rosyidaNo ratings yet
- (Faabay) Anjar Lembayung - LunaDocument285 pages(Faabay) Anjar Lembayung - Lunafirda rosyidaNo ratings yet
- Keywords: Pregnant Women, CED, Balanced Nutrition, Level of KnowledgeDocument9 pagesKeywords: Pregnant Women, CED, Balanced Nutrition, Level of Knowledgefirda rosyidaNo ratings yet
- A Tale of The Broken Heart: Peripartum Cardiomyopathy, A Case ReportDocument6 pagesA Tale of The Broken Heart: Peripartum Cardiomyopathy, A Case Reportfirda rosyidaNo ratings yet
- AckermanDocument11 pagesAckermanVansh JainNo ratings yet
- Texasinstruments Ds90ub960q1evm Datasheets 4805Document60 pagesTexasinstruments Ds90ub960q1evm Datasheets 4805BB minNo ratings yet
- Kinetic Road: By: Rivas, Ghail F. Bsce 5-B To: Arch. Marlon C. Solloso InstructorDocument14 pagesKinetic Road: By: Rivas, Ghail F. Bsce 5-B To: Arch. Marlon C. Solloso InstructorGhail Rivas Gha ILNo ratings yet
- Black Body RadiationDocument14 pagesBlack Body RadiationSaif KhanNo ratings yet
- Thermolysis of Medical Waste (Waste Syringe) To Liquid Fuel Using Semi Batch ReactorDocument8 pagesThermolysis of Medical Waste (Waste Syringe) To Liquid Fuel Using Semi Batch ReactorTheJokerNo ratings yet
- RENK Condition Monitoring For Ships enDocument8 pagesRENK Condition Monitoring For Ships enhumayun121No ratings yet
- Calculo Elite XiaomyDocument12 pagesCalculo Elite Xiaomycesar villalobos valdiviesoNo ratings yet
- Gondola Load Calculations: Yy ZZDocument5 pagesGondola Load Calculations: Yy ZZsaskiaNo ratings yet
- Thera TM015XP PDFDocument2 pagesThera TM015XP PDFAlvin Novandi Ega PradanaNo ratings yet
- Insp Lectures Geometrical Optics - Reflection (Mirrors)Document159 pagesInsp Lectures Geometrical Optics - Reflection (Mirrors)arorayash603No ratings yet
- Iso ComparisonDocument11 pagesIso ComparisonbennyfergusonNo ratings yet
- Comcast Smart ResumeDocument8 pagesComcast Smart Resumewajhnzwhf100% (1)
- Unit 17 Computer Aided Manufacture CamDocument11 pagesUnit 17 Computer Aided Manufacture CamManiDeepNo ratings yet
- Condition Monitoring Framework For Maintenance Management: September 2014Document5 pagesCondition Monitoring Framework For Maintenance Management: September 2014Repositorio MantenimientoNo ratings yet
- Pump Suction Pipe Design Considerations PDFDocument8 pagesPump Suction Pipe Design Considerations PDFhogsp1No ratings yet
- A Meta Model of ChangeDocument25 pagesA Meta Model of Changeraminabk100% (1)
- A Beginners Guide To Practical Astrology (Vivian E. Robson B.SC.)Document184 pagesA Beginners Guide To Practical Astrology (Vivian E. Robson B.SC.)icomatiasNo ratings yet
- TP48200A-DX12A1 Telecom Power User ManualDocument68 pagesTP48200A-DX12A1 Telecom Power User ManualDavid TombeNo ratings yet
- 9 Quick Test: Grammar Tick ( ) A, B, or C To Complete The SentencesDocument3 pages9 Quick Test: Grammar Tick ( ) A, B, or C To Complete The SentencesMaria Guadalupe BedollaNo ratings yet
- Haemoglobin EstimationDocument20 pagesHaemoglobin Estimationanon_719505684No ratings yet
- Cellular AberrationDocument8 pagesCellular AberrationRaymund IdicaNo ratings yet
- A Presentation On Organizational Study of Grohe India PVT - Ltd. & Comparative Analysis of Grohe in Sanitary Ware MarketDocument10 pagesA Presentation On Organizational Study of Grohe India PVT - Ltd. & Comparative Analysis of Grohe in Sanitary Ware MarketMukesh KumarNo ratings yet
- Designing and Analysis of Pumping Solar PV System Using Pvsyst SoftwareDocument5 pagesDesigning and Analysis of Pumping Solar PV System Using Pvsyst SoftwareabfstbmsodNo ratings yet
- Professional AbilitiesDocument154 pagesProfessional AbilitiesChunchu AnilNo ratings yet
- Vasitesa Sygef PVDFDocument380 pagesVasitesa Sygef PVDFIsrael AristaNo ratings yet
- IIT Jee Mayank Test-2Document5 pagesIIT Jee Mayank Test-2kamalkantmbbsNo ratings yet
- Magallona Vs ErmitaDocument13 pagesMagallona Vs ErmitaERNIL L BAWA100% (1)
- Subiect - III - 2019Document4 pagesSubiect - III - 2019Valeriu CondreaNo ratings yet
913
913
Uploaded by
firda rosyidaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
913
913
Uploaded by
firda rosyidaCopyright:
Available Formats
RESEARCH PAPER
Therapeutic Response to Sublingual Methylcobalamin in Children With
Vitamin B12 Deficiency Anemia
CHAHAT SAXENA,1 SWETA KUMARI,1 POOJA DEWAN,1 SUNIL GOMBER,1 RACHNA AGARWAL,2 SANGEETA SHARMA,3
NITA RADHAKRISHNAN,4 MANIDEEPA MAJI4
1Department of Pediatrics, University College of Medical Sciences & GTB Hospital, Delhi.
2Department of Neurochemistry, Institute of Human Behaviour and Allied Sciences, Delhi.
3Department of Neuropsychopharmacology, Institute of Human Behaviour and Allied Sciences, Delhi.
4Department of Pediatric Hematology Oncology, Post Graduate Institute of Child Health, Noida, Uttar Pradesh.
Correspondence to: Objective: To evaluate the efficacy and safety of sublingual methylcobalamin for the treatment
Dr Pooja Dewan, of vitamin B12 deficiency anemia in children. Methods: A single arm intervention study was
Professor of Pediatrics, conducted between November, 2020 and April, 2022 in children aged 1-12 years with vitamin
B12 deficiency anemia. Children aged 1-6 years received a tablet of methylcobalamin (1500
University College of Medical Sciences,
mcg) by sublingual route every alternate day (three doses) while those aged 7-12 years re-
Delhi. ceived five such doses. Thereafter, one such sublingual tablet was given weekly and all partici-
poojadewan@hotmail.com pants were followed-up for 6 weeks. Results: 37 children with a mean (SD) age of 8.2 (4.1)
Received: Feb 23, 2023; years were treated and followed-up. On day 10, no child needed rescue therapy with parenteral
Initial review: March 06, 2023; methylcobalamin. After 6 weeks, the mean (SD) serum cobalamin increased from 123.3 (35.5)
Accepted: May 25, 2023. pg/mL to 507.3 (274.2) pg/mL (P<0.001), plasma homocysteine decreased from 48.9 (17.8)
µmol/L to 16.3 (8.5) µmol/L (P<0.001), the mean (SD) hemoglobin increased by 2.3 (1.1) g/dL
(P<0.001), and MCV decreased by 12.9 (6.8) fL (P<0.001). 67.6% children persisted to have
anemia, albeit majority of them had mild or moderate anemia. There were no unsolicited side-
effects reported. Conclusion: Sublingual methylcobalamin is effective for the treatment of vita-
min B12 deficiency anemia in children; although, the duration of treatment needs to be longer
than six weeks.
Keywords: Homocysteine, Macrocytosis, Management, Nutritional anemia.
Trial registration: Clinical Trial Registry of India: CTRI/2021/03/ Published online: May 30, 2023; PII: S097475591600548
031845
V
itamin B12 deficiency has been recognized as METHODS
a significant health problem in children in India
This prospective single-arm interventional study was
with nearly 25% of children aged 5-19 years
conducted between November, 2020 and April, 2022 in the
having anemia due to vitamin B12 or folate
Department of Pediatrics, of a tertiary care hospital in Delhi,
deficiency [1]. Parenteral therapy is the preferred route for
and the Department of Pediatric Hematology-Oncology of a
Vitamin B12 deficiency as it assures availability of the
teaching institute in Uttar Pradesh. The study protocol was
vitamin; although, oral vitamin preparations have also
approved by the institutional ethics com-mittees of the
shown to be equally safe and effective when compared to
participating centers, and was registered with the Clinical
parenteral vitamin B12 in adults [2,3]. However, given the
Trials Registry of India.
uncertainty of absorption of vitamin B12 given orally due to
interference by food or in the presence of underlying Children presenting with anemia as defined by the World
malabsorption, most physicians continue to prescribe Health Organization [10] and macrocytosis [11] or findings
parenteral vitamin B12 [4]. Sublingual route is being suggestive of underlying vitamin B12 deficiency anemia on
evaluated as an alternative to parenteral therapy as it peripheral smear examination, were evaluated for underlying
bypasses the need for intrinsic factor for vitamin B12 vitamin B12 deficiency anemia was defined as: serum
absorption and is also convenient and cheap [5]. However, cobalamin <200 pg/mL 2], and hemoglobin <11.5 g/dL in 1-
similar studies in children are scant [6-9]. We assessed the 5 years, or hemoglobin <11 g/dL in 5-12 years, and any one
biochemical and hematological response to treatment with of: i) mean corpuscular volume (MCV) > 84+ [age (y) x 0.6]
sublingual methylcobalamin among children with vitamin fL, ii) peripheral smear showing the presence of
B12 deficiency. hypersegmented neutrophils (≥5 lobed nuclei in more than
INDIAN PEDIATRICS 913 VOLUME 60__NOVEMBER 15, 2023
38 SUBLINGUAL VITAMIN B 12 FOR ANEMIA
5% of neutrophils) or macrocytes, or iii) bone marrow levels were below 200 pg/mL, or if any child developed
aspiration (BMA) suggestive of megaloblastic anemia. neurological symptoms during the study, the child was
removed from the study and given parenteral rescue therapy.
Eligible participants were recruited consecutively after
obtaining written informed consent from their parents or Based on a previous study [6] wherein 129 children with
caregivers. Verbal assent was obtained for children aged 7- vitamin B12 deficiency received sublingual vitamin B12,
12 years. Children with neurological symptoms, critical following which mean (SD) vitamin B12 increased from
illnesses, recent blood transfusion, chronic diseases, and 146.7 (40.5) pg/mL to 565.5 (108.1) pg/mL, a sample size of
those receiving hematinics, or drugs affecting vitamin B12 two participants was calculated using Power Sample Size
metabolism were excluded. Tests for complete blood counts calculator software at 90% power and 5% type 1 error. Due
and red cell indices were performed for all participants. A to scant literature on the use of sublingual vitamin B12 in
review of the peripheral smear for red cell size, fragmented children, we considered our study as exploratory in nature
cells, hypersegmented neutrophils, and the presence of and intended to recruit atleast 30 eligible patients during the
thrombocytopenia was done. Serum cobalamin, ferritin, study period, so that tests of significance could be applied.
folate levels and homocysteine were estimated for all
Statistical analysis: Data were analyzed using SPSS
participants. Serum cobalamin levels were estimated by
software version 25 (IBM SPSS Inc). Descriptive statistics
electrochemiluminescence immunoassay technique using
were used for nominal baseline characteristics. Categorical
Cobas e601 immunoassay analyzer, at baseline, day 10 and
data were expressed as proportion, and continuous data
day 42 of treatment. Plasma homocysteine was estimated
were expressed as mean (SD). The change in continuous
using enzyme-linked immunosorbent assay technique.
variables were analyzed by paired t test and categorical
Hyperhomocysteinemia was defined as plasma homo-
variables by Chi-square test. P value of less than 0.05 was
cysteine >15 µmol/L. Severity of hyperhomocysteinemia
considered as statistically significant.
was defined as moderate (15-30 µmol/L), intermediate (31-
100 µmol/L) and severe (>100 µmol/L) [12]. RESULTS
Enrolled children were given a tablet methylcobalamin Forty six children were enrolled, of which 9 children were
by sublingual route (Tablet MecobalOD 1500 µg, Rapross lost to follow-up (Fig. 1). The mean (SD) age of enrolled
Pharma). The first dose was given under the direct super- children was 8.2 (4.1) years, and 35.1% were males. The
vision of the physician. Training of the parent(s) and the child majority of enrolled children were vegetarians (75.7%),
was done by demonstrating the correct administration of with 13.5% non-vegetarians.
sublingual methylcobalamin. The child was asked to drink a
glass of water to avoid mouth dryness and after five minutes The mean (SD) serum cobalamin levels rose signi-
he was asked to hold the tablet under the tongue until it ficantly between day 0 and day 10 (P<0.001). The cobalamin
completely dissolved, given 20-30 minutes before breakfast. levels on day 42 fell from that on day 10 (P<0.001) but were
For children aged 2-6 years, if the child was unable to significantly higher than baseline (P<0.001). None of the
cooperate to take the medicine sublingually, the tablet was children had cobalamin deficiency on day 10 and day 42.
crushed and the powdered tablet was placed under the The mean (SD) hemoglobin levels at baseline, day 10 and
tongue. In children aged 7-12 years, one sublingual tablet day 42 are shown in Table I. Although, two children
was given every alternate day (five doses) while in children presented with hemoglobin levels of 3.4 g/dL and 4.6 g/dL
aged 1-6 years, three such doses were given. Thereafter, one each; none of the participants required blood component
tablet was given weekly and all children were followed up for therapy. Following treatment, the mean (SD) hemoglobin
six weeks. Compliance was checked by asking the parent to increased by 1.1 (0.9) g/dL between day 0 and day 10
bring the empty blister pack of methylcobalamin tablets on (P<0.001), while between day 10 and day 42, the mean (SD)
follow-up visits. In case, a dose was missed, parent was asked hemoglobin increased by 1.1 (1.0) g/dL (P<0.001). Children
to give the missed dose as soon as feasible. In case of with leukopenia, thrombocytopenia, and pancytopenia
concomitant iron deficiency, oral iron was given in a dose of decreased significantly after 6 weeks of therapy (Table I). At
3 mg/kg/day of elemental iron (ferrous fumarate) and folic the time of enrolment, 13.5% of the children had reticulo-
acid 5 mg/day for at least three months. cytopenia. The mean (SD) reticulocyte count (%) increased
considerably between days 0 and day 10 (P=0.002), day 10
Hematological response and changes in serum cobalamin and 42 (P=0.001), and day 0 and day 42 (P=0.01). Five
were assessed on day 10 and day 42 of treatment. Plasma children (13.5%) had evidence of co-existent iron deficiency
homocysteine levels were measured at baseline and day 42 of at initial presentation. None of the participants reported any
treatment. On day 10, if serum cobalamin levels failed to rise side effects following the administration of sublingual
>25% of baseline levels, or if on day 42, serum cobalamin methylcobalamin.
INDIAN PEDIATRICS 914 VOLUME 60__NOVEMBER 15, 2023
SAXENA, ET AL. 39
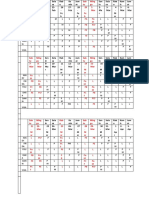
Children aged 1-12 years with signs and symptoms of vitamin B Table I Laboratory Parameters of Children With Vitamin B12
12 deficiency tested for B12 levels (n=135) Deficiency at Baseline, Day 10 and Day 42 (N=37)
↓ Parameters Baseline Day 10 Day 42
Vitamin B12 deficient (n=53) Hemoglobin (g/dL)a 8.4 (2.1) 9.5 (2.1) 10.6 (1.7)
Mean corpusular 102.8 96.2 89.9
Excluded volume (fL)a (15.8) (11.5) (5.7)
Enrolment - Neurological abnormality Serum cobalamin 123.3 820.3 507.3
due to vitamin B12 levels (pg/mL)a (35.8) (451.3) (274.2)
deficiency (n=4)
→ - Severe vitamin B 12
Plasma homocysteine 48.9 (17.8) - 16.3 (8.5)
levels (µmol/L)a
deficiency anemia
Grade of anemiab
requiring red cell
concentrate transfusion Mild anemia 6 (16.2) 9 (24.3) 8 (21.6)
Allocation
(n=3) Moderate anemia 15 (40.5) 16 (43.2) 16 (43.2)
↓ Severe anemia 16 (43.2) 5 (13.5) 1 (2.7)
Sublingual vitamin B12 regimen (n=46) Pancytopenia 4 (10.8) 0 0
Leukopenia 11 (29.7) 7 (18.9) 2 (5.4)
→ Lost to follow-up (n=9)
Thrombocytopenia 14 (37.8) 4 (10.8) 0
Follow-up
↓ Cobalamin deficiency 37 (100) 0 0
Follow-up completed at Day 42 (n=37)
Hyperhomocysteinemia 37 (100) - 17 (45.9)
↓ Macrocytosis 32 (86.4) 28 (75.7) 23 (62.2)
Analyzed Analyzed (n=37) Values expressed as no. (%) or amean (SD). bHemoglobin cutoffs in
children: age 6mo-5y: mild anemia: 10-10.9 g/dL, moderate anemia: 7-
9.9 g/dL, severe anemia: <7 g/dL; 5-12y: mild anemia: 11-11.4 g/dL,
Fig. 1 Study flow chart. moderate anemia: 8-10.9 g/dL, severe anemia: <8 g/dL.
Hyperhomocysteinemia was found in all the enrolled vitamin B12 therapy (30 µg/kg/d). The daily dose of oral
children. None of the participants had severe hyperhomo- vitamin B12 in various studies has varied from 100 µg to
cysteinemia; 89.18% (n=33) had moderate hyperhomo- 1000 µg [14-18], and the schedules followed were variable.
cysteinemia and 10.8% (n=4) had intermediate hyperhomo- The response to these vastly different doses can be explained
cysteinemia. There was a significant decrease in mean (SD) by the fact that with increasing doses there is a diminished
plasma homocysteine levels between day 0 and day 42 percentage absorption of orally administered vitamin B12
(P<0.001). because of saturation of physiological intrinsic factor-
mediated vitamin B12 absorption in the ileum. Similar
DISCUSSION
pharmacodynamics for sublingually administered vitamin
In this single arm trial of 37 children, we found good bio- B12 have not yet been studied.
chemical response to subligual methylcobalamin as evident
We witnessed that at 6 weeks, 67.6% of the children
by normalization of cobalamin levels in all participants by
continued to be anemic. These findings are similar to those
day 10 of therapy. However, on day 42 there was a fall in
observed from a study using sublingual methylcobalamin,
serum cobalamin levels; although, none of the participants
wherein nearly 64% of the children persisted to have anemia
developed subnormal cobalamin levels. This may have
after one month of therapy [8]. Our results affirm that a
been due to a decrease in dosing frequency of sublingual
longer duration of vitamin B12 therapy should be used in
vitamin B12 used in the latter part of our protocol to weekly
children with vitamin B12 deficiency anemia. Similar results
doses. Our findings are akin to previous studies [6,7],
were shown in certain other studies as well [6,14-16]. It has
wherein cobalamin levels have shown complete normali-
previously been reported that blood counts may take up to
zation following intake by sublingual route in children.
eight weeks to normalize [13]. We also noted that at 6 weeks
Both cyanocobalamin as well as methylcobalamin have
follow-up, hyperhomocysteinemia persisted in nearly half
been used by sublingual route [7,8].
the participants. It is recognized that plasma homocysteine is
The doses used in our study were extrapolated from a good marker of functional vitamin B12 deficiency,
doses of oral vitamin B12 used in children. In a study from although it may be elevated due to other causes like folate
northern India [13], a mean rise of 2.8 g/dL in hemoglobin deficiency, hypothyroidism, renal failure, and certain genetic
was observed over a period of one month of daily oral polymorphisms.
INDIAN PEDIATRICS 915 VOLUME 60__NOVEMBER 15, 2023
40 SUBLINGUAL VITAMIN B 12 FOR ANEMIA
WHAT THIS STUDY ADDS?
• Sublingual methylcobalamin is effective in children aged 1-12 years with symptomatic vitamin B12 deficiency
anemia.
A small sample size, short-term follow-up and lack of a 6. Orhan Kiliç B, Kiliç S, Þahin Eroðlu E, et al. Sublingual
comparator arm (oral or intramuscular) are the major limita- methylcobalamin treatment is as effective as intramuscular and
tions of our study. We also did not measure other markers of peroral cyanocobalamin in children age 0-3 years. Hema-
functional vitamin B12 deficiency like holotrancobalamin tology. 2021;26:1013-7.
7. Varkal MA, Karabocuoglu M. Efficiency of the sublingual
and methylmanic acid [2].
route in treating B12 deficiency in infants. Int J Vitam Nutr
We conclude that sublingual methylcobalamin is Res. 2021 Aug 25. Epub ahead of print.
effective and safe for treating symptomatic vitamin B12 8. Kotilea K, Quennery S, Decroës V, Hermans DA. Successful
deficiency anemia in children aged 1-12 years; although, the sublingual cobalamin treatment in a child with short-bowel
syndrome. J Pediatr Pharmacol Ther. 2014;19:60-3.
duration of treatment with vitamin B12 needs to be longer
9. Bensky MJ, Ayalon-Dangur I, Ayalon-Dangur R, et al,
than six weeks.
Comparison of sublingual vs. intramuscular administration of
Ethics clearance: Institutional Ethics Committee for Human vitamin B12 for the treatment of patients with vitamin B12
Research, UCMS; No. IEC-HR/2020/PG/46/64-R1; IEC-HR/ deficiency. Drug Deliv Transl Res. 2019;9:625-30.
2021/51/6. IEC. Post Graduate Institute of Child Health, Noida; 10. World Health Organization. Nutritional anaemias: Tools for
No. 2021-03-IM-14 dated Aug 14, 2021. effective prevention and control. World Health Organization,
Contributors: CS: data collection, data analysis and draft pre- 2017. Accessed March 23, 2023. Available from: http://apps.
paration; SK: data analysis, draft preparation and revised the who.int/iris/bitstream/10665/259425/1/9789241513067-eng.
manuscript; PD: conceptualized the research, supervised the work, pdf?ua=1
analyzed the data and gave critical inputs; SG: supervision of work, 11. Pluncevic Gligoroska J, Gontarev S, Dejanova B, et al. Red
data analysis and critical inputs; RA, SS: laboratory work, data blood cell variables in children and adolescents regarding the
analysis and critical inputs; NR, MM: data collection, analysis and age and sex. Iran J Public Health. 2019;48:704-12.
critical inputs. All authors approved final manuscript and are 12. Maron BA, Loscalzo J. The treatment of hyperhomo-
accountable. cysteinemia. Annu Rev Med. 2009;60:39-54.
Funding: Intramural Research Grant; Competing interests: None 13. Verma D, Chandra J, Kumar P, et al. Efficacy of oral
stated. methylcobalamin in treatment of vitamin B12 deficiency
anemia in children. Pediatr Blood Cancer. 2017;64:e26698.
REFERENCES 14. Bor MV, Cetin M, Aytaç S, et al. Long term biweekly 1 mg
1. International Institute for Population Sciences, ICF Inter- oral vitamin B12 ensures normal hematological parameters,
national. National Family Health Survey (NFHS-4), 2015-16. but does not correct all other markers of vitamin B12
International Institute for Population Sciences, 2017. deficiency; a study in patients with inherited vitamin B12
2. Devalia V, Hamilton MS, Molloy AM, the British Committee deficiency. Haematologica. 2008;93:1755-8.
for Standards in Haematology. Guidelines for the Diagnosis 15. VanderBrink BA, Cain MP, King S, et al. Is oral vitamin B 12
and Treatment of Cobalamin and Folate Disorders. Br J therapy effective for vitamin B12 deficiency in patients with
Haematol. 2014;166:496-513. prior ileocystoplasty? J Urol. 2010;184:1781-5.
3. Wang H, Li L, Qin LL, et al. Oral vitamin B12 versus intra- 16. Altay C, Cetin M. Oral treatment in selective vitamin B12
muscular vitamin B12 for vitamin B12 deficiency. Cochrane malabsorption. J Pediatr Hematol Oncol. 1997;19:245-6.
Database Syst Rev. 2018;3:CD004655. 17. Sezer RG, Bozaykut A, Akoðlu HA, Özdemir GN. The
4. Carmel R. How I treat cobalamin (vitamin B12) deficiency. efficacy of oral vitamin B12 replacement for nutritional
Blood. 2008;112:2214-21. vitamin B12 deficiency. J Pediatr Hematol Oncol. 2018;40:
5. Tuðba-Kartal A, Çaðla-Mutlu Z. Comparison of sublingual e69-e72.
and intramuscular administration of vitamin b12 for the 18. Berlin H, Berlin R, Brante G. Oral treatment of pernicious
treatment of vitamin b12 deficiency in children. Rev Invest anemia with high doses of vitamin B12 without intrinsic
Clin. 2020;72:380-85. factor. Acta Med Scand. 1968;184:247-58.
INDIAN PEDIATRICS 916 VOLUME 60__NOVEMBER 15, 2023
You might also like
- BookofRaziel PDFDocument74 pagesBookofRaziel PDFLoli Darriba Perez100% (1)
- Sezer Et Al. - 2018 - Comparison of The Efficacy of Parenteral and OralDocument6 pagesSezer Et Al. - 2018 - Comparison of The Efficacy of Parenteral and OralVictor MendozaNo ratings yet
- Determinants of Nutritional Anaemia in Children Less Than Five Years AgeDocument6 pagesDeterminants of Nutritional Anaemia in Children Less Than Five Years AgeBaiiqDelaYulianingtyasNo ratings yet
- Demir 2013Document5 pagesDemir 2013박가영No ratings yet
- Vitamin B Deficiency in Children With Infantile Spasms: A Case-Control StudyDocument5 pagesVitamin B Deficiency in Children With Infantile Spasms: A Case-Control StudyireneaureliaNo ratings yet
- Prevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's HospitalDocument4 pagesPrevalence and Risk Factors of Anemia in Under Five-Year-Old Children in Children's Hospitalindahsarizahab 28No ratings yet
- Pengaruh Pemberian Suplemen Vitamin B12 Terhadap Serum Vitamin B12 Dan Hemoglobin Anak PrasekolahDocument9 pagesPengaruh Pemberian Suplemen Vitamin B12 Terhadap Serum Vitamin B12 Dan Hemoglobin Anak PrasekolahAnonymous hTRCQgNo ratings yet
- Iron Def IJPDocument5 pagesIron Def IJPPrahbhjot MalhiNo ratings yet
- Profile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDocument8 pagesProfile of Severe Nutritional Anemia in Children at A Tertiary Care Hospital, South IndiaDr. Krishna N. SharmaNo ratings yet
- Risk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpDocument12 pagesRisk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpSari MustikaNo ratings yet
- 782Document20 pages782Aarathi raoNo ratings yet
- Saudi Med J 2011 32 6 589 592Document4 pagesSaudi Med J 2011 32 6 589 592Shivpartap SinghNo ratings yet
- How Prevalent Is Vitamin B 12 Deficiency Among Vegetarians? - Pawlak 2013Document8 pagesHow Prevalent Is Vitamin B 12 Deficiency Among Vegetarians? - Pawlak 2013acolpoNo ratings yet
- Apem 20 198Document8 pagesApem 20 198Sari MustikaNo ratings yet
- Jurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDocument8 pagesJurnal Pemberian Terapi Mingguan Besi-Asam Folat Dengan Atau Tanpa B12 Pada Remaja: RCTDyah FiharjatinNo ratings yet
- Valproic Acid Therapy Decreases Serum 25-Hydroxyvitamin D Level in Female Infants and Toddlers With Epilepsy - A Pilot Longitudinal StudyDocument7 pagesValproic Acid Therapy Decreases Serum 25-Hydroxyvitamin D Level in Female Infants and Toddlers With Epilepsy - A Pilot Longitudinal StudyAnna FlorentinaNo ratings yet
- Vitamin D Levels in Indian Children With Intrathoracic TuberculosisDocument7 pagesVitamin D Levels in Indian Children With Intrathoracic TuberculosisLawrence NapitupuluNo ratings yet
- AlbuminaDocument8 pagesAlbuminaOctavia RaicaNo ratings yet
- Nutrients: Dietary Determinants of Anemia in Children Aged 6-36 Months: A Cross-Sectional Study in IndonesiaDocument10 pagesNutrients: Dietary Determinants of Anemia in Children Aged 6-36 Months: A Cross-Sectional Study in IndonesiaAriqah GinaNo ratings yet
- B 12Document11 pagesB 12Vijay MgNo ratings yet
- Oral Vitamin B12 For Patients Suspected of Subtle Cobalamin Deficiency: A Multicentre Pragmatic Randomised Controlled TrialDocument8 pagesOral Vitamin B12 For Patients Suspected of Subtle Cobalamin Deficiency: A Multicentre Pragmatic Randomised Controlled TrialJhon Alexander OrmazaNo ratings yet
- Jaundice 1Document4 pagesJaundice 1Ie DochieNo ratings yet
- CnsoapsDocument8 pagesCnsoapsNabilah ShafiraNo ratings yet
- Bhat Et Al., 2009Document5 pagesBhat Et Al., 2009Caoimhe O'BrienNo ratings yet
- Vitamin B12 Pancytopneia RecorrectedDocument8 pagesVitamin B12 Pancytopneia RecorrectedSafdar Shabir AwanNo ratings yet
- Jurnal BayiDocument7 pagesJurnal BayiAnonymous AKr7hWjBiNo ratings yet
- Celiac Disease in Children With Moderate-to-Severe Iron-Deficiency AnemiaDocument4 pagesCeliac Disease in Children With Moderate-to-Severe Iron-Deficiency AnemiaAnda PostovaruNo ratings yet
- The Pathophysiology of Elevated Vitamin B12 in Clinical PracticeDocument11 pagesThe Pathophysiology of Elevated Vitamin B12 in Clinical PracticePanagiotis-Sokratis LoumakisNo ratings yet
- Pi Is 1059131119301219Document6 pagesPi Is 1059131119301219cindyNo ratings yet
- Cow Milk AllergyDocument12 pagesCow Milk AllergyAbi ArifiNo ratings yet
- Maternal Gene Polymorphisms of Vitamin B12 Metabolic Pathway and Their Association With Congenital Heart DiseasesDocument6 pagesMaternal Gene Polymorphisms of Vitamin B12 Metabolic Pathway and Their Association With Congenital Heart DiseasesIJAR JOURNALNo ratings yet
- Severe Vitamin B12 Deficiency in An Exclusively Breastfed 5-Month-Old Italian Infant Born To A Mother Receiving Multivitamin Supplementation During PregnancyDocument5 pagesSevere Vitamin B12 Deficiency in An Exclusively Breastfed 5-Month-Old Italian Infant Born To A Mother Receiving Multivitamin Supplementation During PregnancyRamesh lal ShahNo ratings yet
- Jurnal KFDocument4 pagesJurnal KFSandi Rizki ArdiantoNo ratings yet
- Prevalence of Iron-Deficiency Anaemia Among University Students in Noakhali Region, BangladeshDocument8 pagesPrevalence of Iron-Deficiency Anaemia Among University Students in Noakhali Region, BangladeshFitrah RahmadhaniNo ratings yet
- Netherlands Vitamin B12 Deficiency and The Lack of Its Consequences in Type 2 Diabetes Patients Using MetforminDocument5 pagesNetherlands Vitamin B12 Deficiency and The Lack of Its Consequences in Type 2 Diabetes Patients Using Metforminmachoka.peninaNo ratings yet
- Extended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - EcliniDocument16 pagesExtended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - Eclinironaldquezada038No ratings yet
- Original Research Paper Clinical Research: Anemia in Pregnancy and Its Consequences, and Effect of Maternal EducationDocument2 pagesOriginal Research Paper Clinical Research: Anemia in Pregnancy and Its Consequences, and Effect of Maternal EducationfadilahNo ratings yet
- Risk Factors of Vitamin B12 DeficiencyDocument5 pagesRisk Factors of Vitamin B12 DeficiencySamia LatifNo ratings yet
- Changes of Vitamin D Levels in Parkinson's Disease in LibyaDocument1 pageChanges of Vitamin D Levels in Parkinson's Disease in LibyaJagannadh peelaNo ratings yet
- Effect of Lipid Based Nutrient Supplements On Micronutrie 2024 The AmericanDocument9 pagesEffect of Lipid Based Nutrient Supplements On Micronutrie 2024 The AmericanridhoNo ratings yet
- (20493614 - Endocrine Connections) Vitamin B12 Deficiency and Diabetic Neuropathy in Patients Taking Metformin - A Cross-Sectional StudyDocument6 pages(20493614 - Endocrine Connections) Vitamin B12 Deficiency and Diabetic Neuropathy in Patients Taking Metformin - A Cross-Sectional StudySergio MauricioNo ratings yet
- Pharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminDocument5 pagesPharmaceutical Sciences: Assessment of Vitamin B-12 Deficiency in Type-Ii Diabetics Using MetforminMuhammad ZubairNo ratings yet
- Late Vitamin K Deficiency Bleeding in Infants: Five-Year Prospective StudyDocument6 pagesLate Vitamin K Deficiency Bleeding in Infants: Five-Year Prospective StudyzuliaahmadNo ratings yet
- Article: Vitamin B12 Deficiency: Case Report and Review of LiteratureDocument6 pagesArticle: Vitamin B12 Deficiency: Case Report and Review of LiteratureSilvia Emy RarasNo ratings yet
- Vitamina B12Document5 pagesVitamina B12luisNo ratings yet
- Association of Biochemical B12Document7 pagesAssociation of Biochemical B12Samia LatifNo ratings yet
- Efficacy of Vitamin D Supplementation in Asthmatic Children With Vit9amin D Deficiency A Randomized Controlled Trial (ESDAC Trial)Document11 pagesEfficacy of Vitamin D Supplementation in Asthmatic Children With Vit9amin D Deficiency A Randomized Controlled Trial (ESDAC Trial)mirr daaNo ratings yet
- Vitamine ADocument9 pagesVitamine AAzharuddin AkhtarNo ratings yet
- Association Between Metformin Dose and VitaminDocument8 pagesAssociation Between Metformin Dose and VitaminMaria Bernardino CorrêaNo ratings yet
- Model-Informed Precision Dosing of Antibiotics in Pediatric Patients: A Narrative ReviewDocument11 pagesModel-Informed Precision Dosing of Antibiotics in Pediatric Patients: A Narrative ReviewTatiana MarquesNo ratings yet
- Jamapediatrics Ganmaa 2022 Oi 220071 1672265214.39726Document10 pagesJamapediatrics Ganmaa 2022 Oi 220071 1672265214.39726muradchy321No ratings yet
- Original ArticleDocument8 pagesOriginal ArticleadityaNo ratings yet
- RA Iron Deficiency AnemiaDocument6 pagesRA Iron Deficiency Anemiainggrit06No ratings yet
- 8725-Article Text-16096-1-10-20200713Document9 pages8725-Article Text-16096-1-10-20200713Silvie WidyaNo ratings yet
- S 1368980016000409 ADocument11 pagesS 1368980016000409 Atihemex618No ratings yet
- Iron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripDocument17 pagesIron Deficiency Anemia Among Preschooi Children (2-5) Years in Gaza StripMohammedAAl-HaddadAbo-alaaNo ratings yet
- Study of Prevalence of Vitamin D Deficiency in Nephrotic SyndromeDocument7 pagesStudy of Prevalence of Vitamin D Deficiency in Nephrotic SyndromeDrShibsankar PalNo ratings yet
- Indeks MentzerDocument5 pagesIndeks MentzerRINNY ARDINA S.ST., M.SiNo ratings yet
- Laboratory Report Bahasa InggrisDocument11 pagesLaboratory Report Bahasa Inggrisfx8hmxfmc4No ratings yet
- Serum Vitamin B12 and Folic Acid in Vitiligo Patients: A Case Control StudyDocument3 pagesSerum Vitamin B12 and Folic Acid in Vitiligo Patients: A Case Control StudyvaiyenNo ratings yet
- A Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaFrom EverandA Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaNo ratings yet
- JMedSoc35247-5007162 135431Document1 pageJMedSoc35247-5007162 135431firda rosyidaNo ratings yet
- Epidemic Covid19Document5 pagesEpidemic Covid19firda rosyidaNo ratings yet
- Pembagian Kel. PPDS Periode Jan. 2023 BaruDocument88 pagesPembagian Kel. PPDS Periode Jan. 2023 Barufirda rosyidaNo ratings yet
- Bacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General HospitalDocument7 pagesBacteria Pattern, Results of Antibiotic Sensitivity Test, and Complications of Deep Neck Abscess Patients in Dr. Soetomo General Hospitalfirda rosyidaNo ratings yet
- Peripartum Cardiomyopathy: A Systematic Literature ReviewDocument15 pagesPeripartum Cardiomyopathy: A Systematic Literature Reviewfirda rosyidaNo ratings yet
- Jadwal Poli Feb MeiDocument5 pagesJadwal Poli Feb Meifirda rosyidaNo ratings yet
- Weight Vel Birth To 60 Days BoysDocument1 pageWeight Vel Birth To 60 Days Boysfirda rosyidaNo ratings yet
- (Faabay) Anjar Lembayung - LunaDocument285 pages(Faabay) Anjar Lembayung - Lunafirda rosyidaNo ratings yet
- Keywords: Pregnant Women, CED, Balanced Nutrition, Level of KnowledgeDocument9 pagesKeywords: Pregnant Women, CED, Balanced Nutrition, Level of Knowledgefirda rosyidaNo ratings yet
- A Tale of The Broken Heart: Peripartum Cardiomyopathy, A Case ReportDocument6 pagesA Tale of The Broken Heart: Peripartum Cardiomyopathy, A Case Reportfirda rosyidaNo ratings yet
- AckermanDocument11 pagesAckermanVansh JainNo ratings yet
- Texasinstruments Ds90ub960q1evm Datasheets 4805Document60 pagesTexasinstruments Ds90ub960q1evm Datasheets 4805BB minNo ratings yet
- Kinetic Road: By: Rivas, Ghail F. Bsce 5-B To: Arch. Marlon C. Solloso InstructorDocument14 pagesKinetic Road: By: Rivas, Ghail F. Bsce 5-B To: Arch. Marlon C. Solloso InstructorGhail Rivas Gha ILNo ratings yet
- Black Body RadiationDocument14 pagesBlack Body RadiationSaif KhanNo ratings yet
- Thermolysis of Medical Waste (Waste Syringe) To Liquid Fuel Using Semi Batch ReactorDocument8 pagesThermolysis of Medical Waste (Waste Syringe) To Liquid Fuel Using Semi Batch ReactorTheJokerNo ratings yet
- RENK Condition Monitoring For Ships enDocument8 pagesRENK Condition Monitoring For Ships enhumayun121No ratings yet
- Calculo Elite XiaomyDocument12 pagesCalculo Elite Xiaomycesar villalobos valdiviesoNo ratings yet
- Gondola Load Calculations: Yy ZZDocument5 pagesGondola Load Calculations: Yy ZZsaskiaNo ratings yet
- Thera TM015XP PDFDocument2 pagesThera TM015XP PDFAlvin Novandi Ega PradanaNo ratings yet
- Insp Lectures Geometrical Optics - Reflection (Mirrors)Document159 pagesInsp Lectures Geometrical Optics - Reflection (Mirrors)arorayash603No ratings yet
- Iso ComparisonDocument11 pagesIso ComparisonbennyfergusonNo ratings yet
- Comcast Smart ResumeDocument8 pagesComcast Smart Resumewajhnzwhf100% (1)
- Unit 17 Computer Aided Manufacture CamDocument11 pagesUnit 17 Computer Aided Manufacture CamManiDeepNo ratings yet
- Condition Monitoring Framework For Maintenance Management: September 2014Document5 pagesCondition Monitoring Framework For Maintenance Management: September 2014Repositorio MantenimientoNo ratings yet
- Pump Suction Pipe Design Considerations PDFDocument8 pagesPump Suction Pipe Design Considerations PDFhogsp1No ratings yet
- A Meta Model of ChangeDocument25 pagesA Meta Model of Changeraminabk100% (1)
- A Beginners Guide To Practical Astrology (Vivian E. Robson B.SC.)Document184 pagesA Beginners Guide To Practical Astrology (Vivian E. Robson B.SC.)icomatiasNo ratings yet
- TP48200A-DX12A1 Telecom Power User ManualDocument68 pagesTP48200A-DX12A1 Telecom Power User ManualDavid TombeNo ratings yet
- 9 Quick Test: Grammar Tick ( ) A, B, or C To Complete The SentencesDocument3 pages9 Quick Test: Grammar Tick ( ) A, B, or C To Complete The SentencesMaria Guadalupe BedollaNo ratings yet
- Haemoglobin EstimationDocument20 pagesHaemoglobin Estimationanon_719505684No ratings yet
- Cellular AberrationDocument8 pagesCellular AberrationRaymund IdicaNo ratings yet
- A Presentation On Organizational Study of Grohe India PVT - Ltd. & Comparative Analysis of Grohe in Sanitary Ware MarketDocument10 pagesA Presentation On Organizational Study of Grohe India PVT - Ltd. & Comparative Analysis of Grohe in Sanitary Ware MarketMukesh KumarNo ratings yet
- Designing and Analysis of Pumping Solar PV System Using Pvsyst SoftwareDocument5 pagesDesigning and Analysis of Pumping Solar PV System Using Pvsyst SoftwareabfstbmsodNo ratings yet
- Professional AbilitiesDocument154 pagesProfessional AbilitiesChunchu AnilNo ratings yet
- Vasitesa Sygef PVDFDocument380 pagesVasitesa Sygef PVDFIsrael AristaNo ratings yet
- IIT Jee Mayank Test-2Document5 pagesIIT Jee Mayank Test-2kamalkantmbbsNo ratings yet
- Magallona Vs ErmitaDocument13 pagesMagallona Vs ErmitaERNIL L BAWA100% (1)
- Subiect - III - 2019Document4 pagesSubiect - III - 2019Valeriu CondreaNo ratings yet