Professional Documents
Culture Documents
Reservatório Tardio
Reservatório Tardio
Uploaded by
pamellagoulart2004Copyright:
Available Formats
You might also like
- Wiring Diagram Elevator: 123/INDSBY-ELC/1014Document22 pagesWiring Diagram Elevator: 123/INDSBY-ELC/1014Gogik Anto85% (13)
- Editing Coding and Tabulation of Data-Marketing ResearchDocument16 pagesEditing Coding and Tabulation of Data-Marketing ResearchArivanandan Get Going100% (1)
- Eradication of Human Immunodeficiency Virus Type-1 (HIV-1) - Infected CellsDocument13 pagesEradication of Human Immunodeficiency Virus Type-1 (HIV-1) - Infected CellsDouglas SouzaNo ratings yet
- Viruses 15 00107Document30 pagesViruses 15 00107Trần T. MơNo ratings yet
- Clamidia y VihDocument17 pagesClamidia y VihC JNo ratings yet
- AIDS Word OkokookkDocument6 pagesAIDS Word OkokookkAlberto PiasentierNo ratings yet
- Viruses 07 01578 PDFDocument21 pagesViruses 07 01578 PDFicicle900No ratings yet
- MainDocument10 pagesMainLythuo KryNo ratings yet
- Infección VIH Primer 2023Document21 pagesInfección VIH Primer 2023MedicazoNo ratings yet
- Reservatório HIVDocument22 pagesReservatório HIVpamellagoulart2004No ratings yet
- Hematopoietic Stem Cell Transplantation For HIV Cure: Daniel R. KuritzkesDocument6 pagesHematopoietic Stem Cell Transplantation For HIV Cure: Daniel R. KuritzkesVergio MarkusNo ratings yet
- Humoral and Innate Antiviral Immunity As Tools To Clear Persistent HIV InfectionDocument8 pagesHumoral and Innate Antiviral Immunity As Tools To Clear Persistent HIV InfectionLhorruama DiasNo ratings yet
- Phylogenies ArtDocument9 pagesPhylogenies ArtIris SolarNo ratings yet
- HHS Public Access: HIV-1 Drug Resistance and Resistance TestingDocument42 pagesHHS Public Access: HIV-1 Drug Resistance and Resistance TestingAlfiraNo ratings yet
- Hunter Fitness Cost PolDocument22 pagesHunter Fitness Cost PolJim HunterNo ratings yet
- Main 1Document4 pagesMain 1rest_a2003No ratings yet
- Vaccination of Healthcare Workers A ReviewDocument17 pagesVaccination of Healthcare Workers A Reviewy2h996tnp8No ratings yet
- HIV InfectionDocument22 pagesHIV Infectionquang.14y1543No ratings yet
- Hernandez Martin Simkins 1Document13 pagesHernandez Martin Simkins 1angelNo ratings yet
- Artikel+Kompilasi+OBJ13 3revDocument19 pagesArtikel+Kompilasi+OBJ13 3revAurha Akmal GinarisNo ratings yet
- Therapy For Persistent HIVDocument6 pagesTherapy For Persistent HIVAnonymous ceYk4p4No ratings yet
- CatfluDocument13 pagesCatflumvdaniela.santanaNo ratings yet
- Medical Hypotheses: SciencedirectDocument3 pagesMedical Hypotheses: SciencedirectnordonkNo ratings yet
- Imunopatogenesis - HIVDocument19 pagesImunopatogenesis - HIVlia tri maryaniNo ratings yet
- Johnston 2007Document9 pagesJohnston 2007MedranoReyesLuisinNo ratings yet
- Hiv Diagnosis and Treatment Through Advaced TechDocument16 pagesHiv Diagnosis and Treatment Through Advaced TechAde KurniaNo ratings yet
- coinfeccion determinante de vihDocument8 pagescoinfeccion determinante de vihSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- 10.1128@JVI.00486-20Document59 pages10.1128@JVI.00486-20Aneesh S NairNo ratings yet
- Targeted Shock-And-Kill Hiv-1 Gene Therapy Approach Combining Crispr Activation, Suicide Gene Tbid and Retargeted Adenovirus DeliveryDocument11 pagesTargeted Shock-And-Kill Hiv-1 Gene Therapy Approach Combining Crispr Activation, Suicide Gene Tbid and Retargeted Adenovirus DeliveryMusa MusaNo ratings yet
- Multipurpose Prevention Technologies: The Future of HIV and STI ProtectionDocument8 pagesMultipurpose Prevention Technologies: The Future of HIV and STI ProtectionKaoru Eduardo AtouyatzinNo ratings yet
- HHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideDocument30 pagesHHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideicaeeNo ratings yet
- FetchObject ActionDocument22 pagesFetchObject ActionLucas DutraNo ratings yet
- 1 s2.0 S0022519318301395 MainDocument13 pages1 s2.0 S0022519318301395 MainIntan PermataNo ratings yet
- Herpes Simplex Virus Evasion of Early Host Antiviral ResponsesDocument24 pagesHerpes Simplex Virus Evasion of Early Host Antiviral ResponsesRoberto DurónNo ratings yet
- The Gift of A Lifetime: Analysis of HIV at Autopsy: Frank MaldarelliDocument5 pagesThe Gift of A Lifetime: Analysis of HIV at Autopsy: Frank MaldarelliIrina TănaseNo ratings yet
- Fisiopatología VIHDocument13 pagesFisiopatología VIHjahernandezs0110No ratings yet
- MBS2008 Mutation and Control of The Human Immunodeficiency Virus StengelDocument10 pagesMBS2008 Mutation and Control of The Human Immunodeficiency Virus StengelSaeb AmirAhmadi ChomacharNo ratings yet
- Firdaus 2014Document8 pagesFirdaus 2014Pavithra NNo ratings yet
- Envejecimiento HivDocument8 pagesEnvejecimiento HivJose LunaNo ratings yet
- Seminar: Daniel P Webster, Paul Klenerman, Geoff Rey M DusheikoDocument12 pagesSeminar: Daniel P Webster, Paul Klenerman, Geoff Rey M Dusheikovira khairunisaNo ratings yet
- Antifungal Drugs - The Current Armamentarium and Development of New AgentsDocument20 pagesAntifungal Drugs - The Current Armamentarium and Development of New AgentssovalaxNo ratings yet
- Global Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDDocument15 pagesGlobal Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDbrachiuroNo ratings yet
- Hepatitis C Virus Replication and Potential Targets For Direct-Acting AgentsDocument11 pagesHepatitis C Virus Replication and Potential Targets For Direct-Acting AgentsWael Abdel-MageedNo ratings yet
- AIDS ClassDocument58 pagesAIDS ClassramyaayokeshNo ratings yet
- Rotavirus Related Systemic Diseases Clinical Manifestation Evidence and PathogenesisDocument17 pagesRotavirus Related Systemic Diseases Clinical Manifestation Evidence and PathogenesisDaniela MontecinosNo ratings yet
- Vassilopoulos 2002Document13 pagesVassilopoulos 2002deliaNo ratings yet
- Vih RevDocument25 pagesVih RevANDRÉS FELIPE BUSTILLO GÓMEZNo ratings yet
- 1 s2.0 S0166354222002868 MainDocument8 pages1 s2.0 S0166354222002868 Mainnathanaellee92No ratings yet
- A Special Issue On Infections in Solid Organ Transplant RecipientsDocument3 pagesA Special Issue On Infections in Solid Organ Transplant RecipientsKhushal khanNo ratings yet
- A New Perspective On HIV CureDocument4 pagesA New Perspective On HIV CureRemo Anthony Gonza LuqueNo ratings yet
- Special Issue: Structural and Molecular Biology of HIVDocument2 pagesSpecial Issue: Structural and Molecular Biology of HIVbookmoonNo ratings yet
- Veaa 013Document15 pagesVeaa 013jaspforeverNo ratings yet
- Pathogenesis of HIV Infection: Infectious Disease Reports June 2013Document6 pagesPathogenesis of HIV Infection: Infectious Disease Reports June 2013MILDA KHAERUNNISANo ratings yet
- Pharmacology of HIV RXDocument10 pagesPharmacology of HIV RXdupuytrenNo ratings yet
- revision sistematica multipatogenaDocument7 pagesrevision sistematica multipatogenaSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- Nihms 839861Document40 pagesNihms 839861Faisal JamshedNo ratings yet
- Panther 1999Document9 pagesPanther 1999Araceli Enríquez OvandoNo ratings yet
- The Role of Human Dendritic Cells in HIV-1 InfectionDocument9 pagesThe Role of Human Dendritic Cells in HIV-1 InfectionrizkaNo ratings yet
- Editorial Overview Hildegund CJ Ertl and Antonio LanzavecchiaDocument3 pagesEditorial Overview Hildegund CJ Ertl and Antonio Lanzavecchiahoangan118No ratings yet
- The Spread, Treatment, and Prevention of HIV-1: Evolution of A Global PandemicDocument12 pagesThe Spread, Treatment, and Prevention of HIV-1: Evolution of A Global PandemicLatiefah NWNo ratings yet
- Evidence That Hepatitis C Virus Genome Partly Controls Infection OutcomeDocument15 pagesEvidence That Hepatitis C Virus Genome Partly Controls Infection OutcomeKaritoNo ratings yet
- Infectious Diseases in Solid-Organ Transplant Recipients: A practical approachFrom EverandInfectious Diseases in Solid-Organ Transplant Recipients: A practical approachOriol ManuelNo ratings yet
- Admin,+56 Ism.v11i1.557Document5 pagesAdmin,+56 Ism.v11i1.557Reni Tri AstutiNo ratings yet
- The Material Culture of The Postsocialist CityDocument15 pagesThe Material Culture of The Postsocialist Cityjsgt1980No ratings yet
- 0547 s06 TN 3Document20 pages0547 s06 TN 3mstudy123456No ratings yet
- 3M CorporationDocument3 pages3M CorporationIndoxfeeds GramNo ratings yet
- Alameda Investments - Alameda InvestmentsDocument9 pagesAlameda Investments - Alameda InvestmentsLuisNo ratings yet
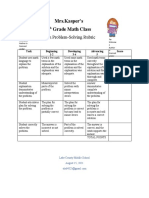
- Problemsolving RubricDocument1 pageProblemsolving Rubricapi-560491685No ratings yet
- March 16 - IM Processors DigiTimesDocument5 pagesMarch 16 - IM Processors DigiTimesRyanNo ratings yet
- Halimatus Islamiah Analisis Jurnal Internasional K3Document3 pagesHalimatus Islamiah Analisis Jurnal Internasional K3TussNo ratings yet
- The Radiology Assistant - Fleischner 2017 GuidelineDocument11 pagesThe Radiology Assistant - Fleischner 2017 GuidelineHenry J. Hernández L.No ratings yet
- Lesson Plan 8 (September) (AutoRecovered) 1Document3 pagesLesson Plan 8 (September) (AutoRecovered) 1Rutchie AbantoNo ratings yet
- Bstem-5 4Document61 pagesBstem-5 4G-SamNo ratings yet
- Huffman Coding - Base of JPEG Image CompressionDocument13 pagesHuffman Coding - Base of JPEG Image CompressionFikaduNo ratings yet
- Quiz For Western Lit.Document25 pagesQuiz For Western Lit.donnie4workingNo ratings yet
- Shahetal.2022 TecGeomorpJhelumDocument21 pagesShahetal.2022 TecGeomorpJhelumAyesha EjazNo ratings yet
- Ballistic - August September 2021Document168 pagesBallistic - August September 2021andrewrowe100% (2)
- Cost Leadership Porter Generic StrategiesDocument7 pagesCost Leadership Porter Generic StrategiesRamar MurugasenNo ratings yet
- Thou Hast Made MeDocument3 pagesThou Hast Made Meyour dady0% (1)
- Ethical Considerations Dissertation ExampleDocument7 pagesEthical Considerations Dissertation ExampleBuyPapersOnlineCanada100% (1)
- Dbms Lab Dbms Lab: 23 March 202Document12 pagesDbms Lab Dbms Lab: 23 March 202LOVISH bansalNo ratings yet
- HG-G9 Module 7 RTP PDFDocument10 pagesHG-G9 Module 7 RTP PDFDaniel Robert BuccatNo ratings yet
- Chapter 1 Peanut Growing and HarvestingDocument18 pagesChapter 1 Peanut Growing and HarvestingKapil BhattNo ratings yet
- VP3401 As04Document2 pagesVP3401 As04shivamtyagi68637No ratings yet
- Peptides and Proteins: M.Prasad Naidu MSC Medical Biochemistry, PH.DDocument30 pagesPeptides and Proteins: M.Prasad Naidu MSC Medical Biochemistry, PH.DDr. M. Prasad NaiduNo ratings yet
- HMT (U4)Document23 pagesHMT (U4)maniNo ratings yet
- Marik ServitorsDocument20 pagesMarik ServitorsDWNloader100% (2)
- Reflection Paper On "Legal Research, Legal Writing, and Legal Analysis: Putting Law School Into Practice" by Suzanne RoweDocument2 pagesReflection Paper On "Legal Research, Legal Writing, and Legal Analysis: Putting Law School Into Practice" by Suzanne RoweRobert Jay Regz Pastrana IINo ratings yet
- Alarm Security Pic - Google ShoppingDocument1 pageAlarm Security Pic - Google Shoppingleeleeleebc123No ratings yet
- Analisis Pemetaan (Jadual Kenalpasti Cu Wa)Document5 pagesAnalisis Pemetaan (Jadual Kenalpasti Cu Wa)En AzermieyNo ratings yet
Reservatório Tardio
Reservatório Tardio
Uploaded by
pamellagoulart2004Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Reservatório Tardio
Reservatório Tardio
Uploaded by
pamellagoulart2004Copyright:
Available Formats
HHS Public Access
Author manuscript
Immunity. Author manuscript; available in PMC 2018 October 22.
Author Manuscript
Published in final edited form as:
Immunity. 2018 May 15; 48(5): 872–895. doi:10.1016/j.immuni.2018.04.030.
Targeting the latent reservoir for HIV-1
Srona Sengupta1,2 and Robert F. Siliciano1,3
1Department of Medicine, Johns Hopkins University School of Medicine, Baltimore MD 21205
2Graduate Program in Immunology and Medical Scientist Training Program, Baltimore MD 21205
3Howard Hughes Medical Institute, Baltimore MD 21205
Author Manuscript
Abstract
Antiretroviral therapy can effectively block HIV-1 viral replication and prevent or reverse
immunodeficiency in HIV-1-infected individuals. However, viral replication resumes within weeks
of treatment interruption. The major barrier to cure is a small pool of resting memory CD4+ T
cells that harbor latent HIV-1 proviruses. This latent reservoir is now the focus of an intense
international research effort. We describe how the reservoir is established, challenges involved in
eliminating it, and pharmacologic and immunologic strategies for targeting this reservoir. The
development of a successful cure strategy will likely require understanding the mechanisms that
maintain HIV-1 proviruses in a latent state and pathways that drive the proliferation of infected
cells, which slows reservoir decay. In addition, cure will require the development of effective
immunologic approaches to eliminating infected cells. There is renewed optimism about the
prospect of a cure, and the interventions discussed here may pave the way.
Author Manuscript
eTOC blurb:
Developing a cure for HIV-1 requires understanding the mechanisms of HIV-1 persistence in the
latent reservoir. In this review, we discuss historical and recent paradigms in the HIV-1 persistence
field as well novel immunologic and pharmacologic strategies to eliminate this reservoir.
Introduction: The case for an HIV-1 cure
In 1983, a ~9.7 kb retrovirus later termed human immunodeficiency virus-1 (HIV-1) was
discovered as the causative agent for an emerging fatal immunodeficiency syndrome (Barré-
Sinoussi et al., 1983). This acquired immunodeficiency syndrome (AIDS) developed in
Author Manuscript
infected individuals years after initial infection. Sensitive assays for HIV-1 RNA in the
plasma (Piatak et al. 1993) revealed that viral replication continues throughout the course of
untreated infection, driving the loss of CD4+ T cells which is the central cause of the
immunodeficiency (Mellors et al. 1996). The urgent need for therapies led to the relatively
rapid development of drugs that block sequential steps in the virus life cycle including
attachment of the virus particle to CD4 and CCR5 on the T cell surface (CCR5 antagonists),
fusion of the viral envelope with the plasma membrane (fusion inhibitors), reverse
transcription of genomic viral RNA into double stranded DNA (nucleoside and non-
Correspondence should be addressed to Robert F. Siliciano, rsiliciano@jhmi.edu.
Sengupta and Siliciano Page 2
nucleoside reverse transcriptase inhibitors), integration of viral DNA into the host cell
Author Manuscript
genome (integrase inhibitors), and maturation of virus particles released following their
assembly from nascent viral RNA and proteins (protease inhibitors). In 1997, combinations
of three antiretroviral drugs were shown to durably suppress viremia to below the limit of
detection of clinical assays (Perelson et al. 1997), consistent with a complete arrest in viral
replication (Ho et al. 1995, Wei et al. 1995). The remarkable efficacy of combination
antiretroviral therapy (cART) reflects unique pharmacologic attributes that may also apply to
the direct acting antiviral drugs that can cure Hepatitis C infection in 12 weeks (Laskey and
Siliciano, 2014; Koizumi et al. 2017) However, despite its remarkable efficacy, cART does
not cure HIV-1 infection, and viremia rebounds within weeks of treatment interruption
(Davey et al. 1999; Chun et al. 1999). This reflects the fact that, unlike Hepatitis C, HIV-1
can establish a state of latency in some infected cells.
The ability of human immunodeficiency virus-1 (HIV-1) to remain quiescent in a latent
Author Manuscript
reservoir in long-lived memory CD4+ T cells is the main barrier to cure (Chun et al. 1995;
Chun et al. 1997a; Chun et al. 1997b; Finzi et al. 1997; Wong et al. 1997). In HIV+
individuals on combination antiretroviral therapy (cART), the primary indication of
persistent HIV-1 infection is integrated viral DNA within the genomes of resting CD4+ T
cells (Chun et al. 1995). Expression of viral RNA and proteins is limited while the cells
remain in a resting state. Infected resting CD4+ T cells are essentially indistinguishable from
uninfected cells, and therefore are not eliminated by cytolytic effectors. Quiescence,
however, is not permanent, and cells containing viral genomes can be reactivated, leading to
virus production (Hill et al. 2014). Upon cessation of cART, the stochastic reactivation of
even a single latently infected CD4+ T cell can result in virion production, infection of other
CD4+T cells, and subsequent exponential viral rebound. In most HIV+ individuals, viremia
becomes measurable within two weeks of treatment interruption (Davey et al. 1999; Chun et
Author Manuscript
al. 1999). The latent reservoir decays slowly, with a t½ of 3.6 years, so even prolonged cART
cannot to eradicate the infection in a patient’s lifetime (Finzi 1999; Siliciano et al. 2003;
Strain et al. 2003; Crooks et al. 2015). Even in HIV+ individuals who are treated early or
who have extremely small reservoirs as a result of bone marrow transplantation, rebound can
occur, and therefore these individuals must stay on cART indefinitely (Chun et al. 1999;
Kaufmann et al. 2004; Persaud et al. 2013; Henrich et al. 2014; Luzuriaga et al. 2015).
Although cART is effective in reducing viremia to below the detection limit of clinical
assays and reversing or preventing immunodeficiency, it has some side effects and is
challenging to deliver in resource-poor areas. In non-adherent HIV+ individuals, HIV-1
variants with drug resistance mutations evolve (Larder et al. 1989). Moreover, despite
advances in HIV-1 treatment and prevention, the global rate of new infections has held
Author Manuscript
steady, at ~2 million new infections per year (UNAIDS 2016 and 2017), adding
continuously to the number of people requiring lifelong treatment. Therefore, an HIV-1 cure
is urgently needed.
Cure efforts have focused on the “shock and kill” strategy for purging the reservoir (Archin
et al. 2014). Reversing latency (“shock”) to allow expression of viral gene products should
allow for the “kill” phase in which infected cells are eliminated by viral cytopathic effects,
for example through Vpr-mediated cycle arrest and apoptosis (Poon et al. 1998; Stewart et
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 3
al. 2000) or by HIV-1-specific cytolytic T lymphocytes (CTL). Such a strategy would be
carried out while HIV+ individuals remain on cART to prevent new infection events.
Author Manuscript
Modeling studies suggest that a reservoir reduction of >4 logs would be required to achieve
a cure (i.e. no viral rebound after withdrawal of cART) in 50% of HIV+ individuals (Hill et
al. 2014). Thus a strong reactivation stimulus and efficient targeted killing of infected cells
are necessary. Importantly, the reactivation stimulus would ideally induce HIV-1 expression
without causing global T cell activation, which is toxic (Prins et al. 1999; Kulkosky et al.
2002). Numerous small molecule latency-reversing agents (LRAs) have been identified for
this purpose, often using in vitro models of HIV-1 latency (Yang et al. 2009). Some have
been tested in cART-treated HIV+ individuals (Archin et al. 2012; Søgaard et al. 2015), in
cART-treated macaques infected with simian immunodeficiency virus (SIV) (Borducchi et
al. 2016) or in HIV-1-infected humanized mice on cART (Halper-Stromberg et al. 2014). A
few studies have reported transient increases in cell-associated RNA consistent with latency
Author Manuscript
reversal in vivo (Archin et al. 2012), while other studies have seen increases in viral RNA in
plasma (Søgaard et al. 2015). Still, evidence for a clear reduction in the latent reservoir is
lacking (Cillo et al. 2014). One concern is that simply reactivating latently infected cells
may not lead to cell death (Shan et al. 2012). Killing of infected cells by CTL or other
cytolytic effector cells may be required. However, multiple questions remain, including
which viral antigens are presented by latently infected cells after induction and whether CTL
or NK cells can effectively recognize and kill these cells. In this review, we discuss the
current understanding of mechanisms of HIV-1 persistence, as well as strategies to
pharmacologically and immunologically limit this persistence, with a particular focus on the
“kill” aspect of “shock and kill” strategies.
A historical perspective
Author Manuscript
By the late 1990s, several studies had shown that HIV-1 gene expression could be
upregulated upon T cell activation through inducible host transcription factors such as NFκB
and NFAT (Nabel and Baltimore 1987; Kinoshita et al. 1998). These factors promote viral
transcription upon binding to the HIV-1 promoter sequence, or long terminal repeat (LTR)
(Nabel and Baltimore 1987; Siekevitz et al. 1987; Böhnlein et al. 1988; Duh et al. 1989;
Kinoshita et al. 1998). Therefore, it seemed likely that low or absent HIV-1 gene expression
representative of viral latency could occur in resting but not activated CD4+ T cells. Indeed,
by 1995, one study had shown that activating resting memory CD4+T cells from HIV+
individuals could induce the release of replication-competent HIV-1 (Chun et al. 1995).
The importance of this discovery only became apparent with the development of cART.
cART blocks new infection events but not virus production from cells that already have an
Author Manuscript
integrated provirus. If the block is complete, decreases in viremia following initiation of
cART reflect the decay rate of productively infected cells. Seminal studies by the
laboratories of David Ho and George Shaw showed that the major population of virus-
producing cells decays rapidly, with a t1/2 of <1 day (Ho et al. 1995; Wei et al. 1995;
Perelson et al. 1997). A second compartment of cells, which may represent recently infected
cells infected with unintegrated HIV-1 (Blankson et al. 2000), decays with a t1/2 of 14 days
(Perelson et al. 1997). In HIV+ individuals on optimal cART, the decay of both of these
compartments reduces viremia to below the limit of detection of clinical assays (Figure 1),
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 4
initially suggesting that these compartments may contain all infected cells (Perelson et al.
Author Manuscript
1997). If this were true, then treatment for 2–3 years would be curative (Perelson et al.
1997). The finding that rebound is observed in the vast majority of HIV+ individuals who
stop treatment, regardless of the time on cART, indicates that there is a third cellular
compartment that serves as a long-lived reservoir of infected cells.
Resting memory cells, already shown to harbor quiescent but inducible HIV-1 (Chun et al.
1995; Chun et al. 1997a) were a clear candidate for this long-lived reservoir. In 1997, three
groups showed that replication-competent HIV-1 could indeed be induced from resting
memory CD4+ T cells from HIV+ individuals on long-term cART (Chun et al. 1997b; Finzi
et al. 1997; Wong et al. 1997). While the cells are in a resting state, HIV-1 is maintained as
latent but inducible proviruses, and no virus is produced without some activating stimulus
(Chun et al. 1995; Finzi et al. 1997; Wong et al. 1997). This population of infected cells
became known as the latent reservoir.
Author Manuscript
In discussions of reservoirs and HIV-1 persistence, definitions are important. Latency can be
defined as a reversible non-productive state of infection of individual cells, and a reservoir
can be defined as a cell type that allows longer-term persistence of replication-competent
virus in the setting of optimal cART. Several recent studies have revealed important features
of persistent HIV-1 that directly impact our understanding of the latent reservoir. Full viral
genome sequencing studies have shown that over 93% of proviruses in resting CD4+T cells
in HIV+ individuals on cART are defective (Ho et al. 2013; Bruner et al. 2016; Imamichi et
al. 2016; Hiener et al. 2017; Lee et al. 2017). These defective proviruses contain large
internal deletions and/or hypermutation mediated by APOBEC3G, a host enzyme that
deaminates dC to dU on the minus strand of HIV-1 cDNA during reverse transcription
(resulting in a G to A hypermutation). For most defective proviruses, the defects are so
Author Manuscript
severe that viral replication is precluded (Ho et al. 2013; Bruner et al. 2016). Therefore,
measurements of latently infected cells via standard PCR analysis of proviral DNA do not
accurately capture the relevant reservoir of replication-competent HIV-1 that can cause viral
rebound upon treatment interruption (Bruner et al. 2016). In this review, we thus define the
latent reservoir as a long-lived population of resting (i.e. possessing a longer half-life than
activated) CD4+ T cells that harbors replication-competent HIV-1 in HIV+ individuals on
optimal cART. Other potential reservoirs are also discussed at the end of this review.
Latency induction and seeding of the reservoir
How HIV-1 establishes latent infection in memory CD4+ T cells has been unclear. Multiple
models exist, but the simplest explanation is that latency is an accident of timing, as is
discussed below. Memory cells are long-lived, and latency would appear to be a means to
Author Manuscript
prolong HIV-1 survival in vivo through immunoevasion, as in the case of herpesviruses.
However, unlike herpesviruses, HIV-1 replicates continuously throughout the course of
untreated infection (Piatak et al. 1993), evading the adaptive immune response via rapid
mutations in antibody and CTL epitopes (Borrow et al. 1997; Price et al. 1997; Wei et al.
2002; Kwong et al. 2002) (Figure 1). This it is not immediately apparent why HIV-1
established latent infection in resting memory CD4+ T cells. HIV-1 does not readily infect
these cells, due to low expression of the co-receptor CCR5 needed for viral entry (Pierson et
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 5
al. 2000) and a reduction in dNTPs needed for reverse transcription resulting from the
Author Manuscript
dNTPase activity of the restriction factor SAMHD1 (Goldstone et al. 2011; Baldauf et al.
2012). Abortive infection of resting CD4+ T cells can occur and may lead to cell death
(Doitsh et al. 2010). In addition, infection of resting CD4+ T cells that have been rendered
permissive by exposure to chemokines in tissue sites may lead to latency (Saleh et al, 2007).
However, the most likely explanation for HIV-1 latency involves viral tropism for activated
CD4+ T cells. T cell activation upregulates the CCR5 co-receptor, so activated CD4+T cells
are readily infected by HIV-1. Normally productive infection rapidly leads to cell death (Wei
et al. 1995; Bleul et al. 1997; Gornalusse et al. 2015). However, infection of activated CD4+
T cells that are reverting to a resting memory state, or effector-to-memory transitioning
(EMT) cells, provides the best conditions for the establishment of latency due to high CCR5
expression, adequate dNTP pools for reverse transcription, and reduced viral gene
expression due to the sequestration of activation-dependent host transcription factors (i.e.
Author Manuscript
NFκB and NFAT) (Shan et al. 2017). For cells in this state, steps in the viral life cycle from
entry to integration can proceed, but gene expression from the integrated provirus is minimal
and transient (Figure 2). Thus these cells are more likely to escape viral cytopathic effects
and immune effector mechanisms and enter a state of latent infection. In other words, a rare
“perfect storm” of events seems to allow for successful viral infection and integration
without cell death.
This model also provides an explanation for the low frequency of latently infected cells in
vivo. Even in the uninfected state, very few activated CD4+T cells progress to a memory
state, with most cells dying during the contraction phase of the immune response. With
HIV-1 infection, even fewer activated CD4+ T cells may escape viral cytopathic effects and
host immune targeting to revert to a memory phenotype, and only rare infection of EMT
cells provides the synergistic conditions that allow for the establishment of latency (Shan et
Author Manuscript
al. 2017). As determined by the limiting dilution quantitative virus outgrowth assay (Q-
VOA), the frequency of latently infected cells in HIV+ individuals is .03–3 infectious units
per million (IUPM) resting CD4+ T cells (Siliciano et al. 2003). This extremely low
frequency of latently infected cells has made biochemical studies of the reservoir
challenging. While seeding of the reservoir is infrequent, the high level of viral replication
during acute infection allows for latency to be established very early after infection. Studies
using SIV have shown that a reservoir is formed within three days of mucosal infection
(Whitney et al. 2014). Early studies estimated that a latent HIV-1 reservoir of 105–107 cells
is established in most individuals during the first weeks of infection (Chun et al. 1997a;
Chun et al. 1998).
Challenges of reservoir reduction
Author Manuscript
The natural longevity of memory CD4+ T cells (Takaki et al. 2000; Hammarlund et al. 2010)
suggested that latent HIV-1 could persist in HIV+ individuals on cART – but for how long?
Early studies on 62 HIV+ individuals on cART for up to seven showed that the half-life of
this population of cells is 43.9 months or ~3.7 years (Siliciano et al. 2003). At this rate, a
population of 1 million latently infected cells would take 73.4 years to naturally decay to
zero, preventing cure in most infected individuals. Recent longitudinal studies of HIV+
individuals on newer cART regimens found a similar decay rate (t½ = 3.6 years) (Crooks et
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 6
al. 2015), suggesting that newer regimens do not hasten decay. Cure through reservoir
Author Manuscript
elimination is referred to as a sterilizing cure (Figure 1). This differs from a functional cure,
in which the reservoir remains but the immune system is modified to allow long-term control
of viral replication without cART. There is a subset of untreated HIV+ individuals known as
“elite controllers” (EC) whose immune response can control viremia to clinically
undetectable levels (Lambotte et al. 2005; Shasha & Walker 2013; Migueles & Connors
2015; O’Connell et al. 2009). Pathogenic, replication-competent HIV-1 can be isolated from
these individuals, but interestingly, their latent reservoirs are 1.5 logs smaller than those in
most other infected individuals (Blankson et al. 2007). While the mechanisms of elite
control remain incompletely understood, it is possible that superior CTL responses may limit
seeding of the reservoir and allow enhanced decay of infected populations that become
reactivated (Migueles & Connors 2015). The example of elite controllers is relevant to
HIV-1 cure because it suggests that in addition to reversing viral latency, it will be important
Author Manuscript
to enhance immune recognition of HIV-1-infected cells. Of note, mathematical models
suggest that these functional cure strategies should be combined with strategies aiming to
purge the reservoir for the greatest likelihood of clinical benefit (Conway & Perelson 2015).
Several informative “near cure” cases directly illustrate the challenge of eradicating the
HIV-1 reservoir. Two individuals known as the “Boston patients” received allogeneic
hematopoietic stem cell transplants (HSCTs) for treatment of hematological malignancies
while they remained on cART. This resulted in reservoir reductions of >2-logs. After
interruption of cART, the patients experienced a long cART-free remission until sudden viral
rebound at 3 and 8 months. Thus, reservoir reduction increased time to rebound (normally 2
weeks), but was not curative (Henrich et al. 2014). In the case of the “Mississippi Child,” a
perinatally infected infant who received cART from 30 hours to 18 months of age, plasma
virus levels remained below the limit of detection for more than 2 years after cART
Author Manuscript
interruption (Persaud et al. 2013). The frequency of latently infected cells in this child was at
least 2.5 logs lower than in a typical treated adult, but the child experienced sudden viral
rebound 27.6 months after cART discontinuation (Luzuriaga et al. 2015; Hill et al. 2016).
What is particularly interesting in these “near cure” cases is that the HIV+ individuals had
very little adaptive immunity to HIV-1, either as a result of the transplant process or very
early treatment (Henrich et al. 2014; Persaud et al. 2013). Without an immune response or
antiretroviral drugs, there is nothing to hold viral replication in check. The long, ART-free
remissions observed in these HIV+ individuals can only be explained by the persistence of a
non-replicating form of the virus in a small number of latently infected cells (Figure 1).
In the only known case of an HIV-1 cure, Timothy Ray Brown (the “Berlin patient”)
underwent a myeloablative HSCT from a donor homozygous for a 32-base pair deletion in
Author Manuscript
the ccr5 gene (CCR5Δ32) followed by cART interruption (Hütter et al. 2009). CD4+ T cells
lacking a functional CCR5 receptor are resistant to infection by the CCR5-tropic (R5) HIV-1
that is responsible for most sexually transmitted cases of infection. An aggressive
conditioning regimen and graft-versus-host disease (GVHD) resulted in complete or near-
complete replacement of recipient immune cells with donor cells. This, together with the
resistance of donor cells to HIV-1 infection, likely led to treatment success. Reservoir assays
suggested that a > 3.5-log reservoir reduction occurred (Yukl et al. 2014; Hill et al. 2016).
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 7
Now eleven years off cART, Mr. Brown has not experienced viral rebound, and all attempts
Author Manuscript
to detect residual HIV-1 have failed (Yukl et al. 2014).
These cases illustrate that a multi-log reduction in the reservoir will be required to prevent
rebound. It is likely that a combination of repeated interventions that induce latency reversal,
cART to prevent viral spread, and cytolytic effector cell killing of productively infected cells
will be needed. In this review, we discuss three major issues that we believe must be
addressed for a successful cure strategy: the mechanisms that maintain latency, the clonal
expansion of infected cells, and immune targeting of HIV-1-infected cells.
Mechanisms of HIV-1 latency
A hallmark of latently infected cells is an integrated but transcriptionally silent HIV-1
provirus (Hermankova et al. 2003). High HIV-1 gene expression leads to a productively
Author Manuscript
infected state, and cells in this state have a short half-life, partly due to the cytopathic effects
of viral gene products (Wei et al. 1995; Perelson et al. 1997). How then is broad-scale
repression of viral gene expression achieved? Mechanisms of HIV-1 latency have been
described in other recent reviews (Peterlin & Price 2006; Karn 2011; van Lint et al. 2013;
Dahabieh et al. 2015) and are only summarized here. Many studies have demonstrated that
stable latency can arise from repressive chromatin states, including obstructive nucleosome
positioning (Verdin et al. 1993; Van Lint et al. 1996), DNA methylation (Kauder et al. 2009),
and posttranslational modifications of histones and non-histone proteins (Van Lint et al.
1996; Coull et al. 2000; Hsia & Shi 2002; Chan & Greene 2011; Williams et al. 2006). Other
mechanisms contributing to stable latency are low levels of host transcription factors (Coiras
et al. 2009) and the HIV-1 Tat protein (Karn 2011), transcriptional interference (Lenasi et al.
2008), and defects in RNA splicing and export (Lassen et al. 2006). It is important to bear in
Author Manuscript
mind that most HIV-1 proviruses in the resting CD4+ T cells of individuals on cART are
defective and should not be considered part of the latent reservoir (Ho et al. 2013; Bruner et
al. 2016). The presence of an excess of defective proviruses complicates measurement of the
latent reservoir and molecular analysis of HIV-1 latency.
Resting CD4+ T cells contain high levels of condensed heterochromatin that limit gene
expression (Festenstein et al. 2003; Tamaru 2010). Early studies tested the hypothesis that
HIV-1 integrates within heterochromatin and that this suppresses gene expression. Indeed, in
the J-lat cell line, an elegant cell line model of HIV-1 latency, some proviruses were found in
heterochromatin-rich regions of the human genome and could produce viral mRNA when
induced by phorbyl esters and TNFα (Jordan et al. 2001). Studies in a an infected SupT1
cell line, however, showed that HIV-1 integrates predominantly within transcribed genes, or
euchromatin (Schröder et al. 2002). In vivo analysis of CD4+ T cells from HIV+ individuals
Author Manuscript
on cART confirmed these latter findings and showed that 93% of integration events occur in
the introns of actively transcribed genes (Han et al. 2008). This phenomenon results partly
from the host factor LEDGF/p75, which binds to HIV-1 integrase and directs HIV-1
integration within active genes (Ciuffi et al. 2005; Meehan et al. 2009). The surprising
finding that HIV-1 can maintain a state of latency while integrated into actively transcribed
host genes suggested that epigenetic silencing must occur through cis-acting elements that
are dominant over the active chromatin state of the host gene.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 8
An integrated HIV-1 provirus contains identical 5’ and 3’ LTRs. While both LTRs can
Author Manuscript
promote transcription, the 5’ LTR serves as the HIV-1 promoter (Ne et al. 2018). The LTR
contains an enhancer, core promoter, and trans-activation response (TAR) region (Ne et al.
2018). Cis- and trans-acting elements interact with the 5’ LTR, allowing HIV-1 transcription
to elegantly synergize with T cell activation and proceed in two stages. Low level-
transcription occurs upon integration and is mediated by the inducible host transcription
factors, NFκB, NFAT, and AP-1, which bind to the viral enhancer (tat-independent phase)
(Nabel and Baltimore 1987; Kinoshita et al. 1998). These factors are sequestered in the
cytosol under resting conditions, but upon T cell activation, they can translocate to the
nucleus, bind to the 5’ LTR, and promote viral transcription by recruiting RNA Pol II and
transcriptional coactivators such as p300/CBP (Molitor et al. 1990; Gerritsen et al. 1997).
Once the viral tat gene is expressed through this early low-level transcription, Tat can bind to
the 5’ end of nascent RNA transcripts and further activate transcription by favoring
Author Manuscript
elongation (tat-dependent phase) (Sodroski et al. 1985; Kao et al. 1987). Major blocks to
HIV-1 gene expression thus arise from the natural physiology of the resting memory CD4+ T
cells that compose the long-lived latent reservoir. In these cells, active forms of the key host
transcription factors are present at only very low levels.
In addition to the lack of host factors important in the initiation of HIV-1 transcription,
repressive epigenetic elements impede transcription initiation. For example, two
nucleosomes, nuc-0 and nuc-1, consistently form within the 5’ LTR even when HIV-1 is
integrated in euchromatin (Verdin et al. 1993) and block host transcriptional machinery. The
fact that histone deacetylase (HDAC) inhibitors can remodel nuc-1 (Laughlin et al. 1993;
Van Lint et al. 1996; El Kharroubi et al. 1998) and that NFκB and other DNA-binding
proteins can recruit HDAC1 to the LTR (Coull et al. 2000) suggests that histone acetylation
controls the position of these nucleosomes. In another example, some studies suggest that
Author Manuscript
DNA methylation at CpG islands near the transcription start site of the 5’ LTR may allow
recruitment of transcriptional repressors (Kauder et al. 2009), although LTR methylation is
not prominent in cells from HIV+ individuals (Ho et al. 2013).
Transcription of HIV-1 in resting CD4+ T cells is also blocked at the level of elongation, due
to low levels of HIV-1 Tat and the host transcription factor P-TEFb (a complex of cyclin T1
and CDK9) (Cary et al., 2016; Budhiraja et al., 2013). Tat enhances HIV-1 expression by
relieving promoter proximal pausing after transcriptional initiation. Specifically, Tat binds to
a TAR mRNA hairpin structure found at the 5’ end of all nascent viral mRNA that is
encoded by the TAR element of the 5’LTR (Feng et al., 1988). The Tat-TAR complex
recruits P-TEFb (Zhu et al. 1997; Mancebo et al. 1997; Wei et al. 1998; Peng et al. 1998),
which can then phosphorylate RNA Pol II, releasing the transcriptional machinery from
Author Manuscript
paused transcription elongation (Parada & Roeder 1996; Bieniasz et al. 1999; Fujinaga et al.
2004). In addition, P-TEFb helps prevent premature Pol II release at terminator sequences
(Bourgeois et al. 2002). Furthermore, in the absence of Tat, P-TEFb can clear negative
regulatory proteins that bind to the LTR and prevent efficient transcription elongation, and
can recruit TATA box binding protein (TBP) to the LTR (Raha et al. 2005). As these
processes lead to more tat transcripts and protein, Tat initiates an explosive positive feedback
loop of viral gene expression. Given the contribution of Tat and P-TEFb to high HIV-1
transcription, the relative absence of Tat and P-TEFb in resting cells from HIV+ individuals
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 9
may promote HIV-1 latency (Karn 2011; Rice 2017). Along these lines, Tat would appear to
Author Manuscript
be an ideal LRA. However, delivery is a challenge and its linker functions would be difficult
to mimic with cell permeable small molecules.
Even if HIV-1 transcriptional initiation and elongation are successful, productive viral gene
expression may not occur. As discussed, HIV-1 primarily integrates into the introns of
actively transcribed genes and is therefore likely subject to transcriptional interference. The
type of interference depends on the orientation of HIV-1 relative to the host gene (Han et al.
2008, Lenasi et al. 2008). In a primary cell model of latency, HIV-1 appeared to show a
slight preference for integration in the same orientation to that of the host gene (Shan et al.,
2011). In such a scenario, an upstream elongating RNA Pol II may displace key transcription
factors on the HIV-1 LTR and maintain viral latency. If HIV-1 is oriented in the opposite
polarity to that of the host gene, collision of opposing RNA Pol II complexes may occur,
causing reduction of one or both transcripts, as well as RNAi and antisense RNA production
Author Manuscript
(Lenasi et al. 2008).
In addition to these distinct mechanisms, there is stochasticity in HIV-1 transcription. This is
likely due to the fact that individual cells differ in metabolic states, stage in the cell cycle,
levels of P-TEFb, and other factors collectively termed “noise” (Ne et al. 2018). However,
after reaching a threshold level, Tat can amplify one outcome (viral reactivation) in a feed-
forward loop (Weinberger & Burnett 2005). This stochasticity may partly explain why not
all proviruses in the latent reservoir are induced upon one round of maximal T cell activation
(Ho et al. 2013; Hosmane et al. 2017). This stochasticity has motivated a search for agents
that can modulate the “noise,” with the idea that agents that increase noise may synergize
with latency reversal therapies to promote viral gene expression (Dar et al. 2014).
Author Manuscript
Latency reversing strategies
Several avenues for identifying LRAs have been explored. The reservoir was originally
demonstrated using T cell activation to reverse latency, and so early studies sought to reverse
latency using the cytokine IL-2 and a T cell receptor (TCR) agonist, murine monoclonal
antibody to CD3. These agents caused severe toxicities without reducing the latent reservoir
(Prins et al. 1999; Kulkosky et al. 2002), a finding which prompted the field to investigate
LRAs that did not induce global T cell activation (Richman et al. 2009). A major problem is
that drug screens using in vitro models of HIV-1 latency identify candidate LRAs that
generally fail to reverse latency in ex vivo studies with cells from HIV+ individuals (Bullen
et al. 2014). To date, the field has focused on LRAs targeting epigenetic mechanisms of
latency, including HDAC inhibitors (Lehrman et al. 2005; Archin et al. 2012; Elliott et al.
2014; Rasmussen et al. 2014; Søgaard et al. 2015), methylation inhibitors (Bouchat et al.
Author Manuscript
2015), and bromodomain and extraterminal domain (BET) protein inhibitors (Lu et al.
2017). One of the first LRAs to be evaluated clinically was valproic acid, a weak HDAC
inhibitor (Lehrman et al. 2005). Unfortunately, HIV+ individuals on chronic valproic acid for
other conditions did not show significant reductions in the reservoir (Siliciano et al. 2007;
Archin et al. 2008; Archin et al. 2010). Recent trials have utilized more potent HDAC
inhibitors originally developed as cancer chemotherapeutic agents. While transient increases
in cell associated and plasma HIV-1 RNA consistent with latency reversal have been seen in
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 10
some clinical studies, no clear reservoir reduction has been reported (Archin et al. 2012;
Author Manuscript
Cillo et al. 2014; Elliott et al. 2014; Rasmussen et al. 2014; Søgaard et al. 2015). These
modest results have led to a renewed interest in T cell activating agents as part of a cure
strategy since T cell activation clearly reverses latency at least in some infected cells.
One type of LRA that induce some degree of T cell activation is protein kinase C (PKC)
agonist class. In a recent study, these were the only LRAs to have an effect across all cell
line models of latency and ex-vivo in patient cells (Bullen et al. 2014). PKC agonists
function as mimics of diacylglycerol and activate cellular PKC isoforms leading to
downstream NFκB activation (for a review, see Jiang & Dandekar 2015). The only clinical
trial using a PKC agonist for HIV-1 eradication involved the natural product PKC agonist
bryostatin-1 (Gutiérrez et al. 2016). Although there was concern about the potential toxicity
of PKC agonists, the study reported no adverse effects in HIV+ individuals. However, no
reduction in the latent reservoir was observed. Notably, conservative drug dosing prevented
Author Manuscript
the drug from reaching detectable systemic concentrations (Spivak and Planelles, 2018). If
studies with PKC agonists move forward, several approaches may mitigate toxicities of
higher PKC agonist dosing. These include administering drugs that target PKC isoforms that
induce proviral gene expression but not proinflammatory cytokines, as well as drugs such as
the JAK inhibitor ruxolitinib (Spivak et al. 2016) or mTOR inhibitors (Martin et al. 2017)
that reduce cytokine production following T cell activation without compromising the
induction of proviral gene expression. The precise effects of these immune-suppressants in
HIV-1 latency reversal continue to be characterized (Besnard et al. 2016). An alternative way
to reduce toxicity from PKC agonists is by using smaller doses that synergize with other
LRA classes. Given the wide array of known factors involved in latency, combinations of
LRAs that act on different pathways may be required to effectively induce viral gene
expression in infected resting memory CD4+ T cells (Bullen et al. 2014). As an example,
Author Manuscript
bryostatin-1 shows synergy in inducing HIV-1 gene expression when paired with the HDAC
inhibitors romidepsin, panobinostat, and vorinostat or with the bromodomain inhibitor JQ1.
Intriguingly, latency reversal by these combinations approaches that seen with T cell
activation (Bullen et al. 2014; Laird et al. 2015; Darcis et al. 2015).
Another approach to latency reversal is based on a prior finding that some latently infected
CD4+T cells are HIV-1-specific (Demoustier et al. 2002; Douek et al. 2002). If a large
fraction of latently infected cells is HIV-1-specific, this population could potentially be
reactivated with an HIV-1 vaccine preparation that provides a near-complete representation
of viral quasispecies (Pankrac et al. 2017). Such a vaccine may also improve CTL priming
and facilitate the “kill” portion of shock and kill strategies (Shan et al. 2012). This approach
illustrates the principle that a latency reversing intervention may involve other cells (in this
Author Manuscript
case, dendritic cells) and induce HIV-1 expression indirectly. Another example is the TLR-7
agonist GS-9620 which has been shown to induce HIV-1 expression in CD4+ T cells
indirectly, possibly by inducing IFNγ release from plasmacytoid dendritic cells (Tsai et al.
2017).
Even if an optimal LRA regimen or a vaccine could reactivate most HIV-1 in aviremic
individuals, it is also important to ensure that these reactivated cells would die. It was
presumed that viral gene products would cause viral cytopathic effects (Roshal et al. 2003;
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 11
Lenardo et al. 2002; Sakai et al. 2006; Shedlock et al. 2008), host immune targeting (Walker
Author Manuscript
et al. 1987; Koup et al. 1994) or both. However, neither viral cytopathic effects nor CTL-
mediated lysis may occur upon latency reversal without additional interventions (Shan et al.
2012). In one study, HIV-1-specific CTL had to be pre-stimulated with HIV-1 peptides in
order to kill autologous patient cells in which latency was reversed (Shan et al., 2012). This
finding may partly explain the failure of several LRA trials to reduce the reservoir. Newer
studies are testing LRAs in conjunction with immune-enhancing vaccine strategies.
Therapeutic vaccination of SIV-infected macaques with Ad26/MVA [recombinant
adenovirus serotype 26 (Ad6) prime, modified vaccine Ankara (MVA) boost] and
stimulation with a TLR7 agonist increased the breadth of SIV-specific immune responses,
decreased viral DNA in lymph nodes and peripheral blood, and delayed rebound upon
treatment interruption (Borducchi et al. 2016). In humans, therapeutic HIV immunization
with Vacc-4×/GM-CSF followed by romidepsin treatment led to a mean reduction of 38% in
Author Manuscript
HIV-1 DNA (Tapia et al. 2017; Leth et al. 2016).
The failure of LRA treatment to reduce the reservoir without additional interventions may
also reflect the interference of certain LRAs (such as the HDAC inhibitors romidepsin,
panobinostat, and SAHA, or combinations of LRAs) with CD8+ T cell effector function
(Jones et al. 2014; Jones et al. 2016; Walker-Sperling et al. 2016; Kwaa et al. 2017), the
prevalence of escape mutations in the latent reservoir (Deng et al., 2015), or CTL exhaustion
(Day et al. 2006) – all described in subsequent sections. In addition, there may be intrinsic
barriers to cell death in latently infected cells (Kim et al. 2018). One example is a relative
decrease in the expression of pro-apoptotic proteins compared to the expression of anti-
apoptotic protein expressions, raising the threshold for apoptosis (Berro et al. 2007;
Neumann et al. 2015; Kim et al. 2018). Therefore, compounds that sensitize latently infected
cells to apoptosis may tip the scale to cell death (Kim et al., 2018). Several of these have
Author Manuscript
been proposed, including Bcl-2 antagonists (Cummins et al. 2016), PI3K/AKT inhibitors
(Lucas et al. 2010), Smac mimetics (Fulda 2015), and the RIG-I inducer acitretin (Li et al.
2016; Garcia-Vidal et al. 2017).
To date, latency reversal has primarily been measured as an increase in cell-associated RNA
following in vitro or ex vivo administration of LRAs (Archin et al. 2012; Søgaard et al.
2015; Elliott et al. 2014; Rasmussen et al. 2014; Archin et al. 2014). An assay that measures
presentation of HIV-1 epitopes by MHC Class I (MHC-I) on CD4+ T cells following latency
reversal would facilitate the evaluation of LRA strategies. The latency clearance assay
(LCA), pioneered by Margolis and colleagues, begins to address this issue (Sung et al.
2015a; Sung et al. 2015b; Sloan et al. 2015; Sung et al. 2017). Briefly, the LCA assay
involves co-culturing CD8+ T cells or ex-vivo expanded HIV-1 specific CD8+ T cells
Author Manuscript
(HXTCs) with autologous resting CD4+ T cells that have been pre-treated with the HDAC
inhibitor vorinostat to induce latency reversal. If latency reversal and CTL-mediated
elimination are successful, fewer latently infected cells remain to produce viral outgrowth
when plated at limiting dilution and maximally stimulated. This was indeed observed, and
the effect was reversed with MHC-I blocking antibodies (Sung et al. 2017).
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 12
HIV-1 persistence due to clonal expansion
Author Manuscript
The remarkable stability of the latent reservoir has been attributed to longevity of the resting
memory CD4+ T cells in which HIV-1 persists (Chun et al. 1997b; Brenchley et al. 2004).
Resting memory CD4+ T cells normally undergo homeostatic and antigen-driven
proliferation (Farber et al. 2014). However, the stimuli that lead to proliferation also lead to
HIV-1 gene expression and consequently viral cytopathic effects, so it was unclear whether
latently infected memory CD4+ T cells could proliferate as well. The earliest evidence of
clonal expansion was provided by the discovery of predominant plasma clones in HIV+
individuals on suppressive cART (Tobin et al. 2005; Bailey et al. 2009). While cART
reduces viremia to levels undetectable by standard clinical tests (limit of detection ~ 50
copies viral RNA/ml), residual viremia at about 1 copy/ml can be detected with special
assays in most treated HIV+ individuals (Dornadula et al. 1999; Maldarelli et al. 2007). This
very low level viremia likely reflects the stochastic daily activation of a small number of
Author Manuscript
latently infected cells (Figure 1). Despite the enormous diversity of viral variants present in
most infected individuals, analysis of plasma HIV-1 RNA sequences from treated HIV+
individuals revealed the presence of many identical sequences that persisted without
evolution over months to years (Bailey et al. 2009). While technical limitations at the time
prevented definitive demonstration that these plasma viruses were derived from a single
productively infected cell clone (as opposed to multiple cells infected with the same virus),
this work provided a conceptual framework for subsequent studies on clonal expansion.
Direct evidence for proliferation of latently infected cells came from an analysis of
integration sites. HIV-1 integrates randomly into transcriptionally active regions of the
human genome (Schröder et al. 2002; Han et al. 2004), and integration sites may therefore
be used as barcodes to distinguish independent infection events. Several groups have
Author Manuscript
reported finding exactly the same HIV-1 integration site in multiple CD4+ T cells from a
given patient on cART (Wagner et al. 2014; Maldarelli et al. 2014; Cohn et al. 2015;
Simonetti et al. 2016). Others have used full-length proviral sequencing (Cohn et al. 2015;
Hosmane et al. 2017) and direct ex-vivo culture systems (Lorenzi et al. 2016; Hosmane et al.
2017; Bui et al. 2017) to provide evidence for clonal expansion of infected cells.
It is important to understand the stimuli driving this proliferative process. Integration of
HIV-1 into pro-growth or cell cycle related genes has been observed and may contribute to
the proliferation of some clones of infected cells (Maldarelli et al. 2014; Wagner et al. 2014).
A pioneering analysis by Chomont et al. suggested that IL-7 and IL-15-driven homeostatic
proliferation could increase numbers of infected CD4+ T cells in vivo (Chomont et al. 2009).
Antigen-driven proliferation (Simonetti et al. 2016) has also been implicated. In the patient
Author Manuscript
studied by Simonetti et al., a massively expanded T cell clone identified by integration site
analysis (Maldarelli et al. 2014) was shown to carry a replication-competent virus.
Intriguingly, plasma viremia produced by this clone paralleled the patient’s natural history of
squamous cell carcinoma: viremia was first detected upon the patient’s initial cancer
diagnosis, decreased upon chemotherapy and radiation treatment, increased during relapse,
and was enriched in tumor tissue at autopsy. These findings raise the possibility that the
expanded clone was proliferating in response to tumor antigen (Simonetti et al. 2016).
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 13
Co-infection with viruses such as CMV and EBV may also lead to antigen-driven
Author Manuscript
proliferation of latently infected cells. In a recent study of 15 HIV-1 infected individuals
who underwent chemotherapy for malignancy, reconstitution of the CD4+ T cell
compartment led to an increase in HIV-1 DNA that was preferentially found in CMV- and
EBV-specific CD4+ T cells (Henrich et al. 2017). However, it remains unclear to what extent
the reservoir is composed of cells specific for these pathogens in the typical patient.
Importantly, most clonal expansion appears to occur in cells carrying defective proviruses
(Cohn et al. 2015). This is expected, as defective proviruses may be less capable of giving
rise to viral proteins that have cytopathic effects, while allowing immune targeting.
However, recent studies have shown that clonal expansion of cells carrying replication-
competent proviruses (Simonetti et al. 2016; Lorenzi et al. 2016; Bui et al. 2017; Hosmane
et al. 2017). This troubling finding suggests that some proliferation indeed drives reservoir
persistence. While some clones of latently infected cells persist, others wax and wane over a
Author Manuscript
period of several years (Wang et al. 2018). These complex dynamics are not consistent with
a cell autonomous proliferative process driven by effects related to integration site.
While proliferation of cells harboring defective proviruses with limited potential for HIV-1
gene expression may occur through normal homeostatic immune processes, clonal
expansion of CD4+T cells harboring replication-competent proviruses is more difficult to
explain. This type of clonal expansion suggests that cellular proliferation may somehow be
decoupled from the activation pathways that turn on HIV-1 expression. Alternatively,
proliferating clones carrying replication-competent proviruses may carry proviruses that are
less susceptible to induction that other proviruses. Stated differently, a single round of T cell
activation does not induce HIV-1 gene expression in all infected cells carrying intact
proviruses (Ho et al. 2013; Hosmane et al. 2017), suggesting that unique factors related to
Author Manuscript
the chromatin environment of individual proviruses or the transcriptional or metabolic state
of the CD4+T cell subset that harbors latent HIV-1 may negatively influence viral
inducibility and allow clonal expansion.
Altogether, these studies show that clonal expansion is a major mechanism for HIV-1
persistence. Three recent studies all show that expanded clones make up 50–60% of the
latent reservoir at any given time (Hosmane et al. 2017; Bui et al. 2017; Lorenzi et al. 2016).
Therefore, in addition to devising novel therapeutic strategies that reactivate and reduce the
reservoir by >4 logs, we must also understand the factors responsible for clonal expansion.
For example, if antigen-driven expansion in response to chronic viral pathogens (e.g. CMV,
EBV) contributes to clonal expansion of the reservoir, therapeutic vaccination of individuals
already infected with these common pathogens may hasten reservoir decay. Cytokine-driven
Author Manuscript
proliferation will be more challenging to intercept therapeutically because it plays an
important role in immune homeostasis (Farber et al. 2014). However, this pathway involves
Jak-Stat signaling through STAT5, and the JAK inhibitors Tofacinib and Ruxolitinib are
approved for long-term use in rheumatoid arthritis, polycythemia vera, and myelofibrosis. In
vitro, these drugs block homeostatic proliferation of CD4+ T cells from aviremic HIV+
individuals without altering T cell effector function (Gavegnano et al. 2017), and it is
possible that these would be used in future cure strategies to prevent reservoir expansion.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 14
Apart from clonal expansion, a controversial mechanism for reservoir persistence involves
Author Manuscript
ongoing cycles of HIV-1 replication despite cART, particularly in potential “sanctuary sites”
such as the lymph node (LN) (Lorenzo-Redondo et al. 2016). Initially, ongoing replication
in treated HIV+ individuals seemed to be a potential mechanism for residual viremia
(Dornadula et al. 1999; Frenkel et al. 2003). In addition, many HIV+ individuals experience
viral “blips,” in which viremia transiently rises above 50 copies/ml. Active viral replication
would inevitably lead to sequence changes given the error-prone nature of the reverse
transcriptase enzyme that copies the viral genome during each cycle. However, direct
sequencing of plasma virus present during blips did not reveal new resistance mutations
(Nettles et al. 2005). Numerous studies have clearly shown that the sequences of integrated
HIV-1 proviruses and of plasma HIV-1 RNA in HIV+ individuals on cART do not evolve
over time (Kieffer et al. 2004; Bailey et al. 2009; Sedaghat et al. 2007; Chomont et al. 2009;
Josefsson et al. 2013; Kearney et al. 2014). Moreover, in a recent study of children who were
Author Manuscript
treated early after perinatally infected, and therefore would have limited viral diversity and
more easily discernable viral evolution, no sequence evolution was observed (van Zyl et al.
2017). The one recent study in which evidence for sequence evolution was presented
(Lorenzo-Redondo et al. 2016) was conducted on lymph node rather than blood samples,
unlike the other studies. However, it has been challenged on methodological grounds
(Rosenbloom et al. 2017).
Further evidence against ongoing cycles of viral replication as a factor in HIV-1 persistence
comes from treatment intensification studies (Figure 1). Intensification of an optimal 3-drug
cART regimen by addition of a fourth antiretroviral drug from another class does not lower
residual viremia (Dinoso et al. 2009; Gandhi et al. 2010; McMahon et al. 2010). Yet another
argument against ongoing viral replication comes from the few “near cure” cases cited
above. If cycles of replication were continuing during cART treatment of these HIV+
Author Manuscript
individuals, then viral rebound should have occurred within 2 weeks of treatment
interruption, as soon as drug levels became sub-therapeutic, given the lack of antiviral
immune responses in these HIV+ individuals.
Directing the immune response to effectively target the reservoir
Latency reversal on its own may not lead to reservoir reduction (Shan et al. 2012). The
immune system must be induced to kill infected cells after latency reversal. CTLs are a
major component of the host response to HIV-1 (Walker et al. 1987; Koup et al. 1994;
Borrow et al. 1997; Schmitz et al. 1999; Gandhi & Walker 2002; Hersperger et al. 2011;
Walker & McMichael 2012). Enhancing CTL responses to viruses harbored in the latent
reservoir requires knowing which antigens will be presented when the cells are activated, an
Author Manuscript
analysis made more complicated by the excess of defective HIV-1 proviruses in vivo.
Moreover, any vaccine strategy must take into account potentially compromised cytolytic
effector function, either from immune exhaustion, impaired memory maintenance, or LRA
interference with effector function. In addition, the approach must also induce proper
trafficking of cytolytic cells to potential “sanctuaries” in the lymph node, and improve the
presentation/processing capacity of antigen presenting cells. These barriers to effective
immune targeting of the reservoir are illustrated in Figure 3 and described below.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 15
Improving CTL recognition of reactivated latently-infected cells
Author Manuscript
The first step in any antiviral memory response is recognition of target cells. For CD8+ T
cells targeting HIV-1 persisting in the latent reservoir, the relevant antigens are peptides
derived from replication-competent proviruses following latency reversal. Technical
limitations currently prevent the physical identification of MHC-I epitopes on infected cells
that have undergone latency reversal. Elution studies and mass spectrometry-based
sequencing – classical methods to obtain proteome-wide views of MHC-I bound peptides –
require 108–1010 cells (Ciudad et al. 2016). As a result, TCR and cell-based biosensors,
which can detect as few as 1 peptide:MHC complex (Irvine et al. 2002), have been used to
assay for specific peptide presentation upon latency reversal (Jones et al. 2016). Proof of
concept studies demonstrated that the IL-15 superagonist ALT-803 can reverse latency in
cells from HIV+ individuals, leading to peptide:MHC presentation detectable by an HLA-
A2-restricted CD8+T cell clone specific for the SLYNTVATL (SL9) peptide from the HIV-1
Author Manuscript
Gag protein (Jones et al. 2016). This immunologic readout provides more direct information
than HIV-1 mRNA induction and encourages further research on “kill” strategies.
Two complications hinder CTL recognition of presented HIV-1 epitopes. First, the latent
reservoir in HIV+ individuals initiating treatment during the chronic stage of infection
contains viruses with escape mutations in immunodominant CTL epitopes (Deng et al.
2015). Escape mutations are selected by potent immune pressure in the early stages of
infection (Goonetilleke et al. 2009; Borrow et al. 1997; Price et al. 1997; Walker &
McMichael 2012). From inoculation until cART initiation, proviral sequences are archived
in the latent reservoir. Therefore, it is unsurprising that the reservoir contains proviruses with
escape mutations to dominant epitopes. What is surprising is that mutant proviruses
comprise the majority of the reservoir unless cART is started within the first months of
infection (Deng et al. 2015). Immunodominance hierarchies may change, but it is clear that
Author Manuscript
any CTL cell-based therapy targeting the reservoir must focus on subdominant epitopes for
which escape mutations have not developed.
A second complication inherent in immune targeting of the latent reservoir is the excess of
defective proviruses. Most defective proviruses appear to have functional LTRs (Ho et al.
2013), and some can be transcribed (Imamichi et al. 2016), giving rise to epitopes that can
be recognized by HIV-1-specific CTL clones (Pollack et al., 2017). Cells carrying defective
proviruses vastly outnumber cells with replication-competent proviruses, so CTL responses
may be diverted by these “decoys” (Pollack et al. 2017).
In a recent study illustrating this potential problem, autologous CTL clones were used to
eliminate infected patient CD4+ T cells that had undergone latency reversal with an IL-15
Author Manuscript
superagonist. While reductions in total HIV-1 DNA were observed, there were no reductions
in the inducible, intact proviruses as measured by the viral outgrowth assay (Huang et al.
2018). The authors concluded that defective proviruses may be preferentially targeted by
CTLs, perhaps due to mutations or deletions in the HIV-1 nef gene (Bruner et al. 2016),
whose protein product downregulates MHC-I (Huang et al. 2018). If so, pharmacologic
blockade of Nef may improve CTL killing of cells harboring intact proviruses and therefore
reduce the reservoir (Mujib et al. 2017a).
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 16
Several strategies may enhance CTL-mediated cure interventions. First, it is critical to target
Author Manuscript
regions of the HIV-1 genome that are relatively conserved across different isolates (Wilson
et al. 2017). Second, because HIV-1 Nef does not downregulate HLA-C or HLA-E
molecules (Cohen et al. 1999), identifying conserved epitopes that may be presented on
these molecules may lead to more effective CTL targeting strategies. Of course, peptide-
based vaccines have limitations (i.e. restricted to particular MHC I alleles, susceptible to
exo- and endopeptidases). Therefore, longer peptides that contain multiple epitopes and are
less subject to degradation may more successfully activate appropriate T cells (Slingluff
2011)
A second approach that may address HIV-1 sequence diversity and immune escape involves
inducing broad immune responses that bypass conventional epitopes. Picker and colleagues
have employed such a strategy in a series of elegant experiments using SIV. A Rhesus
cytomegalovirus (RhCMV) vector was used to deliver SIV antigens to rhesus macaques that
Author Manuscript
were then challenged with SIV. Vaccination led to immune control of SIV viremia in 50% of
monkeys and ultimately complete clearance of the virus after an average of 3.4 years
(Hansen et al. 2009; Hansen et al. 2011; Hansen et al. 2013a). These remarkable results are
likely due to the breadth, promiscuity and non-classical restriction pattern of induced αβ
CD8+ T cells. Specifically, the CD8+ T cells recognized 3 times as many epitopes as CD8+ T
cells induced by conventional adenoviral vectors, and notably, the responses were Class II
and HLA-E restricted (Hansen et al. 2013b; Hansen et al. 2016). The mechanism underlying
this broad, unconventional T cell priming has not been elucidated, but appears to depend on
the replication-competency and tropism of the 68.1 CMV strain used in the vaccine vector
(Hansen et al. 2013b; Hansen et al. 2016).
While more successful than any other preventative HIV-1 or SIVvaccine tested to date, the
Author Manuscript
RhCMV vaccine has not yet been shown to result in cure or control of viremia following
treatment interruption in macaques that were already infected with SIV and would likely
need to be combined with LRAs and cART in curative strategies. It is also unclear whether a
human CMV version of this vaccine vector could be attenuated in a manner that would not
pose a risk for pregnant women or immunocompromised individuals. Regardless,
understanding the mechanism of this remarkable vaccine strategy may yield important
insights into targeting the reservoir. As HLA-E has only two main alleles in the human
population, a vaccine that induces HLA-E-restricted responses should target a large fraction
of infected individuals (Hansen et al. 2016). Class II-restricted CD8+ T cells were reported
recently in a small percent of HIV-1 elite controllers, and HLA-E restricted CD8+ T cell
responses are naturally seen in the human immune response to Mycobacterium tuberculosis
(Joosten et al. 2016). Therefore, it is possible that a strategy to induce non-canonical
Author Manuscript
responses in humans will be successful once we better understand how such responses are
naturally primed.
Antibody targeting of the induced reservoir
Biomarkers of the reservoir—A host cell-surface protein that could easily demark
latently infected cells even without latency reversal could facilitate target cell killing, but has
proven challenging to find. Some studies have suggested that CD4+ T cells expressing
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 17
particular host cell surface proteins contain a large fraction of the HIV-1 reservoir. In the
lymph node, PD-1+ follicular (CXCR5+) and non-follicular CD4+T cells were shown to
Author Manuscript
contain inducible replication-competent virus (Perreau et al. 2013; Banga et al. 2016).
However, these cells may be in an activated state and not therefore representative of the
stable latent reservoir. Moreover, the frequency of these cells decreases over time (Banga et
al. 2016). A separate study in SIV-infected macaques showed that CTLA-4+PD-1– memory
CD4+T cells in the blood, lymph node, spleen, and gut, which share phenotypic markers
with T-regulatory cells, are enriched for replication-competent SIV (McGary et al. 2017).
Another recent report suggested that CD32a, an Fcγ receptor not normally expressed on
CD4+T cells, could serve as a biomarker for the latent reservoir: CD32a+CD4+ T cells were
found to be significantly enriched for HIV-1 DNA and inducible replication-competent virus
(Descours et al., 2017). However, these findings have not been reproduced by other labs
(Bertagnolli et al., 2018) and the search for a latent-reservoir biomarker is ongoing.
Author Manuscript
bNAb targeting of the reservoir—Another strategy for targeting the reservoir is through
the use of antibodies against determinants expressed on infected cells following latency-
reversal. These antibodies may promote lysis of latently infected cells through conjugation
to toxins (Kreitman 2006), antibody-dependent cell mediated cytotoxicity (ADCC) (Horwitz
et al. 2017), or possibly antibody-dependent complement-mediated lysis (ADCML).
Antibody therapy may overcome HLA limitations of peptide-based CTL approaches.
The HIV-1 envelope protein (Env) is synthesized and trafficked to the plasma membrane of
productively infected cells. Antibodies to HIV-1 Env can neutralize HIV-1 and improve
humoral immune responses to the virus (Schoofs et al. 2016). They may also provide
another way to target infected cells following latency reversal. Most HIV+ individuals do not
make neutralizing antibodies to HIV-1 Env until months after initial infection (Maartens et
Author Manuscript
al. 2014). Only a minority of infected individuals make broadly neutralizing antibodies
(bNAbs) against multiple HIV-1 strains (Sather et al. 2009; Mikell et al. 2011). HIV-1 Env
can tolerate extensive mutation with limited viral fitness costs, and steric hindrance from a
glycan sheath can block vulnerable antibody binding sites (Burton and Hangartner 2016).
However, advances in B cell cloning have allowed the HIV-1 vaccine field to produce
bNAbs against vulnerable regions of HIV-1 Env for passive immunization, as described
elsewhere in this issue by John Mascola and Peter Kwong. These antibodies have also
recently been used as research tools to interrogate the latent reservoir. One group recently
used Env-specific bNAbs in a magnetic enrichment and fluorescence-assisted cell sorting
technique (Latency Capture, or LURE) to isolate latently infected cells that were induced to
express Env upon T cell activation (Cohn 2018). Such cells were then subjected to single-
cell RNA-seq analyses to understand transcriptional signatures that may explain the
Author Manuscript
persistence of infected cells.
Recently, bNAbs have been tested in studies targeting the latent reservoir (Halper-Stromberg
et al. 2014). Infusion of bNAbs directed against the CD4+ binding site on the HIV-1 Env
protein led to decreases in viremia in cART-untreated HIV+ individuals (Lynch et al. 2015;
Caskey et al. 2016) and a delay in viral rebound of 4–9 weeks after an analytical cART
interruption in treated HIV+ individuals. (Bar et al. 2016; Scheid et al. 2016; Lu et al. 2016).
Notably, the therapeutic efficacy of one of these antibodies, 3BNC117, was Fc-receptor
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 18
dependent (Bournazos et al., 2014; Lu et al., 2016). Infusion of this antibody enhanced
Author Manuscript
clearance of infected cells and accelerated the emergence of new bNAbs in humans (Scheid
et al. 2016; Lu et al. 2016; Schoofs et al. 2016). Additionally, administering B3NC117 with
the CD4-binding site antibody b12 and the V3-specific monoclonal antibody PGT121
suppressed rebound in macaques chronically infected with pathogenic SHIV, an SIV that
carries the HIV-1 rather than SIV env gene (Barouch et al. 2013). None of these trials
administered bNAbs after latency reversal. Presumably, greater reservoir reductions would
occur in that scenario. An alternative interpretation of the delayed rebound seen in these
studies is that the systemic clearance of antibodies is slower than expected from plasma
measurements, and that it is their continued neutralization potential rather than elimination
of the latent reservoir that delays rebound.
Although bNAbs hold promise for HIV-1 cure, their use has several caveats. Just as
resistance mutations may develop to chemotherapeutic or antiretroviral monotherapy,
Author Manuscript
resistance can develop to single bNAb infusions by selecting for the outgrowth of bNAb-
resistant viruses (Caskey et al. 2016). Therefore, a cocktail of bNAbs may be required
(Mujib et al. 2017b). Impressively engineered bispecific or trispecific bNAbs, capable of
targeting multiple vulnerable sites in Env, may provide an alternative solution (Asokan et al.
2015; Xu et al. 2017). Another caveat is that passive immunization is currently the only
method of delivering bNAbs to HIV+ individuals, and the half-lives of bNAbs, which range
from 12–20 days in HIV+ individuals, will require sequential infusions for improved
reservoir reduction (Caskey et al. 2016; Scheid et al. 2016). However, engineered variants of
bNAbs with substantially longer half-lives are currently being tested (Gaudinski et al.,
2018).
Strategies to induce bNAbs in vivo are ongoing, for instance through delivery via adenovirus
Author Manuscript
serotype 5 (Ad5) or adeno-associated virus serotype 1 (AAV-1) vectors (Badamchi-Zadeh et
al. 2018). Furthermore, Env-reactive non-neutralizing antibodies may still eliminate target
cells through ADCC (Horwitz et al. 2017). This effect may have contributed to the
protection seen in the RV144 trial, the only successful human HIV-1 vaccine trial to date
(Rerks-Ngarm et al. 2009). Finally, other iterations of antibody-based therapy involve
combining bNAb specificity with CTL or NKT activity, through the use of dual-affinity
retargeting (DART) antibodies. These engineered constructs contain a broadly neutralizing
antibody to HIV-1 Env linked to a monoclonal antibody to CD3. DARTS can mediate in
vitro lysis of infected cells that are cultured with autologous CD8+ T cells (Sloan et al. 2015;
Petrovas et al. 2017). Ex-vivo studies have also shown that DARTs can reduce viral
outgrowth from the latent reservoir (Sung et al. 2015b; Sung et al. 2017).
α4β7 immunotherapy—Other antibody-based strategies are also promising. While not a
Author Manuscript
marker of the reservoir per se, the integrin α4β7 expressed on CD4+T cells has become an
interesting antigenic target from a different standpoint. This integrin directs CD4+ T homing
to MAdCAM-expressing mucosal and gut-associated lymphoid tissue (GALT) (Byrareddy et
al. 2016). SIV preferentially infects CD4+ T cells with α4β7 (Kader et al. 2009), and
administration of primatized antibodies against α4β7 integrin (ACT-1) protects macaques
against vaginal challenge with SIV (Byrareddy et al. 2014). In addition, one recent study
found that administration of cART with ACT-1 after 5 weeks of SIV infection led to
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 19
virologic control for up to 9 months after cART interuption in several macaques (Byrareddy
Author Manuscript
et al. 2016). While these results are intriguing, the macaques may have had small reservoirs
due to early treatment (5 weeks), and there is naturally a higher rate of spontaneous control
of SIV compared to HIV-1 (Asquith et al. 2009; Shedlock et al. 2009; Bruel et al. 2015).
Recently, α4β7 was shown to be incorporated in virions, providing another potential
mechanism for control: anti-α4β7 antibodies may both help prevent viral entry and block
new infections, contributing to decreased spreading of viral infection in the gut (Guzzo et al.
2017). An antibody to α4β7 (vedolizumab) is already approved for use in Crohn’s disease,
and provided that it does not induce anti-drug antibodies (as seen with 3 out of 11 tested
macaques) (Byrareddy et al. 2016), it may be an important addition to the HIV-1 cure
regimen in humans. The efficacy of vedolizumab with ART is being tested in a phase I
clinical trial (https://clinicaltrials.gov/ct2/show/NCT02788175).
Reversing effector T cell exhaustion
Author Manuscript
Thus far, this discussion has focused on immune recognition of infected cells. It is also
important to consider factors that compromise effector cell function and migration to target
cells and to design therapies to address these issues. As discussed above, HIV-1-specific
CD8+ T cells from HIV+ individuals on long term cART must be pre-stimulated to kill
infected cells (Shan et al. 2012). This may be due in part to the absence of antigen in HIV+
individuals on long-term cART. In addition, the frequency of Gag-specific CD4+ T cells
decreases with prolonged cART (Pitcher et al. 1999). As antigen-specific CD4+ T cells are
needed for optimal CD8+ T recall responses, decreased frequencies of HIV-1-specific CD4+
T cells may limit CD8+ T cell recall responses. Furthermore, chronic HIV-1 infection leads
to defects in CTL function that are not fully reversed with cART (Kalams et al. 1999). CD4+
and CD8+ T cell exhaustion is a major factor, first defined in pioneering studies using the
Author Manuscript
murine LCMV model (Zajac et al. 1998).
T cell exhaustion arises from persistent antigen exposure and immune activation. It can
occur during chronic viral infections such as HIV-1 or in the setting of malignancy (Day et
al. 2006; Bucks et al. 2009; Streeck et al. 2008; Cockerham et al. 2014). Space and scope
limitations prevent us from detailing underlying mechanisms of exhaustion, but they have
been expertly described at length (Wherry & Kurachi 2015; Hashimoto et al. 2018).
Exhaustion occurs for both CD8+ and CD4+T cells. Antigen-specific effector and memory
cell exhaustion involves a step-wise loss in effector function and proliferative capacity that
can progress in severity until such cells are deleted (Kahan et al. 2015). Exhausted CD8+T
cells have transcriptional and epigenetic profiles distinct from terminally differentiated or
memory CD8+ T cells, secrete fewer cytokines, and are marked by cell-surface expression of
inhibitory receptors such as PD-1, CTLA4, Tim3, TIGIT, CD160, and LAG-3 (Trautmann et
Author Manuscript
al. 2006; Petrovas et al. 2006; Wherry et al., 2007; Jones et al. 2008; Blackburn et al. 2009;
Kahan et al. 2015). Surface expression of inhibitory receptors increases upon activation and
limits excess T cell activation, providing so-called immune checkpoints (IC) (Wherry &
Kurachi 2015). Although these inhibitory receptors are typically downregulated at the
conclusion of an immune response, chronic antigen exposure leads to their persistent
expression on the cell surface. Blocking inhibitory receptors (checkpoint blockade)
rejuvenates certain exhausted anti-viral T cells (Barber et al. 2006; Day et al. 2006;
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 20
Blackburn et al. 2008; Blackburn et al. 2009) as well as CD8+ T cells specific for tumor
antigens (Iwai et al. 2005; Kamphorst et al., 2017). Notably, not all CD8+ T cells respond to
Author Manuscript
checkpoint blockade equally, and combinations of therapies seem to provide the best
recovery of CD8+ T cell function (Blackburn et al. 2008; Im et al. 2016). In the wake of
these studies, several checkpoint therapies have been approved for use in combination cancer
immunotherapy and have revolutionized the oncology field. Such combination therapies may
prove beneficial for the “kill” phase of shock and kill strategies.
If persistent antigen leads to exhaustion, reduced antigen exposure should improve
exhaustion phenotypes. HIV-1-specific CD8+ T cells recovered from the acute phase of
infection in untreated individuals exhibited an exhausted state that is reduced upon cART
treatment or epitope escape (Streeck et al. 2008). However, even in the setting of minimal to
absent persistent antigen, such as in individuals on suppressive cART, effector functions may
not be completely restored. In the lymph node, for example, non-follicular and follicular
Author Manuscript
CD8+ T cells express high levels of PD-1 and TIGIT, and blocking the PD-1/PDL-1 axis in
vitro restores HIV-1-specific CD8+ T cell function in these cells (Petrovas et al. 2017).
Intriguingly, certain IC markers are also present on specific memory CD4+T cells and are
associated with higher HIV-1 DNA content, suggesting that these ICs somehow promote
latency in these subsets (Chomont et al., 2009; Fromentin et al., 2016). As such, anti-
PD-1/PD-L1 antibodies may be useful in HIV-1 cure strategies, as they improve CTL
function (primarily on CXCR5+ expressing CD8+T cells present in the lymph node) and
target a portion of the latent reservoir. A Phase I randomized clinical trial of anti-PD-L1
antibodies showed a trend towards enhanced Gag-specific CD8+T cell responses (Gay et al.
2017).
Diminished CTL functionality and migration into lymph nodes
Author Manuscript
Antigen recognition and dysfunctional effector cells are not the only impediments to killing
of infected cells. Location is another challenge, as effector and target cells must be in close
proximity. Most target cells are located in the lymphoid tissues such as the lymph nodes.
The gut-associated lymphoid tissue (GALT) contains a substantial proportion of the body’s
lymphocytes, and CD4+ T cells in the GALT are the first to be targeted during acute
infection (Veazey 1998). In HIV+ individuals on cART, there is a high frequency of proviral
DNA in CD4+ T cells in the GALT: 5000 copies/1 million cells, nearly five times higher
than that in blood (Chun et al. 2008). This may reflect the increase susceptibility of these
cells to infection due to high frequency of CCR5 expression and the overall higher activation
state of these CD4+ T cells. Although it remains controversial whether the GALT is a major
HIV-1 reservoir (Lerner et al. 2011; Rothenberger et al. 2015), interventions that can
appropriately target infected cells in the GALT may be needed.
Author Manuscript
Within the lymph nodes, CTLA4+CD4+T cells appear to serve as a target cell type for
infection in the T cell zone of the lymph node (McGary et al., 2017), while the CD4+ T
follicular helper (TfH) cell subset within the B cell follicle of the lymph node forms a major
CD4+ compartment for HIV-1 production (Lindqvist et al. 2012; Fukazawa et al. 2012;
Petrovas et al. 2012; Perreau et al. 2013; Boritz et al., 2016). CTLs do not normally express
receptors that allow homing to the B cell follicle until late in untreated infection (Connick et
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 21
al. 2007). Therefore, B cell follicles are considered sanctuary sites for HIV-1 replication as
Author Manuscript
they are shielded from CTL and/or NK cell-mediated cytolysis (Fukazawa et al. 2015; Huot
et al. 2017). Indeed, CTL exclusion from the follicle appears to be the mechanism for viral
replication within TfH cells in elite controller macaques. Depletion of anti-viral CD8+ T
cells leads to SIV replication in non-follicular CD4+ T cells (Fukazawa et al. 2015). Full
reservoir clearance may require inducing HIV-1 expression in TfH cells and then targeting
this compartment with CTLs. Proposed approaches to addressing this dilemma include
temporarily disrupting the B cell follicle with B cell depleting antibodies (anti-CD20) or by
blocking B/T cell interactions (anti-CD40L blockade) (Fukazawa et al. 2015). Additionally,
as CCR7lowCXCR5hi CD8+T cells can home to B cell follicles during late stage infection
and AIDS, therapeutic vaccine approaches that induce this effector cell phenotype should be
pursued (Fukazawa et al. 2015).
Another consideration is that CTL within lymph nodes appear to differ in some respects
Author Manuscript
from CTL in blood. Fewer terminally differentiated effector CD8+T cells are present in the
lymph nodes of HIV+ individuals than in their blood (Reuter et al. 2017). Moreover, lymph
node CTLs have a limited ability to kill targets and express lower levels of perforin, an
essential mediator of cytolysis (Petrovas et al. 2017; Reuter et al. 2017). Similar findings
have been obtained from studies on the human gastrointestinal mucosa of HIV+ individuals
(Kiniry et al. 2017). Differences in transcriptional programming of CTLs in the LN versus
blood may account for these differences (Reuter et al. 2017). Notably, certain LRAs (such as
the TLR7 agonist GS-9620) can actually increase cytolytic activity of CD8+ T cells (Tsai et
al. 2017), and could be used for this purpose.
NK cell escape and immunotherapy approaches
The HIV-1 cure field has focused on inducing T-cell based cytolytic therapies, given that
Author Manuscript
these cells exert potent selection pressure on the virus and the fact that viral control in rare
individuals is linked to CTL responses (Walker et al. 1987; Gandhi & Walker 2002;
Hersperger et al. 2011; Migueles & Connors 2015). However, natural killer (NK) cells may
also play an important role in cure strategies. NK cells, the effectors likely responsible for
antibody-mediated clearance mentioned earlier, have also been implicated in HIV-1 and SIV
control (Alter et al. 2011; Ramsuran et al. 2018). Intriguingly, NK cells localize within and
around lymph nodes in African green monkeys, a natural SIV host in which infection does
not progress to AIDS (Huot et al. 2017). Two major types of NK cells exist in humans,
distinguished by their anatomical location. In blood, 90% of NK cells are CD56dim, express
perforin (Fehniger et al. 2003; Ferlazzo et al. 2004), and can be recruited to the lymph node
in a CCR7-and CXCR3-dependent manner by certain adjuvants or by mature dendritic cell
injection in murine models (Martín-Fontecha et al. 2004). A separate NK cell population
Author Manuscript
predominates in human lymph nodes and is CD56bright. These cells do not express perforin
constitutively, but can upregulate cytolytic function following exposure to low-levels of IL-2
secreted by T cells (Fehniger et al. 2003; Ferlazzo et al. 2004).
While viral escape from CTL-mediated immune pressure has been established (Borrow et al.
1994; Price et al. 1997), more recent studies demonstrate that NK cell-mediated pressure can
also lead to viral sequence changes (Alter et al. 2011). The activation status of NK cells
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 22
depends on the balance between activating and inhibitory receptors (Cassidy et al. 2014).
Author Manuscript
The killer cell immunoglobulin-like receptors (KIR) are inhibitory NK cell receptors that
recognize specific HLA-A, -B, and -C alleles, along with associated peptides (Thananchai et
al. 2007). Mutations in the HIV-1 sequence can influence the nature of peptides that bind to
these MHC molecules, potentially leading to modified binding of inhibitory receptors and
altered NK cell activity. Indeed, in untreated HIV+ individuals homozygous for the
inhibitory receptor KIR2DL, Alter et al. identified several relevant mutations in Env and the
viral protein u (Vpu). CD4+T cells infected with an HIV-1 strain carrying these mutations
were killed less efficiently by KIR2DL+ expressing NK cells (Alter et al. 2011). It is unclear
to what extent the latent reservoir has archived KIR-associated polymorphisms in proviruses
that mediate NK-cell escape. Databases for full-length proviral sequences could be mined to
determine whether resistance to NK-mediated killing is a characteristic of the reservoir
(Ramsuran et al. 2018).
Author Manuscript
In a subset of HIV+ individuals treated with the HDAC inhibitor panobinostat, levels of
HIV-1 DNA decreased by 70–80% and were associated with a slightly longer time to viral
rebound during analytical treatment interruption (Olesen et al. 2015). Interestingly, HIV+
individuals with this favorable outcome had higher frequencies of cytotoxic CD56dim NK
cells (Olesen et al. 2015), and the authors speculate that this may have resulted from LRA-
induced alteration in expression of NK receptor ligands on infected CD4+T cells. In another
study, PEG-IFNα induced NK cell activation in Hepatitis C/HIV-1 coinfected individuals on
long-term suppressive cART; there was a significant correlation between CD56bright NK cell
levels and decreases in cell-associated proviral DNA (Hua et al. 2017). These results
indicate that both types of NK cells may play a role in cytolysis of infected cell targets upon
HIV-1 induction. Thus, agents that activate NK cells – by increasing activating receptor
expression and/or decreasing inhibitory receptor expression – may improve clearance of
Author Manuscript
latently infected cells following latency reversal.
Recently, “memory-like” NK cells have been identified in the murine, macaque, and human
immune systems. These cells are often identified by higher expression of the NKG2C
activating receptors (Lopez-Vergès et al. 2011; Reeves et al. 2015). The fact that memory-
like NK cells were observed in macaques five years after Ad26 vaccination suggests that
persistent antigen may not be required for their survival and that these cells may be induced
through specific vaccination (Reeves et al. 2015). While intriguing, NK cell memory is a
new area with many unknowns. Which subsets of cells serve as “memory” responders and
which ligands induce NK cell memory are unclear (Peng & Tian 2017). Whether such
memory cells can immediately exert effector function after HIV-1 reactivation is also
uncertain (Peng & Tian 2017). Finally, as we still do not know the extent of NK escape
Author Manuscript
mutations in the reservoir, it is possible that such mutations may increase the threshold for
NK cell activation by strengthening inhibitory receptor binding. Despite these caveats,
understanding the basic mechanisms underlying NK cell memory to SIV and HIV-1 is
important for improving vaccine-induced cytolytic therapies.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 23
Other clinically relevant reservoirs in the quest for a cure
Author Manuscript
In this review, we have focused on resting memory CD4+ T cells as the primary and best
understood reservoir of HIV-1. This reservoir contains integrated, replication-competent
HIV-1 that can be reactivated with T cell stimulation, is readily demonstrable in all infected
individuals, and persists indefinitely even in infected individuals on cART. No other
proposed reservoir has yet to been shown to fulfill all of these criteria. Monocytes and
macrophages express low levels of CD4 and CCR5 and are susceptible to infection by R5-
tropic HIV-1 (Gartner et al. 1986; Igarashi et al. 2003). Macrophages are thought to be
especially important in HIV-1 disease pathogenesis and HIV-1-associated dementia (HAD)
as CD4+ T cell targets become depleted. However, their role in HIV-1 persistence in treated
HIV+ individuals remains controversial.
Monocytes are continuously produced in the bone marrow, circulate briefly (half-life in the
Author Manuscript
circulation = 1 day), and then enter tissues and differentiate into macrophages in a tissue-
specific fashion, for example into microglia in the brain. Thus monocytes cannot serve as a
long-lived reservoir. Tissue-resident macrophages derived from monocytes have a relatively
short half-life on the order of weeks, depending on the tissue (Ginhoux & Guilliams 2016),
while those derived from embryonic hematopoetic precursors have a longer half-life of 24–
36 months (Kandathil et al. 2016). Integrated proviral DNA has been observed in brain
astrocytes and microglia (Churchill et al. 2006), which have half-lives on the order of
months and years, respectively (Marban et al. 2016). However, astrocytes are unable to be
infected in vitro and observed integrated DNA may have been due to engulfment of HIV-1
infected cells (Russell et al., 2017). Therefore, of the known long-lived non-T cell subtypes,
embryonically-derived macrophages or microglia could serve as long-term HIV-1 reservoirs.
Author Manuscript
One interesting proposed mechanism of SIV latency in the brain is through infection-
induced IFNβ mRNA production by macrophages. IFNβ mRNA suppresses LTR activity
directly and by inducing a dominant-negative CCAAT/enhancer-binding protein-β (C/EBP-
β) that suppresses histone acetylation at the SIV LTR (Barber et al. 2006). Low
susceptibility of macrophages to CD8+ T cell killing due to decreased granzyme B
sensitivity is another proposed mechanism for HIV-1 and SIV persistence (Vojnov et al.
2012; Rainho et al. 2015; Clayton et al. 2017). Interestingly, retroviral infection of these
non-dividing cell types is unexpected. Degradation of dNTPs by host restriction factor
SAMHD1 within macrophages slows the reverse transcription process and therefore limits
productive infection of macrophages by HIV-1 (Laguette et al. 2011). SIV has developed a
mechanism to address this limitation through its gene product Vpx, which facilitates the
ubiquitination and degradation of SAMHD1. However, HIV-1 lacks Vpx and the extent of
Author Manuscript
macrophage infection by HIV-1 in vivo is still not clear.
While the latent reservoir in resting CD4+ T cells can be readily studied using peripheral
blood samples, analysis of the role of macrophages and other potential reservoirs for HIV-1
persistence requires tissue samples. Few studies have been conducted on tissue macrophages
from HIV+ individuals or SIV-infected macaques on suppressive cART for at least six
months (Thompson et al. 2011; Churchill et al. 2006). The length of treatment is important
because HIV-1 DNA or RNA observed in macrophages from untreated HIV+ individuals or
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 24
those on short-term treatment may not represent stable long-term infection. Notably, residual
free virus has been observed in the cerebrospinal fluid of HIV+ individuals on long-term
Author Manuscript
suppressive cART (Dahl et al. 2014), but it is unclear whether this arises from memory
CD4+ T cells passing through the recently discovered brain lymphatic system (Louveau et
al. 2015) or resident long-lived immune cells harboring latent HIV-1 that have become
activated. Past reports have also shown that macrophages from the lung (alveolar
macrophages) (Cribbs et al. 2015), duodenum (Zalar et al. 2010), and GALT (Josefsson et
al. 2013) contain HIV-1 proviral DNA in infected individuals on cART. However, the
presence of proviral DNA does not prove direct infection unless phagocytosis of debris from
dying CD4+ T cells by macrophages is ruled out (Calantone et al. 2014). In some cases
engulfment can lead to productive macrophage infection in vitro (Baxter et al. 2014).
Observing both TCR and integrated proviral sequences from isolated macrophage DNA
would help address this question.
Author Manuscript
SIV macaque models as well as several mouse models can provide a way around the limited
access to human tissues (DiNapoli et al. 2016; Honeycutt et al. 2017). For example,
reservoir dynamics have been recently studied in an elegant myeloid-only mouse (MoM)
model. Human CD34+ progenitor cells were engrafted into NOD/SCID mice that cannot
support T cell development, thereby allowing for only B cells and myeloid lineage cells to
develop. Mice were infected HIV-1, treated with cART, and then subjected to treatment
interruption. Notably, infected macrophages had a half-life of < 1 day based on the decay of
viremia, and only 33% of mice experienced viral rebound (Honeycutt et al. 2017). Thus in
this model system, infected macrophages decayed so rapidly in vivo that prolonged cART
may be sufficient to dramatically reduce this population. Had cART been extended, it is
possible that none of the animals would have experienced viral rebound. Still, the fact that
some rebound did occur underscores the heterogeneity of macrophages and the fact that
Author Manuscript
some long-lived immune cells, possibly in the brain, may serve as a reservoir. It is important
to address this question, in particular from a non-human primate model or from human
autopsy studies. Novel assays to detect HIV-1 viral outgrowth from macrophages isolated
from treated HIV+ individuals or SIV-infected macaques will be critical in addressing this
question (Avalos et al. 2016; Clayton et al. 2017).
Conclusion
HIV-1 continues to be a global pandemic even with the availability of modern cART, and the
infection remains incurable due to a long-lived reservoir of quiescent CD4+ T cells that
harbor infectious proviruses. For the past twenty years, the field has made remarkable strides
in defining key genetic, molecular, and cellular features of the latent reservoir. This work has
Author Manuscript
led to strategies to “shock” HIV-1 out of latency and “kill” infected cells. As outlined,
however, many hurdles remain to developing a cure strategy that takes into account the
complex mechanisms of HIV-1 persistence. Novel techniques to interrogate the reservoir and
direct killing of the relevant target cells will be critical moving forward. Based on several
exciting near-cure cases and a single cure case, there is considerable optimism about the
prospect of a global cure, and it is likely that several of the pharmacologic and immunologic
interventions discussed here will pave the way for this.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 25
Acknowledgments
Author Manuscript
We thank Janet Siliciano, Kevin Shenderov, and Andrew Timmons for advice on the manuscript. This work was
supported by the NIH Martin Delaney I4C (UM1 AI126603), Beat-HIV (UM1 AI126620) and DARE (UM1
AI12661) Collaboratories, by the Johns Hopkins Center for AIDS Research (P30AI094189), and by the Howard
Hughes Medical Institute and the Bill and Melinda Gates Foundation (OPP1115715).
References
Alter G et al., 2011 HIV-1 adaptation to NK-cell-mediated immune pressure. Nature, 476(7358), pp.
96–101. [PubMed: 21814282]
Archin NM et al., 2012 Administration of vorinostat disrupts HIV-1 latency in patients on
antiretroviral therapy. Nature, 489(7416), p.460.
Archin NM et al., 2010 Antiretroviral intensification and valproic acid lack sustained effect on residual
HIV-1 viremia or resting CD4+ cell infection. PLoS ONE, 5(2): e9390. [PubMed: 20186346]
Archin NM et al., 2014 Eradicating HIV-1 infection: Seeking to clear a persistent pathogen. Nature
Author Manuscript
Reviews Microbiology, 12(11), pp.750–764. [PubMed: 25402363]
Archin NM et al., 2008 Valproic acid without intensified antiviral therapy has limited impact on
persistent HIV infection of resting CD4+ T cells. AIDS, 22(10), pp.1131–1135. [PubMed:
18525258]
Asokan M et al., 2015 Bispecific Antibodies Targeting Different Epitopes on the HIV-1 Envelope
Exhibit Broad and Potent Neutralization. Journal of Virology, 89(24), pp.12501–12512. [PubMed:
26446600]
Asquith B et al., 2009 Lymphocyte kinetics in health and disease. Trends in Immunology, 30(4), pp.
182–189. [PubMed: 19286425]
Avalos CR et al., 2016 Quantitation of Productively Infected Monocytes and Macrophages of Simian
Immunodeficiency Virus-Infected Macaques. Journal of Virology, 90(12), pp.5643–5656. [PubMed:
27030272]
Badamchi-Zadeh A et al., 2018 Therapeutic efficacy of vectored PGT121 gene delivery in HIV-1-
infected humanized mice. Journal of Virology, p.JVI.01925–17.
Bailey JR et al., 2009 Analysis of human immunodeficiency virus type 1 viremia and provirus in
Author Manuscript
resting CD4+ T cells reveals a novel source of residual viremia in patients on antiretroviral
therapy. Journal of virology, 83(17), pp.8470–81. [PubMed: 19535437]
Baldauf H-M et al., 2012 SAMHD1 restricts HIV-1 infection in resting CD4+ T cells. Nature
Medicine, 18(11), pp.1682–1688.
Banga R et al., 2016 PD-1+and follicular helper T cells are responsible for persistent HIV-1
transcription in treated aviremic individuals. Nature Medicine, 22(7), pp.754–761.
Bar KJ et al., 2016 Effect of HIV Antibody VRC01 on Viral Rebound after Treatment Interruption.
New England Journal of Medicine, 375(21), pp.2037–2050. [PubMed: 27959728]
Barber DL et al., 2006 Restoring function in exhausted CD8 T cells during chronic viral infection.
Nature, 439(7077), pp.682–687. [PubMed: 16382236]
Barber SA et al., 2006 Mechanism for the establishment of transcriptional HIV latency in the brain in a
simian immunodeficiency virus-macaque model. The Journal of infectious diseases, 193(7), pp.
963–70. [PubMed: 16518758]
Barouch DH et al., 2013 Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal
Author Manuscript
antibodies in SHIV-infected rhesus monkeys. Nature, 503(7475), pp.224–228. [PubMed:
24172905]
Barré-Sinoussi et al., 1983 Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired
immunodeficiency syndrome (AIDS). Science, 220(4599), pp.868–71. [PubMed: 6189183]
Baxter AE et al., 2014 Macrophage infection via selective capture of HIV-1-infected CD4+ T cells.
Cell Host and Microbe, 16(6), pp.711–721. [PubMed: 25467409]
Berro R et al., 2007 Identifying the membrane proteome of HIV-1 latently infected cells. Journal of
Biological Chemistry, 282(11), pp.8207–8218. [PubMed: 17237230]
Bertagnolli et al., 2018 Substantial Fraction of HIV reservoir is CD32 negative. Nature, in press.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 26
Besnard E et al., 2016 The mTOR Complex Controls HIV Latency. Cell Host and Microbe, 20(6), pp.
785–797. [PubMed: 27978436]
Author Manuscript
Budhiraja et al., 2013 Cyclin T1 and CDK9 T-loop Phosphorylation Are Downregulated during the
Establishment of HIV-1 Latency in Primary Resting Memory CD4+ T cells. Journal of Virology,
87(2), pp.1211–1220. [PubMed: 23152527]
Bieniasz PD et al., 1999 Recruitment of cyclin T1/P-TEFb to an HIV type 1 long terminal repeat
promoter proximal RNA target is both necessary and sufficient for full activation of transcription.
Proceedings of the National Academy of Sciences of the United States of America, 96, pp.7791–6.
[PubMed: 10393900]
Blackburn SD et al., 2009 Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors
during chronic viral infection. Nature Immunology, 10, pp.29–37. [PubMed: 19043418]
Blackburn SD et al., 2008 Selective expansion of a subset of exhausted CD8 T cells by PD-L1
blockade. Proceedings of the National Academy of Sciences, 105(39), pp.15016–15021.
Blankson JN et al., 2000 Biphasic Decay of Latently Infected CD4 + T Cells in Acute Human
Immunodeficiency Virus Type 1 Infection. The Journal of Infectious Diseases, 182(6), pp.1636–
1642. [PubMed: 11069234]
Author Manuscript
Blankson JN et al., 2007 Isolation and characterization of replication-competent human
immunodeficiency virus type 1 from a subset of elite suppressors. Journal of virology, 81(5), pp.
2508–18. [PubMed: 17151109]
Bleul CC et al., 1997 The HIV coreceptors CXCR4 and CCR5 are differentially expressed and
regulated on human T lymphocytes. Immunology, 94(March), pp.1925–1930.
Böhnlein E et al., 1988 The same inducible nuclear proteins regulates mitogen activation of both the
interleukin-2 receptor-alpha gene and type 1 HIV. Cell, 53(5), pp.827–836. [PubMed: 2836068]
Borducchi EN et al., 2016 Ad26/MVA therapeutic vaccination with TLR7 stimulation in SIV-infected
rhesus monkeys. Nature, 540(7632), pp.284–287. [PubMed: 27841870]
Borrow P et al., 1997 Antiviral pressure exerted by HIV-1-specific cytotoxic T lymphocytes (CTLs)
during primary infection demonstrated by rapid selection of CTL escape virus. Nature Medicine,
3(2), pp.205–211.
Borrow P et al., 1994 Virus-Specific CD8+ Cytotoxic T-Lymphocyte Activity Associated with Control
of Viremia in Primary Human-Immunodeficiency-Virus Type-1 Infection. Journal of Virology,
Author Manuscript
68(9), pp.6103–6110. [PubMed: 8057491]
Bouchat S et al., 2015 Sequential treatment with 5-aza-2’-deoxycytidine and deacetylase inhibitors
reactivates HIV- 1. EMBO Molecular Medicine, 8(2), pp.1–22.
Bourgeois CF et al., 2002 Spt5 cooperates with human immunodeficiency virus type 1 Tat by
preventing premature RNA release at terminator sequences. Molecular and cellular biology, 22, pp.
1079–93. [PubMed: 11809800]
Bournazos S et al., 2014 Broadly neutralizing anti-HIV-1 antibodies require Fc effector functions for in
vivo activity. Cell, 156(6), pp. 1243–1253.
Boritz EA et al., 2016 Multiple Origins of Virus Persistence during Natural Control of HIV infection.
Cell, 166, pp. 1004–1015. [PubMed: 27453467]
Brenchley JM et al., 2004 CD4 + T Cell Depletion during all Stages of HIV Disease Occurs
Predominantly in the Gastrointestinal Tract. The Journal of Experimental Medicine, 200(6), pp.
749–759. [PubMed: 15365096]
Bruel T et al., 2015 Long-term control of simian immunodeficiency virus (SIV) in cynomolgus
macaques not associated with efficient SIV-specific CD8+ T-cell responses. Journal of virology,
Author Manuscript
89(7), pp.3542–3556. [PubMed: 25589645]
Bruner KM et al., 2016 Defective proviruses rapidly accumulate during acute HIV-1 infection., 22(9),
pp.1043–1050.
Bucks CM et al., 2009 Chronic Antigen Stimulation Alone Is Sufficient to Drive CD8+ T Cell
Exhaustion. The Journal of Immunology, 182(11), pp.6697–6708. [PubMed: 19454664]
Bui JK et al., 2017 Proviruses with identical sequences comprise a large fraction of the replication-
competent HIV reservoir. PLoS Pathogens, 13(3), pp. e1006283, [PubMed: 28328934]
Bullen CK et al., 2014 New ex vivo approaches distinguish effective and ineffective single agents for
reversing HIV-1 latency in vivo. Nature Medicine, 20(4), pp.425–429.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 27
Burton DR & Hangartner L, 2016 Broadly Neutralizing Antibodies to HIV and Their Role in Vaccine
Design.
Author Manuscript
Byrareddy SN et al., 2016 Sustained virologic control in SIV+ macaques after antiretroviral and 4 7
antibody therapy. Science, 354(6309), pp.197–202. [PubMed: 27738167]
Byrareddy SN et al., 2014 Targeting α4β7 integrin reduces mucosal transmission of simian
immunodeficiency virus and protects gut-associated lymphoid tissue from infection. Nature
Medicine, 20(12), pp.1397–1400.
Calantone N et al., 2014 Tissue myeloid cells in SIV-infected primates acquire viral DNA through
phagocytosis of infected T cells. Immunity, 41(3), pp.493–502. [PubMed: 25238099]
Cary DC, Fujinaga K, and Peterlin BM, 2016 Molecular mechanisms of HIV latency. Journal of
Clinical Investigation, 126(2), pp. 448–454. [PubMed: 26731470]
Caskey M, Klein F, Nussenzweig MC, 2016 Broadly Neutralizing Antibodies for HIV-1 Prevention or
Immunotherapy. New England Journal of Medicine, pp.2019–2021. [PubMed: 27959740]
Cassidy SA, Cheent KS & Khakoo SI, 2014 Effects of peptide on NK cell-mediated MHC I
recognition. Frontiers in Immunology, 5(133), pp.1–8. [PubMed: 24474949]
Chan JKL & Greene WC, 2011 NF-κB/Rel: agonist and antagonist roles in HIV-1 latency. Current
Author Manuscript
opinion in HIV and AIDS, 6, pp.12–8. [PubMed: 21242888]
Chomont N et al., 2009 HIV reservoir size and persistence are driven by T cell survival and
homeostatic proliferation. Nature Medicine, 15(8), pp.893–900.
Chun T et al., 2008 Persistence of HIV in Gut‐Associated Lymphoid Tissue despite Long‐Term
Antiretroviral Therapy. The Journal of Infectious Diseases, 197(5), pp.714–720. [PubMed:
18260759]
Chun TW et al., 1995 In vivo fate of HIV-1-infected T cells: Quantitative analysis of the transition to
stable latency. Nature Medicine, 1(12), pp.1284–1290.
Chun et al., 1997a Quantification of latent tissue reservoirs and total body viral load in HIV-1
infection. Nature, 387(6629), pp.183–188. [PubMed: 9144289]
Chun et al., 1997b Presence of an inducible HIV-1 latent reservoir during highly active antiretroviral
therapy. PNAS, 94(24), pp. 13193–13197. [PubMed: 9371822]
Chun T-W et al., 1998 Early establishment of a pool of latently infected, resting CD4+ T cells during
primary HIV-1 infection. Proceedings of the National Academy of Sciences, 95(15), pp. 8869–
Author Manuscript
8873.
Chun et al., 1999 Re-emergence of HIV after stopping therapy. Nature, 401, pp.874–875. [PubMed:
10553903]
Churchill MJ et al., 2006 Use of laser capture microdissection to detect integrated HIV-1 DNA in
macrophages and astrocytes from autopsy brain tissues. Journal of NeuroVirology, 12(2), pp.146–
152. [PubMed: 16798676]
Cillo AR et al., 2014 Quantification of HIV-1 latency reversal in resting CD4+ T cells from patients on
suppressive antiretroviral therapy. Proceedings of the National Academy of Sciences, 111(19), pp.
7078–7083.
Ciudad MT et al., 2016 Analysis of the HLA-DR peptidome from human dendritic cells reveals high
affinity repertoires and nonconventional pathways of peptide generation. Journal of leukocyte
biology, 101(February), pp.1–13.
Ciuffi A et al., 2005 A role for LEDGF/p75 in targeting HIV DNA integration. Nature Medicine, 11,
pp.1287–1289.
Author Manuscript
Clayton KL et al., 2017 HIV Infection of Macrophages: Implications for Pathogenesis and Cure.
Pathogens and Immunity, 2(2), p.179. [PubMed: 28752134]
Cockerham LR et al., 2014 Programmed death-1 expression on CD4+ and CD8+ T cells in treated and
untreated HIV disease. AIDS (London, England), 28(12), pp.1749–58.
Cohen GB et al., 1999 The selective downregulation of class I major histocompatibility complex
proteins by HIV-1 protects HIV-infected cells from NK cells. Immunity, 10(6), pp.661–671.
[PubMed: 10403641]
Cohn LB et al., 2015 HIV-1 integration landscape during latent and active infection. Cell, 160(3), pp.
420–432. [PubMed: 25635456]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 28
Cohn LB et al., 2018 Clonal CD4+ T cells in the HIV-1 latent reservoir display a distinct gene profile
upon reactivation. Nature Medicine doi:10.1038/s41591-018-0017-7.
Author Manuscript
Coiras M et al., 2009 Understanding HIV-1 latency provides clues for the eradication of long-term
reservoirs. Nature Reviews Microbiology, 7(11), pp.798–812. [PubMed: 19834480]
Connick E et al., 2007 CTL Fail to Accumulate at Sites of HIV-1 Replication in Lymphoid Tissue. The
Journal of Immunology, 178(11), pp.6975–6983. [PubMed: 17513747]
Conway JM & Perelson AS, 2015 Post-treatment control of HIV infection. PNAS, 112(17), pp.5467–
72. [PubMed: 25870266]
Coull JJ et al., 2000 The human factors YY1 and LSF repress the human immunodeficiency virus type
1 long terminal repeat via recruitment of histone deacetylase 1. Journal of virology, 74(15), pp.
6790–9. [PubMed: 10888618]
Cribbs SK et al., 2015 Healthy HIV-1-Infected Individuals on HAART Harbor HIV-1 in their Alveolar
Macrophages. AIDS research and human retroviruses, 31(1), pp.64–70. [PubMed: 25134819]
Crooks AM et al., 2015 Precise Quantitation of the Latent HIV-1 Reservoir: Implications for
Eradication Strategies. Journal of Infectious Diseases, 212(9), pp.1361–1365. [PubMed:
25877550]
Author Manuscript
Cummins NW et al., 2016 Prime, Shock, and Kill: Priming CD4 T Cells from HIV Patients with a
BCL-2 Antagonist before HIV Reactivation Reduces HIV Reservoir Size. Journal of Virology,
90(8), pp.4032–4048. [PubMed: 26842479]
Dahabieh MS, Battivelli E & Verdin E, 2015 Understanding HIV Latency: The Road to an HIV Cure.
Annu. Rev. Med, 66, pp.407–21. [PubMed: 25587657]
Dahl V et al., 2014 Low levels of HIV-1 RNA detected in the cerebrospinal fluid after up to 10 years of
suppressive therapy are associated with local immune activation. AIDS (London, England),
28(15), pp.2251–8.
Dar RD et al., 2014 Screening for noise in gene expression identifies drug synergies. Science,
344(6190), pp.1392–1396. [PubMed: 24903562]
Darcis G et al., 2015 An In-Depth Comparison of Latency-Reversing Agent Combinations in Various
In Vitro and Ex Vivo HIV-1 Latency Models Identified Bryostatin-1+JQ1 and Ingenol-B+JQ1 to
Potently Reactivate Viral Gene Expression. PLoS Pathogens, 11(7), pp. e1005063. [PubMed:
26225566]
Author Manuscript
Davey RT et al., 1999 HIV-1 and T cell dynamics after interruption of highly active antiretroviral
therapy (HAART) in patients with a history of sustained viral suppression. Proceedings of the
National Academy of Sciences of the United States of America, 96(26), pp.15109–14. [PubMed:
10611346]
Day CL et al., 2006 PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and
disease progression. Nature, 443(7109), pp.350–354. [PubMed: 16921384]
Demoustier A et al., 2002 In patients on prolonged HAART, a significant pool of HIV infected CD4 T
cells are HIV-specific. AIDS, 16(13), pp.1749–1754. [PubMed: 12218385]
Deng K et al., 2015 Broad CTL response is required to clear latent HIV-1 due to dominance of escape
mutations. Nature, 517(7534), pp.381–5. [PubMed: 25561180]
Descours et al., 2017 CD32a is a marker of a CD4 T-cell HIV reservoir harbouring replication-
competent proviruses. Nature, 543(7646), pp. 564–567. [PubMed: 28297712]
DiNapoli SR, Hirsch VM & Brenchley JM, 2016 Macrophages in Progressive Human
Immunodeficiency Virus/Simian Immunodeficiency Virus Infections. Journal of virology, 90(17),
pp.7596–606. [PubMed: 27307568]
Author Manuscript
Dinoso JB et al., 2009 Treatment intensification does not reduce residual HIV-1 viremia in patients on
highly active antiretroviral therapy. Proceedings of the National Academy of Sciences, 106(23),
pp.9403–9408.
Doitsh G, et al., 2010 Abortive HIV infection mediates CD4 T cell depletion and inflammation in
human lymphoid tissue. Cell,143(5), pp.789–801. [PubMed: 21111238]
Dornadula G et al., 1999 Residual HIV-1 RNA in blood plasma of patients taking suppressive highly
active antiretroviral therapy. JAMA, 282(17), pp.1627–1632. [PubMed: 10553788]
Douek DC et al., 2002 HIV preferentially infects HIV-specific CD4+T cells. Nature, 417(6884), pp.
95–98. [PubMed: 11986671]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 29
Duh EJ et al., 1989 Tumor necrosis factor alpha activates human immunodeficiency virus type 1
through induction of nuclear factor binding to the NF-kappa B sites in the long terminal repeat.
Author Manuscript
Proceedings of the National Academy of Sciences of the United States of America, 86(15), pp.
5974–8. [PubMed: 2762307]
Elliott JH et al., 2014 Activation of HIV Transcription with Short-Course Vorinostat in HIV-Infected
Patients on Suppressive Antiretroviral Therapy. PLoS Pathogens, 10(10), pp.e1004473. [PubMed:
25393648]
Farber DL, Yudanin NA & Restifo NP, 2014 Human memory T cells: generation,
compartmentalization and homeostasis. Nature reviews. Immunology, 14(1), pp.24–35.
Fehniger TA et al., 2003 CD56bright natural killer cells are present in human lymph nodes and are
activated by T cell-derived IL-2: A potential new link between adaptive and innate immunity.
Blood, 101(8), pp.3052–3057. [PubMed: 12480696]
Ferlazzo G et al., 2004 The Abundant NK Cells in Human Secondary Lymphoid Tissues Require
Activation to Express Killer Cell Ig-Like Receptors and Become Cytolytic. The Journal of
Immunology, 172(3), pp.1455–1462. [PubMed: 14734722]
Feng S, and Holland EC, 1988 HIV-1 tat trans-activation requires the loop sequence within tar. Nature,
Author Manuscript
334(6178), pp. 165–7. [PubMed: 3386755]
Festenstein R et al., 2003 Modulation of heterochromatin protein 1 dynamics in primary Mammalian
cells. Science (New York, NY), 299(5607), pp.719–721.
Finzi D et al., 1997 Identification of a Reservoir for HIV-1 in Patients on Highly Active Antiretroviral
Therapy Identification of a Reservoir for HIV-1 in Patients on Highly Active Antiretroviral
Therapy. Science, 278(5341), pp.1295–1300. [PubMed: 9360927]
Finzi D et al., 1999 Latent infection of CD4+ T cells provides a mechanism for lifelong persistence of
HIV-1, even in patients on effective combination therapy. Nature Medicine, 5(5), pp.1–6.
Frenkel LM et al., 2003 Multiple viral genetic analyses detect low-level human immunodeficiency
virus type 1 replication during effective highly active antiretroviral therapy. Journal of virology,
77(10), pp.5721–30. [PubMed: 12719565]
Fujinaga K et al., 2004 Dynamics of Human Immunodeficiency Virus Transcription: P-TEFb
Phosphorylates RD and Dissociates Negative Effectors from the Transactivation Response
Element. Molecular and Cellular Biology, 24, pp.787–795. [PubMed: 14701750]
Author Manuscript
Fukazawa Y et al., 2015 B cell follicle sanctuary permits persistent productive simian
immunodeficiency virus infection in elite controllers. Nature Medicine, 21(2), pp.132–139.
Fukazawa Y et al., 2012 Lymph node T cell responses predict the efficacy of live attenuated SIV
vaccines. Nature Medicine, 18(11), pp.1673–1681.
Fulda S, 2015 Smac mimetics as IAP antagonists. Seminars in Cell and Developmental Biology, 39,
pp.132–138. [PubMed: 25550219]
Fromentin R, et al., 2016 CD4+T Cells Expressing PD-1, TIGIT and LAG-3 Contribute to HIV
Persistence during ART. Plos Pathogens, 12(7): e1005761. [PubMed: 27415008]
Gandhi RT et al., 2010 The effect of raltegravir intensification on low-level residual viremia in HIV-
infected patients on antiretroviral therapy: A randomized controlled trial. PLoS Medicine, 7(8),
pp.e1000321. [PubMed: 20711481]
Gandhi RT & Walker BD, 2002 Immunologic control of HIV-1. Annual review of medicine, 53, pp.
149–72.
Garcia-Vidal E et al., 2017 Evaluation of the innate immune modulator acitretin as a strategy to clear
the HIV reservoir. Antimicrobial Agents and Chemotherapy, 61(11), pp. e01368–17. [PubMed:
Author Manuscript
28874382]
Gartner S et al., 1986 The role of mononuclear phagocytes in HTLV-III/LAV infection. Science,
233(4760), pp.215–9. [PubMed: 3014648]
Gaudinski MR et al., 2018 Safety and pharmacokinetics of the Fc-modified HIV-1 human monoclonal
antibody VRC01LS: A Phase 1 open-label clinical trial in healthy adults. Plos medicine, 15(1):
e1002493. [PubMed: 29364886]
Gavegnano C et al., 2017 Novel mechanisms to inhibit HIV reservoir seeding using Jak inhibitors.
PLoS Pathogens, 13(12), pp.1–30.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 30
Gay CL et al., 2017 Clinical trial of the anti-PD-L1 antibody BMS-936559 in HIV-1 infected
participants on suppressive antiretroviral therapy. Journal of Infectious Diseases, 215(11), pp.
Author Manuscript
1725–1733. [PubMed: 28431010]
Gerritsen ME et al., 1997 CREB-binding protein/p300 are transcriptional coactivators of p65. Proc.
Natl. Acad. Sci, 94, pp.2927–2932. [PubMed: 9096323]
Ginhoux F & Guilliams M, 2016 Tissue-Resident Macrophage Ontogeny and Homeostasis. Immunity,
44(3), pp.439–449. [PubMed: 26982352]
Goldstone DC et al., 2011 HIV-1 restriction factor SAMHD1 is a deoxynucleoside triphosphate
triphosphohydrolase. Nature, 480(7377), pp.379–382. [PubMed: 22056990]
Goonetilleke N et al., 2009 The first T cell response to transmitted/founder virus contributes to the
control of acute viremia in HIV-1 infection. The Journal of Experimental Medicine, 206(6), pp.
1253–72. [PubMed: 19487423]
Gornalusse GG et al., 2015 Epigenetic mechanisms, T-cell activation, and CCR5 genetics interact to
regulate T-cell expression of CCR5, the major HIV-1 coreceptor. Proceedings of the National
Academy of Sciences, 112(34), pp.E4762–E4771.
Gutiérrez C et al., 2016 Bryostatin-1 for latent virus reactivation in HIV-infected patients on
Author Manuscript
antiretroviral therapy. AIDS (London, England), 30(9), pp.1385–92.
Guzzo C et al., 2017 Virion incorporation of integrin α4β7 facilitates HIV-1 infection and intestinal
homing. Science Immunology, 2(11), p.eaam7341. [PubMed: 28763793]
Halper-Stromberg A et al., 2014 Broadly neutralizing antibodies and viral inducers decrease rebound
from HIV-1 latent reservoirs in humanized mice. Cell, 158(5), pp.989–999. [PubMed: 25131989]
Hammarlund E et al., 2010 Antiviral immunity following smallpox virus infection: a case-control
study. Journal of virology, 84, pp.12754–60. [PubMed: 20926574]
Han Y et al., 2007 Experimental approaches to the study of HIV-1 latency. Nature Reviews
Microbiology, 5(2), pp. 95–106. [PubMed: 17224919]
Han Y et al., 2008 Orientation-Dependent Regulation of Integrated HIV-1 Expression by Host Gene
Transcriptional Readthrough. Cell Host & Microbe, 14(4), pp.134–46.
Han Y et al., 2004 Resting CD4+ T cells from human immunodeficiency virus type 1 (HIV-1)-infected
individuals carry integrated HIV-1 genomes within actively transcribed host genes. Journal of
virology, 78(12), pp.6122–33. [PubMed: 15163705]
Author Manuscript
Hansen SG et al., 2009 Effector memory T cell responses are associated with protection of rhesus
monkeys from mucosal simian immunodeficiency virus challenge. Nature Medicine, 15(3), pp.
293–299.
Hansen SG et al., 2011 Profound early control of highly pathogenic SIV by an effector memory T-cell
vaccine. Nature, 473(7348), pp. 523–7. [PubMed: 21562493]
Hansen SG et al., 2013a Immune clearance of highly pathogenic SIV infection. Nature, 502(7469), pp.
100–104. [PubMed: 24025770]
Hansen SG et al., 2013b Cytomegalovirus Vectors Violate CD8+ T Cell Epitope Recognition
Paradigms. Science, 340(6135), pp.1237874. [PubMed: 23704576]
Hansen SG et al., 2016 Broadly targeted CD8+ T cell responses restricted by major histocompatibility
complex E. Science, 351(6274), pp. 714–720. [PubMed: 26797147]
Hashimoto M et al., 2018 CD8 T Cell Exhaustion in Chronic Infection and Cancer: Opportunities for
Interventions. Annual Review of Medicine, 69(1), pp.301–318.
Henrich TJ et al., 2014 Antiretroviral-Free HIV-1 Remission and Viral Rebound After Allogeneic
Author Manuscript
Stem Cell Transplantation. Annals of Internal Medicine, 161(5), p.319. [PubMed: 25047577]
Henrich TJ et al., 2017 Human Immunodeficiency Virus Type 1 Persistence Following Systemic
Chemotherapy for Malignancy. The Journal of Infectious Diseases, 216(2), pp. 254–262.
[PubMed: 28838149]
Hermankova M et al., 2003 Analysis of human immunodeficiency virus type 1 gene expression in
latently infected resting CD4+ T lymphocytes in vivo. Journal of virology, 77(13), pp.7383–92.
[PubMed: 12805437]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 31
Hersperger AR et al., 2011 Qualitative features of the HIV-specific CD8+ T-cell response associated
with immunologic control. Current Opinion in HIV and AIDS, 6(3), pp.169–173. [PubMed:
Author Manuscript
21399496]
Hiener B et al., 2017 Identification of Genetically Intact HIV-1 Proviruses in Specific CD4 + T Cells
from Effectively Treated Participants. Cell Reports, 21, pp.813–822. [PubMed: 29045846]
Hill AL, et al., 2014 Predicting the outcomes of treatment to eradicate the latent reservoir for HIV-1.
PNAS, 111(37), pp.13475–13480. [PubMed: 25097264]
Hill AL et al., 2016 Real-Time Predictions of Reservoir Size and Rebound Time during Antiretroviral
Therapy Interruption Trials for HIV. PLoS Pathogens, 12(4), pp. e1005535. [PubMed: 27119536]
Ho DD et al., 1995 Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature,
373(6510), pp.123–126. [PubMed: 7816094]
Ho YC et al., 2013 Replication-competent noninduced proviruses in the latent reservoir increase
barrier to HIV-1 cure. Cell, 155(3), pp.540–551. [PubMed: 24243014]
Honeycutt JB et al., 2017 HIV persistence in tissue macrophages of humanized myeloid-only mice
during antiretroviral therapy. Nature Medicine, 23(5), pp. 638–643.
Horwitz JA et al., 2017 Non-neutralizing Antibodies Alter the Course of HIV-1 Infection In Vivo. Cell,
Author Manuscript
170(4), p.637–648. [PubMed: 28757252]
Hosmane NN et al., 2017 Proliferation of latently infected CD4 + T cells carrying replication-
competent HIV-1: Potential role in latent reservoir dynamics. The Journal of Experimental
Medicine, 214(4), pp.959–972. [PubMed: 28341641]
Hsia SC & Shi YB, 2002 Chromatin disruption and histone acetylation in regulation of the human
immunodeficiency virus type 1 long terminal repeat by thyroid hormone receptor. Mol Cell Biol,
22, pp.4043–4052. [PubMed: 12024018]
Hua S et al., 2017 Pegylated Interferon-α–Induced Natural Killer Cell Activation Is Associated With
Human Immunodeficiency Virus-1 DNA Decline in Antiretroviral Therapy–Treated HIV-1/
Hepatitis C Virus–Coinfected Patients. Clinical Infectious Diseases.
Huang SH et al., 2018 Latent HIV reservoirs exhibit inherent resistance to elimination by CD8+t cells.
Journal of Clinical Investigation, 128(2), pp.876–889. [PubMed: 29355843]
Huot N et al., 2017 Natural killer cells migrate into and control simian immunodeficiency virus
replication in lymph node follicles in African green monkeys. Nature Medicine, 23(11), pp.1277–
Author Manuscript
1286.
Hütter G et al., 2009 Long-Term Control of HIV by CCR5 Delta32/Delta32 Stem-Cell
Transplantation. New England Journal of Medicine, 360, pp.692–698. [PubMed: 19213682]
Igarashi T et al., 2003 Macrophage-Tropic Simian/Human Immunodeficiency Virus Chimeras Use
CXCR4, Not CCR5, for Infections of Rhesus Macaque Peripheral Blood Mononuclear Cells and
Alveolar Macrophages. J. Virol, 77(24), pp.13042–13052. [PubMed: 14645561]
Im SJ et al., 2016 Defining CD8+T cells that provide the proliferative burst after PD-1 therapy. Nature,
537(7620), pp.417–421. [PubMed: 27501248]
Imamichi H et al., 2016 Defective HIV-1 proviruses produce novel protein-coding RNA species in
HIV-infected patients on combination antiretroviral therapy. Proceedings of the National
Academy of Sciences, 113(31), pp.8783–8788.
Irvine DJ et al., 2002 Direct observation of ligand recognition by T cells. Nature, 419(6909), pp.845–
849. [PubMed: 12397360]
Iwai Y, Terawaki S & Honjo T, 2005 PD-1 blockade inhibits hematogenous spread of poorly
immunogenic tumor cells by enhanced recruitment of effector T cells. International Immunology,
Author Manuscript
17(2), pp.133–144. [PubMed: 15611321]
Jiang G & Dandekar S, 2015 Targeting NF-κB Signaling with Protein Kinase C Agonists As an
Emerging Strategy for Combating HIV Latency. AIDS Research and Human Retroviruses, 31(1),
pp.4–12. [PubMed: 25287643]
Jones RB et al., 2016 A Subset of Latency-Reversing Agents Expose HIV-Infected Resting CD4+T-
Cells to Recognition by Cytotoxic T-Lymphocytes. PLoS Pathogens, 12(4), pp.e1005545.
[PubMed: 27082643]
Jones RB et al., 2014 Histone deacetylase inhibitors impair the elimination of hiv-infected cells by
cytotoxic T-lymphocytes. PLoS Pathogens, 10(8), pp. e1004287. [PubMed: 25122219]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 32
Jones RB et al., 2008 Tim-3 expression defines a novel population of dysfunctional T cells with highly
elevated frequencies in progressive HIV-1 infection. The Journal of Experimental Medicine,
Author Manuscript
205(12), pp.2763–2779. [PubMed: 19001139]
Joosten SA, Sullivan LC & Ottenhoff THM, 2016 Characteristics of HLA-E Restricted T-Cell
Responses and Their Role in Infectious Diseases. J Immunol Res, 2016(2695396), pp. 1–11.
Jordan A, Defechereux P & Verdin E, 2001 The site of HIV-1 integration in the human genome
determines basal transcriptional activity and response to Tat transactivation. EMBO Journal,
20(7), pp.1726–1738. [PubMed: 11285236]
Josefsson L et al., 2013 The HIV-1 reservoir in eight patients on long-term suppressive antiretroviral
therapy is stable with few genetic changes over time. Proceedings of the National Academy of
Sciences of the United States of America, 110(51), pp.E4987–96. [PubMed: 24277811]
Kader M et al., 2009 α4+β7hiCD4+ memory T cells harbor most Th-17 cells and are preferentially
infected during acute SIV infection. Mucosal Immunology, 2(5), pp.439–449. [PubMed:
19571800]
Kahan SM, Wherry EJ & Zajac AJ, 2015 T cell exhaustion during persistent viral infections. Virology,
479–480, pp.180–193.
Author Manuscript
Kalams SA et al., 1999 Association between virus-specific cytotoxic T-lymphocyte and helper
responses in human immunodeficiency virus type 1 infection. Journal of virology, 73(8), pp.
6715–6720. [PubMed: 10400769]
Kamphorst AO et al., 2017 Proliferation of PD-1+ CD8 T cells in peripheral blood after PD-1–targeted
therapy in lung cancer patients. PNAS, 114(19), pp.4993–4998. [PubMed: 28446615]
Kandathil AJ, Sugawara S & Balagopal A, 2016 Are T cells the only HIV-1 reservoir. Retrovirology,
13(1), pp.1–10. [PubMed: 26728316]
Kao S-Y et al., 1987 Anti-termination of transcription within the long terminal repeat of HIV-1 by tat
gene product. Nature, 330(6147), pp.489–493. [PubMed: 2825027]
Karn J, 2011 The molecular biology of HIV latency: breaking and restoring the Tat-dependent
transcriptional circuit. Current Opinion in HIV and AIDS, 6, pp.4–11. [PubMed: 21242887]
Kauder SE et al., 2009 Epigenetic regulation of HIV-1 latency by cytosine methylation. PLoS
Pathogens, 5(6), pp. e1000495. [PubMed: 19557157]
Kaufmann GR et al., 2004 Long-term virological response to multiple sequential regimens of highly
Author Manuscript
active antiretroviral therapy for HIV infection. Antiviral Therapy, 9(2), pp.263–274. [PubMed:
15134189]
Kearney MF et al., 2014 Lack of Detectable HIV-1 Molecular Evolution during Suppressive
Antiretroviral Therapy. PLoS Pathogens, 10(3).
El Kharroubi A et al., 1998 Transcriptional activation of the integrated chromatin-associated human
immunodeficiency virus type 1 promoter. Molecular and cellular biology, 18(5), pp.2535–2544.
[PubMed: 9566873]
Kieffer TL et al., 2004 Genotypic Analysis of HIV‐1 Drug Resistance at the Limit of Detection: Virus
Production without Evolution in Treated Adults with Undetectable HIV Loads. The Journal of
Infectious Diseases, 189(8), pp.1452–1465. [PubMed: 15073683]
Kim Y, Anderson JL & Lewin SR, 2018 Getting the “Kill” into “Shock and Kill”: Strategies to
Eliminate Latent HIV. Cell Host Microbe, 23(1), pp. 14–26. [PubMed: 29324227]
Kiniry B et al., 2017 Predominance of Weakly Cytotoxic, T-betLow EomesNeg CD8+ T-cells in
Human Gastrointestinal Mucosa: Implications for HIV Infection. Mucosal Immunology, 10(4),
pp.1008–1020. [PubMed: 27827375]
Author Manuscript
Kinoshita S et al., 1998 Host control of HIV-1 parasitism in T cells by the nuclear factor of activated T
cells. Cell, 95(5), pp.595–604. [PubMed: 9845362]
Koizumi Y et al., 2017 Quantifying antiviral activity optimizes drug combinations against hepatitis C
virus infection. Proceedings of the National Academy of Sciences of the United States of
America, 114(8), pp. 1922–1927. [PubMed: 28174263]
Koup RA et al., 1994 Temporal association of cellular immune responses with the initial control of
viremia in primary human immunodeficiency virus type 1 syndrome. Journal of virology, 68(7),
pp.4650–5. [PubMed: 8207839]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 33
Kreitman RJ, 2006 Immunotoxins for targeted cancer therapy. The AAPS Journal, 8(3), pp.E532–
E551. [PubMed: 17025272]
Author Manuscript
Kulkosky J et al., 2002 Intensification and Stimulation Therapy for Human Immunodeficiency Virus
Type 1 Reservoirs in Infected Persons Receiving Virally Suppressive Highly Active
Antiretroviral Therapy. Journal of Infectious Diseases, 186(10), pp.1403–11. [PubMed:
12404155]
Kwaa AK et al., 2017 The effect of Ingenol-B on the suppressive capacity of elite suppressor HIV-
specific CD8+ T cells. PLOS ONE, 12(5), p.e0174516. [PubMed: 28467486]
Kwong PD et al., 2002 HIV-1 evades antibody-mediated neutralization through conformational
masking of receptor-binding sites. Nature, 420(6916), pp.678–682. [PubMed: 12478295]
Laguette N et al., 2011 SAMHD1 is the dendritic- and myeloid-cell-specific HIV-1 restriction factor
counteracted by Vpx. Nature, 474(7353), pp.654–657. [PubMed: 21613998]
Laird GM et al., 2015 Ex vivo analysis identifies effective HIV-1 latency-reversing drug combinations.
Journal of Clinical Investigation, 125(5), pp.1901–1912. [PubMed: 25822022]
Lambotte O et al., 2005 HIV Controllers: A Homogeneous Group of HIV-1--Infected Patients with
Spontaneous Control of Viral Replication. Clinical Infectious Diseases, 41, pp.1053–1056.
Author Manuscript
[PubMed: 16142675]
Larder B, Darby G & Richman D, 1989 HIV with reduced sensitivity to zidovudine (AZT) isolated
during prolonged therapy. Science, 243(4899), pp.1731–1734. [PubMed: 2467383]
Laskey SB& Siliciano RF, 2014 A mechanistic theory to explain the efficacy of antiretroviral therapy.
Nat Rev Microbiol. 12(11), pp:772–780. [PubMed: 25263222]
Lassen KG et al., 2006 Nuclear retention of multiply spliced HIV-1 RNA in resting CD4+T cells.
PLoS Pathogens, 2(7), pp.0650–0661.
Laughlin MA et al., 1993 Sodium Butyrate Treatment of Cells Latently Infected with HIV-1 Results in
the Expression of Unspliced Viral RNA. Virology, 196, pp.496–505. [PubMed: 8372431]
Lee GQ et al., 2017 Clonal expansion of genome-intact HIV-1 in functionally polarized Th1 CD4+ T
cells. The Journal of clinical investigation, 127(7), pp.2689–2696. [PubMed: 28628034]
Lehrman G et al., 2005 Depletion of latent HIV-1 infection in vivo: A proof-of-concept study. Lancet,
366(9485), pp.549–555. [PubMed: 16099290]
Lenardo MJ et al., 2002 Cytopathic Killing of Peripheral Blood CD4 + T Lymphocytes by Human
Author Manuscript
Immunodeficiency Virus Type 1 Appears Necrotic rather than Apoptotic and Does Not Require
env. Journal of Virology, 76(10), pp.5082–5093. [PubMed: 11967324]
Lenasi T, Contreras X & Peterlin BM, 2008 Transcriptional Interference Antagonizes Proviral Gene
Expression to Promote HIV Latency. Cell Host and Microbe, 4(2), pp.123–133. [PubMed:
18692772]
Lerner P et al., 2011 The Gut Mucosal Viral Reservoir in HIV-Infected Patients Is Not the Major
Source of Rebound Plasma Viremia following Interruption of Highly Active Antiretroviral
Therapy. Journal of Virology, 85(10), pp.4772–4782. [PubMed: 21345945]
Leth S et al., 2016 Combined effect of Vacc-4×, recombinant human granulocyte macrophage colony-
stimulating factor vaccination, and romidepsin on the HIV-1 reservoir (REDUC): a single-arm,
phase 1B/2A trial. The Lancet HIV, 3(10), pp.e463–e472. [PubMed: 27658863]
Li P et al., 2016 Stimulating the RIG-I pathway to kill cells in the latent HIV reservoir following viral
reactivation. Nature Medicine, 22(7), pp.807–811.
Lindqvist M et al., 2012 Expansion of HIV-specific T follicular helper cells in chronic HIV infection.
The Journal of clinical investigation, 122(9), pp.3271–80. [PubMed: 22922259]
Author Manuscript
van Lint C et al., 1996 Transcriptional activation and chromatin remodeling of the HIV-1 promoter in
response to histone acetylation. The EMBO journal, 15, pp.1112–20. [PubMed: 8605881]
van Lint C, Bouchat S & Marcello A, 2013 HIV-1 transcription and latency: an update. Retrovirology,
10, p.67. [PubMed: 23803414]
Lopez-Vergès S et al., 2011 Expansion of a unique CD57+NKG2Chi natural killer cell subset during
acute human cytomegalovirus infection. PNAS, 108(36), pp.14725–14732. [PubMed: 21825173]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 34
Lorenzi JCC et al., 2016 Paired quantitative and qualitative assessment of the replication-competent
HIV-1 reservoir and comparison with integrated proviral DNA. PNAS, 113(49), pp.E7908–
Author Manuscript
E7916. [PubMed: 27872306]
Lorenzo-Redondo R et al., 2016 Persistent HIV-1 replication maintains the tissue reservoir during
therapy. Nature, 530(7588), pp.51–56. [PubMed: 26814962]
Louveau A et al., 2015 Structural and functional features of central nervous system lymphatic vessels.
Nature, 523(7560), pp.337–341. [PubMed: 26030524]
Lu C et al., 2016 Enhanced clearance of HIV-1-infected cells by broadly neutralizing antibodies
against HIV-1 in vivo. Science, 352(6288), pp.1001–1005. [PubMed: 27199430]
Lu P et al., 2017 BET inhibitors RVX-208 and PFI-1 reactivate HIV-1 from latency. Scientific Reports,
7(1), pp.1–12. [PubMed: 28127051]
Lucas A et al., 2010 Targeting the PI3K/AKT cell survival pathway to induce cell death of HIV-1
infected macrophages with alkylphospholipid compounds. PLoS ONE, 5(9), pp.e13121.
[PubMed: 20927348]
Luzuriaga K et al., 2015 Viremic Relapse after HIV-1 Remission in a Perinatally Infected Child. New
England Journal of Medicine, 372(8), pp.786–788. [PubMed: 25693029]
Author Manuscript
Lynch RM et al., 2015 Virologic effects of broadly neutralizing antibody VRC01 administration during
chronic HIV-1 infection. Science Translational Medicine, 7(319).
Maartens G et al., 2014 Seminar HIV infection: epidemiology, pathogenesis, treatment, and
prevention. The Lancet, 384(9939), pp.258–271.
Maldarelli F et al., 2007 ART suppresses plasma HIV-1 RNA to a stable set point predicted by
pretherapy viremia. PLoS Pathogens, 3(4), pp.484–488.
Maldarelli F et al., 2014 Specific HIV integration sites are linked to clonal expansion and persistence
of infected cells. Science, 345(6193), pp.179–183. [PubMed: 24968937]
Mancebo HSY et al., 1997 P-TEFb kinase is required for HIV Tat transcriptional activation in vivo and
in vitro. Genes and Development, 11(20), pp.2633–2644. [PubMed: 9334326]
Marban C et al., 2016 Targeting the brain reservoirs: Toward an HIV cure. Frontiers in Immunology,
7(397), pp. 1–13. [PubMed: 26834743]
Martín-Fontecha A et al., 2004 Induced recruitment of NK cells to lymph nodes provides IFN-gamma
for T(H)1 priming. Nature immunology, 5(12), pp.1260–5. [PubMed: 15531883]
Author Manuscript
Martin AR et al., 2017 Rapamycin-mediated mTOR inhibition uncouples HIV-1 latency reversal from
cytokine-associated toxicity. Journal of Clinical Investigation, 127(2), pp.651–656. [PubMed:
28094770]
McGary CS et al., 2017 CTLA-4+PD-1- Memory CD4+ T Cells Critically Contribute to Viral
Persistence in Antiretroviral Therapy-Suppressed, SIV-Infected Rhesus Macaques. Immunity,
47(4), pp.776–788. [PubMed: 29045906]
McMahon D et al., 2010 Short-course raltegravir intensification does not reduce persistent low-level
viremia in patients with HIV-1 suppression during receipt of combination antiretroviral therapy.
Clinical Infectious Diseases, 50(6), pp.912–9. [PubMed: 20156060]
Meehan AM et al., 2009 LEDGF/p75 Proteins with Alternative Chromatin Tethers Are Functional
HIV-1 Cofactors Luban J, ed. PLoS Pathogens, 5, p.e1000522. [PubMed: 19609362]
Mellors JW et al., 1996 Prognosis in HIV-1 infection predicted by the quantity of virus in plasma.
Science, 272(5264), pp. 1167–1170 [PubMed: 8638160]
Migueles SA & Connors M, 2015 Success and failure of the cellular immune response against HIV-1.
Author Manuscript
Nature Immunology, 16(6), pp.563–570. [PubMed: 25988888]
Mikell I et al., 2011 Characteristics of the earliest cross-neutralizing antibody response to HIV-1. PLoS
Pathogens, 7(1), pp.e1001251. [PubMed: 21249232]
Molitor JA et al., 1990 NF-kappa B: a family of inducible and differentially expressed enhancer-
binding proteins in human T cells. Proceedings of the National Academy of Sciences, 87(24).
Mujib S, Liu J, et al., 2017 Comprehensive Cross-Clade Characterization of Antibody-Mediated
Recognition, Complement-Mediated Lysis, and Cell-Mediated Cytotoxicity of HIV-1 Envelope-
Specific Antibodies toward Eradication of the HIV-1 Reservoir. Journal of Virology, 91(16),
pp.e00634–17. [PubMed: 28592534]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 35
Mujib S, Saiyed A, et al., 2017 Pharmacologic HIV-1 Nef blockade promotes CD8 T cell – mediated
elimination of latently HIV-1 – infected cells in vitro. JCI Insight, 2(17), pp.1–18.
Author Manuscript
Nabel and Baltimore, 1987 An inducible transcription factor activates expression of human
immunodeficiency virus in T cells. Nature, 326(6114), pp.711–713. [PubMed: 3031512]
Ne E, Palstra RJ & Mahmoudi T, 2018 Transcription: Insights From the HIV-1 Promoter 1st ed.,
Elsevier Inc.
Nettles RE et al., 2005 Intermittent HIV-1 viremia (blips) and drug resistance in patients receiving
HAART. Journal of the American Medical Association, 293(7), pp.817–829. [PubMed:
15713771]
Neumann S et al., 2015 How do viruses control mitochondria-mediated apoptosis? Virus Research,
209, pp.45–55. [PubMed: 25736565]
O’Connell KA et al., 2009 Role of natural killer cells in a cohort of elite suppressors: low frequency of
the protective KIR3DS1 allele and limited inhibition of human immunodeficiency virus type 1
replication in vitro. Journal of virology, 83, pp.5028–34. [PubMed: 19211742]
Olesen R et al., 2015 Innate Immune Activity Correlates with CD4 T Cell-Associated HIV-1 DNA
Decline during Latency-Reversing Treatment with Panobinostat. Journal of Virology, 89(20), pp.
Author Manuscript
10176–10189. [PubMed: 26223643]
Pankrac J, Klein K & Mann JFS, 2017 Eradication of HIV-1 latent reservoirs through therapeutic
vaccination. AIDS Research and Therapy, 14(1), pp. 45. [PubMed: 28893280]
Parada CA & Roeder RG, 1996 Enhanced processivity of RNA polymerase II triggered by Tat-induced
phosphorylation of its carboxy-terminal domain. Nature, 384, pp.375–378. [PubMed: 8934526]
Peng H & Tian Z, 2017 Natural killer cell memory: Progress and implications. Frontiers in
Immunology, 8(1143), pp.1–10. [PubMed: 28149297]
Peng J et al., 1998 Identification of multiple cyclin subunits of human P-TEFb. Genes and
Development, 12(5), pp.755–762. [PubMed: 9499409]
Perelson AS et al., 1997 Decay characteristics of HIV-1-infected compartments during combination
therapy. Nature, 387(6629), pp.188–191. [PubMed: 9144290]
Perreau M et al., 2013 Follicular helper T cells serve as the major CD4 T cell compartment for HIV-1
infection, replication, and production. The Journal of Experimental Medicine, 210(1), pp.143–
156. [PubMed: 23254284]
Author Manuscript
Persaud D et al., 2013 Absence of Detectable HIV-1 Viremia after Treatment Cessation in an Infant.
New England Journal of Medicine, 369(19), pp.1828–1835. [PubMed: 24152233]
Peterlin BM & Price DH, 2006 Controlling the elongation phase of transcription with P-TEFb.
Molecular cell, 23(3), pp.297–305. [PubMed: 16885020]
Petrovas C et al., 2006 PD-1 is a regulator of virus-specific CD8+ T cell survival in HIV infection. The
Journal of Experimental Medicine, 203(10), pp.2281–92. [PubMed: 16954372]
Petrovas C et al., 2012 CD4 T follicular helper cell dynamics during SIV infection. The Journal of
Clinical Investigation, 122(9), pp.3281–3294. [PubMed: 22922258]
Petrovas C et al., 2017 HIV Follicular CD8 T cells accumulate in HIV infection and can kill infected
cells in vitro via bispecific antibodies. Science Translational Medicine, 9(373), pp.1–14.
Piatak M et al., 1993 High levels of HIV-1 in plasma during all stages of infection determined by
competitive PCR. Science, 259(5102), pp.1749–1754. [PubMed: 8096089]
Pierson T et al., 2000 Characterization of chemokine receptor utilization of viruses in the latent
reservoir for human immunodeficiency virus type 1. Journal of virology, 74(17), pp.7824–33.
Author Manuscript
[PubMed: 10933689]
Pitcher CJ et al., 1999 HIV-1-specific CD4+ T cells are detectable in most individuals with active
HIV-1 infection, but decline with prolonged vital suppression. Nature Medicine, 5(5), pp.518–
525.
Pollack RA et al., 2017 Defective HIV-1 Proviruses Are Expressed and Can Be Recognized by
Cytotoxic T Lymphocytes, which Shape the Proviral Landscape. Cell Host and Microbe, 21(4), p.
494–506. [PubMed: 28407485]
Poon B et al., 1998 Cell cycle arrest by Vpr in HIV-1 virions and insensitivity to antiretroviral agents.
Science, 281(5374), pp.266–269. [PubMed: 9657723]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 36
Price DA et al., 1997 Positive selection of HIV-1 cytotoxic T lymphocyte escape variants during
primary infection. Proceedings of the National Academy of Sciences, 94(5), pp. 1890–5.
Author Manuscript
Prins JM et al., 1999 Immuno-activation with anti-CD3 and recombinant human IL-2 in HIV-1-
infected patients on potent antiretroviral therapy. AIDS (London, England), 13(17), pp.2405–10.
Raha T, Cheng SWG & Green MR, 2005 HIV-1 Tat stimulates transcription complex assembly
through recruitment of TBP in the absence of TAFs. PLoS Biology, 3(2), pp.e44. [PubMed:
15719058]
Rainho JN et al., 2015 Nef Is Dispensable for Resistance of Simian Immunodeficiency Virus-Infected
Macrophages to CD8 + T Cell Killing. Journal of Virology, 89(20), pp.10625–10636. [PubMed:
26269172]
Ramsuran V et al., 2018 Elevated HLA-A expression impairs HIV control through inhibition of
NKG2A-expressing cells. Science, 359(6371), pp.86–90. [PubMed: 29302013]
Rasmussen TA et al., 2014 Panobinostat, a histone deacetylase inhibitor, for latent-virus reactivation in
HIV-infected patients on suppressive antiretroviral therapy: a phase 1/2, single group, clinical
trial. The Lancet HIV, 1(1), pp.e13–21. [PubMed: 26423811]
Reeves RK et al., 2015 Antigen-specific NK cell memory in rhesus macaques. Nature immunology,
Author Manuscript
16(9), pp.927–32. [PubMed: 26193080]
Rerks-Ngarm S et al., 2009 Vaccination with ALVAC and AIDSVAX to Prevent HIV-1 Infection in
Thailand. New England Journal of Medicine, 361(23), pp.2209–2220. [PubMed: 19843557]
Reuter MA et al., 2017 HIV-Specific CD8+T Cells Exhibit Reduced and Differentially Regulated
Cytolytic Activity in Lymphoid Tissue. Cell Reports, 21(12), pp.3458–3470. [PubMed:
29262326]
Rice AP, 2017 The HIV-1 Tat protein: mechanism of action and target for HIV-1 cure strategies.
Current pharmaceutical design, 23, pp.1–5. [PubMed: 28292246]
Richman DD et al., 2009 The challenge of finding a cure for HIV infection. Science, 323(5919), pp.
1304–1307. [PubMed: 19265012]
Rosenbloom DIS et al., 2017 Re-evaluating evolution in the HIV reservoir. Nature, 551(530), pp.51–
56. [PubMed: 29094699]
Roshal M et al., 2003 Activation of the ATR-mediated DNA damage response by the HIV-1 viral
protein R. Journal of Biological Chemistry, 278(28), pp.25879–25886. [PubMed: 12738771]
Author Manuscript
Rothenberger MK et al., 2015 Large number of rebounding/founder HIV variants emerge from
multifocal infection in lymphatic tissues after treatment interruption. PNAS, 112(10), pp.E1126–
E1134. [PubMed: 25713386]
Russell RA, et al., 2017 Astrocytes Resist HIV-1 Fusion but Engulf Infected Macrophage Material.
Cell Reports, 18(6), pp.1473–1483. [PubMed: 28178524]
Sakai K, Dimas J & Lenardo MJ, 2006 The Vif and Vpr accessory proteins independently cause
HIV-1-induced T cell cytopathicity and cell cycle arrest. PNAS, 103(9), pp.3369–3374.
[PubMed: 16492778]
Saleh S, et al., 2007 CCR7 ligands CCL19 and CCL21 increase permissiveness of resting memory
CD4+ T cells to HIV-1 infection: a novel model of HIV-1 latency. Blood, 110(13):4161–4.
[PubMed: 17881634]
Sather DN et al., 2009 Factors associated with the development of cross-reactive neutralizing
antibodies during human immunodeficiency virus type 1 infection. Journal of virology, 83(2), pp.
757–69. [PubMed: 18987148]
Scheid JF et al., 2016 HIV-1 antibody 3BNC117 suppresses viral rebound in humans during treatment
Author Manuscript
interruption. Nature, 535(7613), pp.556–560. [PubMed: 27338952]
Schmitz JE et al., 1999 Control of viremia in simian immunodeficiency virus infection by CD8+
lymphocytes. Science, 283, pp.857–860. [PubMed: 9933172]
Schoofs T et al., 2016 HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune
responses against HIV-1. Science, 352(6288), pp.997–1001. [PubMed: 27199429]
Schröder ARW et al., 2002 HIV-1 integration in the human genome favors active genes and local
hotspots. Cell, 110(4), pp.521–529. [PubMed: 12202041]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 37
Sedaghat AR et al., 2007 Limits on replenishment of the resting CD4+T cell reservoir for HIV in
patients on HAART. PLoS Pathogens, 3(8), pp.1165–1174.
Author Manuscript
Shan L, et al., 2011 Influence of host gene transcription level and orientation on HIV-1 latency in a
primary-cell model. Journal of Virology, 85(11), pp. 5384–93. [PubMed: 21430059]
Shan L et al., 2012 Stimulation of HIV-1-Specific Cytolytic T Lymphocytes Facilitates Elimination of
Latent Viral Reservoir after Virus Reactivation. Immunity, 36(3), pp.491–501. [PubMed:
22406268]
Shan L et al., 2017 Transcriptional Reprogramming during Effector-to-Memory Transition Renders
CD4+T Cells Permissive for Latent HIV-1 Infection. Immunity, 47(4), p.766–775.e3. [PubMed:
29045905]
Shasha D & Walker BD, 2013 Lessons to be Learned from Natural Control of HIV – Future
Directions, Therapeutic, and Preventive Implications. Frontiers in Immunology, 4(162), pp. 1–8.
[PubMed: 23355837]
Shedlock DJ et al., 2008 HIV-1 viral genes and mitochondrial apoptosis. Apoptosis, 13(9), pp.1088–
1099. [PubMed: 18622704]
Shedlock DJ, Silvestri G & Weiner DB, 2009 Monkeying around with HIV vaccines: Using rhesus
Author Manuscript
macaques to define “gatekeepers” for clinical trials. Nature Reviews Immunology, 9(10), pp.717–
728.
Siekevitz M et al., 1987 Activation of the HIV-1 LTR by T cell mitogens and the trans-activator protein
of HTLV-I. Science (New York, N.Y.), 238(4833), pp.1575–8.
Siliciano JD et al., 2003 Long-term follow-up studies confirm the stability of the latent reservoir for
HIV-1 in resting CD4+ T cells. Nature medicine, 9(6), pp.727–728.
Siliciano JD et al., 2007 Stability of the Latent Reservoir for HIV‐1 in Patients Receiving Valproic
Acid. The Journal of Infectious Diseases, 195(6), pp.833–836. [PubMed: 17299713]
Siliciano RF & Greene WC, 2011 HIV Latency. Cold Spring Harbor Perspectives in Medicine, pp.1–
19.
Simonetti FR et al., 2016 Clonally expanded CD4 + T cells can produce infectious HIV-1 in vivo.
Proceedings of the National Academy of Sciences, 113(7), pp.1883–1888.
Slingluff CL, 2011 The present and future of peptide vaccines for cancer: single or multiple, long or
short, alone or in combination? Cancer J, 17(5), pp.343–50. [PubMed: 21952285]
Author Manuscript
Sloan DD et al., 2015 Targeting HIV Reservoir in Infected CD4 T Cells by Dual-Affinity Re-targeting
Molecules (DARTs) that Bind HIV Envelope and Recruit Cytotoxic T Cells. PLoS Pathogens,
11(11).
Sodroski J et al., 1985 Trans-acting transcriptional regulation of human T-cell leukemia virus type III
long terminal repeat. Science, 227(4683), pp.171–3. [PubMed: 2981427]
Søgaard OS et al., 2015 The Depsipeptide Romidepsin Reverses HIV-1 Latency In Vivo. PLoS
Pathogens, 11(9), pp.1–22.
Spivak AM et al., 2016 Janus kinase inhibition suppresses PKC-induced cytokine release without
affecting HIV-1 latency reversal ex vivo. Retrovirology, 13(1), pp. 88. [PubMed: 27998278]
Spivak AM & Planelles V, 2018 Novel Latency Reversal Agents for HIV-1 Cure. Annual Review of
Medicine, 69, pp.421–436.
Stewart SA et al., 2000 Human immunodeficiency virus type 1 vpr induces apoptosis through caspase
activation. Journal of virology, 74(7), pp.3105–3111. [PubMed: 10708425]
Strain MC et al., 2003 Heterogeneous clearance rates of long-lived lymphocytes infected with HIV:
Author Manuscript
Intrinsic stability predicts lifelong persistence. PNAS, 100(8), pp.4819–24. [PubMed: 12684537]
Streeck H et al., 2008 Antigen load and viral sequence diversification determine the functional profile
of HIV-1-specific CD8+ T cells. PLoS Medicine, 5(5), pp.0790–0803.
Sung JA et al., 2015a Expanded cytotoxic T-cell lymphocytes target the latent HIV reservoir. In Journal
of Infectious Diseases. pp. 258–263.
Sung JA et al., 2015b Dual-Affinity Re-Targeting proteins direct T cell-mediated cytolysis of latently
HIV-infected cells. Journal of Clinical Investigation, 125(11), pp.4077–4090. [PubMed:
26413868]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 38
Sung JA et al., 2017 Vorinostat Renders the Replication-Competent Latent Reservoir of Human
Immunodeficiency Virus (HIV) Vulnerable to Clearance by CD8 T Cells. EBioMedicine, 23, pp.
Author Manuscript
52–58. [PubMed: 28803740]
Takaki A et al., 2000 Cellular immune responses persist and humoral responses decrease twodecades
after recovery from a single-source outbreak of hepatitis C. Nature Medicine, 6, pp.578–582.
Tamaru H, 2010 Confining euchromatin/heterochromatin territory: jumonji crosses the line. Genes &
development, 24, pp.1465–78. [PubMed: 20634313]
Tapia G et al., 2017 Sequential Vacc-4× and romidepsin during combination antiretroviral therapy
(cART): Immune responses to Vacc-4× regions on p24 and changes in HIV reservoirs. Journal of
Infection, 75(6), pp.555–571. [PubMed: 28917661]
Thananchai H et al., 2007 Cutting Edge: Allele-Specific and Peptide-Dependent Interactions between
KIR3DL1 and HLA-A and HLA-B. The Journal of Immunology, 178(1), pp.33–37. [PubMed:
17182537]
Thompson KA et al., 2011 Brain cell reservoirs of latent virus in presymptomatic HIV-infected
individuals. American Journal of Pathology, 179(4), pp.1623–1629. [PubMed: 21871429]
Tobin NH et al., 2005 Evidence that Low-Level Viremias during Effective Highly Active Antiretroviral
Author Manuscript
Therapy Result from Two Processes: Expression of Archival Virus and Replication of Virus.
Journal of Virology, 79(15), pp.9625–9634. [PubMed: 16014925]
Trautmann L et al., 2006 Upregulation of PD-1 expression on HIV-specific CD8+T cells leads to
reversible immune dysfunction. Nature Medicine, 12(10), pp.1198–1202.
Tsai A et al., 2017 Toll-Like Receptor 7 Agonist GS-9620 Induces HIV Expression and HIV-Specific
Immunity in Cells from HIV-Infected Individuals on Suppressive Antiretroviral Therapy. Journal
of Virology, 91(8), pp.e02166–16. [PubMed: 28179531]
Veazey RS, 1998 Gastrointestinal Tract as a Major Site of CD4+ T Cell Depletion and Viral
Replication in SIV Infection. Science, 280(5362), pp.427–431. [PubMed: 9545219]
Verdin E et al., 1993 Chromatin disruption in the promoter of human immunodeficiency virus type 1
during transcriptional activation. The EMBO journal, 12, pp.3249–59. [PubMed: 8344262]
Vojnov L et al., 2012 The Majority of Freshly Sorted Simian Immunodeficiency Virus (SIV)-Specific
CD8 + T Cells Cannot Suppress Viral Replication in SIV-Infected Macrophages. Journal of
Virology, 86(8), pp.4682–4687. [PubMed: 22318140]
Author Manuscript
Wagner TA et al., 2014 Proliferation of cells with HIV integrated into cancer genes contributes to
persistent infection. Science, 345(6196), pp.570–573. [PubMed: 25011556]
Walker-Sperling VE et al., 2016 The Effect of Latency Reversal Agents on Primary CD8+ T Cells:
Implications for Shock and Kill Strategies for Human Immunodeficiency Virus Eradication.
EBioMedicine, 8, pp.217–229. [PubMed: 27428432]
Walker B & McMichael A, 2012 The T-Cell Response to HIV. Cold Spring Harb Perspect Med,
2(a007054), pp.1–20.
Walker BD et al., 1987 HIV-specific cytotoxic T lymphocytes in seropositive individuals. Nature,
328(6128), pp.345–8. [PubMed: 3496541]
Wang Z et al., 2018 Expanded cellular clones carrying replication- competent HIV-1 persist, wax, and
wane. Proc. Natl. Acad. Sci, 15(11).
Wei P et al., 1998 A novel CDK9-associated C-type cyclin interacts directly with HIV-1 Tat and
mediates its high-affinity, loop-specific binding to TAR RNA. Cell, 92(4), pp.451–462. [PubMed:
9491887]
Wei X et al., 2002 Emergence of resistant human immunodeficiency virus type 1 in patients receiving
Author Manuscript
fusion inhibitor (T-20) monotherapy. Antimicrobial Agents and Chemotherapy, 46(6), pp.1896–
905. [PubMed: 12019106]
Wei X et al., 1995 Viral dynamics in human immunodeficiency virus type 1 infection. Nature,
373(6510), pp.117–122. [PubMed: 7529365]
Weinberger LS & Burnett JC, 2005 Stochastic Gene Expression in a Lentiviral Positive-Feedback
Loop: HIV-1 Tat Fluctuations Drive Phenotypic Diversity. Cell, 122, pp.169–182. [PubMed:
16051143]
Wherry EJ, et al., 2007 Molecular signature of CD8+T cell exhaustion during chronic viral infection.
Immunity, 27(4), pp. 670–84. [PubMed: 17950003]
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 39
Wherry EJ & Kurachi M, 2015 Molecular and cellular insights into T cell exhaustion. Nature Reviews
Immunology, 15(8), pp.486–499.
Author Manuscript
Whitney JB et al., 2014 Rapid seeding of the viral reservoir prior to SIV viraemia in rhesus monkeys.
Nature, 512, pp.74–77. [PubMed: 25042999]
Williams SA et al., 2006 NF-κB p50 promotes HIV latency through HDAC recruitment and repression
of transcriptional initiation. EMBO Journal, 25(1), pp.139–149. [PubMed: 16319923]
Wilson CC et al., 2017 Development of a DNA Vaccine Designed to Induce Cytotoxic T Lymphocyte
Responses to Multiple Conserved Epitopes in HIV-1.
Wong JK et al., 1997 Recovery of replication-competent HIV despite prolonged suppression of plasma
viremia. Science, 278(5341), pp.1291–1295. [PubMed: 9360926]
Xu L et al., 2017 Trispecific broadly neutralizing HIV antibodies mediate potent SHIV protection in
macaques. Science, 358(6359), pp.85–90. [PubMed: 28931639]
Yang H-C et al., 2009 Small-molecule screening using a human primary cell model of HIV latency
identifies compounds that reverse latency without cellular activation. The Journal of clinical
investigation, 119(11), pp.3473–86. [PubMed: 19805909]
Yukl SA et al., 2014 A comparison of methods for measuring rectal HIV levels suggests that HIV
Author Manuscript
DNA resides in cells other than CD4+ T cells, including myeloid cells. AIDS (London, England),
28, pp.439–42.
Zajac AJ et al., 1998 Viral Immune Evasion Due to Persistence of Activated T Cells Without Effector
Function. The Journal of Experimental Medicine, 188(12), pp.2205–2213. [PubMed: 9858507]
Zalar A et al., 2010 Macrophage HIV-1 infection in duodenal tissue of patients on long term HAART.
Antiviral Research, 87(2), pp.269–271. [PubMed: 20471997]
Zhu Y et al., 1997 Transcription elongation factor P-TEFb is required for HIV-1 Tat transactivation in
vitro. Genes and Development, 11(20), pp.2622–2632. [PubMed: 9334325]
Van Zyl GU et al., 2017 No evidence of HIV replication in children on antiretroviral therapy. Journal
of Clinical Investigation. pp. 3827–3834. [PubMed: 28891813]
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 40
Author Manuscript
Author Manuscript
Author Manuscript
Figure 1.
Viral dynamics in the presence of cART and curative interventions. (Top) Plasma HIV-1
RNA levels in typical patient. Clinical assays detect HIV-1 virions in the plasma through
measurement of genomic HIV-1 RNA by quantitative RT-PCR. Each virion has two copies
of the viral genome. Viremia increases exponentially after exposure, peaking at around two
weeks post infection. Levels of plasma virus then fall, coincident with the development of a
CTL response, to a steady state level (the set point). Viral replication continues through the
course of untreated HIV-1 infection, driving CD4+ T cell depletion. cART produces a rapid
biphasic decay in viremia to below the limit of detection of clinical assays (50 copies of
HIV-1 RNA/ml of plasma), reflecting the short half-lives of two major populations of
Author Manuscript
productively infected cells. However, residual viremia of ~1 copy/ml persists. Treatment
intensification by addition of a fourth antiretroviral drug does not reduce residual viremia
indicating that it is not due to ongoing cycles of replication but rather release of virus from
long-lived latently infected cells that become activated. Nevertheless, with good adherence,
infected individuals can expect continued suppression of viral replication and a near normal
life span. Upon treatment interruption, viremia rebound rapidly, becoming clinically
detectable within weeks of interruption and rising exponentially to the previous set point.
(Middle) Effects of a hypothetical cure strategy in involving LRAs. LRAs may induce
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 41
transient increases in plasma HIV-1 RNA as a result of the induction of viral gene
Author Manuscript
expression from latently infected cells. If the virus producing cells die from viral cytopathic
effects or are eliminated by immune mechanisms, then the reservoir will be reduced. This
will be reflected in a reduction in the level of residual viremia and a delay in rebound
following cART interruption, the length of which is related to the degree of reservoir
reduction (Hill et al. 2014). A sterilizing cure requires complete reservoir elimination.
(Bottom) Hypothetical vaccine strategies that enhance HIV-1-specific immunity to a degree
that allows long-term control of HIV-1 replication would convert HIV+ individuals with
progressive disease into EC and produce a functional cure.
Author Manuscript
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 42
Author Manuscript
Author Manuscript
Author Manuscript
Figure 2.
Proposed mechanism for the establishment of latent infection in resting CD4+ T cells. (A)
Fate of resting CD4+ T cells following antigen (Ag) driven activation (horizontal axis) and
Author Manuscript
following HIV-1 infection at times after activation (vertical axis). (B) Permissiveness of
CD4+ T cells to different steps in the HIV-1 life cycle as a function of time after T cell
activation. Resting CD4+ T cells are relatively resistant to HIV-1 infection due to low
expression of the CCR5 coreceptor and reduced levels of dNTPs required for DNA synthesis
during reverse transcription. Following activation, upregulation of the CCR5 allows viral
entry. Levels of dNTPs increase allowing reverse transcription, and key host transcription
factors translocate to the nucleus allowing viral gene expression and productive infection.
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 43
Activated CD4+ T in a state of productive infection die rapidly. At 6–9 days after activation,
Author Manuscript
CCR5 levels are high and dNTP levels are adequate for reverse transcription. However, viral
gene expression is minimal and transient due to falling levels of activation dependent host
transcription factors. Thus infection of cells during the effector to memory transition can
result in latent infection. (C) Yield of latently infected cells following infection at different
times after T cell activation. Model is based on experiments described in Shan et al., 2017.
Author Manuscript
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 44
Author Manuscript
Author Manuscript
Author Manuscript
Figure 3.
Author Manuscript
Challenges for the “kill” phase of HIV-1 cure strategies. Although HIV-1 induces a strong
CTL response, effective killing of latently infected cells following latency reversal requires
overcoming several challenges. (A) Ideal scenario in which a resting CD4+ T cell with an
integrated provirus (black rectangle) is induced by an LRA to produce viral RNA and
protein, leading to presentation of HIV-1 epitopes (black dot) which can be recognized by
HIV-1-specific CTL after they have been activated by HIV-1 antigen (Ag) or a vaccine
presenting the relevant epitope. (B) Escape mutations in dominant CTL epitopes prevent
Immunity. Author manuscript; available in PMC 2018 October 22.
Sengupta and Siliciano Page 45
targeting of induced cells. (C) Certain LRAs inhibit CTL function. (D) HIV-1-specific CTLs
Author Manuscript
have an exhausted phenotype marked by expression of PC-1 (red). Exhaustion is not fully
reversed by ART, and blockade of inhibitory receptors may be required to re-establish
functionality. (E) Induction of cells carrying defective proviruses may lead to the generation
of target cells that present epitopes, thereby interfering with the lysis of cells carrying intact
proviruses. (F) Some infected cells may reside in tissue sites for which there is limited
access by CTL. See text for details and references.
Author Manuscript
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2018 October 22.
You might also like
- Wiring Diagram Elevator: 123/INDSBY-ELC/1014Document22 pagesWiring Diagram Elevator: 123/INDSBY-ELC/1014Gogik Anto85% (13)
- Editing Coding and Tabulation of Data-Marketing ResearchDocument16 pagesEditing Coding and Tabulation of Data-Marketing ResearchArivanandan Get Going100% (1)
- Eradication of Human Immunodeficiency Virus Type-1 (HIV-1) - Infected CellsDocument13 pagesEradication of Human Immunodeficiency Virus Type-1 (HIV-1) - Infected CellsDouglas SouzaNo ratings yet
- Viruses 15 00107Document30 pagesViruses 15 00107Trần T. MơNo ratings yet
- Clamidia y VihDocument17 pagesClamidia y VihC JNo ratings yet
- AIDS Word OkokookkDocument6 pagesAIDS Word OkokookkAlberto PiasentierNo ratings yet
- Viruses 07 01578 PDFDocument21 pagesViruses 07 01578 PDFicicle900No ratings yet
- MainDocument10 pagesMainLythuo KryNo ratings yet
- Infección VIH Primer 2023Document21 pagesInfección VIH Primer 2023MedicazoNo ratings yet
- Reservatório HIVDocument22 pagesReservatório HIVpamellagoulart2004No ratings yet
- Hematopoietic Stem Cell Transplantation For HIV Cure: Daniel R. KuritzkesDocument6 pagesHematopoietic Stem Cell Transplantation For HIV Cure: Daniel R. KuritzkesVergio MarkusNo ratings yet
- Humoral and Innate Antiviral Immunity As Tools To Clear Persistent HIV InfectionDocument8 pagesHumoral and Innate Antiviral Immunity As Tools To Clear Persistent HIV InfectionLhorruama DiasNo ratings yet
- Phylogenies ArtDocument9 pagesPhylogenies ArtIris SolarNo ratings yet
- HHS Public Access: HIV-1 Drug Resistance and Resistance TestingDocument42 pagesHHS Public Access: HIV-1 Drug Resistance and Resistance TestingAlfiraNo ratings yet
- Hunter Fitness Cost PolDocument22 pagesHunter Fitness Cost PolJim HunterNo ratings yet
- Main 1Document4 pagesMain 1rest_a2003No ratings yet
- Vaccination of Healthcare Workers A ReviewDocument17 pagesVaccination of Healthcare Workers A Reviewy2h996tnp8No ratings yet
- HIV InfectionDocument22 pagesHIV Infectionquang.14y1543No ratings yet
- Hernandez Martin Simkins 1Document13 pagesHernandez Martin Simkins 1angelNo ratings yet
- Artikel+Kompilasi+OBJ13 3revDocument19 pagesArtikel+Kompilasi+OBJ13 3revAurha Akmal GinarisNo ratings yet
- Therapy For Persistent HIVDocument6 pagesTherapy For Persistent HIVAnonymous ceYk4p4No ratings yet
- CatfluDocument13 pagesCatflumvdaniela.santanaNo ratings yet
- Medical Hypotheses: SciencedirectDocument3 pagesMedical Hypotheses: SciencedirectnordonkNo ratings yet
- Imunopatogenesis - HIVDocument19 pagesImunopatogenesis - HIVlia tri maryaniNo ratings yet
- Johnston 2007Document9 pagesJohnston 2007MedranoReyesLuisinNo ratings yet
- Hiv Diagnosis and Treatment Through Advaced TechDocument16 pagesHiv Diagnosis and Treatment Through Advaced TechAde KurniaNo ratings yet
- coinfeccion determinante de vihDocument8 pagescoinfeccion determinante de vihSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- 10.1128@JVI.00486-20Document59 pages10.1128@JVI.00486-20Aneesh S NairNo ratings yet
- Targeted Shock-And-Kill Hiv-1 Gene Therapy Approach Combining Crispr Activation, Suicide Gene Tbid and Retargeted Adenovirus DeliveryDocument11 pagesTargeted Shock-And-Kill Hiv-1 Gene Therapy Approach Combining Crispr Activation, Suicide Gene Tbid and Retargeted Adenovirus DeliveryMusa MusaNo ratings yet
- Multipurpose Prevention Technologies: The Future of HIV and STI ProtectionDocument8 pagesMultipurpose Prevention Technologies: The Future of HIV and STI ProtectionKaoru Eduardo AtouyatzinNo ratings yet
- HHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideDocument30 pagesHHS Public Access: The Immunology of Tuberculosis: From Bench To BedsideicaeeNo ratings yet
- FetchObject ActionDocument22 pagesFetchObject ActionLucas DutraNo ratings yet
- 1 s2.0 S0022519318301395 MainDocument13 pages1 s2.0 S0022519318301395 MainIntan PermataNo ratings yet
- Herpes Simplex Virus Evasion of Early Host Antiviral ResponsesDocument24 pagesHerpes Simplex Virus Evasion of Early Host Antiviral ResponsesRoberto DurónNo ratings yet
- The Gift of A Lifetime: Analysis of HIV at Autopsy: Frank MaldarelliDocument5 pagesThe Gift of A Lifetime: Analysis of HIV at Autopsy: Frank MaldarelliIrina TănaseNo ratings yet
- Fisiopatología VIHDocument13 pagesFisiopatología VIHjahernandezs0110No ratings yet
- MBS2008 Mutation and Control of The Human Immunodeficiency Virus StengelDocument10 pagesMBS2008 Mutation and Control of The Human Immunodeficiency Virus StengelSaeb AmirAhmadi ChomacharNo ratings yet
- Firdaus 2014Document8 pagesFirdaus 2014Pavithra NNo ratings yet
- Envejecimiento HivDocument8 pagesEnvejecimiento HivJose LunaNo ratings yet
- Seminar: Daniel P Webster, Paul Klenerman, Geoff Rey M DusheikoDocument12 pagesSeminar: Daniel P Webster, Paul Klenerman, Geoff Rey M Dusheikovira khairunisaNo ratings yet
- Antifungal Drugs - The Current Armamentarium and Development of New AgentsDocument20 pagesAntifungal Drugs - The Current Armamentarium and Development of New AgentssovalaxNo ratings yet
- Global Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDDocument15 pagesGlobal Epidemiology of Tuberculosis: Philippe Glaziou, MD Katherine Floyd, PHD Mario C. Raviglione, MDbrachiuroNo ratings yet
- Hepatitis C Virus Replication and Potential Targets For Direct-Acting AgentsDocument11 pagesHepatitis C Virus Replication and Potential Targets For Direct-Acting AgentsWael Abdel-MageedNo ratings yet
- AIDS ClassDocument58 pagesAIDS ClassramyaayokeshNo ratings yet
- Rotavirus Related Systemic Diseases Clinical Manifestation Evidence and PathogenesisDocument17 pagesRotavirus Related Systemic Diseases Clinical Manifestation Evidence and PathogenesisDaniela MontecinosNo ratings yet
- Vassilopoulos 2002Document13 pagesVassilopoulos 2002deliaNo ratings yet
- Vih RevDocument25 pagesVih RevANDRÉS FELIPE BUSTILLO GÓMEZNo ratings yet
- 1 s2.0 S0166354222002868 MainDocument8 pages1 s2.0 S0166354222002868 Mainnathanaellee92No ratings yet
- A Special Issue On Infections in Solid Organ Transplant RecipientsDocument3 pagesA Special Issue On Infections in Solid Organ Transplant RecipientsKhushal khanNo ratings yet
- A New Perspective On HIV CureDocument4 pagesA New Perspective On HIV CureRemo Anthony Gonza LuqueNo ratings yet
- Special Issue: Structural and Molecular Biology of HIVDocument2 pagesSpecial Issue: Structural and Molecular Biology of HIVbookmoonNo ratings yet
- Veaa 013Document15 pagesVeaa 013jaspforeverNo ratings yet
- Pathogenesis of HIV Infection: Infectious Disease Reports June 2013Document6 pagesPathogenesis of HIV Infection: Infectious Disease Reports June 2013MILDA KHAERUNNISANo ratings yet
- Pharmacology of HIV RXDocument10 pagesPharmacology of HIV RXdupuytrenNo ratings yet
- revision sistematica multipatogenaDocument7 pagesrevision sistematica multipatogenaSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- Nihms 839861Document40 pagesNihms 839861Faisal JamshedNo ratings yet
- Panther 1999Document9 pagesPanther 1999Araceli Enríquez OvandoNo ratings yet
- The Role of Human Dendritic Cells in HIV-1 InfectionDocument9 pagesThe Role of Human Dendritic Cells in HIV-1 InfectionrizkaNo ratings yet
- Editorial Overview Hildegund CJ Ertl and Antonio LanzavecchiaDocument3 pagesEditorial Overview Hildegund CJ Ertl and Antonio Lanzavecchiahoangan118No ratings yet
- The Spread, Treatment, and Prevention of HIV-1: Evolution of A Global PandemicDocument12 pagesThe Spread, Treatment, and Prevention of HIV-1: Evolution of A Global PandemicLatiefah NWNo ratings yet
- Evidence That Hepatitis C Virus Genome Partly Controls Infection OutcomeDocument15 pagesEvidence That Hepatitis C Virus Genome Partly Controls Infection OutcomeKaritoNo ratings yet
- Infectious Diseases in Solid-Organ Transplant Recipients: A practical approachFrom EverandInfectious Diseases in Solid-Organ Transplant Recipients: A practical approachOriol ManuelNo ratings yet
- Admin,+56 Ism.v11i1.557Document5 pagesAdmin,+56 Ism.v11i1.557Reni Tri AstutiNo ratings yet
- The Material Culture of The Postsocialist CityDocument15 pagesThe Material Culture of The Postsocialist Cityjsgt1980No ratings yet
- 0547 s06 TN 3Document20 pages0547 s06 TN 3mstudy123456No ratings yet
- 3M CorporationDocument3 pages3M CorporationIndoxfeeds GramNo ratings yet
- Alameda Investments - Alameda InvestmentsDocument9 pagesAlameda Investments - Alameda InvestmentsLuisNo ratings yet
- Problemsolving RubricDocument1 pageProblemsolving Rubricapi-560491685No ratings yet
- March 16 - IM Processors DigiTimesDocument5 pagesMarch 16 - IM Processors DigiTimesRyanNo ratings yet
- Halimatus Islamiah Analisis Jurnal Internasional K3Document3 pagesHalimatus Islamiah Analisis Jurnal Internasional K3TussNo ratings yet
- The Radiology Assistant - Fleischner 2017 GuidelineDocument11 pagesThe Radiology Assistant - Fleischner 2017 GuidelineHenry J. Hernández L.No ratings yet
- Lesson Plan 8 (September) (AutoRecovered) 1Document3 pagesLesson Plan 8 (September) (AutoRecovered) 1Rutchie AbantoNo ratings yet
- Bstem-5 4Document61 pagesBstem-5 4G-SamNo ratings yet
- Huffman Coding - Base of JPEG Image CompressionDocument13 pagesHuffman Coding - Base of JPEG Image CompressionFikaduNo ratings yet
- Quiz For Western Lit.Document25 pagesQuiz For Western Lit.donnie4workingNo ratings yet
- Shahetal.2022 TecGeomorpJhelumDocument21 pagesShahetal.2022 TecGeomorpJhelumAyesha EjazNo ratings yet
- Ballistic - August September 2021Document168 pagesBallistic - August September 2021andrewrowe100% (2)
- Cost Leadership Porter Generic StrategiesDocument7 pagesCost Leadership Porter Generic StrategiesRamar MurugasenNo ratings yet
- Thou Hast Made MeDocument3 pagesThou Hast Made Meyour dady0% (1)
- Ethical Considerations Dissertation ExampleDocument7 pagesEthical Considerations Dissertation ExampleBuyPapersOnlineCanada100% (1)
- Dbms Lab Dbms Lab: 23 March 202Document12 pagesDbms Lab Dbms Lab: 23 March 202LOVISH bansalNo ratings yet
- HG-G9 Module 7 RTP PDFDocument10 pagesHG-G9 Module 7 RTP PDFDaniel Robert BuccatNo ratings yet
- Chapter 1 Peanut Growing and HarvestingDocument18 pagesChapter 1 Peanut Growing and HarvestingKapil BhattNo ratings yet
- VP3401 As04Document2 pagesVP3401 As04shivamtyagi68637No ratings yet
- Peptides and Proteins: M.Prasad Naidu MSC Medical Biochemistry, PH.DDocument30 pagesPeptides and Proteins: M.Prasad Naidu MSC Medical Biochemistry, PH.DDr. M. Prasad NaiduNo ratings yet
- HMT (U4)Document23 pagesHMT (U4)maniNo ratings yet
- Marik ServitorsDocument20 pagesMarik ServitorsDWNloader100% (2)
- Reflection Paper On "Legal Research, Legal Writing, and Legal Analysis: Putting Law School Into Practice" by Suzanne RoweDocument2 pagesReflection Paper On "Legal Research, Legal Writing, and Legal Analysis: Putting Law School Into Practice" by Suzanne RoweRobert Jay Regz Pastrana IINo ratings yet
- Alarm Security Pic - Google ShoppingDocument1 pageAlarm Security Pic - Google Shoppingleeleeleebc123No ratings yet
- Analisis Pemetaan (Jadual Kenalpasti Cu Wa)Document5 pagesAnalisis Pemetaan (Jadual Kenalpasti Cu Wa)En AzermieyNo ratings yet