Professional Documents
Culture Documents
00006123-199407000-00004
00006123-199407000-00004
Uploaded by
Dsm DsmCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
00006123-199407000-00004
00006123-199407000-00004
Uploaded by
Dsm DsmCopyright:
Available Formats
Neurosurgery 1992-98 changes in hemostatic parameters associated with
July 1994, Volume 35, Number 1 neurosurgery may result in misinterpreting changes
26 Serial Changes in Hemostasis after Intracranial in the hemostatic systems (7,11,19,26). Indeed, other
Surgery kinds of surgery have been noted to alter the
Clinical Study hemostatic systems (9,10,17). Therefore, it is important
to assess the dynamic changes in hemostasis after
AUTHOR(S): Fujii, Yukihiko, M.D.; intracranial surgery.
Tanaka, Ryuichi, M.D.; Takeuchi, Shigekazu, M.D.; In this study, we performed hemostatic studies,
Koike, Tetsuo, M.D.; Minakawa, Takashi, M.D.; including assays of molecular markers of hemostatic
Sasaki, Osamu, M.D. activation, i.e., substances produced by the activation
of hemostatic systems, on patients undergoing
Department of Neurosurgery, Brain Research clipping of unruptured cerebral aneurysms in order to
Institute, Niigata University (RT, ST, TK, TM), and assess the influence of intracranial surgery itself on
Department of Neurosurgery, Kuwana Hospital (YF, hemostasis.
OS), Niigata, Japan
PATIENTS AND METHODS
Neurosurgery 35; 26-33, 1994 Eight patients (5 men and 3 women) undergoing
clipping of unruptured cerebral aneurysms, who had
ABSTRACT: WE PERFORMED HEMOSTATIC neither neurological deficits nor hemostatic
studies on eight patients undergoing clipping of abnormalities, were studied. The patients ranged in
unruptured cerebral aneurysms to assess the influence age from 41 to 71 (58.3 ± 10.6) years. The site of the
of intracranial surgery itself on hemostasis. Blood cerebral aneurysm was the anterior communicating
samples were collected from each patient 10 times: artery in three patients, the middle cerebral artery in
before and after the induction of anesthesia and 6, 12, two, the distal anterior cerebral artery in one, the
and 24 hours and 2, 3, 5, and 7 days immediately upper basilar artery trunk in one, and the distal
after surgery. The changes and our interpretation of superior cerebellar artery in one. All the patients
them include the following: 1) the elevation of underwent clipping of the aneurysmal neck under
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
thrombin antithrombin III complex levels (activation general anesthesia with nitrous oxide and enflurane,
of blood coagulation) was transient and monophasic; and the surgical procedures were completed within 4
2) the elevation of plasmin α2-antiplasmin complex hours. No patient received osmotic agents during
and D-dimer levels (activation of fibrinolysis) was surgery. The total blood loss was less than 200 ml in
biphasic, despite the monophasic elevation of tissue all cases. As a result, no patient was transfused. Each
plasminogen activator or plasminogen activator patient was given a regular diet and approximately
inhibitor-1 levels; 3) the elevation of β- 1500 ml of isotonic solution intravenously daily.
thromboglobulin and platelet-factor-4 levels Ten ml of blood was collected before (baseline)
(activation of platelet) was also biphasic; 4) and after the induction of anesthesia, immediately
fibrinogen level and α2-antiplasmin activity increased after surgery, 6, 12, 24 hours, and 2, 3, 5, and 7 days
in the acute phase of the postoperative course (acute after surgery. No blood sample was drawn for this
phase reaction); 5) the changes in hematocrit study during the operation. Venipuncture was
appeared to parallel those in various other performed with a 21-gauge siliconized butterfly
parameters, especially platelet count, antithrombin needle. Various tests were performed on blood
III, and plasminogen levels for 1 or 2 days after samples thus collected. Table 1 lists all tests and
surgery; 6) fibronectin appeared to be consumed in parameters assessed in this study, giving their
the acute phase of postoperative course; and 7) meanings. Figure 1 briefly illustrates hemostatic
general anesthesia did not significantly affect systems, i.e., interplay of blood coagulation,
hemostasis. These serial changes seem to be related fibrinolysis, platelets, and blood vessel. The first 1 ml
to the activation of hemostatic systems after of blood was used for blood cell counts, including
intracranial surgery and the subsequent acute phase white blood cell, red blood cell and platelet count,
reaction. hemoglobin, and hematocrit value, using S-PLUS JR
(Coulter, Hialeah, FL). The next 2 ml was used for
KEY WORDS: Blood coagulation; Fibrinolysis; fibrin (-ogen) degradation products assay, using the
Hemostasis; Molecular markers; Neurosurgery; latex photometric immunoassay (LPIA, Iatron,
Platelet; Postoperative state Tokyo, Japan). The next 2.5 ml was carefully placed
into a prechilled glass tube containing an antiplatelet
Patients with neurosurgical diseases have a high risk anticoagulant consisting of theophylline, adenosine,
of developing a number of the disorders of dipyridamole, and sodium citrate, and the plasma
hemostasis, including disseminated intravascular separated was stored frozen at -70°C and used for
coagulation (DIC) (11,15,23) and deep venous batch analyses of β-thromboglobulin and platelet-
thrombosis complicated by pulmonary embolism (4, factor-4 by enzyme immunoassay (Asserachrom,
24)
. Although many clinical studies and trials related Diagnostica Stago, Paris, France). The last 4.5 ml was
to hemostasis in neurosurgical patients have been transferred into a plastic tube containing 1 ml of 3.1%
reported (2,3,5,8,25,28), none appears to have taken into citrated buffer, and the plasma was stored frozen at -
consideration the influence of surgery itself on 70°C until batch analyses were performed by the
hemostasis. The lack of adequate information on following assays: 1) clot-based assays to determine
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
prothrombin time (PT), activated partial were no significant changes in α2-antiplasmin
thromboplastin time, and fibrinogen level activity for 3 days after surgery; however, significant
(Thromboplastin C, Actin, Fibrinogen determination (P < 0.05) increases (116.5% of the baseline value)
set, Baxster-Dade, Miami, FL); 2) chromogenic were observed 5 and 7 days, postoperatively (Fig. 3).
substrate assays to determine antithrombin III, α2- The PAP level became considerably (P < 0.05)
antiplasmin and plasminogen activity (Berichrom, elevated immediately after surgery and, after rapidly
Behringwerke, Marburg, Germany); 3) enzyme returning to the baseline value, began to rise again 3
immunoassay to estimate thrombin antithrombin III days after surgery, significantly (P < 0.05) exceeding
complex (TAT) (Enzygnost TAT, Behringwerke), the baseline value. The D-dimer level (P < 0.01) rose
plasmin α2-antiplasmin complex (PAP) (α2PI significantly immediately after surgery, reaching its
Complex, Teijin, Tokyo, Japan), D-dimer initial peak 6 hours after surgery, then gradually
(Asserachrom, Diagnostica Stago), total tissue decreased to its lowest value 2 days after surgery, and
plasminogen activator (t-PA), and free plasminogen subsequently increased to a higher level than the
activator inhibitor-1 (PAI-1) levels (American initial peak. Its level remained considerably (P <
Diagnostica, Greenwich, CT); and 4) assay to 0.01) higher than the baseline value until the end of
determine fibronectin level using a nephelometer the study (Fig. 4). The fibrin degradation product
(NB100, Behringwerke). All assays were completed level changed in parallel with changes in the D-dimer
within a month after the blood collection. All data level, and the values 6 hours and 7 days after surgery
were expressed as mean ± standard deviation, and the were 4.3 ± 0.9 and 4.8 ± 2.0 µg/ml, respectively. Both
paired Student's t-test was performed to assess t-PA and PAI-1 levels (P < 0.05) increased
statistical changes in hemostatic parameters after significantly immediately after surgery, compared
surgery in comparison with baseline values. with the baseline values, then rapidly decreased and
reached the baseline values within 24 hours after
RESULTS surgery. No significant elevations of t-PA and PAI-1
Clinical outcome followed their initial increase (Fig. 5).
No patients experienced postoperative neurological
deterioration, DIC, or clinical signs of deep vein Platelet system
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
thrombosis. The platelet count increased slightly immediately
after surgery, then gradually decreased, reaching its
Anesthesia nadir 2 days after surgery (81.2% of the baseline
There were no significant differences in any tests value), after which it rapidly increased to become
performed before or after the induction of anesthesia significantly (P < 0.05) higher than the baseline value
(Figs. 2, 3, 4, 5, 6). (Fig. 2C). Both β-thromboglobulin and platelet-factor-
4 levels (P < 0.01) rose significantly immediately
Blood coagulation system after surgery, rapidly decreased, and returned to the
The PT was significantly (P < 0.05) prolonged for baseline values within 24 hours after surgery. They
2 days after surgery (12.2-12.8 ± 0.6 sec), compared then gradually increased again, becoming
with the baseline value (11.4 ± 0.6 sec), but no significantly (P < 0.01) higher than the baseline
significant changes in activated partial values 7 days after surgery (Fig. 6).
thromboplastin time were observed after surgery.
Antithrombin III activity gradually decreased after Fibronectin
surgery, reaching its nadir 2 days after surgery The fibronectin level gradually decreased after
(87.3% of the baseline value), but soon returned to surgery, reached its lowest level (71.8% of the
the baseline value (Fig. 2A). There were no baseline value) 24 hours after surgery, and returned to
significant changes in fibrinogen levels immediately the baseline value 5 days after surgery (Fig. 2C).
and 6 hours after surgery. The fibrinogen level started
to increase 12 hours after surgery, reached its highest Blood cell counts
level 2 or 3 days after surgery (191.0% of the The white blood cell count significantly (P < 0.01)
baseline value), and decreased gradually thereafter. increased over the baseline value immediately after
However, its level remained significantly (P < 0.01) surgery, became peaked (246.9% of the baseline
higher than the baseline value until the end of the value) 6 hours after surgery, gradually decreased
study (Fig. 3). The TAT level (P < 0.01) rose thereafter, and almost returned to the baseline value 5
significantly immediately after surgery, then days after surgery (Fig. 3). Although the red blood
gradually diminished, and returned to within the cell count, hemoglobin, and hematocrit value did not
normal range. Its level, however, remained change immediately after surgery, they gradually
significantly (P < 0.05) higher than the baseline value decreased, reaching their nadir 3 days after surgery
until the end of the study (Fig. 4). (80.0, 77.3, and 76.3% of the baseline values,
respectively), and remained significantly (P < 0.01)
Fibrinolytic system lower than the baseline values until the end of the
Plasminogen activity rapidly decreased, reached its study (Fig. 2).
lowest value 24 hours after surgery (77.3% of the
baseline value), and then gradually increased, DISCUSSION
becoming significantly (P < 0.01) higher than the A few studies on serial changes in limited numbers
baseline value (Fig. 2B). On the other hand, there of hemostatic parameters after abdominal surgery (9,
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
10,17)
and cardiopulmonary bypass (6,14) have been cytokines, mainly interleukin-6 (12). The acute phase
published. Intracranial surgery, however, differs from reaction is a factor that should be considered in
other surgery in many ways, i.e., the brain contains postoperative changes in hemostatic systems. White
singularly high levels of tissue thromboplastin, and blood cell counts and fibrinogen levels increased in
intracranial surgery usually requires craniotomy. the acute phase, and α2-antiplasmin did not decrease
Nevertheless, to the best of our knowledge, no studies despite significant decreases in hematocrit (Fig. 3).
on postoperative changes in hemostasis after Fibrinogen is also an important factor in the
intracranial surgery have been published. In this diagnosis of DIC, and hence we have to bear in mind
study, we performed many hemostatic assays, which that the plasma level of fibrinogen never decreases
enabled us to comprehensively evaluate hemostatic significantly after surgery unless the hematocrit drops
systems, including the coagulation system, precipitously, because fibrinogen is a representative
fibrinolytic system, and platelet system. Moreover, acute phase reactant.
there have been no studies in any specialty in which
such a comprehensive evaluation of hemostatic Activation of the coagulation system
systems has been performed. We investigated only An elevation of TAT means the presence of
patients with an unruptured aneurysm to assess thrombin, a powerful enzyme that catalyzes the
changes in hemostasis associated with intracranial conversion of fibrinogen into fibrin in the circulating
surgery because of the following two reasons: 1) blood, i.e., activation of the coagulation system
patients with other neurosurgical diseases, e.g., (Table 1 and Fig. 1) (20). The TAT elevation after
stroke, brain tumor, and trauma, are expected to have surgery was rapid but transient and was followed by a
hemostatic abnormalities before surgery; and 2) a return to the normal range, although the levels were
number of studies on vasospasm after the rupture of significantly higher than the baseline value until the
cerebral aneurysm have been performed using various end of the study (Fig. 4). From the fact that the
hemostatic tests, such as β-thromboglobulin (7,19,26). changes in the TAT level after intracranial surgery are
monophasic, it is considered that a second elevation
Influence of anesthesia in TAT after surgery may indicate the occurrence of
There were no significant changes in any of the coagulopathy, including DIC, deep vein thrombosis,
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
parameters we assessed after general anesthesia and pulmonary embolism (4).
(Figs. 2, 3, 4, 5, 6). Thus, it appears that the influence
of general anesthesia with nitrous oxide and Activation of the fibrinolytic system
enflurane on the hemostatic systems before surgery is An elevation of PAP means the presence of
of little significance. plasmin, a powerful fibrin-cleaving enzyme in blood
circulation, i.e., activation of the fibrinolytic system
Influence of hemodilution (Table 1 and Fig. 1) (18). The level of PAP, which was
The hematocrit values did not change immediately generated during surgery, rapidly decreased and
after surgery probably because of a balance between returned to the baseline value within 24 hours
blood loss and rehydration during surgery; however, (Fig. 4); however, it gradually increased again and
they did gradually decrease by 23.7% of the baseline became significantly higher than the baseline value.
value as a result of hemodilution after intravenous Thus, the changes in PAP were biphasic,
infusion. The changes in hematocrit appeared to corroborating the findings of Mellbring et al. (17).
affect various hemostatic parameters assessed in this Increases in D-dimer levels indicate the presence of
study, especially platelet count, antithrombin III, and both thrombin and plasmin in the blood, i.e., D-dimer
plasminogen levels (Fig. 2), although the possibility represents degradation products derived from cross-
of their consumption after surgery cannot be linked fibrin but not from fibrinogen (Table 1 and
completely excluded. Platelet count, antithrombin III, Fig. 1) (21). Changes in D-dimer were also biphasic
and plasminogen levels decreased in parallel with the and followed the changes in PAP (Fig. 4), failing to
changes in hematocrit for 1 or 2 days after surgery corroborate the study reported by Kang et al. who
and then started to increase. It is generally accepted claimed that the initial fibrinolytic reaction was not
that concentration levels in various hemostatic associated with D-dimer elevation on the basis of
parameters, such as platelets, fibrinogen, semiquantitative assay (10). Plasmin is generated by a
antithrombin III, α2-antiplasmin, and plasminogen, number of plasminogen activators, e.g., t-PA.
change in parallel with the fall in hematocrit after Although we investigated levels of t-PA and PAI-1
hemodilution (6,13,14,22). Thus, hematocrit seems to be after surgery to assess the relationship between PAP
an important parameter in assessing changes in the and t-PA or PAI-1, the changes were monophasic
hemostatic systems. More significant decreases in rather than biphasic and did not correspond to those
these parameters, especially in platelet count, than in PAP (Fig. 5). It is unclear why the second
those in hematocrit, may indicate pathological (not elevation of PAP was not associated with an elevation
physiological) consumption, e.g., DIC. of the t-PA or PAI-1 level. However, plasminogen
activators other than t-PA may activate plasminogen
(16)
Influence of acute phase reaction , or fibrin deposits in wound healing after surgery
It is well known that increases in the concentration may contribute as potentiating agents in the process
of many hemostatic substances are observed shortly of plasminogen activation (17). Hence, it seems very
after chemical, inflammatory, or physical stimulation, important in assessing hemostatic disorders after
i.e., acute phase reaction, because of the interaction of surgery to be aware that postoperative changes in
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
PAP and D-dimer are biphasic, despite the for his valuable hematological suggestions; Dr.
monophasic changes in t-PA and PAI-1. Takayuki Koizumi, Dr. Yoshiho Honda, and Dr.
Yasusi Itoh for their clinical assistance; and Ms.
Platelet activation Noriko Sakai, Ms. Miho Suga, and Ms. Yoko Ishii for
Platelet factor 4 and β-thromboglobulin are their laboratory assistance.
proteins stored in the α- granules of platelets, and
their elevation in plasma indicates platelet activation Received, April 23, 1993.
(Table 1 and Fig. 1) (27). Changes in platelet-factor-4 Accepted, January 13, 1994.
and β- thromboglobulin levels were also biphasic, Reprint requests: Yukihiko Fujii, M.D.,
and their levels became significantly higher than the Department of Neurosurgery, Brain Research
baseline value in parallel with platelet counts 7 days Institute, Niigata University, 757 Asahimachi 1,
after surgery (Fig. 6). It is also unclear why a second Niigata, 951 Japan.
elevation of their levels was observed. The second
elevation, however, may be relevant to wound REFERENCES: (1-28)
healing and tissue repair after surgery.
1. Beckmann R, Geiger M, De Vries C,
Fibronectin Pannekoek H, Binder BR: Fibronectin
Fibronectin is an adhesive glycoprotein that is decreases the stimulation effect of fibrin and
involved in many biological processes, such as cell fibrinogen fragment FCB-2 on plasmin
adhesion to extracellular matrix, cross-linking of formation by tissue plasminogen activator. J
fibrin or collagen, and platelet aggregation (Table 1 Biol Chem 66:2227-2232, 1991.
and Fig. 1). It can be found on cell surfaces, in 2. Findlay JM: Subarachnoid fibrinolytic
extracellular matrix, and in plasma. The binding and treatment for the prevention of cerebral
cross-linking of fibronectin to fibrin seem to be vasospasm. Semin Neurol 11:400-410, 1991.
important for the attachment and ingrowth of cells 3. Fodstad H, Nilsson IM: Coagulation and
into clot and, therefore, for wound healing and tissue fibrinolysis in blood and cerebrospinal fluid
repair (1). The decrease in fibronectin level was after aneurysmal subarachnoid haemorrhage:
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
greater than the fall in hematocrit (Fig. 2C), which Effect of tranexamic acid (AMCA) Acta
may indicate that the consumption of fibronectin is Neurochir 56:25-38, 1981.
for wound healing and tissue repair after surgery. 4. Fujii Y, Mammen EF, Farag A, Muz J,
Salciccioli GG, Weingerden ST: Thrombosis
CONCLUSION in spinal cord injury. Thromb Res 68:357-
It should always be borne in mind that changes in 368, 1992.
the hemostatic systems associated with intracranial 5. Glick R, Green D, Ts'ao C, Witt WA, Yu
surgery are dynamic and characteristic of the ATW, Raimondi AJ: High dose ε-
individual hemostatic parameters involved. The aminocaproic acid prolongs the bleeding time
following findings are particularly important: 1) the and increases rebleeding and intraoperative
elevation of the TAT level (activation of blood hemorrhage in patients with subarachnoid
coagulation) was transient and monophasic; and 2) hemorrhage. Neurosurgery 9:398-401, 1981.
the elevation of PAP and D-dimer levels (activation 6. Harker LA, Malpass TW, Branson HE, Hassel
of fibrinolysis) was biphasic despite the monophasic EA, Slichter SJ: Mechanism of abnormal
elevation of the t-PA or PAI-1 level; 3) the elevation bleeding in patients undergoing
of β-thromboglobulin and platelet-factor-4 levels cardiopulmonary bypass: Acquired transient
(activation of platelet) was also biphasic; 4) the platelet dysfunction associated with selective
fibrinogen level and α2-antiplasmin activity rose in a-granule release. Blood 56:824-834, 1980.
the acute phase of the postoperative state (acute phase 7. Hasegawa T, Watanabe H, Ishii S: Studies of
reaction); 5) the changes in hematocrit appeared to intravascular components in cerebral
parallel those in various other parameters, especially vasospasm following subarachnoid
platelet counts, antithrombin III, and plasminogen hemorrhage. Neurosurg Rev 3:93-100, 1980.
levels for 1 or 2 days after surgery; 6) the fibronectin 8. Hossmann V, Bewermeyer H, Auel H, Heiss
appeared to be consumed in the acute phase of the WD: Monitoring of antifibrinolytic treatment
postoperative state; and 7) general anesthesia did not in subarachnoid hemorrhage. Eur Neurol
significantly affect hemostasis. These serial changes 24:196-204, 1985.
seem to be related to the activation of hemostatic 9. Kambayashi J, Sakon M, Yokota M, Shiba E,
systems by intracranial surgery and subsequent acute Kawasaki T, Mori T: Activation of
phase reaction. Additional studies seem to be coagulation and fibrinolysis during surgery,
required to assess late postoperative changes in analyzed by molecular markers. Thromb Res
hemostatic systems, because, in this study, we noted 60:157-167, 1990.
some parameters still remained out of the normal 10. Kang J, Kambayashi J, Sakon M, Tsujinaka T,
range 7 days after surgery. Mori T: Postoperative changes in hemostasis
analyzed by the serial determination of
ACKNOWLEDGMENTS fibrinopeptides and D-dimer. Jpn J Surg
The authors thank Dr. Hoyu Takahashi, the 1st 19:262-268, 1989.
Department of Internal Medicine, Niigata University, 11. Kaufman HH, Hui KS, Mattson JC:
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Clinicopathological correlations of 26. Toyoda O, Nakajima H, Nukui H: Changes in
disseminated intravascular coagulation in coagulation and fibrinolysis and effects of
patients with head injury. Neurosurgery ticlopidine and cisternal drainage in the acute
15:34-42, 1984. phase following aneurysm rupture (in
12. Kishimoto T: The biology of interleukin-6. Japanese, English abstr) Neurol Med Chir
Blood 74:1-10, 1989. (Tokyo) 30:670-675, 1990.
13. Laks H, Handin RI, Martin V, Pilon RN: The 27. Walz DA: Platelet-released protein as
effect of acute normovolemic hemodilution on molecular markers for the activation process.
coagulation and blood utilization in major Semin Thromb Hemost 10:270-279, 1984.
surgery. J Surg Res 20:225-230, 1976. 28. Zabramski JM, Spetzler RF, Lee KS,
14. Mammen EF, Koets MH, Washington BC, Papadopoulos SM, Bovill E, Zimmerman RS,
Wolk LW, Brown JM, Burdick M, Selik NR, Bederson JB: Phase I trial of tissue
Wilson RF: Hemostasis changes during plasminogen activator for the prevention of
cardiopulmonary bypass surgery. Semin vasospasm in patients with aneurysmal
Thromb Hemost 11:281-292, 1985. subarachnoid hemorrhage. J Neurosurg
15. Matjasko MJ, Ducker TB: Disseminated 75:189-196, 1991.
intravascular coagulation associated with
removal of a primary brain tumor: A case COMMENTS
report. J Neurosurg 47:476-480, 1977. The authors have made a substantial effort of
16. Matsuda T, Asakura H, Ito K, Sato M, Jokaji documenting the changes that occurred in several
Y, Uotani C, Kumabashiri I: Changes in levels hemostatic parameters immediately and up to 7 days
of t-PA and α2 PI-plasmin complex in plasma after intracranial surgery. The data demonstrate
in patients with DIC. Thromb Res (Suppl) evidence of the activation of the coagulation and the
VIII:143-151, 1988. fibrinolytic systems. However, the overall fibrinolytic
17. Mellbring G, Dahlgren S, Wiman B: Plasma potential of the blood cannot be assessed because the
fibrinolytic activity in patients undergoing assays did not include a measurement of the
major abdominal surgery. Acta Chir Scand fibrinolytic capacity at the various time points. A
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
151:109-114, 1985. fibrinolytic "shut-down" has been described in non-
18. Mimuro J, Koike Y, Sumi Y, Aoki N: neurosurgical patients and has included a rise in
Monoclonal antibodies to discrete regions in plasminogen activator inhibitor-1 and a drop in tissue
α2-plasmin inhibitor. Blood 69:446-453, plasminogen activator (1). The former is well
1987. documented in this study, whereas the latter did not
19. Ohkuma H, Suzuki S, Kimura M, Sobata E: occur.
Role of platelet function in symptomatic It should be noted that this study has included only
cerebral vasospasm following aneurysmal patients with unruptured aneurysms who underwent
subarachnoid hemorrhage. Stroke 22:854- uncomplicated surgery and in whom the brain
859, 1991. parenchyma was not transgressed. It is anticipated
20. Pelzer H, Schwarz A, Heimburger N: that with other more complicated circumstances, such
Determination of human thrombin- as in brain tumor patients, the hemostatic parameters
antithrombin III complex in plasma with an are much more likely to lead to coagulopathies and to
enzyme-linked immunosorbent assay. thromboembolism (2,3).
Thromb Haemost 59:101-106, 1988. The lack of clinical evidence of deep venous
21. Rylatt DB, Blake AS, Cottis LE: An thrombosis in this study does not exclude its
immunoassay for human D-dimer using occurrence at a subclinical level, and future studies
monoclonal antibodies. Thromb Res 31:767- would be more clinically relevant if the significance
778, 1983. of the hemostatic changes were correlated with the
22. Six AJ, Tjon RM, Buys EM, Haas F, hemorrhagic as well as thromboembolic occurrences
Hollander van Zalk A, Haverkate F: The during and after intracranial surgery.
influence of coronary angiography and
angioplasty on parameters of hemostasis and Raymond Sawaya
fibrinolysis. Thromb Haemost 64:113-116, Houston, Texas
1990.
23. Spallone A, Mariani G, Rosa G: Disseminated REFERENCES: (1-3)
intravascular coagulation as a complication of
ruptured intracranial aneurysms. J Neurosurg 1. Kluft C: Fibrinolytic shut-down after surgery,
59:142-145, 1983. in Sawaya R (ed): Fibrinolysis and the
24. Swann KW, Black PM: Deep vein thrombosis Central Nervous System. Philadelphia, Hanley
and pulmonary emboli in neurosurgical & Belfus, 1990, pp 127-140.
patients: A review. J Neurosurg 61:1055- 2. Sawaya R, Glas-Greenwalt P: Postoperative
1062, 1984. venous thromboembolism and brain tumors:
25. Tokiyoshi K, Ohnishi T, Nii Y: Efficacy and Part II: Hemostatic profile. J Neurooncol
toxicity of thromboxane synthetase inhibitor 14:127-134, 1992.
for cerebral vasospasm after subarachnoid 3. Sawaya R, Ramo OJ, Glas-Greenwalt P, Wu
hemorrhage. Surg Neurol 36:112-118, 1991. SZ: Plasma fibrinolytic profile in patients
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
with brain tumors. Thromb Haemost 65:15-
19, 1991.
The authors have completed a detailed, systematic
evaluation of the hemostatic system in relation to
intracranial surgery. Changes in hemostasis in
neurosurgery are most commonly clinically
significant in trauma, where they are an issue in and
of themselves because of problems with intravascular
clotting and bleeding, which appear to be significant
enough to be related separately to outcome (1). This
article suggests the kinds of approach that could also
improve our understanding of coagulopathy in head
injury and can be used as a model for such work.
Howard H. Kaufman
Morgantown, West Virginia
REFERENCES: (1)
1. Olson JD, Kaufman HH, Moake J: The
incidence and significance of hemostatic
abnormalities in head injury. Neurosurgery
24:825-832, 1989.
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
Figure 1. A simplified diagram of the hemostatic
systems, which is facilitated through harmonious
interplay of the blood coagulation system,
fibrinolytic system, platelet system, and blood vessel
wall. The tests and parameters assessed are printed in
bold type.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
Figure 2. Graph showing serial changes in
antithrombin III activity (A), plasminogen activity
(B), platelet counts and fibronectin levels (C), as a
comparison with hematocrit levels after intracranial
surgery. Values are expressed as mean ± standard
deviation (vertical bars). Significant differences (P <
0.05 and P < 0.01) from baseline values are indicated
with * and **, respectively.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
Figure 3. Graph showing serial changes in white
blood cell counts, fibrinogen levels, and α2-
antiplasmin activity after surgery. Values are
expressed as mean ± standard deviation (vertical
bars). Significant differences (P < 0.05 and P < 0.01)
from baseline values are indicated with * and **,
respectively.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Figure 4. Graph showing serial changes in thrombin
antithrombin III complex (TAT), plasmin α2-
antiplasmin complex (PAP), and D-dimer levels after
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
intracranial surgery. Values are expressed as mean ±
standard deviation (vertical bars). Significant
differences (P < 0.05 and P < 0.01) from baseline
values are indicated with * and **, respectively.
Figure 5. Graph showing serial changes in plasmin
α2-antiplasmin complex (PAP), tissue plasminogen
activator (t-PA), and plasminogen activator inhibitor-
1 (PAI-1) levels after intracranial surgery. Values are
expressed as mean ± standard deviation (vertical
bars). Significant differences (P < 0.05 and P < 0.01)
from baseline values are indicated with * and **,
respectively.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Figure 6. Graph showing serial changes in platelet
counts, β-thromboglobulin, and platelet-factor-4
levels after intracranial surgery. Values are expressed
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
as mean ± standard deviation (vertical bars).
Significant differences (P < 0.05 and P < 0.01) from
baseline values are indicated with * and **,
respectively.
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
Redistribution of this article permitted only in accordance with the publisher’s copyright provisions.
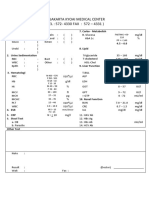
Table 1. List of Tests Assessed in This Study and
Their Meanings
Downloaded from https://academic.oup.com/neurosurgery/article-abstract/35/1/26/2757331
by guest
on 26 March 2018
You might also like
- Nursing Care Plan For Acute Gastrointestinal HemorrhageDocument2 pagesNursing Care Plan For Acute Gastrointestinal HemorrhageCyrus De Asis92% (25)
- Wu2017 PDFDocument6 pagesWu2017 PDFPavel SebastianNo ratings yet
- The Use of Recombinant Factor Viia (Novoseven) For Treatment of Active or Impending Bleeding in Brain Injury: Broadening The IndicationsDocument7 pagesThe Use of Recombinant Factor Viia (Novoseven) For Treatment of Active or Impending Bleeding in Brain Injury: Broadening The IndicationsBig TexNo ratings yet
- Platelet Function After Intramuscular Diclofenac: PagesDocument4 pagesPlatelet Function After Intramuscular Diclofenac: PagesTeguh D. WicaksonoNo ratings yet
- Vertebral Canal Haematoma and Coagulopathy - BjaDocument2 pagesVertebral Canal Haematoma and Coagulopathy - BjaRENAULTNo ratings yet
- Thrombolytic Therapy For Ischemic StrokeDocument7 pagesThrombolytic Therapy For Ischemic StrokechandradwtrNo ratings yet
- Endovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterDocument5 pagesEndovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterAswin ChristantoNo ratings yet
- 2012 Cryocompression Therapy After Elective Arthroplasty of The HipDocument8 pages2012 Cryocompression Therapy After Elective Arthroplasty of The HipGiancarlo Gardella MartínezNo ratings yet
- DIC in PediatricsDocument11 pagesDIC in PediatricsRizky LumalessilNo ratings yet
- Journal Medicine: The New EnglandDocument8 pagesJournal Medicine: The New EnglandDaav L. GuarneriNo ratings yet
- HSR1 04 NaderDocument7 pagesHSR1 04 Naderserena7205No ratings yet
- The Effect of IM Ketorolac Tromethamine On Bleeding Time: A Prospective, Interventional, Controlled StudyDocument3 pagesThe Effect of IM Ketorolac Tromethamine On Bleeding Time: A Prospective, Interventional, Controlled StudyDaniel TelloNo ratings yet
- Short-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismDocument4 pagesShort-And Long-Term Outcomes of Acute Upper Extremity Arterial ThromboembolismWilhelm HeinleinNo ratings yet
- Advances in Acute Ischemic Stroke TherapyDocument22 pagesAdvances in Acute Ischemic Stroke TherapylorenaNo ratings yet
- Surveillance IchDocument6 pagesSurveillance IchGabriel Septiana CitraNo ratings yet
- Methylene Blue: Role in Early Management of Septic Shock Patients?Document9 pagesMethylene Blue: Role in Early Management of Septic Shock Patients?Mahtosurup GodavarthyNo ratings yet
- Int J Dermatology - 2017 - Lee - Percutaneous Sclerotherapy Using Bleomycin For The Treatment of Vascular MalformationsDocument6 pagesInt J Dermatology - 2017 - Lee - Percutaneous Sclerotherapy Using Bleomycin For The Treatment of Vascular Malformationsradhianie djanNo ratings yet
- Dengue Myocarditis: Case ReportDocument3 pagesDengue Myocarditis: Case Reportallfanz_krenNo ratings yet
- Uneventful Epidural Analgesia in A Patient With Cyclic Idiopathic ThrombocytopeniaDocument4 pagesUneventful Epidural Analgesia in A Patient With Cyclic Idiopathic Thrombocytopeniasand52525No ratings yet
- 402 FullDocument7 pages402 Fullyohanes0gadiNo ratings yet
- J JCRC 2013 11 018Document5 pagesJ JCRC 2013 11 018Andres Rojas JerezNo ratings yet
- Preope Mayo Clinic 2020Document16 pagesPreope Mayo Clinic 2020claauherreraNo ratings yet
- Identifying Severe StrokeDocument8 pagesIdentifying Severe StrokekunneiNo ratings yet
- Efficacy and Morbidity of Therapeutic Renal Embolization in The Spectrum of Urologic DiseaseDocument7 pagesEfficacy and Morbidity of Therapeutic Renal Embolization in The Spectrum of Urologic DiseaseElías MendezNo ratings yet
- Hematoma Subdural Crónico: ¿Cuál Es El Tratamiento Quirúrgico de Elección?Document3 pagesHematoma Subdural Crónico: ¿Cuál Es El Tratamiento Quirúrgico de Elección?Brenda LopezNo ratings yet
- Laun 1990Document6 pagesLaun 1990pabloquinterobenavidezNo ratings yet
- Recurrent Venous Thrombosis Following Free Flap Surgery, The Role of Heparin-Induced Thrombocytopenia - Pulsus 2003Document4 pagesRecurrent Venous Thrombosis Following Free Flap Surgery, The Role of Heparin-Induced Thrombocytopenia - Pulsus 2003Nanna de VengerbergNo ratings yet
- Aha 24 HorasDocument17 pagesAha 24 HorasRichard SossaNo ratings yet
- 6 Antithrombotic Therapy in Patients With Infective EndocarditisDocument12 pages6 Antithrombotic Therapy in Patients With Infective Endocarditisabdeali hazariNo ratings yet
- Chirurgia Hemoragiei Din Ganglionii BazaliDocument8 pagesChirurgia Hemoragiei Din Ganglionii BazaliAndreea DanielaNo ratings yet
- BLT 09 336Document3 pagesBLT 09 336ichaNo ratings yet
- Imaging of Intracranial Haemorrhage: ReviewDocument12 pagesImaging of Intracranial Haemorrhage: ReviewNaomiNo ratings yet
- Ischemia-Modified Albumin Use As A Prognostic Factor in Coronary Bypass SurgeryDocument5 pagesIschemia-Modified Albumin Use As A Prognostic Factor in Coronary Bypass SurgerySarah KemalasariNo ratings yet
- Kereiakes - JACC - 1996 - 27 (3) - 536-42 - Dose-Finding Study in PCIDocument7 pagesKereiakes - JACC - 1996 - 27 (3) - 536-42 - Dose-Finding Study in PCIPrayaas GoupNo ratings yet
- Non Analgesic BenefitDocument11 pagesNon Analgesic Benefitajay kumarNo ratings yet
- Impact of Hemodialysis On Bleeding Tendency in End Stage Renal DiseaseDocument7 pagesImpact of Hemodialysis On Bleeding Tendency in End Stage Renal DiseasedrosabryNo ratings yet
- Uso Milrinone VasoespasmoDocument7 pagesUso Milrinone VasoespasmoHernando CastrillónNo ratings yet
- Seizure Txa 1Document9 pagesSeizure Txa 1PeriUmardianaNo ratings yet
- Ehv 217Document8 pagesEhv 217Said Qadaru ANo ratings yet
- Anticoagulant: Problems WithDocument7 pagesAnticoagulant: Problems WithMand BadyNo ratings yet
- Joung2007-BM Mononuclear Cells - MIDocument11 pagesJoung2007-BM Mononuclear Cells - MIiulia andreeaNo ratings yet
- Slide Coagulopathy TiffanyDocument30 pagesSlide Coagulopathy TiffanyAgatha TiffanyNo ratings yet
- Adrenal Cortical Oncocytoma Mimicking PheocromocitomaDocument4 pagesAdrenal Cortical Oncocytoma Mimicking Pheocromocitomatitelascosminas6No ratings yet
- Outcome of Septal Dermoplasty in Patients With Hereditary Hemorrhagic TelangiectasiaDocument5 pagesOutcome of Septal Dermoplasty in Patients With Hereditary Hemorrhagic TelangiectasiaalecsaNo ratings yet
- Biokinetic of Tc99m-TetrofosminDocument7 pagesBiokinetic of Tc99m-TetrofosminKhairul AimanNo ratings yet
- Jurnal VaskularDocument5 pagesJurnal VaskulardrelvNo ratings yet
- Rodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsDocument9 pagesRodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsSyahpikal SahanaNo ratings yet
- No-Reflow Phenomenon: DR - Surinder S HansraDocument17 pagesNo-Reflow Phenomenon: DR - Surinder S HansrasshansraNo ratings yet
- Korean QX Total Pulm Veins 2010Document5 pagesKorean QX Total Pulm Veins 2010Dr. LicónNo ratings yet
- Circulating Microvesicles in Convalescent Ischemic Stroke Patients: A Contributor To High-On-Treatment Residual Platelet Reactivity?Document7 pagesCirculating Microvesicles in Convalescent Ischemic Stroke Patients: A Contributor To High-On-Treatment Residual Platelet Reactivity?Nasdı BabayevaNo ratings yet
- Trombektomi Mekanikal Pada Stroke Iskemik Dengan Awitan Kurang Dari 6 JamDocument7 pagesTrombektomi Mekanikal Pada Stroke Iskemik Dengan Awitan Kurang Dari 6 JamayunaNo ratings yet
- Dental Update 2004. Management of Dental Patients On Warfarin Therapy in A Primary Care SettingDocument5 pagesDental Update 2004. Management of Dental Patients On Warfarin Therapy in A Primary Care Settingdeepak sharmaNo ratings yet
- Conclusion: Long-Term Follow-Up ForDocument31 pagesConclusion: Long-Term Follow-Up ForHima HuNo ratings yet
- Manual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceDocument9 pagesManual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceArdiana FirdausNo ratings yet
- DTN 6 MinutesDocument4 pagesDTN 6 Minutesankur vermaNo ratings yet
- Izumihara 2005Document5 pagesIzumihara 2005CARLOS SANTIAGO PEREZ RODRIGUEZNo ratings yet
- Jdapm 22 61Document5 pagesJdapm 22 61andre krysaNo ratings yet
- Efficacy of Platelet Gel in Reconstructive Bone Surgery: M F, MD P D, MD I F, S D M D G, MD R A, MDDocument3 pagesEfficacy of Platelet Gel in Reconstructive Bone Surgery: M F, MD P D, MD I F, S D M D G, MD R A, MDAnsh Veer ChouhanNo ratings yet
- Early Postoperative ComplicationsDocument6 pagesEarly Postoperative Complications49hr84j7spNo ratings yet
- Volatile Anaesthetic Myocardial Protection: A Review of The Current LiteratureDocument5 pagesVolatile Anaesthetic Myocardial Protection: A Review of The Current Literatureserena7205No ratings yet
- Exercise 6 Crossmatch: Exercise 6 Laboratory Procedure ManualDocument14 pagesExercise 6 Crossmatch: Exercise 6 Laboratory Procedure ManualEmad ManniNo ratings yet
- Pt. Jakarta Kyoai Medical Center (TEL: 572-4330 FAX: 572 - 4331)Document1 pagePt. Jakarta Kyoai Medical Center (TEL: 572-4330 FAX: 572 - 4331)Annisa SeptyaniNo ratings yet
- Diagnosis and Treatment DVTDocument7 pagesDiagnosis and Treatment DVT최연기No ratings yet
- Acute Infectious Purpura FulminansDocument15 pagesAcute Infectious Purpura FulminansFranklin Aranda100% (2)
- Adsorbed PlasmaDocument3 pagesAdsorbed PlasmaDevi OktaviannyNo ratings yet
- An Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownDocument35 pagesAn Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownAmmaarah IsaacsNo ratings yet
- Physio - Chapter 37Document4 pagesPhysio - Chapter 37Regina Ysabel SartagudaNo ratings yet
- HistologyDocument77 pagesHistologyRahul0% (1)
- Protocol For The Preparation of Blood Plasma and SerumDocument2 pagesProtocol For The Preparation of Blood Plasma and Serummakis_sigalasNo ratings yet
- @teamfunnymewat: Rank Booster Test SeriesDocument33 pages@teamfunnymewat: Rank Booster Test SeriesKirtan shuklaNo ratings yet
- Mak Roo 2018Document7 pagesMak Roo 2018my accountNo ratings yet
- Von Willebrand DiseaseDocument4 pagesVon Willebrand DiseaseJohannah DaroNo ratings yet
- Apheresis PrincipleDocument68 pagesApheresis Principlemelisa asibalNo ratings yet
- Blood Clotting Mechanism: Teri Junge, CST, CfaDocument7 pagesBlood Clotting Mechanism: Teri Junge, CST, CfaPoppy ChetriNo ratings yet
- PDF Anemia Concept Map0000Document1 pagePDF Anemia Concept Map0000alvianmerzaradiputraNo ratings yet
- Blood Banking MT1ADocument10 pagesBlood Banking MT1ALeoPaulNo ratings yet
- Acog Practice Bullet In: Management of Alloimmunization During PregnancyDocument9 pagesAcog Practice Bullet In: Management of Alloimmunization During PregnancyTatiiana ZpiitiiaNo ratings yet
- Lec.3 PhlebetomyDocument2 pagesLec.3 PhlebetomyQudamah JasemNo ratings yet
- Plateletcrit As A Screening Tool For Detection of Platelet Quantitative DisordersDocument5 pagesPlateletcrit As A Screening Tool For Detection of Platelet Quantitative DisordersStephanie PattonNo ratings yet
- Laboratory Test Report: Test Name Result Biological Reference Interval ABO Group: RH Typing: MethodDocument1 pageLaboratory Test Report: Test Name Result Biological Reference Interval ABO Group: RH Typing: MethodPrathapuramnarasimhacharyuluNo ratings yet
- Pengaruh Isobutil Metilxantina (IMX) Dan Waktu Pemisahan Terhadap Kualitas Dan Efektifitas Pemisahan Spermatozoa Dengan Metode Kolom Albumin TelurDocument6 pagesPengaruh Isobutil Metilxantina (IMX) Dan Waktu Pemisahan Terhadap Kualitas Dan Efektifitas Pemisahan Spermatozoa Dengan Metode Kolom Albumin Telurparkc6922No ratings yet
- Orca Share Media1668581887938 6998539686907204385Document5 pagesOrca Share Media1668581887938 6998539686907204385Mavrix AgustinNo ratings yet
- Abcd 20759Document1 pageAbcd 20759vaibhav shuklaNo ratings yet
- WhatsApp Image 2023-04-03 at 12.26.59 AMDocument1 pageWhatsApp Image 2023-04-03 at 12.26.59 AMjogendra ponnamandaNo ratings yet
- Anatomy Module 17Document23 pagesAnatomy Module 17JayR MendonesNo ratings yet
- Haematology Laboratory User Handbook - Updated July 2020 JWDocument25 pagesHaematology Laboratory User Handbook - Updated July 2020 JWBassam AlharaziNo ratings yet
- RLCDocument6 pagesRLCPrabhakar BharatamNo ratings yet
- Anatomy and Physiology II - Blood Basics - (Week 3) Flashcards - QuizletDocument7 pagesAnatomy and Physiology II - Blood Basics - (Week 3) Flashcards - QuizletDani AnyikaNo ratings yet
- Information For Patients Needing Irradiated BloodDocument8 pagesInformation For Patients Needing Irradiated BloodCaddy MkaNo ratings yet