Professional Documents
Culture Documents
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Uploaded by
Kevin TapiasCopyright:
Available Formats
You might also like
- Chapter 1 Part 1 Fill in The BlankDocument2 pagesChapter 1 Part 1 Fill in The BlankArlanosaurusNo ratings yet
- Drug Efficacy in The Treatment of Antipsychotic-Induced Akathisia A Systematic Review and Network Meta-AnalysisDocument9 pagesDrug Efficacy in The Treatment of Antipsychotic-Induced Akathisia A Systematic Review and Network Meta-AnalysisalejabotiarNo ratings yet
- Bahji 2020Document31 pagesBahji 2020Abdul Mannan ChatthaNo ratings yet
- Comparative Efficacy and Acceptability of Psychotherapies For Panic Disorder With or Without Agoraphobia Systematic Review and Network Meta Analysis of Randomised Controlled TrialsDocument13 pagesComparative Efficacy and Acceptability of Psychotherapies For Panic Disorder With or Without Agoraphobia Systematic Review and Network Meta Analysis of Randomised Controlled TrialsLOLUIZNo ratings yet
- Jamapsychiatry Papola 2023 Oi 230080 1697118575.84256Document11 pagesJamapsychiatry Papola 2023 Oi 230080 1697118575.84256Renan CruzNo ratings yet
- 1 s2.0 S1525505019311011 MainDocument5 pages1 s2.0 S1525505019311011 MainilonaskorinNo ratings yet
- Gedin 2022 Oi 221233 1668781352.25734Document12 pagesGedin 2022 Oi 221233 1668781352.25734Dragutin PetrićNo ratings yet
- BMJ 2023 078084.fullDocument14 pagesBMJ 2023 078084.fulljayswalrameshNo ratings yet
- jiang et al 2023 pharmacological and behavioral interventions for fatigue in parkinson s disease a meta analysis of (科研通 ablesci.com)Document9 pagesjiang et al 2023 pharmacological and behavioral interventions for fatigue in parkinson s disease a meta analysis of (科研通 ablesci.com)Pei-Hao ChenNo ratings yet
- Appi Focus 16407Document10 pagesAppi Focus 16407MARIALEJ PEREZ MONTALVANNo ratings yet
- Barrionuevo 2018Document7 pagesBarrionuevo 2018hlwNo ratings yet
- Association Between Physical Activity and Risk of Depression A Systematic Review and Meta-AnalysisDocument10 pagesAssociation Between Physical Activity and Risk of Depression A Systematic Review and Meta-AnalysisAna Margarida J. - PsicólogaNo ratings yet
- Light Therapy For Non Seasonal Depression Systematic Review and Meta AnalysisDocument11 pagesLight Therapy For Non Seasonal Depression Systematic Review and Meta AnalysisGabriel VinhattiNo ratings yet
- Comparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisDocument10 pagesComparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisCarolina PradoNo ratings yet
- Fpsyt 11 608896Document20 pagesFpsyt 11 608896shumailaNo ratings yet
- 1 s2.0 S2215036623001992Document13 pages1 s2.0 S2215036623001992Jorge SalazarNo ratings yet
- Review ArticleDocument9 pagesReview ArticleMuhammad YanazNo ratings yet
- Hype or Hope? High Placebo Response in Major Depression Treatment With Ketamine and Esketamine: A Systematic Review and Meta-AnalysisDocument11 pagesHype or Hope? High Placebo Response in Major Depression Treatment With Ketamine and Esketamine: A Systematic Review and Meta-Analysisservicio psiquiatría HCHNo ratings yet
- Hubungan Antara Gejala Depresi Dokter Dan Kesalahan MedisDocument14 pagesHubungan Antara Gejala Depresi Dokter Dan Kesalahan MedisMaikel PakageNo ratings yet
- Artigo Lancet Medicamentos AnsiedadeDocument10 pagesArtigo Lancet Medicamentos AnsiedadeRebecca DiasNo ratings yet
- Magnitude of The Placebo Response Across Treatment Modalities Used For Treatment-Resistant Depression in Adults A Systematic Review and Meta-AnalysisDocument18 pagesMagnitude of The Placebo Response Across Treatment Modalities Used For Treatment-Resistant Depression in Adults A Systematic Review and Meta-AnalysisUSFMFPNo ratings yet
- Medicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaDocument5 pagesMedicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaJoão PauloNo ratings yet
- Medi-100-E27653Document7 pagesMedi-100-E27653Rika TriwardianiNo ratings yet
- Cognitive-Behavioral Therapy For Treating Hypertension: A Systematic Review and Meta-Analysis: PsychDocument1 pageCognitive-Behavioral Therapy For Treating Hypertension: A Systematic Review and Meta-Analysis: PsychJames BalamesNo ratings yet
- Opioid-Sparing Effect of Cannabinoids For AnalgesiaDocument16 pagesOpioid-Sparing Effect of Cannabinoids For Analgesia幸福KoreaNo ratings yet
- Jama Association Between Physical Activity and Risk of DepressionDocument10 pagesJama Association Between Physical Activity and Risk of DepressiongbfascNo ratings yet
- Ketamine NNTDocument8 pagesKetamine NNTBrent AllieNo ratings yet
- The Efficacy and Safety of Diterpene Ginkgolides.17Document11 pagesThe Efficacy and Safety of Diterpene Ginkgolides.17drfperezNo ratings yet
- Metanalise Antidepressivos 2015 PDFDocument18 pagesMetanalise Antidepressivos 2015 PDFFábio C NetoNo ratings yet
- Lee 2018Document24 pagesLee 2018Eliana RieraNo ratings yet
- Gómez-García 2016Document10 pagesGómez-García 2016Rafaela Queiroz MascarenhasNo ratings yet
- Anticonvulsivantes 2018Document8 pagesAnticonvulsivantes 2018ps.ericavillarroelNo ratings yet
- Chen 2021Document13 pagesChen 2021Aitor UzkudunNo ratings yet
- 2022 de VriesDocument8 pages2022 de Vriesmvillar15_247536468No ratings yet
- A Systematic Review and Network Meta-Analysis On Comparative Efficacy, Acceptability, and Safety of Treatments in Acute Bipolar Mania in YouthsDocument14 pagesA Systematic Review and Network Meta-Analysis On Comparative Efficacy, Acceptability, and Safety of Treatments in Acute Bipolar Mania in YouthsDiego HormacheaNo ratings yet
- Efficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisDocument6 pagesEfficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisChica MirandaNo ratings yet
- Hengartner 2017Document7 pagesHengartner 2017Julio JuarezNo ratings yet
- Articulo Sesion Bibliografica Vie. 5 Abril 2024 Dr. Alejandra G. Gonzalez RiiiDocument12 pagesArticulo Sesion Bibliografica Vie. 5 Abril 2024 Dr. Alejandra G. Gonzalez Riiijadebelen29No ratings yet
- Courtney - 2022 - Oi - 211279 - 1643056684.29546 1Document22 pagesCourtney - 2022 - Oi - 211279 - 1643056684.29546 1U of T MedicineNo ratings yet
- Relapse Rates With Paliperidone Palmitate in AdultDocument11 pagesRelapse Rates With Paliperidone Palmitate in AdultdryaeonNo ratings yet
- Efficacy and Safety of Aspirin As An Adjunctive Therapy in TubercularDocument7 pagesEfficacy and Safety of Aspirin As An Adjunctive Therapy in TubercularYunita WidyaningsihNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundPsiquiatría CESAMENo ratings yet
- Nejmoa 2206443Document12 pagesNejmoa 2206443Bryan PalmaNo ratings yet
- Headache 2024 Robblee The 2023 Protocol For Update To Acute TreatmentDocument4 pagesHeadache 2024 Robblee The 2023 Protocol For Update To Acute TreatmentJaqueline CarvalhoNo ratings yet
- Jurnal Reading 2Document6 pagesJurnal Reading 2dezafarista_44587428No ratings yet
- Real-Life Clinical Experience With Cariprazine - A Systematic Review of Case StudiesDocument17 pagesReal-Life Clinical Experience With Cariprazine - A Systematic Review of Case Studiesbelloilportogallo99No ratings yet
- Z Al-Roubaie - 2020Document12 pagesZ Al-Roubaie - 2020Kossay ZaouiNo ratings yet
- ผลัดที่2 6101769 ปภัสรา JCDocument69 pagesผลัดที่2 6101769 ปภัสรา JCpapatsaraNo ratings yet
- Xu 2020Document10 pagesXu 2020Risky PerdanaNo ratings yet
- ketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-reviewDocument12 pagesketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-reviewNuno TorresNo ratings yet
- Antipsychotics For Preventing Delirium in Hospitalized AdultsDocument12 pagesAntipsychotics For Preventing Delirium in Hospitalized AdultsLuis CsrNo ratings yet
- Wakeman 2020 Oi 190774Document12 pagesWakeman 2020 Oi 190774Yed HeeNo ratings yet
- Comparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainDocument15 pagesComparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainRachel PutriNo ratings yet
- In-Silico Studies in Herbal Drugs: A ReviewDocument5 pagesIn-Silico Studies in Herbal Drugs: A ReviewShihan SilvaNo ratings yet
- Biologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysisDocument14 pagesBiologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysislilingNo ratings yet
- bmj.n2321.fullDocument16 pagesbmj.n2321.fulljairo canlasNo ratings yet
- Complementary Therapies in Clinical PracticeDocument7 pagesComplementary Therapies in Clinical PracticeBkash ShahNo ratings yet
- Journal of Affective Disorders: Review ArticleDocument11 pagesJournal of Affective Disorders: Review Article賀立安No ratings yet
- Medicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionDocument5 pagesMedicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionaditNo ratings yet
- Medical Cannabis For The Treatment of DementiaDocument24 pagesMedical Cannabis For The Treatment of DementiaLorina BoligNo ratings yet
- Your Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022From EverandYour Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022No ratings yet
- Nursing Performance Checklist TracheostomyDocument3 pagesNursing Performance Checklist TracheostomySyahrilKiyai100% (1)
- Homeless Deaths ReportDocument102 pagesHomeless Deaths ReportCapital Public RadioNo ratings yet
- Unit 3 Integumentary System Pathological ConditionsDocument43 pagesUnit 3 Integumentary System Pathological Conditionsalmira garciaNo ratings yet
- The Role of The Clinical SupervisorDocument52 pagesThe Role of The Clinical SupervisorDwi NopriyantoNo ratings yet
- Non-Pharmacological Treatment of HypertensionDocument25 pagesNon-Pharmacological Treatment of Hypertensionastrid abrahams0% (2)
- PACS QuestionnaireDocument4 pagesPACS QuestionnaireakashniranjaneNo ratings yet
- Cleft Lip and PalateDocument18 pagesCleft Lip and Palateicywitch100% (1)
- Rajsthan All Surgical Distributor Data ListDocument33 pagesRajsthan All Surgical Distributor Data ListcatalogueNo ratings yet
- Medical & Homeopathic Research, Homeopathic Medical Collage and ResearchDocument145 pagesMedical & Homeopathic Research, Homeopathic Medical Collage and ResearchMitesh KinariwalaNo ratings yet
- Sumu PDFDocument30 pagesSumu PDFalokpalreshaNo ratings yet
- Alejandro Oet Listening PracticeDocument12 pagesAlejandro Oet Listening PracticeChapa BandaraNo ratings yet
- Pivot 4a Lesson Exemplar in Mapeh 6Document7 pagesPivot 4a Lesson Exemplar in Mapeh 6Crisente BarcelonNo ratings yet
- Administration of Topical MedicationsDocument14 pagesAdministration of Topical MedicationsgireeshsachinNo ratings yet
- Module 2Document14 pagesModule 2Muskaan BindalNo ratings yet
- Test Bank For Pathophysiology 6th Edition Jacquelyn L BanasikDocument5 pagesTest Bank For Pathophysiology 6th Edition Jacquelyn L BanasikJesus Carter97% (38)
- Laughter PrescriptionDocument4 pagesLaughter PrescriptionJair Andres Falla AldanaNo ratings yet
- Cultural Humility Versus Cultural Competence - A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education (3) - 0Document10 pagesCultural Humility Versus Cultural Competence - A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education (3) - 0Gabriela BarreiraNo ratings yet
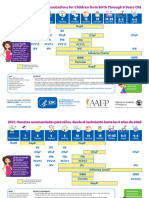
- VACCINES Eng Spa 0 To 6 Years ScheduleDocument4 pagesVACCINES Eng Spa 0 To 6 Years ScheduleMaría del Mar OrtizNo ratings yet
- Bethesda Handbook of HematologyDocument5 pagesBethesda Handbook of HematologyjosephNo ratings yet
- Bioterrorism: An Overview: Rick Roman, M.H.S.ADocument43 pagesBioterrorism: An Overview: Rick Roman, M.H.S.ANurhasan Agung PrabowoNo ratings yet
- Moot Court BrochureDocument16 pagesMoot Court BrochureAkashNo ratings yet
- Unconsciousness: Anil PatidarDocument29 pagesUnconsciousness: Anil Patidarjinal sutharNo ratings yet
- AtpdDocument48 pagesAtpddrkadiyala2100% (2)
- A Roadmap To MCAT Content in Psychology and Sociology TextbooksDocument16 pagesA Roadmap To MCAT Content in Psychology and Sociology TextbooksJenny HuangNo ratings yet
- Sci006-Lev 11Document380 pagesSci006-Lev 11palak320% (1)
- NCP - BronchopneumoniaDocument11 pagesNCP - BronchopneumoniaMaria Ivy Mendoza100% (1)
- Adapted From Family Planning Competency-Based Training: Basic Course HandbookDocument4 pagesAdapted From Family Planning Competency-Based Training: Basic Course HandbookVanessa EnteroNo ratings yet
- Common Acquired and Congenital AnomaliesDocument5 pagesCommon Acquired and Congenital AnomaliesDang SaplanNo ratings yet
- COVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaDocument29 pagesCOVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaEnrita DianNo ratings yet
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Uploaded by
Kevin TapiasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Uploaded by
Kevin TapiasCopyright:
Available Formats
Original Investigation | Psychiatry
Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
A Systematic Review and Network Meta-Analysis
Cyril Gerolymos, MD; Romain Barazer, MD; Dong Keon Yon, MD, PhD; Anderson Loundou, PhD; Laurent Boyer, MD, PhD; Guillaume Fond, MD, PhD
Abstract Key Points
Question Which drugs are associated
IMPORTANCE Antipsychotic-induced akathisia (AIA) occurs in 14% to 35% of patients treated with
with the greatest efficacy in the
antipsychotics and is associated with increased suicide and decreased adherence in patients with
treatment of antipsychotic-induced
schizophrenia. However, no comprehensive review and network meta-analysis has been conducted
akathisia?
to compare the efficacy of treatments for AIA.
Findings This systematic review and
OBJECTIVE To compare the efficacy associated with AIA treatments. network meta-analysis assessed the
global akathisia score of 10 drugs in 15
DATA SOURCES Three databases (MEDLINE, Web of Science, and Google Scholar) were double-blind randomized clinical trials
systematically searched by multiple researchers for double-blind randomized clinical trials (RCTs) with 492 participants. Mirtazapine,
comparing active drugs for the treatment of AIA with placebo or another treatment between May 30 vitamin B6, and biperiden exhibited the
and June 18, 2023. 3 most favorable efficacy and tolerability
profiles; trazodone, mianserin, and
STUDY SELECTION Selected studies were RCTs that compared adjunctive drugs for AIA vs placebo propranolol demonstrated greater
or adjunctive treatment in patients treated with antipsychotics fulfilling the criteria for akathisia, efficacy than the placebo; and
RCTs with sample size of 10 patients or more, only trials in which no additional drugs were cyproheptadine, clonazepam,
administered during the study, and RCTs that used a validated akathisia score. Trials with missing data zolmitriptan, and valproate did not yield
for the main outcome (akathisia score at the end points) were excluded. significant effects.
Meaning Vitamin B6 may have the most
DATA EXTRACTION AND SYNTHESIS Data extraction and synthesis were performed, estimating
favorable efficacy and tolerability
standardized mean differences (SMDs) through pairwise and network meta-analysis with a random-
profile, followed by mirtazapine and
effects model. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)
biperiden, for the treatment of
guideline was followed.
antipsychotic-induced akathisia.
MAIN OUTCOMES AND MEASURES The primary outcome was the severity of akathisia measured
by a validated scale at the last available end point. + Supplemental content
Author affiliations and article information are
RESULTS Fifteen trials involving 492 participants compared 10 treatments with placebo. listed at the end of this article.
Mirtazapine (15 mg/d for ⱖ5 days; SMD, −1.20; 95% CI, −1.83 to −0.58), biperiden (6 mg/d for ⱖ14
days; SMD, −1.01; 95% CI, −1.69 to −0.34), vitamin B6 (600-1200 mg/d for ⱖ5 days; SMD, −0.92;
95% CI, −1.57 to −0.26), trazodone (50 mg/d for ⱖ5 days; SMD, −0.84; 95% CI, −1.54 to −0.14),
mianserin (15 mg/d for ⱖ5 days; SMD, −0.81; 95% CI, −1.44 to −0.19), and propranolol (20 mg/d for
ⱖ6 days; SMD, −0.78; 95% CI, −1.35 to −0.22) were associated with greater efficacy than placebo,
with low to moderate heterogeneity (I2 = 34.6%; 95% CI, 0.0%-71.1%). Cyproheptadine,
clonazepam, zolmitriptan, and valproate did not yield significant effects. Eight trials were rated as
having low risk of bias; 2, moderate risk; and 5, high risk. Sensitivity analyses generally confirmed the
results for all drugs except for cyproheptadine and propranolol. No association between effect sizes
and psychotic severity was found.
(continued)
Open Access. This is an open access article distributed under the terms of the CC-BY License.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 1/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Abstract (continued)
CONCLUSIONS AND RELEVANCE In this systematic review and network meta-analysis,
mirtazapine, biperiden, and vitamin B6 were associated with the greatest efficacy for AIA, with
vitamin B6 having the best efficacy and tolerance profile. Trazodone, mianserin, and propranolol
appeared as effective alternatives with slightly less favorable efficacy and tolerance profiles. These
findings should assist prescribers in selecting an appropriate medication for treating AIA.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527
Introduction
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines akathisia as
“subjective complaints of restlessness, often accompanied by objective excessive movements (such
as continuous leg movements, rocking from foot to foot, pacing, or an inability to sit down and
remain still).”1 This movement disorder primarily occurs in patients treated with antipsychotics,
where it is known as antipsychotic-induced akathisia (AIA). A meta-analysis2 published in 2019 that
compared the tolerability of 32 antipsychotics concluded that first-generation antipsychotics carry a
higher risk of inducing akathisia compared with second-generation antipsychotics, with risks ranging
from 24-fold (zuclopenthixol, a first-generation antipsychotic) to 1.9-fold (aripiprazole, a second-
generation antipsychotic). Overall, the prevalence of AIA ranges from 14% to 35% based on studies
involving patients treated with antipsychotics.3-7 This adverse effect has significant clinical
implications, including an increased risk of suicide (which is the primary cause of mortality in early
schizophrenia) and nonadherence to treatment (which is the primary cause of relapse).8
The primary clinical recommendations for treating AIA are to consider antipsychotic
monotherapy, to reduce the antipsychotic dose, and/or to switch to an antipsychotic associated with
a lower risk of akathisia.9 However, these options are not always feasible in clinical practice, and
addressing akathisia remains challenging in many cases. Therefore, the use of adjunctive drugs is
necessary to alleviate AIA. Because of the lack of comprehensive network meta-analyses that
examine the efficacy of treatments in alleviating akathisia, we performed a meta-analysis to examine
the efficacy of drugs in treating AIA. A secondary objective was to assess the acceptability (defined
as the proportion of dropout due to tolerance issues) and tolerability (defined by the frequency of
adverse events) of each drug.
Methods
This study follows the 2020 Preferred Reporting Items for Systematic Reviews and Meta-analyses
(PRISMA) reporting guideline.10 The protocol has been registered in PROSPERO (CRD42023431136)
without any amendments to the provided information.
Study Eligibility Criteria
Two authors (R.B. and G.F.) searched 3 databases (MEDLINE, Web of Science, and Google Scholar)
from inception, with no language restriction. In case of no consensus on the inclusion of a study, a
third author (L.B.) made the final decision about study inclusion. The systematic review began on
May 30, 2023, and ended on June 18, 2023. The search terms were as follows: akathisia AND
antipsychotic OR neuroleptic OR schizophrenia OR schizoaffective disorder combined with a list of the
different adjunctive drugs. A second search was performed for each drug identified in the first
search: biperiden, clonazepam, cyproheptadine, diazepam, diphenhydramine, mianserin, mirtazapine,
propranolol, trazodone, valproate, vitamin B6, and zolmitriptan. Each drug term was combined with
the term akathisia. The search identified 847 records.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 2/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Inclusion criteria were as follows: randomized clinical trials (RCTs) that (1) compared an
adjunctive drug for AIA vs placebo or adjunctive treatment in patients treated with antipsychotics
fulfilling the criteria for akathisia, (2) had sample sizes of at least 10 patients, (3) had no additional
drugs administered during the study, and (4) used a validated akathisia score. Trials with missing data
for the main outcome (akathisia score at the 2 end points) were excluded.
Outcomes
Our primary outcome was the reduction of the mean akathisia score on the last time point with a
scale assessing global, subjective, and/or objective akathisia. When repeated assessment time points
were recorded, we chose the longest one. For crossover trials, the last scores at the end of the first
period were analyzed. Secondary outcomes were tolerance, defined as the total number of adverse
effects and the total number of serious adverse effects reported at the end of the trial, and
acceptability, defined as the number of dropouts after randomization for tolerance issues (if the
reasons for dropout were not available, the total number of dropouts was included).
Data Extraction
All records were screened and extracted by 2 researchers (R.B. and C.G.). Disagreements were
resolved through discussion with a third author (G.F.). The secondary outcomes were extracted
through the trials, namely, the total number of patients experiencing adverse effects and dropouts.
Percentages relative to the total number of participants in the network meta-analysis are presented.
Twenty-seven baseline characteristics were extracted and are presented in the eMethods in
Supplement 1.
Risk of Bias
We assessed the risk of bias for individual studies according to the Cochrane Handbook for Systematic
Reviews of Interventions using the Risk of Bias 2 tool.11 More details on identification and selection of
studies, outcomes, data extraction, missing data, risk of bias, and the details of statistical analyses are
presented in the eMethods in Supplement 1.
Statistical Analysis
We estimated standardized mean differences (SMDs) and their respective SEs for continuous
outcome using pairwise and network meta-analysis. If the total sample size was 20 or fewer patients,
a Hedges g (SMD) correction was applied.12 If not, a Cohen d (SMD) was calculated. The different
effect sizes were compiled using a frequentist random-effects network meta-analysis model, and
95% CIs are presented. Pooled weights for each intervention were calculated from pairwise
comparisons model.13 Results were resumed in a forest plot and a league table.
The statistical heterogeneity of our model was assessed with I2 and τ2.14,15 A Cochran Q test16
was conducted for overall heterogeneity and inconsistency. The ranking of treatments is presented
through P-score based on the random-effects model. Surface under the cumulative ranking curve
(SUCRA) has been used for the rankogram. To examine the transitivity assumption, we listed relevant
sociodemographic and clinical factors and compared them by means of boxplots. Tests and 2-sided
P value threshold for statistical significance were as follows: Cochran Q test P < .05, Separate Indirect
From Direct Evidence (SIDE) test P < .10, and Egger test, Pustejovsky-Rodgers corrected test, and
Thompson-Sharp test P < .05. All statistical analyses were performed using the netmeta package
(version 2.8-2) in R software, version 4.1.3 (R Project for Statistical Computing).17
Results
Selection, Inclusion, and Characteristics of Studies
Figure 1 illustrates the flowchart of the study analysis. Of the 847 records identified initially in the
databases, we selected 15 double-blind RCTs (1.8%) that met the inclusion criteria for a network
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 3/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
meta-analysis.18-32 The excluded studies and reasons for exclusion are presented in eTable 1 in
Supplement 1.
The 15 included RCTs consist of 10 parallel group trials (66.7%),19-22,26-30,323 crossover trials
(20.0%),18,24,25 and 3 multiarm studies (20.0%)23,25,31 (1 trial has both crossover and multiarm
designs). A total of 492 patients are included, with 324 patients (65.9%) allocated to the
experimental arms and 168 patients (34.1%) to the placebo arm. The placebo acted as the reference
group in 12 studies (80.0%),18,19,21,23-31 whereas in 3 studies (20.0%),20,22,32 an active treatment
served as the reference group (2 studies used propranolol, and 1 study used diphenhydramine). The
RCTs used 5 scores: Barnes Akathisia Rating Scale, Akathisia Rating Scale, Simpson Angus Scale, and 2
scores based on the DSM-5 criteria for akathisia. The descriptions of these scales and the
characteristics of the trials can be found in eTable 2 in Supplement 1.
Regarding the risk of bias assessment, 13 studies (86.7%)18-21,23-32 reported an adequate
randomization process, 12 studies (80.0%)19-21,23-31 did not present any deviations from intended
interventions, 11 studies (73.3%)18-21,24-28,30,31 dealt properly with missing outcome data, 12 studies
(80.0%)18-21,24-28,30,31 used an appropriate way to measure outcome, and 13 studies
(86.7%)18-28,30,31 reported the full results without any selection. Eight studies
(53.3%)19-21,24,25,27,30,31 were at overall low risk of bias and met all the quality criteria, 12 studies
(80.0%)18-21,23-28,30,31 met at least 4 quality criteria, and 13 studies (86.7%)18-21,23-31 met at least 3
quality criteria. Two studies (13.3%)18,26 presented some concerns, whereas 5 studies
(33.3%)22,23,28,29,32 were categorized as high risk of bias. Figure 2 provides details of the risk of bias
assessment.
Network Graph
The network graph is presented in Figure 3. One study22 was excluded from the main network due
to the absence of a comparison linking diazepam or diphenhydramine with other treatments or
placebo in the network, leaving 14 trials in the main network. Individual effect size and calculation for
the study by Gagrat et al22 are described in eTable 3 in Supplement 1. Despite the limited number of
Figure 1. Study Selection Process
847 Records identified from databases
67 MEDLINE
676 Web of Science
104 Google Scholar
828 Excluded
424 Case reports or open trials
376 Missing data on assessment
or randomization
21 Systematic reviews
6 Sample size <10
1 Other treatments that would
skew results
847 Records screened
19 Reports sought for retrieval
3 Reports not retrieved
16 Reports assessed for eligibility
1 Excluded (sample did not match
target population)
15 Studies included in the quantitative Overall, 15 double-blind randomized clinical trials
meta-analysis
corresponding to 12 interventions were included.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 4/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
trials, the network demonstrated overall strong connectivity. The most frequently studied
comparisons involved propranolol, mirtazapine, mianserin, vitamin B6, biperiden, and the placebo
control condition. Cyproheptadine, clonazepam, and zolmitriptan had weak connections within the
network, with only 1 direct comparison each.
eTable 4 in Supplement 1 summarizes the characteristics of the interventions initially included
in the network. In descending order, the placebo, propranolol, mirtazapine, mianserin, vitamin B6,
and biperiden arms account for the highest number of participants.
Network Meta-Analysis for Efficacy
Figure 4 illustrates that the following medications were associated with significantly greater efficacy
than placebo in the treatment of AIA: mirtazapine (15 mg/d for ⱖ5 days; SMD, −1.20; 95% CI, −1.83
to −0.58), biperiden (6 mg/d for ⱖ14 days; SMD, −1.01; 95% CI, −1.69 to −0.34), vitamin B6 (600-
1200 mg/d for ⱖ5 days; SMD, −0.92; 95% CI, −1.57 to −0.26), trazodone (50 mg/d for ⱖ5 days; SMD,
Figure 2. Risk of Bias Assessment for the 15 Studies Included in the Network Meta-Analysis
Study
Gagrat et al,22 1978
Adler et al,18 1986
Friis et al,25 1983
Kramer et al,24 1988
Pujalte et al,19 1994
Poyurovsky et al,29 1999
Miodownik et al,31 2006
Lerner et al,30 2004
Poyurovsky et al,23 2006
Baskak et al,26 2007
Avital et al,32 2009
Stryjer et al,28 2010
Shams-Alizadeh et al,27 2020
Low risk Some concerns High risk Randomization Deviations from the Missing Measurement of Selection of the Overall
process intended interventions outcome data the outcome reported result
Figure 3. Network Graph for Main Results of Meta-Analysis
Cyproheptadine
Clonazepam
Mianserin
Biperiden
Mirtazapine 11
11
22
22
1
11
1 22
22 11
11 Node size is proportional to the total number of
22
22 patients for each intervention. Line thickness is
Zolmitriptan
proportional to weight from the random-effects
1
11
1
11
11 model. The number overlying the lines is equal to the
number of studies corresponding to the comparison.
Placebo 1
22
22 11
1 Triangles represent comparisons for 3-arm studies.
333 Colors of the nodes represent the therapeutic classes
11
11 Vitamin B6 of intervention: β-blocker (propranolol),
22
22
antidepressant (mirtazapine, mianserin, and
trazodone), mood stabilizer (valproate),
Propranolol
anticholinergic (biperiden), antihistaminic
Valproate (cyproheptadine), benzodiazepine (clonazepam), and
Trazodone triptan (zolmitriptan).
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 5/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
−0.84; 95% CI, −1.54 to −0.14), mianserin (15 mg/d for ⱖ5 days; SMD, −0.81; 95% CI, −1.44 to −0.19),
and propranolol (20 mg/d for ⱖ6 days; SMD, −0.78; 95% CI, −1.35 to −0.22) were associated with
greater efficacy than placebo, with low to moderate heterogeneity (I2 = 34.6%; 95% CI, 0.0%-71.1%).
However, cyproheptadine (16 mg/d), clonazepam (0.5-2.5 mg/d), zolmitriptan (7.5 mg/d), and
valproate (1700 mg/d) did not show a significant difference compared with placebo. The SMDs
ranged from −1.20 (95% CI, −1.83 to −0.58) for mirtazapine to −0.18 (95% CI, −1.05 to 0.69) for
valproate. The between-study heterogeneity was estimated at τ2 = 0.0907 (95% CI, 0.0-0.30).
In Figure 5, the head-to-head comparisons of the efficacy of the 10 included treatments and
placebo are presented in order of ranking. None of the network estimates comparing active
treatments reached statistical significance (all 95% CIs of SMDs contain the value 0). There was no
direct evidence comparing cyproheptadine or zolmitriptan with placebo because the trials evaluating
these drugs did not include placebo as a reference group. Only biperiden demonstrated greater
efficacy than valproate (SMD, −0.99; 95% CI, −1.93 to −0.04). There was no significant difference in
efficacy between propranolol and zolmitriptan, cyproheptadine and propranolol, mirtazapine and
propranolol, or vitamin B6 and mianserin.
eFigure 2 in Supplement 1 provides a summary of the ranking using SUCRA. The top 5 ranked
molecules for treating AIA, in decreasing order of probability, are mirtazapine, biperiden, vitamin B6,
cyproheptadine, and trazodone. Mirtazapine had a 33.4% probability of being the top-ranked
molecule, whereas propranolol had a 16.4% probability of being ranked seventh (eTable 5 in
Supplement 1). The P-scores support these findings, ranking mirtazapine (P-score = 0.826),
biperiden (P-score = 0.703), and vitamin B6 (P-score = 0.641) as the 3 most effective therapies for
treating AIA (eFigure 1 in Supplement 1). The results for the efficacy at different time points and the
efficacy on subjective and objective symptoms are presented in the eResults in Supplement 1.
Consistency of the Network and Reporting Bias
We did not find any evidence of inconsistency regarding the SIDE test. None of the 8 comparisons
between direct and indirect evidence reached significance (eTable 6 in Supplement 1). The forest
plot, which separates direct and indirect evidence (eFigure 3 in Supplement 1), revealed that the
network comparison with the most influence on heterogeneity (73%) was propranolol vs placebo.
The proportion of direct and indirect comparisons for each face-to-face intervention is presented in
eFigure 4 in Supplement 1.
Funnel plot analysis did not indicate any skewness (eFigure 5 in Supplement 1). The statistical
significance of the Egger test was not observed. The Pustejovsky-Rodgers corrected test for
Figure 4. Ranked Forest Plot of Network Meta-Analysis for Efficacy of Treatments
in Antipsychotic-Induced Akathisia
Favors Favors
Experimental agent SMD (95% CI) experimental placebo Weight, %
Mirtazapine –1.20 (–1.83 to –0.58) 12.21
Biperiden –1.01 (–1.69 to –0.34) 7.08
Vitamin B6 –0.92 (–1.57 to –0.26) 11.01
Cyproheptadine –0.91 (–2.01 to 0.19) 3.83
Trazodone –0.84 (–1.54 to –0.14) 10.12
Mianserin –0.81 (–1.44 to –0.19) 14.16
Propranolol –0.78 (–1.35 to –0.22) 26.00
Clonazepam –0.56 (–1.86 to 0.74) 4.17
The different treatments are compared with placebo
Zolmitriptan –0.29 (–1.40 to 0.82) 3.70
(the reference group). The more negative the
Valproate –0.18 (–1.05 to 0.69) 7.72
standardized mean difference (SMD) is, the higher the
Heterogeneity: τ2 = 0.0907; I2 = 34.6%; (0.0%-71.1%)
–2 –1 0 1 reduction in akathisia scale score for intervention
Overall Cochran test: Q = 10.70; df = 7 (P = 0.15)
SMD (95% CI) compared with placebo. Weight represents the sum of
Test for heterogeneity (within designs):
Q = 5.28; df = 2 (P = 0.07) the inverse variance of all effect sizes in the pairwise
Test for inconsistency (between designs): comparison model for respective intervention. Square
Q = 5.43; df = 5 (P = 0.37) size is proportional to weight.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 6/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
continuous effect sizes confirmed this trend along with the Thompson-Sharp test, supporting the
absence of reporting bias (eTables 7-9 in Supplement 1).
Acceptability and Tolerability
Details of the tolerability outcomes are reported in eTable 10 in Supplement 1. Significant adverse
effects reported compared with the placebo arm included drowsiness and dizziness for trazodone
and mirtazapine, hypersalivation and depression for valproate, dry mouth and sedation for biperiden
and valproate, hypotension for propranolol, and transient sedation for mianserin. Details of the
acceptability outcomes are given in eTable 11 in Supplement 1.
Transitivity Assumption
All details of the exploratory analysis of the transitivity assumption are summarized in the eResults in
Supplement 1 and detailed in eFigures 6 to 29 in Supplement 1. Except for some outliers, the
transitivity assumption was roughly met.
Sensitivity Analyses
All details regarding the effect size modifiers and subgroup analyses are presented in eFigures 30 to
57 in Supplement 1. In all subgroup analyses, mirtazapine was ranked first, and biperiden remained
in the second position for the first 2 subgroup analyses.
Discussion
This work represents the first network meta-analysis, to our knowledge, to explore the efficacy
associated with adjunctive drugs in AIA, which is a common clinical issue in psychiatric daily practice.
The following adjunctive drugs demonstrated efficacy, listed in decreasing order of effect sizes:
Figure 5. Head-to-Head Comparisons for Efficacy of the 10 Treatments in Antipsychotic-Induced Akathisia
Efficacy (direct treatment estimates) Efficacy (network estimates)
–0.17 -1.34
Mirtazapine NA NA NA NA NA NA NA NA (-2.00 to -0.68)
(–0.95 to 0.60)
-0.19 -0.99 -1.01
Biperiden NA NA NA NA NA NA NA (-1.93 to -0.04) [-1.69 to -0.34)
(-1.11 to 0.73)
-0.29 -0.10 –0.00 -0.98
Vitamin B6 NA NA NA NA NA NA (-1.67 to -0.29)
(-1.19 to 0.62) (-1.04 to 0.85) (–0.84 to 0.84)
-0.29 -0.10 -0.01 –0.13
Cyproheptadine NA NA NA NA NA NA
(-1.46 to 0.87) (-1.40 to 1.19) (-1.29 to 1.27) (–1.07 to 0.82)
-0.36 -0.17 -0.07 -0.07 -0.84
Trazodone NA NA NA NA NA (-1.54 to -0.14)
(-1.30 to 0.58) (-1.14 to 0.80) (-1.03 to 0.89) (-1.37 to 1.24)
-0.39 -0.20 -0.10 -0.10 -0.03 -0.80
Mianserin NA NA NA NA (-1.45 to -0.15)
(-1.28 to 0.50) (-1.12 to 0.72) (-0.83 to 0.62) (-1.36 to 1.17) (-0.97 to 0.91)
-0.42 -0.23 -0.13 -0.13 -0.06 -0.03 -0.49 -0.75
Propranolol NA NA (-1.33 to -0.17)
(-1.10 to 0.26) (-1.11 to 0.65) (-1.00 to 0.73) (-1.07 to 0.82) (-0.96 to 0.84) (-0.87 to 0.81) (-1.45 to 0.46)
-0.65 -0.46 -0.36 -0.35 -0.29 -0.26 -0.23 -0.56
Clonazepam NA NA (-1.86 to 0.74)
(-2.09 to 0.80) (-1.92 to 1.01) (-1.81 to 1.09) (-2.06 to 1.35) (-1.76 to 1.19) (-1.70 to 1.19) (-1.64 to 1.19)
-0.91 -0.72 -0.63 -0.62 -0.55 -0.52 -0.49 -0.27
Zolmitriptan NA NA
(-2.09 to 0.26) (-2.02 to 0.58) (-1.92 to 0.66) (-1.97 to 0.72) (-1.87 to 0.76) (-1.80 to 0.75) (-1.45 to 0.46) (-1.98 to 1.44)
-1.02 -0.83 -0.74 -0.73 -0.66 -0.63 -0.60 -0.38 -0.11 -0.33
Valproate (-1.26 to 0.60)
(-2.09 to 0.05) (-1.71 to 0.05) (-1.82 to 0.35) (-2.12 to 0.67) (-1.78 to 0.45) (-1.70 to 0.44) (-1.64 to 0.43) (-1.94 to 1.19) (-1.52 to 1.30)
-1.20 -1.01 -0.92 -0.91 -0.84 -0.81 -0.78 -0.56 -0.29 -0.18
Placebo
(-1.83 to -0.58) (-1.69 to -0.34) (-1.57 to -0.26) (-2.01 to 0.19) (-1.54 to -0.14) (-1.44 to -0.19) (-1.35 to -0.22) (-1.86 to 0.74) (-1.40 to 0.82) (-1.05 to 0.69)
Drugs are reported by decreasing rank order. Data are standardized mean differences row-defining treatment is compared with column-defining treatment. The SMDs above
(SMDs) (95% CIs). Comparisons should be read from left to right. For the lower triangle 0 favor the column-defining treatment in the lower triangle, whereas they favor the
that reports network estimates, column-defining treatment is compared with row-defining treatment in the upper triangle. NA indicates not applicable.
row-defining treatment. For the upper triangle that reports direct treatment estimates,
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 7/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
mirtazapine (15 mg/d), biperiden (2.5-15 mg/d), vitamin B6 (600 mg/d), mianserin (15 mg/d),
trazodone (100 mg/d), and propranolol (20-120 mg/d). Cyproheptadine also appeared to be
potentially effective, but data were insufficient to fully support its efficacy. Clonazepam and
valproate did not demonstrate superiority over placebo and are not currently recommended. These
results have important implications for clinical practice.
Mirtazapine, biperiden, and vitamin B6 exhibited moderate to large effect sizes with
comparable efficacy, and mirtazapine consistently ranked first in both the main analysis and all
subgroup analyses. However, mirtazapine may be poorly tolerated due to its sedative effects and the
potential for weight gain. Mianserin is also effective, similar to mirtazapine, in reducing akathisia
symptoms. This antidepressant also has a good tolerability profile except for sedation. However, 10%
to 20% of patients do not respond to mirtazapine and mianserin, which suggests that other
mechanisms, apart from serotonin blockade, may be involved in AIA.31
Vitamin B6 may be considered the best option in terms of the risk-benefit ratio for AIA
treatment. In cases involving insomnia, mirtazapine may still be the preferred choice33 for the
treatment of comorbid depressive disorder.34 Vitamin B6 has a moderate to large effect size that also
extends to different subgroup analyses. Its major potency lies in its excellent tolerability and
acceptability profile. Vitamin B6 may play a role, notably as a corrector of dopamine imbalance and a
free radical scavenger.30,31
Biperiden may be the best alternative in the event of vitamin B6 and mirtazapine failure. Its
anticholinergic action has been tested for both oral and intramuscular administration.25,26 However,
sedation occurred in 48% of cases. The effect size of intramuscular biperiden may have been
underestimated, as 1 study evaluated efficacy only 6 hours after administration,26 whereas its half-
life varies from 11 to 24 hours.35 Furthermore, biperiden has been administered at a low dose (2.5-mg
injections), which may have favored tolerance over efficacy. Higher doses and longer evaluation may
provide better efficacy. The optimal dosage for biperiden appears to be 12 mg/d, and the optimal
treatment duration is 14 days.
Trazodone is another antidepressant that has shown a significant effect. The optimal dose
appears to be 100 mg/d. The most common adverse effect associated with trazodone is drowsiness.
A limitation to its use is the absence of marketing authorization in some European countries,
including France and Denmark. Rare cases of priapism have also been reported in men treated with
trazodone.36,37 Additionally, trazodone should be avoided in men who have specific hematologic or
neurologic diseases (such as sickle cell anemia, multiple myeloma, leukemia, hypercoagulable states,
or autonomic nervous system disorders) or in men with anatomical deformations of the penis.38
Propranolol, 50 mg/d for 8 days, is the intervention that contributes the most to the
heterogeneity of our main random-effects model due to the inclusion of trials lasting 2 days or less. It
seems therefore recommended to administer propranolol for AIA with a duration longer than 2
days.18,20,23,32 There is no evidence to suggest that increasing the dosage beyond 50 mg/d enhances
efficacy. Dumon et al39 compared the effects of betaxolol, a selective β-blocker, with those of
propranolol in akathisia and concluded that betaxolol and propranolol demonstrate comparable
efficacy. The shared mechanism of action between the 2 drugs is the blockade of β1-adrenergic
receptors.
Studies on cyproheptadine have produced conflicting results. The SUCRA ranking places it in
fourth position, but the CI of its SMD includes the value of 0, suggesting that cyproheptadine is not
significantly more effective than placebo. Considering the low confidence associated with the SMD of
cyproheptadine, it is important to prioritize these results over the questionable ranking. Rankings
are based on probabilities and do not guarantee reliable results for wide or nonsignificant CIs.40 The
fourth subgroup analysis, pooling by class antihistaminics (cyproheptadine and diphenhydramine),
has shown similar conclusions for the efficacy of antihistaminics. Although cyproheptadine appears
to be as effective as propranolol,20 it cannot be currently recommended, and additional data
are needed.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 8/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Limitations
Limitations of the study included the subgroup analysis for low risk of bias, which should be
interpreted cautiously due to the inclusion of only 8 studies, resulting in low statistical power. The
efficacy of propranolol may be underestimated due to study design. In the study by Kramer et al,24
propranolol did not demonstrate significant efficacy at the end of the first period (2 days), whereas it
showed efficacy at the end of the study (5 days). Some studies excluded benzodiazepines and
anticholinergics, whereas others included them but ensured that they were initiated before the start
of the trial, with constant and balanced doses between arms to avoid confounding effects. Because
only 1.5% of patients were treated with antipsychotic polytherapy, the efficacy of AIA can
theoretically not be extrapolated to patients treated with antipsychotic polytherapy. However,
antipsychotic polytherapy is common in clinical practice and is a recognized risk factor of AIA, and
antipsychotic daily dose was not associated with efficacy in our results. Antipsychotic monotherapy
is still recommended in cases of akathisia induced by antipsychotic polytherapy. Additionally, we did
not use pre-post effect sizes to evaluate the evolution of scores over time because the intertime
correlation coefficient (r) was not reported in the trials. Furthermore, between-group SMDs provide
better control over covariates compared with within-group SMDs.41 Finally, our random-effects
model relies on numerous indirect evidence due to the lack of direct comparisons between active
treatments. The consistency between direct and indirect evidence defends the accuracy of network
estimates.
Conclusions
This systematic review and network meta-analysis found that mirtazapine (15 mg/d for ⱖ5 days),
biperiden (12 mg/d for ⱖ14 days), and vitamin B6 (600 mg/d for ⱖ5 days) were associated with the
greatest efficacy for treating AIA, with vitamin B6 having the best efficacy and tolerance profile.
Because the number of available RCTs remains low and sample sizes are limited, prudence is advised.
Trazodone (100 mg/d for ⱖ5 days), mianserin (15 mg/d for ⱖ5 days), and propranolol (50 mg/d for
ⱖ8 days) may be effective alternatives with less favorable efficacy and tolerance profiles.
ARTICLE INFORMATION
Accepted for Publication: January 18, 2024.
Published: March 7, 2024. doi:10.1001/jamanetworkopen.2024.1527
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2024 Gerolymos
C et al. JAMA Network Open.
Corresponding Author: Guillaume Fond, MD, PhD, Health Service Research and Quality of Life Center (CEReSS),
Assistance Publique-Hôpitaux de Marseille, 276 bd Sainte-Marguerite, 13009 Marseille, France (guillaume.fond@
gmail.com).
Author Affiliations: Health Service Research and Quality of Life Center (CEReSS), Assistance Publique-Hôpitaux
de Marseille, Aix-Marseille Université, Marseille, France (Gerolymos, Barazer, Loundou, Boyer, Fond); FondaMental
Foundation, Creteil, France (Gerolymos, Boyer, Fond); Department of Pediatrics, Kyung Hee University College of
Medicine, Seoul, Republic of Korea (Yon); Center for Digital Health, Medical Science Research Institute, Kyung Hee
University Medical Center, Kyung Hee University College of Medicine, Seoul, Republic of Korea (Yon).
Author Contributions: Dr Gerolymos and Prof Boyer had full access to all of the data in the study and take
responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Gerolymos, Barazer, Boyer, Fond.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Gerolymos, Loundou, Fond.
Critical review of the manuscript for important intellectual content: Gerolymos, Barazer, Yon, Boyer, Fond.
Statistical analysis: Gerolymos, Loundou.
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 9/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
Administrative, technical, or material support: Fond.
Supervision: Yon, Boyer, Fond.
Conflict of Interest Disclosures: None reported.
Data Sharing Statement: See Supplement 2.
Additional Contributions: Mohamed Boucekine, MSc, Health Service Research and Quality of Life Center
(CEReSS), Assistance Publique-Hôpitaux de Marseille, Aix-Marseille Université, Marseille, France, assisted with
data analysis (handling missing data). He was not compensated for this work.
REFERENCES
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American
Psychiatric Association; 2013.
2. Huhn M, Nikolakopoulou A, Schneider-Thoma J, et al. Comparative efficacy and tolerability of 32 oral
antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and
network meta-analysis. Lancet. 2019;394(10202):939-951. doi:10.1016/S0140-6736(19)31135-3
3. Caroff SN, Hurford I, Lybrand J, Campbell EC. Movement disorders induced by antipsychotic drugs: implications
of the CATIE schizophrenia trial. Neurol Clin. 2011;29(1):127-148, viii. doi:10.1016/j.ncl.2010.10.002
4. Halstead SM, Barnes TRE, Speller JC. Akathisia: prevalence and associated dysphoria in an in-patient population
with chronic schizophrenia. Br J Psychiatry. 1994;164(2):177-183. doi:10.1192/bjp.164.2.177
5. Janno S, Holi M, Tuisku K, Wahlbeck K. Prevalence of neuroleptic-induced movement disorders in chronic
schizophrenia inpatients. Am J Psychiatry. 2004;161(1):160-163. doi:10.1176/appi.ajp.161.1.160
6. Modestin J, Wehrli MV, Stephan PL, Agarwalla P. Evolution of neuroleptic-induced extrapyramidal syndromes
under long-term neuroleptic treatment. Schizophr Res. 2008;100(1-3):97-107. doi:10.1016/j.schres.2007.10.018
7. Berna F, Misdrahi D, Boyer L, et al; FACE-SZ (FondaMental Academic Centers of Expertise for Schizophrenia)
Group. Akathisia: prevalence and risk factors in a community-dwelling sample of patients with schizophrenia:
results from the FACE-SZ dataset. Schizophr Res. 2015;169(1-3):255-261. doi:10.1016/j.schres.2015.10.040
8. Cheng HM, Park JH, Hernstadt D. Akathisia: a life-threatening side effect of a common medication. BMJ Case
Rep. Published online May 21, 2013. doi:10.1136/bcr-2012-007713
9. Pringsheim T, Gardner D, Addington D, et al. The assessment and treatment of antipsychotic-induced akathisia.
Can J Psychiatry. 2018;63(11):719-729. doi:10.1177/0706743718760288
10. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting
systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
11. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ.
2019;366:l4898. doi:10.1136/bmj.l4898
12. Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Stat. 1981;6
(2):107-128. doi:10.3102/10769986006002107
13. Rücker G, Nikolakopoulou A, Papakonstantinou T, Salanti G, Riley RD, Schwarzer G. The statistical importance
of a study for a network meta-analysis estimate. BMC Med Res Methodol. 2020;20(1):190. doi:10.1186/s12874-
020-01075-y
14. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327
(7414):557-560. doi:10.1136/bmj.327.7414.557
15. Higgins JPT. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified.
Int J Epidemiol. 2008;37(5):1158-1160. doi:10.1093/ije/dyn204
16. Preuß M, Ziegler A. A simplification and implementation of random-effects meta-analyses based on the exact
distribution of Cochran’s Q. Methods Inf Med. 2014;53(1):54-61. doi:10.3414/ME13-01-0073
17. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment
Health. 2019;22(4):153-160. doi:10.1136/ebmental-2019-300117
18. Adler L, Angrist B, Peselow E, Corwin J, Maslansky R, Rotrosen J. A controlled assessment of propranolol in the
treatment of neuroleptic-induced akathisia. Br J Psychiatry. 1986;149(1):42-45. doi:10.1192/bjp.149.1.42
19. Pujalte D, Bottaï T, Huë B, et al. A double-blind comparison of clonazepam and placebo in the treatment of
neuroleptic-induced akathisia. Clin Neuropharmacol. 1994;17(3):236-242. doi:10.1097/00002826-
199406000-00003
20. Fischel T, Hermesh H, Aizenberg D, et al. Cyproheptadine versus propranolol for the treatment of acute
neuroleptic-induced akathisia: a comparative double-blind study. J Clin Psychopharmacol. 2001;21(6):612-615. doi:
10.1097/00004714-200112000-00013
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 10/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
21. Poyurovsky M, Epshtein S, Fuchs C, Schneidman M, Weizman R, Weizman A. Efficacy of low-dose mirtazapine
in neuroleptic-induced akathisia: a double-blind randomized placebo-controlled pilot study. J Clin
Psychopharmacol. 2003;23(3):305-308. doi:10.1097/01.jcp.0000084027.22282.16
22. Gagrat D, Hamilton J, Belmaker RH. Intravenous diazepam in the treatment of neuroleptic-induced acute
dystonia and akathisia. Am J Psychiatry. 1978;135(10):1232-1233. doi:10.1176/ajp.135.10.1232
23. Poyurovsky M, Pashinian A, Weizman R, Fuchs C, Weizman A. Low-dose mirtazapine: a new option in the
treatment of antipsychotic-induced akathisia: a randomized, double-blind, placebo- and propranolol-controlled
trial. Biol Psychiatry. 2006;59(11):1071-1077. doi:10.1016/j.biopsych.2005.12.007
24. Kramer MS, Gorkin RA, DiJohnson C, Sheves P. Propranolol in the treatment of neuroleptic-induced akathisia
(NIA) in schizophrenics: a double-blind, placebo-controlled study. Biol Psychiatry. 1988;24(7):823-827. doi:10.
1016/0006-3223(88)90260-0
25. Friis T, Christensen TR, Gerlach J. Sodium valproate and biperiden in neuroleptic-induced akathisia,
parkinsonism and hyperkinesia: a double-blind cross-over study with placebo. Acta Psychiatr Scand. 1983;67(3):
178-187. doi:10.1111/j.1600-0447.1983.tb00339.x
26. Baskak B, Atbasoglu EC, Ozguven HD, Saka MC, Gogus AK. The effectiveness of intramuscular biperiden in
acute akathisia: a double-blind, randomized, placebo-controlled study. J Clin Psychopharmacol. 2007;27(3):
289-294. doi:10.1097/jcp.0b013e3180582439
27. Shams-Alizadeh N, Maroufi A, Asadi Z, Rahmani K, Hassanzadeh K. Trazodone as an alternative treatment for
neuroleptic-associated akathisia: a placebo-controlled, double-blind, clinical trial. J Clin Psychopharmacol. 2020;
40(6):611-614. doi:10.1097/JCP.0000000000001286
28. Stryjer R, Rosenzcwaig S, Bar F, Ulman AM, Weizman A, Spivak B. Trazodone for the treatment of neuroleptic-
induced acute akathisia: a placebo-controlled, double-blind, crossover study. Clin Neuropharmacol. 2010;33(5):
219-222. doi:10.1097/WNF.0b013e3181ee7f63
29. Poyurovsky M, Shardorodsky M, Fuchs C, Schneidman M, Weizman A. Treatment of neuroleptic-induced
akathisia with the 5-HT2 antagonist mianserin: double-blind, placebo-controlled study. Br J Psychiatry. 1999;174
(3):238-242. doi:10.1192/bjp.174.3.238
30. Lerner V, Bergman J, Statsenko N, Miodownik C. Vitamin B6 treatment in acute neuroleptic-induced akathisia:
a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2004;65(11):1550-1554. doi:10.4088/
JCP.v65n1118
31. Miodownik C, Lerner V, Statsenko N, et al. Vitamin B6 versus mianserin and placebo in acute neuroleptic-
induced akathisia: a randomized, double-blind, controlled study. Clin Neuropharmacol. 2006;29(2):68-72. doi:10.
1097/00002826-200603000-00002
32. Avital A, Gross-Isseroff R, Stryjer R, Hermesh H, Weizman A, Shiloh R. Zolmitriptan compared to propranolol
in the treatment of acute neuroleptic-induced akathisia: a comparative double-blind study. Eur
Neuropsychopharmacol. 2009;19(7):476-482. doi:10.1016/j.euroneuro.2009.02.006
33. Wichniak A, Wierzbicka A, Walęcka M, Jernajczyk W. Effects of antidepressants on sleep. Curr Psychiatry Rep.
2017;19(9):63. doi:10.1007/s11920-017-0816-4
34. Terevnikov V, Stenberg JH, Tiihonen J, et al. Add-on mirtazapine improves depressive symptoms in
schizophrenia: a double-blind randomized placebo-controlled study with an open-label extension phase. Hum
Psychopharmacol. 2011;26(3):188-193. doi:10.1002/hup.1189
35. Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). Ficha Technika AKINETON 5MG/ML
Solución inyectable. Accessed January 24, 2024. https://cima.aemps.es/cima/dochtml/ft/28994/FT_28994.html
36. Correas Gómez MA, Portillo Martín JA, Martín García B, et al. Priapismo por trazodona. Actas Urol Esp.
2000;24(10):840-842. doi:10.1016/S0210-4806(00)72559-9
37. Mann RA, George AK. Recurrent priapism in a military veteran receiving treatment for PTSD. Mil Med. 2017;
182(11):e2104-e2107. doi:10.7205/MILMED-D-17-00072
38. Fagiolini A, Comandini A, Catena Dell’Osso M, Kasper S. Rediscovering trazodone for the treatment of major
depressive disorder. CNS Drugs. 2012;26(12):1033-1049. doi:10.1007/s40263-012-0010-5
39. Dumon JP, Catteau J, Lanvin F, Dupuis BA. Randomized, double-blind, crossover, placebo-controlled
comparison of propranolol and betaxolol in the treatment of neuroleptic-induced akathisia. Am J Psychiatry. 1992;
149(5):647-650. doi:10.1176/ajp.149.5.647
40. Mbuagbaw L, Rochwerg B, Jaeschke R, et al. Approaches to interpreting and choosing the best treatments in
network meta-analyses. Syst Rev. 2017;6(1):79. doi:10.1186/s13643-017-0473-z
41. Cuijpers P, Weitz E, Cristea IA, Twisk J. Pre-post effect sizes should be avoided in meta-analyses. Epidemiol
Psychiatr Sci. 2017;26(4):364-368. doi:10.1017/S2045796016000809
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 11/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
SUPPLEMENT 1.
eMethods. Identification and selection of studies, outcomes, missing data, and statistical analysis
eResults. Results for the efficacy at different time points and the efficacy on subjective and objective symptoms
eFigure 1. P-score ranking for the 10 interventions treating AIA and placebo
eFigure 2. Bar chart (rankogram) showing Surface Under the Cumulative Ranking (SUCRA) score for the efficacy
of the 10 different treatments in AIA and placebo
eFigure 3. Forest plot separating direct and indirect evidence for pairwise comparisons in NMA
eFigure 4. Plot showing direct and indirect evidence proportions for each network estimate (random-effects
model)
eFigure 5. Funnel plot of NMA showing publication bias assessment
eTable 1. Excluded studies and reasons for exclusion
eTable 2. Characteristics of the included studies comprised in network meta-analysis
eTable 3. Subnetwork for Gagrat 1978 with treatment effect size estimate and calculation method
eTable 4. Characteristics of the interventions comprised in the network meta-analysis
eTable 5. Cross-tabulation of ranking probabilities for the 10 akathisia interventions and placebo
eTable 6. Results for Separate Indirect from Direct Evidence (SIDE) using back-calculation method, testing
agreement between direct and indirect evidence
eTable 7. Egger's test details (publication bias assessment)
eTable 8. Pustejovsky-Rodgers's corrected test details (for standard error of SMD) (publication bias assessment)
eTable 9. Thompson-Sharp's test details (publication bias assessment)
eTable 10. Tolerability outcome details: adverse events for the 10 akathisia interventions and placebo (meta-
analysis level)
eTable 11. Acceptability outcome details: dropouts for the 10 akathisia interventions and placebo (meta-analysis
level)
eFigure 6. Boxplot showing mean ratio clustered by intervention
eFigure 7. Boxplot showing age (mean) clustered by intervention
eFigure 8. Error bars showing mean age ± standard deviation clustered by intervention
eFigure 9. Boxplot showing schizophrenia ratio (DSM-5 diagnosis) in participants clustered by intervention
eFigure 10. Boxplot showing akathisia treatment duration (days) clustered by intervention
eFigure 11. Boxplot showing akathisia treatment dose (mg/day), sort by dose range (A – low dose) for each
intervention
eFigure 12. Boxplots showing akathisia treatment dose (mg/day), sort by dose range (B – intermediate dose, C –
high) for each intervention
eFigure 13. Boxplot showing PANSS severity score at baseline (means) for each intervention
eFigure 14. Error bars showing the mean PANSS scores at baseline ± standard deviation for each intervention
eFigure 15. Boxplot showing first-generation (typical) antipsychotic (FGA) ratio for each intervention
eFigure 16. Boxplot showing chlorpromazine equivalent dose (mg/day) for each intervention
eFigure 17. Error bars showing mean chlorpromazine equivalent dose (mg/day) ± standard deviation for each
intervention
eFigure 18. Boxplot showing ratio of patients treated with anticholinergic as cotreatment for each intervention
eFigure 19. Error bars showing mean biperiden dose (cotreatment drug) (mg/day) ± standard deviation for each
intervention
eFigure 20. Error bars showing mean trihexyphenidyl dose (mg/day) ± standard deviation for each intervention
eFigure 21. Error bars showing mean benztropine dose (A), procyclidine dose (B) and tropatepine dose (C)
(mg/day) ± standard deviation for each intervention
eFigure 22. Boxplot showing ratio of patients treated with benzodiazepine (cotreatment drug) for each
intervention
eFigure 23. Error bars showing mean diazepam dose (cotreatment drug) (mg/day) ± standard deviation for each
intervention
eFigure 24. Error bars showing mean lorazepam dose (mg/day) ± standard deviation for each intervention
eFigure 25. Error bars showing mean nitrazepam dose (A), clonazepam dose (B) (cotreatment drug) and
temazepam dose (C) (mg/day) ± standard deviation for each intervention
eFigure 26. Boxplot showing mean Simpson Angus Scale (SAS) scores at baseline for each intervention
eFigure 27. Error bars showing mean SAS scores at baseline ± standard deviation for each intervention
eFigure 28. Boxplot showing mean Hamilton Depression Rating Scale (HAM-D) scores at baseline for each
intervention
eFigure 29. Error bars showing mean HAM-D scores at baseline ± standard deviation for each intervention
eFigure 30. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to akathisia treatment duration (in days)
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 12/13
Downloaded from jamanetwork.com by guest on 03/16/2024
JAMA Network Open | Psychiatry Drug Efficacy in the Treatment of Antipsychotic-Induced Akathisia
eFigure 31. Error bars showing the different standardized mean differences ± standard deviation for each
intervention, sort by dose range (A – low dose), according to akathisia treatment dose (mg/day)
eFigure 32. Error bars showing the different standardized mean differences ± standard deviation for each
intervention, sort by dose range (B – intermediate dose, C – high dose), according to akathisia treatment dose
(mg/day)
eFigure 33. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to PANSS score (mean)
eFigure 34. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to chlorpromazine equivalent dose (mg/day)
eFigure 35. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to biperiden mean dose (mg/day), used as cotreatment drug
eFigure 36. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to trihexyphenidyl mean dose (mg/day)
eFigure 37. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to benztropine mean dose (mg/day)
eFigure 38. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to diazepam mean dose (mg/day), used as cotreatment drug
eFigure 39. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to lorazepam mean dose (mg/day)
eFigure 40. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to nitrazepam mean dose (mg/day)
eFigure 41. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to Simpson Angus Scale score (mean)
eFigure 42. Error bars showing the different standardized mean differences ± standard deviation for each
intervention according to Hamilton Depression Rating Scale (mean)
eFigure 43. Low-risk bias assessment, subgroup 1: network graph (random-effects model)
eFigure 44. Low-risk bias assessment, subgroup 1: forest plot (random-effects model)
eFigure 45. Low-risk bias assessment, subgroup 1: league table (random-effects model)
eFigure 46. Akathisia treatment duration > two days, subgroup 2: network graph (random-effects model)
eFigure 47. Akathisia treatment duration > two days, subgroup 2: forest plot (random-effects model)
eFigure 48. Akathisia treatment duration > two days, subgroup 2: league table (random-effects model)
eFigure 49. BARS as akathisia scale, subgroup 3: network graph (random-effects model)
eFigure 50. BARS as akathisia scale, subgroup 3: forest plot (random-effects model)
eFigure 51. BARS as akathisia scale, subgroup 3: league table (random-effects model)
eFigure 52. Benzodiazepines, antihistaminics and other actives vs placebo, subgroup 4: network graph (random-
effects model)
eFigure 53. Benzodiazepines, antihistaminics and other actives vs placebo, subgroup 4: forest plot (random-
effects model)
eFigure 54. Benzodiazepines, antihistaminics and other actives vs placebo, subgroup 4: league table (random-
effects model)
eFigure 55. Therapeutic classes in akathisia vs placebo, subgroup 5: network graph (random-effects model)
eFigure 56. Therapeutic classes in akathisia vs placebo, subgroup 5: forest plot (random-effects model)
eFigure 57. Therapeutic classes in akathisia vs placebo, subgroup 5: league table (random-effects model)
eReferences
SUPPLEMENT 2.
Data Sharing Statement
JAMA Network Open. 2024;7(3):e241527. doi:10.1001/jamanetworkopen.2024.1527 (Reprinted) March 7, 2024 13/13
Downloaded from jamanetwork.com by guest on 03/16/2024
You might also like
- Chapter 1 Part 1 Fill in The BlankDocument2 pagesChapter 1 Part 1 Fill in The BlankArlanosaurusNo ratings yet
- Drug Efficacy in The Treatment of Antipsychotic-Induced Akathisia A Systematic Review and Network Meta-AnalysisDocument9 pagesDrug Efficacy in The Treatment of Antipsychotic-Induced Akathisia A Systematic Review and Network Meta-AnalysisalejabotiarNo ratings yet
- Bahji 2020Document31 pagesBahji 2020Abdul Mannan ChatthaNo ratings yet
- Comparative Efficacy and Acceptability of Psychotherapies For Panic Disorder With or Without Agoraphobia Systematic Review and Network Meta Analysis of Randomised Controlled TrialsDocument13 pagesComparative Efficacy and Acceptability of Psychotherapies For Panic Disorder With or Without Agoraphobia Systematic Review and Network Meta Analysis of Randomised Controlled TrialsLOLUIZNo ratings yet
- Jamapsychiatry Papola 2023 Oi 230080 1697118575.84256Document11 pagesJamapsychiatry Papola 2023 Oi 230080 1697118575.84256Renan CruzNo ratings yet
- 1 s2.0 S1525505019311011 MainDocument5 pages1 s2.0 S1525505019311011 MainilonaskorinNo ratings yet
- Gedin 2022 Oi 221233 1668781352.25734Document12 pagesGedin 2022 Oi 221233 1668781352.25734Dragutin PetrićNo ratings yet
- BMJ 2023 078084.fullDocument14 pagesBMJ 2023 078084.fulljayswalrameshNo ratings yet
- jiang et al 2023 pharmacological and behavioral interventions for fatigue in parkinson s disease a meta analysis of (科研通 ablesci.com)Document9 pagesjiang et al 2023 pharmacological and behavioral interventions for fatigue in parkinson s disease a meta analysis of (科研通 ablesci.com)Pei-Hao ChenNo ratings yet
- Appi Focus 16407Document10 pagesAppi Focus 16407MARIALEJ PEREZ MONTALVANNo ratings yet
- Barrionuevo 2018Document7 pagesBarrionuevo 2018hlwNo ratings yet
- Association Between Physical Activity and Risk of Depression A Systematic Review and Meta-AnalysisDocument10 pagesAssociation Between Physical Activity and Risk of Depression A Systematic Review and Meta-AnalysisAna Margarida J. - PsicólogaNo ratings yet
- Light Therapy For Non Seasonal Depression Systematic Review and Meta AnalysisDocument11 pagesLight Therapy For Non Seasonal Depression Systematic Review and Meta AnalysisGabriel VinhattiNo ratings yet
- Comparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisDocument10 pagesComparative e Cacy and Acceptability of Antimanic Drugs in Acute Mania: A Multiple-Treatments Meta-AnalysisCarolina PradoNo ratings yet
- Fpsyt 11 608896Document20 pagesFpsyt 11 608896shumailaNo ratings yet
- 1 s2.0 S2215036623001992Document13 pages1 s2.0 S2215036623001992Jorge SalazarNo ratings yet
- Review ArticleDocument9 pagesReview ArticleMuhammad YanazNo ratings yet
- Hype or Hope? High Placebo Response in Major Depression Treatment With Ketamine and Esketamine: A Systematic Review and Meta-AnalysisDocument11 pagesHype or Hope? High Placebo Response in Major Depression Treatment With Ketamine and Esketamine: A Systematic Review and Meta-Analysisservicio psiquiatría HCHNo ratings yet
- Hubungan Antara Gejala Depresi Dokter Dan Kesalahan MedisDocument14 pagesHubungan Antara Gejala Depresi Dokter Dan Kesalahan MedisMaikel PakageNo ratings yet
- Artigo Lancet Medicamentos AnsiedadeDocument10 pagesArtigo Lancet Medicamentos AnsiedadeRebecca DiasNo ratings yet
- Magnitude of The Placebo Response Across Treatment Modalities Used For Treatment-Resistant Depression in Adults A Systematic Review and Meta-AnalysisDocument18 pagesMagnitude of The Placebo Response Across Treatment Modalities Used For Treatment-Resistant Depression in Adults A Systematic Review and Meta-AnalysisUSFMFPNo ratings yet
- Medicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaDocument5 pagesMedicine: Comparison Between Acupuncture and Cognitive Behavioral Therapy For Primary InsomniaJoão PauloNo ratings yet
- Medi-100-E27653Document7 pagesMedi-100-E27653Rika TriwardianiNo ratings yet
- Cognitive-Behavioral Therapy For Treating Hypertension: A Systematic Review and Meta-Analysis: PsychDocument1 pageCognitive-Behavioral Therapy For Treating Hypertension: A Systematic Review and Meta-Analysis: PsychJames BalamesNo ratings yet
- Opioid-Sparing Effect of Cannabinoids For AnalgesiaDocument16 pagesOpioid-Sparing Effect of Cannabinoids For Analgesia幸福KoreaNo ratings yet
- Jama Association Between Physical Activity and Risk of DepressionDocument10 pagesJama Association Between Physical Activity and Risk of DepressiongbfascNo ratings yet
- Ketamine NNTDocument8 pagesKetamine NNTBrent AllieNo ratings yet
- The Efficacy and Safety of Diterpene Ginkgolides.17Document11 pagesThe Efficacy and Safety of Diterpene Ginkgolides.17drfperezNo ratings yet
- Metanalise Antidepressivos 2015 PDFDocument18 pagesMetanalise Antidepressivos 2015 PDFFábio C NetoNo ratings yet
- Lee 2018Document24 pagesLee 2018Eliana RieraNo ratings yet
- Gómez-García 2016Document10 pagesGómez-García 2016Rafaela Queiroz MascarenhasNo ratings yet
- Anticonvulsivantes 2018Document8 pagesAnticonvulsivantes 2018ps.ericavillarroelNo ratings yet
- Chen 2021Document13 pagesChen 2021Aitor UzkudunNo ratings yet
- 2022 de VriesDocument8 pages2022 de Vriesmvillar15_247536468No ratings yet
- A Systematic Review and Network Meta-Analysis On Comparative Efficacy, Acceptability, and Safety of Treatments in Acute Bipolar Mania in YouthsDocument14 pagesA Systematic Review and Network Meta-Analysis On Comparative Efficacy, Acceptability, and Safety of Treatments in Acute Bipolar Mania in YouthsDiego HormacheaNo ratings yet
- Efficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisDocument6 pagesEfficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisChica MirandaNo ratings yet
- Hengartner 2017Document7 pagesHengartner 2017Julio JuarezNo ratings yet
- Articulo Sesion Bibliografica Vie. 5 Abril 2024 Dr. Alejandra G. Gonzalez RiiiDocument12 pagesArticulo Sesion Bibliografica Vie. 5 Abril 2024 Dr. Alejandra G. Gonzalez Riiijadebelen29No ratings yet
- Courtney - 2022 - Oi - 211279 - 1643056684.29546 1Document22 pagesCourtney - 2022 - Oi - 211279 - 1643056684.29546 1U of T MedicineNo ratings yet
- Relapse Rates With Paliperidone Palmitate in AdultDocument11 pagesRelapse Rates With Paliperidone Palmitate in AdultdryaeonNo ratings yet
- Efficacy and Safety of Aspirin As An Adjunctive Therapy in TubercularDocument7 pagesEfficacy and Safety of Aspirin As An Adjunctive Therapy in TubercularYunita WidyaningsihNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundPsiquiatría CESAMENo ratings yet
- Nejmoa 2206443Document12 pagesNejmoa 2206443Bryan PalmaNo ratings yet
- Headache 2024 Robblee The 2023 Protocol For Update To Acute TreatmentDocument4 pagesHeadache 2024 Robblee The 2023 Protocol For Update To Acute TreatmentJaqueline CarvalhoNo ratings yet
- Jurnal Reading 2Document6 pagesJurnal Reading 2dezafarista_44587428No ratings yet
- Real-Life Clinical Experience With Cariprazine - A Systematic Review of Case StudiesDocument17 pagesReal-Life Clinical Experience With Cariprazine - A Systematic Review of Case Studiesbelloilportogallo99No ratings yet
- Z Al-Roubaie - 2020Document12 pagesZ Al-Roubaie - 2020Kossay ZaouiNo ratings yet
- ผลัดที่2 6101769 ปภัสรา JCDocument69 pagesผลัดที่2 6101769 ปภัสรา JCpapatsaraNo ratings yet
- Xu 2020Document10 pagesXu 2020Risky PerdanaNo ratings yet
- ketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-reviewDocument12 pagesketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-reviewNuno TorresNo ratings yet
- Antipsychotics For Preventing Delirium in Hospitalized AdultsDocument12 pagesAntipsychotics For Preventing Delirium in Hospitalized AdultsLuis CsrNo ratings yet
- Wakeman 2020 Oi 190774Document12 pagesWakeman 2020 Oi 190774Yed HeeNo ratings yet
- Comparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainDocument15 pagesComparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainRachel PutriNo ratings yet
- In-Silico Studies in Herbal Drugs: A ReviewDocument5 pagesIn-Silico Studies in Herbal Drugs: A ReviewShihan SilvaNo ratings yet
- Biologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysisDocument14 pagesBiologic Therapy For Psoriatic Arthritis or Moderate To Severe Plaque Psoriasis: Systematic Review With Pairwise and Network Meta-AnalysislilingNo ratings yet
- bmj.n2321.fullDocument16 pagesbmj.n2321.fulljairo canlasNo ratings yet
- Complementary Therapies in Clinical PracticeDocument7 pagesComplementary Therapies in Clinical PracticeBkash ShahNo ratings yet
- Journal of Affective Disorders: Review ArticleDocument11 pagesJournal of Affective Disorders: Review Article賀立安No ratings yet
- Medicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionDocument5 pagesMedicine: Pharmacological and Psychotherapeutic Interventions For Management of Poststroke DepressionaditNo ratings yet
- Medical Cannabis For The Treatment of DementiaDocument24 pagesMedical Cannabis For The Treatment of DementiaLorina BoligNo ratings yet
- Your Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022From EverandYour Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022No ratings yet
- Nursing Performance Checklist TracheostomyDocument3 pagesNursing Performance Checklist TracheostomySyahrilKiyai100% (1)
- Homeless Deaths ReportDocument102 pagesHomeless Deaths ReportCapital Public RadioNo ratings yet
- Unit 3 Integumentary System Pathological ConditionsDocument43 pagesUnit 3 Integumentary System Pathological Conditionsalmira garciaNo ratings yet
- The Role of The Clinical SupervisorDocument52 pagesThe Role of The Clinical SupervisorDwi NopriyantoNo ratings yet
- Non-Pharmacological Treatment of HypertensionDocument25 pagesNon-Pharmacological Treatment of Hypertensionastrid abrahams0% (2)
- PACS QuestionnaireDocument4 pagesPACS QuestionnaireakashniranjaneNo ratings yet
- Cleft Lip and PalateDocument18 pagesCleft Lip and Palateicywitch100% (1)
- Rajsthan All Surgical Distributor Data ListDocument33 pagesRajsthan All Surgical Distributor Data ListcatalogueNo ratings yet
- Medical & Homeopathic Research, Homeopathic Medical Collage and ResearchDocument145 pagesMedical & Homeopathic Research, Homeopathic Medical Collage and ResearchMitesh KinariwalaNo ratings yet
- Sumu PDFDocument30 pagesSumu PDFalokpalreshaNo ratings yet
- Alejandro Oet Listening PracticeDocument12 pagesAlejandro Oet Listening PracticeChapa BandaraNo ratings yet
- Pivot 4a Lesson Exemplar in Mapeh 6Document7 pagesPivot 4a Lesson Exemplar in Mapeh 6Crisente BarcelonNo ratings yet
- Administration of Topical MedicationsDocument14 pagesAdministration of Topical MedicationsgireeshsachinNo ratings yet
- Module 2Document14 pagesModule 2Muskaan BindalNo ratings yet
- Test Bank For Pathophysiology 6th Edition Jacquelyn L BanasikDocument5 pagesTest Bank For Pathophysiology 6th Edition Jacquelyn L BanasikJesus Carter97% (38)
- Laughter PrescriptionDocument4 pagesLaughter PrescriptionJair Andres Falla AldanaNo ratings yet
- Cultural Humility Versus Cultural Competence - A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education (3) - 0Document10 pagesCultural Humility Versus Cultural Competence - A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education (3) - 0Gabriela BarreiraNo ratings yet
- VACCINES Eng Spa 0 To 6 Years ScheduleDocument4 pagesVACCINES Eng Spa 0 To 6 Years ScheduleMaría del Mar OrtizNo ratings yet
- Bethesda Handbook of HematologyDocument5 pagesBethesda Handbook of HematologyjosephNo ratings yet
- Bioterrorism: An Overview: Rick Roman, M.H.S.ADocument43 pagesBioterrorism: An Overview: Rick Roman, M.H.S.ANurhasan Agung PrabowoNo ratings yet
- Moot Court BrochureDocument16 pagesMoot Court BrochureAkashNo ratings yet
- Unconsciousness: Anil PatidarDocument29 pagesUnconsciousness: Anil Patidarjinal sutharNo ratings yet
- AtpdDocument48 pagesAtpddrkadiyala2100% (2)
- A Roadmap To MCAT Content in Psychology and Sociology TextbooksDocument16 pagesA Roadmap To MCAT Content in Psychology and Sociology TextbooksJenny HuangNo ratings yet
- Sci006-Lev 11Document380 pagesSci006-Lev 11palak320% (1)
- NCP - BronchopneumoniaDocument11 pagesNCP - BronchopneumoniaMaria Ivy Mendoza100% (1)
- Adapted From Family Planning Competency-Based Training: Basic Course HandbookDocument4 pagesAdapted From Family Planning Competency-Based Training: Basic Course HandbookVanessa EnteroNo ratings yet
- Common Acquired and Congenital AnomaliesDocument5 pagesCommon Acquired and Congenital AnomaliesDang SaplanNo ratings yet
- COVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaDocument29 pagesCOVID 19 Guideline To Resume Paediatric Dental Services in MalaysiaEnrita DianNo ratings yet