Professional Documents
Culture Documents
sjdbv
sjdbv
Uploaded by
adamilzaryCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
sjdbv
sjdbv
Uploaded by
adamilzaryCopyright:
Available Formats
Open Access Case
Report DOI: 10.7759/cureus.53434
Basal Ganglia Calcification: A Case Report of Two
Siblings With Fahr's Disease
Review began 01/24/2024
Margarida Magalhães 1, Margarida Alves 1, Luís Paulino Ferreira 1, 2, Janice Alves 3, Diana Durães 1
Review ended 01/31/2024
Published 02/02/2024 1. Department of Psychiatry and Mental Health, Setúbal Hospital Centre, Setúbal, PRT 2. Department of Neurosciences,
© Copyright 2024 Nova Medical School, Lisbon, PRT 3. Department of Neurology, Setúbal Hospital Centre, Setúbal, PRT
Magalhães et al. This is an open access
article distributed under the terms of the
Corresponding author: Margarida Magalhães, maria.m.lopes@chs.min-saude.pt
Creative Commons Attribution License CC-
BY 4.0., which permits unrestricted use,
distribution, and reproduction in any
medium, provided the original author and
source are credited. Abstract
Fahr's disease is a rare neurodegenerative disorder caused by bilateral and usually symmetrical intracranial
calcifications. In most cases, it exhibits an autosomal dominant pattern of inheritance and genetic
heterogeneity. Patients may present with movement disorders, cognitive impairment, and psychiatric
disorders. Currently, there are no disease-modifying drugs, so the management is based on the treatment of
the symptoms. We present two cases involving male siblings, both with psychiatric symptoms as the initial
presentation of the disease. Brain computed tomography revealed bilateral calcifications in the basal ganglia
for which no underlying cause was found. In both cases, remission of behavioural changes and psychiatric
symptoms was achieved with psychotropic drugs.
Categories: Neurology, Psychiatry
Keywords: computed tomography, case report, neuropsychiatry, basal ganglia calcification, fahr's disease
Introduction
Fahr's disease (FD), also known as idiopathic basal ganglia calcification, was first described by Karl T. Fahr in
1930. It is a rare neurodegenerative disorder caused by bilateral and usually symmetrical basal ganglia
calcifications, although it may extend to other regions as well [1]. According to recent data, it has an
estimated prevalence of 4.5 per 10,000 persons [2]. It commonly exhibits an autosomal dominant
inheritance, and seven genes have been implicated in its genetic aetiology, of which four with dominant
inheritance (SLC20A2, PDGFB, PDGFRB, XPR1) and three with recessive inheritance (MYORG, JAM2,
CMPK2) [1,3]. The mean age of clinical onset is around 40-50 years, but symptoms can manifest at any age
[4]. Patients with FD may be asymptomatic [1]. However, they can present with cognitive impairment,
movement disorders (for example, parkinsonism), and psychiatric disorders such as anxiety, depression, or
psychotic symptoms [1]. This clinical heterogeneity can be partly explained by the basal ganglia's division
into dorsal and ventral systems. The dorsal striatum is associated with motor and cognitive functions,
whereas the ventral striatum is responsible for motivational functions [1]. Calcified areas are identified
as hyperdense lesions on unenhanced brain computed tomography (CT), which is the most reliable exam for
the diagnosis. These calcifications are commonly symmetrical, most frequently found in the basal ganglia,
but they may also involve the cerebellar dentate nuclei, thalamus, cerebral cortex, subcortical white matter,
and hippocampus [3,5].
We present two cases of siblings, one aged 46 (case 1) and the other aged 42 (case 2), both with psychiatric
symptoms as the initial presentation of FD. This paper will also discuss the neuropathological aspects,
clinical manifestations, features related to evaluation and diagnosis, and management of FD/syndrome.
Case Presentation
Case 1
Mr. S, a 46-year-old Angolan man, presented to the emergency room (ER) with complaints of behavioural
alterations, including aggressiveness, psychomotor agitation, and suicidal ideation. According to his past
medical history, he had normal psychomotor development until he was about one and a half years of age
when he presented with a loss of some acquired skills (walking and talking). Later, he exhibited severe
cognitive impairment. In school, he struggled to learn how to read or write, perform simple calculations, or
understand the value of money. Throughout his life, he needed help to perform daily activities such as
personal hygiene and feeding, remaining unable to become independent.
In his 40s, he began experiencing episodes of psychomotor agitation and aggressiveness and was prescribed
risperidone 1 mg (once per day), mirtazapine 15 mg (once per day), and clonazepam 0.5 mg (once per day),
leading to the remission of symptoms. However, a few months prior to the ER visit, he had discontinued all
medication, which led to the behavioural alterations previously described. He was referred to a psychiatry
consultation and restarted his medication.
Laboratory investigations revealed mild pancytopenia. Other laboratory findings, including urinalysis,
How to cite this article
Magalhães M, Alves M, Paulino Ferreira L, et al. (February 02, 2024) Basal Ganglia Calcification: A Case Report of Two Siblings With Fahr's
Disease. Cureus 16(2): e53434. DOI 10.7759/cureus.53434
fasting blood glucose, blood electrolytes, phosphate, creatine phosphokinase, vitamin D, thyroid hormones,
hepatic enzymes, and iron and transferrin levels, showed no abnormalities. Blood calcium was 8.8 mg/dl
(normal range: 8.4-10.2 mg/dl), and parathyroid hormone levels were 54.1 pg/ml (normal range: 15-68.3
pg/ml), all within normal limits. There was no laboratory evidence of infectious diseases, including infection
with human immunodeficiency viruses 1 and 2, hepatitis B and C, and syphilis.
A brain CT scan revealed bilateral calcifications in the basal ganglia involving the head of the caudate
nucleus and anterior lenticular regions, indicated by high-density white areas, as illustrated in Figure 1. The
electroencephalogram (EEG) showed a general slowing of brain activity with no paroxysmal activity.
FIGURE 1: Brain CT scan image (axial section) of case 1 showing
bilateral calcifications in the basal nuclei (blue arrows).
CT: computed tomography
A neuropsychological assessment was conducted (intelligence quotient was not quantified), revealing
limited cognitive-operative plasticity suggestive of impairment in the frontal-limbic pathways, which
translates into a severe intellectual developmental disorder, particularly affecting the conceptual, social,
and practical domains.
During the examination, he was vigilant and cooperative within his means. However, there was
disorientation regarding place and time. Speech was dysarthric, sparse, and only provoked; at times, words
were incomprehensible. Thought capacity was poor, with marked psychomotor lentification. The mood was
dysphoric. There were no delusional ideas or hallucinations. Physical examination also revealed walking
impairment, characterized by a wide-based gait and imbalance. There was no evidence suggestive of bipolar
disorder.
On evaluation during psychiatric consultation, after resuming previous medications, the patient showed a
positive response, with the remission of behavioural alterations and suicidal ideation. However, he
continued to experience the aforementioned cognitive and gait impairment.
2024 Magalhães et al. Cureus 16(2): e53434. DOI 10.7759/cureus.53434 2 of 6
Case 2
Mr. T, a 42-year-old Angolan man, was referred to a psychiatric consultation by his family doctor due to
anxiety and depressive mood, without psychotic symptoms. According to his past medical history, he
experienced normal psychomotor development until the age of nine months when he suffered
meningoencephalitis caused by the measles virus. Subsequently, he began to exhibit delayed cognitive
development and generalized tonic-clonic seizures. However, he has been seizure-free since adolescence
and has not required antiepileptic medication. He faced learning difficulties in school and was never able to
get a job. Also, he is partially dependent on others for everyday activities, such as cooking meals.
During the psychiatric observation, he was vigilant, calm, and collaborative, with a depressive and anxious
mood. No delusional ideas or hallucinations were observed. There was no evidence of focal or pyramidal
deficits, changes in coordination, or alterations in cranial nerves or gait. There was no evidence suggestive
of bipolar disorder.
Laboratory findings, including urinalysis, blood count, fasting blood glucose, blood electrolytes, vitamin D,
thyroid hormones, phosphate, creatine phosphokinase, hepatic enzymes, and iron and transferrin levels,
showed no abnormalities. Blood calcium was 9.7 mg/dl (normal range: 8.4-10.2 mg/dl), and parathyroid
hormone levels were 61.3 pg/ml (normal range: 15-68.3 pg/ml). There was no laboratory evidence of
infectious diseases, including infection with human immunodeficiency viruses 1 and 2, hepatitis B and C,
and syphilis.
A brain CT scan (Figure 2) revealed calcifications in the head of the caudate nucleus, as well as in the
lenticular nuclei bilaterally and adjacent to Monroe's foramina, with a more pronounced presence on the left
side. Additionally, calcifications were identified next to the wall of the left lateral ventricle, particularly near
the left frontal horn. The EEG showed slightly slow baseline electrogenesis with no paroxysmal activity.
FIGURE 2: Brain CT scan images (A, axial section; B, coronal section) of
case 2 showing bilateral calcifications in the caudate nucleus and
lenticular nuclei (blue arrows).
CT: computed tomography
He was prescribed escitalopram 10 mg per day and gabapentin 100 mg three times a day, resulting in a
complete symptomatic response.
Discussion
FD is predominantly autosomal dominantly inherited, and mutations have been identified in four causative
genes (SLC20A2, XPR1, PDGFB, and PDGFRB) [1]. Nevertheless, around 50% of FD patients have yet to
receive a genetic diagnosis [6]. The physiopathological mechanism of FD is not completely understood.
Anatomopathological alterations were mainly observed in small vessels, perivascular regions, neuroglia,
and neurons [7].
However, one must distinguish FD from Fahr's syndrome. FD is idiopathic or genetic. In Fahr's syndrome,
the basal ganglia calcifications are secondary to an underlying systemic disease, such as parathyroid
abnormalities, mitochondrial myopathies, and infections. FD must also be distinguished from "radiological"
basal ganglia calcification without clinical features, which is found on CT scans in 0.9% of the general
population [8].
2024 Magalhães et al. Cureus 16(2): e53434. DOI 10.7759/cureus.53434 3 of 6
The available epidemiological data suggests that this disease is more common in men [9], with clinical onset
typically occurring around 40-50 years of age. Clinical manifestations can range from asymptomatic cases to
more severe courses, even among individuals within the same family [10]. Severe forms may lead to
progressive deterioration, encompassing psychosis, depression, dementia, gait disturbance, speech
difficulties, basal ganglia movement disorders, and cerebellar signs [5,10,11].
Motor manifestations were reported in approximately one-third of patients [3]. About 42% of cases display
anxiety, psychosis, cognitive decline, and headache [3]. Parkinsonism represents the primary motor
phenotype in FD [12].
The diagnosis of FD relies on the identification of bilateral basal ganglia calcifications through brain
imaging (CT scan) and the exclusion of secondary causes of calcium deposition in the brain [3]. These
secondary causes encompass persistent hypocalcemia resulting from calcium metabolism alterations,
infectious diseases, as well as other rare neurodegenerative conditions [3].
The diagnostic criteria for FD, originally derived from Moskowitz et al., have undergone modifications and
can be outlined as follows [13,14]: (a) bilateral calcification of the basal ganglia or other brain regions; (b)
progressive neurologic dysfunction, most often a movement disorder and/or neuropsychiatric
manifestations; (c) onset typically occurs in the fourth or fifth decade; (d) absence of a mitochondrial or
metabolic disease or other systemic disorder; (e) absence of an infectious, toxic, or traumatic cause; and (f)
family history consistent with autosomal dominant inheritance.
In our case report, all the diagnostic criteria were met for case 1, and five of the diagnostic criteria were met
for case 2. Laboratory screening should include a complete calcium metabolism assessment, lactic acid, and
creatine phosphokinase (potentially increased in mitochondrial diseases) [11]. In individuals diagnosed with
FD, serum levels of calcium, phosphate, alkaline phosphatase, and parathyroid hormone are within normal
ranges [1]. Concerning imaging tests, a brain CT scan is the most sensitive modality for localizing and
assessing the extent of calcium deposits. The lenticular nucleus, particularly the internal globus pallidus, is
the most affected area. A fluorodeoxyglucose-positron emission tomography (FDG-PET) may also be
required and is expected to show decreased FDG uptake, especially in the basal ganglia [11].
The calcifications appear to follow a typical progression, starting with mild calcification limited to the
lentiform nucleus and caudate nucleus and advancing to severe calcification affecting all basal ganglia
except the midbrain [4]. The severity of calcifications on CT is positively correlated with age, and
symptomatic patients exhibit more calcifications compared to asymptomatic patients [2]. Radiological
follow-up has limited value in clinical practice. This is because it is not possible to establish the disease
prognosis based on radiological findings, even in cases where the progression of calcification on brain
imaging is demonstrable over time [3].
Our cases, both males and brothers, have experienced some degree of cognitive and motor impairment since
childhood. Case 2 has a history of childhood infection, while Case 1 has no history of infection or traumatic
events. They presented with neuropsychiatric symptoms (anxiety, depression, suicidal crisis) starting in the
fifth decade of life, revealing significant calcifications in the basal ganglia during neuroimaging assessment.
Blood tests showed no significant abnormalities: blood count, renal function tests, parathyroid hormone,
thyroid hormones, and vitamin D were all normal. In our cases, five of the diagnostic criteria were met. The
absence of laboratory findings, EEG changes, and somatic characteristics suggestive of mitochondrial,
metabolic, or other systemic diseases reinforces the diagnosis of FD.
Currently, there is no disease-modifying therapy for FD to reduce brain calcification or prevent its
progression; thus, the treatment is mainly symptomatic [6]. Due to the large clinical heterogeneity, various
medications are employed, including antipsychotics, anticonvulsants, antidepressants, mood stabilizers,
antiparkinsonian drugs, analgesics, and benzodiazepines [15].
Selective serotonin reuptake inhibitors (SSRIs) are employed for managing depression, obsessive-
compulsive behaviours, and anxiety in FD. Caution is warranted when using carbamazepine and
barbiturates, as they may exacerbate gait dysfunction [11]. Psychiatrists and neurologists should exercise
great caution with the use of antidepressants and anxiolytics, as these drugs can have a low threshold for
side effects in FD patients. Additionally, lithium has been associated with an increased seizure risk, and
neuroleptics may worsen extrapyramidal symptoms.
Effective therapies to control the progression of brain calcification have been rarely reported.
Bisphosphonates have been reported to improve symptoms in isolated cases, although a demonstrated
reduction in calcium deposition remains lacking [15].
Conclusions
As FD exhibits clinical heterogeneity, the diagnosis relies on neuroimaging when no alternative explanation
for bilateral and symmetrical basal ganglia calcifications is evident. Treatment is tailored to symptom
2024 Magalhães et al. Cureus 16(2): e53434. DOI 10.7759/cureus.53434 4 of 6
control for FD and correction of underlying metabolic abnormalities.
The cases presented intend to highlight the clinical and diagnostic methods and effective treatment of FD.
FD is often unfamiliar to non-psychiatrists and non-neurologists, potentially leading to misdiagnosis,
underdiagnosis, and inadequate treatment for affected patients. Increasing access to this information among
physicians and students is essential for prompt diagnosis, enhancing the quality of care for these patients
and reducing morbidity.
Additional Information
Author Contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the
work.
Concept and design: Margarida Magalhães, Margarida Alves, Diana Durães
Acquisition, analysis, or interpretation of data: Margarida Magalhães, Margarida Alves, Luís Paulino
Ferreira, Janice Alves
Drafting of the manuscript: Margarida Magalhães, Margarida Alves, Luís Paulino Ferreira
Critical review of the manuscript for important intellectual content: Margarida Magalhães, Margarida
Alves, Luís Paulino Ferreira, Janice Alves, Diana Durães
Supervision: Luís Paulino Ferreira, Diana Durães
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In
compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services
info: All authors have declared that no financial support was received from any organization for the
submitted work. Financial relationships: All authors have declared that they have no financial
relationships at present or within the previous three years with any organizations that might have an
interest in the submitted work. Other relationships: All authors have declared that there are no other
relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
Margarida Magalhães and Margarida Alves contributed equally to the work and should be considered co-first
authors.
References
1. Peters ME, de Brouwer EJ, Bartstra JW, et al.: Mechanisms of calcification in Fahr disease and exposure of
potential therapeutic targets. Neurol Clin Pract. 2020, 10:449-57. 10.1212/CPJ.0000000000000782
2. Nicolas G, Charbonnier C, Campion D, Veltman JA: Estimation of minimal disease prevalence from
population genomic data: application to primary familial brain calcification. Am J Med Genet B
Neuropsychiatr Genet. 2018, 177:68-74. 10.1002/ajmg.b.32605
3. Carecchio M, Mainardi M, Bonato G: The clinical and genetic spectrum of primary familial brain
calcification. J Neurol. 2023, 270:3270-7. 10.1007/s00415-023-11650-0
4. Ramos EM, Carecchio M, Lemos R, et al.: Primary brain calcification: an international study reporting novel
variants and associated phenotypes. Eur J Hum Genet. 2018, 26:1462-77. 10.1038/s41431-018-0185-4
5. Durante A, Audino N, Cristiano M, et al.: Basal ganglia calcification: a Fahr's disease case report . Radiol Case
Rep. 2021, 16:3055-9. 10.1016/j.radcr.2021.07.042
6. Chen SY, Ho CJ, Lu YT, Lin CH, Lan MY, Tsai MH: The genetics of primary familial brain calcification: a
literature review. Int J Mol Sci. 2023, 24:10886. 10.3390/ijms241310886
7. Subedi S, Mukhi S, Pandey P: Fahr's disease presenting with manic symptoms . JNMA J Nepal Med Assoc.
2018, 56:553-5.
8. Siddiqui WT, Brar G, Bilori B: Fahr's disease. Postgrad Med J. 2022, 98:e39. 10.1136/postgradmedj-2021-
140309
9. Shahid N, Dosu A, Nasser F: Fahr's disease: case presentation with facial numbness . Cureus. 2023,
15:e43786. 10.7759/cureus.43786
10. Nicolas G, Pottier C, Charbonnier C, et al.: Phenotypic spectrum of probable and genetically-confirmed
idiopathic basal ganglia calcification. Brain. 2013, 136:3395-407. 10.1093/brain/awt255
11. Amisha F, Munakomi S: Fahr Syndrome. StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL);
2023.
12. Tadic V, Westenberger A, Domingo A, Alvarez-Fischer D, Klein C, Kasten M: Primary familial brain
calcification with known gene mutations: a systematic review and challenges of phenotypic
characterization. JAMA Neurol. 2015, 72:460-7. 10.1001/jamaneurol.2014.3889
13. Moskowitz MA, Winickoff RN, Heinz ER: Familial calcification of the basal ganglions: a metabolic and
2024 Magalhães et al. Cureus 16(2): e53434. DOI 10.7759/cureus.53434 5 of 6
genetic study. N Engl J Med. 1971, 285:72-7. 10.1056/NEJM197107082850202
14. Ooi HW, Er C, Hussain I, Kuthiah N, Meyyur Aravamudan V: Bilateral basal ganglia calcification: Fahr's
disease. Cureus. 2019, 11:e4797. 10.7759/cureus.4797
15. Xu X, Sun H, Luo J, et al.: The pathology of primary familial brain calcification: implications for treatment .
Neurosci Bull. 2023, 39:659-74. 10.1007/s12264-022-00980-0
2024 Magalhães et al. Cureus 16(2): e53434. DOI 10.7759/cureus.53434 6 of 6
You might also like
- CHCCCS025Document80 pagesCHCCCS025kul199080% (20)
- MeningoceleDocument33 pagesMeningoceleAnkira Findoro100% (1)
- Os Roent PDFDocument87 pagesOs Roent PDFTJ OberioNo ratings yet
- 10.1016@B978 0 444 64012 3.00003 4Document13 pages10.1016@B978 0 444 64012 3.00003 4loloasbNo ratings yet
- FTD Psychiatric DDDocument11 pagesFTD Psychiatric DDlaraviNo ratings yet
- The Psychiatric Comorbidity of Epilepsy PDFDocument14 pagesThe Psychiatric Comorbidity of Epilepsy PDFTanjung E SumekarNo ratings yet
- CTP NotesDocument8 pagesCTP Notesrupangishah7No ratings yet
- 1311 IjirmsDocument4 pages1311 Ijirmsbayekha04No ratings yet
- 52 Tripathy EtalDocument5 pages52 Tripathy EtaleditorijmrhsNo ratings yet
- Neuromodulation For The Treatment of Prader-Willi Syndrome - A Systematic ReviewDocument9 pagesNeuromodulation For The Treatment of Prader-Willi Syndrome - A Systematic ReviewCristina Sánchez MoralesNo ratings yet
- Bipolaridade e Esclerose MúltiplaDocument4 pagesBipolaridade e Esclerose MúltiplaLucasFelipeRibeiroNo ratings yet
- Moyamoya-Patient-With-Schizophrenia ACPDocument5 pagesMoyamoya-Patient-With-Schizophrenia ACPCatalinaNo ratings yet
- Adult Presentation of Dyke Davidoff Masson Syndrome With Schizoaffective Disorder - A Case Report - EditedDocument5 pagesAdult Presentation of Dyke Davidoff Masson Syndrome With Schizoaffective Disorder - A Case Report - Editedgion.nandNo ratings yet
- Prion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDDocument12 pagesPrion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDMerari Lugo Ocaña100% (1)
- Fulltext Jmbmi v3 Id1023Document3 pagesFulltext Jmbmi v3 Id1023adinda.larastitiNo ratings yet
- Indicator of Dyscirculatory Encephalopathy in HypothyroidismDocument4 pagesIndicator of Dyscirculatory Encephalopathy in HypothyroidismresearchparksNo ratings yet
- Neurobiology of SchizophreniaDocument11 pagesNeurobiology of SchizophreniaJerry JacobNo ratings yet
- Braga-13 EOAD PSEN1 Clinica de SCADocument3 pagesBraga-13 EOAD PSEN1 Clinica de SCAMARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- The Successful Treatment of DisinhibitioDocument4 pagesThe Successful Treatment of DisinhibitioVicky NotesNo ratings yet
- Enfermedad de Hungtinton, Afectafción de Ganglios de La Base y Síntomas PsiquiátricosDocument7 pagesEnfermedad de Hungtinton, Afectafción de Ganglios de La Base y Síntomas PsiquiátricosLaura VargasNo ratings yet
- Enf de PickDocument11 pagesEnf de PickAnonymous QzobWmNo ratings yet
- Material Extra Sobre EH - Caso ÚnicoDocument10 pagesMaterial Extra Sobre EH - Caso ÚnicoLaura Andrea Roldan SanchezNo ratings yet
- Neurodevelopmental Risk Factors in SchizophreniaDocument9 pagesNeurodevelopmental Risk Factors in SchizophreniatiwiyunNo ratings yet
- Delirious Mania - An Approach To Diagnosis and TreatmentDocument10 pagesDelirious Mania - An Approach To Diagnosis and TreatmentJaviera Paz Guerrero CassanelloNo ratings yet
- Wjarr 2024 1024Document4 pagesWjarr 2024 1024mcvallespinNo ratings yet
- Fahr's Disease and Psychiatric Syndromes - A Case SeriesDocument3 pagesFahr's Disease and Psychiatric Syndromes - A Case SeriesubuntumicNo ratings yet
- Pisa Syndrome Source Clin Neuropharmacol SO 2015 Jul Aug 38 4 135 40 (PMIDT26166239)Document6 pagesPisa Syndrome Source Clin Neuropharmacol SO 2015 Jul Aug 38 4 135 40 (PMIDT26166239)dai shujuanNo ratings yet
- Behavioural-Variant Frontotemporal Dementia: An Update: Dementia E Neuropsychologia March 2013Document10 pagesBehavioural-Variant Frontotemporal Dementia: An Update: Dementia E Neuropsychologia March 2013claudiaNo ratings yet
- Conversion Disorder: The Brain's Way of Dealing With Psychological Conflicts. Case Report of A Patient With Non-Epileptic SeizuresDocument7 pagesConversion Disorder: The Brain's Way of Dealing With Psychological Conflicts. Case Report of A Patient With Non-Epileptic SeizuresMaria Von Shaft100% (1)
- 2017 - Ijaims - Psychiatric Comorbidities in Patients With EpilepsyDocument5 pages2017 - Ijaims - Psychiatric Comorbidities in Patients With EpilepsySantosh KumarNo ratings yet
- 1 s2.0 S0140673617312874 MainDocument15 pages1 s2.0 S0140673617312874 MainmeryemNo ratings yet
- Frontotemporaldementia: Nicholas T. Olney,, Salvatore Spina,, Bruce L. MillerDocument36 pagesFrontotemporaldementia: Nicholas T. Olney,, Salvatore Spina,, Bruce L. MillerDaniel MartinezNo ratings yet
- Neurologic Manifestations of Wilson's DiseaseDocument6 pagesNeurologic Manifestations of Wilson's DiseaseBarry SeeboNo ratings yet
- Bipolar Disorder and Epilepsy A Bidirectional Relation Neurobiological Underpinnings Current Hypotheses and Future Research DirectionsDocument14 pagesBipolar Disorder and Epilepsy A Bidirectional Relation Neurobiological Underpinnings Current Hypotheses and Future Research DirectionsRudolph MuliawanNo ratings yet
- Leukodystrophy Paper August 27thDocument7 pagesLeukodystrophy Paper August 27thZorbey TurkalpNo ratings yet
- Author 'S Accepted Manuscript: 10.1016/j.psym.2016.05.005Document40 pagesAuthor 'S Accepted Manuscript: 10.1016/j.psym.2016.05.005jose luisNo ratings yet
- Dementia FrontotemporalDocument24 pagesDementia FrontotemporalTeologia GamalielNo ratings yet
- Schneider-11 HD SimilaresDocument12 pagesSchneider-11 HD SimilaresMARIA MONTSERRAT SOMOZA MONCADANo ratings yet
- Fahr Syndrome PDFDocument9 pagesFahr Syndrome PDFRaluca-Andreea IgnatNo ratings yet
- Roberts Psychiatric 1992Document3 pagesRoberts Psychiatric 1992Drashua AshuaNo ratings yet
- Tab VS DFTDocument15 pagesTab VS DFTAntu NandaNo ratings yet
- Essential Tremor: Clinical PracticeDocument9 pagesEssential Tremor: Clinical PracticeDaniel Torres100% (1)
- A Case of Cycloid Psychotic Disorder: M C F, T S - F, B SDocument2 pagesA Case of Cycloid Psychotic Disorder: M C F, T S - F, B Syeremias setyawanNo ratings yet
- hadjsjDocument6 pageshadjsjadamilzaryNo ratings yet
- A New Familial Adult-Onset Leukodystrophy Manifesting As Cerebellar Ataxia and DementiaDocument9 pagesA New Familial Adult-Onset Leukodystrophy Manifesting As Cerebellar Ataxia and DementiaKristineNo ratings yet
- A Case of Sporadic Creutzfeldt-JakobDocument5 pagesA Case of Sporadic Creutzfeldt-JakobVlad PopescuNo ratings yet
- Neuroimaging in Bipolar DisorderDocument13 pagesNeuroimaging in Bipolar DisorderAngie GiraldoNo ratings yet
- Edwards Mark J Why Functional Neurological Disorder IsDocument11 pagesEdwards Mark J Why Functional Neurological Disorder IsSiddika PanjwaniNo ratings yet
- DELIRIUMDocument9 pagesDELIRIUMCaio AlvesNo ratings yet
- A Case of Psychosis Due To Fahr S Syndrome And.19Document3 pagesA Case of Psychosis Due To Fahr S Syndrome And.19VYNo ratings yet
- Creutzfeldt JakobDocument15 pagesCreutzfeldt JakobNicolas RodriguezNo ratings yet
- Case 40-2021 - A 9-Year-Old - Enf - MoyamoyaDocument10 pagesCase 40-2021 - A 9-Year-Old - Enf - MoyamoyaJuan C. Salazar PajaresNo ratings yet
- Bipolar AJMG 2003Document9 pagesBipolar AJMG 2003Gerald Lagi NgantukNo ratings yet
- Review of Hereditary and Acquired Rare ChoreasDocument24 pagesReview of Hereditary and Acquired Rare ChoreasleaNo ratings yet
- PIIS0885392412001224Document12 pagesPIIS0885392412001224Catinca DobroghiiNo ratings yet
- Neurobiology of Bipolar DisorderDocument9 pagesNeurobiology of Bipolar DisorderJerry JacobNo ratings yet
- Neuroimage: Clinical: SciencedirectDocument9 pagesNeuroimage: Clinical: SciencedirectMostafa FakhriNo ratings yet
- Greyson Alexander JNMD 2018Document4 pagesGreyson Alexander JNMD 2018Tibor AbaiNo ratings yet
- Case Report-Traducción LauraDocument4 pagesCase Report-Traducción LauraPablo GuzmánNo ratings yet
- Uncovering The Lifespan Neurobehavioral Comorbidities of EpilepsyDocument30 pagesUncovering The Lifespan Neurobehavioral Comorbidities of EpilepsydhruvaNo ratings yet
- GeneticsDocument10 pagesGeneticsapi-3835615No ratings yet
- Subacute Sclerosing Panencephalitis A Clinical and Pathological Study - 101 108Document7 pagesSubacute Sclerosing Panencephalitis A Clinical and Pathological Study - 101 108Bhanu PratapNo ratings yet
- Neurometabolic Hereditary Diseases of AdultsFrom EverandNeurometabolic Hereditary Diseases of AdultsAlessandro P. BurlinaNo ratings yet
- Magnetic Resonance Imaging: Key Points: CT ImagingDocument5 pagesMagnetic Resonance Imaging: Key Points: CT ImagingadamilzaryNo ratings yet
- Magnetic Resonance Imaging: Key Points: CT ImagingDocument7 pagesMagnetic Resonance Imaging: Key Points: CT ImagingadamilzaryNo ratings yet
- Magnetic Resonance Imaging: Key Points: CT ImagingDocument8 pagesMagnetic Resonance Imaging: Key Points: CT ImagingadamilzaryNo ratings yet
- Magnetic Resonance Imaging: Key Points: CT ImagingDocument8 pagesMagnetic Resonance Imaging: Key Points: CT ImagingadamilzaryNo ratings yet
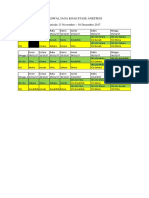
- Jadwal Jaga Koas Stase Anestesi Periode 13 November - 10 Desember 2017Document1 pageJadwal Jaga Koas Stase Anestesi Periode 13 November - 10 Desember 2017adamilzaryNo ratings yet
- University of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingDocument69 pagesUniversity of Saint Louis Tuguegarao City, Philippines: Maternal and Child Health NursingErica Veluz LuyunNo ratings yet
- Clinical Review: Common Skin Infections in ChildrenDocument5 pagesClinical Review: Common Skin Infections in ChildrenkhairaniNo ratings yet
- Yetmgeta Abdella 2018Document11 pagesYetmgeta Abdella 2018Shafici CqadirNo ratings yet
- Mental Status ExaminationDocument98 pagesMental Status ExaminationFatima 'No ratings yet
- Varicella Immunization CertDocument2 pagesVaricella Immunization CertShaikahamedNo ratings yet
- The OMT Classification of Congenital Anomalies - Michael A. TonkinDocument7 pagesThe OMT Classification of Congenital Anomalies - Michael A. TonkindougortoNo ratings yet
- Abstract Book PVSM2021 FinalDocument374 pagesAbstract Book PVSM2021 FinalnitaNo ratings yet
- Longrichglobal Retail or Maintenance BonusDocument1 pageLongrichglobal Retail or Maintenance BonusdxpfzbbcqvNo ratings yet
- Medical ReportsDocument1 pageMedical Reportsraheemtimo1No ratings yet
- Baroreflex Failure: A Neglected Type of Secondary HypertensionDocument5 pagesBaroreflex Failure: A Neglected Type of Secondary HypertensionMichel HaddadNo ratings yet
- Mamusha PDFDocument72 pagesMamusha PDFFikadu WendmtayeNo ratings yet
- A Study On Impact of Covid - 19 On Indian Pharmaceutical CompaniesDocument9 pagesA Study On Impact of Covid - 19 On Indian Pharmaceutical CompaniesAnonymous CwJeBCAXpNo ratings yet
- 432 eDocument404 pages432 eIJAZ M RAHMANNo ratings yet
- JACC Volume 78, Issue 11 SeptemberDocument122 pagesJACC Volume 78, Issue 11 SeptemberFareesha KhanNo ratings yet
- DivergentesDocument12 pagesDivergentesA LunaNo ratings yet
- Annotated Bibliography of Traditional Medicine Research Carried Out at DMR (LM) During 1965-2011Document271 pagesAnnotated Bibliography of Traditional Medicine Research Carried Out at DMR (LM) During 1965-2011AyeChan AungNo ratings yet
- Part 1 Module First Aid and CPRDocument25 pagesPart 1 Module First Aid and CPRWinter SongNo ratings yet
- Primer: Frozen ShoulderDocument16 pagesPrimer: Frozen ShoulderJose PerezNo ratings yet
- MEDICAL-REIUMBURSEMENT-G O Ms No 74Document19 pagesMEDICAL-REIUMBURSEMENT-G O Ms No 74cgr7880% (5)
- Pericardial Diseases: Dr. Abazie, Ugochi CDocument63 pagesPericardial Diseases: Dr. Abazie, Ugochi CUgochi AbazieNo ratings yet
- Flash CardsDocument793 pagesFlash CardsbtheresakNo ratings yet
- NatureDP 2015 Chronic Obstructive Pulmonary DiseaseDocument21 pagesNatureDP 2015 Chronic Obstructive Pulmonary DiseasePaloma GBNo ratings yet
- Cobas b101 PDFDocument6 pagesCobas b101 PDFGolden Flower ATLMNo ratings yet
- Lai Et Al-2016-Cochrane Database of Systematic ReviewsDocument181 pagesLai Et Al-2016-Cochrane Database of Systematic ReviewsIgnacia VergaraNo ratings yet
- The Principles of The Surgical Management of Gastric CancerDocument5 pagesThe Principles of The Surgical Management of Gastric CancerRobert ChristevenNo ratings yet
- MS2760 HiViral Mediu de Transport KitDocument2 pagesMS2760 HiViral Mediu de Transport KitLidia NarbNo ratings yet
- International Journal of Nursing Studies: Qi Lu, Jan Mårtensson, Yue Zhao, Linda JohanssonDocument8 pagesInternational Journal of Nursing Studies: Qi Lu, Jan Mårtensson, Yue Zhao, Linda JohanssonAbdul HadiNo ratings yet