Professional Documents
Culture Documents
SDCEP+OHAR+Quick+Ref+Guide+2pg
SDCEP+OHAR+Quick+Ref+Guide+2pg
Uploaded by
Anney Cherian DrimanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SDCEP+OHAR+Quick+Ref+Guide+2pg
SDCEP+OHAR+Quick+Ref+Guide+2pg
Uploaded by
Anney Cherian DrimanCopyright:
Available Formats
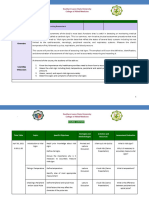
Oral Health Assessment and Review - Quick Reference Guide Oral Health Assessment and Review - Quick Reference
Oral Health Assessment and Review - Quick Reference Guide
Scottish Dental
Clinical Effectiveness Programme SDcep
Risk Assessment Personal Care Planning
Assigning a risk for the development of oral disease Points to consider in the development of a personal care plan
Oral Health Assessment and Review
Are any non-protective Disease Diagnosis Quick Reference Guide
modifying factors present? and Extent and Rate Clinical Findings
of Progression
Overview
YES NO
Risk Assessment Patient’s General Oral Health Focussed Oral
Are the modifying factors Personal Care Health
of clinical concern?
Assessment Health Review
Plan comprehensive specific elements only
YES NO
Assessment of
Care Options Patient Histories
Risk-based (e.g. patient advice, Personal details
Is disease present? Is disease present? Review Interval prevention, treatment, Social history
maintenance, referral) Dental history
Patient
Medical history
Preferences and Anxiety level
Expectations
YES NO YES NO
Assessment of Oral
Health Status
Is the disease of Is the disease of Variation in personal care plans for the three overall risk levels every 24 months Head and neck
Oral mucosal tissue at risk-based
clinical concern? clinical concern? for adults or
Periodontal tissue intervals
12 months for
Teeth between OHAs
High Risk Medium Risk Low Risk children Other (e.g. dentures)
YES NO
Enhanced Prevention Enhanced Prevention Standard Prevention
Diagnosis and Risk
YES
Interventive treatment Interventive treatment Assessment
and/or referral, if required and/or referral, if required Form diagnosis
Analyse risk information
NO
Short interval Medium interval
Focussed Oral Health Focussed Oral Health
Reviews to check risk areas, Reviews to check risk areas,
High Risk Medium Risk Low Risk compliance and review compliance and review Personal Care Plan
recall interval recall interval that is specific for the patient
Minimum interval of Minimum interval of and includes a risk-based
3 months 6 months interval for a Focussed Oral
between reviews between reviews Health Review
© Scottish Dental Clinical Effectiveness Programme Oral Health Assessment Oral Health Assessment Oral Health Assessment
at 24 months for adult, at 24 months for adult, at 24 months for adult,
Scottish Dental Clinical Effectiveness Programme 12 months for child 12 months for child 12 months for child
Dundee Dental Education Centre, Frankland Building, Small’s Wynd, Dundee DD1 4HN
Email scottishdental.cep@nes.scot.nhs.uk
Tel 01382 425751 / 425771 Note that for a new patient assessed as low risk, a conservative interval for Focussed Oral Health Reviews is advised For further details, refer to the Guidance in Brief and full guidance available at
Website www.scottishdental.org/cep initially which can be extended incrementally if no new problems are encountered. www.scottishdental.org/cep
ORAL - QUICK REF GUIDE.indd 1 16/03/2011 10:52
Modifying Factors
Oral Health Assessment and Review - Quick Reference Guide
Modifying factors include risk and protective factors, behaviours and clinical findings that
• Low saliva flow rate (dry mouth) Tooth Surface Loss
may be identified from patient histories or the assessment of oral health status. These factors
• Mucosal lesion present • Bruxism
are associated with the development of oral disease and conditions and should be considered
when determining the risk-based frequency of Focussed Oral Health Reviews. • Outdoor workers • Clinical evidence of tooth wear
• Tobacco use • High and/or frequent dietary acid intake (e.g. high consumption of acidic drinks such as
Patient Histories carbonated drinks, citrus fruit and fruit juices)
Periodontal Tissue
• Predisposing medical and drug factors: for example, impaired salivary production or
• Conditions that increase a patient’s risk of developing dental disease (e.g. diabetes, • Bony loss observed on sequential radiographs buffering ability; gastric reflux (often associated with Hiatus hernia); eating disorders
xerostomia as a result of, for example, Sjogrens syndrome, certain drugs or head and • BPE scores of 3,4,* in patients under 35 years of age such as anorexia nervosa, bulimia and pica; and the frequent use of some medicines
neck radiation therapy) • Concurrent medical factor that is directly affecting the periodontal tissues (e.g. and supplements such as steroid-containing asthma inhalers, vitamin C tablets and
• Conditions that might complicate dental treatment or the patient’s ability to maintain diabetes, stress, certain medication) effervescent preparations
their oral health (e.g. special needs or anxious, nervous, phobic conditions) • Evidence of gingivitis • Rapid progression of tooth wear
• Conditions where dental disease could put the patient’s general health at increased risk • Family history of chronic or aggressive (early onset/juvenile) periodontitis • Stress and/or anxiety
(e.g. patients on warfarin, immunosuppression)
• Family history of early tooth loss due to periodontal disease Tooth Abnormalities
• Excessive alcohol use (>21 units of alcohol per week for men; >14 units of alcohol per
• High % of bleeding on probing in relation to a low plaque index
week for women)
• Poor level of oral hygiene • Family history
• Family history of chronic or aggressive (early onset/juvenile) periodontitis
• Presence of plaque-retaining factors • Tooth abnormalities (tooth number, size, shape, colour)
• Ghukta, Paan (betel quid with tobacco), Areca nut use
• Previous history of treatment for periodontal disease
• High and/or frequent dietary acid intake Fluorosis
• Rapid periodontal breakdown >2mm attachment loss per year
• High and/or frequent sugar intake
• Root morphology that affects prognosis • Eating/licking toothpaste habit
• High caries rates in mother and siblings (applies to children only)
• Smoking 10+ cigarettes a day • Exposure to fluoridated water, in conjunction with other factors, up to 3 years of age
• Poor level of oral hygiene
• Inappropriate use of fluoride supplements or toothpaste
• Residence in a deprived (low SIMD) area Dental Caries
• Unsupervised toothbrushing (under 6 years)
• Tobacco use
• Anterior caries or restorations
• Use of ≥1000 ppm fluoride toothpaste (protective factor) Orthodontic Status
• Healthcare worker’s opinion (esp. children)
• Use of other sources of fluoride or resident in a water-fluoridated area (protective
• Heavily restored dentition • Canine in the line of the arch but failing to erupt, 10–13 years of age
factor)
• High and/or frequent sugar intake • Failure of teeth to erupt at the expected time
Head and Neck • High caries rates in mother and siblings (applies to children only) • First permanent molars of poor prognosis when hypodontia or skeletal discrepancy
• Low saliva flow rate (dry mouth) present
• Craniofacial abnormalities
• New lesions since last check-up • Palatally ectopic or buccally impacted canines
• Limited mouth opening
• Past root caries or large number of exposed roots • Patients requiring orthodontics as part of a multidisciplinary treatment plan
• Neck (lymph node) swelling
• Suspicious skin lesions (basal or squamous cell carcinomas, melanomas) • Poor dietary behaviours Dentures
• TMJ problems • Poor level of oral hygiene
• Premature extractions because of caries • Poor denture and oral hygiene
Oral Mucosal Tissue • Previous carious experience
• Betel quid chewing • Resident in an area of deprivation
• Diets low in fruit and vegetables • Use of ≥1000 ppm fluoride toothpaste (protective factor) Modifying factors are listed in alphabetical order.
• Excessive alcohol use (>21 units of alcohol per week for men; >14 units of alcohol per • Use of other sources of fluoride or resident in a water-fluoridated area (protective
week for women) factor)
ORAL - QUICK REF GUIDE.indd 2 16/03/2011 10:52
You might also like
- 2 Nursing Foundation II Including Health Assessment Module-Converted - 020222Document17 pages2 Nursing Foundation II Including Health Assessment Module-Converted - 020222Akshata BansodeNo ratings yet
- Par Index JurnalDocument10 pagesPar Index JurnalFaathir PutriNo ratings yet
- Clinical Practice Guidelines of Using Acupuncture For Low Back Pain PDFDocument13 pagesClinical Practice Guidelines of Using Acupuncture For Low Back Pain PDFdiegolsdcastroNo ratings yet
- Academic Audit: Suggested Methods To Assess Medical Teachers PerformanceDocument11 pagesAcademic Audit: Suggested Methods To Assess Medical Teachers Performancesp_rao2000No ratings yet
- School Nurse Powerpoint Presentation For PSADocument22 pagesSchool Nurse Powerpoint Presentation For PSAmarierose matugasNo ratings yet
- Opportunity and Benefits: Prof DR Tan Malaka, Moh, DRPH, Spok, Hiu Ketua Perhimpunan Profesi Higiene Industri IndonesiaDocument29 pagesOpportunity and Benefits: Prof DR Tan Malaka, Moh, DRPH, Spok, Hiu Ketua Perhimpunan Profesi Higiene Industri IndonesiaHamid FaoziNo ratings yet
- IH Monitoring Prof TanDocument29 pagesIH Monitoring Prof TanMuhammad Teguh DPNo ratings yet
- NCP LectureDocument38 pagesNCP Lecturesamarshahab320No ratings yet
- Background Methods: Review' (OHAR) Guidance in BriefDocument1 pageBackground Methods: Review' (OHAR) Guidance in BriefBibek RajNo ratings yet
- ACG Clinical Guidelines Management of Benign Anorectal DisordersDocument22 pagesACG Clinical Guidelines Management of Benign Anorectal DisordersCirugia Santa ClaraNo ratings yet
- Equality Work Plan PDFDocument16 pagesEquality Work Plan PDFGilbert KamanziNo ratings yet
- Part 1 Lec 5 A. Assessment of Nutrition Status Part 1Document20 pagesPart 1 Lec 5 A. Assessment of Nutrition Status Part 1Shikinah LaroyaNo ratings yet
- Autor Guidelines #Author-GuidelinesDocument4 pagesAutor Guidelines #Author-GuidelinesTeofilo Palsimon Jr.No ratings yet
- Pengenalan Mata Kuliah Diagnosa Gizi: Susetyowati, DCN.M.KesDocument38 pagesPengenalan Mata Kuliah Diagnosa Gizi: Susetyowati, DCN.M.Kesshienyoel100% (1)
- Proses Asuhan Gizi Terstandar (PAGT) Atau Nutrition Care Proc Ess (NCP)Document61 pagesProses Asuhan Gizi Terstandar (PAGT) Atau Nutrition Care Proc Ess (NCP)Indah RatnasariNo ratings yet
- Adj 67 S3Document11 pagesAdj 67 S3Wallacy MoraisNo ratings yet
- Nutrition Care ProcessDocument89 pagesNutrition Care ProcessRanier Ravyalo100% (2)
- Lesson PhysicalDocument22 pagesLesson PhysicalrumasadraunaNo ratings yet
- Unit PlanDocument10 pagesUnit PlankhhhhsamimNo ratings yet
- Nutrition Care ProcessDocument38 pagesNutrition Care ProcessChristelle Kay AsisNo ratings yet
- NCM 101 - Health AssessmentDocument15 pagesNCM 101 - Health AssessmentJhon Lazaga100% (1)
- Surgical Skin Preparation Quality Improvement Guide - AWDocument24 pagesSurgical Skin Preparation Quality Improvement Guide - AWali aliNo ratings yet
- Dental Caries Prevention and TreatmentDocument7 pagesDental Caries Prevention and TreatmentJOHN HAROLD CABRADILLANo ratings yet
- Paper Enfoque VortexDocument8 pagesPaper Enfoque VortexcNo ratings yet
- NCM 02 MidtermsDocument18 pagesNCM 02 Midtermss.bparzagaNo ratings yet
- Face Q Scales For Health Related Quality of Life Development and ValidationDocument12 pagesFace Q Scales For Health Related Quality of Life Development and ValidationRoxana MilicaNo ratings yet
- Abstract Success IndicatorsDocument9 pagesAbstract Success IndicatorsDR CYRUZNo ratings yet
- Nursing ProcessDocument4 pagesNursing Processkaylajw15No ratings yet
- SNLE Applicant GuideDocument20 pagesSNLE Applicant GuideJancy RaniNo ratings yet
- The Collecting and Analyzing Data Mind MapDocument1 pageThe Collecting and Analyzing Data Mind MapGel VillaverdeNo ratings yet
- Jurnal UtamaDocument5 pagesJurnal UtamaCynthia WihardjaNo ratings yet
- E RadiographsDocument2 pagesE Radiographsamila.zukanovicNo ratings yet
- School Health & Preventive Care Programs in India Jarma WellnessDocument3 pagesSchool Health & Preventive Care Programs in India Jarma WellnessJarma WellnessNo ratings yet
- Foundation Class PlanningDocument9 pagesFoundation Class Planningsourav deyNo ratings yet
- FOTTDocument6 pagesFOTTCarolina Lissette Poblete BeltránNo ratings yet
- Quality Assurance & ImprovementDocument8 pagesQuality Assurance & ImprovementBassam Al-HimiariNo ratings yet
- 3 Leadership and GovernanceDocument39 pages3 Leadership and GovernanceayeleNo ratings yet
- (According To Priority) (Cues & Evidences/ Objective & Subjective) (Objectives-Long Term & Short Term)Document1 page(According To Priority) (Cues & Evidences/ Objective & Subjective) (Objectives-Long Term & Short Term)opxNo ratings yet
- Empowerment of Individuals With Enduring Mental Health ProblemsDocument9 pagesEmpowerment of Individuals With Enduring Mental Health ProblemsNurulhikmah RoslanNo ratings yet
- UNDP - S7 - Labour Guidance Note - June2021Document43 pagesUNDP - S7 - Labour Guidance Note - June2021Mikaye WrightNo ratings yet
- O Brian 2011 PDFDocument13 pagesO Brian 2011 PDFmariaNo ratings yet
- Practice Advisory For Preanesthesia EvaluationDocument17 pagesPractice Advisory For Preanesthesia EvaluationAdrian WirahamediNo ratings yet
- Health Care Guideline-LaborDocument61 pagesHealth Care Guideline-LaborsitiurifahNo ratings yet
- PAMI Dosing Guide Nov.2.2020Document2 pagesPAMI Dosing Guide Nov.2.2020Rafael RiveraNo ratings yet
- Nutrition Lab Nutri Care ProcessDocument41 pagesNutrition Lab Nutri Care ProcessErika Anne Mercado CadawanNo ratings yet
- Course Plan Nursing Foundation Sem 2Document11 pagesCourse Plan Nursing Foundation Sem 2harpreetNo ratings yet
- Dieta e DiabetesDocument10 pagesDieta e DiabetesdramorimcostaNo ratings yet
- Skala Prilaku FranklDocument6 pagesSkala Prilaku FranklMeta Anjany FirmansyahNo ratings yet
- Laboratory Manual Nursing P PDFDocument280 pagesLaboratory Manual Nursing P PDFGeta KindsewNo ratings yet
- Health Education PlanDocument4 pagesHealth Education PlanKristine MerhanNo ratings yet
- 2021 OncologyNutrition Standards HighlightsDocument2 pages2021 OncologyNutrition Standards HighlightsPrincess Angie GonzalesNo ratings yet
- 65 FullDocument2 pages65 FullDavidNo ratings yet
- Screening Nutrition Care ProcessDocument70 pagesScreening Nutrition Care ProcessSiwonniekyubum DijaNo ratings yet
- Nutrition Care Process (NCP) : Dadang Arief PrimanaDocument105 pagesNutrition Care Process (NCP) : Dadang Arief Primanayoga saputraNo ratings yet
- Measuring Children's Dental Anxiety: Oral Cancer /paediatric DentistryDocument2 pagesMeasuring Children's Dental Anxiety: Oral Cancer /paediatric DentistryManda JoanNo ratings yet
- J Esthet Restor Dent - 2019 - Frese - The Dental Esthetic Screening Index A New Tool For Assessment of Dento FacialDocument11 pagesJ Esthet Restor Dent - 2019 - Frese - The Dental Esthetic Screening Index A New Tool For Assessment of Dento Facialsiti sunarintyasNo ratings yet
- NCP InterventionDocument17 pagesNCP InterventionNurul Huda HekmutiarNo ratings yet
- Treatment Planning in Restorative Dentistry and Implant ProsthodonticsFrom EverandTreatment Planning in Restorative Dentistry and Implant ProsthodonticsNo ratings yet
- Introduction to Clinical Effectiveness and Audit in HealthcareFrom EverandIntroduction to Clinical Effectiveness and Audit in HealthcareNo ratings yet
- Pranic PsychotherapyDocument57 pagesPranic Psychotherapyarjun crasto100% (2)
- Jsa For Radiography WorkDocument2 pagesJsa For Radiography WorkVipul ShankarNo ratings yet
- Catlist MMDocument19 pagesCatlist MMWilfredVincentNo ratings yet
- CraniectomyDocument5 pagesCraniectomytabanaoNo ratings yet
- Declaration Form - Work From Home Attachment 2Document1 pageDeclaration Form - Work From Home Attachment 2BAGUIO CATSNo ratings yet
- "After All, There Is Nothing As Interesting As People, and One Can Never Study Them Enough" Vincent Van GoghDocument38 pages"After All, There Is Nothing As Interesting As People, and One Can Never Study Them Enough" Vincent Van GoghAnonymous 1gH7ra9ANo ratings yet
- Trojan Battery Company Valve Regulated Lead Acid Battery Safety Data SheetDocument12 pagesTrojan Battery Company Valve Regulated Lead Acid Battery Safety Data SheetNels OdrajafNo ratings yet
- SynopsisDocument8 pagesSynopsisarunNo ratings yet
- Mini HabitsDocument33 pagesMini HabitsNeven Ilak100% (2)
- Rose Doe v. The City of New York, Et. Al.Document57 pagesRose Doe v. The City of New York, Et. Al.Daily Caller News FoundationNo ratings yet
- Condylar Fracture: Muhammad Tahoor D17015Document36 pagesCondylar Fracture: Muhammad Tahoor D17015Umair KhalidNo ratings yet
- BERSHAM AND ADWY GIRLS SCHOOL LOGS. Book 2 August 1889 - JANUARY 1915Document80 pagesBERSHAM AND ADWY GIRLS SCHOOL LOGS. Book 2 August 1889 - JANUARY 1915Annette EdwardsNo ratings yet
- NIRS-InVOS - Reference - Guide For Pediatric UseDocument50 pagesNIRS-InVOS - Reference - Guide For Pediatric UseRaluca LNo ratings yet
- Injury Biomechanics: AAMIR SOHAIL - Student ID 163101039 - December 16, 2016Document12 pagesInjury Biomechanics: AAMIR SOHAIL - Student ID 163101039 - December 16, 2016Aamir SohailNo ratings yet
- A Study of Work Life Balance of Female Employee With Refrence To HDFC Bank at MoradabadDocument72 pagesA Study of Work Life Balance of Female Employee With Refrence To HDFC Bank at MoradabadbuddysmbdNo ratings yet
- Applied PsychologyDocument362 pagesApplied Psychologyprajjwal100% (1)
- Preparation For An Alpine Ascents' Mount Everest ClimbDocument3 pagesPreparation For An Alpine Ascents' Mount Everest ClimbjosethompsonNo ratings yet
- Training Tips For Hypertrophy - Renaissance Periodization - Dr. Mike IsraetelDocument7 pagesTraining Tips For Hypertrophy - Renaissance Periodization - Dr. Mike IsraetelShrenik NaharNo ratings yet
- Chris Hemsworth's God-Like Thor WorkoutDocument8 pagesChris Hemsworth's God-Like Thor WorkoutmarticarrerasNo ratings yet
- NMC Eligibililty ApplicationDocument2 pagesNMC Eligibililty ApplicationYergnoirNo ratings yet
- Rehabilitation MedicaleDocument458 pagesRehabilitation MedicaleactoneNo ratings yet
- Written Report Abnormal PsychologyDocument23 pagesWritten Report Abnormal PsychologyCy Esquibel LingaNo ratings yet
- Lab Report For ParacetamolDocument5 pagesLab Report For Paracetamol9gcfz8zf9xNo ratings yet
- 1574-Article Text-2641-1-10-20181107Document5 pages1574-Article Text-2641-1-10-20181107Faraz HaiderNo ratings yet
- Monitoring The Fermentation of GlucoseDocument4 pagesMonitoring The Fermentation of GlucoseSonia IsaacsNo ratings yet
- Child Rights and You - Wikipedia PDFDocument14 pagesChild Rights and You - Wikipedia PDFpatel mariyamNo ratings yet
- Cowan 1999Document20 pagesCowan 1999ggggggggggg32No ratings yet
- Behcet's Disease (Adamantiades Syndrome) : DefinitionDocument9 pagesBehcet's Disease (Adamantiades Syndrome) : DefinitionNuzairah AynoorNo ratings yet
- Kit For Human Thyroid Stimulating Hormone (HTSH) : Irmak-9Document2 pagesKit For Human Thyroid Stimulating Hormone (HTSH) : Irmak-9micky mouseNo ratings yet
- Admissions RequirementsDocument3 pagesAdmissions Requirementsjames singwahNo ratings yet