Professional Documents
Culture Documents
Laporan Kasus
Laporan Kasus
Uploaded by
Novia DamayantiCopyright:
Available Formats
You might also like
- Physics1100 Lab Manual (Iolab Revision)Document105 pagesPhysics1100 Lab Manual (Iolab Revision)Tri NguyenNo ratings yet
- English File Fourth Edition Intermediate WorkbookDocument82 pagesEnglish File Fourth Edition Intermediate WorkbookАнатоль БумберсNo ratings yet
- A Rare Cause of Hearing Loss: Susac SyndromeDocument3 pagesA Rare Cause of Hearing Loss: Susac SyndromeBeny Pratama SidabutarNo ratings yet
- Angioinvasive Cerebral Aspergillosis Presenting As Acute Ischaemic Stroke in A Patient With Diabetes MellitusDocument4 pagesAngioinvasive Cerebral Aspergillosis Presenting As Acute Ischaemic Stroke in A Patient With Diabetes MellitusKamil HannaNo ratings yet
- Nutrimentum Vascularum As Pulsatile TinnitusDocument6 pagesNutrimentum Vascularum As Pulsatile TinnitusJuthika Rai ShettyNo ratings yet
- Tuli Mnedadak NcbiDocument6 pagesTuli Mnedadak NcbiMiss AmyNo ratings yet
- Tinnitus Update 2021Document10 pagesTinnitus Update 2021tumi maryNo ratings yet
- Seminar: Benjamin E Schreiber, Charlotte Agrup, Dorian O Haskard, Linda M LuxonDocument9 pagesSeminar: Benjamin E Schreiber, Charlotte Agrup, Dorian O Haskard, Linda M Luxonmaria_garaveNo ratings yet
- Neuroanatomical Considerations of Isolated Hearing Loss in Thalamic HemorrhageDocument3 pagesNeuroanatomical Considerations of Isolated Hearing Loss in Thalamic HemorrhageBella Cynthia BettabestariNo ratings yet
- Schwannoma Vestibular TinnitusDocument6 pagesSchwannoma Vestibular TinnitusThomasMáximoMancinelliRinaldoNo ratings yet
- Original Article: Study of Computed Tomography (CT) Scan Finding in Neurofibromatosis Type 2Document4 pagesOriginal Article: Study of Computed Tomography (CT) Scan Finding in Neurofibromatosis Type 2Lisa SariNo ratings yet
- Musical Hallucinations Following Insular Glioma Resection: Case ReportDocument4 pagesMusical Hallucinations Following Insular Glioma Resection: Case ReportMalcoci MihaiNo ratings yet
- Laporan KasusDocument4 pagesLaporan KasusNovia DamayantiNo ratings yet
- American Journal of OtolaryngologyDocument4 pagesAmerican Journal of OtolaryngologyDear Farah SielmaNo ratings yet
- Decreased Consciousness Bithalamic InfarcDocument3 pagesDecreased Consciousness Bithalamic InfarcshofidhiaaaNo ratings yet
- Bilateral Sudden Sensorineural Hearing Loss: Review: Sasara, B M Teh, P FriedlandDocument12 pagesBilateral Sudden Sensorineural Hearing Loss: Review: Sasara, B M Teh, P FriedlandMariaAmeliaGoldieNo ratings yet
- Traumatic Ossicular Dislocations: Etiology and ManagementDocument6 pagesTraumatic Ossicular Dislocations: Etiology and ManagementlawrensiusrNo ratings yet
- AICA InfarctDocument6 pagesAICA InfarctReynard FebrianNo ratings yet
- Management of Adult Sensorineural Hearing Loss: EtiologiesDocument10 pagesManagement of Adult Sensorineural Hearing Loss: EtiologiesaldimugniNo ratings yet
- A Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary PancreatitisDocument5 pagesA Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary Pancreatitisbijnn journalNo ratings yet
- Main PDFDocument3 pagesMain PDFanton MDNo ratings yet
- Vocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDocument4 pagesVocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDivine Jane PurciaNo ratings yet
- IJC Heart & VasculatureDocument2 pagesIJC Heart & VasculatureGledia LindaNo ratings yet
- Artery of Percheron Infarct: An Acute Diagnostic Challenge With A Spectrum of Clinical PresentationsDocument9 pagesArtery of Percheron Infarct: An Acute Diagnostic Challenge With A Spectrum of Clinical PresentationsMaria JimenezNo ratings yet
- 3504-Article Text-11497-1-10-20200318Document3 pages3504-Article Text-11497-1-10-20200318Ade Puji AstutiNo ratings yet
- J Clinph 2013 03 031Document7 pagesJ Clinph 2013 03 031Andres Rojas JerezNo ratings yet
- Tinnitus PDFDocument10 pagesTinnitus PDFАлександра КондряNo ratings yet
- SD GradiDocument3 pagesSD GradiPabloMrchNo ratings yet
- Auricula 2 PDFDocument27 pagesAuricula 2 PDFCamy Alejandra Gonzales GonzalesNo ratings yet
- Neuro 0392-100X-30-217Document5 pagesNeuro 0392-100X-30-217pauloNo ratings yet
- Sudden Deafness JournalDocument2 pagesSudden Deafness JournalRestiNo ratings yet
- Acu Accident LumbarDocument2 pagesAcu Accident Lumbarrswongym449No ratings yet
- Neuro4Nurses Acustic NeuromaDocument2 pagesNeuro4Nurses Acustic Neuromaputri auliyahNo ratings yet
- Otology: Special Paper in Celebration of Prof. Yang'S 50 Years Career in MedicineDocument6 pagesOtology: Special Paper in Celebration of Prof. Yang'S 50 Years Career in Medicinechipta lestariNo ratings yet
- Epilepsy & Behavior Case Reports: 10.1016/j.ebcr.2017.07.003Document21 pagesEpilepsy & Behavior Case Reports: 10.1016/j.ebcr.2017.07.003Faras ArinalNo ratings yet
- D Evaluation For Resective Epilepsy SurgeryDocument104 pagesD Evaluation For Resective Epilepsy SurgeryYusuf BrilliantNo ratings yet
- Neewzealand JournalDocument5 pagesNeewzealand JournalFuji Seprinur HidayatNo ratings yet
- Posterior Reversible Encephalopathy Syndrome After Lumbar PunctureDocument2 pagesPosterior Reversible Encephalopathy Syndrome After Lumbar PunctureMedtext PublicationsNo ratings yet
- Case Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationDocument16 pagesCase Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationLídia YoshiharaNo ratings yet
- Dapus 9Document9 pagesDapus 9martina marthaNo ratings yet
- Presentasi Kasus Sudden Deafness Dhana 2017Document9 pagesPresentasi Kasus Sudden Deafness Dhana 2017Pradhana FwNo ratings yet
- Mus 27395Document9 pagesMus 27395Denis Jesus Salgado GutierrezNo ratings yet
- TinitusDocument4 pagesTinitusFridaZorayaNo ratings yet
- Journal of Clinical NeuroscienceDocument3 pagesJournal of Clinical NeurosciencejicarrerNo ratings yet
- Acoustic NeuromaDocument6 pagesAcoustic NeuromaMartha AsikoNo ratings yet
- MRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyDocument3 pagesMRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyJan JanNo ratings yet
- The FACIAL NERVE Current Trends in Diagnosis, Treatment, and RehabilitationDocument17 pagesThe FACIAL NERVE Current Trends in Diagnosis, Treatment, and RehabilitationkrazeedoctorNo ratings yet
- Jurding Elmo H3a021009Document39 pagesJurding Elmo H3a021009Elmo KrisnawanNo ratings yet
- Fneur 13 962376Document8 pagesFneur 13 962376Miss AmyNo ratings yet
- Lee 2015Document12 pagesLee 2015Bagus Pithu Ha SpingNo ratings yet
- Sudden Deafness 2Document8 pagesSudden Deafness 2Aldhi Putra PradanaNo ratings yet
- Meniere DiseaseDocument16 pagesMeniere DiseaseNavjot Brar100% (2)
- Spectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioDocument4 pagesSpectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioImroatul hafidzahNo ratings yet
- Trigeminal Neuralgia A Case Report With Review of LiteratureDocument4 pagesTrigeminal Neuralgia A Case Report With Review of LiteratureFauziah KautsaraNo ratings yet
- Oliveira 2020Document5 pagesOliveira 20202907tranthaonguyenNo ratings yet
- 3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftDocument5 pages3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftabhishekbmcNo ratings yet
- Bilateral Vestibular Schwannoma Associated Neurofibromatosis Type 2Document1 pageBilateral Vestibular Schwannoma Associated Neurofibromatosis Type 2Anonymous ocfZSRrrONo ratings yet
- AcousticNeuromaVestibularSchwannoma StatPearls NCBIBookshelfDocument6 pagesAcousticNeuromaVestibularSchwannoma StatPearls NCBIBookshelfarifbudipraNo ratings yet
- Neurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL TjiaDocument6 pagesNeurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL Tjiarani suwadjiNo ratings yet
- Planum Sphenoidal MeningiomaDocument5 pagesPlanum Sphenoidal MeningiomaNidya TiazNo ratings yet
- Echography and Doppler of the BrainFrom EverandEchography and Doppler of the BrainChiara RobbaNo ratings yet
- SGD Case 2 Written Output-1Document19 pagesSGD Case 2 Written Output-1Jam PanumpangNo ratings yet
- Low-Loss Power Splitters - Multi-Band 800 - 2500 MHZ 860 10017, 860 10018, 860 10019Document1 pageLow-Loss Power Splitters - Multi-Band 800 - 2500 MHZ 860 10017, 860 10018, 860 10019Zoheir KacimiNo ratings yet
- (2024년 예상) 다정고등학교 (세종 전체) 1-1 중간 영어 족보 (천재 (김태영) ) (Q) 2회Document11 pages(2024년 예상) 다정고등학교 (세종 전체) 1-1 중간 영어 족보 (천재 (김태영) ) (Q) 2회y2un.t1130No ratings yet
- I Cannot Live With You PoemsDocument4 pagesI Cannot Live With You PoemsDaeng ArifNo ratings yet
- 490806Document2 pages490806Informative InsaanNo ratings yet
- Original Research Paper Geography: M.A Geography, UGC NET-JRF (Government P.G College Badli, Haryana)Document4 pagesOriginal Research Paper Geography: M.A Geography, UGC NET-JRF (Government P.G College Badli, Haryana)neeraj kumarNo ratings yet
- Stolarska Radionica - Procjena Troškova: Vrsta Naziv Slika Link Cijena Total VrstaDocument7 pagesStolarska Radionica - Procjena Troškova: Vrsta Naziv Slika Link Cijena Total VrstaMarko PalicNo ratings yet
- IW2P1Document3 pagesIW2P1Eong Huat Corporation Sdn BhdNo ratings yet
- Magallona Vs ErmitaDocument13 pagesMagallona Vs ErmitaERNIL L BAWA100% (1)
- Nanazoxid 0Document5 pagesNanazoxid 0hnn9gfqzqxNo ratings yet
- L A Level Physics A MS Jun 07 Old g481Document88 pagesL A Level Physics A MS Jun 07 Old g481dasha962No ratings yet
- Safety-Overall MEO Class 4 Part BDocument21 pagesSafety-Overall MEO Class 4 Part Blazyreaderr100% (1)
- Apple Airpods Max Complete Features Instructions ManualDocument7 pagesApple Airpods Max Complete Features Instructions ManualIlaria iudiceNo ratings yet
- Inta Commercial Collection April 2011Document59 pagesInta Commercial Collection April 2011Robin FisherNo ratings yet
- Certificate of Calibration: Customer InformationDocument2 pagesCertificate of Calibration: Customer InformationSazzath HossainNo ratings yet
- Astm A570 1979Document5 pagesAstm A570 1979set_ltdaNo ratings yet
- X-Ray For BoneDocument2 pagesX-Ray For BoneLILISNo ratings yet
- Zernack Et Al 2009. Sedimentary Signatures of Cyclic Growth and Destruction of Stratovolcanoes. A Case Study From Mt. Taranaki, New Zealand PDFDocument18 pagesZernack Et Al 2009. Sedimentary Signatures of Cyclic Growth and Destruction of Stratovolcanoes. A Case Study From Mt. Taranaki, New Zealand PDFAndres Almanza SoteloNo ratings yet
- KhatDocument1 pageKhatricomusongNo ratings yet
- 16216l5 16494Document2 pages16216l5 16494Saul AlbertoNo ratings yet
- Science and Technology Research Partnership For Sustainable Development (Satreps) Proposal On Iot X SDG X IndonesiaDocument6 pagesScience and Technology Research Partnership For Sustainable Development (Satreps) Proposal On Iot X SDG X IndonesiaelektroftuhNo ratings yet
- Manual Lab e Coli Lab 6Document9 pagesManual Lab e Coli Lab 6Siti Mastura Abdul RahmanNo ratings yet
- SketchUp Tutorial 1 - TableDocument19 pagesSketchUp Tutorial 1 - TablenphilippNo ratings yet
- Lesson Plan Preparing For Parenthood Pregnancy and Labor - 0Document15 pagesLesson Plan Preparing For Parenthood Pregnancy and Labor - 0Sweta ManandharNo ratings yet
- Hspice Simulation of SRAM PDFDocument65 pagesHspice Simulation of SRAM PDFYatheesh KaggereNo ratings yet
- Annual Day AnchoringDocument5 pagesAnnual Day AnchoringPooja ChuriwalNo ratings yet
- Brunnstrom's ApproachDocument37 pagesBrunnstrom's Approachdexter veracityNo ratings yet
- Arne JaconsenDocument20 pagesArne JaconsenXavier Ernesto100% (1)
Laporan Kasus
Laporan Kasus
Uploaded by
Novia DamayantiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laporan Kasus
Laporan Kasus
Uploaded by
Novia DamayantiCopyright:
Available Formats
TYPE Case Report
PUBLISHED 05 May 2023
DOI 10.3389/fmed.2023.1174512
Case report: Bilateral sudden
OPEN ACCESS deafness in acute middle
cerebellar peduncle infarction:
EDITED BY
Wen-Jun Tu,
Chinese Academy of Medical Sciences and
Peking Union Medical College, China
REVIEWED BY
central or peripheral?
Jeremy Hornibrook,
University of Canterbury, New Zealand
Yongwei Zhang, Ziyun Yuan1 , Lei Xiang2 , Ran Liu2 and Wei Yue1,2*
Second Military Medical University, China
1
Enis Alpin Guneri, Clinical College of Neurology, Neurosurgery and Neurorehabilitation, Tianjin Medical University, Tianjin,
Dokuz Eylül University, Türkiye China, 2 Department of Neurology, Tianjin Huanhu Hospital, Tianjin, China
*CORRESPONDENCE
Wei Yue
hhyuewei2008@163.com Background: The middle cerebellar peduncle (MCP) is the most common site
RECEIVED 26 February 2023 associated with hearing impairment in acute ischaemic stroke. Narrowing or
ACCEPTED 13 April 2023 occlusion of the vertebrobasilar artery due to atherosclerosis is thought to be the
PUBLISHED 05 May 2023
main pathogenesis of MCP infarction. Most previous reports of MCP infarction
CITATION
have not been clear whether the patient’s hearing impairment is localized to the
Yuan Z, Xiang L, Liu R and Yue W (2023) Case
report: Bilateral sudden deafness in acute center or periphery.
middle cerebellar peduncle infarction: central
Case presentation: We report 44-year-old man with vertigo, tinnitus, and bilateral
or peripheral? Front. Med. 10:1174512.
doi: 10.3389/fmed.2023.1174512 sudden sensorineural hearing loss (SSNHL) as the first symptoms. Pure Tone
COPYRIGHT
Audiogram revealed complete hearing loss in both ears. Acute bilateral MCP
© 2023 Yuan, Xiang, Liu and Yue. This is an infarction was diagnosed by repeated brain magnetic resonance imaging (MRI).
open-access article distributed under the terms The brainstem auditory evoked potential (BAEP) and the electrocochleography
of the Creative Commons Attribution License
(CC BY). The use, distribution or reproduction
were normal. The otoacoustic emissions showed binaural cochlear dysfunctions.
in other forums is permitted, provided the After the antiplatelet, lipid-lowering, steroids and hyperbaric oxygen therapy, the
original author(s) and the copyright owner(s) pure-tone average (PTA) showed a clear improvement with 67 decibels (dB) on
are credited and that the original publication in
this journal is cited, in accordance with
the right and 73 dB on the left at the 3-month follow-up.
accepted academic practice. No use, Conclusion: Vertebrobasilar diseases due to atherosclerosis should be routinely
distribution or reproduction is permitted which
does not comply with these terms.
considered in middle-aged and elderly patients with vascular risk factors and
bilateral hearing loss. Bilateral SSNHL can be a prodrome of acute MCP infarction
and it can be peripheral. Brain MRI, brain magnetic resonance angiogram (MRA),
brain and neck computed tomography angiography (CTA), BAEP, otoacoustic
emissions, and Pure Tone Audiogram help to localize and qualify the diagnosis.
Bilateral SSNHL localized to the periphery usually improves better and has
a good prognosis. Early detection of hearing loss and intervention can help
patients recover.
KEYWORDS
bilateral sudden sensorineural hearing loss, middle cerebellar peduncle infarction,
anterior inferior cerebellar artery, audiological examination, cochlear, prognosis
1. Introduction
SSNHL refers to a rapid-onset hearing loss occurring within 3 days, with
hearing loss ≥30 dB in at least three contiguous audiometric frequencies (1).
The global annual incidence of SSNHL is approximately 5–27 per 100,000
people, in which hearing impairment is commonly unilateral (2). Viral
infection, vascular occlusion, and autoimmune diseases have been implicated as
Frontiers in Medicine 01 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
causes of SSNHL, with vascular occlusion being one of the most otoacoustic emissions showed binaural cochlear dysfunctions.
common causes in older patients (3). The internal auditory artery Bithermal caloric test indicated bilateral horizontal semicircular
(IAA), which supplies blood to the inner ear, originates from canal low-frequency dysfunction.
the vertebral basilar artery system, commonly from the anterior The patient’s symptoms improved after several days of
inferior cerebellar artery (AICA), or less commonly from the basilar antiplatelet, lipid-lowering, steroids and hyperbaric oxygen
artery (BA), and infrequently from the posterior inferior cerebellar therapy. The patient was given oral prednisone at a dose of 60 mg
artery (PICA). The IAA is a long and slender terminal artery for 4 consecutive days, followed by a reduction of 10 mg every 2
without collateral circulation, which is why sudden deafness is days. Hyperbaric oxygen therapy was administered once a day for
possibly a prodrome of AICA stenosis or occlusion. Almost all the 10 sessions. Three months later, Pure Tone Audiogram showed
MCP is supplied by the AICA; therefore, bilateral MCP infarcts that SSNHL persisted; however, there was a clear improvement,
may be accompanied by hearing loss. Patients with MCP infarction with PTA average of 67 dB on the right and 73 dB on the left
who present with SSNHL are less likely to be reported due to (Figure 1B). The speech audiometry showed 55 dB with 100%
the omission of audiological examination, especially in the case of speech discrimination on the right and 60 dB with 100% speech
bilateral hearing loss where patients tend to overlook mild hearing discrimination on the left. His left-limb strength and coordination
loss. And the hearing loss revealed by PTA alone in some cases is improved steadily over 3 months. The patient had no complaints at
not sufficient to confirm whether it is central or peripheral. Here, we the 2-year follow-up visit to the stroke outpatient clinic. However,
report on a patient with vertigo, tinnitus, and SSNHL as a prodrome the patient continued to experience bilateral hearing loss, without
of acute MCP infarction, and demonstrate the localization of any new neurological events. Unfortunately, we did not have access
bilateral deafness. to his new PTA results at the 2-year follow-up. A time-course
diagram of disease progression is shown in Figure 3.
2. Case presentation
3. Discussion
A 44-year-old man with hypertension, suddenly developed
vertigo, tinnitus, and bilateral hearing loss 1 day before admission. Bilateral SSNHL is rare, accounting for approximately 4.9% of
The patient was hospitalized in Tianjin Huanhu Hospital after all SSNHL (3), and cerebrovascular disease is more likely to be
the above symptoms persisted without improvement. Up on overlooked in this group of patients. When patients present with
physical examination, he did not have dysarthria, limb weakness, vertigo and sudden hearing loss without other neurological signs
ataxia, or spontaneous nystagmus, but sustained horizontal gaze- and symptoms, they are usually first seen in the ENT department.
evoked nystagmus to the right or left in both eyes, abnormal In a retrospective analysis of 103 case reports associated with
horizontal head impulse test and absent skew. PTA showed a bilateral SSNHL, the vascular condition was diagnosed as a
total SSNHL of 112 dB in the right ear and 115 dB in the pathophysiological factor in 17 patients (16.5%) (8). Vertigo and
left ear (Figure 1A), and no infarct foci were found on the sudden hearing loss are the only signs of early AICA stroke
head MRI. (9), and AICA territory is most commonly associated with
Three days after the initial onset of the hearing loss and hearing disorders.
vertigo, the patient’s symptoms worsened. Clinical neurological Bilateral sudden hearing loss with acute MCP infarction
examination revealed cerebellar dysarthria, gaze-evoked has been described in several reports, of which audiological
nystagmus, and ataxia. Reexamination of the brain MRI examinations were performed in three cases (Table 1) (4–7). All
demonstrated an acute infarction in the bilateral cerebellum patients were middle-aged to elderly, with a mean age of 57.3
(Figures 2A, B). years and with a male-to-female ratio of 3:1. Mid-total hearing
After 10 days of hospitalization, the patient developed left- impairment and vertigo were the most common symptoms, with
limb weakness and worsening ataxia. A brain MRI revealed a new facial palsy (n = 1), facial sensory disturbance (n = 1), ataxia
acute infarction extending to the bilateral MCP (Figures 2C, D). (n = 3), and nystagmus (n = 4), also reported. All new AICA
Laboratory results indicated hyperlipidemia with plasma total infarcts were seen from 0 to 7 days after the onset of symptoms,
cholesterol (TC) 7.05 mmol/L and low-density lipoprotein such as hearing loss. Two patients (patients 2, 4) had moderately
cholesterol (LDL-C) 4.30 mmol/L. Brain and neck CTA showed severe to total hearing loss with normal BAEP, and our patient
occlusion of the bilateral vertebral artery (VA) V3 segment, had normal electrocochleography, abnormal otoacoustic emissions
proximal V4 segment, and bilateral AICA as well as severe stenosis indicating cochlear dysfunction and horizontal semicircular canal
of the distal left VA V4 segment (Figures 2E, F). The BEAP low-frequency dysfunction; one patient (patient 3) had moderate
showed normal elicitation of I, III, and V waves, as well as to moderately severe hearing loss with good speech discrimination.
normal waveforms and amplitudes in each wave, and latencies All these findings suggested that the hearing impairment was
and interpeak latencies within the normal range on day 14. localized to the cochlea, and the central system function was
The electrocochleogram showed the binaural SP/AP ratio in the intact. The patients’ other neurological symptoms were mild and
normal range at 90 dBnHL, with the left ear SP/AP ratio of most of the hearing impairment had improved significantly (mild
0.33 and the right ear SP/AP ratio of 0.25 (Figure 1C). The to severe hearing loss) at follow-up. Patients are detected early,
tympanogram type was A, without the stapedial reflex bilaterally. without vertigo, with mild hearing loss and an upwards-sloping
Transient evoked otoacoustic emissions and distortion product audiogram, which is considered to be associated with a good
Frontiers in Medicine 02 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
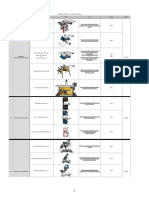
FIGURE 1
(A) PTA on admission: total SSNHL in both ears: 112 dB on the right and 115 on the left. (B) PTA after 3-month follow-up: severe hearing loss in both
ears: 67 dB on the right and 73 on the left. (C) The electrocochleogram showed the binaural SP/AP ratio in the normal range at 90 dBnHL, with the
left ear SP/AP ratio of 0.33 and the right ear SP/AP ratio of 0.25. PTA, pure-tone average; SSNHL, sudden sensorineural hearing loss; dB, decibel; SP,
summating potential; AP, action potential; dBnHL, decibel normal hearing level; R, right; L, left.
Frontiers in Medicine 03 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
FIGURE 2
(A, B) 3rd day, diffusion-weighted MRI showed hyperintense foci at the bilateral cerebellum; (C, D) 10 days later, diffusion-weighted MRI showed new
hyperintense foci at the bilateral MCP; (E, F) brain and neck CTA revealed occlusion of the bilateral VA V3 segment, proximal V4 segment and bilateral
AICA, severe stenosis of the distal left VA V4 segment. MRI, magnetic resonance imaging; MCP, middle cerebellar peduncle; CTA, computed
tomography angiography; VA, vertebral artery; AICA, anterior inferior cerebellar artery.
FIGURE 3
Time course of the disease. Diagram illustrating time course of disease in our patient. PTA, pure-tone average; R, right; L, left; MRI, magnetic
resonance imaging; MCP, middle cerebellar peduncle.
prognosis (10). Timely treatment of steroids and hyperbaric oxygen loss with MCP infarction demonstrated that mild hearing loss
therapy can help hearing recovery (11). Previous studies have with severely impaired speech discrimination and absence of
reported an improvement rate of 69.2% for the treatment of auditory evoked responses are typical findings in central lesions
idiopathic SSNHL with hyperbaric oxygen in combination with such as stroke affecting the vestibulocochlear nucleus (12). Another
intravenous steroids (11). Lee et al. in their summary of hearing patient (patient 1), with bilateral PTA ≥ 95 dB showed absence
Frontiers in Medicine 04 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
TABLE 1 Reviewing the literature on bilateral MCP with audiological examination.
References Bovo et al. (4) Renard et al. (5) Lee et al. (6) Present study
No. Patient 1 Patient 2 Patient 3 Patient 4
Age 65 54 66 44
Gender Female Male Male Male
Risk factors H, CA H, HC, S D H
Vertigo (+) (+) (+) (+)
Ear symptoms Binaural tinnitus and Bilateral SSNHL Bilateral SSNHL, tinnitus in right Binaural tinnitus and SSNHL
SSNHL ear
Nystagmus Horizontal right-beating Gaze-evoked nystagmus Spontaneous left-beating nystagmus Gaze-evoked nystagmus
nystagmus
Other symptoms and signs - Ataxia Diminished right-sided facial Ataxia
sensation; right peripheral facial
palsy; ataxia
Grades of hearing loss (7) Total hearing loss Profound hearing loss Moderate (L), moderately severe (R) Total hearing loss
hearing loss
Which ear Both Both Both Both
Degree (dB HL) R, L ≥ 95 R 80; L > 90 R 55; L 45 R, L ≥ 95
Bithermal caloric test - - right horizontal semicircular canal Bilateral horizontal semicircular
low-frequency dysfunction canal low-frequency dysfunction
BAEP Absent at the maximum Normal - Normal
intensity
Localization of hearing loss Central or mixed Cochlea Cochlea Cochlea
mechanism
Lesion location Bilateral MCP Bilateral MCP and the Bilateral MCP, right lateral pons Bilateral occipital lobe and
anterior inferior cerebellum cerebellum, left thalamus and
bilateral MCP
Vascular abnormality MRA, brain angiograms: MRA, CTA: multifocal MRA: moderately severe stenosis of CTA: occlusion of the bilateral VA
occlusion of BA vertebrobasilar stenosis distal RVA and the middle third of V3, proximal V4 and bilateral AICA,
BA stenosis at the distal LVA V4
Follow up no improvement in the - Vertigo, nausea and the level of the levels of hearing recovery in the
auditory threshold after hearing recovery in the left ear was both ears were slight improvement
10 months partial recovery at discharge after 3 months
D, diabetes; H, hypertension; CA, cerebrovascular accident; HC, hypercholesteremia; S, smoke; -, not obtained; R, right; L, left; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol;
TIA, transient ischemic attack.
of otoacoustic emissions, no waveforms in BAEP, and bilateral the IAA is occluded at an early stage, it may only present with
MCP infarction involving the bilateral cochlear and inferior hearing loss or vertigo without the formation of intracerebral
vestibular nucleus. The patient’s hearing loss was considered to infarction. This situation should alert physicians. When the patient
be central or mixed and her recovery was found to be poor at presents with hearing loss but no infarct foci on head MRI, and
the 10-month follow-up. The audiogram showed no change in a three-step bedside oculomotor exam do not all suggest central
auditory threshold. disease, the patient should be closely monitored for changes in
All patients had one or more risk factors associated the condition and possible subsequent AICA infarction. Our
with systemic diseases, such as hypertension, diabetes, or patient’s initial symptoms were vertigo, tinnitus and bilateral
hyperlipidemia. This is consistent with the literature, which hearing loss, with no significant abnormalities on the head MRI.
reported that 38% of bilateral SSNHL were associated with There was a change in condition on days 3 and 10, and the
such systemic diseases (13). Most angiographic findings were repeated head MRI suggested bilateral cerebellar and bilateral
suggestive of vertebrobasilar artery stenosis and occlusion. In MCP infarcts, respectively. Therefore, we consider the hearing
most cases, bilateral AICA emanate symmetrically from the loss to be the prodromal symptom, with bilateral cerebellar and
BA. Almost all MCP is supplied by the AICA. Owing to severe MCP infarcts occurring sequentially after the hearing loss at
stenosis or occlusion of the vertebrobasilar artery, when the lesion time intervals.
is in the vicinity of the inferior segment of the BA branching The purpose of this case report was to characterize the nature
off the bilateral AICA, it tends to cause ischemia in the IAA of deafness in the patient by performing detailed audiological
supplying the inner ear. Damage to auditory hair cells and and neurological investigations, such as the head MRI, pure
vestibular organs of the inner ear, which are extremely sensitive tone audiometry, speech audiometry, acoustic immittancemetry,
to ischemia and hypoxia, can cause SSNHL and vertigo. When BEAP, and otoacoustic emissions to define the location of lesions
Frontiers in Medicine 05 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
associated with hearing loss. Our patient had persistent, bilateral, Data availability statement
severe hearing loss on PTA, but limb strength and coordination
gradually resolved over time, with no significant abnormalities The original contributions presented in the study are included
in BEAP. At the same time, the symptoms of the facial and in the article/supplementary material, further inquiries can be
abducens nuclei and sensory tracts did not manifest during directed to the corresponding author.
the course of the disease. We determined that bilateral hearing
loss was affecting the cochlear rather than the retrocohlear sites
such as the vestibulocochlear nerve, brainstem nucleus or other Ethics statement
central pathways, as a result of ischemic infarction. Moreover,
the retrocochlear acoustic nerve is believed to have an abundant Ethical review and approval was not required for the study
collateral blood supply, which has a lower probability of injury (14). on human participants in accordance with the local legislation
Meanwhile, the fact that patients are less sensitive to hearing loss and institutional requirements. The patients/participants provided
than vestibular symptoms, has led to a lower incidence of auditory their written informed consent to participate in this study. Written
symptoms, as described in previous case reports of AICA infarction informed consent was obtained from the individual(s) for the
(15). Audiological examinations should not be neglected in patients publication of any potentially identifiable images or data included
with MCP infarction, as it is important for the localization of in this article.
the disease.
Moreover, our patient had persistent bilateral deafness 10 days
before the diagnosis of bilateral MCP infarction, which was a Author contributions
much longer interval than previous bilateral MCP infarction cases.
In a study of 16 patients with unilateral AICA infarcts, isolated Material preparation was performed by RL. Data analysis was
recurrent vertigo, fluctuating hearing loss, and tinnitus, as the first performed by ZY and LX. The first draft of the manuscript was
symptoms, occurred in 31% (n = 5) of patients within 1–10 days written by ZY. WY contributed to the study conception and
before the onset of the brainstem and cerebellar symptoms (15). approved the final manuscript. All authors commented on previous
In 82 cases of AICA infarcts, MRA of patients with and without versions of the manuscript. All authors contributed to the article
prodromal symptoms of the auditory vestibular system showed and approved the submitted version.
that stenosis of the basilar artery near the beginning of AICA was
more common in the former (62 vs. 13%) (16). Bilateral AICA
occlusion in our patient was considered to be related to severe VA Acknowledgments
stenosis with thrombosis obstructing the orifices of both AICA,
which is consistent with the mechanism reported by Ogawa et al. We appreciated the participated patient in our study.
(17). Zhang et al. confirmed the value of basi-parallel anatomic
scanning magnetic resonance imaging (BPARS-MRI) in clarifying
the diagnosis of the vascular etiology of AICA infarcts, which can Conflict of interest
reveal an accurate outer contour of the vascular wall (18).
We describe the case of a patient with bilateral symmetric The authors declare that the research was conducted
MCP infarction who presented with sudden bilateral deafness as in the absence of any commercial or financial relationships
the initial symptom. Vertebrobasilar diseases should be routinely that could be construed as a potential conflict
considered in middle-aged and elderly patients with vascular risk of interest.
factors and bilateral hearing loss. Diagnosis can easily be delayed
when patients have only symptoms such as hearing loss and vertigo,
with few typical stroke symptoms. Brain MRI, brain MRA, BAEP, Publisher’s note
otoacoustic emissions, and Pure Tone Audiogram help to localize
and qualify the diagnosis. We emphasized the cochlear, not the All claims expressed in this article are solely those of the
retrocochlear, as the localization of bilateral deafness in this patient authors and do not necessarily represent those of their affiliated
with bilateral MCP infarction. Early detection of hearing loss organizations, or those of the publisher, the editors and the
and intervention can help patients recover. Bilateral hearing loss reviewers. Any product that may be evaluated in this article, or
localized to the periphery usually improves better after treatment claim that may be made by its manufacturer, is not guaranteed or
and has a better prognosis. endorsed by the publisher.
References
1. Olex-Zarychta D. Hyperbaric oxygenation as adjunctive therapy in 2. Chandrasekhar SS, Do BST, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA,
the treatment of sudden sensorineural hearing loss. Int J Mol Sci. (2020) et al. Clinical practice guideline: Sudden hearing loss (update). Otolaryngol Head Neck
21:228588. doi: 10.3390/ijms21228588 Surg. (2019) 161:1–45. doi: 10.1177/0194599819859885
Frontiers in Medicine 06 frontiersin.org
Yuan et al. 10.3389/fmed.2023.1174512
3. Yamada S, Kita J, Shinmura D, Nakamura Y, Sahara S, Misawa K, et al. Update on 11. Deng Y, Shi J, Zhang M, Qi X. Clinical characteristics of cerebral hemorrhage
findings about sudden sensorineural hearing loss and insight into its pathogenesis. J with bilateral sudden deafness as the first symptom. Neurol Sci. (2021) 42:141–
Clin Med. (2022) 11:216387. doi: 10.3390/jcm11216387 50. doi: 10.1007/s10072-020-04515-1
4. Bovo R, Ortore R, Ciorba A, Berto A, Martini A. Bilateral sudden 12. Lee H, Sohn S-I, Jung D-K, Cho Y-W, Lim J-G, Yi S-D, et al. Sudden
profound hearing loss and vertigo as a unique manifestation of bilateral deafness and anterior inferior cerebellar artery infarction. Stroke. (2002) 33:2807–
symmetric inferior pontine infarctions. Ann OtolRhinolLaryngol:. (2007) 12. doi: 10.1161/01.STR.0000038692.17290.24
116:407–10. doi: 10.1177/000348940711600603
13. Chen YH, Young YH. Bilateral simultaneous sudden sensorineural hearing loss.
5. Renard D, Taieb G, Castelnovo G, Ghanem S, Ayrignac X, Labauge P. Isolated J Neurol Sci. (2016) 362:139–43. doi: 10.1016/j.jns.2016.01.029
bilateral anterior inferior cerebellar artery infarction. Arch Neurol. (2010) 67:766–
14. Lee H. Recent advances in acute hearing loss due to posterior circulation
7. doi: 10.1001/archneurol.2010.114
ischemic stroke. J Neurol Sci. (2014) 338:23–9. doi: 10.1016/j.jns.2013.12.048
6. Lee H, Whitman GT, Lim JG, Lee SD, Park YC. Bilateral sudden deafness as
15. Lee H, Cho YW. Auditory disturbance as a prodrome of anterior inferior
a prodrome of anterior inferior cerebellar artery infarction. Arch Neurol. (2001)
cerebellar artery infarction. J Neurol Neurosurg Psychiatry. (2003) 74:1644–
58:1287–9. doi: 10.1001/archneur.58.8.1287
8. doi: 10.1136/jnnp.74.12.1644
7. World Health Organization. World Report on Hearing. Geneva: WHO (2021).
16. Lee H, Kim JS, Chung E-J, Yi H-A, Chung I-S, Lee S-R, et al. Infarction in the
8. Sara SA, Teh BM, Friedland P. Bilateral sudden sensorineural hearing loss: territory of anterior inferior cerebellar artery: Spectrum of audiovestibular loss. Stroke.
Review. J LaryngolOtol. (2014) 128(Suppl.1):S8–15. doi: 10.1017/S00222151130 (2009) 40:3745–51. doi: 10.1161/STROKEAHA.109.564682
0306X
17. Ogawa K, Suzuki Y, Takahashi K, Akimoto T, Kamei S, Soma
9. Li BL, Xu JY, Lin S. Sudden deafness as a prodrome of cerebellar M. Clinical study of seven patients with infarction in territories of
artery infarction: Three case reports. World J Clin Cases. (2022) 10:4895– the anterior inferior cerebellar artery. J Stroke Cerebrovasc Dis. (2017)
903. doi: 10.12998/wjcc.v10.i15.4895 26:574–81. doi: 10.1016/j.jstrokecerebrovasdis.2016.11.118
10. Kim YS, Tehrani ASS, Lee HS. Sudden unilateral hearing loss and 18. Zhang Z-Y, Zhou Z, Zhang H-B, Jiao J-S. Case report: The etiology
vertigo following isolated cerebellar hypoperfusion without infarction due to of anterior inferior cerebellar artery infarction: what does basi-parallel
vertebral artery dissection. BMC Neurol. (2022) 22:489. doi: 10.1186/s12883-022-03 anatomic scanning magnetic resonance imaging tell us? BMC Neurol. (2021)
024-2 21:299. doi: 10.1186/s12883-021-02309-2
Frontiers in Medicine 07 frontiersin.org
You might also like
- Physics1100 Lab Manual (Iolab Revision)Document105 pagesPhysics1100 Lab Manual (Iolab Revision)Tri NguyenNo ratings yet
- English File Fourth Edition Intermediate WorkbookDocument82 pagesEnglish File Fourth Edition Intermediate WorkbookАнатоль БумберсNo ratings yet
- A Rare Cause of Hearing Loss: Susac SyndromeDocument3 pagesA Rare Cause of Hearing Loss: Susac SyndromeBeny Pratama SidabutarNo ratings yet
- Angioinvasive Cerebral Aspergillosis Presenting As Acute Ischaemic Stroke in A Patient With Diabetes MellitusDocument4 pagesAngioinvasive Cerebral Aspergillosis Presenting As Acute Ischaemic Stroke in A Patient With Diabetes MellitusKamil HannaNo ratings yet
- Nutrimentum Vascularum As Pulsatile TinnitusDocument6 pagesNutrimentum Vascularum As Pulsatile TinnitusJuthika Rai ShettyNo ratings yet
- Tuli Mnedadak NcbiDocument6 pagesTuli Mnedadak NcbiMiss AmyNo ratings yet
- Tinnitus Update 2021Document10 pagesTinnitus Update 2021tumi maryNo ratings yet
- Seminar: Benjamin E Schreiber, Charlotte Agrup, Dorian O Haskard, Linda M LuxonDocument9 pagesSeminar: Benjamin E Schreiber, Charlotte Agrup, Dorian O Haskard, Linda M Luxonmaria_garaveNo ratings yet
- Neuroanatomical Considerations of Isolated Hearing Loss in Thalamic HemorrhageDocument3 pagesNeuroanatomical Considerations of Isolated Hearing Loss in Thalamic HemorrhageBella Cynthia BettabestariNo ratings yet
- Schwannoma Vestibular TinnitusDocument6 pagesSchwannoma Vestibular TinnitusThomasMáximoMancinelliRinaldoNo ratings yet
- Original Article: Study of Computed Tomography (CT) Scan Finding in Neurofibromatosis Type 2Document4 pagesOriginal Article: Study of Computed Tomography (CT) Scan Finding in Neurofibromatosis Type 2Lisa SariNo ratings yet
- Musical Hallucinations Following Insular Glioma Resection: Case ReportDocument4 pagesMusical Hallucinations Following Insular Glioma Resection: Case ReportMalcoci MihaiNo ratings yet
- Laporan KasusDocument4 pagesLaporan KasusNovia DamayantiNo ratings yet
- American Journal of OtolaryngologyDocument4 pagesAmerican Journal of OtolaryngologyDear Farah SielmaNo ratings yet
- Decreased Consciousness Bithalamic InfarcDocument3 pagesDecreased Consciousness Bithalamic InfarcshofidhiaaaNo ratings yet
- Bilateral Sudden Sensorineural Hearing Loss: Review: Sasara, B M Teh, P FriedlandDocument12 pagesBilateral Sudden Sensorineural Hearing Loss: Review: Sasara, B M Teh, P FriedlandMariaAmeliaGoldieNo ratings yet
- Traumatic Ossicular Dislocations: Etiology and ManagementDocument6 pagesTraumatic Ossicular Dislocations: Etiology and ManagementlawrensiusrNo ratings yet
- AICA InfarctDocument6 pagesAICA InfarctReynard FebrianNo ratings yet
- Management of Adult Sensorineural Hearing Loss: EtiologiesDocument10 pagesManagement of Adult Sensorineural Hearing Loss: EtiologiesaldimugniNo ratings yet
- A Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary PancreatitisDocument5 pagesA Case Report of Posterior Reversible Encephalopathy Syndrome in A Patient Diagnosed With Emphysematous Necrotizing Biliary Pancreatitisbijnn journalNo ratings yet
- Main PDFDocument3 pagesMain PDFanton MDNo ratings yet
- Vocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDocument4 pagesVocal Cord Palsy: An Uncommon Presenting Feature of Myasthenia GravisDivine Jane PurciaNo ratings yet
- IJC Heart & VasculatureDocument2 pagesIJC Heart & VasculatureGledia LindaNo ratings yet
- Artery of Percheron Infarct: An Acute Diagnostic Challenge With A Spectrum of Clinical PresentationsDocument9 pagesArtery of Percheron Infarct: An Acute Diagnostic Challenge With A Spectrum of Clinical PresentationsMaria JimenezNo ratings yet
- 3504-Article Text-11497-1-10-20200318Document3 pages3504-Article Text-11497-1-10-20200318Ade Puji AstutiNo ratings yet
- J Clinph 2013 03 031Document7 pagesJ Clinph 2013 03 031Andres Rojas JerezNo ratings yet
- Tinnitus PDFDocument10 pagesTinnitus PDFАлександра КондряNo ratings yet
- SD GradiDocument3 pagesSD GradiPabloMrchNo ratings yet
- Auricula 2 PDFDocument27 pagesAuricula 2 PDFCamy Alejandra Gonzales GonzalesNo ratings yet
- Neuro 0392-100X-30-217Document5 pagesNeuro 0392-100X-30-217pauloNo ratings yet
- Sudden Deafness JournalDocument2 pagesSudden Deafness JournalRestiNo ratings yet
- Acu Accident LumbarDocument2 pagesAcu Accident Lumbarrswongym449No ratings yet
- Neuro4Nurses Acustic NeuromaDocument2 pagesNeuro4Nurses Acustic Neuromaputri auliyahNo ratings yet
- Otology: Special Paper in Celebration of Prof. Yang'S 50 Years Career in MedicineDocument6 pagesOtology: Special Paper in Celebration of Prof. Yang'S 50 Years Career in Medicinechipta lestariNo ratings yet
- Epilepsy & Behavior Case Reports: 10.1016/j.ebcr.2017.07.003Document21 pagesEpilepsy & Behavior Case Reports: 10.1016/j.ebcr.2017.07.003Faras ArinalNo ratings yet
- D Evaluation For Resective Epilepsy SurgeryDocument104 pagesD Evaluation For Resective Epilepsy SurgeryYusuf BrilliantNo ratings yet
- Neewzealand JournalDocument5 pagesNeewzealand JournalFuji Seprinur HidayatNo ratings yet
- Posterior Reversible Encephalopathy Syndrome After Lumbar PunctureDocument2 pagesPosterior Reversible Encephalopathy Syndrome After Lumbar PunctureMedtext PublicationsNo ratings yet
- Case Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationDocument16 pagesCase Report A Chinese Patient With Spinocerebellar Ataxia Finally Confirmed As Gerstmann-Sträussler-Scheinker Syndrome With P102L MutationLídia YoshiharaNo ratings yet
- Dapus 9Document9 pagesDapus 9martina marthaNo ratings yet
- Presentasi Kasus Sudden Deafness Dhana 2017Document9 pagesPresentasi Kasus Sudden Deafness Dhana 2017Pradhana FwNo ratings yet
- Mus 27395Document9 pagesMus 27395Denis Jesus Salgado GutierrezNo ratings yet
- TinitusDocument4 pagesTinitusFridaZorayaNo ratings yet
- Journal of Clinical NeuroscienceDocument3 pagesJournal of Clinical NeurosciencejicarrerNo ratings yet
- Acoustic NeuromaDocument6 pagesAcoustic NeuromaMartha AsikoNo ratings yet
- MRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyDocument3 pagesMRI Findings in Post-Operative Bilateral Posterior Ischemic Optic NeuropathyJan JanNo ratings yet
- The FACIAL NERVE Current Trends in Diagnosis, Treatment, and RehabilitationDocument17 pagesThe FACIAL NERVE Current Trends in Diagnosis, Treatment, and RehabilitationkrazeedoctorNo ratings yet
- Jurding Elmo H3a021009Document39 pagesJurding Elmo H3a021009Elmo KrisnawanNo ratings yet
- Fneur 13 962376Document8 pagesFneur 13 962376Miss AmyNo ratings yet
- Lee 2015Document12 pagesLee 2015Bagus Pithu Ha SpingNo ratings yet
- Sudden Deafness 2Document8 pagesSudden Deafness 2Aldhi Putra PradanaNo ratings yet
- Meniere DiseaseDocument16 pagesMeniere DiseaseNavjot Brar100% (2)
- Spectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioDocument4 pagesSpectrum of Mri Findings in Pediatric Epilepsy Medical and Surgical Causes of Epilepsy in Children and Its Radiological CorrelatioImroatul hafidzahNo ratings yet
- Trigeminal Neuralgia A Case Report With Review of LiteratureDocument4 pagesTrigeminal Neuralgia A Case Report With Review of LiteratureFauziah KautsaraNo ratings yet
- Oliveira 2020Document5 pagesOliveira 20202907tranthaonguyenNo ratings yet
- 3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftDocument5 pages3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftabhishekbmcNo ratings yet
- Bilateral Vestibular Schwannoma Associated Neurofibromatosis Type 2Document1 pageBilateral Vestibular Schwannoma Associated Neurofibromatosis Type 2Anonymous ocfZSRrrONo ratings yet
- AcousticNeuromaVestibularSchwannoma StatPearls NCBIBookshelfDocument6 pagesAcousticNeuromaVestibularSchwannoma StatPearls NCBIBookshelfarifbudipraNo ratings yet
- Neurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL TjiaDocument6 pagesNeurol J Southeast Asia 1999 4: 83 - 88: LCS Tan, YY Sitoh, HTL Tjiarani suwadjiNo ratings yet
- Planum Sphenoidal MeningiomaDocument5 pagesPlanum Sphenoidal MeningiomaNidya TiazNo ratings yet
- Echography and Doppler of the BrainFrom EverandEchography and Doppler of the BrainChiara RobbaNo ratings yet
- SGD Case 2 Written Output-1Document19 pagesSGD Case 2 Written Output-1Jam PanumpangNo ratings yet
- Low-Loss Power Splitters - Multi-Band 800 - 2500 MHZ 860 10017, 860 10018, 860 10019Document1 pageLow-Loss Power Splitters - Multi-Band 800 - 2500 MHZ 860 10017, 860 10018, 860 10019Zoheir KacimiNo ratings yet
- (2024년 예상) 다정고등학교 (세종 전체) 1-1 중간 영어 족보 (천재 (김태영) ) (Q) 2회Document11 pages(2024년 예상) 다정고등학교 (세종 전체) 1-1 중간 영어 족보 (천재 (김태영) ) (Q) 2회y2un.t1130No ratings yet
- I Cannot Live With You PoemsDocument4 pagesI Cannot Live With You PoemsDaeng ArifNo ratings yet
- 490806Document2 pages490806Informative InsaanNo ratings yet
- Original Research Paper Geography: M.A Geography, UGC NET-JRF (Government P.G College Badli, Haryana)Document4 pagesOriginal Research Paper Geography: M.A Geography, UGC NET-JRF (Government P.G College Badli, Haryana)neeraj kumarNo ratings yet
- Stolarska Radionica - Procjena Troškova: Vrsta Naziv Slika Link Cijena Total VrstaDocument7 pagesStolarska Radionica - Procjena Troškova: Vrsta Naziv Slika Link Cijena Total VrstaMarko PalicNo ratings yet
- IW2P1Document3 pagesIW2P1Eong Huat Corporation Sdn BhdNo ratings yet
- Magallona Vs ErmitaDocument13 pagesMagallona Vs ErmitaERNIL L BAWA100% (1)
- Nanazoxid 0Document5 pagesNanazoxid 0hnn9gfqzqxNo ratings yet
- L A Level Physics A MS Jun 07 Old g481Document88 pagesL A Level Physics A MS Jun 07 Old g481dasha962No ratings yet
- Safety-Overall MEO Class 4 Part BDocument21 pagesSafety-Overall MEO Class 4 Part Blazyreaderr100% (1)
- Apple Airpods Max Complete Features Instructions ManualDocument7 pagesApple Airpods Max Complete Features Instructions ManualIlaria iudiceNo ratings yet
- Inta Commercial Collection April 2011Document59 pagesInta Commercial Collection April 2011Robin FisherNo ratings yet
- Certificate of Calibration: Customer InformationDocument2 pagesCertificate of Calibration: Customer InformationSazzath HossainNo ratings yet
- Astm A570 1979Document5 pagesAstm A570 1979set_ltdaNo ratings yet
- X-Ray For BoneDocument2 pagesX-Ray For BoneLILISNo ratings yet
- Zernack Et Al 2009. Sedimentary Signatures of Cyclic Growth and Destruction of Stratovolcanoes. A Case Study From Mt. Taranaki, New Zealand PDFDocument18 pagesZernack Et Al 2009. Sedimentary Signatures of Cyclic Growth and Destruction of Stratovolcanoes. A Case Study From Mt. Taranaki, New Zealand PDFAndres Almanza SoteloNo ratings yet
- KhatDocument1 pageKhatricomusongNo ratings yet
- 16216l5 16494Document2 pages16216l5 16494Saul AlbertoNo ratings yet
- Science and Technology Research Partnership For Sustainable Development (Satreps) Proposal On Iot X SDG X IndonesiaDocument6 pagesScience and Technology Research Partnership For Sustainable Development (Satreps) Proposal On Iot X SDG X IndonesiaelektroftuhNo ratings yet
- Manual Lab e Coli Lab 6Document9 pagesManual Lab e Coli Lab 6Siti Mastura Abdul RahmanNo ratings yet
- SketchUp Tutorial 1 - TableDocument19 pagesSketchUp Tutorial 1 - TablenphilippNo ratings yet
- Lesson Plan Preparing For Parenthood Pregnancy and Labor - 0Document15 pagesLesson Plan Preparing For Parenthood Pregnancy and Labor - 0Sweta ManandharNo ratings yet
- Hspice Simulation of SRAM PDFDocument65 pagesHspice Simulation of SRAM PDFYatheesh KaggereNo ratings yet
- Annual Day AnchoringDocument5 pagesAnnual Day AnchoringPooja ChuriwalNo ratings yet
- Brunnstrom's ApproachDocument37 pagesBrunnstrom's Approachdexter veracityNo ratings yet
- Arne JaconsenDocument20 pagesArne JaconsenXavier Ernesto100% (1)