Professional Documents
Culture Documents
What Psychology do Medical Students Need to Know An Evidence Based Approach to Curriculum Development
What Psychology do Medical Students Need to Know An Evidence Based Approach to Curriculum Development
Uploaded by
fptintiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
What Psychology do Medical Students Need to Know An Evidence Based Approach to Curriculum Development
What Psychology do Medical Students Need to Know An Evidence Based Approach to Curriculum Development
Uploaded by
fptintiCopyright:
Available Formats
Health and Social Care Education
ISSN: (Print) 2051-0888 (Online) Journal homepage: www.tandfonline.com/journals/rhep15
What Psychology do Medical Students Need to
Know? An Evidence Based Approach to Curriculum
Development
L. Cordingley, S. Peters, J. Hart, J. Rock, L. Hodges, J. McKendree & C. Bundy
To cite this article: L. Cordingley, S. Peters, J. Hart, J. Rock, L. Hodges, J. McKendree & C. Bundy
(2013) What Psychology do Medical Students Need to Know? An Evidence Based Approach
to Curriculum Development, Health and Social Care Education, 2:2, 38-47, DOI: 10.11120/
hsce.2013.00029
To link to this article: https://doi.org/10.11120/hsce.2013.00029
Published online: 15 Dec 2015.
Submit your article to this journal
Article views: 8352
View related articles
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=rhep15
38
PRACTICE PAPER
What Psychology do Medical Students
Need to Know? An Evidence Based
Approach to Curriculum Development
L. Cordingley1, S. Peters2, J. Hart3, J. Rock4, L. Hodges5, J. McKendree6 & C. Bundy1
1
Dermatological Sciences, Institute for Inflammation and Repair, University of Manchester and Manchester Academic
Health Sciences Centre, Manchester, UK
2
Manchester Centre for Health Psychology, School of Psychological Sciences, University of Manchester and Manchester
Academic Health Sciences Centre, Manchester, UK
3
Manchester Medical School, Manchester Centre for Health Psychology, Manchester, UK
4
Keele Medical School, University of Keele, Keele, UK
5
University of Edinburgh, Edinburgh, UK
6
Hull York Medical School, Hull and York, UK
Abstract
While the contribution of behavioural and social
sciences for understanding health, illness and medical
practice is made explicit in documents such as
Tomorrow’s Doctors, research shows that the proportion
of curriculum space given to psychology in
undergraduate curricula varies widely between medical
schools. In the US, recommendations for behavioural
sciences education for medical undergraduates have
been developed. However, the United Kingdom has
yet to produce agreed curriculum outcomes for
behavioural sciences in medical education.
We aimed to develop an evidence-based consensus
behavioural sciences curriculum for undergraduate
medical education. This paper reports a novel
technique for curriculum development that utilises
knowledge and expertise of key stakeholders from
medicine, medical education and behavioural
sciences. It was successfully used to develop a
psychology core curriculum for undergraduate
medicine in the UK.
Keywords: behavioural and social sciences, medical
education, curriculum development
Corresponding author:
Dr Christine Bundy, 6.10 Williamson Building University Background
of Manchester, Oxford Rd, Manchester, M13 7PT, UK
Email: christine.bundy@manchester.ac.uk, Phone: + 44 (0) Social and behavioural factors are important in the
1612 755231 treatment and prevention of almost all the major
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
L. Cordingley et al. 39
diseases and nearly half of preventable deaths can that undergraduate education in the UK was not fit
be linked to behaviours (McGinnis & Foege 1993). for purpose over a decade ago. The result, a set of
Psychological factors such as beliefs and recommendations published as GMC Tomorrow’s
expectations also influence progress in long-term Doctors (1993) signalled a shift in emphasis away
conditions (LTCs) and impact on health outcomes from the learner simply acquiring factually based
and a substantial body of literature has now information to the new graduate being able to
accrued outlining the actual and potential pathways apply the knowledge and skills acquired to medical
between psychological factors and disease end practice. The primary recommendations were to
points (Kawachi et al. 1996, Barefoot et al. 2000, reduce the factual content of programmes,
Andersen 2002, Smith & Ruiz 2002). contextualise the learning and make better use of
modern teaching and learning methods. It was
In addition, the practice of medicine is intellectually,
recommended that the B&SS be included in the
emotionally and behaviourally demanding. Doctors
curriculum on a ‘need to know’ rather than ‘nice to
experience higher levels of divorce, alcoholism and
know’ basis and strongly recommended that more
burnout compared with other professional groups
emphasis be placed on learning to communicate
(Vaillant et al. 1972) and medical practitioners as a
better.
group demonstrate higher levels of stress compared
with other professional groups Firth-Cozens 2003, Further, Tomorrow’s Doctors revisions (GMC 2001,
Taylor et al. 2005) and they tend to be overly self- GMC 2006) reinforce the value of the B&SS in
critical as students, which predicts later distress teaching programmes. Furthermore, psychological
(Firth-Cozens 1992). These are not just problems for principles underpin a range of related topics such
the practitioners themselves and their families, but as patient safety, communication and patient
constitute a quality of care issue, as stressed doctors centredness. In fact, communication skills training
are more prone to making errors (Jones et al. 1988). has been the vehicle for delivery of much of the
B&SS curriculum in undergraduate education.
Despite longstanding arguments for the inclusion of
Behavioural and Social Sciences (B&SS) in medical The current situation in the UK reflects local centres
education (Flexner 1910), the establishment of the of excellence; a small number of departments that
first department of B&SS in a North American have well established expertise. But most medical
medical school in 1959 (Dacey & Weintrob 1973) schools show wide variability in the B&SS curricular
and the incorporation of B&SS in assessment in the content; the teaching delivery methods and the
US in 1976 (Wexler 1976), in the UK systematic learning outcomes are different, assessment
incorporation of B&SS is a relatively recent strategies differ and the B&SS in medical education
occurrence, and attempts to integrate with remain largely invisible other than those
medicine have been met with varying degrees of components embedded in communication training
success (Benbassat et al. 2003). There is as yet no (Russell et al. 2004). In addition, the degree of
dedicated B&SS department in a UK medical school horizontal integration between specialities differs
and no consensus on what should be taught, or between medical schools. Vertical integration
how it should be delivered, when, and by whom. (whether subject teaching spans the whole
programme or is confined to the pre-clinical years)
Developments within UK Medicine is also dependent on the institution. Finally, some
This is not to say that the potential contribution of staff delivering this component are not subject
B&SS equipping medical students with knowledge specialists; some may possess a first degree in a
that will both improve their own effectiveness with related discipline, while others posses a related
patients, and offer protection from ‘burnout’ by allied health qualification only (Russell et al. 2004).
identifying and managing sources of stress, has not Of those who are B&SS discipline experts, many
been acknowledged in the UK. The Royal quickly become dissatisfied and leave because they
Commission on Medical Education (the Todd Report are poorly supported and there is an absence of
1968) and General Medical Council’s (GMC) career development pathways for those in post
Education Committee Working Party on The (Litva & Peters 2008).
Teaching of the Behavioural Sciences, Community Development of learning and teaching
Medicine and General Practice in Basic Medical opportunities are also affected by a variety of
Education report (GMC Education Committee 1987), attitudes and beliefs about B&SS. The conceptual
demonstrate respectively awareness of the need to and theoretical perspectives advanced in B&SS may
improve B&SS teaching for medical undergraduates clash with those dominant in medicine (Jaco 1960),
and progress to the point where virtually every the focus on exploratory and discursive techniques
medical undergraduate curriculum has a well- may be perceived as less useful than those that
developed syllabus in B&SS (most of them emphasise acquisition of facts and practice of skills.
concentrating upon psychology). Further Senior role models may not value or endorse B&SS
developments followed the UK GMC recognition
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
40 What Psychology do Medical Students Need to Know?
perspectives and approaches. There may be hostility the depth or level of study specified in a core
to perceived threats to medical autonomy and curriculum for medicine. A final list of 49 separate
perceptions that B&SS lack scientific legitimacy topics were identified in seven areas (Box 1).
(Dacey & Weintrob 1973, Litva & Peters 2008).
They may see it as valuable only as a contribution
to systematic thinking, if it has application as a Box 1 The basic areas of psychology used for the
contributor to, for example psychiatry, or as an Phase 1 topic mapping task
adjunct to development of interpersonal skills
Cognitive (How people remember, think,
relevant to medical consultations (Sheldrake 1973).
Psychology learn, perceive, attend to and
The status of B&SS academics may be perceived to manage information.)
limit their contribution to medical education and
Social (How individuals think and interact
they have been criticised for a lack of attention
Psychology at individual, group and societal
to application of their expert knowledge to levels.)
medicine (Dacey & Weintrob 1973, Bolman 1995,
Developmental (Acquisition and changes in
Benbassat et al. 2003). They may be perceived as Psychology psychological processes from
too critical of medicine and unhelpful to students conception to old age.)
(Tait 1973, Peters & Litva 2006). As a result students
Individual (Factors accounting for differences
become critical and dismissive of B&SS seeing the Differences between individuals, in particular
disciplines as subjective, not amenable to scientific intelligence and personality.)
study, and not having any evidence base other than
Research (Quantitative and qualitative design,
“common sense” (Rees et al. 2002). B&SS may be Methods analysis, ethics, governance and
perceived as nice to know but not need to know measurement.)
populated with concepts that are not familiar and Health and (Psychological processes that
require work if they are to derive the relevance to Clinical contribute to physical and
medical practice (Tait 1973). Psychology mental health and illness.)
Occupational (Psychological processes involved
Need to develop a core curriculum Psychology in performance at work, in
training, how organisations
for the B&SS in Medicine function.)
The GMC recommends that graduates should “…
apply psychological principles, method and
knowledge to medical practice” (GMC Tomorrow’s
Doctors 2009, p15). In this study we focus on Participants were recruited at workshops conducted
defining the relevant aspects of psychology that at two international medical education conferences
medical graduates need to know based on a (one in the US and one in the Netherlands) and
rigorous and inclusive methodology, utilising the worked in six mixed professional groups. At each
model for integrating B&SS developed by US workshop a 15-minute presentation was delivered
medical schools (Cuff & Vanselow 2004). In to orientate participants to the sorting task. It
developing a core curriculum recommendation that covered the GMC’s Good Medical Practice (GMP)
was evidence-based, relevant to clinical practice and framework and the concepts in the BPS Core
acceptable to stakeholders, a novel consultative Curriculum.
methodology was employed.
Individuals formed small mixed professional groups
Method (six to eight participants) and were each given a
set of cards that contained definitions and examples
Three phases of work comprised data collection: of the 49 psychology concepts and an A0 size map
1) topic mapping; 2) topic prioritisation; and 3) data of the GMP categories (Figure 1). To make the
interpretation, integration and validation. sorting task more engaging, the cards were divided
into four ‘suits’ using the familiar playing card
Phase 1: Mapping psychology to medical
symbols: 15 cognitive and developmental
education and practice
psychology topics (clubs); 11 social psychology
Procedure and individual differences topics (spades); 9 Health
and Clinical psychology topics (hearts) and 14
We sampled psychology topics taken from the
Organizational Psychology topics (diamonds).
British Psychological Society (BPS) minimum
syllabus for graduate basis for registration with the Participants were instructed to discuss each topic as
BPS (The British Psychological Society, BPS 2004) it arose from the deck and to place it on the
the BPS syllabus topic areas for postgraduate category of GMP on the map. Blank cards were
qualifications in Health Psychology and Occupational issued if people wanted to place one concept on
Psychology (BPS 2004 a,b). These lists did not imply more than one GMP category. If a concept could
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
L. Cordingley et al. 41
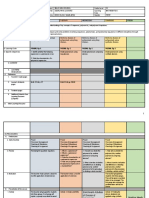
Figure 1 Task mat used in mapping phase
not be placed in any of the seven GMC categories it Phase 2: Topic prioritisation
was recorded as not relevant. Consensus was
Procedure
sought, but if the group could not agree on a
particular concept this was also recorded. A national meeting was arranged for 30 experts
from the newly formed UK Psychology in Medicine
The atmosphere created was congenial and
network, all of whom were currently involved in
encouraged discussion and interaction within the
medical education. Prior to the meeting, the topic
groups with a deliberate attempt to break down
list (Box 1) was sent to delegates. A definition, one
barriers between participants from different
or two indicative key aspects of the topic and
disciplinary/professional backgrounds. Organisers
illustrative examples were provided alongside each
aimed to ensure that participants did not focus on
topic (Figure 2). Apart from the topic that was
defining jargon or become too engrossed with
unanimously viewed as irrelevant in Phase 1, all
detail or disagreement about what the GMP
topics were included. Participants were asked to
categories meant. The aim was to keep participants’
judge whether the topic should be high, medium,
thinking at the level of ‘how could this psychology
low or no priority, or whether it was an area for
topic contribute to good medical practice?’. Each
postgraduate medicine only. The priority levels are
workshop took an hour to complete and the data
shown in Box 2.
on the categories and topics were recorded.
Documents were distributed in advance of the
Results from Phase 1
meeting to ensure they had sufficient time to
Forty-seven participants took part in a workshop. consider the materials and make their priorities.
Of these, thirty-three (57.6%) were medical During the meeting participants were allocated into
practitioners, ten were psychologists (30.3%), three groups of five to six delegates each and asked
and the remaining four stated that they were to discuss the prioritisation task and topics. Each
medical educationalists (12.1%). These formed group recorded on a flipchart the points to emerge
six groups. from the discussion and in turn reported these to
The vast majority of topics were viewed as relevant the group as a whole.
to Good Medical Practice with most cards placed in Results from Phase 2
two or more of the GMP sections. Very few cards
were placed only in one GMC category, with the Detailed findings are provided in Table 1. The topic
majority placed in two or more (range 0–6 from a priorities reported are the modal option for the
possible total of 7). Only one topic was discarded by whole sample. Where no modal option appeared,
participants as not relevant. Specifics of psychology the lower priority was given, thereby giving a
topics mapped to GMP sections are detailed in the conservative view of relevance. Group discussions
core curriculum document (BeSST 2010). during the event were recorded and that data were
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
42 What Psychology do Medical Students Need to Know?
Figure 2 Topic layout used in prioritisation response task with example
Topic: D3. Cognitive & Social
Definition: The changes as a function of age and experience during later life.
Aspects of Aging
Indicative Key Points: Examples: Topic Priority
• Normal Ability to differentiate normal changes in cognitive function High Priority
from those caused by disease. Medium Priority
Low Priority
• Relationships over the lifespan Role of social support in illness prevention in old age. Not relevant
Postgrad only
Box 2 Definition of priority levels used in Phase 2
High Priority: Core knowledge – undergraduate medical students should learn basic psychological concepts
and application in medicine.
Medium Priority: Core knowledge – undergraduate medical students should learn how the psychological
concepts involved are applicable to medicine (but not the basic psychological concept).
Low Priority: Useful knowledge but not essential for all UK undergraduate medical programmes.
Postgrad only: Not appropriate for an undergraduate curriculum but should be included in specialist
postgraduate education or training.
Not relevant: Not relevant to medical education or training.
subjected to thematic analysis. The following main scientists, the depth of understanding need
points were identified. not mirror that of graduate psychology
students.
a. Relevance and context. Whilst most viewed the
majority of areas as relevant, all participants c. Gaps in the topic list. Additional core topics
stressed the need to contextualise psychology (identified by at least three participants)
topics by embedding teaching activities within included pain, mental illness, bereavement,
other disciplinary areas and with the patient body image and addiction. The large group
experience. Some concern was expressed that a discussion included substantial debate about
curriculum could simply be seen “as a checklist” the role of psychology in the professional and
and that medical schools would not “think out intellectual development of medics. Thus, as
of the box”. Curriculum integration was seen as well as core knowledge, other aspects of
having particular importance for social and psychology were judged to be crucial to
behavioural sciences. teaching, learning, assessment, and professional
practice.
Additionally, it was recognised that the way the
d. Overlap with other disciplines. Participants
topics were presented needed to reflect the
emphasised the importance of the interfacing of
priorities of medical rather than psychology
psychology with key areas, such as public
curricula. Thus new topic headings that
health, medical sociology, ethics and psychiatry.
highlighted patients’ experiences, doctors’
Topics such as poverty and service delivery
experiences and the learning process were
were viewed as relevant, but as belonging in
elicited, debated and agreed.
the domains of sociology or social policy rather
b. Depth. The group emphasised the need for than psychology, and were therefore omitted.
medical students to have sufficient knowledge
Readers recognised that research methods training
of psychological principles that would allow
was a particularly strong component of
them to apply this knowledge and recognise
undergraduate psychology curricula, but some were
their use of them in practice. However, they
wary of presenting the view that this area is the
were also clear that although as medical
sole remit of ‘psychology’. There was disagreement
practitioners they will be working as applied
as to whether ‘research methods’ was an area that
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
L. Cordingley et al. 43
Table 1 Findings from Phase 2 – Psychology core knowledge with prioritisation levels
1. Psychological factors in health and illness
Topic Priority
Psychological factors in health promotion and illness prevention High
Psychological interventions High
Psychological processes in disease High
Pain High
Genes and behaviour High
Mental health and mental Illness High
2. Psychological responses to illness
Emotional, cognitive and behavioural responses to illness High
Coping with illness High
3. Psychology across the life span
Cognitive development High
Cognitive aspects of ageing High
Social development across the lifespan High
Death, dying and bereavement High
Assessment of cognitive function over the age span Medium
Attachment Medium
4. Cognitive functioning in health and illness
Memory High
Learning High
Sleep and consciousness High
Attention Medium
Perception High
Language High
5. Psychology for professional practice
Clinical reasoning and decision making High
Human communication and communication skills training High
Research methods and evidence based medicine Medium
Social processes shaping professional behaviour High
Stress, well-being and burnout High
Leadership and team-working High
Teaching the next generation of doctors High
should be taught by psychology experts. It was they linked with. We aimed to embed the
decided not to proclaim this area as solely the prioritised aspects of psychology with medical
domain of psychology, but that it would be helpful topics in order demonstrate integration and
for students to be aware of specific areas of learning opportunities in the curricula.
expertise such as assessment of quality of life,
The majority of topics were grouped under the
attitudes and other complex constructs. This would
heading of Psychology – core knowledge, with the
complement other research methods and statistical
remainder as Psychology for professional practice
analyses teaching in epidemiology.
and Psychology – contribution to the educational
Phase 3: Data interpretation, integration process. The detailed output of this phase forms
and validation the curriculum document (BeSST 2010). Table 2
outlines key topic areas under each of these
Topics selected as high priority from Phase 2 were sections. Topics that were identified as more
organised according to which aspects of medicine, suitable for postgraduate level study are included
medical education and professional development in Table 3.
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
44 What Psychology do Medical Students Need to Know?
Table 2 Integrated curriculum summary Table 3 Topics identified as post graduate level only
1. Psychology – core knowledge Leadership – The exercise of influence Organisational
1.1 Psychological factors in health and illness over a group or individual to achieve Psychology
certain goals.
1.2 Psychological responses to illness
Selection and Appraisal – The use of Organisational
1.3 Psychology across the life span psychological methods to inform Psychology
1.4 Cognitive functioning in health and illness selection and appraisal processes.
Organisational Change – Managing Organisational
2. Psychology for professional practice change processes. Psychology
2.1 Clinical reasoning and decision making
2.2 Human communication and communication skills
training
2.3 Research methods and evidence-based medicine Discussion
2.4 Social processes shaping professional behaviour This paper describes the application of an expert
2.5 Stress, well-being and burnout consensus technique, an iterative process of
2.6 Leadership and team-working consultation, participation and integration, to the
development of an evidence based core curriculum
2.7 Teaching the next generation of doctors
in behavioural sciences for undergraduate medicine.
3. Psychology – contribution to the educational process Each phase of the process required stakeholders to
3.1 Learning to learn
interrogate aspects of psychology and agree on
how they could be applied to undergraduate
3.2 Skills training
medical education. The result is a curriculum that
3.3 Reflective practice reflects current population health needs as viewed
3.4 Situated learning by medical educators and behavioural and social
3.5 Feedback and appraisal scientists.
3.6 Assessment design and quality assurance A manageable and coherent curriculum, the outline
of which appears in BeSST (2010), can be applied to
4. Psychology topics – Post graduate level only medical undergraduate programmes in the UK. This
4.1 Leadership curriculum has the support of prominent
psychologists, medical educationalists and
4.2 Selection and Appraisal
practitioners and has been endorsed by the BPS
4.3 Organisational Change
and GMC Education committee.
Experts agreed the depth of coverage of particular
areas should be limited to what newly graduating
Validation doctors require. Medical students should not be
Critical readers – all experts in UK medical required to know details of theory development,
programmes and each with at least ten years rather they need to achieve sufficient
involvement with undergraduate medicine delivery understanding of a topic to inform their practice
and all currently professorial appointments – were and decision making at this stage of their career.
asked to read the curriculum and comment on Consideration of a number of issues is crucial in
appropriateness, relevance and structure. They ensuring successful implementation of this core
included heads of UK medical schools, professors curriculum, these include:
of medical education and professors of psychology.
Hidden curriculum. Only by understanding the
The process and content has been endorsed by six barriers to why the B&SS have not been
senior colleagues (see foreword to the core incorporated into medical undergraduate
curriculum in BeSST (2010)), all of the written programmes can any future attempts to implement
comments were positive and stressed the urgency this integrated core curriculum stand a better
for making the recommended curriculum available chance of succeeding. Implicit values are conveyed
for use in designing/re-designing existing to students through the hidden curriculum
programmes. ASME, HEA subject centres and the (Hafferty 1998). It is likely the hidden curriculum
BPS have also endorsed the core curriculum. In undermines the perceived relevance of the B&SS
addition, the core curriculum was referenced in the component of medical undergraduate programmes
latest GMC guidelines to medical schools (GMC and changing that culture may be the biggest
Tomorrow’s Doctors 2009). challenge to B&SS experts in the next decade.
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
L. Cordingley et al. 45
Establishing relevance is crucial, especially in the UK and experience in medical education have
where medical students are younger and may enter provided schools with detailed content and
with less developed understanding of the suggestions for integration and implementation.
psychological aspects of health, illness and medical
2. Better standardisation of the students’
practice. Thus, integrated curricula may have
experiences of teaching and learning about the
greater value to non-graduate entry programmes
psychology contribution to medicine across UK
and overcome some of the attitudinal barriers
medical schools. This encourages medical
towards B&SS in medical curricula. Recent work in
graduates to view psychology as making an
the US has attempted to understand more about
important contribution to their practice, sending
integration (Satterfield et al. 2010). The corollary of
a signal to students that it is core rather than
this, however, is that B&SS experts have to be
optional knowledge for practising medicine.
suitably equipped with a sound understanding of
the practice of medicine and medical education. 3. Providing opportunities for quality control by
internal assurance and external validation
procedures. It would help to build a bank of
Conclusion expertise that could be used to evaluate
This managed process of engaging both medical programmes across the UK.
and psychology experts in a common, focused task 4. Providing opportunities for further development
resulted in consensus of what psychology is of competencies in the B&SS by generating
relevant to undergraduate medicine, and may have interest in developing a forum for sharing best
contributed to the creation of more open and practice and for facilitating research in order to
positive views of psychology in a medical facilitate good medical practice.
curriculum. This process could facilitate the
adoption of a more systematic and evidence-based 5. A core curriculum will support the professional
curriculum for psychology in medical education and identity and develop career pathways of subject
could be used by the other disciplines in medicine experts who may be relatively isolated in
including; medical sociology and healthcare ethics medical schools. This would prevent the loss of
and law. It may have relevance for development of such expertise from medicine to other areas of
B&SS teaching in other healthcare professions. health care.
6. It could facilitate sharing assessment material
Recommendations across universities (for example via the UK
medical schools national assessment
We recommend the adoption of a core curriculum partnership).
for psychology in medicine. A core curriculum in
the UK has the following advantages: 7. Finally, the most important outcome is the
expectation that better knowledge and skill in
1. Supporting medical schools to deliver key the B&SS domains will have an impact on
components of Tomorrow’s Doctors. Medical patient health outcomes.
practitioners and psychologists with expertise
References BeSST (2010) A core curriculum for psychology in
undergraduate medical education. A report from the
Andersen, B.L. (2002) Biobehavioural outcomes Behavioral & Social Sciences Teaching in Medicine
following psychological interventions for cancer (BeSST) Psychology Steering Group. Higher Education
patients. Journal of Consulting and Clinical Academy. ISBN: 978-1-907207-15-0.
Psychology 70 (3), 590–610.
Boelen, C. (2002) A new paradigm for medical
Barefoot, J., Brummett, B. and Helms, M. (2000) schools a century after Flexner's report. Bulletin of
Depressive symptoms and survival of patients with the World Health Organisation 80 (7), 592–593.
coronary artery disease. Psychosomatic Medicine
62 (6), 790–795. Bolman, W.M. (1995) The place of behavioural
science in medical education and practice. Academic
Benbassat, J., Baumal, R., Borkan, J.M. and Ber, R. Medicine 70 (10), 873–878.
(2003) Overcoming barriers to teaching the
behavioural and social sciences to medical students. Cuff, P. and Vanselow, N. (2004) Improving medical
Academic Medicine 78, 372–380. education: enhancing the behavioral and social
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
46 What Psychology do Medical Students Need to Know?
science content of medical school curricula. Knight, L.V. (2006) A silly expression: consultants’
Washington, DC: National Academies Press. implicit and explicit understanding of Medical
Humanities. A qualitative analysis. Med Humanities
Dacey, A. and Weintrob, J. (1973) Human behaviour:
32 (2), 119–124.
the teaching of social and behavioural sciences in
medical schools. Social Science and Medicine 7 (12), Litva, A. and Peters, S. (2008) Exploring barriers to
943–957. teaching behavioural and social sciences in medical
education. Medical Education 42 (3), 309–314.
Firth-Cozens, J. (1992) The role of early family
experiences in the perception of organizational McGinnis, J. and Foege, W. (1993) Actual causes of
stress: fusing clinical and organizational death in the US. JAMA 270 (18), 2207–2212.
perspectives. Journal of Occupational and
Peters, S. and Litva, A. (2006) Relevant behavioural
Organizational Psychology 65, 61–75.
and social science for medical undergraduates: a
Firth-Cozens, J. (2003) Doctors, their wellbeing, and comparison of specialist and non-specialist
their stress. British Medical Journal 326 (7391), 670–671. educators. Medical Education 40 (10), 1020–1026.
Flexner, A. (1910) Medical education in the United States Rees, C.E., Sheard, C.E. and McPherson, A.C. (2002) A
and Canada. A report to the Carnegie Foundation for the qualitative study to explore undergraduate medical
Advancement of Teaching. Boston, MA: Updyke. students’ attitudes towards communication skills
learning. Med Teach 24 (3), 289–93.
GMC (2001) Good Medical Practice. The Duties of a
Doctor Registered with the GMC. London: General Russell, A., Van Teijlingen, E., Lambert, H. and Stacy, R.
Medical Council. (2004) Social and behavioural science education in
UK medical schools: current practice and future
GMC (2006) Good Medical Practice. The Duties of a
directions. Medical Education 38 (4), 409–417.
Doctor Registered with the GMC. London: General
Medical Council. Satterfield, J.M., Adler, S.R., Chen, H.C., Hauer, K.E.,
Saba, G.W. and Salazar, R. (2010) Creating an ideal
GMC Education Committee (1987) The teaching of
social and behavioural sciences curriculum for medical
behavioural sciences, community medicine and
students. Medical Education 44 (12), 1194–1202.
general practice in basic medical education. London:
General Medical Council. Sheldrake, P. (1973) Behavioural science in the
medical curriculum. Social Science and Medicine
GMC Tomorrow’s Doctors (1993) Recommendations
7 (12), 967–973.
on undergraduate medical education. London:
General Medical Council. Smith, T. and Ruiz, J. (2002), Psychosocial influences
on the development and course of coronary heart
GMC Tomorrow’s Doctors (2003) Recommendations
disease: current status and implications for research
on undergraduate medical education. London:
and practice. Journal of Consulting and Clinical
General Medical Council.
Psychology 70 (3), 548–568.
GMC Tomorrow’s Doctors (2009) Tomorrow’s
Tait, I. (1973) Behavioural science in medical
Doctors. Outcomes and Standards for Undergraduate
education and clinical practice. Social Science and
Medical Education. London: General Medical Council.
Medicine 7, 1003–1011.
Hafferty, F. (1998) Beyond curriculum reform:
Taylor, C., Graham, J., Potts, H.W.W., Richards, M.A.
confronting medicine's hidden curriculum. Academic
and Ramirez, A.J. (2005) Changes in mental health
Medicine 73 (4), 403–7.
of UK hospital consultants since the mid-1990s. The
Jaco, E.G. (1960) Problems and prospects of the Lancet 366 (9487), 742–744.
social sciences in medical education. Journal of
The British Psychological Society (BPS) (2004)
Health and Human Behavior 1, 29.
Membership and Qualifications Board. Revised Syllabus
Jones, J.W., Barge, B.N., Fay, L.M., Kunz, L.K., for the Qualifying Examination. BPS publications.
Wuebker, L.J. and Steffy, B.D. (1988) Stress and
The British Psychological Society (BPS) (2004a)
medical malpractice: organizational risk assessment
Available at http://www.bps.org.uk/networks-
and intervention. Journal of Applied Psychology
communities/member-networks/divisions/division-
73 (4), 727–735.
health-psychology/division-health-psychology.
Kawachi, I., Colditz, G.A., Ascherio, A., Rimm, E.B.,
The British Psychological Society (BPS) (2004b)
Giovannucci, E., Stampfer, M.J. and Willett, W.C.
Availaible at http://www.bps.org.uk/networks-
(1996) A prospective study of social networks in
communities/member-networks/divisions/division-
relation to total mortality and cardiovascular disease
occupational-psychology/division-occupationa.
in men in the USA. J Epidemiol Community Health
50 (3), 245–251.
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
L. Cordingley et al. 47
Vaillant, G., Sobowale, N. and McArthur, C. (1972) Wexler, M. (1976) The behavioural sciences in medical
Some psychological vulnerabilities of physicians. education. American Psychologist 31 (4), 275–283.
New England Journal of Medicine 287, 372–375.
WHO (1970) The social sciences in medical
education. WHO Chronicles 24, 478.
© 2013 S.P. Forrest, HSCE, Vol 2, Issue 2 (October 2013)
The Higher Education Academy doi:10.11120/hsce.2013.00029
You might also like
- LABOR by Poquiz PDFDocument23 pagesLABOR by Poquiz PDFAnonymous 7BpT9OWP100% (3)
- The Renaissance Period in EducationDocument8 pagesThe Renaissance Period in EducationAngelo Ace M. Mañalac0% (1)
- Robert N. Shaffer, MD at 90: An Oral History and MemoirDocument112 pagesRobert N. Shaffer, MD at 90: An Oral History and MemoirGlaucoma Research FoundationNo ratings yet
- Medical Students' Educational Strategies in An Environment of Prestige Hierarchies of Specialties and DiseasesDocument17 pagesMedical Students' Educational Strategies in An Environment of Prestige Hierarchies of Specialties and DiseasesKavirm35No ratings yet
- Evolution of Clinical Reasoning in Dental EducationDocument8 pagesEvolution of Clinical Reasoning in Dental EducationlauraNo ratings yet
- Emotional IntelligenceDocument8 pagesEmotional IntelligenceAnca OPREANo ratings yet
- BrauerDocument12 pagesBrauerNader ElbokleNo ratings yet
- Some of The Best Articles of Our First 10 Years AnDocument6 pagesSome of The Best Articles of Our First 10 Years AnJamilNo ratings yet
- How Medical Education Is ChangingDocument3 pagesHow Medical Education Is ChangingCindy ChiribogaNo ratings yet
- A Guide To Competencies, Educational Goals, and Learning Objectives For Teaching Medical Histology in An Undergraduate Medical Education SettingDocument12 pagesA Guide To Competencies, Educational Goals, and Learning Objectives For Teaching Medical Histology in An Undergraduate Medical Education SettingahmedNo ratings yet
- Defining Clinical Education Parallels in PracticeDocument9 pagesDefining Clinical Education Parallels in Practiceprakritibhatnagar1511No ratings yet
- How Can We Improve Medical EducationDocument9 pagesHow Can We Improve Medical EducationJOMARI MANALONo ratings yet
- Declaración de Consenso Sobre El Contenido de Los Currículos de Razonamiento Clínico en La Educación Médica de Pregrado 2020 INGLESDocument9 pagesDeclaración de Consenso Sobre El Contenido de Los Currículos de Razonamiento Clínico en La Educación Médica de Pregrado 2020 INGLESjaldoquiNo ratings yet
- Depression in Medical Students Current InsightsDocument11 pagesDepression in Medical Students Current InsightsKoas HAYUU 2022No ratings yet
- Community Medicine in Homoeopathy - Way Forward To Reform and InstituteDocument4 pagesCommunity Medicine in Homoeopathy - Way Forward To Reform and InstituteDr JeshNo ratings yet
- RetrieveDocument8 pagesRetrieveSahian Montserrat Angeles HortaNo ratings yet
- Integration of The Sciences Basic To Medicine... Mennin 2016Document17 pagesIntegration of The Sciences Basic To Medicine... Mennin 2016André OliveiraNo ratings yet
- A Conceptual Framework For Continuing Medical Education and Population HealthDocument16 pagesA Conceptual Framework For Continuing Medical Education and Population HealthDr. MomNo ratings yet
- First Year Doctors Experience of Work Related Wellbeing and Implications For Educational ProvisionDocument7 pagesFirst Year Doctors Experience of Work Related Wellbeing and Implications For Educational ProvisionBhagoo HatheyNo ratings yet
- Prevalence and Predictors of Anxiety in Healthcare Professions StudentsDocument10 pagesPrevalence and Predictors of Anxiety in Healthcare Professions StudentsMihaela PanaitNo ratings yet
- Erosion of Empathy in Medical SchoolDocument1 pageErosion of Empathy in Medical SchoolChristian ObandoNo ratings yet
- An Evidence Based Patient Centered Method Makes The Biopsychosocial Model ScientificDocument6 pagesAn Evidence Based Patient Centered Method Makes The Biopsychosocial Model Scientificlumi_vulpitzaNo ratings yet
- Medical Education in The United States. The Role of AndragogyDocument5 pagesMedical Education in The United States. The Role of AndragogydarkbyronsNo ratings yet
- Contuinity of EducationDocument9 pagesContuinity of EducationAngelina CalistaNo ratings yet
- Nursing ResearchDocument15 pagesNursing Researchsubhashreepal13No ratings yet
- Depression and Anxiety Among Medical StudentsDocument6 pagesDepression and Anxiety Among Medical StudentsAlejandro MartinezNo ratings yet
- Geneticsgenomics in Nursing and Health CareDocument15 pagesGeneticsgenomics in Nursing and Health Careapi-215814528No ratings yet
- Philippe Chastonay, Nu Viet Vu, Jean-Paul Humair, Emmanuel Kabengele Mpinga and Laurent BernheimDocument14 pagesPhilippe Chastonay, Nu Viet Vu, Jean-Paul Humair, Emmanuel Kabengele Mpinga and Laurent BernheimtimtimNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Biochemistry in The Medical CurriculumDocument4 pagesBiochemistry in The Medical CurriculumMarites L. DomingoNo ratings yet
- A_New_Teaching_Forum_to_Aid_the_PromotioDocument85 pagesA_New_Teaching_Forum_to_Aid_the_PromotioSGT NEXTNo ratings yet
- Clinical Reasoning What Do Nurses Physicians and Students Reason AboutDocument10 pagesClinical Reasoning What Do Nurses Physicians and Students Reason AboutUmam AcademyNo ratings yet
- Final NaDocument42 pagesFinal NaChastin PeriasNo ratings yet
- Psych 06 00025 v2Document12 pagesPsych 06 00025 v2enrichedenlightenment05No ratings yet
- Mental Health in Medical FacultiesDocument3 pagesMental Health in Medical Facultiestegen79876No ratings yet
- Content ServerDocument11 pagesContent ServerMona AL-FaifiNo ratings yet
- Putting It All Together: Building A Four-Year Curriculum: S. Edwards Dismuke, MD, MSPH, and Alicia M. Mcclary, MS, EddDocument3 pagesPutting It All Together: Building A Four-Year Curriculum: S. Edwards Dismuke, MD, MSPH, and Alicia M. Mcclary, MS, EddtimtimNo ratings yet
- Incorporating Spirituality Into Health Sciences - Schonfeld 2014Document12 pagesIncorporating Spirituality Into Health Sciences - Schonfeld 2014Mércia FiuzaNo ratings yet
- Course Orientation - Preventive Medicine 4 - AY 2021-2022 - SignedDocument24 pagesCourse Orientation - Preventive Medicine 4 - AY 2021-2022 - SignedJolaine ValloNo ratings yet
- Psychological Well-Being in Nursing Students: A Multicentric, Cross-Sectional StudyDocument11 pagesPsychological Well-Being in Nursing Students: A Multicentric, Cross-Sectional StudyLohree Mie HanoyanNo ratings yet
- Yjbm 93 3 433Document7 pagesYjbm 93 3 433daeron42No ratings yet
- Baldassin2008 FDocument8 pagesBaldassin2008 FJr SparkNo ratings yet
- Psychiatry Research: Letter To The EditorDocument2 pagesPsychiatry Research: Letter To The EditorZachNo ratings yet
- Better Together A NaturalistiDocument10 pagesBetter Together A Naturalistinurlaila marasabessyNo ratings yet
- Health Promotion in Medical Education Lessons From A Major Undergraduate Curriculum ImplementationDocument10 pagesHealth Promotion in Medical Education Lessons From A Major Undergraduate Curriculum ImplementationKAREN VANESSA MUÑOZ CHAMORRONo ratings yet
- Module 1 Scholarly Writing Self ReflectionDocument9 pagesModule 1 Scholarly Writing Self Reflectionapi-643329064No ratings yet
- Maintaining Well-Being: A Narrative Review On Burnout Experienced by Medical Students and ResidentsDocument18 pagesMaintaining Well-Being: A Narrative Review On Burnout Experienced by Medical Students and ResidentsClau TomNo ratings yet
- Narrative Review Burnout Students and ResidentsDocument19 pagesNarrative Review Burnout Students and ResidentsStefania TacuNo ratings yet
- Hangbook MBBS Addendum Year3,4,5Document30 pagesHangbook MBBS Addendum Year3,4,5ambreenayub23No ratings yet
- Students' Perception of Medical School Stress and TheirDocument8 pagesStudents' Perception of Medical School Stress and TheirPamela Francisca Bobadilla BurgosNo ratings yet
- Psychological distress among undergraduate medical students the influence of excessive daytime sleepiness and family functioningDocument16 pagesPsychological distress among undergraduate medical students the influence of excessive daytime sleepiness and family functioningsebas paezNo ratings yet
- Medical Student Mental Health 3.0 ImprovingDocument5 pagesMedical Student Mental Health 3.0 Improvingmemmuse95No ratings yet
- Anxiety Among Medical StudentsDocument4 pagesAnxiety Among Medical Studentsvihaan chaudharyNo ratings yet
- Assignment - Essential QuestionsDocument5 pagesAssignment - Essential QuestionsFionah RetuyaNo ratings yet
- Contemporary Global Perspectives of Medical Students On Research During Undergraduate Medical Education A Systematic Literature ReviewDocument14 pagesContemporary Global Perspectives of Medical Students On Research During Undergraduate Medical Education A Systematic Literature Reviewhabihabi0609No ratings yet
- DOT-syllabus 220130 163901Document19 pagesDOT-syllabus 220130 163901Angkasa LamaNo ratings yet
- Articulo PDFDocument9 pagesArticulo PDFNathalie EstephaniaNo ratings yet
- GROUP 1 - Chapter 2 (Revised)Document9 pagesGROUP 1 - Chapter 2 (Revised)itsgumbololNo ratings yet
- School Based Interventions To Improve Health.17Document9 pagesSchool Based Interventions To Improve Health.17lengers poworNo ratings yet
- Health Promotion in Context: A Reflective-Analytical ModelDocument6 pagesHealth Promotion in Context: A Reflective-Analytical Modelmitha letoNo ratings yet
- Mak, 2018. Estilo de Vida Promotor de La Salud y Calidad de Vida Entre Los Estudiantes de Enfermería ChinosDocument8 pagesMak, 2018. Estilo de Vida Promotor de La Salud y Calidad de Vida Entre Los Estudiantes de Enfermería ChinosIván Lázaro IllatopaNo ratings yet
- Shared Goals For Mental Health Research What Why and When For The 2020sDocument10 pagesShared Goals For Mental Health Research What Why and When For The 2020saimeejacobs370No ratings yet
- The Question of Competence: Reconsidering Medical Education in the Twenty-First CenturyFrom EverandThe Question of Competence: Reconsidering Medical Education in the Twenty-First CenturyNo ratings yet
- Reading7th 2 - Ready D Complete and AdptedDocument3 pagesReading7th 2 - Ready D Complete and AdptedRosa Maria Sá RibeiroNo ratings yet
- Foundation Forum: College and Career Center Tops The Priority ListDocument4 pagesFoundation Forum: College and Career Center Tops The Priority ListnsidneyNo ratings yet
- Teaching AptitudeDocument9 pagesTeaching AptitudeSAFA's CreationNo ratings yet
- Fazmeer Rasheed CV (Accountant) FDocument4 pagesFazmeer Rasheed CV (Accountant) FImam HusainNo ratings yet
- Lesson PlanDocument22 pagesLesson PlanHarim Qudsi100% (2)
- CAP Knowledge and Skills - IsADocument1 pageCAP Knowledge and Skills - IsAengr_khalid1No ratings yet
- Public Speaking - Reading Material Week 1Document20 pagesPublic Speaking - Reading Material Week 1Linh KhánhNo ratings yet
- Teaching P.E and Health in Elementary Grades: MC PehDocument5 pagesTeaching P.E and Health in Elementary Grades: MC PehIra BerunioNo ratings yet
- My CVDocument2 pagesMy CVapi-546470778No ratings yet
- Daily Lesson LOG: M10AL-Ig-1 M10AL-Ig-1 M10AL-Ig-1 M10AL-Ig-1Document4 pagesDaily Lesson LOG: M10AL-Ig-1 M10AL-Ig-1 M10AL-Ig-1 M10AL-Ig-1ederlynNo ratings yet
- NOTESmtlaws LectureDocument11 pagesNOTESmtlaws LectureCharlemagne GuiribaNo ratings yet
- HAP44 Advanced Manual 10-08-08Document226 pagesHAP44 Advanced Manual 10-08-08chirijas208390% (10)
- Seminar Evaluation and Feedback FormDocument2 pagesSeminar Evaluation and Feedback FormMa. Venus A. Carillo100% (2)
- MechanicalDocument16 pagesMechanicalBluesunset1No ratings yet
- ACTIVITY SHEET PR1 WEEK 14 Q4 Finding Answers Through Data CollectionDocument4 pagesACTIVITY SHEET PR1 WEEK 14 Q4 Finding Answers Through Data CollectionAlyssa AngananganNo ratings yet
- Fool Proof MarketingDocument290 pagesFool Proof MarketingKrzysieko0100% (2)
- A Detailed Lesson Plan in Teaching Mathematics VDocument15 pagesA Detailed Lesson Plan in Teaching Mathematics VKimberly Ann M. AbalosNo ratings yet
- T-TESS Rubric & Documentation: Domain 1.1: Standards and AlignmentDocument17 pagesT-TESS Rubric & Documentation: Domain 1.1: Standards and AlignmentSofia Violeta100% (1)
- Internal Audit ProjectDocument38 pagesInternal Audit ProjectStoryKing100% (1)
- Course Outline in Assessment 1 and Principle 2Document14 pagesCourse Outline in Assessment 1 and Principle 2Benjie Moronia Jr.No ratings yet
- Advanced Scenario 5 - Samantha Rollins (2018)Document10 pagesAdvanced Scenario 5 - Samantha Rollins (2018)Center for Economic Progress0% (1)
- Enrolment Proceedings in GJCSDocument2 pagesEnrolment Proceedings in GJCSDeleter DoraNo ratings yet
- Losoff Haley Resume 2024Document2 pagesLosoff Haley Resume 2024api-736612890No ratings yet
- STID1013 Silibus First Sem 2011Document6 pagesSTID1013 Silibus First Sem 2011Sharifah RubyNo ratings yet
- Introduction To The Special Issue The Ethnomusicology of Western Art Music PDFDocument17 pagesIntroduction To The Special Issue The Ethnomusicology of Western Art Music PDFSamuel TanNo ratings yet
- Using ChatGPT and Prompting Like Leonardo Da VinciDocument58 pagesUsing ChatGPT and Prompting Like Leonardo Da VinciKamal A. AL-HumaidiNo ratings yet
- Khalsa College For Women, Civil Lines, Ludhiana: .. Shaping Careers For A Better TomorrowDocument2 pagesKhalsa College For Women, Civil Lines, Ludhiana: .. Shaping Careers For A Better TomorrowPooja ChatleyNo ratings yet