Professional Documents
Culture Documents
pyelonephritis
pyelonephritis
Uploaded by
AndreaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
pyelonephritis
pyelonephritis
Uploaded by
AndreaCopyright:
Available Formats
Acute Pyelonephritis in Adult Patients:
Diagnosis and Management
NOTE: This guideline does not apply to chronic or recurrent pyelonephritis.
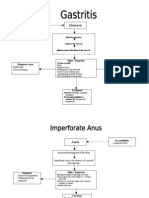
Patient presents with symptoms of pyelonephritis:
Fever > 100.4°F
CVA tenderness
Shaking chills/rigors
New onset of delirium
Dysuria
Urinary urgency and/or frequency
Suprapubic or flank pain
Note: See OSUWMC Urinary Tract Infection in Adult Patients: Diagnosis
and Management guideline.
Consider alternative diagnosis:
Tube-ovarian abscess
Nephrolithiasis
Appendicitis
Positive
No Pancreatitis
urinalysis?
Perforated viscus
Tubal pregnancy
Yes Pelvic inflammatory disease
Lower lobe pneumonia
Indications for observation / admission?
Inability to take PO fluids or medications
Significant dehydration Discharge to home
Uncertainty about the diagnosis Collect urine culture (prior to antibiotics)
Severe illness (high fevers: > 100.4ºF; abnormal vital signs: Give first dose of antibiotics
No
HR < 90 bpm, BP >120/80 mmHg, RR > 20 breath per ○ See Table 1 for recommended empiric
minute) antibiotics
High likelihood of non-compliance with outpatient therapy Follow up on cultures and sensitivities
Poor access to resources
Immunosuppression
Yes
Complicating factors?
Renal transplantation
UNCOMPLICATED Pyelonephritis
Obstruction
Begin antibiotic regimen
Nephrolithiasis
○ See Table 1 for recommended empiric
Anatomic abnormality
antibiotics
Neurogenic bladder No
Imaging generally not indicated*
Pregnancy
Transition to oral therapy as soon as tolerated
Indwelling urinary catheter
Follow up on cultures and sensitivities and de-
Failed outpatient therapy
escalate therapy as appropriate
Healthcare-associated infection
Recent instrumentation (ureteral stent, cystoscopy)
Yes CDU / Observation
COMPLICATED Pyelonephritis
Obtain blood cultures
Begin antibiotic regimen (See Table 2 for recommended empiric antibiotics) Collect urine culture prior to antibiotics
Consider imaging for suspected infection* Check CBC and Chem 6, if not done
○ When imaging is necessary, CT is still the recommended Supportive care as indicated (IV fluids,
modality. antipyretics; consider early removal of
○ See pyelonephritis algorithm in the OSUWMC Diagnostic Imaging urinary catheters, ureteral stents, etc.)
During Pregnancy guideline.
Consultation based on results as appropriate (Infectious Diseases, Urology)
Follow up on cultures and sensitivities and de-escalate therapy as
appropriate Admit to hospital
Consider longer duration of therapy (at least 14 days)
*Note: See ACR Appropriateness Criteria® for Acute Pyelonephritis
2
Table 1. Empiric Antibiotics Recommended for UNCOMPLICATED Pyelonephritis
• Due to increasing prevalence of resistance in E. coli, TMP/SMX, ciprofloxacin, and ampicillin are
generally not recommended for therapy, but may be an option when susceptibilities are known.
• First-generation cephalosporins can be used based on OSUWMC’s current antibiogram.
• Cephalosporins are ineffective for the treatment of Enterococcus.
• Doses are for patients with normal renal function.
o Modified doses may be required in renal insufficiency.
Medication* Dose Notes
Cephalexin 500-1000 mg Q6-8 hrs. X 10-14 days (Oral) • One-time dose of ceftriaxone is required
in addition per IDSA dosing.
Ceftriaxone 1 g every 24 hrs. (IV or IM)
Cefdinir 300 mg Q12 hrs. X 7 days (Oral)
Cefazolin 1 g Q8 hrs. X 7 days (IV)
Levofloxacin 750 mg Q24 hrs. X 7 days (IV or Oral) • Caution in patients who are elderly or
who have history of multiple urinary tract
infections due to increased resistance.
• Should be reserved for use in patients
that are penicillin allergic.
*Listed in order of preference
Table 2. Empiric Antibiotics Recommended for COMPLICATED Pyelonephritis
• Cephalosporins are ineffective for the treatment of Enterococcus.
• Doses are for patients with normal renal function. Modified doses may be required in renal insufficiency.
• Initial treatment should be modified based upon the results of urine culture and sensitivity.
• Extended spectrum beta-lactamase organisms (ESBL) risk factors: history of ESBL infection, nursing
home resident exposure to multiple antibiotics.
Medication Dose Notes
Piperacillin / 4.5 g Q8 hrs. X 14 days (IV) • β-lactamase inhibitor (tazobactam) may
tazobactam (preferred) provide broader coverage for some Gram-
negative enterics.
• Recommended if ampicillin-susceptible
Enterococcus or pseudomonas suspected.
Cefepime 1 g Q12 hrs. X 14 days (IV) • Use for penicillin allergy.
3
References
• International Clinical Practice Guidelines for the
Treatment of Acute Uncomplicated Acute Cystitis
and Acute Pyelonephritis in Women: A 2010
Update by the Infectious Diseases Society for
America and the European Society for
Microbiology and Infectious Diseases. Clinical
Infectious Diseases 2011; 52:e103-e120.
• ACR Appropriateness Criteria®. Acute
Pyelonephritis. American College of Radiology -
Medical Specialty Society. 1995 (revised 2012)
• Management of Suspected Bacterial Urinary Tract
Infection in Adults - A National Clinical Guideline.
Scottish Intercollegiate Guidelines Network. July
2006.
Order Sets
• OSU IP GU: Admission Urology (aka
pyelonephritis)
• OSU IP ED: CDU/OBS Pyelonephritis
Quality Measures
For ICU and Non-ICU patients:
• Percent of patients with CT imaging
• Appropriate antibiotics ordered based on
urine or blood work
Guideline Authors
• Kurt Stevenson, MD, MPH
• Erica Reed, PharmD, BCPS
• C. Alexander Grieco, MD
• Jason Prosek, MD
• Harrison Weed, MD
Guideline Approved
April 27, 2016. Fourth Edition.
Disclaimer: Clinical practice guidelines and
algorithms at The Ohio State University Wexner
Medical Center (OSUWMC) are standards that are
intended to provide general guidance to clinicians.
Patient choice and clinician judgment must remain
central to the selection of diagnostic tests and
therapy. OSUWMC’s guidelines and algorithms are
reviewed periodically for consistency with new
evidence; however, new developments may not be
represented.
Copyright © 2016. The Ohio State University Wexner
Medical Center. All rights reserved. No part of this
document may be reproduced, displayed, modified, or
distributed in any form without the express written
permission of The Ohio State University Wexner
Medical Center.
You might also like
- Infectious Diseases - Gorbach & Bartlett, 3E (2004)Document2,559 pagesInfectious Diseases - Gorbach & Bartlett, 3E (2004)Mădălina SuciuNo ratings yet
- Drug Study: Beta-Lactmase-Producing Strains of S. Aureus, or by Piperacillin Tazobactam SusceptibleDocument2 pagesDrug Study: Beta-Lactmase-Producing Strains of S. Aureus, or by Piperacillin Tazobactam SusceptibleKristine Young83% (6)
- UTI TreatmentDocument3 pagesUTI TreatmentMaria RezitadinaNo ratings yet
- UTI Treatment Algorithm - Sharp Mesa Vista 2Document3 pagesUTI Treatment Algorithm - Sharp Mesa Vista 2Fitri 1997No ratings yet
- Augmenten (Amoxicillin Clavulan)Document2 pagesAugmenten (Amoxicillin Clavulan)Adrianne BazoNo ratings yet
- Cefuroxime Losartan DRUG STUDYDocument7 pagesCefuroxime Losartan DRUG STUDYKiela Therese LabroNo ratings yet
- Classification: Cefditoren, As This Agent May CauseDocument3 pagesClassification: Cefditoren, As This Agent May CauseHavier EsparagueraNo ratings yet
- AppendectomyDocument6 pagesAppendectomyapi-3797941100% (10)
- Paediatric ManualDocument223 pagesPaediatric ManualKyra PoggenpoelNo ratings yet
- Drug AnalysisDocument8 pagesDrug AnalysisDaniel Andre S. SomorayNo ratings yet
- Infection Antimicrobial Medication CardsDocument16 pagesInfection Antimicrobial Medication Cards方郝建No ratings yet
- Name of Drugs, Classification, Dosage & Route Action Indication Side Effects Nursing ResponsibilitiesDocument5 pagesName of Drugs, Classification, Dosage & Route Action Indication Side Effects Nursing ResponsibilitiesAiramCeszDelaCruzNo ratings yet
- Acute Abdominal Pain: DR Naing Naing Oo Senior LecturerDocument28 pagesAcute Abdominal Pain: DR Naing Naing Oo Senior LecturerAbdulrahman NajiNo ratings yet
- Gastro PathophysiologyDocument4 pagesGastro PathophysiologyPaul JoloNo ratings yet
- Omep, Ceftriaxone, FurosemideDocument3 pagesOmep, Ceftriaxone, FurosemideThyataira chuaNo ratings yet
- Urinary Tract Infection and Pyelonephritis AIIMS Kalyani 7th SemesterDocument39 pagesUrinary Tract Infection and Pyelonephritis AIIMS Kalyani 7th Semesterrakesh raushanNo ratings yet
- Shivani PDFDocument3 pagesShivani PDFdeepukumarNo ratings yet
- Chapter 36 The Urinary System in GynaecologyDocument19 pagesChapter 36 The Urinary System in Gynaecologypmj050gpNo ratings yet
- By: Clarissa E. Guifaya BSN301/GROUP 3Document17 pagesBy: Clarissa E. Guifaya BSN301/GROUP 3Clarissa GuifayaNo ratings yet
- Drug StudyDocument22 pagesDrug StudySierraSiwaNo ratings yet
- Drug StudyDocument22 pagesDrug StudySierraSiwaNo ratings yet
- Urinary Tract InfectionDocument42 pagesUrinary Tract InfectionhaniNo ratings yet
- Morning Report - PyelonephritisDocument54 pagesMorning Report - PyelonephritisjonNo ratings yet
- The Diagnosis and Treatment of Adult Urinary Tract Infections inDocument22 pagesThe Diagnosis and Treatment of Adult Urinary Tract Infections inPaola Andrea Balsero SalgadoNo ratings yet
- CeftriaxoneDocument5 pagesCeftriaxoneCastillo MikaellaNo ratings yet
- PeritonitisDocument15 pagesPeritonitiscgqphqdrytNo ratings yet
- A Case Study: Nephrolit HiasisDocument19 pagesA Case Study: Nephrolit HiasisCarna BuenconsejoNo ratings yet
- CefalexinDocument1 pageCefalexinVien Demasu-ayNo ratings yet
- Acute Pyelonephritis: Causes/ Risk FactorsDocument6 pagesAcute Pyelonephritis: Causes/ Risk FactorsShiraishiNo ratings yet
- Appendicitis: Diseases and Conditions: AppendicitisDocument6 pagesAppendicitis: Diseases and Conditions: AppendicitisWen RodsaNo ratings yet
- Invanz (Ertapenem)Document2 pagesInvanz (Ertapenem)E100% (1)
- JM Drug Study CaseDocument4 pagesJM Drug Study CaseMilky Lescano LargozaNo ratings yet
- Dipolog Medical Center College Foundation Inc. College of NursingDocument16 pagesDipolog Medical Center College Foundation Inc. College of NursingTiffany AdriasNo ratings yet
- DS - Mod9Document2 pagesDS - Mod9designericlelynsoronioNo ratings yet
- Drug StudyDocument12 pagesDrug StudyJessica Pacris MaramagNo ratings yet
- Generic Name Dosage / Frequency Action Side Effects Nursing ResponsibilityDocument9 pagesGeneric Name Dosage / Frequency Action Side Effects Nursing Responsibilityorhocelo6908No ratings yet
- Olores Drugstudy Cephalothin SodiumDocument7 pagesOlores Drugstudy Cephalothin SodiumTintin KingNo ratings yet
- Rle Rot 4Document3 pagesRle Rot 4Elle RosalesNo ratings yet
- HyperbilirubinemiaDocument10 pagesHyperbilirubinemiachiboogs456100% (1)
- Pancreatitis Group 3 NCM 116Document21 pagesPancreatitis Group 3 NCM 116Diana Jane LauretaNo ratings yet
- JFP - 1986 09 - v23 - I3 - A Case of Chronic AppendicitisDocument2 pagesJFP - 1986 09 - v23 - I3 - A Case of Chronic AppendicitisBilalNo ratings yet
- PyelonephritisDocument10 pagesPyelonephritisalina abu rumi100% (1)
- Evangelista Drug-StudyDocument15 pagesEvangelista Drug-Studydinglasanerica57No ratings yet
- 4 Cefazolin Drug StudyDocument4 pages4 Cefazolin Drug Studyshadow gonzalezNo ratings yet
- Canuuc - Uti May 2017Document31 pagesCanuuc - Uti May 2017Praluki HerliawanNo ratings yet
- Tamoxifen NolvadexDocument1 pageTamoxifen NolvadexAdrianne Bazo100% (1)
- Surgical AbdomenDocument3 pagesSurgical Abdomendude dNo ratings yet
- UTI Disorder PDFDocument23 pagesUTI Disorder PDFMonarahayuNo ratings yet
- Acute Appendicitis: History and ExaminationDocument6 pagesAcute Appendicitis: History and ExaminationPraktek Dokter Umum drjosefdrelsyNo ratings yet
- Does My Patient Need To Be Screened or Treated For A Urinary Tract InfectionDocument4 pagesDoes My Patient Need To Be Screened or Treated For A Urinary Tract Infectiontsiko111No ratings yet
- Cefuroxime Drug StudyDocument3 pagesCefuroxime Drug StudyRem remNo ratings yet
- 5551 13868 1 PBDocument6 pages5551 13868 1 PBNanaNo ratings yet
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDocument2 pagesDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNo ratings yet
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- The Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesFrom EverandThe Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- The Perfect Neutropenic Diet Cookbook; The Complete Nutrition Guide To Reinstating Overall Health For General Wellness With Delectable And Nourishing RecipesFrom EverandThe Perfect Neutropenic Diet Cookbook; The Complete Nutrition Guide To Reinstating Overall Health For General Wellness With Delectable And Nourishing RecipesNo ratings yet
- HandoutsDocument74 pagesHandoutschayChay gapolNo ratings yet
- Theories of Disease Causation Level200Document5 pagesTheories of Disease Causation Level200Annan Agyekum JoshuaNo ratings yet
- Tigecycline Alone or in CombinationDocument13 pagesTigecycline Alone or in CombinationSanjay NavaleNo ratings yet
- Essay:-''Coronaviruses Are A Family of Viruses Known For Containing Strains That Cause PotentiallyDocument4 pagesEssay:-''Coronaviruses Are A Family of Viruses Known For Containing Strains That Cause PotentiallymuddasirnaddemNo ratings yet
- Lec 5Document16 pagesLec 5Bassam AlgalalyNo ratings yet
- Binda BIO3219 Lab5Document12 pagesBinda BIO3219 Lab5Ronaldo BindaNo ratings yet
- Part IIDocument15 pagesPart IIIan LapidezNo ratings yet
- A Plant Pathologist or A Student Taking Plant Pathology Is Often Asked by Friends or Associates The Following QuestionsDocument21 pagesA Plant Pathologist or A Student Taking Plant Pathology Is Often Asked by Friends or Associates The Following QuestionsMirza ZiaaNo ratings yet
- Cosmetic Contact Lens-Related Corneal Infections in AsiaDocument8 pagesCosmetic Contact Lens-Related Corneal Infections in AsiaAnggitaNo ratings yet
- WHO IVB 15.09 EngDocument59 pagesWHO IVB 15.09 EngAbdul AhadNo ratings yet
- Otitis MediaDocument2 pagesOtitis MediaKoushik Mazumder ShuvoNo ratings yet
- 2022.11.30 - Celeste Solum - Moving in For The KillDocument20 pages2022.11.30 - Celeste Solum - Moving in For The KillJFBrNo ratings yet
- WJG 27 1691Document26 pagesWJG 27 1691Valentina QuinteroNo ratings yet
- Summary OphthalmologyDocument86 pagesSummary Ophthalmologymarina_shawkyNo ratings yet
- Uhuru's Sixteenth Presidential Address On Covid-19Document10 pagesUhuru's Sixteenth Presidential Address On Covid-19The Star KenyaNo ratings yet
- Lab Manual - Sputum - Microscopy (Final)Document117 pagesLab Manual - Sputum - Microscopy (Final)kushwaha.santosh290No ratings yet
- IN893000 v6.0 Clearview PBP2a SA Culture Colony ProducDocument101 pagesIN893000 v6.0 Clearview PBP2a SA Culture Colony ProducRazaz AdilNo ratings yet
- Tubex Test PDFDocument2 pagesTubex Test PDFHenry Philip Sabado Presto100% (1)
- infection 7 (تم حفظه تلقائيا)Document22 pagesinfection 7 (تم حفظه تلقائيا)مرتضى محمد منصورNo ratings yet
- Vaccines of The National Immunization Program of TDocument7 pagesVaccines of The National Immunization Program of T1BSN04 DE GUZMAN, LEMARRY JOYCE V.No ratings yet
- Molecular Biology of The Gene: Chapter ObjectivesDocument17 pagesMolecular Biology of The Gene: Chapter Objectivesirene9tan9ailianNo ratings yet
- Schematic Diagram of Pleural EffusionDocument2 pagesSchematic Diagram of Pleural EffusionJesselle Laserna0% (1)
- The Concept of Public HealthDocument13 pagesThe Concept of Public Healthhamza althariNo ratings yet
- Water Pollution and Human HealthDocument5 pagesWater Pollution and Human HealthPurusottam AgarwalNo ratings yet
- ST George Respiratory QUestionnaireDocument6 pagesST George Respiratory QUestionnaireFranciscoJ.ReynaSepúlvedaNo ratings yet
- What Are Bacteroides ?Document13 pagesWhat Are Bacteroides ?u77No ratings yet
- Reflection: "See The Light at The End of The Tunnel"Document2 pagesReflection: "See The Light at The End of The Tunnel"John Flex SingculanNo ratings yet
- Health and IllnessDocument3 pagesHealth and Illnessfrico13No ratings yet
- Environmental Hazards and Human HealthDocument36 pagesEnvironmental Hazards and Human HealthJohn Mark CelosaNo ratings yet