Professional Documents
Culture Documents
mellman2003
mellman2003
Uploaded by
Georgia MouraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
mellman2003
mellman2003
Uploaded by
Georgia MouraCopyright:
Available Formats
Psychotherapy Competencies: Development and
Implementation
Lisa A. Mellman, M.D.
Eugene Beresin, M.D.
New requirements by the Psychiatry Residency Review Committee of the Accreditation
Council for Graduate Medical Education maintain that residents must be competent in five
specified psychotherapies. This shift toward evidence-based education and assessment high-
lights psychotherapy as an integral part of a psychiatrist’s training and identity, while in-
troducing accountability of training programs, faculty, and individual residents. Training
directors must now find the resources in faculty, patients, and residency teaching time to
teach, supervise and assess residents so they graduate with competency. The American As-
sociation of Directors of Residency Training (AADPRT) appointed a Task Force on Compe-
tency to assist training directors with the new requirements. The Task Force, through the
establishment of five workgroups, has written sample competencies for each required psy-
chotherapy: brief, cognitive behavioral, psychodynamic, supportive and combined psycho-
therapy and psychopharmacology. In this article, the authors describe the historical context
of the new requirements, and the goals, process and issues that arose in the development of
the sample competencies. (Academic Psychiatry 2003; 27:149–153)
T he Psychiatry Residency Review Committee
(RRC) issued new regulations that stipulate, ef-
fective January 1, 2001, residency programs must
over the past two decades. Biological psychiatry and
new technologies offered greater understanding of
psychiatric disorders and the brain while promising
demonstrate that residents are competent in five rapid remission of disease. The pharmaceutical in-
specified psychotherapies: brief, cognitive behav- dustry attained significant control over the direction
ioral, psychodynamic, supportive and combined psy- and funding of clinical psychiatric research through
chotherapy and psychopharmacology (1). These new large-scale drug studies. The soaring cost of health-
regulations, an outgrowth of the Outcomes Project of care, stigma of mental illness, and competition from
the Accreditation Council for Graduate Medical Edu- less expensive providers led managed care to further
cation (ACGME) (2), are part of the growing shift to- diminish the role of psychotherapy in the definition
ward evidence-based medical education and public of a psychiatrist (5,6). Specifically, the managed care
accountability (3,4). In the Outcomes Project, the movement systematically argued for fewer psychia-
ACGME mandated that all medical specialties ensure
that its residents develop competency in six core ar- Dr. Mellman is Associate Clinical Professor and Associate
eas: patient care, medical knowledge, interpersonal Director of Training in the Department of Psychiatry, Columbia
University College of Physicians and Surgeons, New York State
and communication skills, practice-based learning Psychiatric Institute, New York, NY. Dr. Beresin is Associate Pro-
and improvement, professionalism, and systems- fessor of Psychiatry, Department of Psychiatry, Harvard Medical
based practice. Only psychiatry has additional re- School, Boston, Massachusetts. Dr. Beresin is also Media Column
Editor for Academic Psychiatry. Address correspondence to Dr.
quirements for competency in the five specified types
Mellman, New York State Psychiatric Institute, 1051 Riverside
of psychotherapy. Dr., New York, NY 10032, lam3@columbia.edu (E-mail).
Psychotherapy training has gradually eroded Copyright 䉷 2003 Academic Psychiatry.
Academic Psychiatry, 27:3, Fall 2003 149
DEVELOPMENT AND IMPLEMENTATION
trists and a re-definition of the role of psychiatrist as ment modalities. Residents could meet these require-
“consultant” for diagnostic evaluations and medica- ments passively by completing rotations, showing up
tion management. Its demand for limited lengths of for sessions with patients, and attending classes and
treatment, brief visits, and reduced reimbursement supervision. Second, as psychotherapy teaching and
for psychotherapy, in conjunction with decreased fed- supervision gradually diminished in importance and
eral funding for residency education, has impacted as lengths of stay decreased, residents were only ex-
the way residents are trained. Meanwhile, psycho- posed to the treatment modalities available on their
analysts, formerly the prototypical clinician teachers rotations. Opportunities for conducting psychother-
and chairs in academic medical centers, became relics apy disappeared from most inpatient units, and out-
of the past in many training centers, losing their es- patient psychotherapy training has never been uni-
teemed place in residency education. form. Third, since the psychotherapy modalities
Erosion of psychotherapy training results in res- taught in any depth varied across residencies, the lack
idency graduates who may be unskilled in conduct- of uniform standards in psychotherapy left psycho-
ing psychotherapy and unaware of deficiencies in therapy teaching to the discretion of each program.
their understanding of a biopsychosocial model. Se- In many programs, specific types of psychotherapy
nior examiners at the psychiatry oral board exami- were amalgamated and lost any differentiation. Ro-
nations, themselves well trained in psychotherapy, tation sites often were determined by the source of
often lament this change as they examine board can- funding for the resident line or position, sometimes
didates who do not understand that symptoms may further diminishing psychotherapy exposure. Finally,
have arisen in the context of life events or relation- even in areas of the country where postresidency psy-
ships which have particular meanings to the patient. choanalytic training used to be common, residents no
Residencies vary widely in psychotherapy education. longer routinely enter personal psychotherapy or
Some programs and geographic areas have no ex- psychoanalysis. In many programs faculty identify-
perts in a particular modality, or at least none on fac- ing themselves as psychopharmacologists and psy-
ulty. In an informal 2001 survey of psychodynamic chotherapists lived often in separate worlds. Few res-
psychotherapy training in residency, didactic course idency programs fully addressed details of combined
hours ranged from 24 hours to 200, treatment hours treatment, for example, considering how medication
from 100 to 650, and supervision hours from 50 to 400 might impact on psychotherapy, or how taking med-
hours per resident (Mellman, unpublished). In con- ication affects the treatment relationship. Although
trast, Wallerstein reported up to 3,000 hours during supervisory reports for psychotherapy trainees were
residency training devoted to learning psychother- required, the specific teaching goals were up to each
apy shortly after World War II (7). program and often not comprehensively specified.
Using a food analogy, psychotherapeutic foods were
How Was Psychotherapy Taught? sampled by residents, but a balanced diet and atten-
tion to comprehensive nutrition was not necessarily
The adage in medical school is, “See one, do one, guaranteed.
teach one.” Psychotherapy training has traditionally
followed an apprenticeship model. “Seeing” included Renewed Interest in Psychotherapy Training
undertaking one’s own personal psychotherapy and
observing senior experts interview patients and con- In 1994, the American Association of Directors of Psy-
duct psychotherapies, “doing” meant spending chotherapy Training (AADPRT) established a Task
hours treating patients and receiving one-on- one su- Force on Psychotherapy to address the diminished
pervision, and “teaching” began during residency or place of psychotherapy education in residency. Over
afterwards, often amidst further psychotherapy train- 6 years, six initial participants grew to over 80 as in-
ing. Several factors have contributed to the gradual terest in psychotherapy training increased, and mem-
decrease in psychotherapy training. First, until re- bers participated in a survey of essential psychother-
cently, residency requirements for accreditation by apy skills in residents (Goldberg et al unpublished).
the RRC included timed rotations and exposure to These results were endorsed by AADPRT as impor-
particular diagnoses, groups of patients, and treat- tant skills for residents. In 1996, the American Psy-
150 Academic Psychiatry, 27:3, Fall 2003
MELLMAN AND BERESIN
chiatric Association (APA) established the Commis- able to identify and manage all types of transference,
sion on Psychotherapy by Psychiatrists (COPP) to or only those that jeopardize treatment? To what ex-
focus on psychotherapy education and revitalize psy- tent should residents be competent in guided discov-
chotherapy. Members of COPP have published data ery and bridging between sessions in cognitive be-
on psychotherapy efficacy (8), teaching (9,10,11), and havioral therapy? Must all competencies be met for
supervision (12), and conducted several psychother- graduation, or only a majority? If psychotherapy ex-
apy education programs for residency training direc- perts were consulted, would they realistically under-
tors and educators. stand a resident’s capability or impose even higher
standards of expertise? Questions emerged regarding
AADPRT Task Force on Competency teaching and assessment by faculty. To what extent
would all supervisory faculty be able to use the same
When the ACGME announced the outcome project in standards of assessment reliably? To what extent
1999, AADPRT established a Task Force on Compe- would programs lacking faculty expertise and other
tency. Its mandate was to assist the field in imple- resources balk at these competencies? To what extent
menting and assessing the core competencies and five do programs have adequate resources for remedia-
psychotherapy competencies. Once the initial mis- tion? Will programs unable to demonstrate compe-
sion of developing sample core competencies for the tence fail accreditation and close?
field was completed in 2000, the Task Force began to After wrestling with these questions, AADPRT
address psychotherapy competencies. AADPRT and and the Task Force leadership decided to develop
Task Force leaders raised several questions. Who workgroups to write competencies for each of the re-
should develop psychotherapy competencies-indi- quired psychotherapies. Most of the workgroup
vidual programs, a national organization, or a coali- members were to be training directors with specific
tion? Should the competencies be a “gold standard” interests and expertise in psychotherapy education.
endorsed by national organizations such as AADPRT, Psychotherapy experts and residents were also to
or samples to guide training directors? How reliable participate. The APA Task Force on Competency, with
and valid are the current assessment methods that are representatives from major psychiatric organizations
used, including supervisor reports from process involved in education and accreditation, offered sup-
notes, audio and videotapes, and direct observation? port and recommended consultation from COPP for
Could new assessment methods be developed? If so, psychotherapy expertise. One expert from COPP was
who might fund their development? invited into each workgroup and asked to write an
Since AADPRT is an organization of training di- initial set of competencies for the assigned modality.
rectors with substantial expertise in residency train- The psychodynamic psychotherapy workgroup al-
ing and recognizes that differences exist among pro- ready had three psychoanalyst members to help write
grams in size, location, resources and emphasis, the the initial draft. Authors were instructed to write one
Task Force chose to develop sample competencies for section each on knowledge, skills and attitudes, and
the field. These were intended to serve as guides to reminded to be cognizant that residents are not ex-
program directors and could be revised by each pro- perts. Task Force leaders determined that assessment
gram to meet its specific needs. methods would be addressed at another time.
Further questions emerged. What is the defini- The completed first drafts of psychotherapy com-
tion of competency? Should the threshold for com- petencies were then sent by e-mail to each workgroup
petency be set at low levels which most residents member for comments and revision. Task Force co-
could readily meet? Should the threshold be set chairs incorporated the revisions and provided fur-
higher so that competency has increased specificity ther editing to insure uniformity of language and
and is more meaningful? Can differences in compe- comprehensiveness. Next, each workgroup member
tency be specified for PGY 2’s, 3’s and 4’s? How does was sent copies of all five revised sets of competencies
the “competency” of a residency graduate compare by e-mail, and asked for further comments. Addi-
with that of experienced clinicians who have prac- tional revisions were made. Final meetings of all
ticed for 10 years? How comprehensive should the workgroups were planned for the AADPRT 2001
competencies be? For example, should residents be meeting in Seattle where final changes were to be
Academic Psychiatry, 27:3, Fall 2003 151
DEVELOPMENT AND IMPLEMENTATION
made. The Seattle earthquake prevented some mem- training directors and their faculties. First, all clinical
bers from attending, but those not present faxed in and academic components of the program must be
their comments. The members in attendance met for specified in writing, in terms of knowledge, skills and
lengthy discussion and reached consensus about the attitudes for all general and psychotherapy compe-
scope of the competencies, thresholds to set, and de- tencies. Such descriptions become the official goals
grees of comprehensiveness for all five psychothera- and objectives of the residency curriculum, which
pies. need to be evaluated systematically, and whose out-
comes are to be demonstrated to the RRC at the time
SOCIOCULTURAL ISSUES of site visits. Educational mandates of programs are
often determined by departmental chairs in conjunc-
Sociocultural issues are imbedded in all therapeutic tion with their training directors and education com-
relationships, and certainly in psychotherapies. mittees. How will departments find the resources to
Though quite important, they are easily ignored or fulfill these new requirements? Teaching time in the
mishandled through personal bias, countertransfer- curriculum is already thinly divided between a myr-
ence and ignorance. To explore understanding of the iad of required, important and competing topics.
sociocultural issues related to the core and psycho- Now programs face a triple threat: They must re-de-
therapy competencies, the Center for Mental Health fine what they are already doing in terms of the com-
Services and APA held an invitational conference on petencies; add specific, systematic training in the five
Cultural Competence in June of 2001. AADPRT lead- psychotherapies; and devise reliable and valid as-
ers participated in the conference, which shed further sessment measures for all activities. These are time-
light on how sociocultural issues impact patients and consuming activities to be imposed on faculty who
therapists engaged in psychotherapy. The goals of are already stretched to their limits. In addition to
psychotherapy, establishing a therapeutic alliance, specifying and evaluating these competencies, train-
and decisions regarding whom the therapist involves ing directors and faculty are now mandated to pro-
in the treatment are all impacted by sociocultural is- vide and document remediation of deficits where
sues. Content themes that emerge in therapy, and outcome measures indicate deficiencies in compe-
transferences and countertransferences, particularly tency. Such remediation will require additional re-
those concerning authority, deference, assertiveness, sources from faculty.
and gender are also affected by sociocultural factors. Accountability creates liability for all parties in-
Furthermore, balancing the importance of family vs. volved: programs, faculty, training directors and their
individual values is also influenced by sociocultural departments. The new RRC Essentials require train-
issues in patients and therapists. In response to at- ing directors to write summary documents for all
tending this conference, Task Force co-chairs further graduates indicating that they have met the program
revised the sample competencies to include sociocul- requirements, are ethically and professionally sound,
tural issues before sending final drafts of the sample and are competent to practice independently. What if
competencies to the AADPRT Executive Council for a resident is found to be incompetent in psychother-
approval. The sample competencies were approved apy, and remediation attempts fail? Must such a res-
and distributed to all AADPRT members in Decem- ident fail the program? What happens to the brilliant
ber 2001. (See sample competencies at end of this ar- resident researcher who never intends to practice
ticle.) psychotherapy and who never attains competence in
psychotherapy? If a residency graduates a resident
PROBLEMS FOR TRAINING PROGRAMS and certifies competence in psychotherapy and the
resident is subsequently sued for incompetence by a
The announcement of the new RRC Essentials for patient, to what extent might the residency and train-
psychotherapy competencies generated significant ing director be held liable?
anxiety among training directors, who quickly Where will resources such as salary or faculty
grasped the difficulties that would arise in meeting come from if a resident needs remediation? Should
these challenges. Implementing both general and residents requiring remediation be expected to pay
psychotherapy competencies places new demands on for these resources themselves?
152 Academic Psychiatry, 27:3, Fall 2003
MELLMAN AND BERESIN
THE FUTURE strated sound psychometric properties (Mullen, un-
published). The Cognitive Behavioral Therapy Su-
Although the initial task of writing psychotherapies pervision Checklist by Wright, Sudak, Beck and
was complex, more difficult tasks lie ahead. Training Bienenfield will also be available shortly (Wright, un-
directors have just begun to implement the language published). Developing novel valid and reliable as-
of competency in their teaching and supervisory sessment methods is costly and time-consuming but
goals and to revise their evaluation methods and additional methods are needed.
forms to reflect the new competencies. Old methods Meanwhile, some training programs have al-
of assessment including direct observation, process ready benefited from the focus on outcome. Training
notes, audiotaped and videotaped interviews, and directors have new leverage to require resources from
chart reviews are still the major methods used, and their departments. Since many chairs and faculty
updated versions of these methods are emerging. Re- members are not aware of the magnitude of the new
mediation for deficient performance is now required. RRC requirements, training directors need to educate
A few new methods of psychotherapy assessment them about the new requirements and work to de-
have developed. Mullen, Rieder and Glick developed velop resources for training and evaluation. The in-
the multiple-choice Columbia Psychotherapy Test for tended goal of educational improvement is one we
psychodynamic psychotherapy and have demon- can all share.
References
1. www.acgme.org/RRC/Psy_Req.asp 9. Beitman B. A time-efficient, research based, outcomes-
2. ACGME: ACGME: outcome project. ACGME General Com- measured psychotherapy training program. Academic Psy-
petencies Version 1.3, 2000. 9.28.99 chiatry
3. Leach DC. The ACGME competencies: substance or form? J 10. Goldberg DA. Structuring training goals for psychodynamic
Am Coll Surg 2001; 192(3):396–398 training. J Psychotherapy Prac Res 1998; 7:10–22
4. Cohen JJ. Leadership for medicine’s promising future. Aca- 11. Wright JH, Beck AT. Cognitive therapy, in Textbook of Psy-
demic Medicine 1998; 73(2):132–137 chiatry. Third Edition. Edited by Hales RE, Yudofsky SC and
5. Lieberman JA, Rush AJ. Redefining the role of psychiatry in Talbott JA. Washington, D.C. American Psychiatric Press,
medicine. Am J Psychiatry 1996; 153(11):1388–1397 1999, pp 1205–1241
6. Tasman A. Presidential Address: The doctor-patient relation- 12. Goin MK, Kline FM. Supervision observed. J Nerv Ment Dis
ship. Am J Psychiatry 2000; 157(11):1763–1768 1974; 158(3): 208–213
7. Wallerstein RS. THE FUTURE of psychotherapy. Bull Men- 13. Committee on Cultural Psychiatry, Group for the Advance-
ninger Clin 1991; 55(4): 421–443 ment of Psychiatry. Cultural Formulation: Description and
8. Lazar SG, Gabbard GO. The cost effectiveness of psycho- Clinical Use in Cultural Assessment in Clinical Psychiatry.
therapy. J Psychother Pract Res 1997; 6(4):307–314 Washington, D.C., American Psychiatric Publishing, Inc., 2002
Academic Psychiatry, 27:3, Fall 2003 153
You might also like
- Dual Disorders: Counseling Clients with Chemical Dependency and Mental IllnessFrom EverandDual Disorders: Counseling Clients with Chemical Dependency and Mental IllnessNo ratings yet
- The Great Psychotherapy Debate PDFDocument223 pagesThe Great Psychotherapy Debate PDFCasey Lewis100% (10)
- Crown LengtheningDocument54 pagesCrown Lengtheningkevin1678100% (1)
- Introduction To PsychoeducationDocument9 pagesIntroduction To PsychoeducationAneeh100% (1)
- The Psychoeducation Model. Definition, Contemporary Roots and Content - Authier (1977)Document8 pagesThe Psychoeducation Model. Definition, Contemporary Roots and Content - Authier (1977)Eduardo Aguirre DávilaNo ratings yet
- Teaching Supportive Psychotherapy 2012Document9 pagesTeaching Supportive Psychotherapy 2012Elizabeth Paola CabreraNo ratings yet
- Curriculum de Psicoterapia para Estudiantes de MedicinaDocument5 pagesCurriculum de Psicoterapia para Estudiantes de MedicinapsychforallNo ratings yet
- Professional Issues in Clinical PsychologyDocument5 pagesProfessional Issues in Clinical PsychologyJohn Moone100% (2)
- Cognitive Behavorial Therapy PDFDocument6 pagesCognitive Behavorial Therapy PDFViannys PaterninaNo ratings yet
- Making Therapy Widely Available: Clinical Research Triumph or Existential Catastrophe?Document4 pagesMaking Therapy Widely Available: Clinical Research Triumph or Existential Catastrophe?benediktNo ratings yet
- Lay Mental Health CounselingDocument6 pagesLay Mental Health CounselingpangaribuansantaNo ratings yet
- Transference Focused Psychotherapy Training During Residency An Aide To Learning Psychodynamic PsychotherapyDocument22 pagesTransference Focused Psychotherapy Training During Residency An Aide To Learning Psychodynamic PsychotherapyLíaNo ratings yet
- Current Issues in Clinical Psychology Group 3Document20 pagesCurrent Issues in Clinical Psychology Group 3ngbwxm9zf2No ratings yet
- They Should Summarize From TIMOTHY J's Clinical Psychology BookDocument15 pagesThey Should Summarize From TIMOTHY J's Clinical Psychology BookScribdTranslationsNo ratings yet
- Lesson 1 Clinical PsychologyDocument7 pagesLesson 1 Clinical PsychologyTin EupenaNo ratings yet
- PsychoeducationDocument9 pagesPsychoeducationSrinivas Pandeshwar100% (1)
- The Therapist A Neglected Variable in Psychotherapy ResearchDocument4 pagesThe Therapist A Neglected Variable in Psychotherapy ResearchPaulo GomesNo ratings yet
- Clinical Psychology Assginment No 2Document3 pagesClinical Psychology Assginment No 2Hamza BukhariNo ratings yet
- Leichsenring 06Document29 pagesLeichsenring 06ФффФффNo ratings yet
- Practice Guidelines For Psychiatric Consultation in The General Medical SettingDocument23 pagesPractice Guidelines For Psychiatric Consultation in The General Medical Settingpsychforall100% (1)
- Y ModelDocument8 pagesY ModelÁngela AgudeloNo ratings yet
- Entrenamiento en Medicina para Residentes de PsiquiatríaDocument3 pagesEntrenamiento en Medicina para Residentes de PsiquiatríapsychforallNo ratings yet
- Topic 5Document16 pagesTopic 5Insta viralNo ratings yet
- Documentary of ExplanationDocument17 pagesDocumentary of ExplanationMuhammad Hamza AshfaqNo ratings yet
- Psychotherapy of SchizophreniaDocument6 pagesPsychotherapy of SchizophreniaFaizaminNo ratings yet
- Brief Therapy in College Counseling and Mental Health - EBSCOhostDocument8 pagesBrief Therapy in College Counseling and Mental Health - EBSCOhostjanettst2No ratings yet
- Unit 1 ClinicalDocument11 pagesUnit 1 Clinicalashlinanand2021psyNo ratings yet
- Fields of PsychologyDocument14 pagesFields of Psychologyhumna naeemNo ratings yet
- Cognitive Behavioral Therapy For Psychotic SymptomsDocument149 pagesCognitive Behavioral Therapy For Psychotic SymptomsCrina SerbanNo ratings yet
- PsychotherapyDocument4 pagesPsychotherapyFaustrock Dionyso MingonkNo ratings yet
- CIIS 2017 Certificate in Psychedelic Therapy and ResearchDocument22 pagesCIIS 2017 Certificate in Psychedelic Therapy and Researchcristie StrongmanNo ratings yet
- Positive Affect Treatment For Depression and Anxiety Therapist Guide Michelle G Craske All ChapterDocument67 pagesPositive Affect Treatment For Depression and Anxiety Therapist Guide Michelle G Craske All Chapterkaren.dixon505100% (10)
- A Systematic Scoping Review of Psychological Therapies For Psychosis Within Acute Psychiatric In-Patient Settings.Document8 pagesA Systematic Scoping Review of Psychological Therapies For Psychosis Within Acute Psychiatric In-Patient Settings.Eric KatškovskiNo ratings yet
- Nature, Scope, Role, History and Current Status of Clinical Psychology and AssessmentsDocument15 pagesNature, Scope, Role, History and Current Status of Clinical Psychology and Assessmentsabisha.angeline22No ratings yet
- FINAL Overview - Evidence - Base - BriefingDocument11 pagesFINAL Overview - Evidence - Base - BriefingManuela MesquitaNo ratings yet
- Riess Et Al (2012)Document7 pagesRiess Et Al (2012)Alicia BrevaNo ratings yet
- Lesson 2 The Skills Activities of A Clinical PsychologistDocument6 pagesLesson 2 The Skills Activities of A Clinical PsychologistReg RoseteNo ratings yet
- (Treatments That Work) Kelly J Rohan - Coping With The Seasons - A Cognitive Behavioral Approach To Seasonal Affective Disorder, Therapist Guide-Oxford University Press, USA (2008)Document152 pages(Treatments That Work) Kelly J Rohan - Coping With The Seasons - A Cognitive Behavioral Approach To Seasonal Affective Disorder, Therapist Guide-Oxford University Press, USA (2008)Jack MertensNo ratings yet
- Evidence based-WPS OfficeDocument6 pagesEvidence based-WPS OfficeSalima HabeebNo ratings yet
- Murphy Et Al (2018) A-systematic-review-and-meta-AcceptedDocument30 pagesMurphy Et Al (2018) A-systematic-review-and-meta-AcceptedMichelle KellyNo ratings yet
- Overview of Practice of Consultation Liaison.4Document10 pagesOverview of Practice of Consultation Liaison.4Sweet Memories JayaVaniNo ratings yet
- Therapeutic Stance Towards Persons With PsychosisDocument18 pagesTherapeutic Stance Towards Persons With PsychosisPetar DimkovNo ratings yet
- Person-Based Contextual Therapy Applied To A Complex Case of SchizophreniaDocument9 pagesPerson-Based Contextual Therapy Applied To A Complex Case of Schizophreniavince232No ratings yet
- Assignment On Psychotherapy: Submitted by Maj Mercy Jacob 1 Yr MSC Trainee Officer Con CH (Ec) KolkataDocument27 pagesAssignment On Psychotherapy: Submitted by Maj Mercy Jacob 1 Yr MSC Trainee Officer Con CH (Ec) KolkataMercy Jacob100% (2)
- Instant Download Ebook PDF A Systematic and Integrative Model For Mental Health Assessment and Treatment Planning PDF ScribdDocument48 pagesInstant Download Ebook PDF A Systematic and Integrative Model For Mental Health Assessment and Treatment Planning PDF Scribdandrew.lints179100% (53)
- Lesson 2 The Skills Activities of A Clinical PsychologistDocument6 pagesLesson 2 The Skills Activities of A Clinical Psychologistjericho anchetaNo ratings yet
- Teaching FCC To Psych - FullDocument9 pagesTeaching FCC To Psych - FullStgo NdNo ratings yet
- Chochinov - Dignity Therapy - A Feasibility Study of EldersDocument13 pagesChochinov - Dignity Therapy - A Feasibility Study of Eldersjuarezcastellar268No ratings yet
- Psychoeducation in Psychiatric DisorderDocument23 pagesPsychoeducation in Psychiatric Disorderishita aggarwal100% (1)
- Internship ReportDocument80 pagesInternship ReportSafa AliNo ratings yet
- History of Psychotherapy Continuity and Change (2nd Ed.) .Document7 pagesHistory of Psychotherapy Continuity and Change (2nd Ed.) .psicandreia100% (1)
- ClinicalDocument19 pagesClinicalVukashin.meNo ratings yet
- Good Enough Psychiatric Residency Training In.6Document11 pagesGood Enough Psychiatric Residency Training In.6Anonymous Fqa80pKNo ratings yet
- The Efficacy of Psychodynamic PsychotherapyDocument12 pagesThe Efficacy of Psychodynamic Psychotherapyadam sturmNo ratings yet
- Research in Supportive Psychotherapy 1994Document9 pagesResearch in Supportive Psychotherapy 1994Elizabeth Paola CabreraNo ratings yet
- From Skepticism to Competence: How American Psychiatrists Learn PsychotherapyFrom EverandFrom Skepticism to Competence: How American Psychiatrists Learn PsychotherapyNo ratings yet
- Psychiatric Mental Health Nursing Made Easy: Beginner's Guide to Mental Health NursingFrom EverandPsychiatric Mental Health Nursing Made Easy: Beginner's Guide to Mental Health NursingNo ratings yet
- High Risk Pregnancy NewDocument16 pagesHigh Risk Pregnancy NewSurya SasidharanNo ratings yet
- EDocument75 pagesEAneleNo ratings yet
- U-4 Pharmacology-L AS5Document16 pagesU-4 Pharmacology-L AS5kahega5291No ratings yet
- Patricia Benner FinalDocument54 pagesPatricia Benner FinalNarena Bonite100% (1)
- Orphan Drug Act: History, Perspective and Challenges For FutureDocument12 pagesOrphan Drug Act: History, Perspective and Challenges For FutureYuniar ASPNo ratings yet
- 182 604 1 PBDocument10 pages182 604 1 PBAngel Nikiyuluw100% (1)
- Beyond Borders Siloam Hospitals GroupDocument11 pagesBeyond Borders Siloam Hospitals GroupRizal FahmyNo ratings yet
- Sample Agenda For ACLS Traditional Course - Ucm - 506682Document2 pagesSample Agenda For ACLS Traditional Course - Ucm - 506682du.sto.fa.ppea.r.an.ce678No ratings yet
- OBV Survey Report - 2024Document52 pagesOBV Survey Report - 2024fridakaraniNo ratings yet
- Get Application Hall PDFDocument1 pageGet Application Hall PDFKaran JaiswalNo ratings yet
- GWU MBA BrochureDocument4 pagesGWU MBA BrochureKobby KatalistNo ratings yet
- Condom Use and Associated Factors Among Hiv PDFDocument114 pagesCondom Use and Associated Factors Among Hiv PDFBuleloNo ratings yet
- PR 3Document23 pagesPR 3Jaylanie MabagaNo ratings yet
- IRR RA 10354 RH LawDocument81 pagesIRR RA 10354 RH LawCBCP for LifeNo ratings yet
- About MADocument14 pagesAbout MADd DdNo ratings yet
- Case Slip Minor CaseDocument1 pageCase Slip Minor CaseRhea May CaporNo ratings yet
- History of Psychiatry in IndiaDocument6 pagesHistory of Psychiatry in IndiaMarbe HmtNo ratings yet
- MIS of A Hospital: Assignment-IDocument16 pagesMIS of A Hospital: Assignment-IjashanNo ratings yet
- Theranos WhistleblowersDocument2 pagesTheranos WhistleblowersAnnabella LacunaNo ratings yet
- Shanghai Ninth People's Hospital, OverviewDocument3 pagesShanghai Ninth People's Hospital, OverviewGhulam Mohey-ud-din0% (1)
- PT BooksDocument2 pagesPT BooksNelle Sardido0% (1)
- Gambaran Tingkat Kebutuhan Perawatan Ortodonti Di SMPN 2 Takisung BerdasarkanDocument6 pagesGambaran Tingkat Kebutuhan Perawatan Ortodonti Di SMPN 2 Takisung BerdasarkanFerdyelvNo ratings yet
- Thai Breastfeeding AtlasDocument270 pagesThai Breastfeeding Atlasdr. Fadhilah Az ZahroNo ratings yet
- TraditionalMedicine DelMundoGandol-2Document27 pagesTraditionalMedicine DelMundoGandol-2Larah GandolNo ratings yet
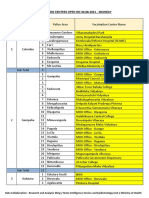
- Vaccination Centers On 30.08.2021Document11 pagesVaccination Centers On 30.08.2021Chanu On CTNo ratings yet
- Maklumat Vaksinasi: Vaccination DetailsDocument2 pagesMaklumat Vaksinasi: Vaccination DetailsDerek ReggieNo ratings yet
- Bioavailabilitas & BioekivalensiDocument19 pagesBioavailabilitas & BioekivalensiCandriya LaelNo ratings yet
- NOTES Hypertensive Cardiovascular DiseaseDocument6 pagesNOTES Hypertensive Cardiovascular DiseaseLunaNo ratings yet
- Indices For Periodontal DestructionDocument4 pagesIndices For Periodontal DestructionDinky Jain100% (1)