Professional Documents
Culture Documents
mgNGS_clinmicrob_watts2020
mgNGS_clinmicrob_watts2020
Uploaded by
Krisztián TóthCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Practice Toeic Reading Test 2021 03 - Tests + AnswerDocument19 pagesPractice Toeic Reading Test 2021 03 - Tests + AnswerAVRILLIA CLEMENTINENo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Unit Operation in Food Processing Chapter 6 ProblemsDocument12 pagesUnit Operation in Food Processing Chapter 6 ProblemsTeh Sze Yin100% (3)
- Gross National Income Per Capita 2019, Atlas Method and PPPDocument4 pagesGross National Income Per Capita 2019, Atlas Method and PPPElisha WankogereNo ratings yet
- InterSchool Activity ScriptDocument7 pagesInterSchool Activity ScriptJessica Loren Leyco87% (15)
- Swarm WhitepaperDocument46 pagesSwarm WhitepaperJoel Dietz100% (1)
- Instagram Creators Handbook - IGTV PDFDocument48 pagesInstagram Creators Handbook - IGTV PDFAndrei Neațu100% (1)
- NGS_biothreat_applicationsDocument10 pagesNGS_biothreat_applicationsKrisztián TóthNo ratings yet
- 2017 - Ruud H. Deurenberga, - Journal of BiotechnologyDocument9 pages2017 - Ruud H. Deurenberga, - Journal of BiotechnologyNeha PalNo ratings yet
- NGSplatforms_metagenomic_blood_pathogensDocument14 pagesNGSplatforms_metagenomic_blood_pathogensKrisztián TóthNo ratings yet
- NGS_in_clinmicrob_genes-13-01566Document24 pagesNGS_in_clinmicrob_genes-13-01566Krisztián TóthNo ratings yet
- WHO Influenza PrimersDocument1 pageWHO Influenza PrimersKrisztián TóthNo ratings yet
- 1-s2.0-S0197458019301083-mainDocument12 pages1-s2.0-S0197458019301083-mainKrisztián TóthNo ratings yet
- Cytokines: Names and Numbers You Should Care About: Stephen R. Holdsworth and Poh-Yi GanDocument12 pagesCytokines: Names and Numbers You Should Care About: Stephen R. Holdsworth and Poh-Yi GanKrisztián TóthNo ratings yet
- Opal2000 PDFDocument11 pagesOpal2000 PDFKrisztián TóthNo ratings yet
- Bulletin: Medical University of InnsbruckDocument5 pagesBulletin: Medical University of InnsbruckKrisztián TóthNo ratings yet
- Sikafloor®-169: Product Data SheetDocument4 pagesSikafloor®-169: Product Data SheetMohammed AwfNo ratings yet
- Taxation: Bmbes 2020 Barangay Micro Business Enterprise BMBE Law's ObjectiveDocument3 pagesTaxation: Bmbes 2020 Barangay Micro Business Enterprise BMBE Law's Objectivekris mNo ratings yet
- 05 - Quiz - 1 - HRMDocument3 pages05 - Quiz - 1 - HRMMillania ThanaNo ratings yet
- Question BankDocument9 pagesQuestion Bankshama JNo ratings yet
- Quectel M12 at Commands Manual V3 2Document195 pagesQuectel M12 at Commands Manual V3 2kalpeshbrNo ratings yet
- Pwwha: Delhi 10RDocument44 pagesPwwha: Delhi 10Rserrano.flia.coNo ratings yet
- DMTR DataDocument3 pagesDMTR DataŽiga PosediNo ratings yet
- 21cs644 Module 3Document95 pages21cs644 Module 3gmaheshreddy229No ratings yet
- Garden Growers Nursery Technician: Job DescriptionDocument2 pagesGarden Growers Nursery Technician: Job DescriptionKevin PittNo ratings yet
- 21810, Ultrapure Water Breakpoint CL andDocument5 pages21810, Ultrapure Water Breakpoint CL andWaleed EmaraNo ratings yet
- CE409 Quantity Surveying and ValuationDocument2 pagesCE409 Quantity Surveying and ValuationBala GopalNo ratings yet
- RCC Teen - Task 5 - BandwidthDocument2 pagesRCC Teen - Task 5 - BandwidthRares AndreiNo ratings yet
- Auction News Journal 3.1.14Document15 pagesAuction News Journal 3.1.14Etrans 1No ratings yet
- Production Line Resume SampleDocument2 pagesProduction Line Resume SampleadityadhimanNo ratings yet
- WALL STREET JOURNAL. CLASSROOM EDITION Chapter 14Document2 pagesWALL STREET JOURNAL. CLASSROOM EDITION Chapter 14Toby trittschlerNo ratings yet
- PMIT Admission Brochure - Spring 2021Document3 pagesPMIT Admission Brochure - Spring 2021Shayekh Mohiuddin Ahmed NavidNo ratings yet
- EN 12663-1 - 2010 - IndiceDocument6 pagesEN 12663-1 - 2010 - IndiceOhriol Pons Ribas67% (3)
- Chap 7Document38 pagesChap 7احمد نصارNo ratings yet
- PFMAT Budgeting - Framework - BOM - 2016 For PresentattionDocument33 pagesPFMAT Budgeting - Framework - BOM - 2016 For PresentattionJ Andrea Jaca100% (1)
- Nguyen Dai Duo NGDocument7 pagesNguyen Dai Duo NGtuan leNo ratings yet
- FOURNIER RF-5B - Sperber Flight Manual (English)Document29 pagesFOURNIER RF-5B - Sperber Flight Manual (English)Rene QueirozNo ratings yet
- EIC5000 Electronic Indicator Control Installation and Operation InstructionsDocument8 pagesEIC5000 Electronic Indicator Control Installation and Operation InstructionsАртемNo ratings yet
- Introduction To GNU Radio and Software RadioDocument4 pagesIntroduction To GNU Radio and Software RadioDinesh VermaNo ratings yet
- BEKIER Et Al v. COMMONWEALTH CONSTRUCTION COMPANY, INC. Et Al - Document No. 8Document12 pagesBEKIER Et Al v. COMMONWEALTH CONSTRUCTION COMPANY, INC. Et Al - Document No. 8Justia.com100% (1)
mgNGS_clinmicrob_watts2020
mgNGS_clinmicrob_watts2020
Uploaded by
Krisztián TóthCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
mgNGS_clinmicrob_watts2020
mgNGS_clinmicrob_watts2020
Uploaded by
Krisztián TóthCopyright:
Available Formats
Clinical CMN
Microbiology
Stay Current...
Stay Informed.
N e w s l e t t e r
Vol. 42, No. 7
April 1, 2020 Metagenomic Next-Generation Sequencing in
www.cmnewsletter.com
Clinical Microbiology
I n Th is Issu e George S. Watts, Ph.D. and Bonnie L. Hurwitz, Ph.D., University of Arizona, Tucson Arizona
53 Metagenomic
Abstract
Next-Generation Identification of causative pathogens in infectious disease is a critical component of health care, as
Sequencing in Clinical infectious diseases continue to be a leading cause of mortality and morbidity worldwide. In addition,
Microbiology the detection of drug resistance by traditional and novel antimicrobial susceptibility testing methods
is becoming ever more important as antimicrobial resistance continues to emerge and spread. While
culture-based methods are the current reference standard for identifying microbes, the time required to
achieve results and the difficulty in culturing certain fastidious organisms have led to the development
of multiple alternatives. Alternatives to culture, such as polymerase chain reaction (PCR) assays, sero-
logic assays, matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF
MS), and 16S rRNA gene sequencing have been used in clinical laboratories, and positive impacts on
patient care have been documented. Nonetheless, such methods require either presumption about the
type of microbes present in the sample or growth of the organism(s) before analysis. Subsequently, there
are some documented limitations in the routine detection methods for clinically relevant organisms.
In contrast to the routine alternatives listed above, modern nucleic acid sequencing platforms sup-
port sequencing of random DNA strands, an approach known as “shotgun” sequencing of the DNA,
also known as metagenomic next-generation sequencing (mNGS) present in the sample. The mNGS
approach offers an unbiased and hypothesis-free approach to pathogen identification with the future
potential to (i) achieve results in 12 to 24 hours; (ii) avoid the challenges associated with growth of
fastidious organisms; (iii) avoid the biased growth that occurs when only routine culture medium is
used; (iv) detect viral, fungal, and parasitic organisms in the same assay; and (v) detect the presence
of drug resistance genes. Advances in mNGS technology and data analysis have reduced testing costs
to the point where the potential advantages of mNGS over culture and other methods warrant its
development for use in clinical settings. In this review, the mNGS approach is discussed, along with a
comparison to other methods, limitations, and suggestions for further development and overcoming
hurdles to adoption in the clinical setting.
Background culture methods and a variety of alternative
methods, the causative agent in many infections
Identification of pathogens associated with infec-
Corresponding author: often remains unknown. Routine culture can
tious diseases can provide valuable diagnostic
George S. Watts, Department have a high false-negative rate in certain disease
of Pharmacology, University of information, which in turn can guide treatment.
Prompt and appropriate antimicrobial therapy states. The problem was highlighted in a study
Arizona Cancer Center, Room
3927, 3838 N Campbell Ave., is of great importance, particularly when the of 3,756 neutropenic patients that found only
Tucson, AZ 85719. Tel.: patient is immunocompromised, whether due to 609 of all blood cultures collected (~20%) were
520-626-4724. E-mail: age, disease (e.g., infection with human immu- culture positive [1]. As one would expect, the risk
gwatts@email.arizona.edu nodeficiency virus or diabetes), or medication of death associated with bloodstream infections
0196-4399/©2020 Elsevier Inc. (e.g., chemotherapy or treatments for rheumatoid varied by the patient’s immune status and the
All rights reserved arthritis). Despite the widespread use of routine causative microorganism. Of note, the hazard
Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier 53
ratio of dying was nearly four-fold higher in culture-negative with emphasis on the technology and applications [9], regulatory
patients than in patients for whom no blood culture was collected and interpretation issues [10], and hurdles to implementation [11].
and submitted, presumably due to lack of symptoms suggestive of
bacteremia or sepsis [1]. Since blood cultures are only capable of
The mNGS Approach
detecting cultivatable bacteria and fungi, it is not surprising that Most commonly, mNGS analysis directly from clinical samples
other sources of infection can be overlooked using current blood involves isolating DNA; determining its sequence; and then ana-
culture-based technology. lyzing that sequence in the context of a reference database to deter-
mine which organisms are present, and their potential phenotypes,
based on their genetic content (Fig. 1). Of note, if only DNA is
Lacking knowledge of the identity and antimicrobial suscepti-
extracted, then many viral pathogens will not be detectable.
bility of the causative pathogen, clinicians use broad-spectrum
antibiotics as the first line of therapy, whether using blood cul- Immediately, several questions come to mind related to nucleic
tures or mNGS. Unfortunately, empiric therapy does not always acids, testing, and sequence reads (a sequence read is the string
adequately treat the causative pathogen. Perhaps most notably of nucleotides identified from a fragment of the genomes pres-
for immunocompromised patients, the higher incidence of fun- ent in the sample). The following are examples of such questions.
gal and viral infection exacerbates the mismatch between therapy How should the DNA be isolated? How many sequence reads
and pathogen because the infection may be initially assumed to are needed? How should the sequence reads be analyzed? What
be bacterial in origin. are the assay’s limits of detection? What is the false-positive rate?
Consideration of the goals of the analysis and the sample type
being analyzed allows some initial answers and becomes a starting
Transitioning from culture to mNGS may improve the frequency
point for mNGS design and analysis. For example, the genome
and speed with which pathogens are identified in patients with sus-
sizes in question ranges from a few thousand base pairs in the case
pected infections. By providing clinicians with evidence to inform
of viruses to a few million for bacteria to approximately 15 mil-
rational antimicrobial choices and guide treatment, mNGS could
lion base pairs for clinically relevant fungi (e.g., Candida albicans).
benefit patients and society through improved patient outcomes,
If we assume that 5 megabases is a reasonable genome size esti-
reduced health care costs, and better antimicrobial stewardship.
mate for bacteria and conservatively assume there will be 100-bp
As such, mNGS of pathogens from whole blood and other sample
read lengths, then 50,000 reads would provide 1× coverage of the
types have been referred to as the “holy grail” of infection diagno-
genome, meaning that on average each nucleotide in the genome
sis [2]. Not surprisingly, the development of mNGS is currently
will have been sequenced once. If we prefer 10× coverage of the
being explored for used in clinical applications, with successes in
genomes present in a sample that could contain 10 microbes, then
meningitis [3], culture-negative sepsis [4], febrile neutropenia [5],
the number of reads required becomes 5 million—easily achiev-
and nosocomial transmission of drug-resistant Klebsiella pneumoniae
able on several NGS platforms. Sequencing platform outputs have
[6]. Further development has included the use of rapid, portable
been reviewed by Deurenberg et al. [9].
sequencing technology [7]. In particular, the use of mNGS to
track a carbapenem-resistant Klebsiella sp. outbreak demonstrated To date, most mNGS studies have selected an approach in which
the epidemiological value of mNGS in tracking the sources of the sample is not enriched for microbes, resulting in the great
outbreaks [6]. Lastly, the first prospective study of mNGS was majority (often >99%) of the sequence reads being derived from
reported in meningitis, with positive results [3]. Adoption of the (human) host. With so much of the data generated being
mNGS not only can improve individual patient outcomes, but uninformative from the standpoint of identifying microbes, the
also enhances hospital and community antimicrobial stewardship approach is inefficient, increases costs, and reduces diagnostic pos-
to protect the potency of currently available antimicrobials [8]. sibilities [12], although it has been argued that some benefit can be
Several reviews were previously published on the topic of mNGS, gained from insights into the host response available in the host
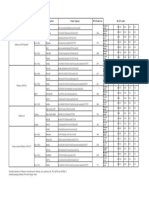
Figure 1. Schematic of mNGS workflow showing the three principal steps: (i) isolation of the DNA from the sample with or without enrichment for
microbial DNA, (ii) creation of a library and sequencing, and (iii) analysis of the sequence reads to determine the organisms present, their relative
abundances, and the presence of drug resistance genes.
54 Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier
sequence [11]. Simple sample preparation techniques are available As a first step, an mNGS dataset must be compared to genetic
to enrich samples for microbes; they include centrifugation, filtra- databases to detect host contamination and to determine the abun-
tion, and chemical treatment (e.g., propidium monoazide [PMA]) dance of known microbes. Recently, fast k-mer-based algorithms
of the sample to destroy cell-free DNA [13-15]. Consideration have been used to classify metagenomic reads against known bacte-
of the sample type, the expected number of microbes, and the rial genomes with remarkable throughput and speed. Specifically,
microbial abundance can help to guide sample preparation and the CLARK (classifier based on reduced k-mers) [16], USEARCH
the number of sequence reads required for the assay. [17], KRAKEN [18], and NBC (naive Bayes classifier) [19] clas-
sifiers offer composition-based approaches to quickly identify
For example, a whole-blood sample from a suspected case of a
microbial species present in a metagenome. In each case, the
bloodstream infection would be expected to contain several sources
sequence reads are broken down into shorter fragments (typically
of DNA. There is significant host DNA in human white cells, as
15 to 30 bp in length), and the frequency profiles of k-mers from
well as cell-free circulating human DNA; in addition, there could
microbial genomes are analyzed to rapidly assign the read from
be microbial DNA inside white cells (due to phagocytosis), as well
which the k-mers were derived to genomes in a reference database
as free circulating microbes. Plasma and serum samples represent
[16,18,20,21]. Although these methods are exceptionally fast and
similar challenges, but to a lesser extent. In this circumstance,
outperform alignment-based methods, building and using the fre-
centrifugation and filtration could be used to remove human cells,
quency profile for the reference database requires large amounts of
along with PMA treatment to destroy cell-free DNA. For patients
memory (>128 GB of RAM) [16]. Further, these methods are con-
with recent antibiotic therapy, PMA also has the potential benefit
strained by the representation of genomes and proteins in known
of destroying DNA from dead bacteria, which could cause false-
databases, making it difficult to illuminate “microbial dark matter.”
positive results due to nonviable microbes.
Microbial dark matter received its name because of the difficulty
The potential for the pathogen to be of fungal, viral, or parasitic in effectively studying it as a result of its inability to be cultured
origin may also affect how the sample DNA may be isolated, by current methods. Although the inability to culture the species
although protocols could be developed that cover all possibili- included in microbial dark matter makes it difficult to estimate its
ties. Establishing a validated sample preparation protocol that relative magnitude, the accepted gross estimate is that less than
can successfully isolate microbial DNA from diverse sample types 1% of all microbial species in a given ecological niche are cultur-
and microbes will be a significant step toward widespread mNGS able. In the clinical setting, the amount of microbial dark matter
adoption in clinical settings. is unknown but is likely to be far less due to the intense interest
in clinically relevant microbes over the past 100 years.
Once microbial DNA is isolated, sequencing libraries are prepared
using manufacturer-specific protocols. A collection of sequence- In addition to taxonomic identification, recently, approaches have
able DNA fragments of uniform size is created and fragments are been developed for rapid annotation of short reads against pro-
then sequenced. DNA library technology uses several techniques, tein reference databases that are orders of magnitude faster than
in this case a “library” is a collection of DNA fragments generated alignment-based (e.g. BLASTx) searches. Such options include
from the mNGS process. These libraries are tagged with a library- USEARCH, PAUDA, RAPSearch2, UProC, RAST, and DIA-
specific DNA sequence, referred to as a molecular “barcode,” a MOND [17,22-26]. These fast protein searches use either indexes
tag allowing multiple libraries to be pooled and sequenced simul- or suffix arrays for complete k-mer matching of a query to refer-
taneously. Following sequencing, the reads are separated by their ence databases or match unique protein domains to find protein
barcodes into pools of sample-specific data for analysis. Barcod- families [23,26]. In either case, these algorithms are often con-
ing libraries serves two purposes; they allow optimal use of the strained by system memory. For example, DIAMOND requires
output capacity of high-throughput sequencers and increases the ~1.6 TB (~100 GB) of memory for the NCBI-nr database [22], and
number of samples that can be analyzed in a single sequencing UProc requires 16 GB (~4GB) of memory for the Pfam database
run. Improved data analysis protocols and reference databases are [23]. Thus, although these algorithms move us one step closer to
needed to accommodate the diverse species that may be detected, comparisons of a complete set of reference proteins, they are not
their genome sizes, and the number of species in the metagenome. scalable and use computational resources that are not often acces-
sible to the clinical laboratory community. Further, these analyses
The Benefit of Using Bioinformatics Pipelines still neglect microbial dark matter and offer a limited perspective
Bioinformatics pipelines that streamline data analysis are in active of just the known cultivable microbes.
development, yet to date no clear methods for mNGS analysis
have emerged. Issues in analyses include removing contaminating False-Positive and -Negative Results
human host DNA reads without inadvertently removing micro- As with all techniques, mNGS for pathogen identification has to
bial sequences, identifying pathogens using incomplete genome deal with false-positive and false-negative results. Some of the
databases, detecting the abundance and prevalence of pathogens in sources of error could be overcome, while others are inherent to
polymicrobial clinical samples, and differentiating pathogens from sample collection. The first issue is contamination arising from
commensals that may affect treatment decisions. The development reagents, personnel, and the laboratory environment. Reagent con-
of rapid clinical diagnostics for rational therapy choices depends tamination with bacterial DNA is a well-known problem [27] that
on overcoming these bioinformatics challenges. is not surprising, since many molecular biology reagents used to
Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier 55
perform mNGS are isolated from microbes (e.g., polymerase and while suppressing stochastic false positives by providing a template
ligases), making bacterial DNA contamination likely. In response, for library preparation.
commercial products that have been treated to remove bacterial Work in this area suggests that when a sample is truly negative,
DNA have been developed, and such specialized reagents should false positives from contaminants and commensals arise, while
certainly be used in mNGS for clinical purposes. Other sources of true infection appears to suppress background [15]. In the future,
contamination can be reduced by creating dedicated workspaces providing a spiked positive control in the assay could provide the
and following procedures to reduce microbes and microbial DNA same suppression of background, but studies will need to deter-
in the laboratory environment. These procedures are not particu- mine how the positive control affects the limit of detection while
larly different than those that one would use to prevent contami- seeking a balance with background suppression.
nation of cell cultures or PCR methods; for example, molecular
laboratory practices and cleaning protocols, such as wiping down Standard of Care Techniques which Could be Supplemented
work surfaces with disinfectants, single-use gowns, hairnets and or Replaced by mNGS
face masks, pipette tips, and gloves are used along with molecular The competitive landscape for mNGS consists of both compet-
laboratory unidirectional workflow. ing technologies for identifying microbes by sequence analysis
Unfortunately, even with the aforementioned precautions, contam- and other traditional approaches to providing diagnostic infor-
mation. When laboratories consider the use of mNGS, careful
ination of samples will occur by the very nature of sample collec-
cost comparisons must be performed, as well as the impact to
tion. For example, any sample collected via a needle (e.g., blood or
workflow and productivity must be considered. Most importantly,
cerebrospinal fluid) will always pose the risk of contamination from
cost-benefit analysis is critical to assess which patient populations
skin commensal microbes, such as Cutibacterium acnes (formerly
or sample types would be most efficacious. For the sake of com-
Propionibacterium acnes), Staphylococcus epidermidis, and Corynebac-
parison, traditional technologies in use in clinical laboratories are
terium spp. Unfortunately, these organisms can cause infectious
described here.
disease, especially in immunocompromised individuals, and their
presence cannot be disregarded as a false positive. The problem Conventional or routine culture
of skin commensals will plague any technique, as it is inherent to The first methods developed to identify microorganisms involved
sample collection, but since it has always been a problem in the growth in culture to isolate a pure sample, followed by phenotypic
clinical setting, standard procedures have been established to deal analysis of features, such as microscopic morphology (e.g., cocci
with it, such as repeated assaying and careful cleaning of the skin versus rods and clusters versus chains); ability to grow on specific
before sample collection. One way in which mNGS may be able culture media; stains (e.g., Gram stain); and biochemical attributes,
to overcome these challenges is that mNGS can provide a quanti- such as the ability to alter particular substrates (e.g., hemolysis or
tative abundance of the organism(s) detected, much like a routine enzyme presence, such as beta-galactosidase positive). The pri-
culture uses relative abundance to differentiate normal flora from mary drawback of culture-based methods is that enrichment by
pathogens when some microbes can fall into both categories. It culture can be highly biased, since some organisms present in the
may prove possible to set thresholds for the number of reads of an sample do not grow in the enrichment media and some organisms
organism that would be required to consider reporting its pres- grow more rapidly and can potentially obscure the presence and/
ence and thus ignore the false positives that can arise from needle or the abundance of other organisms in the sample. In addition
punctures and other types of sample collection. to the bias inherent to culture, the method itself can take several
days, all while empiric antibiotic therapy is utilized until a specific
Lastly, there is the challenge of an assay’s limit of detection. In a
antimicrobial result can be attained. Finally, culture is not gener-
scenario in which infection may be suspected but uncertain, the
ally applicable to bacteria, fungi, viruses, and parasites using the
question becomes, how many sequence reads from an organism
same culture media and methods, and is similar to metagenomics
represent a true positive? The issue can be thought of in terms
in that regard. Thus, separate assays must be performed for each
of the DNA of the organism in competition with sources of con-
class of organism, typically sequentially, with further delays and
tamination. If no true infection is present, then contaminants can
costs for each one.
amplify during the preparation of the mNGS library, leading to
false positives, so even if a pathogenic organism is present, its Fluorescence microscopy
abundance may be too low, and contaminants may out-compete it A modern microscopy-based approach to microbial identification
in the PCR phase of the assay. As the abundance of the causative has been developed that utilizes a short culture period followed by
organism increases, at some point, its presence will be detected fluorescence-based tagging of microbes with antibodies and DNA
reliably—that point is called the assay’s limit of detection. The probes. The sample then flows across the microscope field, with
effect of sample type on the limit of detection needs to be inves- automated computer-based identification of microbial shape and
tigated in relation to the number of reads generated from the automated fluorescence detection. Problems with this type of mod-
sample for clinical implementation. Furthermore, a strategy in ern approach include reliance on culture to enrich the microbes,
which samples are spiked with a positive control may simultane- bias in detection due to the need to pick antibodies and probes
ously provide a benchmark for monitoring the limit of detection to utilize, and difficulties in identifying non-bacterial microbes.
56 Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier
Mass spectrometry regions, amplicons containing one or more divergent regions can
Matrix-assisted laser desorption ionization–time of flight mass be created and sequenced. By comparing the sequence to a ref-
spectrometry (MALDI-TOF MS) has been developed for the iden- erence database of known organisms and their 16S rRNA gene
tification of bacteria and fungi. In this approach, a pure culture is sequences, identifications can be made, often to the species level.
ionized, and the mass spectra of the resulting protein fragments The approach allows the identification of fastidious organisms and
are compared to a reference database to match patterns of known the analysis of samples containing many organisms, such as gut
organisms. Recent advances in the method allow cruder prepara- microbiomes. While it is powerful, drawbacks arise when species’
tions to be analyzed and even negate the need for culture. The sequences are not divergent enough to allow discrimination (e.g.,
method is rapid and low cost once the initial equipment has been Escherichia coli and Shigella spp.).
installed. Drawbacks to the method include difficulty in detecting
Serologic assays
drug resistance and virulence and in detecting viruses and parasites.
Lastly, complex mixtures of organisms present potentially unsolv- With the development of molecular biologic techniques in the last
able mass spectra making it best suited to scenarios in which only few decades, it has become possible to generate specific antibodies
a single organism is expected. to antigens present on the surfaces of microbes. These antibod-
ies can be utilized in various ways to detect the presence of and
Polymerase chain reaction even quantitate specific organisms or their products (e.g., toxins)
Polymerase chain reaction (PCR) allows sensitive and rapid detec- in a sample. Antibody-antigen complexes are detected in various
tion of specific nucleic acid sequences from even complex pools of ways, including precipitation reactions, agglutination reactions,
starting material. By targeting unique sequences in the genomes complement fixation, labeling the antibody with fluorescent mol-
or transcriptomes of organisms, the creation and detection of an ecules, and immobilizing either the antigen or antibody, followed
amplicon can be used to indicate the presence of the organisms in by various enzyme-linked immunosorbent assay approaches. A
a sample. Additional primers can be designed to indicate the pres- widely utilized example of antibody-based detection of a microbe
ence of drug resistance and virulence gene sequences. Variations is the rapid strep test, which allows a clinician to confirm bacterial
of PCR have been developed since its inception several decades pharyngitis caused by group A streptococci during a patient’s visit,
ago, with modern approaches including droplet-based PCR, high thus providing the information required to guide management of
levels of automation, miniaturization, and rapid cycling times. the infection by prescription of antibiotics. Unlike the approaches
Drawbacks to this approach include the limited range of organ- described above, antibody-based detection of specific microbes
isms that can reasonably be identified, inability to identify organ- can be performed within minutes without special equipment once
isms that are not present in the panel design, the specificity of the a specific organism is identified; however, clinical sensitivity and
reaction, and the assumption that target sequences will always be specificity may not be optimal.
unique to one organism.
Antimicrobial drug resistance
Microarray
Bacterial drug resistance is a serious worldwide human health
Microarrays are a miniaturized and multiplexed version of a tra- problem, and its detection in clinical samples can be more impor-
ditional membrane-based hybridization method, such as South- tant than the species-level identification possible from mNGS.
ern blotting, with the additional distinction that the probes are For example, detection of “methicillin-resistant Gram-positive
attached to the substrate while the targets are hybridized. Multiple cocci” by culture or mNGS is more relevant to a clinical decision-
DNA probes are fixed to a solid surface and hybridized to sample making and therapy than a result simply describing detection of
DNA fragments that are modified (typically with fluorescent tags “Staphylococcus aureus.” If mNGS that misses the presence of the
or a means to generate fluorescence following hybridization) to mecA gene conferring methicillin resistance, a significant gap to the
allow detection of probes with hybridized sample DNA. The high result relevance occurs. There are definite limits to the detection
number of probes that can be put on a single microarray provides of drug resistance by mNGS due to the diversity of drug resis-
the ability to detect and identify a broad range of organisms and tance mechanisms; multidrug resistance; and limitations arising
their drug resistance and virulence sequences in a single assay. from incomplete coverage, leading to insufficient sequence reads
Furthermore, microarrays can be utilized to analyze mixtures of to detect the presence of drug resistance genes. Currently, mNGS
organisms through careful choice of probes that distinguish one is considered too immature for inferring drug susceptibility clini-
organism from another. Drawbacks include the need to know the cally [28]. Nonetheless, there are numerous examples of success-
sequences of the organisms being queried to design appropriate ful identification of drug resistance in samples analyzed by mNGS
probes, difficulties in distinguishing organisms at the strain level, [3,29,30]. Consideration of the sample type and the number of
issues of specificity, and time required to perform the assay. organisms expected can assist in ensuring enough sequence reads
16S rRNA gene sequencing are generated to detect resistance genes.
The 16S rRNA gene sequencing approach takes advantage of the These considerations are demonstrated by work to identify the
alternating regions of high sequence conservation with interven- mecA sequence in three samples from two ventilator-acquired
ing regions of high sequence divergence found along the length pneumonia patients that were culture-positive for methicillin-
of the 16S rRNA gene. By designing PCR primers to conserved resistant S. aureus. Low coverage in two of the samples prevented
Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier 57
detection of the mecA gene, but the third had enough reads so that utility, as alluded to above (lowered mortality, morbidity, health
the entirety of the mecA gene was covered between 2× and 17×. In care costs, etc.). Demonstrating clinical validity can only be done
the sample in which mecA was detected, 619,389 sequence reads by comparison to culture or other alternatives in prospective
were classified as S. aureus from a total of 2.7 million. In contrast, studies. Aside from the difficulty of getting funding for testing
just 472 and 962 sequence reads were classified as S. aureus in the and the challenging issues with this type of study design, only
samples in which mecA was not detected [15]. Given the critical samples that are positive by the standard can be fully compared.
importance of drug resistance to the success of antibiotic therapy, The design ignores samples in which mNGS detects a pathogen
the interplay between the total number of reads obtained, the that was not identified by culture or whichever assay is used as the
number of reads classified to a pathogen, the number of reads clas- reference standard. This drawback could be overcome eventually
sified to the host genome, and the relative genome sizes involved by studies to demonstrate clinical utility. While we may never be
will need to be carefully explored for successful clinical transla- able to assess the validity of mNGS in culture-negative samples,
tion of mNGS. if treatment decisions are made based on the diagnostic informa-
tion provided and patient outcomes are better than with empiri-
While mNGS can detect the presence of DNA coding for drug
cal antimicrobial therapy, then the evidence to support the use of
resistance genes, there is no guarantee that a gene is active. While
mNGS clinically is obtainable. Of course, the adoption of mNGS
there is evidence that genotype accurately predicts phenotype, at
will be far less black and white than this. The recent publication of
least in S. aureus [29], there are scenarios in which this is not the
a prospective trial of mNGS in meningitis demonstrated various
case, such as S. aureus carrying the mecA gene but with a mutation
ways in which mNGS could be used as an adjunct or supplement
in the promoter that greatly alters the phenotype [31]. This sce-
to culture rather than outright replacement. A final consideration
nario led to suggestions that a more relevant material for mNGS
for the adoption of mNGS is the costs associated with establishing
is the RNA of the sample, which could provide information on
a capable laboratory and the personnel to perform it and interpret
what proteins the microbes are synthesizing and thus whether drug
the results. Given the complexities, the temptation would be to
resistance genes are active, along with a more accurate picture of
establish a few specialized laboratories to which samples could be
the active metabolic pathways. Such an approach would come at
sent for analysis. However, this approach would add at least 24
the cost of reducing discriminatory sequences or polymorphisms
hours to the turnaround time as the samples are mailed overnight
that could allow accurate discrimination between closely related
from their collection point to the laboratory. Instead, it seems
species or track specific strains in an outbreak in which just a few
more likely that as medical personnel become more familiar with
nucleotides per genome may be informative. Here again, consid-
the methods, standardized protocols become established, costs
eration of the setting and questions at hand could help guide the
come down, and evidence of clinical utility accumulates, mNGS
choice of DNA versus RNA.
will be adopted in regional centers with dedicated microbiology
Hurdles to mNGS Adoption laboratories with active research efforts.
While mNGS has clear potential to provide diagnostic informa- The availability of mNGS sequencing platforms presents and
tion, several hurdles to widespread adoption exist. Regulatory important challenge for medical laboratory scientists — know-
hurdles and issues of reimbursement certainly limit the wholesale ing how to make sense of the massive sequence data generated
replacement of culture, but as with other alternatives to culture, by new sequencing technologies. When performing testing on
mNGS will likely find use where culture has already failed or site, suitable IT infrastructure and well-trained bioinformatics
cannot provide the necessary information (e.g., strain outbreaks). scientists are required prior to adopting the mNGS for clinical
While cost is of concern, it is not unreasonable that the cost of use — this infrastructure is expensive and suitable trained staff
sequencing a sample could drop to a few hundred dollars soon, can be hard to find. Even when sending samples to reference
which would bring mNGS into the same cost range as targeted or for-profit boutique laboratories, the clinical laboratory must
PCR or some high-end cultures. Despite the concerns of the cost understand the technology well enough to select a suitable labo-
of mNGS, it should be kept in mind that while the cost of the ratory. Simple reports and simple and user-friendly bioinformat-
assay may never be as low as that of alternatives, such as routine ics work-flow is mandatory, but there are currently few products
culture, overall health care costs may be reduced by increasing that meet the needs of non-research-based, non-reference-based
the rate of diagnoses with mNGS, leading to improved therapy and non-profit clinical laboratories. Reference databases, gene
and patient outcomes and reduced hospitalizations, morbidity, calling software, protocols for microbial identification and cost-
and mortality. Of more immediate concern will be establishing effective technology utilization are all key challenges that require
standard protocols for sample preparation, sequencing, and data cost-effective solutions. Currently, mNGS sequencing quality
analysis. Furthermore, spiked controls need to be developed that is a topic being addressed by the Division of Laboratory Sys-
can simultaneously suppress background and allow absolute quan- tems, at the Center for Disease Control and Prevention (https://
titation, which could allow clinicians to differentiate between true www.cdc.gov/cliac/docs/fall-2019/6_Fitzgerald_NGS-Quality-
positives and commensals. Lastly, the limits of detection need to CLIAC_Nov_2019_FINAL.pdf ). The American Public Health
be determined for each clinical setting in which mNGS will be Association posts additional guidance about mNGS implementa-
applied. Once these technical details are in place, the pipelines tion (https://www.aphl.org/aboutAPHL/publications/Documents/
will have to demonstrate not just clinical validity, but clinical ID-NGS-Implementation-Guide102016.pdf ). The Association
58 Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier
for Molecular Pathology provides support to assess cost-benefit [13] Marotz CA, Sanders JG, Zuniga C, Zaramela LS, Knight R, Zengler
of mNGS ((https://www.amp.org/advocacy/advocacy-resources/ K. Improving saliva shotgun metagenomics by chemical host DNA
depletion. Microbiome 2018;6.
coverage-and-reimbursement/ngs-pricing-project/).
[14] Watanabe N, Kryukov K, Nakagawa S, Takeuchi JS, Takeshita M,
Kirimura Y, et al. Detection of pathogenic bacteria in the blood from
Summary
sepsis patients using 16S rRNA gene amplicon sequencing analysis.
Although there are limitations and challenges, the mNGS PLoS One 2018;13:e0202049.
approach offers an unbiased and hypothesis-free approach to [15] Watts GS, Thornton JE, Jr, Youens-Clark K, Ponsero AJ, Slepian
pathogen identification with the potential to detect uncultivable MJ, Menashi E, et al. Identification and quantitation of clinically
relevant microbes in patient samples: comparison of three k-mer
bacterial, viral, fungal, and parasitic organisms in the same assay. based classifiers for speed, accuracy, and sensitivity. PLoS Comput
Advances in mNGS technology and data analysis will likely reduce Biol 2019;15:e1006863.
testing costs to the point where the advantages of mNGS over [16] Ounit R, Wanamaker S, Close TJ, Lonardi S. CLARK: fast and
culture warrant its use in some clinical settings. accurate classification of metagenomic and genomic sequences using
discriminative k-mers. BMC Genomics 2015;16:236.
References [17] Edgar RC. Search and clustering orders of magnitude faster than
BLAST. Bioinformatics 2010;26:2460-1.
[1] van Walraven C, Wong J. Independent influence of negative blood [18] Wood DE, Salzberg SL. Kraken: ultrafast metagenomic sequence
cultures and bloodstream infections on in-hospital mortality. BMC classification using exact alignments. Genome Biol 2014;15:R46.
Infect Dis 2014;14:36.
[19] Rosen G, Garbarine E, Caseiro D, Polikar R, Sokhansanj B. Metage-
[2] Ecker DJ, Sampath R, Li H, Massire C, Matthews HE, Toleno D, nome fragment classification using n-mer frequency profiles. Adv
et al. New technology for rapid molecular diagnosis of bloodstream Bioinform 2008;2008.
infections. Expert Rev Mol Diagn 2010;10:399-415.
[20] Rosen GL, Reichenberger ER, Rosenfeld AM. NBC: the Naive
[3] Wilson MR, Sample HA, Zorn KC, Arevalo S, Yu G, Neuhaus J, et Bayes Classification tool webserver for taxonomic classification of
al. Clinical metagenomic sequencing for diagnosis of meningitis and metagenomic reads. Bioinformatics 2011;27:127-9.
encephalitis. N Engl J Med 2019;380:2327-40. [21] Bazinet AL, Cummings MP. A comparative evaluation of sequence
[4] Dai Y, Chen L, Chang W, Lu H, Cui P, Ma X. Culture-negative classification programs. BMC Bioinform 2012;13:92.
Streptococcus suis infection diagnosed by metagenomic next-generation [22] Buchfink B, Xie C, Huson DH. Fast and sensitive protein alignment
sequencing. Front Public Health 2019;7:379. using DIAMOND. Nat Methods 2015;12:59-60.
[5] Parize P, Muth E, Richaud C, Gratigny M, Pilmis B, Lamamy A, et [23] Meinicke P. UProC: tools for ultra-fast protein domain classification.
al. Untargeted next-generation sequencing-based first-line diagnosis Bioinformatics 2015;31:1382-8.
of infection in immunocompromised adults: a multicentre, blinded, [24] Zhao Y, Tang H, Ye Y. RAPSearch2: a fast and memory-efficient
prospective study. Clin Microbiol Infect 2017;23:574.e1-e6. protein similarity search tool for next-generation sequencing data.
[6] Snitkin ES, Zelazny AM, Thomas PJ, Stock F, NISC Compara- Bioinformatics 2012;28:125-6.
tive Sequencing Program Group, Henderson DK, et al. Tracking a [25] Huson DH, Xie C. A poor man’s BLASTX—high-throughput
hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with metagenomic protein database search using PAUDA. Bioinformatics
whole-genome sequencing. Sci Transl Med 2012;4:148ra116. 2014;30:38-9.
[7] Nakagawa S, Inoue S, Kryukov K, Yamagishi J, Ohno A, Hayashida [26] Aziz RK, Bartels D, Best AA, DeJongh M, Disz T, Edwards RA, et al.
K, et al. Rapid sequencing‐based diagnosis of infectious bacterial The RAST Server: rapid annotations using subsystems technology.
species from meningitis patients in Zambia. Clin Transl Immunol BMC Genomics 2008;9:75.
2019;8:e0202049. [27] Salter SJ, Cox MJ, Turek EM, Calus ST, Cookson WO, Moffatt MF,
[8] Ventola CL. The antibiotic resistance crisis: part 2: management et al. Reagent and laboratory contamination can critically impact
strategies and new agents. P T 2015;40:344-52. sequence-based microbiome analyses. BMC Biol 2014;12:87.
[28] Ellington MJ, Ekelund O, Aarestrup FM, Canton R, Doumith M,
[9] Deurenberg RH, Bathoorn E, Chlebowicz MA, Couto N, Ferdous
Giske C, et al. The role of whole genome sequencing in antimicrobial
M, García-Cobos S, et al. Application of next generation sequenc-
susceptibility testing of bacteria: report from the EUCAST Subcom-
ing in clinical microbiology and infection prevention. J Biotechnol
mittee. Clin Microbiol Infect 2017;23:2-22.
2017;243:16-24.
[29] Stoesser N, Batty EM, Eyre DW, Morgan M, Wyllie DH, Del Ojo
[10] Goldberg B, Sichtig H, Geyer C, Ledeboer N, Weinstock GM. Elias C, et al. Predicting antimicrobial susceptibilities for Escherichia
Making the leap from research laboratory to clinic: challenges and coli and Klebsiella pneumoniae isolates using whole genomic sequence
opportunities for next-generation sequencing in infectious disease data. J Antimicrob Chemother 2013;68:2234-44.
diagnostics. MBio 2015;6:e01888-15.
[30] Aanensen DM, Feil EJ, Holden MTG, Dordel J, Yeats CA, Fedosejev
[11] Simner PJ, Miller S, Carroll KC. Understanding the promises and A, et al. Whole-genome sequencing for routine pathogen surveillance
hurdles of metagenomic next-generation sequencing as a diagnostic in public health: a population snapshot of invasive Staphylococcus
tool for infectious diseases. Clin Infect Dis 2018;66:778-88. aureus in Europe. MBio 2016;7.
[12] Frey KG, Herrera-Galeano JE, Redden CL, Luu TV, Servetas SL, [31] Chen F-J, Wang C-H, Chen C-Y, Hsu Y-C, Wang K-T. Role of
Mateczun AJ, et al. Comparison of three next-generation sequencing the mecA gene in oxacillin resistance in a Staphylococcus aureus clini-
platforms for metagenomic sequencing and identification of patho- cal strain with a pvl-positive ST59 genetic background. Antimicrob
gens in blood. BMC Genomics 2014;15:96. Agents Chemother 2014;58:1047-54.
Clinical Microbiology Newsletter 42:7,2020 | ©2020 Elsevier 59
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5825)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (403)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Practice Toeic Reading Test 2021 03 - Tests + AnswerDocument19 pagesPractice Toeic Reading Test 2021 03 - Tests + AnswerAVRILLIA CLEMENTINENo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Unit Operation in Food Processing Chapter 6 ProblemsDocument12 pagesUnit Operation in Food Processing Chapter 6 ProblemsTeh Sze Yin100% (3)
- Gross National Income Per Capita 2019, Atlas Method and PPPDocument4 pagesGross National Income Per Capita 2019, Atlas Method and PPPElisha WankogereNo ratings yet
- InterSchool Activity ScriptDocument7 pagesInterSchool Activity ScriptJessica Loren Leyco87% (15)
- Swarm WhitepaperDocument46 pagesSwarm WhitepaperJoel Dietz100% (1)
- Instagram Creators Handbook - IGTV PDFDocument48 pagesInstagram Creators Handbook - IGTV PDFAndrei Neațu100% (1)
- NGS_biothreat_applicationsDocument10 pagesNGS_biothreat_applicationsKrisztián TóthNo ratings yet
- 2017 - Ruud H. Deurenberga, - Journal of BiotechnologyDocument9 pages2017 - Ruud H. Deurenberga, - Journal of BiotechnologyNeha PalNo ratings yet
- NGSplatforms_metagenomic_blood_pathogensDocument14 pagesNGSplatforms_metagenomic_blood_pathogensKrisztián TóthNo ratings yet
- NGS_in_clinmicrob_genes-13-01566Document24 pagesNGS_in_clinmicrob_genes-13-01566Krisztián TóthNo ratings yet
- WHO Influenza PrimersDocument1 pageWHO Influenza PrimersKrisztián TóthNo ratings yet
- 1-s2.0-S0197458019301083-mainDocument12 pages1-s2.0-S0197458019301083-mainKrisztián TóthNo ratings yet
- Cytokines: Names and Numbers You Should Care About: Stephen R. Holdsworth and Poh-Yi GanDocument12 pagesCytokines: Names and Numbers You Should Care About: Stephen R. Holdsworth and Poh-Yi GanKrisztián TóthNo ratings yet
- Opal2000 PDFDocument11 pagesOpal2000 PDFKrisztián TóthNo ratings yet
- Bulletin: Medical University of InnsbruckDocument5 pagesBulletin: Medical University of InnsbruckKrisztián TóthNo ratings yet
- Sikafloor®-169: Product Data SheetDocument4 pagesSikafloor®-169: Product Data SheetMohammed AwfNo ratings yet
- Taxation: Bmbes 2020 Barangay Micro Business Enterprise BMBE Law's ObjectiveDocument3 pagesTaxation: Bmbes 2020 Barangay Micro Business Enterprise BMBE Law's Objectivekris mNo ratings yet
- 05 - Quiz - 1 - HRMDocument3 pages05 - Quiz - 1 - HRMMillania ThanaNo ratings yet
- Question BankDocument9 pagesQuestion Bankshama JNo ratings yet
- Quectel M12 at Commands Manual V3 2Document195 pagesQuectel M12 at Commands Manual V3 2kalpeshbrNo ratings yet
- Pwwha: Delhi 10RDocument44 pagesPwwha: Delhi 10Rserrano.flia.coNo ratings yet
- DMTR DataDocument3 pagesDMTR DataŽiga PosediNo ratings yet
- 21cs644 Module 3Document95 pages21cs644 Module 3gmaheshreddy229No ratings yet
- Garden Growers Nursery Technician: Job DescriptionDocument2 pagesGarden Growers Nursery Technician: Job DescriptionKevin PittNo ratings yet
- 21810, Ultrapure Water Breakpoint CL andDocument5 pages21810, Ultrapure Water Breakpoint CL andWaleed EmaraNo ratings yet
- CE409 Quantity Surveying and ValuationDocument2 pagesCE409 Quantity Surveying and ValuationBala GopalNo ratings yet
- RCC Teen - Task 5 - BandwidthDocument2 pagesRCC Teen - Task 5 - BandwidthRares AndreiNo ratings yet
- Auction News Journal 3.1.14Document15 pagesAuction News Journal 3.1.14Etrans 1No ratings yet
- Production Line Resume SampleDocument2 pagesProduction Line Resume SampleadityadhimanNo ratings yet
- WALL STREET JOURNAL. CLASSROOM EDITION Chapter 14Document2 pagesWALL STREET JOURNAL. CLASSROOM EDITION Chapter 14Toby trittschlerNo ratings yet
- PMIT Admission Brochure - Spring 2021Document3 pagesPMIT Admission Brochure - Spring 2021Shayekh Mohiuddin Ahmed NavidNo ratings yet
- EN 12663-1 - 2010 - IndiceDocument6 pagesEN 12663-1 - 2010 - IndiceOhriol Pons Ribas67% (3)
- Chap 7Document38 pagesChap 7احمد نصارNo ratings yet
- PFMAT Budgeting - Framework - BOM - 2016 For PresentattionDocument33 pagesPFMAT Budgeting - Framework - BOM - 2016 For PresentattionJ Andrea Jaca100% (1)
- Nguyen Dai Duo NGDocument7 pagesNguyen Dai Duo NGtuan leNo ratings yet
- FOURNIER RF-5B - Sperber Flight Manual (English)Document29 pagesFOURNIER RF-5B - Sperber Flight Manual (English)Rene QueirozNo ratings yet
- EIC5000 Electronic Indicator Control Installation and Operation InstructionsDocument8 pagesEIC5000 Electronic Indicator Control Installation and Operation InstructionsАртемNo ratings yet
- Introduction To GNU Radio and Software RadioDocument4 pagesIntroduction To GNU Radio and Software RadioDinesh VermaNo ratings yet
- BEKIER Et Al v. COMMONWEALTH CONSTRUCTION COMPANY, INC. Et Al - Document No. 8Document12 pagesBEKIER Et Al v. COMMONWEALTH CONSTRUCTION COMPANY, INC. Et Al - Document No. 8Justia.com100% (1)