Professional Documents
Culture Documents
dextrose
dextrose
Uploaded by
NindiantiSaputriCopyright:
Available Formats
You might also like
- Greenbook Research Industry Trends Report 2020Document126 pagesGreenbook Research Industry Trends Report 2020Paul KendallNo ratings yet
- Art. 1474 - PRICEDocument4 pagesArt. 1474 - PRICEjamaica_maglinteNo ratings yet
- DextroseDocument4 pagesDextroseMaria HowayNo ratings yet
- s12884 023 05935 5Document7 pagess12884 023 05935 5Vargas Robles MayelaNo ratings yet
- Misoprostol For Prevention Postpartum HemorageDocument5 pagesMisoprostol For Prevention Postpartum Hemorageyanjangmed rspdsNo ratings yet
- Metanalisis Carbetocina Vs OxiDocument7 pagesMetanalisis Carbetocina Vs OxiSergio ZhinaNo ratings yet
- Postpartum HemorrageDocument6 pagesPostpartum HemorrageSherly Shabrina MustafaKamalNo ratings yet
- CarbetocinDocument23 pagesCarbetocinAulia RahmaNo ratings yet
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDocument5 pagesClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageTasya Arsy LiyanaNo ratings yet
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDocument5 pagesClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageMuhammad Ghifari RifanshaNo ratings yet
- Efficacy of Rectal Misoprostol For Prevention of Postpartum HemorrhageDocument6 pagesEfficacy of Rectal Misoprostol For Prevention of Postpartum HemorrhageArlinda Putry Manda SaryNo ratings yet
- Single Dose MisoprosotolDocument4 pagesSingle Dose MisoprosotolIce burgNo ratings yet
- Ijms 22 06985Document6 pagesIjms 22 06985krisnawatiNo ratings yet
- Ijgo 12687 PDFDocument6 pagesIjgo 12687 PDFDjlatino LatinoNo ratings yet
- GETEA2020Document5 pagesGETEA2020cours3bioNo ratings yet
- Journal EBM OBDocument15 pagesJournal EBM OBMary Paula EstiveNo ratings yet
- Ajol File Journals - 79 - Articles - 178373 - Submission - Proof - 178373 937 455552 1 10 20181010Document5 pagesAjol File Journals - 79 - Articles - 178373 - Submission - Proof - 178373 937 455552 1 10 20181010PMKP RSIAANUGRAHNo ratings yet
- Efficacy of Prophylactic Intravenous Tranexamic Acid in Preventing Postpartum Haemorrhage in Parturients With Risk Factors: A Randomized Control TrialDocument6 pagesEfficacy of Prophylactic Intravenous Tranexamic Acid in Preventing Postpartum Haemorrhage in Parturients With Risk Factors: A Randomized Control TrialInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- International Journal of Gynecology and ObstetricsDocument4 pagesInternational Journal of Gynecology and ObstetricsmerawatidyahsepitaNo ratings yet
- JournalDocument5 pagesJournalAfiyah putri zadaNo ratings yet
- 484 ArticleText 1393 2 10 20201115Document8 pages484 ArticleText 1393 2 10 20201115speedyz3377No ratings yet
- OB TXA Case Study - 090752Document10 pagesOB TXA Case Study - 090752Marlin LopezNo ratings yet
- P10 Nejmoa1805489Document10 pagesP10 Nejmoa1805489SEPTIANA SAPUTRINo ratings yet
- Medicina 56 00299 PDFDocument12 pagesMedicina 56 00299 PDFannisa sakinahNo ratings yet
- Preoperative Miso Pros To LDocument7 pagesPreoperative Miso Pros To LDrHariom KeshariNo ratings yet
- 1 s2.0 S1110569017300493 Main PDFDocument5 pages1 s2.0 S1110569017300493 Main PDFLeão ForteNo ratings yet
- Postpartum Hemorrhage in The Developed World: Whither Misoprostol?Document3 pagesPostpartum Hemorrhage in The Developed World: Whither Misoprostol?Tracy VillegasNo ratings yet
- JournalDocument10 pagesJournalAfwan saidiNo ratings yet
- Clinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyDocument7 pagesClinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyTri Anna FitrianiNo ratings yet
- Carbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewDocument7 pagesCarbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewOscar Gregorio Coronado MacdanielNo ratings yet
- ejpmrhydatidiformmoleDocument5 pagesejpmrhydatidiformmoleTô ThuỷNo ratings yet
- 2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionDocument8 pages2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionHAVIZ YUADNo ratings yet
- Management of Third Stage of Labor: A Comparison of Intraumbilical Oxytocin and Placental Cord DrainageDocument8 pagesManagement of Third Stage of Labor: A Comparison of Intraumbilical Oxytocin and Placental Cord DrainageesterNo ratings yet
- Hemorragia Tubo DigestivoDocument23 pagesHemorragia Tubo DigestivoNadia DeschampsNo ratings yet
- Integrative Review 1Document20 pagesIntegrative Review 1api-391839992No ratings yet
- Oxytocin Before Vs After Placental Delivery Prevent Postpartum HemorrhageDocument5 pagesOxytocin Before Vs After Placental Delivery Prevent Postpartum HemorrhageRafael MarvinNo ratings yet
- Estudio RefillDocument15 pagesEstudio RefillmiltoncesargomezNo ratings yet
- B85. gui235CPG0910Document7 pagesB85. gui235CPG0910jhon heriansyahNo ratings yet
- W 3 e WDDocument6 pagesW 3 e WDsupaidi97No ratings yet
- Oxytocin Is Not Associated With Postpartum Hemorrhage in Labor Augmentation in A Retrospective Cohort Study in The United StatesDocument9 pagesOxytocin Is Not Associated With Postpartum Hemorrhage in Labor Augmentation in A Retrospective Cohort Study in The United Statesstat madeeasyNo ratings yet
- CD009332 AbstractDocument4 pagesCD009332 AbstractLilik AnggrainiNo ratings yet
- cm9 134 1043Document9 pagescm9 134 1043Yudha PramanaNo ratings yet
- Bushaqer-2018-Follicular Aspiration Versus CoaDocument6 pagesBushaqer-2018-Follicular Aspiration Versus Coanathalieleclef125No ratings yet
- Prolonged LaborDocument8 pagesProlonged LaborMisnariahIdrusNo ratings yet
- Update On The New Modalities On The Prevention and PDFDocument20 pagesUpdate On The New Modalities On The Prevention and PDFSamuel SammyNo ratings yet
- The Effect of Saline Lock On Phlebitis Rates of Patients in Cardiac Care UnitsDocument7 pagesThe Effect of Saline Lock On Phlebitis Rates of Patients in Cardiac Care UnitsVianne MaryNo ratings yet
- Evaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article ReviewDocument7 pagesEvaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article Reviewindex PubNo ratings yet
- Assessment of Oxidative Stress Markers in Cord Blood of Newborns To Patients With Oxytocin-Induced Labor.Document6 pagesAssessment of Oxidative Stress Markers in Cord Blood of Newborns To Patients With Oxytocin-Induced Labor.OSMAN EVLİYAOĞLUNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptBella DirkNo ratings yet
- s00404 019 05340 4Document8 pagess00404 019 05340 4Tanaporn ThongpolNo ratings yet
- Ursodeoxycholic Acid Versus Placebo in Women With Intrahepatic Cholestasis of Pregnancy (PITCHES) - A Randomised Controlled TrialDocument12 pagesUrsodeoxycholic Acid Versus Placebo in Women With Intrahepatic Cholestasis of Pregnancy (PITCHES) - A Randomised Controlled TrialcohortehospitalevitaNo ratings yet
- Research ArticleDocument10 pagesResearch ArticleAnonymous SbnDyANo ratings yet
- Use of A Condom To Control Massive Postpartum Hemorrhage.: January 2007Document13 pagesUse of A Condom To Control Massive Postpartum Hemorrhage.: January 2007asm obginNo ratings yet
- Research ArticleDocument9 pagesResearch Articlesukakitkat1418No ratings yet
- 30911-Article Text-57585-1-10-20210504Document15 pages30911-Article Text-57585-1-10-20210504Team - MEDICALSERVICESNo ratings yet
- The Effect of Cesarean Section and Vaginal Delivery On Ovarian Reserve in Infertile Women (#1118806) - 2437043Document5 pagesThe Effect of Cesarean Section and Vaginal Delivery On Ovarian Reserve in Infertile Women (#1118806) - 2437043Tandyo TriasmoroNo ratings yet
- 01 M039 43754Document16 pages01 M039 43754DrDeepak PawarNo ratings yet
- Comparative Efficacy and Safety of Urate-Lowering Therapy For The Treatment of Hyperuricemia: A Systematic Review and Network Meta-AnalysisDocument13 pagesComparative Efficacy and Safety of Urate-Lowering Therapy For The Treatment of Hyperuricemia: A Systematic Review and Network Meta-AnalysisWoo Rin ParkNo ratings yet
- Management of Ovarian EndometriomaDocument13 pagesManagement of Ovarian EndometriomaAghnia PutriNo ratings yet
- Active Management of The Third Stage of Labor With.17-2Document7 pagesActive Management of The Third Stage of Labor With.17-2Maleny FloresNo ratings yet
- Anti-Aging Therapeutics Volume XIVFrom EverandAnti-Aging Therapeutics Volume XIVRating: 3 out of 5 stars3/5 (1)
- Impact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyFrom EverandImpact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyNo ratings yet
- La Bugal V RamosDocument141 pagesLa Bugal V Ramosabo8008No ratings yet
- Distress Tolerance Handout 5 - Pros and Cons PDFDocument1 pageDistress Tolerance Handout 5 - Pros and Cons PDFRobinNo ratings yet
- TL-WN722N (UN) (US) V2 Datasheet PDFDocument4 pagesTL-WN722N (UN) (US) V2 Datasheet PDFBender :DNo ratings yet
- Bio-Valley Day Spa (Final Proposal To Submit) MDocument85 pagesBio-Valley Day Spa (Final Proposal To Submit) MAtiqah Hasan100% (4)
- Better Get 'It in Your SoulDocument4 pagesBetter Get 'It in Your SoulJeremiah AnnorNo ratings yet
- Andheri WestDocument60 pagesAndheri WestNikunj VaghasiyaNo ratings yet
- Notice 1658958950Document64 pagesNotice 1658958950Subrat NaikNo ratings yet
- Buy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlineDocument5 pagesBuy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlinelorendesuzaNo ratings yet
- B412 TM Vol 1 Bell 412 EPDocument288 pagesB412 TM Vol 1 Bell 412 EPAri100% (1)
- WikiHow Is An Online WikiDocument4 pagesWikiHow Is An Online Wikiksdnfi ouvynNo ratings yet
- Billing Reports Export 1702384478083Document82 pagesBilling Reports Export 1702384478083vinjamuriraviteja123No ratings yet
- TRP 8750DDocument276 pagesTRP 8750DKentNo ratings yet
- Optimization Module For Abaqus/CAE Based On Genetic AlgorithmDocument1 pageOptimization Module For Abaqus/CAE Based On Genetic AlgorithmSIMULIACorpNo ratings yet
- Staircase Lift Design For Elderly at HomeDocument19 pagesStaircase Lift Design For Elderly at Homesabareesh91mechNo ratings yet
- Sankaran, Mahesh - Scogings, Peter F - Savanna Woody Plants and Large Herbivores (2020, John Wiley & Sons LTD)Document781 pagesSankaran, Mahesh - Scogings, Peter F - Savanna Woody Plants and Large Herbivores (2020, John Wiley & Sons LTD)Ariadne Cristina De AntonioNo ratings yet
- Passive VoiceDocument2 pagesPassive VoiceJoseph HopperNo ratings yet
- Capr-Iii En4115 PDFDocument49 pagesCapr-Iii En4115 PDFYT GAMERSNo ratings yet
- (Lovebook care - Anh) Đề thi thử THPTQG trường THPT Chuyên Cao Bằng lần 1Document16 pages(Lovebook care - Anh) Đề thi thử THPTQG trường THPT Chuyên Cao Bằng lần 1Dương Viết ĐạtNo ratings yet
- Basic Law 01Document33 pagesBasic Law 01MitchNo ratings yet
- Seminar - Diabetes Mellitus Final VersionDocument14 pagesSeminar - Diabetes Mellitus Final Versionmustafalotfy01No ratings yet
- 1 Cyber Law PDFDocument2 pages1 Cyber Law PDFKRISHNA VIDHUSHANo ratings yet
- Java Cheat Sheet & Quick ReferenceDocument16 pagesJava Cheat Sheet & Quick Referencedad dunnoNo ratings yet
- MATH CHALLENGE GRADE 2 - Google FormsDocument5 pagesMATH CHALLENGE GRADE 2 - Google FormsAivy YlananNo ratings yet
- BMR 2105 PDFDocument6 pagesBMR 2105 PDFSitoraKodirovaNo ratings yet
- Automated Guided VehicleDocument14 pagesAutomated Guided VehicleSRI RAMNo ratings yet
- Bal Natu - Glimpses of The God-Man, Meher Baba - 1943-1948 (Vol. I) (1997)Document431 pagesBal Natu - Glimpses of The God-Man, Meher Baba - 1943-1948 (Vol. I) (1997)Kumar KNo ratings yet
- 107 Hand Tool Field Maintenance v0311Document8 pages107 Hand Tool Field Maintenance v0311rabbit_39No ratings yet
- Kult - The Dark Art PDFDocument7 pagesKult - The Dark Art PDFalnevoNo ratings yet
dextrose
dextrose
Uploaded by
NindiantiSaputriCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
dextrose
dextrose
Uploaded by
NindiantiSaputriCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/335400486
Comparing the Effect of Dextrose and Oxytocin to Reduce Postpartum
Haemorrhage: Randomised Controlled Trial
Article in Journal of Clinical and Diagnostic Research · July 2019
DOI: 10.7860/JCDR/2019/35479.12987
CITATIONS READS
0 522
4 authors:
Zainab Suhrabi Malihe Akbari
Ilam University of Medical Sciences University of Medical Sciences of Ilam
20 PUBLICATIONS 476 CITATIONS 9 PUBLICATIONS 348 CITATIONS
SEE PROFILE SEE PROFILE
Hamid Taghinejad Golnaz Azami
Ilam University of Medical Sciences Kurdistan University of Medical Sciences
42 PUBLICATIONS 612 CITATIONS 25 PUBLICATIONS 274 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Golnaz Azami on 16 February 2020.
The user has requested enhancement of the downloaded file.
DOI: 10.7860/JCDR/2019/35479.12987
Original Article
Comparing the Effect of Dextrose and Oxytocin
Obstetrics and Gynaecology
to Reduce Postpartum Haemorrhage:
Section
Randomised Controlled Trial
Zainab Suhrabi1, Malihe Akbari2, Hamid Taghinejad3, Golnaz Azami4
ABSTRACT dextrose solution (intervention group). The primary outcome
Introduction: Post-partum haemorrhage is a leading cause of measured in this study was amount of blood loss. The outcome
maternal mortality and morbidity worldwide. There are different was assessed at 1 hour and 2 hours. Data were analysed using
management procedures adopted for the treatment of post- SPSS version 22.0, chi-square and student’s t-tests. Authors
partum haemorrhage. used expected maximisation to handle missing data to enable
an intention-to-treat analysis.
Aim: To evaluate the efficacy of dextrose in Post-partum
Haemorrhage (PPH) and compare it with Oxytocin (a conventional Results: At baseline, the groups were homogeneous in regards
method). to socio-demographic variables. The average blood loss was
significantly lower in the intervention group (dextrose 10%)
Materials and Methods: A two-arm randomised controlled
compared to the control group (oxytocin) (p<0.05).
trial was conducted among 120 pregnant women admitted to
the delivery room of the Obstetric and Gynaecological Unit of Conclusion: Administering of dextrose 10% to pregnant women
a Teaching Hospital. Participants were randomised to receive at the third stage of labour was associated with lower post-
either 20 unit of oxytocin in 1000 mL ringer lactate solution partum haemorrhage than oxytocin.
(routine administration, control group) or 200 mL of 10%
Keywords: Blood loss, Oxytocin, Vaginal delivery
INTRODUCTION managed by giving intravenous injection of glucose [3]. Recent
Post-Partum Haemorrhage (PPH) is the third cause of maternal data suggest that injection of dextrose 10% can effectively
mortality and accounts for the majority of the 14 million cases stimulate uterine contraction after caesarean section [9]. The
annually [1]. PPH is defined as the loss of ≥500 mL of blood (or vaginal delivery is the optimal method of childbirth [10,11].
1000 mL) in the first 24 hours after delivery. The global prevalence Researchers should try to identify safe techniques to follow in
of PPH ranged from 7.2% in Oceania to 25.7% in Africa. The order to reduce labour complications rate. Thus, the present
prevalence of PPH in Iran is 4% [2,3]. The most common cause study aimed to compare the effect of dextrose 10% and oxytocin
of PPH is failure of uterine contraction (uterine atony) following on PPH after the delivery.
delivery. There are several known factors that cause uterine atony
including prolonged labour, excessive enlargement of the uterus, MATERIALS AND METHODS
multi-fetal pregnancy and multiparity. The first-line treatment for
Study Design
PPH is administration of Oxytocin, Carboprost, Tromethamine
1. A two-armed randomised trial over 11 months (from April
and Metyl Orgonat. Oxytocin (20 IU in 1000 mL ringer lactate
solution) is infused for 1 hour after delivery in order to retain the 2012 till February 2013) was conducted. Participants were
normal uteral tone [4-6]. However, these drugs have several side- randomised into the two groups.
effects. For example, common side-effects of oxytocin include: 2. Receiving 20 unit of oxytocin in 1000 mL ringer lactate solution
hypertension, tachycardia, reduced myocardial perfusion, cardiac (routine administration, control group).
arrest and water intoxication [7]. Other common adverse-effect 3. Receiving 200 mL of 10% dextrose solution (intervention group).
of oxytocin include water retention and seizure secondary to
hyponatremia [8]. As mentioned earlier, many of the currently Study Setting
marketed drugs have several side-effects and limitation, which Participants were recruited from an urban primary and secondary
makes it necessary to study alternatives to these drugs. There is hospital in Ilam city, Iran. All pregnant women who were admitted
evidence of the influential effects of glucose (dextrose) on smooth
to labour room for delivery during the study period were invited to
muscle cells [9]. Glycogen serves as the most important source of
participate in this study. Participants were eligible if they were in
energy for the muscle contractions (glycogen is the storage form
the third phase of vaginal delivery, singleton pregnancies, aged 18-
of glucose). Maternal stress leads to muscle cells contraction and
potentially cause glucose uptake [3]. These contractions act as 35 years-old, and fetus weight of 2500-4500 grams. Participants
a fatigue factor on the myometrium muscles and thus lead to were excluded if they had hypertension, placenta previa, placental
postpartum atony. A low level of glucose will lead to low level abruption, anemia (haemoglobin <12 g/mL), the first stages of delivery
of insulin. Consequently, the body will produce ketones to fuel lasted more than 15 hours, polyhydramnios, multiple pregnancy,
the body cells. A build-up of ketones in the blood can lead to past or present history of vaginal bleeding during pregnancy and
ketoacidosis which can effectively decrease the frequency and delivery, curettage, cesarean section, operative vaginal delivery and
intensity of uterine contractions. This can be prevented and history of anticoagulant therapy.
Journal of Clinical and Diagnostic Research. 2019 Jul, Vol-13(7): QC09-QC11 9
Zainab Suhrabi et al., A New Approach to Reduce Postpartum Bleeding www.jcdr.net
Determination of Sample Size weighed and recorded at first and second hour after delivery. One-
Sample size was estimated at the desired significance level of gram increase in the weight of the gauzes is equal to one millilitre
5%, two-sided alpha of 0.05 and 90% power to detect a 3 mL of blood loss. Gauze samples were weighted by a digital sensitive
difference in blood loss. Primary outcome was amount of PPH. weighing balance (Scoute, Ohaus, 0.1 g accuracy) [6,12-15].
The sample was calculated based on the amount of blood loss
differences between two groups. Hence, sample size calculations Ethical Consideration
show that at least 60 subjects in each group were needed to detect The Ilam University of Medical Science approved this study. All eligible
a statistical difference. participants were provided with oral and written informed consent
prior to initiation of the study and were asked to sign consent form.
Recruitment and Randomisation Process
The recruitment process was conducted in two stages. At the first Trial Registry
stage, to achieve adequate participant enrolment, advertising flyers This trial was registered in the world health organisation approved
were placed on the notice boards of the hospital. In the second Committee of the Iranian Clinical Trial Registry with registration
stage, all participants went through a screening process conducted number IRCT201304146790N6.
by the researchers. Based on the inclusion and exclusion criteria
120 patients were screened for eligibility by the study researchers. Statistical Analysis
The screening process was standardised with a comprehensive case Descriptive statistics were presented using frequencies for
report form, on which each respondent’s results were recorded. The categorical data and means and Standard Deviation (SD) for
information collected included socio-demographic profiles, medical continuous variables. The normality of the data was assessed
and drug history and amount of bleeding. Prior to enrolment, eligible using Shapiro-Wilk tests. Baseline characteristics of the two
participants were provided with a detailed description of the study. groups (Homogeneity of sample) were assessed using analysis
Following examination and enrolment, eligible respondents were of variance for continuous variables and chi-square statistics for
sequentially numbered and randomly allocated into two groups categorical variables. Chi-square and independent t-test were used
using a computer generated random number. The person (the first to determine the effect of the intervention within the groups during
author) conducting the randomisation, received only participants the study period (one and two hours after delivery). All data were
IDs and was hence completely blind to the respondent’s information analysed using SPSS, (version 16, SPSS Inc, Chicago, IL, USA).
and identities [Table/Fig-1].
RESULTs
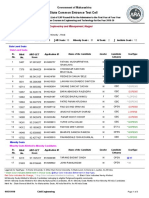
As shown in [Table/Fig-2], the two groups had similar characteristics
at baseline. Further, the mean differences for each covariate
between two groups were not statistically significant. Two
independent sample t-tests were conducted to compare the effect
of administering oxytocin and Dextrose 10% on the amount of PPH
after delivery. The first sample t-test indicated that there was a
significant difference in the scores of dextrose 10% (142.17±61.15)
and oxytocin (196.27±56.24) on the amount of PPH one hour after
delivery (p=0.001). The second sample t-test indicated that there was
a significant difference in the score of dextrose 10% (81.65±15.45)
and oxytocin (102.65±13.32) on the amount of PPH two hours after
delivery (p=0.002) [Table/Fig-3]. As shown in this study, dextrose
10% was more effective in controlling PPH as compared to oxytocin
during the first and second hours after delivery.
Groups/Variable Oxytocin Mean±SD Dextrose Mean±SD p-value
Mothers age 29.15±4.13 28.64±4.09 0.62
BMI 23.82±1.3 24.55±2.3 0.56
Gestational age (week) 38.89±1.1 39.45±0.9 0.48
Gravity (number) 1.82±0.7 1.76±0.5 0.53
Term of active phase
251.71±53.7 260.27±43.3 0.53
(minute)
Second stage period
51.79±8.62 59.45±7.51 0.087
(minute)
[Table/Fig-1]: CONSORT flow chart. The time of lactation
28.25±5.8 32.15±4.8 0.21
starting *(minute)
The Intervention Neonate weigh (gram) 3200±330 3250±219 0.32
Immediately after the delivery, routine haemorrhage control was APGAR 8.98±0.08 9.15±0.02 0.55
performed with intravenous infusion of oxytocin (20 units of oxytocin
[Table/Fig-2]: Comparison of demographic data, midwifery factor and neonatal
in 1000 mL ringer lactate solution) in control group. Participants in factor in two groups.
the intervention group received 200 mL of 10% dextrose solution *time between childbirth and beginning of breastfeeding
intravenously to prevent any potential PPH. For each patient,
systolic and diastolic blood pressure, body temperature, pulse and Bleeding (CC)/Time Oxytocin Mean±SD Dextrose Mean±SD p-value
respiratory rate were continuously measured and recorded each The amount of bleeding
196.27±56.24 142.17±61.15 0.001
quarter during the first 48 hours after delivery. The volume of blood (first hour) (mL)
loss was calculated by subtracting the weight of gauzes placed The amount of bleeding
102.65±13.32 81.65±15.45 0.002
(second hour) (mL)
under the patient’s buttocks before delivery from the weight of the
Shawn after all visible blood were wiped away. Gauze samples were [Table/Fig-3]: Mean±SD of Blood loss during two hours after delivery in two groups.
10 Journal of Clinical and Diagnostic Research. 2019 Jul, Vol-13(7): QC09-QC11
www.jcdr.net Zainab Suhrabi et al., A New Approach to Reduce Postpartum Bleeding
DISCUSSION Funding/Support: This study was supported by Ilam University of
PPH is considered as one of the most important factor Medical Sciences.
contributed to maternal mortality and life-threatening situation
in developing countries [16]. Uterine atony is the most common References
[1] Sahhaf F, Abbasalizadeh S, Ghojazadeh M, Velayati A, Khandanloo R, Saleh
cause of PPH, accounting for 80% of PPH cases. To prevent
P, et al. Comparison effect of intravenous tranexamic acid and misoprostol for
PPH due to ineffective uterine contractions, effective strategies postpartum haemorrhage. Nigerian Medical Journal. 2014;55(4):348.
to prevent and manage bleeding, need be applied. The present [2] Calvert C, Thomas SL, Ronsmans C, Wagner KS, Adler AJ, Filippi V. Identifying
study indicated that the intravenous administration of dextrose regional variation in the prevalence of postpartum haemorrhage: a systematic
review and meta-analysis. PloS One. 2012;7(7):e41114.
10% is an appropriate strategy for controlling PPH. Dextrose is [3] Mirtimori MK, F. Borayri, T. A comparison of therapeutic effect between
more effective than oxytocin in controlling blood loss during the intravenous calcium gluconate and hypertonic glucose on atonic uterine in
two hours after delivery. This result is in line with the findings maternity hospital in Zahedan, Iran. Asrar- Journal of Sabzevar School of Medical
Sciences and Health Services. 2003;02.
of the previous study by Rafiee MS et al., [9]. Previous studies [4] Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum
have compared the effectiveness of date fruit consumption and hemorrhage in a large, nationwide sample of deliveries. Anesthesia & Analgesia.
oxytocin on the amount of bleeding following normal delivery. 2010;110(5):1368-73.
[5] Coker A, Lawal AH, Abu J, Cowen MJ. The B-Lynch surgical technique for the
Results of these studies suggested that blood loss during the
control of massive postpartum haemorrhage: an alternative to hysterectomy?
first two hours after delivery were lower in those participants who Five cases reported. BJOG: An International Journal of Obstetrics & Gynaecology.
received date fruit when compared to those who received oxytocin 1997;104(3):372-75.
(p<0.005) [8,9]. Hatami Rad R NS and Hekmat KH, compared [6] Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C. Williams
Obstetrics Edition T, editor. tehran: Golban nashr; 2014.
the effectiveness of Normal saline and Dextrose saline on Labour [7] Grady K, Johnston T. Maternal collapse, including massive obstetric haemorrhage,
period and delivery outcomes in nulliparous women. The finding amniotic fluid embolism and cardiac arrest. Core Topics in Obstetric Anaesthesia.
from this study indicated that duration of labour can be decreased 2015;191.
[8] Silva P, Allan MS. Water Intoxication due to high doses of synthetic oxytocin:
by the administration of intravenous dextrose [11]. Rahmani
report of a case. Obstetrics & Gynaecology. 1966;27(4):517-20.
Bilandi R MA et al., conducted a clinical study to examine the [9] Rafiee MS, M. Noureddini, M. Azar Mehr, F. Mousavi SGA. Comparing the efficacy
effectiveness of food intake during labour on obstetric outcomes. of 10% dextrose with 40 units of oxytocin per liter in uterine involution after
Participants were divided into two groups: consumption of a light Cesarean. Journal of Lorestan University of Medical Sciences. 2006;8(1):13-19.
[10] Taghinejad H, Delpisheh A, Suhrabi Z. Comparison between massage
diet or water during labour. This study indicates that the duration and music therapies to relieve the severity of labour pain. Women’s Health.
of labour was shorter in those who consume a light diet [17]. With 2010;6(3):377-81.
regard to the effect of dextrose 10% on postpartum haemorrhage, [11] Hatami Rad R NS, Hekmat KH. Effects of intravenous normal saline with and
without dextrose on labour duration and delivery outcomes in nulliparous women.
it was hypothesised that activation of voltage-gated calcium (Ca2+) Koomesh. 2012;13(4):434-39.
channels initiate contraction of myometer directly by increasing [12] Fakour F, Mirzayi M, Naghipour MR, Ebrahimi H, Mahdavi M. Comparison
cytosolic Ca2+ concentration. In particular, the role of potassium between sublingual misoprostol and intravenous oxytocin in management of third
stage of labour. The Iranian Journal of Obstetrics, Gynaecology and Infertility.
channels must not be ignored. Potassium channels have inhibitory
2012;15(34):7-14.
effect on calcium L-type channels [9]. [13] Shripad H, Rai L, Mohan A. Comparison of blood loss in induced vs. Spontaneous
There is some evidence that shows that acute hyperglycaemia vaginal delivery using specialized blood collection bag. Journal of Clinical and
Diagnostic Research: JCDR. 2014;8(4):OC01.
cause vasodilatation by increasing opening of potassium channels [14] Suhrabi Z, Taghinejad H, Direkvand-Moghadam A, Akbari M. The effect of
and Protein Kinase C (PKC) [9,18-20]. oxygen inhalation plus oxytocin compared with oxytocin only on postpartum
haemorrhage: A randomized clinical trial. Journal of Clinical and Diagnostic
Research: JCDR. 2016;10(9):QC01.
LIMITATION [15] Tourne G, Collet F, Lasnier P, Seffert P. Usefulness of a collecting bag for the
Because of ethical consideration, we could not deprive one group diagnosis of post-partum hemorrhage. Journal De Gynécologie, Obstétrique Et
from intervention and compare intervention groups with control (no Biologie De La Reproduction. 2004;33(3):229-34.
[16] Narenji FB, Z Mirzaie R. Comparison of the effect of oxytocin IM injection and
intervention) group. nipple stimulation on bleeding and length of third stage of delivery. Complementary
Medicine Journal. 2012;2(1):119-25.
CONCLUSION [17] Rahmani Bilandi R MA, Rahmani Bilandi MR, Askari F. The effect of food intake
during labour on maternal outcomes: A Randomized Controlled Trial. Ofogh-e-
Administering of dextrose 10% to pregnant women at the third Danesh GMUHS Journal. 2009;15(2):17-23.
stage of labour is associated with lower postpartum haemorrhage [18] Kinoshita H, Azma T, Nakahata K, Iranami H, Kimoto Y, Dojo M, et al. Inhibitory
effect of high concentration of glucose on relaxations to activation of ATP-
compared to Oxytocin.
sensitive K+ channels in human omental artery. Arteriosclerosis, thrombosis, and
vascular biology. 2004;24(12):2290-95.
Acknowledgements [19] Li H, Chai Q, Gutterman DD, Liu Y. Elevated glucose impairs cAMP-mediated
Special thanks go to all the patients that participated in the present dilation by reducing Kv channel activity in rat small coronary smooth muscle
cells. American Journal of Physiology-Heart and Circulatory Physiology.
study. 2003;285(3):H1213-H9.
Author’s Contribution: MA, HT, ZS, GA were responsible for the [20] Longo M, Jain V, Vedernikov Y, Hankins G, Garfield R, Saade G. Effects of L-type
Ca2+-channel blockade, K+ ATP-channel opening and nitric oxide on human
study conception, design, literature review, data analysis, and uterine contractility in relation to gestational age and labour. Molecular Human
manuscript preparation. Reproduction. 2003;9(3):159-64.
PARTICULARS OF CONTRIBUTORS:
1. PhD Student, Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran; MSc of Midwifery,
Department of Midwifery, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
2. Lecturer, Department of Midwifery, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
3. Associate Professor, Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
4. Assistant Professor, Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Hamid Taghinejad,
Ilam University of Medical Sciences, Ilam, Iran. Date of Submission: Jan 07, 2018
E-mail: taghinejad-h@medilam.ac.ir Date of Peer Review: Mar 19, 2018
Date of Acceptance: Nov 05, 2018
Financial OR OTHER COMPETING INTERESTS: As declared above. Date of Publishing: Jul 01, 2019
Journal of Clinical and Diagnostic Research. 2019 Jul, Vol-13(7): QC09-QC11 11
View publication stats
You might also like
- Greenbook Research Industry Trends Report 2020Document126 pagesGreenbook Research Industry Trends Report 2020Paul KendallNo ratings yet
- Art. 1474 - PRICEDocument4 pagesArt. 1474 - PRICEjamaica_maglinteNo ratings yet
- DextroseDocument4 pagesDextroseMaria HowayNo ratings yet
- s12884 023 05935 5Document7 pagess12884 023 05935 5Vargas Robles MayelaNo ratings yet
- Misoprostol For Prevention Postpartum HemorageDocument5 pagesMisoprostol For Prevention Postpartum Hemorageyanjangmed rspdsNo ratings yet
- Metanalisis Carbetocina Vs OxiDocument7 pagesMetanalisis Carbetocina Vs OxiSergio ZhinaNo ratings yet
- Postpartum HemorrageDocument6 pagesPostpartum HemorrageSherly Shabrina MustafaKamalNo ratings yet
- CarbetocinDocument23 pagesCarbetocinAulia RahmaNo ratings yet
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDocument5 pagesClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageTasya Arsy LiyanaNo ratings yet
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDocument5 pagesClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageMuhammad Ghifari RifanshaNo ratings yet
- Efficacy of Rectal Misoprostol For Prevention of Postpartum HemorrhageDocument6 pagesEfficacy of Rectal Misoprostol For Prevention of Postpartum HemorrhageArlinda Putry Manda SaryNo ratings yet
- Single Dose MisoprosotolDocument4 pagesSingle Dose MisoprosotolIce burgNo ratings yet
- Ijms 22 06985Document6 pagesIjms 22 06985krisnawatiNo ratings yet
- Ijgo 12687 PDFDocument6 pagesIjgo 12687 PDFDjlatino LatinoNo ratings yet
- GETEA2020Document5 pagesGETEA2020cours3bioNo ratings yet
- Journal EBM OBDocument15 pagesJournal EBM OBMary Paula EstiveNo ratings yet
- Ajol File Journals - 79 - Articles - 178373 - Submission - Proof - 178373 937 455552 1 10 20181010Document5 pagesAjol File Journals - 79 - Articles - 178373 - Submission - Proof - 178373 937 455552 1 10 20181010PMKP RSIAANUGRAHNo ratings yet
- Efficacy of Prophylactic Intravenous Tranexamic Acid in Preventing Postpartum Haemorrhage in Parturients With Risk Factors: A Randomized Control TrialDocument6 pagesEfficacy of Prophylactic Intravenous Tranexamic Acid in Preventing Postpartum Haemorrhage in Parturients With Risk Factors: A Randomized Control TrialInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- International Journal of Gynecology and ObstetricsDocument4 pagesInternational Journal of Gynecology and ObstetricsmerawatidyahsepitaNo ratings yet
- JournalDocument5 pagesJournalAfiyah putri zadaNo ratings yet
- 484 ArticleText 1393 2 10 20201115Document8 pages484 ArticleText 1393 2 10 20201115speedyz3377No ratings yet
- OB TXA Case Study - 090752Document10 pagesOB TXA Case Study - 090752Marlin LopezNo ratings yet
- P10 Nejmoa1805489Document10 pagesP10 Nejmoa1805489SEPTIANA SAPUTRINo ratings yet
- Medicina 56 00299 PDFDocument12 pagesMedicina 56 00299 PDFannisa sakinahNo ratings yet
- Preoperative Miso Pros To LDocument7 pagesPreoperative Miso Pros To LDrHariom KeshariNo ratings yet
- 1 s2.0 S1110569017300493 Main PDFDocument5 pages1 s2.0 S1110569017300493 Main PDFLeão ForteNo ratings yet
- Postpartum Hemorrhage in The Developed World: Whither Misoprostol?Document3 pagesPostpartum Hemorrhage in The Developed World: Whither Misoprostol?Tracy VillegasNo ratings yet
- JournalDocument10 pagesJournalAfwan saidiNo ratings yet
- Clinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyDocument7 pagesClinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyTri Anna FitrianiNo ratings yet
- Carbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewDocument7 pagesCarbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewOscar Gregorio Coronado MacdanielNo ratings yet
- ejpmrhydatidiformmoleDocument5 pagesejpmrhydatidiformmoleTô ThuỷNo ratings yet
- 2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionDocument8 pages2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionHAVIZ YUADNo ratings yet
- Management of Third Stage of Labor: A Comparison of Intraumbilical Oxytocin and Placental Cord DrainageDocument8 pagesManagement of Third Stage of Labor: A Comparison of Intraumbilical Oxytocin and Placental Cord DrainageesterNo ratings yet
- Hemorragia Tubo DigestivoDocument23 pagesHemorragia Tubo DigestivoNadia DeschampsNo ratings yet
- Integrative Review 1Document20 pagesIntegrative Review 1api-391839992No ratings yet
- Oxytocin Before Vs After Placental Delivery Prevent Postpartum HemorrhageDocument5 pagesOxytocin Before Vs After Placental Delivery Prevent Postpartum HemorrhageRafael MarvinNo ratings yet
- Estudio RefillDocument15 pagesEstudio RefillmiltoncesargomezNo ratings yet
- B85. gui235CPG0910Document7 pagesB85. gui235CPG0910jhon heriansyahNo ratings yet
- W 3 e WDDocument6 pagesW 3 e WDsupaidi97No ratings yet
- Oxytocin Is Not Associated With Postpartum Hemorrhage in Labor Augmentation in A Retrospective Cohort Study in The United StatesDocument9 pagesOxytocin Is Not Associated With Postpartum Hemorrhage in Labor Augmentation in A Retrospective Cohort Study in The United Statesstat madeeasyNo ratings yet
- CD009332 AbstractDocument4 pagesCD009332 AbstractLilik AnggrainiNo ratings yet
- cm9 134 1043Document9 pagescm9 134 1043Yudha PramanaNo ratings yet
- Bushaqer-2018-Follicular Aspiration Versus CoaDocument6 pagesBushaqer-2018-Follicular Aspiration Versus Coanathalieleclef125No ratings yet
- Prolonged LaborDocument8 pagesProlonged LaborMisnariahIdrusNo ratings yet
- Update On The New Modalities On The Prevention and PDFDocument20 pagesUpdate On The New Modalities On The Prevention and PDFSamuel SammyNo ratings yet
- The Effect of Saline Lock On Phlebitis Rates of Patients in Cardiac Care UnitsDocument7 pagesThe Effect of Saline Lock On Phlebitis Rates of Patients in Cardiac Care UnitsVianne MaryNo ratings yet
- Evaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article ReviewDocument7 pagesEvaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article Reviewindex PubNo ratings yet
- Assessment of Oxidative Stress Markers in Cord Blood of Newborns To Patients With Oxytocin-Induced Labor.Document6 pagesAssessment of Oxidative Stress Markers in Cord Blood of Newborns To Patients With Oxytocin-Induced Labor.OSMAN EVLİYAOĞLUNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptBella DirkNo ratings yet
- s00404 019 05340 4Document8 pagess00404 019 05340 4Tanaporn ThongpolNo ratings yet
- Ursodeoxycholic Acid Versus Placebo in Women With Intrahepatic Cholestasis of Pregnancy (PITCHES) - A Randomised Controlled TrialDocument12 pagesUrsodeoxycholic Acid Versus Placebo in Women With Intrahepatic Cholestasis of Pregnancy (PITCHES) - A Randomised Controlled TrialcohortehospitalevitaNo ratings yet
- Research ArticleDocument10 pagesResearch ArticleAnonymous SbnDyANo ratings yet
- Use of A Condom To Control Massive Postpartum Hemorrhage.: January 2007Document13 pagesUse of A Condom To Control Massive Postpartum Hemorrhage.: January 2007asm obginNo ratings yet
- Research ArticleDocument9 pagesResearch Articlesukakitkat1418No ratings yet
- 30911-Article Text-57585-1-10-20210504Document15 pages30911-Article Text-57585-1-10-20210504Team - MEDICALSERVICESNo ratings yet
- The Effect of Cesarean Section and Vaginal Delivery On Ovarian Reserve in Infertile Women (#1118806) - 2437043Document5 pagesThe Effect of Cesarean Section and Vaginal Delivery On Ovarian Reserve in Infertile Women (#1118806) - 2437043Tandyo TriasmoroNo ratings yet
- 01 M039 43754Document16 pages01 M039 43754DrDeepak PawarNo ratings yet
- Comparative Efficacy and Safety of Urate-Lowering Therapy For The Treatment of Hyperuricemia: A Systematic Review and Network Meta-AnalysisDocument13 pagesComparative Efficacy and Safety of Urate-Lowering Therapy For The Treatment of Hyperuricemia: A Systematic Review and Network Meta-AnalysisWoo Rin ParkNo ratings yet
- Management of Ovarian EndometriomaDocument13 pagesManagement of Ovarian EndometriomaAghnia PutriNo ratings yet
- Active Management of The Third Stage of Labor With.17-2Document7 pagesActive Management of The Third Stage of Labor With.17-2Maleny FloresNo ratings yet
- Anti-Aging Therapeutics Volume XIVFrom EverandAnti-Aging Therapeutics Volume XIVRating: 3 out of 5 stars3/5 (1)
- Impact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyFrom EverandImpact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health: Volume 8: Frontiers in Gynecological EndocrinologyNo ratings yet
- La Bugal V RamosDocument141 pagesLa Bugal V Ramosabo8008No ratings yet
- Distress Tolerance Handout 5 - Pros and Cons PDFDocument1 pageDistress Tolerance Handout 5 - Pros and Cons PDFRobinNo ratings yet
- TL-WN722N (UN) (US) V2 Datasheet PDFDocument4 pagesTL-WN722N (UN) (US) V2 Datasheet PDFBender :DNo ratings yet
- Bio-Valley Day Spa (Final Proposal To Submit) MDocument85 pagesBio-Valley Day Spa (Final Proposal To Submit) MAtiqah Hasan100% (4)
- Better Get 'It in Your SoulDocument4 pagesBetter Get 'It in Your SoulJeremiah AnnorNo ratings yet
- Andheri WestDocument60 pagesAndheri WestNikunj VaghasiyaNo ratings yet
- Notice 1658958950Document64 pagesNotice 1658958950Subrat NaikNo ratings yet
- Buy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlineDocument5 pagesBuy Xanax Online To Treat With Stress and Anxiety - Order Xanax OnlinelorendesuzaNo ratings yet
- B412 TM Vol 1 Bell 412 EPDocument288 pagesB412 TM Vol 1 Bell 412 EPAri100% (1)
- WikiHow Is An Online WikiDocument4 pagesWikiHow Is An Online Wikiksdnfi ouvynNo ratings yet
- Billing Reports Export 1702384478083Document82 pagesBilling Reports Export 1702384478083vinjamuriraviteja123No ratings yet
- TRP 8750DDocument276 pagesTRP 8750DKentNo ratings yet
- Optimization Module For Abaqus/CAE Based On Genetic AlgorithmDocument1 pageOptimization Module For Abaqus/CAE Based On Genetic AlgorithmSIMULIACorpNo ratings yet
- Staircase Lift Design For Elderly at HomeDocument19 pagesStaircase Lift Design For Elderly at Homesabareesh91mechNo ratings yet
- Sankaran, Mahesh - Scogings, Peter F - Savanna Woody Plants and Large Herbivores (2020, John Wiley & Sons LTD)Document781 pagesSankaran, Mahesh - Scogings, Peter F - Savanna Woody Plants and Large Herbivores (2020, John Wiley & Sons LTD)Ariadne Cristina De AntonioNo ratings yet
- Passive VoiceDocument2 pagesPassive VoiceJoseph HopperNo ratings yet
- Capr-Iii En4115 PDFDocument49 pagesCapr-Iii En4115 PDFYT GAMERSNo ratings yet
- (Lovebook care - Anh) Đề thi thử THPTQG trường THPT Chuyên Cao Bằng lần 1Document16 pages(Lovebook care - Anh) Đề thi thử THPTQG trường THPT Chuyên Cao Bằng lần 1Dương Viết ĐạtNo ratings yet
- Basic Law 01Document33 pagesBasic Law 01MitchNo ratings yet
- Seminar - Diabetes Mellitus Final VersionDocument14 pagesSeminar - Diabetes Mellitus Final Versionmustafalotfy01No ratings yet
- 1 Cyber Law PDFDocument2 pages1 Cyber Law PDFKRISHNA VIDHUSHANo ratings yet
- Java Cheat Sheet & Quick ReferenceDocument16 pagesJava Cheat Sheet & Quick Referencedad dunnoNo ratings yet
- MATH CHALLENGE GRADE 2 - Google FormsDocument5 pagesMATH CHALLENGE GRADE 2 - Google FormsAivy YlananNo ratings yet
- BMR 2105 PDFDocument6 pagesBMR 2105 PDFSitoraKodirovaNo ratings yet
- Automated Guided VehicleDocument14 pagesAutomated Guided VehicleSRI RAMNo ratings yet
- Bal Natu - Glimpses of The God-Man, Meher Baba - 1943-1948 (Vol. I) (1997)Document431 pagesBal Natu - Glimpses of The God-Man, Meher Baba - 1943-1948 (Vol. I) (1997)Kumar KNo ratings yet
- 107 Hand Tool Field Maintenance v0311Document8 pages107 Hand Tool Field Maintenance v0311rabbit_39No ratings yet
- Kult - The Dark Art PDFDocument7 pagesKult - The Dark Art PDFalnevoNo ratings yet