Professional Documents
Culture Documents
article-maps-2407
article-maps-2407
Uploaded by
Marilia InacioCopyright:
Available Formats
You might also like
- Instrument Assisted Soft Tissue MobilizationDocument5 pagesInstrument Assisted Soft Tissue MobilizationJordan QuillNo ratings yet
- CE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Document4 pagesCE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Rizky Meilynno CrisvantiknoNo ratings yet
- Nonpharmacologic Management of Pain: Scott F. Nadler, DODocument7 pagesNonpharmacologic Management of Pain: Scott F. Nadler, DOGopi KrishnanNo ratings yet
- Comparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMDocument6 pagesComparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMkrayfieldNo ratings yet
- Soft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationDocument7 pagesSoft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationfilzahNo ratings yet
- Minimizar Efeitos Adversos Com Dry NeedlingDocument12 pagesMinimizar Efeitos Adversos Com Dry NeedlingRafel FisioNo ratings yet
- Dewitte 2014Document8 pagesDewitte 2014soylahijadeunvampiroNo ratings yet
- Comparison of Radial Shockwave and Dry Needling Therapies in The Treatment of Myofascial Pain SyndromeDocument8 pagesComparison of Radial Shockwave and Dry Needling Therapies in The Treatment of Myofascial Pain SyndromeJoseph Dos SantosNo ratings yet
- Artículo Inglés I 1364Document7 pagesArtículo Inglés I 1364wuendy morenoNo ratings yet
- Best Practice For Cutaneous Manual Therapy: Adam J. Thompson, PHD, Lat, Atc Indiana Wesleyan UniversityDocument61 pagesBest Practice For Cutaneous Manual Therapy: Adam J. Thompson, PHD, Lat, Atc Indiana Wesleyan UniversityлеонидNo ratings yet
- Deep Massage TendinopathyDocument7 pagesDeep Massage Tendinopathysilvaines06No ratings yet
- Transcranial Direct Current Stimulation TDCS in M - 2024 - International JourDocument5 pagesTranscranial Direct Current Stimulation TDCS in M - 2024 - International JourRonald QuezadaNo ratings yet
- Plantar FacitisDocument20 pagesPlantar FacitisMarifatul HusnaNo ratings yet
- IJFMTDocument8 pagesIJFMTHeni KhoirunisaNo ratings yet
- The Effects of Mulligan Mobilisation With Movement and Taping Techniques On Pain, Grip Strength, and Function in Patients With Lateral EpicondylitisDocument5 pagesThe Effects of Mulligan Mobilisation With Movement and Taping Techniques On Pain, Grip Strength, and Function in Patients With Lateral EpicondylitisMawaddah SalehaNo ratings yet
- The Effects of Mulligan Mobilisation Wit PDFDocument5 pagesThe Effects of Mulligan Mobilisation Wit PDFHevin GokulNo ratings yet
- (1960) Califmed00101-0080Document4 pages(1960) Califmed00101-0080Novia RambakNo ratings yet
- A Comparison of Two Scar Massage Protocols in Pediatric Burn Survi - 2020 - BurnDocument8 pagesA Comparison of Two Scar Massage Protocols in Pediatric Burn Survi - 2020 - BurnDmytro ChopovskyiNo ratings yet
- Rehab Approach PainDocument14 pagesRehab Approach PainarmeiliaNo ratings yet
- tanach-chongkriengkrai-effectiveness-of-high-intensityDocument7 pagestanach-chongkriengkrai-effectiveness-of-high-intensityEduardo RetamaNo ratings yet
- 1756 153545044822 25Document4 pages1756 153545044822 25sonuNo ratings yet
- UggvbnuuuyDocument5 pagesUggvbnuuuyVinh TqNo ratings yet
- Massange PostburnDocument12 pagesMassange PostburnAfnes Astriani100% (1)
- International Journal of Physical Medicine & RehabilitationDocument8 pagesInternational Journal of Physical Medicine & RehabilitationfaisalNo ratings yet
- Minimizing Pain Wound CareDocument6 pagesMinimizing Pain Wound CareRizki Tri RamadaniNo ratings yet
- Use of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessDocument5 pagesUse of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessNararyo anantoNo ratings yet
- Yjmt 26 1505328Document9 pagesYjmt 26 1505328RahmatNo ratings yet
- Overview of The Management of Overuse (Persistent) TendinopathyDocument19 pagesOverview of The Management of Overuse (Persistent) TendinopathyHenrique CavagnoliNo ratings yet
- Anaesthesia - 2008 - Fischer - A Procedure Specific Systematic Review and Consensus Recommendations For PostoperativeDocument19 pagesAnaesthesia - 2008 - Fischer - A Procedure Specific Systematic Review and Consensus Recommendations For PostoperativemclimacoNo ratings yet
- A Retrospective Audit Exploring The Use of RelaxationDocument4 pagesA Retrospective Audit Exploring The Use of Relaxationmaria joseNo ratings yet
- Ijerph 20 02777Document14 pagesIjerph 20 02777Paola ClaudetNo ratings yet
- Randomized Controlled Trial of The Immediate and Long-Term Effect of Massage On Adult Postburn ScarDocument12 pagesRandomized Controlled Trial of The Immediate and Long-Term Effect of Massage On Adult Postburn ScariwanNo ratings yet
- E000514 FullDocument6 pagesE000514 FullRenan O. Pravatta PivettaNo ratings yet
- BBRC Vol 14 No 04 2021-80Document5 pagesBBRC Vol 14 No 04 2021-80Dr Sharique AliNo ratings yet
- Manipulation Under Anesthesia Versus Physiotherapy Treatment in Stage Two of A Frozen Shoulder: A Study Protocol For A Randomized Controlled TrialDocument12 pagesManipulation Under Anesthesia Versus Physiotherapy Treatment in Stage Two of A Frozen Shoulder: A Study Protocol For A Randomized Controlled TrialKristiyan winniNo ratings yet
- Use of A Simple Relaxation Technique in Burn Care Literature ReviewDocument12 pagesUse of A Simple Relaxation Technique in Burn Care Literature ReviewGuillermo923No ratings yet
- Treatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFDocument16 pagesTreatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFFranciscoJavierRoblesNo ratings yet
- Journal of Yoga & Physical TherapyDocument4 pagesJournal of Yoga & Physical Therapykhadesakshi55No ratings yet
- 105221-Article Text-284848-1-10-20140710Document6 pages105221-Article Text-284848-1-10-20140710hariNo ratings yet
- Tprelease PDFDocument6 pagesTprelease PDFtvmNo ratings yet
- EJHC Volume 11 Issue 4 Pages 566-581Document16 pagesEJHC Volume 11 Issue 4 Pages 566-581احمد العايديNo ratings yet
- 10 1179@0886963413z 0000000002Document7 pages10 1179@0886963413z 0000000002hilderhNo ratings yet
- 2018 Article 3036Document10 pages2018 Article 3036Rodrigo ValadasNo ratings yet
- Percutaneous US Guided Treatment of Shoulder Tendon CalcificationsDocument11 pagesPercutaneous US Guided Treatment of Shoulder Tendon Calcificationspepona89No ratings yet
- Webinar: Bandaging (Group A2)Document15 pagesWebinar: Bandaging (Group A2)Josie GullasNo ratings yet
- Jurnal 1Document9 pagesJurnal 1nur aisahNo ratings yet
- Clin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyDocument7 pagesClin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyNatalie JaraNo ratings yet
- Advances in The Management of Persistent Pain.110Document5 pagesAdvances in The Management of Persistent Pain.110EmaDiaconuNo ratings yet
- J JHT 2017 02 005Document8 pagesJ JHT 2017 02 005Marina UlfaNo ratings yet
- SqsqsDocument11 pagesSqsqsAnonymous RxjOeoYn9No ratings yet
- The Effectiveness of Soft Tissue Release For Healing Lower Limb InjuryDocument3 pagesThe Effectiveness of Soft Tissue Release For Healing Lower Limb InjuryVũ Đức ChínhNo ratings yet
- 4-Intermittent Versus Continuous Traction 32-1-2158Document7 pages4-Intermittent Versus Continuous Traction 32-1-2158Mohamed Serag El-deinNo ratings yet
- Heart & LungDocument8 pagesHeart & LungBella AnggitaNo ratings yet
- Cyriax Technique: Submitted To Submitted byDocument38 pagesCyriax Technique: Submitted To Submitted byAkanksha Kulvanshi100% (2)
- BMC Musculoskeletal DisordersDocument5 pagesBMC Musculoskeletal DisordersBogdan TudorNo ratings yet
- FT. en EspasticidadDocument6 pagesFT. en Espasticidadrocioag87No ratings yet
- A Note To The Musculoskeletal PhysiotherapistDocument6 pagesA Note To The Musculoskeletal PhysiotherapistDiana SchlittlerNo ratings yet
- Jurnal MassageDocument8 pagesJurnal Massagesaidah arianyNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- PT Job Description PowerbackDocument3 pagesPT Job Description Powerbackdk15janNo ratings yet
- Muscles Origin Insertion Action Location/Unique Adductors (3 Ducks Pecking Grass)Document5 pagesMuscles Origin Insertion Action Location/Unique Adductors (3 Ducks Pecking Grass)jnicolemcarthurNo ratings yet
- RandomDocument2 pagesRandomlea jumawanNo ratings yet
- IE Format 1Document9 pagesIE Format 1Alyssa GicaroNo ratings yet
- Hip FracturesDocument8 pagesHip FracturesNithu shanNo ratings yet
- Acute Pain - Marcos NCPDocument4 pagesAcute Pain - Marcos NCPArian May MarcosNo ratings yet
- Posterior Ankle Impingement 211123 - HariniDocument26 pagesPosterior Ankle Impingement 211123 - HariniharNo ratings yet
- Dr. Ramadan IbrahimDocument6 pagesDr. Ramadan IbrahimShorbanNo ratings yet
- Physical Therapy For Cerebellar AtaxiaDocument19 pagesPhysical Therapy For Cerebellar AtaxiaiOne TechNo ratings yet
- Glory's Techinical ReportDocument19 pagesGlory's Techinical ReportLoveth BethelNo ratings yet
- The Common Acute and Chronic Injuries in WrestlingDocument35 pagesThe Common Acute and Chronic Injuries in WrestlingShubham MarothiNo ratings yet
- Direct Access, Independent Practice and Scope of PracticeDocument7 pagesDirect Access, Independent Practice and Scope of Practicewasim.imiNo ratings yet
- 0 Orthotics Bhargava Et Al 2023Document11 pages0 Orthotics Bhargava Et Al 2023David MonroyNo ratings yet
- Introduction To Anatomy NMS Week 2: Catherine MooreDocument33 pagesIntroduction To Anatomy NMS Week 2: Catherine Mooreabdifatah omer100% (1)
- 2022 Clinical Pain Management 2022Document508 pages2022 Clinical Pain Management 2022rosangelaNo ratings yet
- Research Paper OverviewDocument1 pageResearch Paper Overviewapi-593661416No ratings yet
- Biomechanics of Cycling A Review 1991Document8 pagesBiomechanics of Cycling A Review 1991b.avilla9408No ratings yet
- AO Trauma Vol.2Document100 pagesAO Trauma Vol.2Cujba GheorgheNo ratings yet
- Documentation For The Physical Therapist Assistant 4th EdDocument280 pagesDocumentation For The Physical Therapist Assistant 4th Edpipit sopianNo ratings yet
- Chapter 2: Looking Back: A History of Occupational Therapy: Liceo de CagayanDocument11 pagesChapter 2: Looking Back: A History of Occupational Therapy: Liceo de CagayanDevy CaruzNo ratings yet
- Ao2019 0060Document19 pagesAo2019 0060Charlemagne Sabio GalamgamNo ratings yet
- Klem Et Al 2021 - Part 1 What Is Qualitative ResearchDocument2 pagesKlem Et Al 2021 - Part 1 What Is Qualitative ResearchNora ElaNo ratings yet
- Joint Structure and Function A Comprehensive Analysis Fifth Edition PDFDocument41 pagesJoint Structure and Function A Comprehensive Analysis Fifth Edition PDFrandy.beard30195% (42)
- Health 10 LAS Q4Document19 pagesHealth 10 LAS Q4JOSH ELORDENo ratings yet
- Seat Belt Syndrome PTH 630 Anatomy and PhysDocument7 pagesSeat Belt Syndrome PTH 630 Anatomy and Physapi-621438645No ratings yet
- EBOOK Chiropractic Technique Principles and Procedures 3Rd Edition Download Full Chapter PDF KindleDocument61 pagesEBOOK Chiropractic Technique Principles and Procedures 3Rd Edition Download Full Chapter PDF Kindlefrank.mathews913100% (44)
- Aditi Jadhav Wellness RetreatDocument17 pagesAditi Jadhav Wellness RetreatSasha BlouseNo ratings yet
- Muscle Innervation Chart IIDocument7 pagesMuscle Innervation Chart IIkimsue9448No ratings yet
- MPT Sports SyllabusDocument26 pagesMPT Sports Syllabusdr kailash jainNo ratings yet
- History 2021Document3 pagesHistory 2021api-450895824No ratings yet
article-maps-2407
article-maps-2407
Uploaded by
Marilia InacioCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
article-maps-2407
article-maps-2407
Uploaded by
Marilia InacioCopyright:
Available Formats
F A C H A R T I K E L
The right dose to the right target:
notes on hand treatment of stiffness
using mechanotherapy (MAPS Method)
Vicenç Punsola-Izard, Gemma Romera-Orfila, Aroa Casado Rodríguez
Context and Rationale: case study example, this approach address stiffness involves preventive
Stiffness is one of the most common significantly improves patient outco- measures, including protocols for
conditions treated in Hand Therapy. mes, and enables therapists to con- early mobilization and edema control
Traditionally, splinting and other mo- duct more effective and efficient ses- protocols that help to prevent the
bilization techniques of low-intensity sions. onset of stiffness (Feehan/Basset
and long-duration have been used to 2004). While this strategy can mini-
modify the length and volume of tis- Conclusion: mize the development of stiffness, it
sue restricting movement. However, The integration of progressive mobili- is not always successful in preventing
in the absence of bone deformity, zation techniques and the use of its establishment. Once stiffness is
these classic techniques often reach mechanotherapy devices represents a established, it is critical to identify the
their limits of effectiveness. significant advancement in the treat- most effective treatment strategy.
ment of hand stiffness, especially in The first challenge in treating stiffness
Methods: cases without bone deformity. This is to clearly understand how it deve-
This article proposes an innovative method not only improves the effica- lops and behaves. We know that the
method, called the MAPS (Mechano- cy of the treatment, but also optimi- initial observed loss of mobility is
therapy-Assisted Progressive and zes the efficiency of the therapeutic associated with edema and inflam-
Sequential) approach, which offers session mation. However, once this is resol-
new tools in addition to traditional ved, scar-related stiffness becomes
splinting combined with a clinical rea- Keywords: more apparent between the prolifera-
soning procedure. This approach is • Stiffness tive and maturation phases of the
based on a mechanical assessment • Contracture healing process (Rodrigues et al
that allows the therapist to determine • Arthrofibrosis 2019). This stiffness is sometimes
the ideal treatment dosage (intensi- • Pain temporary and self-limiting, and can
ty). Progressive and sequential analy- resolve spontaneously as seen in con-
tical mobilization techniques are Introduction: ditions such as frozen shoulder. In
introduced, applying low-intensity Hand stiffness is one of the main other cases, scar tissue can shorten
and long-duration doses using me- complications encountered following and thicken structures, narrow joint
chanotherapy devices. hand trauma and surgery (Akeson et spaces, and affect planes of gliding
al 1987). The management of this (Curtis 1954). In these cases, stiffness
Results: condition remains a significant chal- sets in decisively without showing
Implementation of this new method lenge due to the various factors that signs of resolving (Wong et al 2017),
has demonstrated more precise and can influence its progression. In Hand making therapy essential.
effective mobilization. Through a Therapy, the primary approach to When stiffness manifests as a clear
32 Zeitschrift für Handtherapie 1/2024
F A C H A R T I K E L
sign of movement limitation, it is treatment of stiffness in the presence field of Hand Therapy, the techniques
often accompanied by a variety of of pain is the identification of ische- that have proven to be most effective
symptoms that need to be identified mic pain. This type of pain only indi- are those employing low-intensity
and effectively neutralized. Among cates the limit of the patient's ability and long-duration mobilizations (LLPS)
these, pain is the most prominent to move and generally carries no (Light et al 1984). For this reason,
symptom and can pose a direct con- additional risks for the patient or the most therapists focus on improving
traindication to therapeutic treatment existing injury (Butler 2000). This mobility by using splints.
if not properly managed. Typically, understanding is crucial to ensure Research has shown that time is a
pain associated with stiffness is rela- that the treatment is not only safe, crucial factor in the effectiveness of
ted to tissue damage and the healing but also effective in improving the techniques aimed at improving stiff-
process. For this reason, such pain patient´s mobility and the quality of ness. This principle is known as Total
exhibits distinctly nociceptive charac- life. End Range Time (TERT), which refers
teristics, which can be associated Furthermore, it is appropriate to to the total number of daily hours
with inflammatory symptoms when apply mobilization techniques specifi- during which a constant force is app-
the tissue is highly irritated, or even cally to the structure causing the lied via a splint to modify stiffness;
ischemic symptoms when the tissue is restriction, with the explicit therapeu- the longer the time, the greater the
particularly stiff (Smart et al. 2010). tic goal of improving its kinematics daily accumulated TERT and the grea-
In addition, pain may be linked to (Michlovitz et al 2004). Sometimes, ter the improvement (Flowers/LaStayo
various complications, including neu- the stiffness may originate directly 1994; Glasgow et al 2003; Prosser
ropathic or dysfunctional disorders. In from the scarring of the injured struc- 1996; Punsola-Izard et al 2023a). Alt-
cases of neuropathic pain, it is crucial ture. In such cases, it is crucial to pro- hough relatively few studies focus on
to ensure that the irritative mecha- ceed with caution during mobiliza- the intensity of the force applied,
nism affecting the nerve is not active. tion to avoid any excessive stress that recommendations based on expert
If this mechanism has been neutrali- could further damage the affected experience suggest that modulation
zed, it is necessary to focus on redu- structure. If the stiffness is due to of intensity is crucial (Bell-Krotoski/
cing the patient's symptoms before excessive scarring also involving adja- Figarola 1995).
proceeding with other techniques cent uninjured structures, or if the Using splints that apply continuous
aimed at addressing stiffness. Someti- stiffness is in the injury but past the forces can be counterproductive if
mes, this pain may be related to a high-risk period, mobilization techni- the applied pressure is excessive, as
process of central sensitization, ma- ques can be safely applied. However, this may reduce the patient's toleran-
king it essential to recognize psycho- it is essential that these techniques be ce for using the splint (Glasgow et al
logical factors such as fear, catastro- performed with carefully controlled 2012). Therefore, splint application
phizing, and kinesiophobia, which and progressive intensities, always time should be adjusted inversely
can significantly influence pain per- respecting the limits imposed by the proportional to the pressure it exerts
ception and treatment response patient's pain level. These precau- on the skin, maintaining a careful
(Smart et al. 2010). tions ensure that the treatment is not balance to maximize both patient
In situations where pain-related com- only effective but also respects the comfort and treatment effectiveness
plications occur, an extremely cau- structural and functional integrity of (Punsola-Izard et al 2023b). When an
tious treatment approach is required, the affected area. optimal balance between pressure
although the treatment of stiffness is There is a broad consensus among and time is achieved, patients tend to
not explicitly contraindicated. specialists that traditional mobiliza- tolerate the splints better, and it is
It is essential that the patients have a tion techniques, which involve inten- possible to increase the TERT, leading
clear and complete understanding of sive mobilizations using maximum to a faster and more efficient impro-
their medical condition, and it is force and long levers, are not only vement in mobility (Punsola-Izard et
equally important to provide them ineffective in altering stiffness, but al 2023c). However, it is important to
with the necessary tools and strate- may also induce prolonged inflamma- recognize that this type of treatment
gies to effectively manage their situa- tory responses that worsen the clini- is not universally effective in all cases.
tion. A key aspect in advancing the cal situation (Light et al 1984). In the In clinical practice, there are occa-
Zeitschrift für Handtherapie 1/2024 33
F A C H A R T I K E L
involves extending the duration
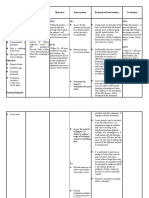
Table 1. Treatment strategies based on patient response of the treatment over time to
to mobilization therapy (Author's property) consolidate and maintain impro-
Tolerance Issue Patient Type Strategy vements in mobility, reducing the
likelihood of relapses.
No tolerance Reactive Patient Reduce symptom
Does not yield Resistant Patient Increase intensity dose The application of Total End Range
Time Treatment (TERT) (Table 2) is
Recurs Recurrent Patient Increase dose by accumulated TERT
most straightforward when stiffness
is limited to a single joint and in one
direction (Bell-Krotoski/Figarola 1995).
However, when stiffness affects a
Table 2. Distribution of Total End Range Time (TERT)
based on joint complexity (Author's property) joint in multiple directions or multiple
joints simultaneously, a more integra-
Difficulty Level in TERT
Description ted approach combining the use of
Distribution
splints and therapeutic exercises is
One joint, one direction Maximum daily TERT towards main direction
required (Midgley 2016). In these
One joint, two directions Sub-maximum daily TERT distributed cases, it is inevitable to assume the
risk of reducing daily TERT. The situa-
More than one joint Reduced TERT in multiple directions
tion becomes even more complex
when the stiffness is extensive and
involves multiple joints and tendons,
sions when, despite the use of recog- hest intensity they can tolerate, requiring a more sophisticated thera-
nized effective mobilization techni- but stiffness is not completely peutic approach (Kaplan 2010). In
ques, the expected results are not modified or only partially modi- response to these challenges, it is
achieved for a variety of specific rea- fied. These patients, known as crucial to implement therapeutic stra-
sons (Table 1): "resistant patients", require a tre- tegies that allow for an increased tre-
atment adjustment, which typi- atment dose through more analytical
1. Reactive patients: In some cases, cally involves increasing the inten- techniques. These techniques should
even at low intensities, some sity of the mobilization applica- be able to precisely target the struc-
patients do not tolerate the treat- tions. Since the TERT dose is al- tures causing stiffness to increase the
ment due to significant pain and ready maximized and cannot be effectiveness of the treatment. This
discomfort. In these situations, a increased further, the necessary approach includes managing an
further reduction in intensity and adjustment focuses on the inten- increase in treatment intensity to
duration of treatment is required. sity of the treatment to attempt directly address the affected areas
However, this change may result to overcome the stiffness resis- (Flowers 2002) and precisely reaching
in inadequate stiffness modifica- tance. the structures responsible for stiffness
tion. In these patients, identified to optimize outcomes (Cyriax 1996).
as "reactive patients", the thera- 3. Recurrent patients: There is also Achieving these objectives presents
peutic approach must focus on a group of patients who, alt- certain technical limitations. For
neutralizing the painful symptoms hough they initially respond well example, when managing numerous
to improve their ability to tolerate to treatment and show significant movement restrictions in the same
the treatment and thus allow for improvement in movement, do patient, conventional therapy ses-
more effective intervention. not maintain these results in the sions may be insufficiently short. The
long term and tend to relapse. use of techniques based on therapeu-
2. Resistant patients: Other pa- These "recurrent patients" requi- tic exercise that allow the patient to
tients may receive the maximum re a therapeutic approach that work with greater autonomy under
allowed dose of TERT at the hig- increases accumulated TERT. This the supervision of the therapist can
34 Zeitschrift für Handtherapie 1/2024
F A C H A R T I K E L
help overcome this limitation, making This order is critical to ensure that the sion, affecting one or more joints.
the treatment not only more mana- treatment is administered in a logical Muscles and tendons will produce
geable but also more efficient. This and systematic manner, addressing polyarticular deficits affecting move-
increased autonomy facilitates a the most critical areas first and pro- ment in the plane they manage and
more extensive and effective applica- gressing in a manner that maximizes will influence both passive movement
tion of the treatment in the context the effectiveness of the treatment. in the direction of stretching and acti-
of the patient's daily life, which can This step ensures that each therapy ve movement in the direction of con-
significantly contribute to improving session is meticulously planned and traction (Kilgore et al 1975). Joint-
long-term outcomes. executed with precision. Once these level dysfunctions will affect a single
three steps are completed, the thera- joint level and can have two clearly
Methodology pist is prepared to proceed with the differentiated aspects. On the one
The MAPS method (Progressive and mobilization treatment in an appro- hand, there will be retraction-like
Sequential Analytical Mobilization) is priate and effective manner. This alterations where movement restric-
an advanced approach to the treat- structured approach not only allows tions in one direction are found (Mac-
ment of hand immobility, using speci- for a more targeted and personalized Conaill/Basmajian 1969), and on the
fic techniques applied through treatment, but also maximizes the other hand, there will be conditions
mechanotherapy devices. This me- patient´s chances of functional reco- such as arthrofibrosis that create multi-
thod is particularly effective because very, allowing for faster and more directional restrictions (Usher et al
it complements and extends the tra- lasting improvements in mobility. 2019).
ditional tools used in Hand Therapy.
To effectively carry out these techni- Step One: Diagnosis Step Two: Identify the therapeutic
ques, it is essential to follow a struc- In the first step, we will conduct a moment for intervention
tured clinical reasoning process in diagnosis of the movement dysfunc- The goal of the second step is to
three fundamental phases. That sets tions of the hand. Based on the determine the appropriate treatment
the stage for the effective application patient's explanation, we will identify dose to establish a therapeutic pro-
of mobilization techniques to optimi- the pathology and determine when it gression to be applied. This progres-
ze the improvement of the patient's first occurred. From this point, we will sion is primarily related to two fac-
movement. The first step in this pro- carry out a functional assessment to tors: the biological state of the tissues
cess is the diagnosis. During this initi- understand which functional activi- and the accompanying symptoms.
al phase, the therapist assesses and ties are most altered. Finally, we will As therapists, we are familiar with
diagnoses the specific nature of the perform an analytical diagnosis to the different phases of the healing
patient's immobility. This involves a identify all the anatomical structures process and have an approximate
detailed analysis of the patient's cur- that contribute to the movement dys- understanding of the duration of
rent condition, identifying specific function. each phase and subphase. By kno-
movement deficits and possible There are many different structures wing the patient’s history and symp-
underlying causes. The second step is that can restrict movement (Kaplan tom characteristics, it is easy to deter-
to determine the appropriate treat- 2010). From superficial to deep, mine at what point in the healing
ment doses to be applied. This step these include the skin, cutaneous ner- process the therapeutic intervention
requires careful consideration of the ves, fascia, muscle, tendon, and cap- is taking place.
intensity, duration, and frequency of suloligamentous elements. Each of Based on the symptoms and signs the
the mobilization sessions, tailored these elements can cause movement patient is presenting, we can determi-
specifically to the patient´s individual restrictions with distinct characte- ne wether these symptoms or signs
needs. Determining these doses is ristics. The implementation of selecti- correspond to the actual therapeutic
crucial to ensuring that the treatment ve tension tests will allow us to preci- moment or if they are outside of the
is not only effective but also safe for sely detect the various structures con- temporal graph. If the signs or symp-
the patient. The third and final step is tributing to stiffness (Cyriax 1996). toms do not match to the phase we
to determine which specific structu- Skin and fascia will affect movement are in, we can hypothesize what is
res will be treated and in what order. globally in the direction of their ten- happening and why.
Zeitschrift für Handtherapie 1/2024 35
F A C H A R T I K E L
Nociceptive pain would be one of the Therapeutic Intervention ring the maturation phase. The pa-
main symptoms we might encounter. Once the clinical reasoning process is tient presented a with non-painful
If these symptoms do not change complete, we can begin the thera- stiffness in the metacarpophalangeal
over time, we can intervene to modi- peutic intervention. This intervention joint (MCP) extension and in the pro-
fy them, but if they persist or worsen, is carried out through therapeutic ximal interphalangeal joint (PIP) fle-
we can suspect that some kind of exercises performed on specially desi- xion. The mobility restriction was cha-
painful complication is developing. gned mechanotherapy devices. These racterized by joint-specific features,
Painful complications will be associa- devices allow us to stabilize the seg- including collateral ligament retrac-
ted with neuropathic pain or dysfunc- ments of the hand that we do not tion at the MCP and palmar plate at
tional pain. The presence of these want to move and release the seg- the PIP. The limitation being unidirec-
symptoms is not an impediment to ments that we want to mobilize. tional toward flexion at the MCP and
performing treatment per se, but Mobilization techniques can be app- extension at the PIP. The tendons
there are circumstances that require lied passively to structures that need appeared free within this range, as
adaptability on the part of the thera- to improve their movement by wor- neither proximal nor distal gliding of
pist. With this information, we can king on their flexibility and extensibili- the flexor and extensor tendons were
determine the doses necessary to ty through oscillatory mobilization symptomatic. Given the duration and
treat immobility, adapting our techni- techniques such as Maitland-like lack of improvement, the patient was
ques to the state of the tissue. exercises (Maitland 1991) or through considered a “resistant patient”. We
maintained Kaltenborn-like exercises decided to initiate low-load prolon-
Step Three: Treatment sequence (Kaltenborn 1989) performed on the ged stretch techniques to modify
In the third step, we must determine mechanotherapy devices. Active mo- stiffness and stabilize the result with
the therapeutic sequence to be used bilization techniques are used to serial splinting, The first treatment
for our patient. Both the injured address muscle contraction and pro- goal was to achieve a maximum daily
structures and the affected structures ximal tendon gliding. All these tech- Total End Range Time (TERT) on the
will be considered in this sequence. niques can be adapted in terms of MCP, addressing one direction at a
The injured structures should be pro- range, intensity, and time to the state time.
tected to facilitate their healing, al- of the tissues at any given therapeu- At the beginning of the first session,
though we can apply the maximum tic moment. These techniques are the patient showed 30 degrees of
dose of mobilization that will not jeo- performed under the supervision of MCPJ flexion. We used three techni-
pardize the integrity of the structure. the therapist, but are self-controlled ques: an elastic tension technique
The affected structures can be mobili- by the patient. This application will towards flexion, a second-level IV
zed with higher doses, taking care to allow for a reduction of in the time oscillatory technique in flexion, and a
respect the symptoms so as not to the therapist intervenes, will increase third technique involving anterior
cause painful complications. the dose of TERT, will allow effective translation of the first phalanx. This
pain management, and will reduce its resulted in an increase of 35º, rea-
Once we have identified all the perceived risk during the session ching 65° degrees of flexion at the
restrictions to be addressed, we can (Caneiro et al 2022). end of the session after 45 min,
prioritize treatment based on the which we then stabilized with a
patient's functional needs and the Results: splint.
safety of the hand. In this step, we A patient suffered a metacarpal frac- In the second session, the increase of
establish the treatment sequence for ture in November 2023 and under- mobility was maintained. We reapp-
all structures contributing to immobi- went surgical stabilization with plate lied the oscillatory translation techni-
lity and define the types of techni- and screw osteosynthesis three weeks que of the first phalanx anteriorly at
ques that will be required. We must post-injury (Fig. 1, Fig. 2 and Fig. 3). level IV, reaching 80° degrees. We
accurately assess the progression of Despite daily rehabilitation, no im- observed difficulty in the gliding of
the treatment and adapt it to chan- provement was observed at the six- the extensor tendons distally and
ges in symptoms and new therapeu- month follow-up. The healing pro- added another technique for distal
tic goals as they emerge. cess was advanced and stable, ente- gliding of the extensors in zones 5-6.
36 Zeitschrift für Handtherapie 1/2024
F A C H A R T I K E L
Fig. 1. Initial examination session Day 0: Patient with a pre-treatment Fig, 4. Beginning of the second
contracture on the MCP joint and PIP joint. treatment session a week after the
first session Day 8: Patient maintains
the results of the previous sessions
and shows a clear gain in the MCP
joint mobility.
By the end of the session, full fist clo-
sure was achieved. We stabilized the
MCP with a splint.
In the third session, we noticed a
slight loss of MCP extension of about
Fig, 2. First treatment session: Patient working during a therapy session 15 degrees, The first day we got full
using the MAPS method to correct the fifth finger limitation. From left to extension at the MCPJ. We addressed
right, we can observe the progressive placement of the MAPS pegs to achieve
this and within 10 minutes achieved
the progressive MCP joint flexion. From left to right is an elastic tension
technique, an active assisted exercise and self-range exercise. The therapist full extension without losing any fle-
can control the intensity to increase the TERT dose. xion; the extension stiffness did not
recur. We started treating the PIP
towards extension to test elasticity.
We improved from -35 degrees to
-25 degrees in 10 minutes. We fabri-
cated a PIP extension splint to be
used for four hours a day but conti-
nued to use the MCP splint without
alteration to stabilize the result and
confirm the non-recurrence of the
MCP problems.
Since the flexion of the MCPJ was
preserved by the fourth session we
Fig. 3. First treatment session: Patient after 40 min. completing the
began to work on the PIPJ. Achieving
MAPS session. The figure on the left shows the gained mobility degrees.
To maintain this improvement, a serial casting is made to keep the desired a nice intrinsic plus and intrinsic
posture in the patient. minus position.
Zeitschrift für Handtherapie 1/2024 37
F A C H A R T I K E L
Discussion:
Traditional Hand Therapy techniques,
such as early mobilization and the
use of splinting, play a crucial role in
managing many of the challenges
encountered during treatment.
However, these techniques are often
limited when faced with complex
cases. It is essential to have a clinical
Fig. 5. Second treatment session: From left to right, we can observe the progressive
reasoning process that evaluates the placement of the MAPS pegs to achieve the progressive MCP joint flexion. From left
tissues and assesses their mechanical to right is two exercises of self-range exercises for flexion of the MCP joint and
capabilities. This process enables the- then two exercises for distal gliding of the extensor tendons in zone 5-6.
rapists to be more confident in selec-
ting the most appropriate technique
for each specific case.
The incorporation of mechanothera-
py-assisted mobilization techniques
significantly expands the therapeutic
arsenal available to Hand Therapists,
offering new technical possibilities
Fig. 6. End of the second session: Fig. 7. Third treatment session two
that integrate seamlessly with exis-
Patient after completing the MAPS weeks after starting the treatment
ting methods. This synergy allows for session shows a full fist. To maintain Day 15: patient evaluation before star-
more effective therapy outcomes to this improvement, a splint is made to ting the session. The patient maintains
be achieved in less time and facilita- keep the desired posture in the the results of the previous sessions and
patient. shows a clear gain in mobility.
tes the establishment of a safer, and
more personalized exercise protocol
tailored to each patient's unique
needs.
This methodology not only makes the
treatments more effective and effi-
cient but also maximizes the produc-
tivity of each session. Continuous re-
evaluation throughout the course of Fig. 8. Third treatment session two weeks after starting the treatment:
Starting the PIPJ treatment to improve extension. From left to right passive
treatment enables therapists to provi- extension exercise, self-range exercise, passive extension obtained and elastic
de patients with a clearer prognosis tension digital neoprene orthosis to improve extension.
regarding the duration of treatment
and a more accurate prediction of
potential outcomes.
By adapting the therapy in response
to ongoing assessments, therapists
can adjust treatment strategies to
better match the patient´s evolving
condition, thereby increasing the ove-
rall effectiveness of the therapy.
Fig. 9. At three weeks full fist and full extension is obtained but treatment is not
ended more time is needed to stabilize the result.
38 Zeitschrift für Handtherapie 1/2024
F A C H A R T I K E L
Conclusions:
Hand Therapy is a broad discipline
that encompasses a variety of patho- Mit der richtigen Intensität ans Ziel:
logical scenarios and diverse thera- Anmerkungen zur Handbehandlung
peutic needs. While the current array
of techniques available to therapists
von Bewegungseinschränkungen und
is extensive, they often encounter Gewebesteifigkeit mit Hilfe der
challenging limitations, whether due
Mechanotherapie (MAPS-Methode)
to time constraints, resource availabi-
lity, or the inherent capabilities of tra-
ditional methods. In today's healthca- Kontext und Begründung: Rigidität ist eine der am häufigsten
re landscape, where insurance com- behandelten Symptome in der Handtherapie. Traditionell werden
panies are tightening budgets and Schienen und andere Mobilisierungstechniken mit geringer Intensität
reducing allotted time for therapy und langer Dauer eingesetzt, um die Länge und das Volumen des
sessions, it is imperative to explore bewegungseinschränkenden Gewebes zu verändern. Manchmal
and adopt new tools that comple- stoßen Therapeuten mit diesen klassischen Techniken jedoch an
ment existing techniques and ad- Grenzen.
equately meet patient needs.
Methoden: In diesem Artikel wird der MAPS-Ansatz (Mechano-
therapy-Assisted Progressive and Sequential) vorgestellt. Eine innova-
Mechanotherapy mobilization techni-
tive Methode, die die traditionelle Schienenbehandlung durch einen
ques offer a wealth of benefits that
neuen, klinisch erprobten Ansatz ergänzt. Dieser basiert auf einer
address these challenges: They offer
differenzierten Untersuchung, die es dem Therapeuten ermöglicht,
high precision in application, increase
die ideale Behandlungsintensität zu bestimmen. Es werden progressi-
the TERT available to patients, allow
ve, sequentielle Mobilisierungstechniken eingesetzt, bei denen Be-
for controlled adjustment of intensity
handlungen mit geringer Intensität und langer Dauer mit Hilfe von
levels, and enable patient-managed
Mechanotherapiegeräten durchgeführt werden.
therapy under professional supervi-
sion without the need for additional Ergebnisse: Diese neue Methode ermöglicht eine präzise und wirk-
therapist time. All of this is integrated same Mobilisierung. Ein Fallbeispiel zeigt, dass dieser Ansatz die
into a carefully structured clinical rea- Ergebnisse für die Patienten deutlich verbessert und es den Thera-
soning process. peuten ermöglicht, effektivere und effizientere Sitzungen durchzu-
führen.
These innovations make it possible to
provide more contemporary Hand Schlussfolgerung: Die Integration von progressiven Mobilisations-
Therapy services that meet today´s techniken und der Einsatz von Mechanotherapiegeräten stellt einen
needs. By incorporating such advan- bedeutenden Fortschritt in der Behandlung von Bewegungsein-
ced techniques, therapists can deliver schränkungen durch Gewebesteifigkeiten an der Hand und an den
more personalized and effective treat- Fingern dar, insbesondere in Fällen ohne knöcherne Deformität.
ments that are better suited to the Diese Methode verbessert nicht nur die Wirksamkeit der Behand-
evolving dynamics of healthcare deli- lung, sondern optimiert auch die Effizienz der Therapiesitzungen.
very and patient expectations. These
Schlüsselwörter:
options not only increase the efficacy
• Steifheit
of the treatments, but also improve
• Kontraktur
the efficiency of therapy sessions,
• Arthrofibrose
making it possible to achieve signifi-
cant therapeutic outcomes within • Schmerz
the constraints imposed by today's
healthcare systems.
Zeitschrift für Handtherapie 1/2024 39
F A C H A R T I K E L
Authors
Hand Therapy Barcelona
Physical Therapy and
Clinical Investigation
Center
Corresponding Author:
v.punsola@handtherapy.com
Vicenç Punsola- Gemma Romera- Aroa Casado
Izard, PhD Orfila, PT Rodríguez, PhD
Director Therapist Research Scientist
References
• Akeson WH, Amiel D, Abel MF, Garfin SR, Woo SL. • MacConaill MA, Basmajian JV. Muscles and Movements: A
Effects of immobilization on joints. Clin Orthop Relat Res. Basis for Human Kinesiology. Baltimore, MD: Williams & Wilkins
1987;(219):28-37. Co.; 1969.
• Bell-Krotoski JA, Figarola JH. Biomechanics of soft-tissue • Maitland GD. Peripheral Manipulation. 3rd ed. Boston, MA:
growth and remodeling with plaster casting. J Hand Ther. Butterworth-Heinemann; 1991.
1995;8(2):131-137. doi:10.1016/s0894-1130(12)80310-3 • Michlovitz SL, Harris BA, Watkins MP. Therapy interventions
• Butler DS. The Sensitive Nervous System. Adelaide: NOI Group for improving joint range of motion: A systematic review. J Hand
Publications; 2000. Ther. 2004;17(2):118-131. doi:10.1197/j.jht.2004.02.002
• Caneiro JP, Smith A, Bunzli S, Linton S, Moseley GL, • Midgley R. Case Report: The casting motion to mobilize stiff-
O'Sullivan P. From Fear to Safety: A Roadmap to Recovery ness technique for rehabilitation after a crush and degloving
From Musculoskeletal Pain. Phys Ther. 2022;102(2):pzab271. injury of the hand. J Hand Ther. 2016;29(3):323-333.
doi:10.1093/ptj/pzab271 doi:10.1016/j.jht.2016.03.013
• Curtis RM. Capsulectomy of the interphalangeal joints of the • Prosser R. Splinting in the management of proximal interphal-
fingers. J Bone Joint Surg Am. 1954;36-A(6):1219-1232. angeal joint flexion contracture. J Hand Ther. 1996;9(4):378-
• Cyriax JH, Cyriax PH, eds. Cyriax's Illustrated Manual of 386. doi:10.1016/s0894-1130(96)80045-7
Orthopedic Medicine. 2nd ed. Edited by Yvonne R. Burns and • Punsola-Izard V, Carnicero N, Ozaes-Lara E, et al. A Cadaver
Julie MacDonald. London, UK: WB Saunders Company Ltd; Based Comparison of Two Elastic Tension Proximal Interphalan-
Butterworth and Heinemann; 1996. ISBN 0-7020-1942-9; geal Joint (PIPJ) Extension Orthoses with Focus on Force Genera-
ISBN 0-7506-3274-4. tion and Pressure Distribution. J Clin Med. 2023;12(8):2855.
• Feehan LM, Bassett K. Is there evidence for early mobilization Published 2023 Apr 13. doi:10.3390/jcm12082855
following an extraarticular hand fracture?. J Hand Ther. • Punsola-Izard V, Casado A, Carnicero N, et al. A Comparison
2004;17(2):300-308. doi:10.1197/j.jht.2004.02.014 between Two Intervals of Daily Total End Range Time for Treat-
• Flowers KR, LaStayo P. Effect of total end range time on ment of Proximal Interphalangeal Joint Flexion Contracture
improving passive range of motion. J Hand Ther. 1994;7(3): Using an Elastic Tension Digital Neoprene Orthosis. J Clin Med.
150-157. doi:10.1016/s0894-1130(12)80056-1 2023;12(5):1987. Published 2023 Mar 2. doi:10.3390/
• Flowers KR. A proposed decision hierarchy for splinting the stiff cm12051987
joint, with an emphasis on force application parameters. J Hand • Punsola-Izard V, Schultz KS, Ozaes-Lara E, et al. Preliminary
Ther. 2002;15(2):158-162. doi: 10.1053/hanthe.2002.v15.015015 study of elastic-tension digital neoprene orthoses for proximal
• Glasgow C, Fleming J, Tooth LR, Peters S. Randomized con- interphalangeal joint flexion contracture. Hand Surg Rehabil.
trolled trial of daily total end range time (TERT) for Capener 2023;42(1):69-74. doi:10.1016/j.hansur.2022.10.006
splinting of the stiff proximal interphalangeal joint. Am J Occup • Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound
Ther. 2012;66(2):243-248. doi:10.5014/ajot.2012.002816 Healing: A Cellular Perspective. Physiol Rev. 2019;99(1):665-
• Glasgow C, Wilton J, Tooth L. Optimal daily total end range 706. doi:10.1152/physrev.00067.2017
time for contracture: resolution in hand splinting. J Hand Ther. • Smart KM, Blake C, Staines A, Doody C. Clinical indicators of
2003;16(3):207-218. doi:10.1016/s0894-1130(03)00036-x 'nociceptive', 'peripheral neuropathic' and 'central' mechanisms
• Kaltenborn FM. Manual Mobilization of the Extremity Joints: of musculoskeletal pain. A Delphi survey of expert clinicians.
Basic Examination and Treatment Techniques. 4th ed. Oslo, Man Ther. 2010;15(1):80-87. doi:10.1016/j.math. 2009.07.005
Norway: Olaf Norlis Bokhandel; 1989. • Usher KM, Zhu S, Mavropalias G, Carrino JA, Zhao J, Xu J.
• Kaplan FT. The stiff finger. Hand Clin. 2010;26(2):191-204. Pathological mechanisms, and therapeutic outlooks for arthrofi-
doi:10.1016/j.hcl.2010.02.001 brosis. Bone Res. 2019;7:9. Published 2019 Mar 26.
doi:10.1038/s41413-019-0047-x
• Kilgore ES Jr, Graham WP 3rd, Newmeyer WL, Brown LG.
The extensor plus finger. Hand. 1975;7(2):159-165. • Wong CK, Levine WN, Deo K, et al. Natural history of frozen
shoulder: fact or fiction? A systematic review. Physiotherapy.
• Light KE, Nuzik S, Personius W, Barstrom A. Low-load pro-
2017;103(1):40-47. doi:10.1016/j.physio.2016.05.009
longed stretch vs. high-load brief stretch in treating knee contrac-
tures. Phys Ther. 1984;64(3):330-333. doi:10.1093/ptj/64.3.330
40 Zeitschrift für Handtherapie 1/2024
You might also like
- Instrument Assisted Soft Tissue MobilizationDocument5 pagesInstrument Assisted Soft Tissue MobilizationJordan QuillNo ratings yet
- CE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Document4 pagesCE (Ra1) F (SHU) PF1 (PAB) PN (SHU)Rizky Meilynno CrisvantiknoNo ratings yet
- Nonpharmacologic Management of Pain: Scott F. Nadler, DODocument7 pagesNonpharmacologic Management of Pain: Scott F. Nadler, DOGopi KrishnanNo ratings yet
- Comparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMDocument6 pagesComparison and Review of Indirect Myofascial Release Therapy, IASTM, and ART To Inform CDMkrayfieldNo ratings yet
- Soft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationDocument7 pagesSoft Occlusal Splint Therapy in The Management of Myofascial Pain Dysfunction Syndrome: A Follow-Up Study in Kashmiri PopulationfilzahNo ratings yet
- Minimizar Efeitos Adversos Com Dry NeedlingDocument12 pagesMinimizar Efeitos Adversos Com Dry NeedlingRafel FisioNo ratings yet
- Dewitte 2014Document8 pagesDewitte 2014soylahijadeunvampiroNo ratings yet
- Comparison of Radial Shockwave and Dry Needling Therapies in The Treatment of Myofascial Pain SyndromeDocument8 pagesComparison of Radial Shockwave and Dry Needling Therapies in The Treatment of Myofascial Pain SyndromeJoseph Dos SantosNo ratings yet
- Artículo Inglés I 1364Document7 pagesArtículo Inglés I 1364wuendy morenoNo ratings yet
- Best Practice For Cutaneous Manual Therapy: Adam J. Thompson, PHD, Lat, Atc Indiana Wesleyan UniversityDocument61 pagesBest Practice For Cutaneous Manual Therapy: Adam J. Thompson, PHD, Lat, Atc Indiana Wesleyan UniversityлеонидNo ratings yet
- Deep Massage TendinopathyDocument7 pagesDeep Massage Tendinopathysilvaines06No ratings yet
- Transcranial Direct Current Stimulation TDCS in M - 2024 - International JourDocument5 pagesTranscranial Direct Current Stimulation TDCS in M - 2024 - International JourRonald QuezadaNo ratings yet
- Plantar FacitisDocument20 pagesPlantar FacitisMarifatul HusnaNo ratings yet
- IJFMTDocument8 pagesIJFMTHeni KhoirunisaNo ratings yet
- The Effects of Mulligan Mobilisation With Movement and Taping Techniques On Pain, Grip Strength, and Function in Patients With Lateral EpicondylitisDocument5 pagesThe Effects of Mulligan Mobilisation With Movement and Taping Techniques On Pain, Grip Strength, and Function in Patients With Lateral EpicondylitisMawaddah SalehaNo ratings yet
- The Effects of Mulligan Mobilisation Wit PDFDocument5 pagesThe Effects of Mulligan Mobilisation Wit PDFHevin GokulNo ratings yet
- (1960) Califmed00101-0080Document4 pages(1960) Califmed00101-0080Novia RambakNo ratings yet
- A Comparison of Two Scar Massage Protocols in Pediatric Burn Survi - 2020 - BurnDocument8 pagesA Comparison of Two Scar Massage Protocols in Pediatric Burn Survi - 2020 - BurnDmytro ChopovskyiNo ratings yet
- Rehab Approach PainDocument14 pagesRehab Approach PainarmeiliaNo ratings yet
- tanach-chongkriengkrai-effectiveness-of-high-intensityDocument7 pagestanach-chongkriengkrai-effectiveness-of-high-intensityEduardo RetamaNo ratings yet
- 1756 153545044822 25Document4 pages1756 153545044822 25sonuNo ratings yet
- UggvbnuuuyDocument5 pagesUggvbnuuuyVinh TqNo ratings yet
- Massange PostburnDocument12 pagesMassange PostburnAfnes Astriani100% (1)
- International Journal of Physical Medicine & RehabilitationDocument8 pagesInternational Journal of Physical Medicine & RehabilitationfaisalNo ratings yet
- Minimizing Pain Wound CareDocument6 pagesMinimizing Pain Wound CareRizki Tri RamadaniNo ratings yet
- Use of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessDocument5 pagesUse of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessNararyo anantoNo ratings yet
- Yjmt 26 1505328Document9 pagesYjmt 26 1505328RahmatNo ratings yet
- Overview of The Management of Overuse (Persistent) TendinopathyDocument19 pagesOverview of The Management of Overuse (Persistent) TendinopathyHenrique CavagnoliNo ratings yet
- Anaesthesia - 2008 - Fischer - A Procedure Specific Systematic Review and Consensus Recommendations For PostoperativeDocument19 pagesAnaesthesia - 2008 - Fischer - A Procedure Specific Systematic Review and Consensus Recommendations For PostoperativemclimacoNo ratings yet
- A Retrospective Audit Exploring The Use of RelaxationDocument4 pagesA Retrospective Audit Exploring The Use of Relaxationmaria joseNo ratings yet
- Ijerph 20 02777Document14 pagesIjerph 20 02777Paola ClaudetNo ratings yet
- Randomized Controlled Trial of The Immediate and Long-Term Effect of Massage On Adult Postburn ScarDocument12 pagesRandomized Controlled Trial of The Immediate and Long-Term Effect of Massage On Adult Postburn ScariwanNo ratings yet
- E000514 FullDocument6 pagesE000514 FullRenan O. Pravatta PivettaNo ratings yet
- BBRC Vol 14 No 04 2021-80Document5 pagesBBRC Vol 14 No 04 2021-80Dr Sharique AliNo ratings yet
- Manipulation Under Anesthesia Versus Physiotherapy Treatment in Stage Two of A Frozen Shoulder: A Study Protocol For A Randomized Controlled TrialDocument12 pagesManipulation Under Anesthesia Versus Physiotherapy Treatment in Stage Two of A Frozen Shoulder: A Study Protocol For A Randomized Controlled TrialKristiyan winniNo ratings yet
- Use of A Simple Relaxation Technique in Burn Care Literature ReviewDocument12 pagesUse of A Simple Relaxation Technique in Burn Care Literature ReviewGuillermo923No ratings yet
- Treatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFDocument16 pagesTreatment of Tendinopathy What Works, What Does Not, and What Is On The Horizon PDFFranciscoJavierRoblesNo ratings yet
- Journal of Yoga & Physical TherapyDocument4 pagesJournal of Yoga & Physical Therapykhadesakshi55No ratings yet
- 105221-Article Text-284848-1-10-20140710Document6 pages105221-Article Text-284848-1-10-20140710hariNo ratings yet
- Tprelease PDFDocument6 pagesTprelease PDFtvmNo ratings yet
- EJHC Volume 11 Issue 4 Pages 566-581Document16 pagesEJHC Volume 11 Issue 4 Pages 566-581احمد العايديNo ratings yet
- 10 1179@0886963413z 0000000002Document7 pages10 1179@0886963413z 0000000002hilderhNo ratings yet
- 2018 Article 3036Document10 pages2018 Article 3036Rodrigo ValadasNo ratings yet
- Percutaneous US Guided Treatment of Shoulder Tendon CalcificationsDocument11 pagesPercutaneous US Guided Treatment of Shoulder Tendon Calcificationspepona89No ratings yet
- Webinar: Bandaging (Group A2)Document15 pagesWebinar: Bandaging (Group A2)Josie GullasNo ratings yet
- Jurnal 1Document9 pagesJurnal 1nur aisahNo ratings yet
- Clin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyDocument7 pagesClin Psychology and Psychoth - 2017 - Durá Ferrandis - Confirming The Mechanisms Behind Cognitive Behavioural TherapyNatalie JaraNo ratings yet
- Advances in The Management of Persistent Pain.110Document5 pagesAdvances in The Management of Persistent Pain.110EmaDiaconuNo ratings yet
- J JHT 2017 02 005Document8 pagesJ JHT 2017 02 005Marina UlfaNo ratings yet
- SqsqsDocument11 pagesSqsqsAnonymous RxjOeoYn9No ratings yet
- The Effectiveness of Soft Tissue Release For Healing Lower Limb InjuryDocument3 pagesThe Effectiveness of Soft Tissue Release For Healing Lower Limb InjuryVũ Đức ChínhNo ratings yet
- 4-Intermittent Versus Continuous Traction 32-1-2158Document7 pages4-Intermittent Versus Continuous Traction 32-1-2158Mohamed Serag El-deinNo ratings yet
- Heart & LungDocument8 pagesHeart & LungBella AnggitaNo ratings yet
- Cyriax Technique: Submitted To Submitted byDocument38 pagesCyriax Technique: Submitted To Submitted byAkanksha Kulvanshi100% (2)
- BMC Musculoskeletal DisordersDocument5 pagesBMC Musculoskeletal DisordersBogdan TudorNo ratings yet
- FT. en EspasticidadDocument6 pagesFT. en Espasticidadrocioag87No ratings yet
- A Note To The Musculoskeletal PhysiotherapistDocument6 pagesA Note To The Musculoskeletal PhysiotherapistDiana SchlittlerNo ratings yet
- Jurnal MassageDocument8 pagesJurnal Massagesaidah arianyNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- PT Job Description PowerbackDocument3 pagesPT Job Description Powerbackdk15janNo ratings yet
- Muscles Origin Insertion Action Location/Unique Adductors (3 Ducks Pecking Grass)Document5 pagesMuscles Origin Insertion Action Location/Unique Adductors (3 Ducks Pecking Grass)jnicolemcarthurNo ratings yet
- RandomDocument2 pagesRandomlea jumawanNo ratings yet
- IE Format 1Document9 pagesIE Format 1Alyssa GicaroNo ratings yet
- Hip FracturesDocument8 pagesHip FracturesNithu shanNo ratings yet
- Acute Pain - Marcos NCPDocument4 pagesAcute Pain - Marcos NCPArian May MarcosNo ratings yet
- Posterior Ankle Impingement 211123 - HariniDocument26 pagesPosterior Ankle Impingement 211123 - HariniharNo ratings yet
- Dr. Ramadan IbrahimDocument6 pagesDr. Ramadan IbrahimShorbanNo ratings yet
- Physical Therapy For Cerebellar AtaxiaDocument19 pagesPhysical Therapy For Cerebellar AtaxiaiOne TechNo ratings yet
- Glory's Techinical ReportDocument19 pagesGlory's Techinical ReportLoveth BethelNo ratings yet
- The Common Acute and Chronic Injuries in WrestlingDocument35 pagesThe Common Acute and Chronic Injuries in WrestlingShubham MarothiNo ratings yet
- Direct Access, Independent Practice and Scope of PracticeDocument7 pagesDirect Access, Independent Practice and Scope of Practicewasim.imiNo ratings yet
- 0 Orthotics Bhargava Et Al 2023Document11 pages0 Orthotics Bhargava Et Al 2023David MonroyNo ratings yet
- Introduction To Anatomy NMS Week 2: Catherine MooreDocument33 pagesIntroduction To Anatomy NMS Week 2: Catherine Mooreabdifatah omer100% (1)
- 2022 Clinical Pain Management 2022Document508 pages2022 Clinical Pain Management 2022rosangelaNo ratings yet
- Research Paper OverviewDocument1 pageResearch Paper Overviewapi-593661416No ratings yet
- Biomechanics of Cycling A Review 1991Document8 pagesBiomechanics of Cycling A Review 1991b.avilla9408No ratings yet
- AO Trauma Vol.2Document100 pagesAO Trauma Vol.2Cujba GheorgheNo ratings yet
- Documentation For The Physical Therapist Assistant 4th EdDocument280 pagesDocumentation For The Physical Therapist Assistant 4th Edpipit sopianNo ratings yet
- Chapter 2: Looking Back: A History of Occupational Therapy: Liceo de CagayanDocument11 pagesChapter 2: Looking Back: A History of Occupational Therapy: Liceo de CagayanDevy CaruzNo ratings yet
- Ao2019 0060Document19 pagesAo2019 0060Charlemagne Sabio GalamgamNo ratings yet
- Klem Et Al 2021 - Part 1 What Is Qualitative ResearchDocument2 pagesKlem Et Al 2021 - Part 1 What Is Qualitative ResearchNora ElaNo ratings yet
- Joint Structure and Function A Comprehensive Analysis Fifth Edition PDFDocument41 pagesJoint Structure and Function A Comprehensive Analysis Fifth Edition PDFrandy.beard30195% (42)
- Health 10 LAS Q4Document19 pagesHealth 10 LAS Q4JOSH ELORDENo ratings yet
- Seat Belt Syndrome PTH 630 Anatomy and PhysDocument7 pagesSeat Belt Syndrome PTH 630 Anatomy and Physapi-621438645No ratings yet
- EBOOK Chiropractic Technique Principles and Procedures 3Rd Edition Download Full Chapter PDF KindleDocument61 pagesEBOOK Chiropractic Technique Principles and Procedures 3Rd Edition Download Full Chapter PDF Kindlefrank.mathews913100% (44)
- Aditi Jadhav Wellness RetreatDocument17 pagesAditi Jadhav Wellness RetreatSasha BlouseNo ratings yet
- Muscle Innervation Chart IIDocument7 pagesMuscle Innervation Chart IIkimsue9448No ratings yet
- MPT Sports SyllabusDocument26 pagesMPT Sports Syllabusdr kailash jainNo ratings yet
- History 2021Document3 pagesHistory 2021api-450895824No ratings yet