Professional Documents
Culture Documents
Knoe Rns Child 2000
Knoe Rns Child 2000
Uploaded by
Rafaelly CubasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Knoe Rns Child 2000
Knoe Rns Child 2000
Uploaded by
Rafaelly CubasCopyright:
Available Formats
Periodontal tissue responses after insertion of artificial crowns and fixed
partial dentures
Kent L. Knoernschild, DMD, MS,a and Stephen D. Campbell, DDS, MMScb
College of Dentistry, University of Illinois at Chicago, Chicago, Ill.
Purpose. The purpose of this review was, first, to critically evaluate published evidence on the effects of
artificial crowns and fixed partial dentures (FPDs) on adjacent periodontal tissue health, and second to
synthesize this evidence into meaningful summaries. Restoration qualities that contribute to inflammatory
responses were identified based on strength of evidence, and variables that should be controlled in future
investigations were outlined. Such information is necessary to accurately predict the prognosis of peri-
odontal tissues adjacent to crowns or FPDs.
Methods. Clinical trial and epidemiologic evidence published in English was collected. The effects of
crowns or FPDs on gingival inflammation, probing depths, and bone loss were evaluated based on accu-
racy of measurement, reliability of measurement, and/or appropriateness of data analysis.
Results. Crowns and FPDs increased the incidence of advanced gingival inflammation adjacent to
restorations, particularly if restorations had intracrevicular finish line placement, poor marginal adaptation,
or rough surfaces. However, because of the limitation in the accuracy and reliability of probing depth
measurements, reports of greater mean probing depths of crowned teeth, which tended to be less than
1 mm greater than control teeth, should be questioned. Finally, crowns and FPDs in general did not
accelerate the rate of adjacent bone loss.
Conclusion. Clinically deficient restorations, as well as clinically acceptable restorations, can contribute
to gingival inflammation. However, with the limitations of the applied methods of measurement, current
evidence has not shown an increased attachment loss adjacent to crowns or FPDs. Future trials should
document periodontal health before therapy and periodically after restoration insertion so that each tooth
serves as its own control. In future studies, the periodontal disease history of the patient, the influence of
the restoration on plaque formation, and the composition of the crevicular microflora must be recorded.
(J Prosthet Dent 2000;84:492-8.)
CLINICAL IMPLICATIONS
Gingivitis may develop after insertion of questionable restorations, as well as appro-
priately contoured, highly polished crowns or FPDs with well-adapted, intracrevicular
margins, but severity in response differs among patients. Specific reasons for develop-
ment of inflammation have been difficult to discern because of the diversity in
investigative design among studies. Well-controlled, clinical trials and epidemiologic
studies should be performed to further determine fundamental reasons for advanced
periodontal inflammation in some patients. Clinicians will then be able to accurately
predict the prognosis of periodontal tissues adjacent to crowns or fixed partial dentures.
T he goal of the prosthodontist is to control oral
disease while restoring esthetics and function with
the available evidence, which includes published clini-
cal trials, anecdotal reports from peers, and personal
durable, biocompatible restorations. Knowledge of the clinical experiences. Critical evaluation of evidence
responses of periodontal tissues to artificial crowns and should be included in the decision-making processes
fixed partial dentures (FPDs) is crucial in the develop- for a predictable result.
ment of treatment plans with predictable prognoses. Clinical research has focused on the effect of indi-
During diagnosis, treatment planning, and active ther- rect restorations on periodontal tissues. Studies have
apy, each patient’s needs must be considered in light of reported that poor marginal adaptation,1-8 deeper
intracrevicular margin placement,9-22 rougher restoration
Presented at the American Academy of Fixed Prosthodontics Annual
surfaces,23-30 and overcontoured restorations31-35 can
Meeting, February 19, 1999. contribute to localized periodontal inflammation.
aAssociate Professor, Department of Restorative Dentistry. Inflammation commonly develops because these
bProfessor and Head, Department of Restorative Dentistry.
restorations can provide a protected environment in
492 THE JOURNAL OF PROSTHETIC DENTISTRY VOLUME 84 NUMBER 5
KNOERNSCHILD AND CAMPBELL THE JOURNAL OF PROSTHETIC DENTISTRY
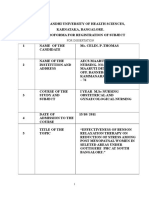
Fig. 1. Gingival index score incidence in crowned and control teeth (Bader et al20).
which the indigenous microbial population matures form among the studies, important conclusions can
into a more periodontopathic flora.33 These studies be garnered from this body of evidence that elevates
have forced clinicians and researchers to focus on the one’s awareness of how periodontal tissues respond to
fundamental qualities of crowns or FPDs during fabri- fixed prosthodontic restorations.
cation that reduce the restoration’s contribution to The following sections present a critical evalua-
gingival inflammation. tion of the literature regarding the response of
The clinician must have a clear understanding of the periodontal tissues to artificial crowns and FPDs.
clinical trial or the epidemiologic study design to state Results of clinical trials and epidemiologic studies in
confidently that restorations can adversely affect tis- humans that evaluated the degree of gingival inflam-
sues. Trials have commonly started approximately 1 mation and attachment loss after crown placement
month after insertion of the artificial crown, and teeth are discussed. Studies are limited to those published
with crowns were evaluated using surrogate measures in English, and the evidence is synthesized into con-
such as probing depths, radiographically determined cise, comprehensive summaries based on surrogate
alveolar bone levels, and gingival index scores. Similar measure precision, surrogate measure reliability,
measurements were also made on each patient’s con- and/or appropriateness of data analysis. Suggestions
tralateral tooth as the control. Means and standard are also proposed that apply to the development of
deviations of restored and control groups were usually future studies that address periodontal tissue
reported, and additional statistical analyses were per- responses to restorations.
formed to determine differences among groups.
INFLAMMATION AFTER CROWN OR
Epidemiologic studies reported data in a similar way,
FPD PLACEMENT
but the dates of restoration insertion were not known.
Most studies exhibit similar basic designs, but Most studies concluded that artificial crowns and
diversity in approach to determine the influence of FPDs could contribute to periodontal inflammation.
crowns or FPDs on periodontal tissue health has Statistically significant differences in mean scores
made meaningful synthesis of the evidence difficult. between a restored tooth and contralateral control
Investigations varied with respect to selection of teeth were observed in many patient populations using
patients and types of restorations evaluated. the Loe and Silness36 Gingival Index (GI) scale.
Moreover, 2 factors that could adversely influence the Clinical trial and epidemiologic investigations consis-
periodontal response, the degree of marginal adapta- tently reported mean restored tooth GI scores greater
tion and the intracrevicular depth of the preparation than mean GI scores for control groups. Differences
finish line, were not reported in most studies. between mean restored and control tooth groups were
Although control of important variables was not uni- as great as 0.90 units.12
NOVEMBER 2000 493
THE JOURNAL OF PROSTHETIC DENTISTRY KNOERNSCHILD AND CAMPBELL
Fig. 2. Gingival index score incidence in crowned and control teeth (Valderhaug et al22).
Number of teeth exhibiting index scores of “2” or “3” are presented to allow for comparisons
of incidence of more advanced gingival inflammation over 15 years.
SUMMARY
The methods of statistical analyses in many studies
biased the interpretation of results. GI scores were Artificial crowns and FPDs increased the incidence
ordinal data, meaning that increasing index score cor- of advanced gingival inflammation. Moreover, studies
related with increasing inflammation recognized by have shown that mean crowned tooth GI scores are
specific criteria. However, because the data were not consistently greater than mean control tooth scores,
continuous, a score of 2 did not indicate that the peri- which further supported that trend. Restoration fac-
odontal tissue was twice as inflamed as tissues with a tors such as intracrevicular margin placement, poor
score of 1. Therefore, reporting calculation of GI score margin adaptation, poor restoration contours, and
means and standard deviations, which is better suited for restoration surface roughness were frequently associated
interval or ratio scale data, was not necessarily appropri- with inflammation.
ate. In addition, the “statistically significant” mean
ATTACHMENT LOSS AFTER CROWN
differences reported in studies that were as small as 0.2
PLACEMENT
index units cannot be recognized clinically. Finally, just
as means and mean differences between groups should Accelerated loss of alveolar bone height or an
be reported with the same significance as raw data, cal- increase in probing depths compared with other teeth
culated differences should have been reported as in a dentition could indicate that restoration fabrica-
whole numbers. tion procedures or the restoration itself contributed to
Perhaps the most meaningful method to describe injury of periodontal architecture. Pihlstrom37 stated
associations between gingival inflammation and crown that in long-term clinical trials of periodontal health,
placement was by reporting frequencies of index scores. the radiographically determined attachment level
Valderhaug et al22 reported frequencies after a 15-year should be the primary focus, but probing depths
clinical trial (Fig. 1), and one can easily appreciate that should be recorded. The following sections present
crowned teeth more frequently exhibited GI scores of studies that address how crowns affected probing
2 and 3 compared with control teeth. A similar depths and alveolar bone loss.
approach was used in the Bader et al 20 epidemio-
PROBING DEPTHS
logic study (Fig. 2), and trends that corroborated the
evidence of Valderhaug et al were observed. In the Trials9,10,13-17,19,20,22 in which patients were fol-
Bader et al study, baseline data were not reported, lowed up for as long as 15 years after the insertion of
whereas in the Valderhaug et al trial, baseline data were crowns or FPDs reported mean crowned tooth prob-
collected after crown insertion. No studies have recorded ing depths 0.05 to 0.5 mm greater than mean control
each patient’s periodontal status before crown or FPD depths. Mean probing depth increases could be com-
insertion and linked the initial periodontal tissue con- pared over time because these studies tracked probing
dition to the response after restoration insertion. depth changes from known dates of insertion. In general,
494 VOLUME 84 NUMBER 5
KNOERNSCHILD AND CAMPBELL THE JOURNAL OF PROSTHETIC DENTISTRY
mean crowned tooth probing depths of 0.1 to 0.2 mm these reports must be evaluated individually on the
greater than mean control depths were frequently basis of each study’s research design. The lack of con-
reported. No studies reported mean crowned tooth trol of experimental variables and the use of
probing depths significantly less than those of teeth questionable controls in some studies diminished the
not restored. credence of their conclusions. Moreover, because an
Although these studies reported similar results, they examiner’s accuracy in evaluating probing depths is
had different research designs. Careful control of ±1 mm, commonly reported mean changes in prob-
numerous variables such as initial health of the peri- ing depth of 0.2 mm have limited clinical meaning, as
odontium, occlusogingival position of the finish line, the changes were within the error of probing depth
contour of the restoration, and adaptation of the measurements.
restoration margin are critical for accurate assessment
BONE LOSS
of probing depth outcomes. Not all studies reported
methods that controlled these and other patient selec- Change in periodontal probing depths or in radio-
tion variables. Therefore, because of the lack of graphic bone height should be used separately and in
uniformity in inclusion criteria among studies, a state- combination43 for the determination of attachment
ment that crowns cause increased probing depths has loss. Visual interpretation, direct measurement, or dig-
been inappropriate. Diversity in research designs dis- ital image analysis can identify radiographically
guised the factor(s) that has had the most influence. determined alveolar bone loss. The most precise mea-
A lack of uniformity also existed in establishment of surement of bone loss has been determined through
control teeth among studies. In many studies, control standardized radiographs, which permit measurement
teeth were similar contralateral teeth. Sometimes the of changes as small as 0.2 mm when computerized
control was previously restored with a direct restora- methods are used.44
tion. In other studies, caries developed in the control, Attachment loss after crown placement has been
which was restored during the trial but remained in reported in longitudinal studies13,16,17,19,22 with clini-
the control group. The influence of the control groups cal data that extended from 1 to 15 years. Attachment
on observed differences in probing depths is uncertain loss was reported using probing depth measure-
because directly restored teeth in some studies served ments or radiographic examinations, but these
as controls. Previously reported minute differences in studies did not use the precise computerized method.
probing depth changes after crown insertion could Investigators who used probing depths reported
have been greater if controls remained unrestored. means and standard deviations by making measure-
Conversely, with carefully selected controls and con- ments from the crown margins to the depth of the
trolled experimental variables, minimal differences sulcus. Studies that used radiograph measurements did
between crowned and control tooth groups may have not report data in such detail, but they presumably
been observed. measured interproximally from radiographic crown
A third consideration relates to accuracy of probing margin to alveolar crest. These studies reported mean
depth measurement techniques. A mean increase in attachment losses ranging from 0.15 to 1.3 mm dur-
probing depths after artificial crown insertion of 0.1 to ing trial periods, which can be calculated to a reported
0.2 mm was often reported and could be meaningful. loss of 0.04 and 0.24 mm per year.
However, this should be interpreted in light of mea- One longitudinal report22 recorded no difference in
surement accuracy. Variations in probing force, size incidence of crowned or control teeth that developed 0 to
and shape of tip, location of tip placement, detection 1 mm horizontal bone loss or 1 to 2 mm horizontal
of reference landmarks for attachment level probing, bone loss. The lack of increase in bone loss after crown
and degree of gingival inflammation could adversely insertion is also corroborated by the comparison of
influence accuracy.38 Moreover, error in conventional studies that evaluated crowned teeth to other studies in
probing measurements can be 0.5 mm or greater39 which crowned teeth were not the investigative focus.
with errors depending on pocket depth, tooth, site Several studies45-48 reported alveolar bone resorption
location, and patient.40 Finally, probes of the same in controlled periodontal patients of 0.03 to 0.07 per
design and batch from the manufacturer have varied in year. These reports did not assess differences in
marking placement by as much as 0.5 mm.41 crowned versus unrestored teeth, and one could
Therefore, only probing depths that have increased assume that both types were present in the patient pop-
more than 1 mm should serve as a diagnostic test with ulations. Evidence also suggested that crowns did not
high sensitivity and specificity.42 increase the rate of bone loss because attachment loss
between these 2 groups of studies was similar.
SUMMARY
Other factors could influence attachment loss after
Although mean probing depth increases after artifi- insertion of crowns or FPDs. Valderhaug and
cial crown or FPD placement were often reported, Birkeland13 reported an accelerated rate of attachment
NOVEMBER 2000 495
THE JOURNAL OF PROSTHETIC DENTISTRY KNOERNSCHILD AND CAMPBELL
loss during the first 2 years after crown insertion. crowned teeth may have a greater incidence of
These results suggested that factors related to crown advanced gingival inflammation. However, studies
fabrication could contribute to increased attachment have not confirmed that gingival tissues consistently
loss. Albandar et al49 have reported that, in descend- developed an increase in inflammation after crown
ing order of importance, that tooth type, initial bone insertion. Teeth generally have received extensive
level, age, sex, calculus, restoration margins, and prox- direct restorative therapy that included intracrevicular
imal surface are responsible for only 20% of the restorations before crown therapy. Amalgam or com-
variance leading to alveolar bone loss. Thus, many fac- posite restorations could contribute to gingival
tors could be influential, and future, well-controlled inflammation before fixed prosthodontic therapy that
studies should address these issues in detail. would not resolve after crown or FPD insertion. In
fact, removal of caries and the replacement of poorly
SUMMARY
contoured or poorly adapted direct restorations with
Evidence has not shown that artificial crown or well-fabricated crowns or FPDs could improve peri-
FPD insertion results in accelerated bone loss. odontal tissue health. Therefore, before fixed
Investigators have reported that the distance from the prosthodontic therapy, future clinical investigations
crown margin to the probed depth of the sulcus or the should document the tooth’s restorative history and
distance from the crown margin to the radiographic initial periodontal status as contributing variables so
alveolar bone level increased over time. However, that each crowned tooth serves as its own control.
mean attachment loss in crowned teeth was similar to A fourth consideration relates to the limited infor-
loss observed with control teeth. mation available regarding the effects that preparation,
tissue retraction, impression, provisionalization, and
FUTURE RESEARCH
luting procedures have on periodontal health. This
Although investigators have focused mainly on broad-based consideration is complicated and difficult
restoration qualities and biomaterial properties to to control because one procedure must be completed
improve tissue responses adjacent to restored teeth, immediately after the last. If a tooth is prepared for a
other factors not related to the restoration could be crown, impressed, and provisionally restored, one can-
more critical. For example, the history of the patient’s not determine which of the previous procedures
periodontal disease before therapy could be a contrib- contributed to the inflammation that might develop.
utor to periodontal inflammation that develops after Moreover, with clinical trials, baseline gingival index
crown or FPD insertion. Previous trials and epidemio- scores collected after crown insertion could represent
logic studies have not reported the patient’s only partial resolution of inflammation that developed
periodontal disease background, which could influ- from previous procedures. This further underscores
ence observed gingival inflammation, probing depths, the importance of tracking the periodontal health of
or attachment loss throughout a study. Future clinical individual teeth before the initiation of therapy.
trials should include this history as a contributing vari- Finally, the influence of restorative materials on peri-
able. If greater inflammation and/or recession were odontal health must be considered. Biomaterials must
expected because of the patient’s history, the clinician be developed with low surface-free energies, as higher
could better predict final tissue responses before the surface energy materials such as casting alloys and
initiation of therapy. ceramics may lead to greater plaque adherence and mat-
The indigenous microbial flora composition and the uration.28,50-52 The degree of in vivo plaque formation
patient’s response to toxins produced by that flora are differs among materials.53-55 Therefore, a fundamental
probably important contributors to periodontal health understanding of initial pellicle biofilm formation,
during and after therapy. If a cast restoration has pro- which influences initial bacterial adhesion through spe-
vided a protected environment in which a pathogenic cific and nonspecific mechanisms,56-61 is necessary. In
flora can develop, patients with a more aggressive addition, bacterial toxins adhere to a variety of restora-
indigenous flora could have greater inflammation devel- tive materials,62-65 and a greater understanding must be
op. However, inflammation could occur only if a patient developed regarding bacterial toxin contribution to
were not resistant to the pathogenic flora’s metabolic biofilm formation and bacterial adhesion.
products. Considerable research has been conducted The influences of restorative materials on the
regarding immunologic responses to periodontal mature crevicular microflora composition could be
pathogens, and further research is needed relating to the critical because microflora composition beneath porce-
pathogenesis of periodontal inflammation. lain pontics adjacent to inflamed tissues differed from
The restoration history of a specific tooth before microflora beneath alloy pontics adjacent to inflamed
fixed prosthodontic therapy is likely to be a third vari- tissues.66 Clinicians and researchers are expected to
able that contributes to alveolar bone resorption.49 develop a more fundamental understanding of how
Trial and epidemiologic evidence have suggested that restorative materials influence the crevicular environ-
496 VOLUME 84 NUMBER 5
KNOERNSCHILD AND CAMPBELL THE JOURNAL OF PROSTHETIC DENTISTRY
ment. New biocompatible materials can then be devel- tions in patients treated with removable partial dentures and artificial
oped that favorably influence the microflora crowns. A longitudinal two-year study. Acta Odontol Scand 1971;29:621-
38.
composition for periodontal health. 11. Larato DC. Effects of artificial crown margin extension and tooth brush-
ing frequency on gingival pocket depth. J Prosthet Dent 1975;34:640-3.
CONCLUSIONS 12. Newcomb GM. The relationship between the location of subgingival
crown margins and gingival inflammation. J Periodontol 1974;45:151-4.
Evidence suggests that restoration factors such as 13. Valderhaug J, Birkeland JM. Periodontal conditions in patients 5 years
poor margin adaptation, intracrevicular margin place- following insertion of fixed prostheses. Pocket depth and loss of attach-
ment, rough surfaces, and overcontouring could ment. J Oral Rehabil 1976;3:237-43.
14. Valderhaug J, Heloe LA. Oral hygiene in a group of supervised patients
contribute to localized gingival inflammation, with fixed prostheses. J Periodontol 1977;48:221-4.
increased probing depths, and bone resorption. 15. Jameson LM. Comparison of the volume of crevicular fluid from restored
Crown insertion increased the incidence of advanced and non-restored teeth. J Prosthet Dent 1979;41:209-14.
16. Valderhaug J. Periodontal conditions and carious lesions following the
gingival inflammation adjacent to restorations. insertion of fixed prostheses: a 10-year follow-up study. Int Dent J
However, because of the limitation in accuracy of 1980;30:296-304.
probing depth measurements, commonly reported 17. Muller HP. The effect of artificial crown margins at the gingival margin
on the periodontal conditions in a group of periodontally supervised
greater mean probing depths of crowned teeth com- patients treated with fixed bridges. J Clin Periodontol 1986;13:97-102.
pared with control teeth should be questioned. 18. Orkin DA, Reddy J, Bradshaw D. The relationship of the position of
Horizontal bone loss was not accelerated after crown crown margins to gingival health. J Prosthet Dent 1987;57:421-4.
19. Reichen-Graden S, Lang NP. Periodontal and pulpal conditions of abut-
placement. ment teeth. Status after four to eight years following the incorporation of
Although studies have reported a greater incidence fixed reconstructions. Schweiz Monatsschr Zahnmed 1989;99:1381-5.
of gingival inflammation adjacent to crowns, studies 20. Bader JD, Rozier RG, McFall WT Jr, Ramsey DL. Effect of crown margins
on periodontal conditions in regularly attending patients. J Prosthet Dent
have not documented an increase in inflammation 1991;65:75-9.
compared with periodontal status before the insertion 21. Freilich MA, Niekrash CE, Katz RV, Simonsen RJ. Periodontal effects of
of crowns or FPDs. Every tooth accumulates a unique fixed partial denture retainer margins: configuration and location. J
Prosthet Dent 1992;67:184-90.
restorative history, so future trials should document 22. Valderhaug J, Ellingsen JE, Jokstad A. Oral hygiene, periodontal condi-
periodontal health before crown therapy and periodi- tions and carious lesions in patients treated with dental bridges. A
cally after crown insertion. Each tooth would then 15-year clinical and radiographic follow-up study. J Clin Periodontol
1993;20:482-9.
serve as its own control. Future studies should also 23. Waerhaug J. Effect of rough surfaces upon gingival tissue. J Dent Res
document the periodontal disease history of the 1956;35:323.
patient as well as the influence of the restoration on 24. Schwarz ML, Phillips RW. Comparison of bacterial accumulations on
rough and smooth enamel surfaces. J Periodontol 1957;28:304-7.
pellicle formation, plaque formation, and microflora 25. Mormann W, Regolati B, Renggli HH. Gingival reaction to well-fitted
composition. These considerations will improve the subgingival proximal gold inlays. J Clin Periodontol 1974;1:120-5.
understanding of the influences of crowns and FPDs 26. Keenan MP, Shillingburg HT Jr, Duncanson MG Jr, Wade CK. Effects of
cast gold surface finishing on plaque retention. J Prosthet Dent
on periodontal health such that the clinician can 1980;43:168-73.
obtain the most predictable periodontal tissue 27. Shafagh I. Plaque accumulation on cast gold complete crowns polished
response after restoration insertion. by a conventional and an experimental method. J Prosthet Dent
1986;55:339-42.
28. Quirynen M, Marechal M, Busscher HJ, Weerkamp AH, Darius PL, van
Steenberghe D. The influence of surface free energy and surface rough-
REFERENCES
ness on early plaque formation. An in vivo study in man. J Clin
1. Bjorn AL, Bjorn H, Grkovic B. Marginal fit of restorations and its relation Periodontol 1990;17:138-44.
to periodontal bone level. II. Crowns. Odontol Revy 1970;21:337-46. 29. Quirynen M, van der Mei HC, Bollen CM, Schotte A, Marechal M,
2. Gilmore N, Sheiham A. Overhanging dental restorations and periodon- Doombusch GI, et al. An in vivo study of the influence of the surface
tal disease. J Periodontol 1971;42:8-12. roughness of implants on the microbiology of supra- and subgingival
3. Highfield JE, Powell RN. Effects of removal of posterior overhanging plaque. J Dent Res 1993;72:1304-9.
metallic margins of restorations upon the periodontal tissues. J Clin 30. Bollen CM, Papaioanno W, Van Eldere J, Schepers E, Quirynen M, van
Periodontol 1978;5:169-81. Steenberghe D. The influence of abutment surface roughness on plaque
4. Jeffcoat MK, Howell TH. Alveolar bone destruction due to overhanging accumulation and peri-implant mucositis. Clin Oral Implants Res
amalgam in periodontal disease. J Periodontol 1980;51:599-602. 1996;7:201-11.
5. Turner CH. A retrospective study of the fit of jacket crowns placed 31. Perel ML. Periodontal considerations of crown contours. J Prosthet Dent
around gold posts and cores, and the associated gingival health. J Oral 1971;26:627-30.
Rehabil 1982;9:427-34. 32. Silness J, Ohm E. Periodontal conditions in patients treated with dental
6. Lang NP, Kiel RA, Anderhalden K. Clinical and microbiological effects of bridges. V. Effects of splinting adjacent abutment teeth. J Periodontal Res
subgingival restorations with overhanging or clinically perfect margins. J 1974;9:121-6.
Clin Periodontol 1983;10:563-78. 33. Parkinson CF. Excessive crown contours facilitate endemic plaque nich-
7. Sorensen SE, Larsen IB, Jorgensen KD. Gingival and alveolar bone reac- es. J Prosthet Dent 1976;35:424-9.
tion to marginal fit of subgingival crown margins. Scand J Dent Res 34. Sackett BP, Gildenhuys RR. The effect of axial crown overcontour on
1986;94:109-14. adolescents. J Periodontol 1976;47:320-3.
8. Felton DA, Kanoy BE, Bayne SC, et al. Effect of in vivo crown margin dis- 35. Ehrlich J, Hochman N. Alterations on crown contour—effect on gingival
crepancies on periodontal health. J Prosthet Dent 1991;65:357-64. health in man. J Prosthet Dent 1980;44:523-5.
9. Silness J. Periodontal conditions in patients treated with dental bridges. 36. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and
3. The relationship between the location of the crown margin and the severity. Acta Odont Scand 1963;21:533-51.
periodontal condition. J Periodontal Res 1970;5:225-9. 37. Pihlstrom B. Issues in the evaluation of clinical trials of periodontitis: a
10. Bergman B, Hugoson A, Olsson CO. Periodontal and prosthetic condi- clinical perspective. J Periodontal Res 1992;27:433-41.
NOVEMBER 2000 497
THE JOURNAL OF PROSTHETIC DENTISTRY KNOERNSCHILD AND CAMPBELL
38. Reddy MS, Palcanis KG, Geurs NC. A comparison of manual and con- 55. Adamczyk E, Spiechowicz E. Plaque accumulation on crowns made of
trolled-force attachment-level measurements. J Clin Periodontol various materials. Int J Prosthodont 1990;3:285-91.
1997;24:920-6. 56. Busscher HJ, Cowan MM, van der Mei HC. On the relative importance
39. Grossi SG, Dunford RG, Ho A, Koch G, Machter EE, Genco RJ. Sources of specific and non-specific approaches to oral microbial adhesion.
of error for periodontal probing measurements. J Periodontal Res FEMS Microbiol Rev 1992;8:199-209.
1996;31:330-6. 57. Satou J, Fukunaga A, Morikawa A, Matsumae I, Satou N, Shintani H.
40. Gunsolley JC, Williams DA, Schenkein HA. Variance component model- Streptococcal adherence to uncoated and saliva-coated restoratives. J
ing of attachment level measurements. J Clin Periodontol 1994;21:289-95. Oral Rehabil 1991;18:421-9.
41. Van der Zee E, Davies EH, Newman HN. Marking width, calibration 58. Scheie AA. Mechanisms of dental plaque formation. Adv Dent Res
from tip and tine diameter of periodontal probes. J Clin Periodontol 1994;8:246-53.
1991;18:516-20. 59. Ellen RP, Lepine G, Nghiem PM. In vitro models that support adhesion
42. Aeppli DM, Boen JR, Bandt CL. Measuring and interpreting increases in specificity in biofilms of oral bacteria. Adv Dent Res 1997;11:33-42.
probing depth and attachment loss. J Periodontol 1985;56:262-4. 60. Busscher HJ, van der Mei HC. Physico-chemical interactions in initial
43. Hausmann E, Allen K, Norderyd J, Ren W, Shibly O, Machtei E. Studies microbial adhesion and relevance for biofilm formation. Adv Dent Res
on the relationship between changes in radiographic bone height and 1997;11:24-32.
probing attachment. J Clin Periodontol 1994;21:128-32. 61. Bos R, van der Mei HC, Busscher HJ. Physico-chemistry of initial micro-
44. Benn DK. Limitations of the digital image subtraction technique in bial adhesive interactions—its mechanisms and methods for study. FEMS
assessing alveolar bone crest changes due to misalignment errors during Microbiol Rev 1999;23:179-230.
image capture. Dentomaxillofac Radiol 1990;19:97-104. 62. Knoernschild KL, Lefebvre CA, Schuster GS, Payant LM, Gagnon FM.
45. Selikowitz HS, Sheiham A, Albert D, Williams GM. Retrospective longi- Endotoxin adherence to and elution from two casting alloys. Int J
tudinal study of the rate of alveolar bone loss in humans using bite-wing Prosthodont 1994;7:22-9.
radiographs. J Clin Periodontol 1981;8:431-8. 63. Knoernschild KL, Tompkins GR, Lefebvre CA, Griffiths LL, Schuster GS.
46. Rohner F, Cimasoni G, Vuagnat P. Longitudinal radiographical study on Effect of pH on Porphyromonas gingivalis endotoxin affinity for resins. Int
the rate of alveolar bone loss in patients of a dental school. J Clin J Prosthodont 1996;9:239-47.
Periodontol 1983;10:643-51. 64. Nelson SK, Knoernschild KL, Robinson FG, Schuster GS. Lipopolysaccharide
47. Papapanou PN, Wennstrom JL, Grondahl K. A 10-year retrospective study affinity for titanium implant biomaterials. J Prosthet Dent 1997;77:76-82.
of periodontal disease progression. J Clin Periodontol 1989;16:403-11. 65. Knoernschild KL, Tompkins GR, Schuster GS, Lefebvre CA, Russell CM.
48. Lavstedt S, Bolin A, Henrikson CO. Proximal alveolar bone loss in a lon- Effect of treatment concentration on lipopolysaccharide affinity for two
gitudinal radiographic investigation. II. A 10-year follow-up study of an alloys. Dent Mater 1997;13:111-7.
epidemiologic material. Acta Odontol Scand 1986;44:199-205. 66. Wang JC, Lai CH, Listgarten MA. Porphyromonas gingivalis, Prevotella
49. Albandar JM, Rise J, Abbas DK. Radiographic quantification of alveolar intermedia and Bacteroides forsythus in plaque subjacent to bridge pon-
bone level changes. Predictors of longitudinal bone loss. Acta Odontol tics. J Clin Periodontol 1998;25:330-3.
Scand 1987;45:55-9.
50. Clayton JA, Green E. Roughness of pontic materials and dental plaque. J Reprint requests to:
Prosthet Dent 1970;23:407-11. DR KENT L. KNOERNSCHILD
51. Quirynen M, Marechal M, Busscher HJ, Weerkamp AH, Arends J, Darius UIC COLLEGE OF DENTISTRY (MC555)
PL, et al. The influence of surface free-energy on planimetric plaque 801 S PAULINA ST
growth in man. J Dent Res 1989;68:796-9. CHICAGO, IL 60612-7212
52. Tsibouklis J, Stone M, Thorpe AA, Graham P, Peters V, Heerlien R, et al. FAX: (312)996-6989
Preventing bacterial adhesion onto surfaces: the low-surface-energy E-MAIL: KentK@uic.edu
approach. Biomaterials 1999;20:1229-35.
53. Olsson J, van der Heijde Y, Holmberg K. Plaque formation in vivo and Copyright © 2000 by The Editorial Council of The Journal of Prosthetic
bacterial attachment in vitro on permanently hydrophobic and Dentistry.
hydrophilic surfaces. Caries Res 1992;26:428-33. 0022-3913/2000/$12.00 + 0. 10/1/110262
54. Savitt ED, Malament KA, Socransky SS, Melcer AJ, Backman KJ. Effects
on colonization of oral microbiota by a cast glass-ceramic restoration. Int
J Periodontics Restorative Dent 1987;7:22-35. doi:10.1067/mpr.2000.110262
Bound volumes available to subscribers
Bound volumes of The Journal of Prosthetic Dentistry are available to subscribers (only) for
the 2000 issues from the publisher at a cost of $92.00 ($106.00 international) for Vol. 83
(January-June) and Vol. 84 (July-December). Shipping charges are included. Each bound volume
contains a subject and author index, and all advertising is removed. Copies are shipped within
30 days after publication of the last issue in the volume. The binding is durable buckram with the
journal name, volume number, and year stamped in gold on the spine. Volumes 81 and 82 are
also available. Payment must accompany all orders. Contact Mosby, Subscription Customer
Service, 6277 Sea Harbor Dr, Orlando, FL 32887, or call 800-654-2452 or 407-345-4000.
Subscriptions must be in force to qualify. Bound volumes are not available in place of
a regular Journal subscription.
498 VOLUME 84 NUMBER 5
You might also like
- Massage Therapy and MedicationsOxfordDocument232 pagesMassage Therapy and MedicationsOxfordboutique.chersNo ratings yet
- Treatment Planning of Teeth With Compromised Clinical Crowns Endodontic, Reconstructive, and Surgical StrategyDocument20 pagesTreatment Planning of Teeth With Compromised Clinical Crowns Endodontic, Reconstructive, and Surgical Strategyfloressam2000No ratings yet
- Autism For DummiesDocument11 pagesAutism For Dummiesgocyndigo72yahoocomNo ratings yet
- American Academy of Periodontology Best Evidence Consensus Statement On Modifying Peridontal Phenotype in Preparation For Orthodontic and Restorative Treatment 2019Document10 pagesAmerican Academy of Periodontology Best Evidence Consensus Statement On Modifying Peridontal Phenotype in Preparation For Orthodontic and Restorative Treatment 2019Implant DentNo ratings yet
- CD Manual 09Document99 pagesCD Manual 09Matthew Ho100% (2)
- Fire Station Design GuideDocument6 pagesFire Station Design GuideAtmrezaNo ratings yet
- Case Write Up-DengueDocument16 pagesCase Write Up-DengueSyafi'ie Syukri100% (1)
- Ercoli Et Al-2018-Journal of Clinical PeriodontologyDocument12 pagesErcoli Et Al-2018-Journal of Clinical PeriodontologyTeresa BeltranNo ratings yet
- Ercoli 2020Document47 pagesErcoli 2020Miguel Angel Cabrera DiazNo ratings yet
- Periodontally Compromised vs. Periodontally Healthy Patients and Dental Implants: A Systematic Review and Meta-AnalysisDocument19 pagesPeriodontally Compromised vs. Periodontally Healthy Patients and Dental Implants: A Systematic Review and Meta-AnalysisLuis Fernando RodriguesNo ratings yet
- Defectos de Furca y Regeneracion TisularDocument21 pagesDefectos de Furca y Regeneracion TisularSebastián BernalNo ratings yet
- Dental Prostheses and Tooth-Related FactorsDocument14 pagesDental Prostheses and Tooth-Related FactorsMartty BaNo ratings yet
- Journal of Periodontology - 2018 - Ercoli - Dental Prostheses and Tooth Related FactorsDocument14 pagesJournal of Periodontology - 2018 - Ercoli - Dental Prostheses and Tooth Related FactorsTesis Luisa MariaNo ratings yet
- Peri-Implant Health, Peri-Implant Mucositis, and Peri-Implantitis: Case Definitions and Diagnostic ConsiderationsDocument9 pagesPeri-Implant Health, Peri-Implant Mucositis, and Peri-Implantitis: Case Definitions and Diagnostic ConsiderationsFrancisca Cardenas OñateNo ratings yet
- Periodontology 2000 - 2003 - SANZ - Focus On Furcation Defects Guided Tissue RegenerationDocument21 pagesPeriodontology 2000 - 2003 - SANZ - Focus On Furcation Defects Guided Tissue Regenerationcarla lopezNo ratings yet
- New Paradigms in Prosthodontic Treatment PlanningDocument8 pagesNew Paradigms in Prosthodontic Treatment PlanningNanda Iswa MaysferaNo ratings yet
- Insights Into The June 2020 Issue of The JOE - 2020Document2 pagesInsights Into The June 2020 Issue of The JOE - 2020MarielEsmeraldaNo ratings yet
- Berglundh Et Al-2018-Journal of Clinical PeriodontologyDocument6 pagesBerglundh Et Al-2018-Journal of Clinical PeriodontologyCristian CulcitchiNo ratings yet
- Nobre 2016Document10 pagesNobre 2016MonicaNo ratings yet
- JIAP October 2011 - The Influence of Restorations and Prosthetic Crowns Finishing Lines On Inflammatory Levels After Non-Surgical Periodontal TherapyDocument8 pagesJIAP October 2011 - The Influence of Restorations and Prosthetic Crowns Finishing Lines On Inflammatory Levels After Non-Surgical Periodontal TherapyMedstudNo ratings yet
- NIH Public Access: Development of Prognostic Indicators Using Classification and Regression Trees (CART) For SurvivalDocument17 pagesNIH Public Access: Development of Prognostic Indicators Using Classification and Regression Trees (CART) For Survivalregina marthaNo ratings yet
- Influence of Tooth Location On Coronally Advanced Flap Procedures For Root CoverageDocument44 pagesInfluence of Tooth Location On Coronally Advanced Flap Procedures For Root Coveragemaria.lorcagNo ratings yet
- Changes in Correlations Between Cervical Crown EdgDocument3 pagesChanges in Correlations Between Cervical Crown EdgAngela RamirezNo ratings yet
- Clinical, Histological, and Microbiological Findings in Peri-Implant Disease: A Pilot StudyDocument11 pagesClinical, Histological, and Microbiological Findings in Peri-Implant Disease: A Pilot StudyPeter von TanNo ratings yet
- Effectiveness of Interceptive Orthodontic Treatment in Reducing MalocclusionsDocument8 pagesEffectiveness of Interceptive Orthodontic Treatment in Reducing MalocclusionsAriana de LeonNo ratings yet
- Endodontology: Editor: Larz S. W. Spa NgbergDocument6 pagesEndodontology: Editor: Larz S. W. Spa NgbergHenrique Silva PessoaNo ratings yet
- Periodontal Restorative Inter-Relationship: A ReviewDocument9 pagesPeriodontal Restorative Inter-Relationship: A ReviewKrupali JainNo ratings yet
- Diagnostics 12 00919Document29 pagesDiagnostics 12 00919Minh KhueNo ratings yet
- Renvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1Document9 pagesRenvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1FelipeOyarceSalazarNo ratings yet
- GOBBATODocument11 pagesGOBBATOBianca MarcheziNo ratings yet
- Dimensional Changes in Free Epithelialized Gingival/mucosal Grafts at Tooth and Implant Sites: A Prospective Cohort StudyDocument10 pagesDimensional Changes in Free Epithelialized Gingival/mucosal Grafts at Tooth and Implant Sites: A Prospective Cohort StudyDiana Pellecer de SmithNo ratings yet
- Histological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesDocument8 pagesHistological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesGilmer Solis SánchezNo ratings yet
- 10 1002@jper 20-0598Document7 pages10 1002@jper 20-0598yalocim666No ratings yet
- Chen 2019Document9 pagesChen 2019Tiara HapkaNo ratings yet
- 35journal of Periodontology - 2018 - Renvert - Peri Implant Health Peri Implant Mucositis and Peri Implantitis CaseDocument9 pages35journal of Periodontology - 2018 - Renvert - Peri Implant Health Peri Implant Mucositis and Peri Implantitis CaseMax Flores RuizNo ratings yet
- Pontoriero 2001Document8 pagesPontoriero 2001bruno mañonNo ratings yet
- Vitali - 2021 - Asociación Entre Tto Ortodoncia y Cambios PulparesDocument14 pagesVitali - 2021 - Asociación Entre Tto Ortodoncia y Cambios PulparesMICHAEL ERNESTO QUINCHE RODRIGUEZNo ratings yet
- Abstracts: Abstracts On This Page Have Been Chosen and Edited by DR Trevor WattsDocument1 pageAbstracts: Abstracts On This Page Have Been Chosen and Edited by DR Trevor WattsNifarea Anlila VesthiNo ratings yet
- PERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 pagesPERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasNo ratings yet
- Articulo para DesarrollarDocument9 pagesArticulo para DesarrollarMafe Durán RangelNo ratings yet
- El Efecto de Las Discrepancias Oclusales y La PeriodontitisDocument11 pagesEl Efecto de Las Discrepancias Oclusales y La PeriodontitisNERY OSWALDO GARCIA ANZUETONo ratings yet
- Journal of Periodontology - 2019 - Kim - Effect of Gingival Phenotype On The Maintenance of Periodontal Health An AmericanDocument28 pagesJournal of Periodontology - 2019 - Kim - Effect of Gingival Phenotype On The Maintenance of Periodontal Health An AmericanLEONARDO ALBERTO CRESPIN ZEPEDANo ratings yet
- Reconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical TrialDocument24 pagesReconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical Trialrmartins76No ratings yet
- Long-Term Results of Peri-Implant Conditions in Periodontally Compromised Patients Following Lateral Bone AugmentationDocument10 pagesLong-Term Results of Peri-Implant Conditions in Periodontally Compromised Patients Following Lateral Bone AugmentationNosaci AndreiNo ratings yet
- Role of Thin Gingival Phenotype and Inadequate Keratinized Mucosa Width ( - 2 MM) As Risk Indicators For Peri Implantitis and Peri Implant MucositisDocument10 pagesRole of Thin Gingival Phenotype and Inadequate Keratinized Mucosa Width ( - 2 MM) As Risk Indicators For Peri Implantitis and Peri Implant MucositisAdil KaukabNo ratings yet
- French 2019Document7 pagesFrench 2019Netra TaleleNo ratings yet
- Occlusal Trauma and Excessive Occlusal Forces: Narrative Review, Case Definitions, and Diagnostic ConsiderationsDocument8 pagesOcclusal Trauma and Excessive Occlusal Forces: Narrative Review, Case Definitions, and Diagnostic ConsiderationsJoss ZapataNo ratings yet
- Effect of Gingival Biotype On Orthodontic TreatmenDocument8 pagesEffect of Gingival Biotype On Orthodontic Treatmensolodont1No ratings yet
- Japid 12 3Document8 pagesJapid 12 3hugorhadelNo ratings yet
- Berglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1Document9 pagesBerglundh Et Al (2018) - Peri Implant Diseases and Conditions - Consensus Report of Workgroup 4 - 1FelipeOyarceSalazarNo ratings yet
- Mucogingival Conditions in The Natural DentitionDocument9 pagesMucogingival Conditions in The Natural Dentitionclaudyedith197527No ratings yet
- Artículo PerioDocument5 pagesArtículo PerioMIRSHA IRAZEMA SAMAN HERNANDEZNo ratings yet
- Jper.19 0310 1Document13 pagesJper.19 0310 1Iga OktawisdoNo ratings yet
- Cre2 10Document15 pagesCre2 10jhonatan gaspariNo ratings yet
- 软组织相关的并发症风险Document15 pages软组织相关的并发症风险xiaoxin zhangNo ratings yet
- Orto Paro 2Document6 pagesOrto Paro 2adk eijfNo ratings yet
- Prognosis of Dental Implants in Patients With Low Bone Density: A Systemic Review and Meta-AnalysisDocument10 pagesPrognosis of Dental Implants in Patients With Low Bone Density: A Systemic Review and Meta-AnalysisNathan LouisNo ratings yet
- Research Article: Periodontal ScienceDocument10 pagesResearch Article: Periodontal ScienceJontavius GilbertNo ratings yet
- Bilhan 2012Document7 pagesBilhan 2012laur112233No ratings yet
- Clinical Oral Implants Res - 2015 - Sousa - A Systematic Review of Implant Outcomes in Treated Periodontitis PatientsDocument58 pagesClinical Oral Implants Res - 2015 - Sousa - A Systematic Review of Implant Outcomes in Treated Periodontitis Patientskokorafat636No ratings yet
- Localised Periodontitis With Trauma From OcclusionDocument13 pagesLocalised Periodontitis With Trauma From OcclusionAliyah SaraswatiNo ratings yet
- OOOO Ricucci 2000Document6 pagesOOOO Ricucci 2000karlaNo ratings yet
- A Multifactorial Analysis To Identify Predictors of Implant Failure and Peri-Implant Bone LossDocument10 pagesA Multifactorial Analysis To Identify Predictors of Implant Failure and Peri-Implant Bone LossstortoNo ratings yet
- Future Biotechnology: The Eurobiotech JournalDocument4 pagesFuture Biotechnology: The Eurobiotech JournalsaraNo ratings yet
- Bilal Ahmad Khan CVDocument2 pagesBilal Ahmad Khan CVfr.faisal8265No ratings yet
- Factor Affecting The Development of FetusDocument8 pagesFactor Affecting The Development of FetusWhye Jun CheongNo ratings yet
- CraniectomyDocument5 pagesCraniectomytabanaoNo ratings yet
- Dental MaterialsDocument11 pagesDental MaterialsShweta RangharNo ratings yet
- Section 8 The CTA Written Examination PDFDocument10 pagesSection 8 The CTA Written Examination PDFBojana VulasNo ratings yet
- Passenger Locator Form: Non-Red ListDocument4 pagesPassenger Locator Form: Non-Red ListSamadrukNo ratings yet
- ComplaintDocument52 pagesComplaintmarwaNo ratings yet
- Anatomi Dan Fisiologi PerkemihanDocument89 pagesAnatomi Dan Fisiologi Perkemihannia djNo ratings yet
- 12.2 - Regulation of Body TemperatureDocument38 pages12.2 - Regulation of Body Temperature022797SemelllNo ratings yet
- Deep Fat FryingDocument2 pagesDeep Fat FryingalinawidagdoNo ratings yet
- Knauf - Insulation Godisnji Izvestaj PDFDocument29 pagesKnauf - Insulation Godisnji Izvestaj PDFDifermoNo ratings yet
- ალერგიული რინიტი=20Document31 pagesალერგიული რინიტი=20Dali KochalidzeNo ratings yet
- Coriander (Corindrum Sativum L) and Its Bioactive ConstituentsDocument19 pagesCoriander (Corindrum Sativum L) and Its Bioactive ConstituentsFirda AuliyaNo ratings yet
- Prevention & Management of Sports Injuries: Quimcy Dsouza Fybms-Sm (B) 75Document26 pagesPrevention & Management of Sports Injuries: Quimcy Dsouza Fybms-Sm (B) 75Quimcy100% (1)
- Fluid Therapy in Cardiac Surgery PatientsDocument37 pagesFluid Therapy in Cardiac Surgery PatientsaymxNo ratings yet
- For DissertationDocument13 pagesFor DissertationRegi viniciyaNo ratings yet
- The Results of MasturbationDocument1 pageThe Results of MasturbationAkash DeepNo ratings yet
- Margaret Paul - Taking The Lid Off Your FeelingsDocument4 pagesMargaret Paul - Taking The Lid Off Your FeelingspapetologeneNo ratings yet
- Central HypotoniaDocument5 pagesCentral HypotoniaayunisallehNo ratings yet
- Medical Condition Report Free PDF TemplateDocument2 pagesMedical Condition Report Free PDF Templateapi-340236228No ratings yet
- Written Report Abnormal PsychologyDocument23 pagesWritten Report Abnormal PsychologyCy Esquibel LingaNo ratings yet
- S M A R T: 201 A TEST #3 Define and Discuss The Purpose of Outcome IdentificationDocument6 pagesS M A R T: 201 A TEST #3 Define and Discuss The Purpose of Outcome IdentificationLindsay JonesNo ratings yet
- Child Rights and You - Wikipedia PDFDocument14 pagesChild Rights and You - Wikipedia PDFpatel mariyamNo ratings yet
- Kohler Students Scores Tops in The State Again For ACT ScoresDocument20 pagesKohler Students Scores Tops in The State Again For ACT ScoresThe Kohler VillagerNo ratings yet