Professional Documents
Culture Documents
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Uploaded by
النشر العربيCopyright:
Available Formats
You might also like
- 100 Q&A of GCE O'Level Economics 2281Document32 pages100 Q&A of GCE O'Level Economics 2281Hassan Asghar100% (4)
- The Cartography of Crete in The 17thDocument28 pagesThe Cartography of Crete in The 17thΕυτύχης ΤζιρτζιλάκηςNo ratings yet
- Evaluation_of_dosing_strategy_for_pembrolizumab_foDocument9 pagesEvaluation_of_dosing_strategy_for_pembrolizumab_foالنشر العربيNo ratings yet
- Estimation of Cefuroxime Dosage Using Pharmacodynamic Targets, MIC DistributionsDocument13 pagesEstimation of Cefuroxime Dosage Using Pharmacodynamic Targets, MIC DistributionsLuciana OliveiraNo ratings yet
- Modeling & Simulation: ToolkitDocument24 pagesModeling & Simulation: ToolkitArchana MishraNo ratings yet
- Cancer Immunotherapy Trials Leading A Paradigm Shift in Drug DevelopmentDocument8 pagesCancer Immunotherapy Trials Leading A Paradigm Shift in Drug Development49qmzqdpndNo ratings yet
- Early stage TNBC - Time to Optimize Personalized Strategies 2022Document10 pagesEarly stage TNBC - Time to Optimize Personalized Strategies 2022VistieruBeatriceNo ratings yet
- Research Pharmacogenomics PDFDocument10 pagesResearch Pharmacogenomics PDFmohammedNo ratings yet
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDocument6 pagesNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanNo ratings yet
- Treatment of Patients With Small-Cell Lung Cancer From Meta-AnalysesDocument9 pagesTreatment of Patients With Small-Cell Lung Cancer From Meta-AnalysesmaleticjNo ratings yet
- Biology Project On Ai in MedicineDocument10 pagesBiology Project On Ai in Medicinejapmansingh45678No ratings yet
- Anticancer Dose Adjustment For Patients With Renal and Hepatic Dysfunction: From Scientific Evidence To Clinical ApplicationDocument16 pagesAnticancer Dose Adjustment For Patients With Renal and Hepatic Dysfunction: From Scientific Evidence To Clinical ApplicationRiz Qie NaNo ratings yet
- Imaging in Clinical TrialsDocument9 pagesImaging in Clinical Trialsenq0r3No ratings yet
- Evidence-Based Treatmentsin Pemphigusvulgaris Andpemphigus FoliaceusDocument8 pagesEvidence-Based Treatmentsin Pemphigusvulgaris Andpemphigus FoliaceusCharly EscobarNo ratings yet
- Precision Medicine For RheumatologistsDocument9 pagesPrecision Medicine For Rheumatologistsmihaelaatanasova123No ratings yet
- Risk of Clinically Relevant Pharmacokinetic-based Drug-drug Interactions with Drugs ApprovedDocument155 pagesRisk of Clinically Relevant Pharmacokinetic-based Drug-drug Interactions with Drugs Approvedamnaakb197No ratings yet
- BR 7 1 3 PDFDocument3 pagesBR 7 1 3 PDFalejandro.rivera2570No ratings yet
- phar.2753Document10 pagesphar.2753Mohammed VHNo ratings yet
- Biomedicines 06 00014 v2Document11 pagesBiomedicines 06 00014 v2yihuiNo ratings yet
- Research, Collegeville, Pennsylvania and 3division of Infectious Diseases, Hartford Hospital, HartfordDocument11 pagesResearch, Collegeville, Pennsylvania and 3division of Infectious Diseases, Hartford Hospital, HartfordAriana EmiliaNo ratings yet
- Pan 2014Document5 pagesPan 2014Rafaela Queiroz MascarenhasNo ratings yet
- Comparative Effectiveness of Avelumab Versus Chemotherapy in Merkel Cell Carcinoma: Innovative Use of Patient InsightsDocument10 pagesComparative Effectiveness of Avelumab Versus Chemotherapy in Merkel Cell Carcinoma: Innovative Use of Patient InsightsRui TachibanaNo ratings yet
- Biomarkers For Immunotherapy of Cancer: Methods and ProtocolsDocument730 pagesBiomarkers For Immunotherapy of Cancer: Methods and ProtocolsMD Oscar Rodriguez BejaranoNo ratings yet
- 2017 Treatment Outcomes For Metastatic Melanoma of Unknown Primary in The New Era - A Single-Institution Study and Review of The LiteratureDocument10 pages2017 Treatment Outcomes For Metastatic Melanoma of Unknown Primary in The New Era - A Single-Institution Study and Review of The LiteratureAndrés WunderwaldNo ratings yet
- PK ProblemsDocument18 pagesPK ProblemsJosephine Valsa JoseNo ratings yet
- Pharmacokinetics, PharmacodynamicsDocument18 pagesPharmacokinetics, PharmacodynamicspinkbutterNo ratings yet
- Population Pharmacokinetics IDocument5 pagesPopulation Pharmacokinetics IJosé David Sanabria VanegasNo ratings yet
- 1078 0432.CCR 16 0230Document42 pages1078 0432.CCR 16 0230肖茹雪No ratings yet
- Dose Translation Between Laboratory Animals and Human in Preclinical and Clinical Phases of Drug DevelopmentDocument11 pagesDose Translation Between Laboratory Animals and Human in Preclinical and Clinical Phases of Drug DevelopmentDaniel Olivier OlmadNo ratings yet
- 1 s2.0 S1525730423002681 MainDocument10 pages1 s2.0 S1525730423002681 MainTrọngNguyễnĐìnhNo ratings yet
- FB BerDocument18 pagesFB BeryuliaNo ratings yet
- Report A4 Week 7Document15 pagesReport A4 Week 7Amasi Al-khiderNo ratings yet
- Three Pillars of Drug Development Case StudyDocument2 pagesThree Pillars of Drug Development Case StudyVVBNo ratings yet
- Journal Pcbi 1001043Document8 pagesJournal Pcbi 1001043kushalshaNo ratings yet
- Machine Learning Approaches To Drug Response Prediction: Challenges and Recent ProgressDocument10 pagesMachine Learning Approaches To Drug Response Prediction: Challenges and Recent ProgressKunel KumarNo ratings yet
- FDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerDocument6 pagesFDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerasdffdsaNo ratings yet
- 14.beyond Conventional Chemotherapy, Targeted Therapy and ImmunotherapyDocument8 pages14.beyond Conventional Chemotherapy, Targeted Therapy and ImmunotherapyLavanya SundarNo ratings yet
- ASCO Antiemetic Guidelines Update Aug 2020Document18 pagesASCO Antiemetic Guidelines Update Aug 2020catalina roa zagalNo ratings yet
- 1933 0715 Article p350Document8 pages1933 0715 Article p350Alan padilla sesmaNo ratings yet
- BMC CancerDocument6 pagesBMC CancerJose Antonio VenacostaNo ratings yet
- Aston2017 PDFDocument10 pagesAston2017 PDFTorres Pineda OsvaldoNo ratings yet
- Barsanti-Innes The Oncologist - 2016Document8 pagesBarsanti-Innes The Oncologist - 2016Liz BethNo ratings yet
- Updated Version: Mol Cancer TherDocument13 pagesUpdated Version: Mol Cancer TherSakshi IssarNo ratings yet
- Pembrolizumab For Previously TreatedDocument11 pagesPembrolizumab For Previously Treatedalex.losadaNo ratings yet
- Relapse Rates With Paliperidone Palmitate in AdultDocument11 pagesRelapse Rates With Paliperidone Palmitate in AdultdryaeonNo ratings yet
- DC Vaksin For GBM-Jurnal RevisiDocument8 pagesDC Vaksin For GBM-Jurnal Revisiallyssa rahmadittaNo ratings yet
- Emerging Trends at The Interface of Chemistry and Biology: Applications To The Design of Human TherapeuticsDocument11 pagesEmerging Trends at The Interface of Chemistry and Biology: Applications To The Design of Human TherapeuticssuryasanNo ratings yet
- Endpoints in Advanced Breast Cancer: Methodological Aspects & Clinical ImplicationsDocument6 pagesEndpoints in Advanced Breast Cancer: Methodological Aspects & Clinical ImplicationsJauhar FirdausNo ratings yet
- How Artificial Intelligence Could Redefine Clinical Trials in Cardiovascular Medicine: Lessons Learned From OncologyDocument6 pagesHow Artificial Intelligence Could Redefine Clinical Trials in Cardiovascular Medicine: Lessons Learned From OncologySAMUEL ESCARESNo ratings yet
- Modeling Cancer-Immune Responses To TherapyDocument18 pagesModeling Cancer-Immune Responses To TherapyCarolina RibeiroNo ratings yet
- DTH 14650Document19 pagesDTH 14650Evelyn LimNo ratings yet
- Nejme 1200409Document2 pagesNejme 1200409Arie Krisnayanti Ida AyuNo ratings yet
- The Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Document7 pagesThe Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Andrea SbranaNo ratings yet
- Vanco & Ag PK 2018Document35 pagesVanco & Ag PK 2018Nguyen GeenNo ratings yet
- Analytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitDocument14 pagesAnalytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitngobaochanNo ratings yet
- Clinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot StudyDocument8 pagesClinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot Studyyafit_armon5854No ratings yet
- Bradley J Monk First Line Pembrolizumab ChemotherapyDocument9 pagesBradley J Monk First Line Pembrolizumab ChemotherapyRaúl DíazNo ratings yet
- Rates of Uptake of Novel Agents in CancerpdfDocument1 pageRates of Uptake of Novel Agents in CancerpdfmaleticjNo ratings yet
- Efficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesDocument11 pagesEfficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesJOSE DIAZNo ratings yet
- An Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesDocument9 pagesAn Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesBobNo ratings yet
- Dose Finding For New Vaccines: The Role For Immunostimulation/immunodynamic ModellingDocument14 pagesDose Finding For New Vaccines: The Role For Immunostimulation/immunodynamic ModellingKikyNo ratings yet
- The Titans Curse - Robert VendittiDocument134 pagesThe Titans Curse - Robert VendittimarianaqueirosluzNo ratings yet
- Written Report: Lydia Hall: Care, Cure, Core Nursing TheoryDocument12 pagesWritten Report: Lydia Hall: Care, Cure, Core Nursing TheoryAldrin Limcuando100% (1)
- Martin Luther King Jr. - A True Historical Examination. (N.D.) - Retrieved OctoberDocument5 pagesMartin Luther King Jr. - A True Historical Examination. (N.D.) - Retrieved Octoberapi-336574490No ratings yet
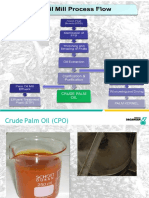
- Palm Oil MillDocument52 pagesPalm Oil MillengrsurifNo ratings yet
- Perfecto Floresca Vs Philex Mining CorporationDocument11 pagesPerfecto Floresca Vs Philex Mining CorporationDelsie FalculanNo ratings yet
- Bbyct 131 em 2024 MPDocument26 pagesBbyct 131 em 2024 MPDanish AfrozNo ratings yet
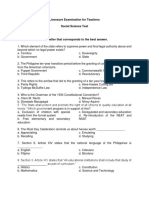
- Licensure Examination For TeachersDocument14 pagesLicensure Examination For Teachersonin saspaNo ratings yet
- LEGAL REASONING SKILLS ProjectDocument19 pagesLEGAL REASONING SKILLS ProjectShreya Ghosh DastidarNo ratings yet
- Solid Edge Mold ToolingDocument3 pagesSolid Edge Mold ToolingVetrivendhan SathiyamoorthyNo ratings yet
- Sample QuestionsDocument15 pagesSample QuestionsAnonymous MtKJkerbpUNo ratings yet
- LSM MockDocument5 pagesLSM MockKazi Rafsan NoorNo ratings yet
- Atr Summary Assignment 1Document6 pagesAtr Summary Assignment 1Livingstone OlekanmaNo ratings yet
- Ruq Abdominal PainDocument55 pagesRuq Abdominal PainriphqaNo ratings yet
- Social Work As A ProfessionDocument4 pagesSocial Work As A ProfessionIssa KhalidNo ratings yet
- (Download PDF) Deviance and Social Control A Sociological Perspective 2Nd Edition PDF Full Chapter PDFDocument53 pages(Download PDF) Deviance and Social Control A Sociological Perspective 2Nd Edition PDF Full Chapter PDFyoichiolanzo100% (9)
- In The District of Columbia Court of Appeals: Applicant, VDocument26 pagesIn The District of Columbia Court of Appeals: Applicant, VMartin AustermuhleNo ratings yet
- I Love Algorithms - Machine Learning CardsDocument6 pagesI Love Algorithms - Machine Learning CardsCarlos Manuel Ventura MatosNo ratings yet
- Before Reading: An Encyclopedia EntryDocument6 pagesBefore Reading: An Encyclopedia EntryĐào Nguyễn Duy TùngNo ratings yet
- Case Study 01 - Cincinnati ZooDocument3 pagesCase Study 01 - Cincinnati Zoononaddd1236hhNo ratings yet
- vịt batmanDocument14 pagesvịt batmanTú Lệ100% (1)
- Easy Chicken Satay With Peanut Chilli SauceDocument18 pagesEasy Chicken Satay With Peanut Chilli SauceCarina LopesNo ratings yet
- Group2 Non Executive ResultsDocument3 pagesGroup2 Non Executive ResultsGottimukkala MuralikrishnaNo ratings yet
- Synopsis Car Showroom ManagementDocument18 pagesSynopsis Car Showroom ManagementRaj Bangalore50% (4)
- Combichem: Centrifugal PumpsDocument8 pagesCombichem: Centrifugal PumpsrizkyNo ratings yet
- CAN LIN ProtocolDocument60 pagesCAN LIN ProtocolBrady BriffaNo ratings yet
- Final Artifact Management Theory IIDocument11 pagesFinal Artifact Management Theory IIapi-651643566No ratings yet
- HetzerDocument4 pagesHetzerGustavo Urueña ANo ratings yet
- Percakapan 1Document2 pagesPercakapan 1Legend AbadiNo ratings yet
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Uploaded by
النشر العربيCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Pembrolizumab_Role_of_Modeling_and_Simulation_in_B
Uploaded by
النشر العربيCopyright:
Available Formats
Pembrolizumab: Role of Modeling and Simulation in Bringing a Novel Immunotherapy to
Patients With Melanoma
Running Title: Modeling and Simulation of Pembrolizumab
Rik de Greefa*, Jeroen Elassaiss-Schaapb, Manash Chatterjee, David C. Turner, Malidi
Ahamadi, Mark Forman, David Cutler, Dinesh P. de Alwis, Anna Kondic, Julie Stone
Merck & Co., Inc., Kenilworth, NJ, USA
a
Former employee of Merck; currently employed at Quantitative Solutions, a Certara company,
Oss, The Netherlands
b
Former employee of Merck; currently employed at PD-Value, Houten, The Netherlands
*Correspondence: Anna Kondic
Merck & Co., Inc.
90 E Scott Ave
34/569
Rahway, New Jersey 07065, USA
Tel: +1-732-594-7362
E-mail: anna.kondic@merck.com
Journal: CPT: Pharmacometrics & Systems Pharmacology
Introduction: 75 (limit, 75 excluded from rest of main text)
Word count: 1483 (limit, 1600 excluding introduction, references, tables, and figures)
This article has been accepted for publication and undergone full peer review but has not been
through the copyediting, typesetting, pagination and proofreading process which may lead to
differences between this version and the Version of Record. Please cite this article as an
‘Accepted Article’, doi: 10.1002/psp4.12131
This article is protected by copyright. All rights reserved.
Tables/figures: <<1; limit 2>>
References: 10 (maximum, 10)
Keywords: Biologics, Oncology, Model-based drug development, Clinical pharmacology,
Immunotherapy
This article is protected by copyright. All rights reserved.
Introduction
Recently, immunotherapy has yielded promising results in several cancer types. Contrary to the
established classical chemotherapy dosing paradigm, a maximum tolerated dose (MTD)
approach does not always produce better clinical outcomes for novel targeted therapies, as their
efficacy is frequently robust at pharmacologically active doses below the MTD. Integrated safety
and efficacy assessments are needed to inform clinical dose and trial design, and to support an
early identification of potentially safe and efficacious combination treatments.1
PHARMACOMETRICS
The field of pharmacometrics builds upon the pharmacology and disease knowledge to develop
an integrated mathematical representation of drug response. This ability to integrate data and
information using a structured approach brings considerable advantage in a small, fast-moving
oncology program with challenges coming from data imbalances, sparseness of data,
heterogeneity of data and response, and multiple sources of variability. Conceptually and
practically, the use of modeling and simulation enables more efficient development of targeted
therapies in oncology and aids in bringing these promising treatments to patients.2
PEMBROLIZUMAB IN MELANOMA: CLINICAL OVERVIEW
Pembrolizumab, a recently introduced immunotherapy, is a potent and highly selective
humanized IgG4 kappa monoclonal antibody directed to the programmed death 1 (PD-1)
receptor and is designed to block the interaction between the receptor and its ligands, PD-L1
and PD-L2.3 The PD-1 pathway represents a major immune switch that tumor cells use to
counteract antitumor T-cell activity. When this pathway is blocked on T cells, antitumor activity is
reactivated.4 Given that PD-L1 is expressed on melanoma tumor cells,5 the initial clinical
development of anti–PD-1 treatment focused on that indication.
This article is protected by copyright. All rights reserved.
Clinical development and initial registration of pembrolizumab was largely built upon a
single clinical trial: KEYNOTE-001 (Clinicaltrials.gov identifier, NCT01295827), which was an
international, open-label, multicohort, phase Ib study of the safety and efficacy of
pembrolizumab. Following an initial dose escalation in patients with various solid tumors,
treatment of patients with advanced melanoma was initiated. Early efficacy and safety results
indicated a favorable benefit-risk profile that led to the decision to seek fast-track development
for regulatory submission at a time when little dose ranging had been conducted in the
program.6-8 The single expanded phase I study (N = 411)9 would eventually form the basis of the
initial approval of pembrolizumab in the United States for the treatment of unresectable or
metastatic melanoma. Modeling and simulation were key components supporting the dose
setting and characterization of the clinical pharmacology of pembrolizumab for the US label in
lieu of extensive dose-finding and dedicated clinical pharmacology studies which could have
slowed the program or been challenging to implement. A summary of these activities is provided
herein, and a visual overview of the applied modeling and simulation strategy is presented in the
Figure. More detailed reports on the different components of this strategy can be found
elsewhere in this issue (Ahamadi et al, manuscript submitted; Chatterjee et al, manuscript
submitted; Elassaiss-Schaap et al, manuscript submitted; Lindauer et al, manuscript submitted).
DOSE SETTING FOR EFFICACY STUDIES
As initial clinical evidence indicated promising efficacy for pembrolizumab, a focused clinical
development plan was begun. At the time of planning for the pivotal assessments of clinical
efficacy and safety, 3 key questions were identified that would be primarily addressed through
pharmacometric efforts: (1) What is the appropriate dose range for investigation in the clinical
studies as informed by estimates of minimal effective dose? (2) What is the appropriate dosage
regimen balancing benefits and risks to inform the Dosage and Administration section of the
This article is protected by copyright. All rights reserved.
label? and (3) What is the impact of intrinsic and extrinsic factors on exposure, and do these
effects require any guidance around dose adjustment in subpopulations?
Two complementary modeling and simulation approaches were developed to inform the
question around dose ranges for clinical investigation. The first utilized exploratory ex vivo
peripheral blood mononuclear cell (PBMC) biomarker and pharmacokinetic (PK) data obtained in
the initial cohorts of the clinical study, as described by Elassaiss-Schaap et al. (unpublished
data). A critical aspect of this approach was the inclusion of a dedicated intrapatient dose-
escalation cohort to strengthen the empirical PK–pharmacodynamic (PD) analysis. An
understanding of the pembrolizumab concentrations and doses at which maximal target
engagement was achieved helped to define the lower end of the dose range to be tested in the
pivotal efficacy and safety cohorts.
The second analysis to support the minimal effective dose used a translational PK–PD
modeling approach, based on integration of available preclinical PK data, PD-1 receptor
occupancy, antitumor efficacy data from a syngeneic mouse model, human tumor growth
kinetics, and early clinical PK data (Lindauer et al, manuscript submitted). In this approach, a
semimechanistic model capturing key physiologic and biological features of response (such as
antibody distribution to tumor tissue and effect of PD-1 inhibition on tumor growth) was
developed. Subsequently, the model was adapted for prediction of expected clinical responses,
with a focus on determining the lowest doses that have a high probability of achieving maximal
efficacy.
The ex vivo approach was based on clinical data but required assumptions regarding the
link between PBMC target engagement and efficacy, whereas the translational PK–PD approach
based in part on animal data relied on a physiology-based interspecies extrapolation. Despite
these differences, the 2 methods converged on a similar answer of a regimen of 1 to 2 mg/kg
administered every 3 weeks (Q3W) as the lowest dose with high optimal likelihood of maximizing
clinical efficacy. The potential for lesser efficacy was predicted at doses below 1 mg/kg. Thus, a
This article is protected by copyright. All rights reserved.
dosage regimen of 2 mg/kg Q3W was brought forward into the pivotal cohorts of the KEYNOTE-
001 trial, along with the previously planned higher-dosage regimens of 10 mg/kg Q3W and
10 mg/kg every 2 weeks (Q2W), to inform the dose selection for registration.
MODEL-BASED SUPPORT FOR REGISTRATION AND LABELING
The initial submission of pembrolizumab for the treatment of advanced melanoma relied on the
data from a single clinical study. Therefore, the focus of clinical pharmacology characterization
was on model-based approaches that could leverage sparse PK, safety, and efficacy data. The
foundation for the resulting model framework was provided by a population PK analysis
(Ahamadi et al, manuscript submitted); the latest and most mature version of the population PK
model will be continually refined. Furthermore, the analysis was central to the assessment of the
impact of key patient covariates on pembrolizumab exposure. In fact, all statements in the
special populations sections of the clinical pharmacology portion of the US label are supported
by the results of the population PK analysis. Given this critical role, special attention was given
to robustly evaluate the ability of the model to pick up covariate effects through extensive
simulations and reestimations under a variety of scenarios. Additionally, the population PK
analysis produced individual pembrolizumab exposure estimates that were included in
exposure–response relationships for efficacy and safety to support both the proposed dose
regimen and the therapeutic window for pembrolizumab.
For all melanoma submissions to date, overall survival data were not sufficiently mature
to establish robust exposure–response relationships. Therefore, exposure–efficacy evaluations
supporting pembrolizumab dose selection centered on tumor size kinetics (longitudinal scans
captured by the sum of longest dimensions of the target tumor lesions). As treatment with
immunotherapy can result in a wide array of tumor growth characteristics atypical for traditional
cytotoxic or other targeted therapies, development of a tailored tumor size model was required.
As described by Chatterjee et al., 2 approaches were explored, found to have much
This article is protected by copyright. All rights reserved.
commonality, and successfully implemented at different stages in the program.10 The results of
all exposure–tumor size assessments indicated a flat exposure–response relationship for tumor
size response for pembrolizumab across the 2 mg/kg Q3W to 10 mg/kg Q2W dosage range,
indicating that a near-maximal response was achieved at 2 mg/kg Q3W.
In addition to efficacy exposure-response, an exposure-response assessment for safety
was performed, focusing on specific categories of adverse events (AEs), with an emphasis on
immune-related AEs. Logistic regression and time-to-event approaches were utilized to assess
the potential dependence of the occurrence of these AEs on pembrolizumab exposure. The
results of these studies will be reported separately, but overall, these assessments also
indicated a flat exposure-response relationship. Collectively, the efficacy and safety exposure–
response analyses provided strong support for pembrolizumab 2 mg/kg Q3W as the proposed
dosage for the treatment of patients with unresectable or metastatic melanoma.
CONCLUSION
An integrated set of modeling and simulation evaluations was successfully applied during the
clinical development and registration of pembrolizumab, a breakthrough therapy for cancer. In
the absence of dedicated clinical studies, the analyses support the dose selection and
characterization of critical elements of the compound’s clinical pharmacology profile. As such,
the work was instrumental in rapidly bringing this treatment at an optimized dosage regimen to
patients with advanced melanoma.
Acknowledgments. Medical writing and editorial support in the preparation of this manuscript
was provided by Tricia Brown, MS, and Melanie Leiby, PhD (ApotheCom, Yardley, PA, USA)
and was funded by Merck & Co., Inc. (Kenilworth, NJ, USA).
Author Contributions
This article is protected by copyright. All rights reserved.
All authors were involved in the writing and review of the manuscript.
Conflict of Interest
All authors are employees of the stated companies. Dr. de Greef reports personal fees from
Merck & Co., Inc., during the conduct of the study; Dr. Elassaiss-Schaap reports personal fees
from Merck & Co., Inc., during the conduct of the study and after leaving started an independent
consultancy company as indicated in the affiliation; Dr. Chatterjee has nothing additional to
disclose; Dr. Turner has nothing additional to disclose; Dr. Ahamadi has nothing additional to
disclose; Dr. Forman has nothing additional to disclose; Dr. Cutler holds stock in Merck & Co.,
Inc.,; Dr. de Alwis has nothing additional to disclose; Dr. Kondic has nothing additional to
disclose; Dr. Stone reports financial activity with Merck & Co., Inc., outside of the submitted
work.
This article is protected by copyright. All rights reserved.
References
1. Melero, I., Berman, D.M., Aznar, M.A., Korman, A.J., Pérez Gracia, J.L. & Haanen, J.
Evolving synergistic combinations of targeted immunotherapies to combat cancer. Nat.
Rev. Cancer 15, 457–472 (2015).
2. Madorsky Rowdo, F.P., Baron, A., Urrutia, A., Mordoh, J. Immunotherapy in cancer: a
combat between tumors and the immune system; you win some, you lose some. Front.
Immunol. 6, 127 (2015).
3. Keytruda (pembrolizumab) for injection, for intravenous use [package insert]. Whitehouse
Station, NJ: Merck & Co, Inc. (2015).
4. Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev.
Cancer 12, 252–264 (2012).
5. Mellman, I., Coukos, G. & Dranoff, G. Cancer immunotherapy comes of age. Nature 480,
480–489 (2011).
6. Hamid, O. et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma.
N. Engl. J. Med. 369, 134–144 (2013).
7. Robert, C. et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in
ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a
phase 1 trial. Lancet 384, 1109–1117 (2014).
8. Hamid, O. et al. Randomized comparison of two doses of the anti-PD-1 monoclonal
antibody MK-3475 for ipilimumab-refractory (IPI-R) and IPI-naive (IPI-N) melanoma (MEL).
J. Clin. Oncol. 32(5 suppl), abstract 3000 (2014).
This article is protected by copyright. All rights reserved.
9. Ribas, A.F. et al. Efficacy and safety of the anti-PD-1 monoclonal antibody MK-3475 in 411
patients (pts) with melanoma (MEL). J. Clin. Oncol. 32 (5 suppl), abstract LBA9000
(2014).
10. Chatterjee, M. et al. Model-based analysis of the relationship between pembolizumab
exposure and efficacy in patients with melanoma and NSCLC: across indication
comparison. 2015 Annual Meeting of the Population Approach Group in Europe June 2-5;
Hersonissos, Greece; 2015.
10
This article is protected by copyright. All rights reserved.
Figure Pembrolizumab modeling and simulation strategy in melanoma. Various analyses inform
and support dose selection, registration, and the label for pembrolizumab.
11
This article is protected by copyright. All rights reserved.
Elassaiss-Schaap et al
IniƟal dose seƫng
Target
IniƟal engagement (IL-2)
pharmacokineƟc
model
Mouse tumor size
Lindauer et al
RegistraƟon and labeling
Clinical tumor size Overall Survival
PopulaƟon
pharmacokineƟc ChaƩerjee et al
model
Ahamadi et al
Adverse events
This article is protected by copyright. All rights reserved.
You might also like
- 100 Q&A of GCE O'Level Economics 2281Document32 pages100 Q&A of GCE O'Level Economics 2281Hassan Asghar100% (4)
- The Cartography of Crete in The 17thDocument28 pagesThe Cartography of Crete in The 17thΕυτύχης ΤζιρτζιλάκηςNo ratings yet
- Evaluation_of_dosing_strategy_for_pembrolizumab_foDocument9 pagesEvaluation_of_dosing_strategy_for_pembrolizumab_foالنشر العربيNo ratings yet
- Estimation of Cefuroxime Dosage Using Pharmacodynamic Targets, MIC DistributionsDocument13 pagesEstimation of Cefuroxime Dosage Using Pharmacodynamic Targets, MIC DistributionsLuciana OliveiraNo ratings yet
- Modeling & Simulation: ToolkitDocument24 pagesModeling & Simulation: ToolkitArchana MishraNo ratings yet
- Cancer Immunotherapy Trials Leading A Paradigm Shift in Drug DevelopmentDocument8 pagesCancer Immunotherapy Trials Leading A Paradigm Shift in Drug Development49qmzqdpndNo ratings yet
- Early stage TNBC - Time to Optimize Personalized Strategies 2022Document10 pagesEarly stage TNBC - Time to Optimize Personalized Strategies 2022VistieruBeatriceNo ratings yet
- Research Pharmacogenomics PDFDocument10 pagesResearch Pharmacogenomics PDFmohammedNo ratings yet
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDocument6 pagesNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanNo ratings yet
- Treatment of Patients With Small-Cell Lung Cancer From Meta-AnalysesDocument9 pagesTreatment of Patients With Small-Cell Lung Cancer From Meta-AnalysesmaleticjNo ratings yet
- Biology Project On Ai in MedicineDocument10 pagesBiology Project On Ai in Medicinejapmansingh45678No ratings yet
- Anticancer Dose Adjustment For Patients With Renal and Hepatic Dysfunction: From Scientific Evidence To Clinical ApplicationDocument16 pagesAnticancer Dose Adjustment For Patients With Renal and Hepatic Dysfunction: From Scientific Evidence To Clinical ApplicationRiz Qie NaNo ratings yet
- Imaging in Clinical TrialsDocument9 pagesImaging in Clinical Trialsenq0r3No ratings yet
- Evidence-Based Treatmentsin Pemphigusvulgaris Andpemphigus FoliaceusDocument8 pagesEvidence-Based Treatmentsin Pemphigusvulgaris Andpemphigus FoliaceusCharly EscobarNo ratings yet
- Precision Medicine For RheumatologistsDocument9 pagesPrecision Medicine For Rheumatologistsmihaelaatanasova123No ratings yet
- Risk of Clinically Relevant Pharmacokinetic-based Drug-drug Interactions with Drugs ApprovedDocument155 pagesRisk of Clinically Relevant Pharmacokinetic-based Drug-drug Interactions with Drugs Approvedamnaakb197No ratings yet
- BR 7 1 3 PDFDocument3 pagesBR 7 1 3 PDFalejandro.rivera2570No ratings yet
- phar.2753Document10 pagesphar.2753Mohammed VHNo ratings yet
- Biomedicines 06 00014 v2Document11 pagesBiomedicines 06 00014 v2yihuiNo ratings yet
- Research, Collegeville, Pennsylvania and 3division of Infectious Diseases, Hartford Hospital, HartfordDocument11 pagesResearch, Collegeville, Pennsylvania and 3division of Infectious Diseases, Hartford Hospital, HartfordAriana EmiliaNo ratings yet
- Pan 2014Document5 pagesPan 2014Rafaela Queiroz MascarenhasNo ratings yet
- Comparative Effectiveness of Avelumab Versus Chemotherapy in Merkel Cell Carcinoma: Innovative Use of Patient InsightsDocument10 pagesComparative Effectiveness of Avelumab Versus Chemotherapy in Merkel Cell Carcinoma: Innovative Use of Patient InsightsRui TachibanaNo ratings yet
- Biomarkers For Immunotherapy of Cancer: Methods and ProtocolsDocument730 pagesBiomarkers For Immunotherapy of Cancer: Methods and ProtocolsMD Oscar Rodriguez BejaranoNo ratings yet
- 2017 Treatment Outcomes For Metastatic Melanoma of Unknown Primary in The New Era - A Single-Institution Study and Review of The LiteratureDocument10 pages2017 Treatment Outcomes For Metastatic Melanoma of Unknown Primary in The New Era - A Single-Institution Study and Review of The LiteratureAndrés WunderwaldNo ratings yet
- PK ProblemsDocument18 pagesPK ProblemsJosephine Valsa JoseNo ratings yet
- Pharmacokinetics, PharmacodynamicsDocument18 pagesPharmacokinetics, PharmacodynamicspinkbutterNo ratings yet
- Population Pharmacokinetics IDocument5 pagesPopulation Pharmacokinetics IJosé David Sanabria VanegasNo ratings yet
- 1078 0432.CCR 16 0230Document42 pages1078 0432.CCR 16 0230肖茹雪No ratings yet
- Dose Translation Between Laboratory Animals and Human in Preclinical and Clinical Phases of Drug DevelopmentDocument11 pagesDose Translation Between Laboratory Animals and Human in Preclinical and Clinical Phases of Drug DevelopmentDaniel Olivier OlmadNo ratings yet
- 1 s2.0 S1525730423002681 MainDocument10 pages1 s2.0 S1525730423002681 MainTrọngNguyễnĐìnhNo ratings yet
- FB BerDocument18 pagesFB BeryuliaNo ratings yet
- Report A4 Week 7Document15 pagesReport A4 Week 7Amasi Al-khiderNo ratings yet
- Three Pillars of Drug Development Case StudyDocument2 pagesThree Pillars of Drug Development Case StudyVVBNo ratings yet
- Journal Pcbi 1001043Document8 pagesJournal Pcbi 1001043kushalshaNo ratings yet
- Machine Learning Approaches To Drug Response Prediction: Challenges and Recent ProgressDocument10 pagesMachine Learning Approaches To Drug Response Prediction: Challenges and Recent ProgressKunel KumarNo ratings yet
- FDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerDocument6 pagesFDA Approval Summary - Atezolizumab and Durvalumab in Combination With Platinum-Based Chemotherapy in Extensive Stage Small Cell Lung CancerasdffdsaNo ratings yet
- 14.beyond Conventional Chemotherapy, Targeted Therapy and ImmunotherapyDocument8 pages14.beyond Conventional Chemotherapy, Targeted Therapy and ImmunotherapyLavanya SundarNo ratings yet
- ASCO Antiemetic Guidelines Update Aug 2020Document18 pagesASCO Antiemetic Guidelines Update Aug 2020catalina roa zagalNo ratings yet
- 1933 0715 Article p350Document8 pages1933 0715 Article p350Alan padilla sesmaNo ratings yet
- BMC CancerDocument6 pagesBMC CancerJose Antonio VenacostaNo ratings yet
- Aston2017 PDFDocument10 pagesAston2017 PDFTorres Pineda OsvaldoNo ratings yet
- Barsanti-Innes The Oncologist - 2016Document8 pagesBarsanti-Innes The Oncologist - 2016Liz BethNo ratings yet
- Updated Version: Mol Cancer TherDocument13 pagesUpdated Version: Mol Cancer TherSakshi IssarNo ratings yet
- Pembrolizumab For Previously TreatedDocument11 pagesPembrolizumab For Previously Treatedalex.losadaNo ratings yet
- Relapse Rates With Paliperidone Palmitate in AdultDocument11 pagesRelapse Rates With Paliperidone Palmitate in AdultdryaeonNo ratings yet
- DC Vaksin For GBM-Jurnal RevisiDocument8 pagesDC Vaksin For GBM-Jurnal Revisiallyssa rahmadittaNo ratings yet
- Emerging Trends at The Interface of Chemistry and Biology: Applications To The Design of Human TherapeuticsDocument11 pagesEmerging Trends at The Interface of Chemistry and Biology: Applications To The Design of Human TherapeuticssuryasanNo ratings yet
- Endpoints in Advanced Breast Cancer: Methodological Aspects & Clinical ImplicationsDocument6 pagesEndpoints in Advanced Breast Cancer: Methodological Aspects & Clinical ImplicationsJauhar FirdausNo ratings yet
- How Artificial Intelligence Could Redefine Clinical Trials in Cardiovascular Medicine: Lessons Learned From OncologyDocument6 pagesHow Artificial Intelligence Could Redefine Clinical Trials in Cardiovascular Medicine: Lessons Learned From OncologySAMUEL ESCARESNo ratings yet
- Modeling Cancer-Immune Responses To TherapyDocument18 pagesModeling Cancer-Immune Responses To TherapyCarolina RibeiroNo ratings yet
- DTH 14650Document19 pagesDTH 14650Evelyn LimNo ratings yet
- Nejme 1200409Document2 pagesNejme 1200409Arie Krisnayanti Ida AyuNo ratings yet
- The Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Document7 pagesThe Role of Automated Cytometry in The New Era of Cancer Immunotherapy (Review)Andrea SbranaNo ratings yet
- Vanco & Ag PK 2018Document35 pagesVanco & Ag PK 2018Nguyen GeenNo ratings yet
- Analytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitDocument14 pagesAnalytical Validation of A Novel UHPLC-MS MS Method For 19 Antibiotics Quantification in Plasma Implementation in A LC-MS MS KitngobaochanNo ratings yet
- Clinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot StudyDocument8 pagesClinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot Studyyafit_armon5854No ratings yet
- Bradley J Monk First Line Pembrolizumab ChemotherapyDocument9 pagesBradley J Monk First Line Pembrolizumab ChemotherapyRaúl DíazNo ratings yet
- Rates of Uptake of Novel Agents in CancerpdfDocument1 pageRates of Uptake of Novel Agents in CancerpdfmaleticjNo ratings yet
- Efficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesDocument11 pagesEfficacy, Safety, and Health-Related Quality of Life With Camrelizumab Plus Pemetrexed and Carboplatin As First-Line Treatment For Advanced Nonsquamous NSCLC With Brain MetastasesJOSE DIAZNo ratings yet
- An Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesDocument9 pagesAn Unbiased Oncology Compound Screen To Identify Novel Combination StrategiesBobNo ratings yet
- Dose Finding For New Vaccines: The Role For Immunostimulation/immunodynamic ModellingDocument14 pagesDose Finding For New Vaccines: The Role For Immunostimulation/immunodynamic ModellingKikyNo ratings yet
- The Titans Curse - Robert VendittiDocument134 pagesThe Titans Curse - Robert VendittimarianaqueirosluzNo ratings yet
- Written Report: Lydia Hall: Care, Cure, Core Nursing TheoryDocument12 pagesWritten Report: Lydia Hall: Care, Cure, Core Nursing TheoryAldrin Limcuando100% (1)
- Martin Luther King Jr. - A True Historical Examination. (N.D.) - Retrieved OctoberDocument5 pagesMartin Luther King Jr. - A True Historical Examination. (N.D.) - Retrieved Octoberapi-336574490No ratings yet
- Palm Oil MillDocument52 pagesPalm Oil MillengrsurifNo ratings yet
- Perfecto Floresca Vs Philex Mining CorporationDocument11 pagesPerfecto Floresca Vs Philex Mining CorporationDelsie FalculanNo ratings yet
- Bbyct 131 em 2024 MPDocument26 pagesBbyct 131 em 2024 MPDanish AfrozNo ratings yet
- Licensure Examination For TeachersDocument14 pagesLicensure Examination For Teachersonin saspaNo ratings yet
- LEGAL REASONING SKILLS ProjectDocument19 pagesLEGAL REASONING SKILLS ProjectShreya Ghosh DastidarNo ratings yet
- Solid Edge Mold ToolingDocument3 pagesSolid Edge Mold ToolingVetrivendhan SathiyamoorthyNo ratings yet
- Sample QuestionsDocument15 pagesSample QuestionsAnonymous MtKJkerbpUNo ratings yet
- LSM MockDocument5 pagesLSM MockKazi Rafsan NoorNo ratings yet
- Atr Summary Assignment 1Document6 pagesAtr Summary Assignment 1Livingstone OlekanmaNo ratings yet
- Ruq Abdominal PainDocument55 pagesRuq Abdominal PainriphqaNo ratings yet
- Social Work As A ProfessionDocument4 pagesSocial Work As A ProfessionIssa KhalidNo ratings yet
- (Download PDF) Deviance and Social Control A Sociological Perspective 2Nd Edition PDF Full Chapter PDFDocument53 pages(Download PDF) Deviance and Social Control A Sociological Perspective 2Nd Edition PDF Full Chapter PDFyoichiolanzo100% (9)
- In The District of Columbia Court of Appeals: Applicant, VDocument26 pagesIn The District of Columbia Court of Appeals: Applicant, VMartin AustermuhleNo ratings yet
- I Love Algorithms - Machine Learning CardsDocument6 pagesI Love Algorithms - Machine Learning CardsCarlos Manuel Ventura MatosNo ratings yet
- Before Reading: An Encyclopedia EntryDocument6 pagesBefore Reading: An Encyclopedia EntryĐào Nguyễn Duy TùngNo ratings yet
- Case Study 01 - Cincinnati ZooDocument3 pagesCase Study 01 - Cincinnati Zoononaddd1236hhNo ratings yet
- vịt batmanDocument14 pagesvịt batmanTú Lệ100% (1)
- Easy Chicken Satay With Peanut Chilli SauceDocument18 pagesEasy Chicken Satay With Peanut Chilli SauceCarina LopesNo ratings yet
- Group2 Non Executive ResultsDocument3 pagesGroup2 Non Executive ResultsGottimukkala MuralikrishnaNo ratings yet
- Synopsis Car Showroom ManagementDocument18 pagesSynopsis Car Showroom ManagementRaj Bangalore50% (4)
- Combichem: Centrifugal PumpsDocument8 pagesCombichem: Centrifugal PumpsrizkyNo ratings yet
- CAN LIN ProtocolDocument60 pagesCAN LIN ProtocolBrady BriffaNo ratings yet
- Final Artifact Management Theory IIDocument11 pagesFinal Artifact Management Theory IIapi-651643566No ratings yet
- HetzerDocument4 pagesHetzerGustavo Urueña ANo ratings yet
- Percakapan 1Document2 pagesPercakapan 1Legend AbadiNo ratings yet