Professional Documents
Culture Documents
Biochemistry & Pharmacology of Major Depressive Disorder (MDD)
Biochemistry & Pharmacology of Major Depressive Disorder (MDD)
Uploaded by
RPh Krishna Chandra JagritOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Biochemistry & Pharmacology of Major Depressive Disorder (MDD)
Biochemistry & Pharmacology of Major Depressive Disorder (MDD)
Uploaded by
RPh Krishna Chandra JagritCopyright:
Available Formats
Biochemistry & Pharmacology of major depressive disorder (MDD)
Facts
Prevalence = 12.7% in men, 21.3% in women Age on onset = 20-25y (has decreased over the past 2 decades) Can be life-threatening (suicide & anorexia) - 1 million suicides a year (& 10 million attempts) (Mann, 2003) - > 50% occur during an episode of depression - 15% of people with untreated depression die by their won hand (suicide) - treatment doesnt only improve quality of life, but also saves lives! Has huge economic costs - in USA = $43 billion per annum
Theories Strong genetic component (50% concordance MZ) Life stress is a major predictor of MDD Stress-diathesis models (favoured model) Biochemical theories of depression History The Ancient Greeks believed that depression was a result of an imbalance in the 4 humours; too much black bile (this is where the term melancholia comes from). Monoamine is a generic term for the The most common theory = Monoamine Theory neurotransmitters; It has shadowed various theories proposed, and Noradrenaline suggests that depression is caused by a deficit in NA (NA) and/or serotonin
Monoamine theory
Origin (Reviewed by McNeal & Cimbolic, 1986) 1950s Scientists were observing the effect of RESERPINE (drug) on behavioural and psychological effect of blood pressure (its an antihypertensive drug) - By chance, they noticed that it induced severe depressive reactions in normal patients (and precipitates depression in remitted patients) How does it work What they found is; reserpine causes vesicular leakage (damages the membrane) in the presynaptic membrane, so stores of NA and 5-HT are depleted What does that tell us If artificial depletion of NA and 5-HT induces a depressive like state, then it implies that depression itself is caused by a natural depletion in these resources!!!! Therefore, alleviating the symptoms should be achievable by restoring the neurotransmitter levels! Basically depression is caused by less NA and 5HT So increasing levels should cure it!
SUPPORT
Tyrosine MHPG
Dopa Dopamine
NA
Tryptophan 5-HIAA Basic
amino acid in your
5-hydroxytryptophan
Broke down by
5-HT
Metabolite = safe form of the AA, so it can be removed from
Biochemistry = Support Above is the metabolic processes involved in the synthesis and degradation of the neurotransmitters involved. IF (like hypothesised) depression is associated with lower than normal functioning of NA and 5-HT in the brain then there should be lower levels of their metabolite (their broken down components; MHPG &/or 5-HIAA) in blood, urine & CSF of depressed patients (compared to controls) McNeal &Cimbolic (1986) Findings = Hollister & Claghom a) Both are abnormally low in depressed patients (1993) b) 5-HT is particularly low in suicidal depression (5-HT is Fava & Kendler (2000) Mann (2003) associated with a disorder of impulse control)
What else do these findings tell us about the neurochemistry of depression? Depression can be cause be either NA or 5-HT (or both) Maas (1975) Depressed patients can be either normal OR below normal for NA function (*see later notes by Praag) Asberg et al. (1976) Depressed patients can be either normal OR below normal for 5-HT function This implies depression has (biochemical) sub-types Low NA or low 5-HT * Biochemical analysis could be used to confirm/refine diagnosis and aid targeted medication
First generation of antidepressants = Support In the late 50s, the first effective anti-depressant was discovered (by accident, and its mechanism was unknown) They were used because they worked, NOT because they knew how they were working! It was later found, that, the drugs were effective, as they were consistent with the monoamine theory, by increasing synaptic levels of NA and 5-HT by; Blocking degradation Monoamine oxidase Hollister & Claghem inhibitors (MAOI) block the degrading enzyme (MAO) so (1993) the effect of the neurotransmitter can continue
Schloss & Henn (2004)
Blocking the reuptake process Tricyclic antidepressants (TCA) block the reuptake process, so the neurotransmitter is still present in the synaptic cleft, to bind to the post0-synampitc membrane
Sooo Support so far Reserpine depletes NE & 5-HT stores = induces depression Spillman et al, (2001) Neumeister et al. Implies NA & 5-HT deficits cause depression (2004) Depression is associated with low NA & 5-HT, and their metabolites First generation anti-depressants alleviated the effects of depression = increase NA & 5-HT levels = therefore implying low levels causes the deficit itself Blocking the synthesis of NA or 5-HT leads to rapid relapse in patients
This begs the questions; Are both monoamines involved? Is one more important than the other? Are there two biochemical sub-types of depression?
Van Praag (1977) Sub-types Van Pragg extended Maas research (1975) in the possibility of sub-types of depression (* see above). He found that there were, apparently, two subgroups of depressed patients; 1. Patients normal in NA functioning (presumed deficit in 5-HT) (A) 2. Patients deficient in NA function (B) Furthermore, TCAs (Tricyclic antidepressants) vary in their effect on NA and 5-HT a. Amitriptyline (AMI) effective on 5-HT reuptake b. Desipramine (DES) effective on NA reuptake Praag tested both types of TCA on both groups of patients A = responded well to AMI, but not to DES B = responded well to DES, but not to AMI This therefore provides evidence for the division between the subtypes of depression Na deficient depression 5-HT deficient depression This is the story so far. BUT! Theres more
Beyond the first generation
The late 70s provided pressure to develop new antidepressants, this was due to; Treatment resistance in 30% of patients Therapeutic delay (effect of drugs takes about 3-4 weeks, and this needed to be reduced) Predictions were made on sub-types, which was gaining more and more opposition Side-effects MAOI (cheese effect) MAOIs inhibit the breakdown/metabolism (deamination) of dietary amines (eg/ tyramine) in the liver, so that they are not broken into safe components. This basically leaves poisonous acids in the body to circulate, and even cross the blood-brain barrier.
TCA these can cause sedation and cardiac arrests
Because of these problems, rational drug development proceded the first generation antidepressants;
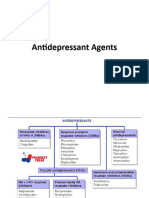
Second generation antidepressants
So how do they work Antidepressants work on either NA or 5-HT receptors; however, the effect they have on either is ultimately the same;
Hollister & Claghorn (1993), Eriksson (2000), Vetulani & Nalepa (2000), Wong & Licino (2001), Papakostas et al.
NA & 5-HT receptors are hypersensitive (Both pre(inhibitory autoreceptors) and post- synaptic receptors) NA pre = 2 & post = 5-HT pre = 5-HT1A & post = 5-HT2A The latter is a consequence of the former; Pre-synaptic auto-receptors remove neurotransmitters too quickly = very little in the cleft = depriving the post-synaptic receptor = they too become hypersensitive Antidepressants normalize the levels of the neurotransmitter levels in the cleft, desensitizing both lots of receptors, so normal levels of the neurotransmitter can be released naturally. The different drugs create this effect in different ways; NA reuptake inhibitors - NARI (eg/ Maprotiline) 5-HT reuptake inhibitors - SSRI (eg/ Fluoxetine (Prozac)) MAO-A inhibitors (eg/ moclobemide) NA/5-HT reuptake inhibitors - SNRI (eg/ venlafaxine) less side effects! Atypical antidepressants (eg/ mianserin, trazodone) dont prevent reuptake or degradation
* For a diagrammatic version, see the next handout!
Evaluation Generally better, as theyre based on understanding, not trial and error NARI and SSRIs have equal effectiveness This therefore questioned the idea of a subtype previously proposed! Fewer and less serious side-effects
Some other stuff Therapeutic delay Antidepressants take approximately 3-4 weeks to begin to take effect. Antidepressants would be much more effective if the therapeutic delay was reduced. With SSRIs (5-HT orientated Antidepressants), the therapeutic delay is due to the initial low 5-HT release, because 5-HT1a receptors have already been activated to initiate the negative feedback. (this can actually cause symptoms to be worse in the early stages of treatment) This is where the 3-4 week delay comes from Reducing the therapeutic delay Pindolol is a drug that blocks (antagonistic) the 5-HT1A receptors, so that the negative feedback system wont be initiated, and so normal levels of 5-HT will be released. By combining this drug with SSRI drugs, the therapeutic delay should be reduced
Perez et al. (1999) & Artigas et al (2001) = confirmed a significantly faster therapeutic response (days in contrast to weeks) when the two were combined = pinolol augmentation therapy
What causes the initial hypersensitivity of NA and 5-HT receptors? Genetic abnormality - Kendler et al. (1996) Stress and failure to cope - Nemeroff (1998) Stress is a strong predictor of MDD MDD is associated with hypercortisolaemia When we are stressed, our hypothalamic-pituitary-adrenal (HPA) axis is triggered, which indirectly causes cortisol to be secreted In acute stress, negative feedback prevents cortisol levels rising too high, but in prolonged/chronic stress, negative feedback is disrupted (Seyle, 1950s) Therefore, there is constant activation of the HPA axis and brains GR receptors. This causes the GR receptors to desensitize, so their negative feedback on the HPA is reduced resulting in high levels of cortisol, ultimately affecting the sensitivity of NA and 5-HT receptors while also causing atrophy and cell death Atrophy is commonly found in the temporal lobes (eg/ hippocampus) Auer et al (2005) Damage to the hippocampus is associated with the memory loss experienced by many depressed patients Loss of gray matter in the temporal lobe is associated with impairments in planning and motivation Therapeutic implications hypercortisolaemia may be a primary biological dysfunction (system coping failure). So reducing HPA hyperactivity may have a therapeutic value Blocking CFR receptors (Zobel et al., 2000) Blocking cortisol receptors (Belanoff et al., 2001) Criticism Not everyone who is stressed become depressed Stress diathesis (interaction) - Caspi et al. (2003); Heim et al. (2004); Taylor et al. (2006) Alleles (Caspi et al., 2003) Deficient 5-HT levels is possibly due to malfunctioning 5-HT transporter cells 5-HT transporter (5-HTT) gene exists in several forms (short and long) SHORT allele = more likely to react to stress with depressive behaviours Future directions Dopamine as recently stepped into the lime light (it is also a monamine) Dopamine is a major neurotransmitter in pleasure/reward, as well as anhedonia (obviously a major factor in depression) by using DA in treatment patients pleasure may be increased, potentially reducing the therapeutic delay!
Diagram page!!!!!
(I hope this makes it a bit easier!) Noradrenaline
Normal NA is released from the presynaptic membrane, into the cleft, where it binds to
-receptors. Once the message has been sent; NA transporter molecules remove excess NA from the cleft 2-receptors govern a negative feedback system, so detection of high concentrations of NA causes the neurotransmitter to stop being released Deprssion 2 receptors are hypersensitive, so negative feedback kicks in too soon. Therefore, less NA is released Because less NA is released, the -receptors become hypersensitive Antidepressants 2 receptors are desensitized NA release is normalized Therefore, -receptors desensitized (as they are exposed of normal NA levels) * Atypical antidepressants (mianserin) blocks 2 receptors, which also normalizes the NA release Basically the same story
Seratonin
Normal 5-HT is released from the presynaptic membrane 5-HT transporter molecules remove excess autoreceptors govern a negative feedback system Deprssion 5-HT1A receptors are hypersensitive, so negative feedback kicks in too soon = less 5-HT Causing the 5-HT2A to become hypersensitive Antidepressants 5-HT1A receptors are desensitized 5-HT release is normalized 5-HT2A desensitized
Gauntlet believed that depression is fundamentally a seratonin deficit (Blier & DeMontigny (1994): every known antidepressant drug (&ECT) increases 5-HT function in the brain) ** The time scale of this maps on well to the therapeutic delay!!!!!
You might also like
- Krav Maga Pressure Points - Military Hand To Hand Combat GuideDocument27 pagesKrav Maga Pressure Points - Military Hand To Hand Combat Guidebrogan98% (135)
- Psychopharmacology 2 AntidepressantsDocument7 pagesPsychopharmacology 2 AntidepressantsBea Samonte100% (2)
- Ziva Meditation Ebook PDFDocument33 pagesZiva Meditation Ebook PDFneeta50% (4)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- NURSING CARE PLAN - Breast CancerDocument2 pagesNURSING CARE PLAN - Breast Cancerderic100% (3)
- Chapter 21 Antidepressant AgentsDocument4 pagesChapter 21 Antidepressant AgentsNicolle Lisay IlaganNo ratings yet
- Mantras - English - KundaliniDocument7 pagesMantras - English - KundaliniRPh Krishna Chandra JagritNo ratings yet
- Halberstein - 2005 - Annals of Epidemiology PDFDocument14 pagesHalberstein - 2005 - Annals of Epidemiology PDFWindhy HaningNo ratings yet
- Skimming and Scanning QuizDocument15 pagesSkimming and Scanning Quizeagle777jay0% (1)
- 11 Chapter 2Document8 pages11 Chapter 2Muhammad Tariq RazaNo ratings yet
- 15Document36 pages15michelleNo ratings yet
- Slides Mood DisordersDocument15 pagesSlides Mood DisordersEesha TahirNo ratings yet
- Antidepressant Drugs: Presented By-K.Vinod Dept. of PharmacologyDocument38 pagesAntidepressant Drugs: Presented By-K.Vinod Dept. of PharmacologyVinod GuruNo ratings yet
- Pharmacology of Mood Stabilizers: DR - Datten Bangun, MSC, SPFK Dept - Farmakologi & Terapetik Fak - Kedokteran Uhn MedanDocument51 pagesPharmacology of Mood Stabilizers: DR - Datten Bangun, MSC, SPFK Dept - Farmakologi & Terapetik Fak - Kedokteran Uhn MedanFansisca SiallaganNo ratings yet
- Biology of DepressionDocument5 pagesBiology of DepressionScience RespondsNo ratings yet
- AntidepressantsDocument36 pagesAntidepressantsLloyd Daniel BarrantesNo ratings yet
- "Serotonin Syndrome Causes HARM": Psychiatry PharamacologyDocument9 pages"Serotonin Syndrome Causes HARM": Psychiatry Pharamacologytycobb63100% (4)
- Antidepressants (ME216) 20 5Document40 pagesAntidepressants (ME216) 20 5Dineish MurugaiahNo ratings yet
- Lecture 2 (Psychotropic Drugs)Document17 pagesLecture 2 (Psychotropic Drugs)ahmadslayman1No ratings yet
- Class 1 Antidepressents 2020Document21 pagesClass 1 Antidepressents 2020Arafat 039No ratings yet
- Antidepressent (AutoRecovered)Document11 pagesAntidepressent (AutoRecovered)chakdiva11No ratings yet
- Inhibidores Recep Serotonina 2Document14 pagesInhibidores Recep Serotonina 2FarmaFMNo ratings yet
- Antidepressants AntidepressantsDocument38 pagesAntidepressants AntidepressantsjaneNo ratings yet
- Depression: Types Symptoms Diagnosis Causes TreatmentDocument32 pagesDepression: Types Symptoms Diagnosis Causes TreatmentThea MallariNo ratings yet
- Name: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicDocument16 pagesName: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of Submission: TopicAnoosha FarooquiNo ratings yet
- Pharmacology 402 February 24, 2010 Mark Hamblin, MD, PHDDocument54 pagesPharmacology 402 February 24, 2010 Mark Hamblin, MD, PHDKarmila Novianti100% (1)
- Anti-Depressants: Bitek BrianDocument28 pagesAnti-Depressants: Bitek BrianMwanja MosesNo ratings yet
- Depression: Psychiatric DisordersDocument21 pagesDepression: Psychiatric DisordersNdoo NdooNo ratings yet
- Antidepressants: Samaiya Mushtaq CHEM 5398Document33 pagesAntidepressants: Samaiya Mushtaq CHEM 5398Renuga DeviNo ratings yet
- Extrapyramidal SymptomsDocument5 pagesExtrapyramidal SymptomsGenette Sy SolisNo ratings yet
- Artigo Fisiopato DepressãoDocument21 pagesArtigo Fisiopato DepressãoJ VichhyNo ratings yet
- Transmitters and Disorders HandoutDocument3 pagesTransmitters and Disorders HandoutfrazzycakebossNo ratings yet
- Treatment of Depressive DisordersDocument96 pagesTreatment of Depressive DisordersAbelNo ratings yet
- Neurobiologi Depresi 2000 WFDocument6 pagesNeurobiologi Depresi 2000 WFKim AntelNo ratings yet
- AntidepressantsDocument28 pagesAntidepressantsakoeljames8543No ratings yet
- W3 Bipolar Disorder. Therapies. T2 2022-23Document41 pagesW3 Bipolar Disorder. Therapies. T2 2022-23Nayanaa VarsaaleNo ratings yet
- Slides SchizophreniaDocument28 pagesSlides SchizophreniaEesha TahirNo ratings yet
- Chapter 46 - 50Document74 pagesChapter 46 - 50mer12sswNo ratings yet
- Biological FactorsDocument3 pagesBiological FactorsDEEPIKA PREMLAL 2170101No ratings yet
- Antidepressant DrugsDocument55 pagesAntidepressant Drugsmaheen aurangzaib100% (2)
- Antidepressants AntianxietyDocument95 pagesAntidepressants AntianxietyCharles YiuNo ratings yet
- B2B Psychopharmacology 2015Document128 pagesB2B Psychopharmacology 2015Soleil DaddouNo ratings yet
- Depressive - EtiologyDocument35 pagesDepressive - EtiologygunjaNo ratings yet
- Antidepressant DrugsDocument47 pagesAntidepressant DrugsOjambo Flavia75% (4)
- Antidepressants and Treatment of Mood DisordersDocument24 pagesAntidepressants and Treatment of Mood DisordersFuad HadiNo ratings yet
- InsomniaDocument3 pagesInsomniaYudi MahardikaNo ratings yet
- Antidepressants ChristianDocument37 pagesAntidepressants ChristianciaranNo ratings yet
- Clinical PharmacologyDocument29 pagesClinical PharmacologyBilal KhanNo ratings yet
- Antidepressant DrugsDocument15 pagesAntidepressant DrugsDr. Mushfique Imtiaz ChowdhuryNo ratings yet
- Depression Theory PDFDocument2 pagesDepression Theory PDFdonkeyendutNo ratings yet
- Biological Therapies For Depression: Ask YourselfDocument6 pagesBiological Therapies For Depression: Ask YourselfAnni Christoforou100% (1)
- Antidepressant AgentsDocument45 pagesAntidepressant Agentsmadeha goharNo ratings yet
- AntidepressantsDocument59 pagesAntidepressantsanon_189054600100% (2)
- DepressionDocument26 pagesDepressionkanwalsweetNo ratings yet
- L7-Depression and BipolarDocument36 pagesL7-Depression and Bipolar120420314No ratings yet
- Antidepreesent AgentsDocument34 pagesAntidepreesent Agentsmaryamkefahn2003No ratings yet
- The PSYCH MAP ColoredDocument2 pagesThe PSYCH MAP Coloredcentrino17No ratings yet
- 3 Anti-Depressant DrugsDocument30 pages3 Anti-Depressant DrugsAjigotto ubiq.No ratings yet
- HypothesisDocument2 pagesHypothesisJomana MacalnasNo ratings yet
- WahabDocument7 pagesWahabwahabahmad4604No ratings yet
- Lecture 7bDocument8 pagesLecture 7bBetty MaiNo ratings yet
- The Nervous System: Blood Brain BarrierDocument17 pagesThe Nervous System: Blood Brain BarrierSuleiman AbdallahNo ratings yet
- Anti Depressants 2Document24 pagesAnti Depressants 2Ayesha AyeshaNo ratings yet
- Antidepressants Ssris, Snris: Selective Serotonin Reuptake Inhibitors Norepinephrine Reuptake InhibitorsDocument23 pagesAntidepressants Ssris, Snris: Selective Serotonin Reuptake Inhibitors Norepinephrine Reuptake InhibitorsJosh SchultzNo ratings yet
- Michelle Gillis - Phenylethylamine: More Than Just A Pea-Sized NeurochemicalDocument3 pagesMichelle Gillis - Phenylethylamine: More Than Just A Pea-Sized NeurochemicalNeerFamNo ratings yet
- نسخة ANTI-ARRHYTHMIC 2Document28 pagesنسخة ANTI-ARRHYTHMIC 2ManWol JangNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- About MeningiomaDocument5 pagesAbout MeningiomaRPh Krishna Chandra JagritNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- HTML-XHTML Tag SheDocument6 pagesHTML-XHTML Tag SheabcjohnNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- About This Tutorial: Version HistoryDocument328 pagesAbout This Tutorial: Version HistoryKate CorralesNo ratings yet
- MantrasDocument24 pagesMantrasg_gaurishankar@rediffmail.com100% (4)
- Super Fast Mental Math - Vedic Math HistoryDocument51 pagesSuper Fast Mental Math - Vedic Math Historyvedicmath98% (42)
- Martial Arts - Bruce Lee's Training SecretsDocument3 pagesMartial Arts - Bruce Lee's Training Secretsbrogan91% (34)
- Martial Arts - Bruce Lee's Speed TrainingDocument4 pagesMartial Arts - Bruce Lee's Speed Trainingbrogan97% (33)
- Web DesigningDocument638 pagesWeb DesigningRPh Krishna Chandra JagritNo ratings yet
- Math Olympiad Problems Collection-V1Document97 pagesMath Olympiad Problems Collection-V1RPh Krishna Chandra Jagrit100% (1)
- Tally 9.2 NotesDocument1,918 pagesTally 9.2 NotesRamesh80% (5)
- Introduction in Human AnatomyDocument60 pagesIntroduction in Human AnatomyRPh Krishna Chandra JagritNo ratings yet
- Medicinal PlantsDocument29 pagesMedicinal PlantsGANESH KUMAR JELLANo ratings yet
- General KnowledgeDocument141 pagesGeneral KnowledgeRAVI KUMAR83% (12)
- General Pharmacology MCQDocument6 pagesGeneral Pharmacology MCQShrikant ThakurNo ratings yet
- Curriculum VitaeDocument2 pagesCurriculum VitaeRPh Krishna Chandra JagritNo ratings yet
- Aspire Products, The Makers of EMST150, Announces A New & Improved WebsiteDocument2 pagesAspire Products, The Makers of EMST150, Announces A New & Improved WebsiteAlexandra HartNo ratings yet
- Romsons All ProductDocument53 pagesRomsons All ProductBoyke WinterbergNo ratings yet
- Acupuncture For BurnsDocument34 pagesAcupuncture For BurnsIvonne Flores FernándezNo ratings yet
- Contact Dermatitis Guidelines 2017Document13 pagesContact Dermatitis Guidelines 2017Imam Muhamad RissandyNo ratings yet
- Anaesthesia - 2021 - Feray - PROSPECT Guidelines For Video Assisted Thoracoscopic Surgery A Systematic Review andDocument15 pagesAnaesthesia - 2021 - Feray - PROSPECT Guidelines For Video Assisted Thoracoscopic Surgery A Systematic Review andboby abdul rahmanNo ratings yet
- Evolution Occlusion and Occlusal Instruments: AcademicsDocument11 pagesEvolution Occlusion and Occlusal Instruments: AcademicsMelissa Perez GuerreroNo ratings yet
- Diclofenac: Mechanism of ActionDocument7 pagesDiclofenac: Mechanism of ActionaditNo ratings yet
- J 1600-0757 1998 tb00129 PDFDocument6 pagesJ 1600-0757 1998 tb00129 PDFdwinugrohojuandaNo ratings yet
- My - Lectures.Updated - II 2015Document137 pagesMy - Lectures.Updated - II 2015prasadmvk100% (1)
- Cerenia Combo PI May2012Document2 pagesCerenia Combo PI May2012wvhvet100% (1)
- Antalya Medical Tourism Guide 2014Document59 pagesAntalya Medical Tourism Guide 2014pilgrim13No ratings yet
- Basic Foundation of Iv TherapyDocument10 pagesBasic Foundation of Iv Therapyjanna mae patriarcaNo ratings yet
- AcsDocument103 pagesAcsVikrant WankhedeNo ratings yet
- Nephrology Curriculum - الزمالة المصرية للكليDocument60 pagesNephrology Curriculum - الزمالة المصرية للكليbook1man100% (1)
- Curriculum Vitae: 1. Personal Details: Ms. Jayanthi.JDocument6 pagesCurriculum Vitae: 1. Personal Details: Ms. Jayanthi.JRadha ThangamNo ratings yet
- Immunotherapy Post TransplantDocument12 pagesImmunotherapy Post TransplantaymenNo ratings yet
- Humms 11 Pasay Diass s2 q1 w4Document20 pagesHumms 11 Pasay Diass s2 q1 w4Victoria De Los SantosNo ratings yet
- Thoma 2015Document39 pagesThoma 2015Izabella de LimaNo ratings yet
- MCQ PneuDocument60 pagesMCQ PneuYanesh Bishundat0% (1)
- Azithromycin in PediatricsDocument40 pagesAzithromycin in PediatricsKishore ChandkiNo ratings yet
- HPLP II-English VersionDocument3 pagesHPLP II-English VersionGarr LordemadNo ratings yet
- Cyst and Cystlike Lung LesionsDocument57 pagesCyst and Cystlike Lung LesionsAna StankovicNo ratings yet
- Enrofloxacin: Therapeutic ReviewDocument4 pagesEnrofloxacin: Therapeutic ReviewAndi Dytha Pramitha SamNo ratings yet
- RADIOLOGYDocument3 pagesRADIOLOGYwendy carinoNo ratings yet
- An Introduction To Grounding: The Healing Chalet in The WoodsDocument7 pagesAn Introduction To Grounding: The Healing Chalet in The Woodse.j.wardNo ratings yet