Professional Documents
Culture Documents
Semester 2 Drug List
Semester 2 Drug List
Uploaded by
Nam_Pham_6481Copyright:
Available Formats
You might also like
- PSY 441 Global Psychology PrePost Test National UniversityDocument7 pagesPSY 441 Global Psychology PrePost Test National UniversityTammy Smith67% (3)
- Pharmacology Main DrugsDocument14 pagesPharmacology Main DrugsSabir KhanNo ratings yet
- Lowenthal - The Crimes of Fascist Occupants and Their Collaborators Against The Jews of Yugoslavia (Balkan Holocaust in WW2) (1957)Document299 pagesLowenthal - The Crimes of Fascist Occupants and Their Collaborators Against The Jews of Yugoslavia (Balkan Holocaust in WW2) (1957)Testerasa TesterNo ratings yet
- FortiAnalyzer 6.0 Study Guide-Online PDFDocument253 pagesFortiAnalyzer 6.0 Study Guide-Online PDFDavid50% (2)
- Emg 2303 NotesDocument65 pagesEmg 2303 NotesAnonymous UnchpksNo ratings yet
- Genitourinary System: Renal FailureDocument6 pagesGenitourinary System: Renal FailureEn ConejosNo ratings yet
- Gyneacology Revision by All TeamDocument14 pagesGyneacology Revision by All TeamSara EhabNo ratings yet
- A Bunch of Pharm ShitDocument2 pagesA Bunch of Pharm ShitkatNo ratings yet
- Tumor Immunology: I. Common Tumor MarkersDocument2 pagesTumor Immunology: I. Common Tumor MarkersDivineGloryMalbuyoNo ratings yet
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Present at 4-12 Months, Development Arrest From Pre-B To BDocument2 pagesPresent at 4-12 Months, Development Arrest From Pre-B To BWaoNo ratings yet
- Differential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersDocument3 pagesDifferential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersNurhayati HasanahNo ratings yet
- Abdo Exam TableDocument2 pagesAbdo Exam Tableapi-195986134No ratings yet
- Antimycobacterial Drugs PDFDocument3 pagesAntimycobacterial Drugs PDFCas BuNo ratings yet
- The Better You Get at Something, The More Enjoyable It Can BecomeDocument6 pagesThe Better You Get at Something, The More Enjoyable It Can BecomeAshNo ratings yet
- Drug CardsDocument3 pagesDrug CardsDave HillNo ratings yet
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocument19 pagesNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- Salmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersDocument8 pagesSalmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersNatalia_WiryantoNo ratings yet
- Bio Chem 1Document5 pagesBio Chem 1Reynaldo RiveraNo ratings yet
- Precipitating Factors:: Myocardial Cell Death (NecrosisDocument2 pagesPrecipitating Factors:: Myocardial Cell Death (NecrosisLean Ashly MacarubboNo ratings yet
- CVR PharmacologyDocument6 pagesCVR PharmacologyRebecca MarshallNo ratings yet
- Handouts Integumentary Sys Sp11 B201Document7 pagesHandouts Integumentary Sys Sp11 B201Kelly TrainorNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- Acid BaseDocument1 pageAcid BasesccctutorNo ratings yet
- Diseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality DiseaseDocument7 pagesDiseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality Diseasenreena aslamNo ratings yet
- Ultimate Pharm GuideDocument41 pagesUltimate Pharm GuideeanguyenNo ratings yet
- MC Tumor MC Ca MC 1° Ca BrainDocument12 pagesMC Tumor MC Ca MC 1° Ca BrainRyan TurnerNo ratings yet
- Dysrhythmias: Cardiac Conduction System Rhythm Strip RecognitionDocument5 pagesDysrhythmias: Cardiac Conduction System Rhythm Strip Recognitiontantalizin marieNo ratings yet
- Common Medications UsedDocument3 pagesCommon Medications UsedRay Michael CasupananNo ratings yet
- Complement SystemDocument4 pagesComplement SystemFait HeeNo ratings yet
- Antibiotics in ActionDocument1 pageAntibiotics in Actionjuan esteban MonroyNo ratings yet
- Kidney NewDocument4 pagesKidney NewParth BhayanaNo ratings yet
- Med CardsDocument4 pagesMed CardsSonia FernandesNo ratings yet
- SketchyPath ChecklistDocument1 pageSketchyPath ChecklistFajar Raza100% (1)
- Low BP - Decreased Cardiac Output - Improved Renal Blood FlowDocument2 pagesLow BP - Decreased Cardiac Output - Improved Renal Blood Flowtantalizin marieNo ratings yet
- Lippincott Illustrated Reviews (PDFDrive) - Pages-396Document1 pageLippincott Illustrated Reviews (PDFDrive) - Pages-396Eman ShalabyNo ratings yet
- Abnormal LFTsDocument2 pagesAbnormal LFTsRenu RosyNo ratings yet
- 1 Ge Stimulations Mast Cell Degeneration Asthma AttackDocument4 pages1 Ge Stimulations Mast Cell Degeneration Asthma Attacknebbie06No ratings yet
- CHEM-Year 2 Chemistry Cheat Sheet For EDEXCELDocument12 pagesCHEM-Year 2 Chemistry Cheat Sheet For EDEXCELraiabhijith586No ratings yet
- Organism Description Drug of ChoiceDocument14 pagesOrganism Description Drug of ChoiceMary YongcoNo ratings yet
- Antifungal Agents: EchinocandinsDocument2 pagesAntifungal Agents: EchinocandinsCourtney TownsendNo ratings yet
- Drugs World: Anti-PsychoticsDocument1 pageDrugs World: Anti-Psychoticsapi-26228251No ratings yet
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- Hi Stop Hath Ology 2Document22 pagesHi Stop Hath Ology 2vivek govardhanamNo ratings yet
- STEP 1 ChecklistDocument11 pagesSTEP 1 ChecklistHasan Khan RoudbaryNo ratings yet
- Anatomy - UPPER LIMB - 3 Muscles, Innervation and Compartments of The Upper Limb PDFDocument20 pagesAnatomy - UPPER LIMB - 3 Muscles, Innervation and Compartments of The Upper Limb PDFDr Ahmed NabilNo ratings yet
- Poliomyelitis Haemophilus Influenzae Type B VariecellaDocument4 pagesPoliomyelitis Haemophilus Influenzae Type B VariecellaJeanna Chong100% (1)
- Neisseria Meningitidis Strep Pneumoniae E. ColiDocument3 pagesNeisseria Meningitidis Strep Pneumoniae E. ColiÐr SalmaNo ratings yet
- Mean Standard Deviation: Antonio Mirano - 2018Document8 pagesMean Standard Deviation: Antonio Mirano - 2018jNo ratings yet
- Ekg Full BibleDocument6 pagesEkg Full BibleTJNo ratings yet
- MnemonicsDocument3 pagesMnemonicsXyzhie McCrudenNo ratings yet
- Concept Map Et Al 11-04-15Document7 pagesConcept Map Et Al 11-04-15api-353656227No ratings yet
- Poison & Antidote Chart IWK Regional Poison Cen PDFDocument1 pagePoison & Antidote Chart IWK Regional Poison Cen PDFdeeptiNo ratings yet
- ECG Demographics Rate: 300/# Large Box in RR IntervalDocument11 pagesECG Demographics Rate: 300/# Large Box in RR IntervalJonathan DavisNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Disorders of The BoneDocument2 pagesDisorders of The BoneRPh Krishna Chandra JagritNo ratings yet
- Electrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionDocument6 pagesElectrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionmkninnyNo ratings yet
- Abg InterpretationDocument1 pageAbg InterpretationPrincess EspadaNo ratings yet
- Zyloprim Drug CardDocument1 pageZyloprim Drug CardSheri490No ratings yet
- Classification of Drugs NewDocument15 pagesClassification of Drugs NewAbdul SamadNo ratings yet
- Children's Respiratory NursingFrom EverandChildren's Respiratory NursingJanice MightenNo ratings yet
- 99 Names of Allah SWT and Mohammed (PBUH)Document11 pages99 Names of Allah SWT and Mohammed (PBUH)api-26870382100% (1)
- Chapter 7 Fiduciary RelationshipDocument18 pagesChapter 7 Fiduciary RelationshipMarianne BautistaNo ratings yet
- Application Activity: Giving BackDocument3 pagesApplication Activity: Giving BackHillary Anne BautistaNo ratings yet
- Description: P Ack AgeDocument3 pagesDescription: P Ack AgeAlexandru CioponeaNo ratings yet
- Registers and StatementsDocument7 pagesRegisters and StatementsspiceshivNo ratings yet
- Assignment 1Document3 pagesAssignment 1Hafez MohammedNo ratings yet
- Jadual Alimah 2021.V3Document6 pagesJadual Alimah 2021.V3maryam cookNo ratings yet
- Microsoft Word - Muffovan-DatasheetEN - 16 - v2Document2 pagesMicrosoft Word - Muffovan-DatasheetEN - 16 - v2Uswatul HasanahNo ratings yet
- Asd Wei Gang Tuo 10 PDFDocument2 pagesAsd Wei Gang Tuo 10 PDFEagle EyeNo ratings yet
- WLC UpgradeDocument13 pagesWLC Upgradeapi-3703368No ratings yet
- Geronimo StiltonDocument2 pagesGeronimo StiltonRajeshNo ratings yet
- PRM AnswerDocument28 pagesPRM AnswerMinh TrangNo ratings yet
- Vocabulary + Grammar Unit 3 Test ADocument3 pagesVocabulary + Grammar Unit 3 Test AJoana FernandesNo ratings yet
- The Crucial Difference Between Creativity and InnovationDocument14 pagesThe Crucial Difference Between Creativity and InnovationTamara KlicekNo ratings yet
- Signed Off Understanding Culture11 q1 m2 Defining Culture and Politics v3 RemovedDocument24 pagesSigned Off Understanding Culture11 q1 m2 Defining Culture and Politics v3 Removedrhaybien vinluanNo ratings yet
- (Lesson2) Cultural, Social, and Political Institutions: Kinship, Marriage, and The HouseholdDocument5 pages(Lesson2) Cultural, Social, and Political Institutions: Kinship, Marriage, and The HouseholdPlat JusticeNo ratings yet
- Concerto in C Minor - Johann Christian Bach - CelloDocument24 pagesConcerto in C Minor - Johann Christian Bach - CellojosianeNo ratings yet
- Step 7 Err Code125936644Document37 pagesStep 7 Err Code125936644mohammadNo ratings yet
- Managerial EconomicsDocument15 pagesManagerial EconomicsAditi WaliaNo ratings yet
- Leadership Styles For 5 StagesDocument18 pagesLeadership Styles For 5 Stagesbimal.greenroadNo ratings yet
- Thou Shall Not StealDocument4 pagesThou Shall Not StealGiselle MarNo ratings yet
- Crowdfunding For Research: A Case Study in Research Management Centre in MalaysiaDocument8 pagesCrowdfunding For Research: A Case Study in Research Management Centre in MalaysiaCk WongNo ratings yet
- The Passion of Jesus Christ: BY Saint Alphonsus de LiguoriDocument67 pagesThe Passion of Jesus Christ: BY Saint Alphonsus de Liguorisatya0988No ratings yet
- Sustainable Project ManagementDocument4 pagesSustainable Project ManagementafirulNo ratings yet
- CFX-Intro 17.0 Lecture07 MovingZonesDocument41 pagesCFX-Intro 17.0 Lecture07 MovingZonesFabiano LebkuchenNo ratings yet
- Chakra Stones Cheat SheetDocument1 pageChakra Stones Cheat SheetamjohnpeterNo ratings yet
Semester 2 Drug List
Semester 2 Drug List
Uploaded by
Nam_Pham_6481Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Semester 2 Drug List
Semester 2 Drug List
Uploaded by
Nam_Pham_6481Copyright:
Available Formats
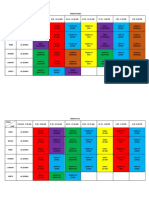
Drug Class
Drug Name
Enalapril, Captopril
MOA
- block conversion of angiotensin I to angiotensin II - block degradation of bradykinin - blockage of ATII reduction in vasoconstriction, Na+ retention and aldosterone release - AT1 receptors constriction - AT2 receptors vasodilation - blocks AT1 block vasoconstriction, block aldosterone release and Na+ reabsorption, bradykinin breakdown not inhibited - mech 1: diuretic that decrease blood vol and TPR - mech 2: decrease TPR by modulating activity of K+ channels in arterioles
Uses
Side Effects
- first dose effect steep fall in BP (susceptible to volume depleted patients - hyperkalaemia - dry cough - oedema - taste disturbance - dizziness - headache - hyperkalaemia - first dose hypotension - Li+ toxicity - hypokalaemia - metabolic alkalosis - dizziness, weakness, muscle cramps, hypotension, hypercalcaemia - hypercalcaemia - hyperuricaemia - adverse lipid profile effect -erectile dysfunction
Miscellaneous info
- need to stop K+ supplements - temp stop of diuretics - start therapy on low dose - check renal function C/I pregnancy and renal artery stenosis - interact with diuretics, NSAIDs, Li+ toxicity risks - K+ sparing diuretics may increase risk of hyperkalaemia - thiazides plateau in BP treatment i.e. increasing thiazide dose beyond threshold will not change BP but side effects will continue to increase - thiazide and ACEI have additive effects
Anti-hypertensives
- anti-hypertension - recomm. For patients with heart failure and for diabetics with proteinuria
ACEI (-pril)
ATII receptor antags (sartan)
Losartan, Irbesartan, Candesartan, Telmisartan Bendrofluazide, Hydrochlorthiazid e
- anti hypertensives - better than ACEI due to selectivity for AT1 as ACEI stops AT production hence not ATII action - anti-hypertensive
Thiazides
K+ sparing diuretics
Amiloride Triamterene (both avail in combo with hydrochlorothiazi de) Spironolactone
- block Na+ channels in distal tubules no Na+/K+ exchange K+ excretion reduced
- anti-hypertensive
Aldosterone antag Propranolol and Metopolol both lipid soluble Atenolol less lipid soluble Carvedilol mixed 1 blocking ability Dihydropyridines : nifedipine, amlodipine, Benzothiazepines : diltiazem Phenylalkylamine s: verapamil
- aldosterone antagonist - competes with aldosterone for receptors in distal tubule
- anti-hypertensive
-blockers (olol)
- acts on 1 - -ve inotropic and chronotropic effects decrease CO and HR - acts in CNS to decrease sym outflow - reduce renin production in kidney - blocks pre-synaptic which would facilitate NA release to decrease BP - block Ca2+ channel relax vascular SMM decrease peripheral vascular resistance decrease BP - dihydropyridines: most vascular selective - benzothiazepines: acts on cardiac + vascular SMM - phenylalkylamines: greater cardiac effects
- anti-hypertensive vasodilation
- endocrine adverse effect gynecomastia, menstural abnormalities - due to aldosterone being secreted from adrenal cortex - heart failure - bradycardia - bronchospasm - peripheral vascular disease - CNS effects (lipid soluble) i.e. dizziness, nightmares, depression
Ca2+ blocker (dipine)
- for cardiac decompensation - cardiac decompensation: inability of heart to maintain adequate circulation
- headache - flushing - postural hypotension - chest pain due to HR increase to compensate for sudden drop in BP - bleeding gums - oedema
- no reflex increase in peripheral vascular resistance - C/I in asthmatics, heart block, peripheral vascular disease, hyperlipidaemia, diabetes - effective for Caucasians, myocardial infarct, ischaemia, angina, phaechromocytoma - can be sued in combo with blocker to prevent reflex tachycardia - not good for Africans - patients with diabetes or hyperlipidaemia no metabolic effects
Drug Class
Drug Name
MOA
Uses
Side Effects
Miscellaneous info
1 selective blockers
Doxazosin, Prazosin, Terazosin
- block 1 post synaptic in arteries and veins vasodilation decrease peripheral vascular resistance - does not block 2 feedback inhibition of NA can still occur reflex tachycardia unlikely to occur - H1 receptors contraction of gut and airways; vasodilation
- asthmatics - patients with peripheral vascular disease, hyperlipidaemia, prostate symptoms, impotence
dizziness postural hypotension nasal congestion headaches weakness, fatigue, drowsiness stress incontinence in women
- first dose hypotension - withhold diuretic before starting blocker
Autacoids
H1 antag Mepyramine, terfenidine, fexofenadine, loratadine, promethazine Cimetidine, Ranitidine, famotidine, nizatidine Buspirone (5HT1A) Sumatriptan (5HT1B/D) - sedative: from histaminergic neurones from hypothalamus - atropinic effects - anti-emetic effect through vomiting centre - peptic ulcer - non-sedating anti-his have potentially fatal tachycardia - terf, fexo and lora nonsedating anti-histamine dont pass BBB
H2 antag
- competitive antag - inhibit ACh, gastrin and histamine induced acid secretion - decreases 5-HT from tryptaminergic nerves by action on auto-receptor - abnormal discharge from brainstem causes 5HT release transgeminal nerve activation SP release vasodilation and oedema of blood vessels - sumatriptan acts directly on blood vessels to cause constriction
- reduce anxiety - decrease aggression - migraine - cerebral vasoconstrictor
5-HT agonist
- dizziness, flushing, weakness, fatigue - maybe nausea and vomiting - pain or sensations may be caused by vasospasms
- non-sedating - no addictive effects
Ketanserin (5HT2A) Mianserin (5HT2C) Ondansetron (5HT3) Cisapride/ metoclopramide (5-HT4) Alprosadil (PGE1) Prostin E2 (PGE2) Prostin F2 (PGF2 salt) Prostin VR (PGE1) Misoprostol (PGE1) - cytoprotective action protect gut lining - decrease acid secretion
- anti-hypertensive -research only - anti-hypertensive - passes BBB - anti-emetic - adjunct to chemo
5-HT antag
- GI stimulant (transit); Metoclopramide (5-HT agonist) gastrointestinal motility Antiemetic (5-HT antagonist) - general vasodilator for SMM - erectile dysfunction - ripen cervix and induce labour - therapeutic abortion - dilation of ductus arteriosus in neonates (heart problems) - protection against NSAID gastric damage/peptic ulcer
PGs
- diarrhoea
Drug Class
Drug Name
MOA
Uses
Side Effects
Miscellaneous info
SAIDs
NSAIDs
Aspirin, indomethacin, ibuprofen
- induce formation of lipocortin decrease phospholipase A - phospholipase A required to make arachidonic acid - arachidonic acid acted on by COX makes PGH2 - reacts with serine on COX inactivates enzyme no PG - indomethacin: reversible non-competitive - ibuprofen: rapid, reversible, competitive
- anti-inflammatory
- withdrawal due to adrenal suppression - chronic use: hypertension, osteoporosis, growth retardation, increase infections - dizziness, tinnitus, headache (toxicity related) - increase in resp - gastric and renal damage, delays labour -decrease GFR
- analgesic - found to have protective action against colon cancer
Leukotrienes? ?
Nitric Oxide
Glyceryl trinitrate, amyl nitrate, sodium nitroprusside, Isosorbide dinitrate, Monnitrate - dont act to increase production of NO, act as if NO would i.e. directly diffusing into SMM to cause relaxation - vasodilator - relax SMM of lungs in resp distress syndrome - hypertrophic pyloric stenosis - impotence headache skin reactions postural hypotension dizziness reflex tachycardia nausea vomiting - cross tolerance between nitrates can occur - CI in hypotension, cardiomyopathy and hypersensitivity to nitrates - interacts with antihypertensives, sildenafil, alcohol, TCAs
Increase NO
NOS inhibitors Castor oil, bisacodyl, senna NO-NSAID Other NO drugs Sildenafil
- competitive inhibitors - prevents conversion of L-Arg NO - increase NOS activity in GIT increase fluid secretion and relaxation - same effect as aspirin but causes release of NO instead - increase mucosal secretion to counter stomach SE - inhibit COX-I and COX-II - potentiation of NO-stim cGMP pathway - inhibit phosphodiesterase relaxation of cavernosal SMM - KATP channel activator - causes vasodilation - D antag acts in chemoreceptor trigger zone - D2 antag - D2 antag
migraine neurodegenerative disorders hypotensive crisis laxative
- pain relief??
Nicorandil
- vasodilator
Central Nervous System
Domperidone Prochlorperazine Anti-emetics Chlropromazine - anti-emetic - anti-emetic - Schizophrenia D antag in mesocortical/limbic sys - Parkinsons D antag in nigrostriatal path - extrapyramidal side effects i.e. loss of fine motor control - doesnt cross BBB hence wont cause Parkinsons like SE
Drug Class
Drug Name
MOA
Uses
Side Effects
Miscellaneous info
Emetics
Ipecachuanha, heavy metal salts Apomorphine Pentelenetetrazol e, Bemegride strychnine
- act as irritants to the stomach to causing vomiting - D2 agonist - acts on chemoreceptor trigger zone
- emesis - emesis
- glycine antag - GABA antag (competitive) - GABA antag (non-competitive - Benzodiazepine antag
Resp stimulants
Bicuculline Picrotoxin Flumazenil
Anti-psychotics
Typical Phenothiazine s and butyronpheno nes (-zines) Chlorpromazine (CPZ) Haloperidol (Promethazine, Prochloroperazin e, thioridazine little antipsychotic action) Clozapine, Risperidone, Olanzapine, Quetiapine Atypical (-pines) Aripiprazole anti-psychotic D2 antag anti-N catalepsy cataplexy (muscle relaxation local anaesthetic decrease aggression/agitation decrease epileptic fits - anti-psychotic - CPZ best binding to H1 and 5-HT2 - anti-emetic H1 antag (Prochloroperazine) - anti-histamine (sedation through H1) (Promethazine) - anti-psychotic - convulsions, drowsiness - extrapyramidal effects i.e. Parkinsons, dyskinesia - weight gain - endocrine problems block DA increases prolactin - anti-M i.e. anti-SLUD - jaundice, clouding of lens - skin rash - increase risk to diabetes from Cloz and Olan but not Risper cells of pancreas blocked decrease insulin - weight gain from Cloz and Olan - headache - agitation - insomnia - takes several weeks to take effect - not very effective - low compliance due to SE - not effective for control of ve symptoms for schizo
Amisulpride
- initiate response from mesocortical D system - increase DA in prefrontal cortex (reverse of typicals) - 5-HT2A antag - 5-HT1A agonist - weak D2 antag - partial agonist: D2, D3 and 5-HT1A - antag: 5-HT2A - D2 stabilise dopaminergic neurotransmission - 5-HT1A effective for ve symptoms - 5-HT2A decrease chance of EPS - D2 and D3 antag limbic system - if antag in striatum SE much worse block neuronal uptake of NA and 5-HT block H1, M, 5-HT, 1/2 1 block decrease feedback increase NA improves mood and decreases aggression decrease 1, 2, 5-HT2 receptors
- no extrapyramidal effects - better for treating ve symptoms - higher affinity for 5-HT2A than D2 - less risk of suicide
- D system stabiliser
- good for ve symptoms
- Insomnia - EPS but much less than typicals - initial: sedation, confusion, motor unco-ordination - chronic: atropinic effects, postural hypotension (thru medullary vasomotor centre), hyperpyrexia, arrhythmia
- no catalepsy, fewer EPS
Anti-depressants
Amitriptyline (AMI), Clomipramine (CMI), Doxepin, Dothiepin - depression - enuresis through M block - sedation/hypnotic - takes a few weeks to notice changes - interacts with sedatives (increase effect of OH), MAOIs and Phenothiazines potentially lethal, Clonidine
Tri-cyclics
Drug Class
SSRI
Drug Name
Fluoxetine, Citalopram, Sertraline,
MOA
- 5-HT brake - 5-HT1A pre +post synaptic on cell bodies; involved in neuronal firing (more important)
Uses
- anti-depressant - Cit., Fluoxetine, Ser. Have active metabolites
Side Effects
- low SE profile due to decrease affinity for D (not anti-psy), M (less atropinic effects), H (decrease
Miscellaneous info
- 2o changes down regulate (reduce receptors) of 5-HT1A on Raphe nucleus increase 5-HT
Paroxetine, Fluvoxamine
- 5-HT1B pre-synaptic nerve terminals; involved in decreasing 5-HT release - acts to increase 5-HT release - meaning non-selective for either isoenzyme - blocks conversion of catecholamines to aldehyde derivatives - since NT breakdown blocked NT spill out of neurone increasing transmission - can displace NA from presynaptic nerves - more A than B in intestine - found predominantly in NA neurones, gut, liver - substrates: tyramine, D, 5-HT, NA - more B than A in brain - found predominantly in 5-HT and H neurones - substrates: tyramine, D, phenyl amines - 2 antag - blocks uptake of NA - 2 antag - 5-HT2/3 antag
- Paro., Fluvox., do not have active metabolites
sedation) and (less drop in BP) - nausea, vomiting, insomnia, sweating, diarrhoea, decrease libido
release - interact with MAOI serotonin syndrome - no potentiation of alcohol effects but still not advised
Non-selective: Iproniazid, Isocarboxazid, Phenelzine, Pragyline, Tranyclopromine MAOI MAO-A selective: Clorgyline, Moclobemide (reversible) MOA-B selective: Selegiline Mianserin
- anti-depressant - jaundice - hypotension reflex bradycardia - CNS stim excitement, agitation, insomnia - nausea - possible hypertensive crisis due to tyramine displacing NA NA leaks out increase BP - need to avoid cheeses
- moclobemide: depression, Parkinsons <ONLY NEED TO KNOW MOCLOBEMIDE FOR EXAM> - anti-depressant
- 2o adaptive changes down regulate 1, 2, 5-HT2 receptors
- anti-depressant
Tetracyclic (Atypical)
Mirtazapine (NA and specific serotonergic NSSA) Venlafaxine (SNRI) Bupropion
- anti-depressant
- block reuptake of 5-HT and NA - weak DA uptake inhibitor - no affinity for M, H1, or - NA and D uptake inhibitor - increases D in reward centres of brain - monoamine uptake inhibitor more action on 5-HT and NA than D
- anti-depressant
- increase appetite and weight gain 5-HT2 block - drowsiness H1 block - CNS excitation - seizures, tremor, mania - fatigue, nausea, dizziness, drowsiness, nervousness, headache, constipation, impotence
- well absorbed - interacts with CNS depressants i.e. alcohol, benzos or MAOIs
- no anti-M, sedation or BP effects - has active metabolite - no interaction with alcohol
Other antidepressants
- only used for nicotine dependence - many interactions with metabolising enzymes
St. Johns Wort
Pain
Naloxone Naltrexone Opioids Buprenorphine, Meptazinol - agonis, antag - opioid antagonist - antag - for reversing opioid OD - alcohol dependence decreases voluntary intake - opioid dependence - relief of moderate/severe pain - used in opioid dependency - nausea - hepatotoxicities - resp depression - hypotension - bradycardia - short half life - CI for opioid analgesics, reduced hepatic function - long half-life - CI for resp compromised, hepatic insufficiency, alcohol and CNS depressants
Drug Class
Opioids
Drug Name
Morphine, Codeine
MOA
- natural opioid agonist ( ) - behavioural: lethargy, drowsiness - analgesic: mimics enkephalins in dorsal horn - nausea and vomiting: acts on chemoreceptor trigger zone
Uses
- mild to moderate pain treatment - cough suppressant - diarrhoea - sedation -
Side Effects
resp depression light headed nausea vomiting sweating
Miscellaneous info
Nalorphine, nalbuphine, butorphanol Pethidine
- miosis: pin-point pupils - thermoregulation: decrease body T - resp system: decrease rate and response to CO2 and H+; bronchoconstriction - CV: postural hypotension - GI: decrease coordination, increase tone, sphincter spasm - bile duct: causes biliary colic - genitor-urinary: increase detrusor and sphincter tone, increase ADH - antag, agonist
sedation -dyspnoea/pulmonary oedema
- constipation - dry mouth - opioid dependence
- agonist
- colic less SMM effects as morphine - for moderate/severe pain - moderate/severe pain greater analgesic potential than morphine - not used for opioid dependence - less abuse potential - moderate/severe pain - adjunct to general anaesthetics
- toxicities causing convulsions and excitement prevent its use for chronic pain treatment - similar profile to other opioid agonists
Hydromorphone
- agonist
Tramadol
- agonist - inhibits NA and 5-HT re-uptake stops SP release - agonist (similar to pethidine)
- nausea, vomiting, dizziness, constipation, asthenia (tingling), fatigue, allergic reactions, headache, sedation
Fentanyl
- shorter onset than morphine - shorter duration than morphine - not as active as morphine - DI for MAOI - shorter half life than morphine - rapid absorption orally - DI for MAOI and CNS depressants - metabolite has greater affinity for receptor than tramadol itself - hypersensitivities - CI for MAOIs and CNS depressants - only for short term analgesic - DI for MAOI and CNS depressants - tumescent: swollen or become swollen - blocks small diameter fibres more readily than large fibres
Local anaesthetics
Local Anaesthetics Esters: Cocaine, Procaine, Benzocaine Amides: Ligno., Dibucaine, Prilocaine etc. Alcohol - blocks Na+ channels from inside nerve(charged form) - enters nerve through Na+ channel or through membrane - used under occlusive dressing - infiltrating tissue hypersensitivity double vision tinnitus light-headedness anxiety, tremor, resp depression arrhythmia, hypotension
Social drugs
Social Drugs - chronic effects: anaemia, increase in GI ulcers - foetal effects: retardation, hyperactivity, decrease in social skills
Drug Class
Drug Name
Nicotine
MOA
- induces CYP1A2 isoenzyme - accumulate in tissues extends half life
Uses
- increase HR, BP and vasoconstriction, increase ADH, increase resp rate - increase alertness, calms ppl in stressful situations - temazepam increase opioid effect - flunitrazepam hypnotic
Side Effects
- cancer, peripheral vascular disease, coronary heart disease, COPD, pregnant women
Miscellaneous info
Benzodiazepin es
Temazepam, flunitrazepam
- facilitates action of opioids
drink spiking Cannabis Ecstasy - acts on CB1 neuronal or CB2 spleen, immune system - increase 5-HT release - increase HR and appetite, decrease BP, muscle strength, body T and intraocular P - boosts self confidence, emotional and sensual effects - causes dementia, mental confusion, ataxia, decrease learning and memory, oedema, hepatotoxicities - increased sweating, blurred vision, ataxia, insomnia, muscle tension - OD: tachycardia, hypertension, hyperthermia, renal failure
- residual effects: flashbacks, anxiety, rage, psychosis
You might also like
- PSY 441 Global Psychology PrePost Test National UniversityDocument7 pagesPSY 441 Global Psychology PrePost Test National UniversityTammy Smith67% (3)
- Pharmacology Main DrugsDocument14 pagesPharmacology Main DrugsSabir KhanNo ratings yet
- Lowenthal - The Crimes of Fascist Occupants and Their Collaborators Against The Jews of Yugoslavia (Balkan Holocaust in WW2) (1957)Document299 pagesLowenthal - The Crimes of Fascist Occupants and Their Collaborators Against The Jews of Yugoslavia (Balkan Holocaust in WW2) (1957)Testerasa TesterNo ratings yet
- FortiAnalyzer 6.0 Study Guide-Online PDFDocument253 pagesFortiAnalyzer 6.0 Study Guide-Online PDFDavid50% (2)
- Emg 2303 NotesDocument65 pagesEmg 2303 NotesAnonymous UnchpksNo ratings yet
- Genitourinary System: Renal FailureDocument6 pagesGenitourinary System: Renal FailureEn ConejosNo ratings yet
- Gyneacology Revision by All TeamDocument14 pagesGyneacology Revision by All TeamSara EhabNo ratings yet
- A Bunch of Pharm ShitDocument2 pagesA Bunch of Pharm ShitkatNo ratings yet
- Tumor Immunology: I. Common Tumor MarkersDocument2 pagesTumor Immunology: I. Common Tumor MarkersDivineGloryMalbuyoNo ratings yet
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Present at 4-12 Months, Development Arrest From Pre-B To BDocument2 pagesPresent at 4-12 Months, Development Arrest From Pre-B To BWaoNo ratings yet
- Differential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersDocument3 pagesDifferential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersNurhayati HasanahNo ratings yet
- Abdo Exam TableDocument2 pagesAbdo Exam Tableapi-195986134No ratings yet
- Antimycobacterial Drugs PDFDocument3 pagesAntimycobacterial Drugs PDFCas BuNo ratings yet
- The Better You Get at Something, The More Enjoyable It Can BecomeDocument6 pagesThe Better You Get at Something, The More Enjoyable It Can BecomeAshNo ratings yet
- Drug CardsDocument3 pagesDrug CardsDave HillNo ratings yet
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocument19 pagesNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- Salmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersDocument8 pagesSalmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersNatalia_WiryantoNo ratings yet
- Bio Chem 1Document5 pagesBio Chem 1Reynaldo RiveraNo ratings yet
- Precipitating Factors:: Myocardial Cell Death (NecrosisDocument2 pagesPrecipitating Factors:: Myocardial Cell Death (NecrosisLean Ashly MacarubboNo ratings yet
- CVR PharmacologyDocument6 pagesCVR PharmacologyRebecca MarshallNo ratings yet
- Handouts Integumentary Sys Sp11 B201Document7 pagesHandouts Integumentary Sys Sp11 B201Kelly TrainorNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- Acid BaseDocument1 pageAcid BasesccctutorNo ratings yet
- Diseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality DiseaseDocument7 pagesDiseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality Diseasenreena aslamNo ratings yet
- Ultimate Pharm GuideDocument41 pagesUltimate Pharm GuideeanguyenNo ratings yet
- MC Tumor MC Ca MC 1° Ca BrainDocument12 pagesMC Tumor MC Ca MC 1° Ca BrainRyan TurnerNo ratings yet
- Dysrhythmias: Cardiac Conduction System Rhythm Strip RecognitionDocument5 pagesDysrhythmias: Cardiac Conduction System Rhythm Strip Recognitiontantalizin marieNo ratings yet
- Common Medications UsedDocument3 pagesCommon Medications UsedRay Michael CasupananNo ratings yet
- Complement SystemDocument4 pagesComplement SystemFait HeeNo ratings yet
- Antibiotics in ActionDocument1 pageAntibiotics in Actionjuan esteban MonroyNo ratings yet
- Kidney NewDocument4 pagesKidney NewParth BhayanaNo ratings yet
- Med CardsDocument4 pagesMed CardsSonia FernandesNo ratings yet
- SketchyPath ChecklistDocument1 pageSketchyPath ChecklistFajar Raza100% (1)
- Low BP - Decreased Cardiac Output - Improved Renal Blood FlowDocument2 pagesLow BP - Decreased Cardiac Output - Improved Renal Blood Flowtantalizin marieNo ratings yet
- Lippincott Illustrated Reviews (PDFDrive) - Pages-396Document1 pageLippincott Illustrated Reviews (PDFDrive) - Pages-396Eman ShalabyNo ratings yet
- Abnormal LFTsDocument2 pagesAbnormal LFTsRenu RosyNo ratings yet
- 1 Ge Stimulations Mast Cell Degeneration Asthma AttackDocument4 pages1 Ge Stimulations Mast Cell Degeneration Asthma Attacknebbie06No ratings yet
- CHEM-Year 2 Chemistry Cheat Sheet For EDEXCELDocument12 pagesCHEM-Year 2 Chemistry Cheat Sheet For EDEXCELraiabhijith586No ratings yet
- Organism Description Drug of ChoiceDocument14 pagesOrganism Description Drug of ChoiceMary YongcoNo ratings yet
- Antifungal Agents: EchinocandinsDocument2 pagesAntifungal Agents: EchinocandinsCourtney TownsendNo ratings yet
- Drugs World: Anti-PsychoticsDocument1 pageDrugs World: Anti-Psychoticsapi-26228251No ratings yet
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- Hi Stop Hath Ology 2Document22 pagesHi Stop Hath Ology 2vivek govardhanamNo ratings yet
- STEP 1 ChecklistDocument11 pagesSTEP 1 ChecklistHasan Khan RoudbaryNo ratings yet
- Anatomy - UPPER LIMB - 3 Muscles, Innervation and Compartments of The Upper Limb PDFDocument20 pagesAnatomy - UPPER LIMB - 3 Muscles, Innervation and Compartments of The Upper Limb PDFDr Ahmed NabilNo ratings yet
- Poliomyelitis Haemophilus Influenzae Type B VariecellaDocument4 pagesPoliomyelitis Haemophilus Influenzae Type B VariecellaJeanna Chong100% (1)
- Neisseria Meningitidis Strep Pneumoniae E. ColiDocument3 pagesNeisseria Meningitidis Strep Pneumoniae E. ColiÐr SalmaNo ratings yet
- Mean Standard Deviation: Antonio Mirano - 2018Document8 pagesMean Standard Deviation: Antonio Mirano - 2018jNo ratings yet
- Ekg Full BibleDocument6 pagesEkg Full BibleTJNo ratings yet
- MnemonicsDocument3 pagesMnemonicsXyzhie McCrudenNo ratings yet
- Concept Map Et Al 11-04-15Document7 pagesConcept Map Et Al 11-04-15api-353656227No ratings yet
- Poison & Antidote Chart IWK Regional Poison Cen PDFDocument1 pagePoison & Antidote Chart IWK Regional Poison Cen PDFdeeptiNo ratings yet
- ECG Demographics Rate: 300/# Large Box in RR IntervalDocument11 pagesECG Demographics Rate: 300/# Large Box in RR IntervalJonathan DavisNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Disorders of The BoneDocument2 pagesDisorders of The BoneRPh Krishna Chandra JagritNo ratings yet
- Electrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionDocument6 pagesElectrolyte Imbalance Cause Signs and Symptoms Intervention ConnectionmkninnyNo ratings yet
- Abg InterpretationDocument1 pageAbg InterpretationPrincess EspadaNo ratings yet
- Zyloprim Drug CardDocument1 pageZyloprim Drug CardSheri490No ratings yet
- Classification of Drugs NewDocument15 pagesClassification of Drugs NewAbdul SamadNo ratings yet
- Children's Respiratory NursingFrom EverandChildren's Respiratory NursingJanice MightenNo ratings yet
- 99 Names of Allah SWT and Mohammed (PBUH)Document11 pages99 Names of Allah SWT and Mohammed (PBUH)api-26870382100% (1)
- Chapter 7 Fiduciary RelationshipDocument18 pagesChapter 7 Fiduciary RelationshipMarianne BautistaNo ratings yet
- Application Activity: Giving BackDocument3 pagesApplication Activity: Giving BackHillary Anne BautistaNo ratings yet
- Description: P Ack AgeDocument3 pagesDescription: P Ack AgeAlexandru CioponeaNo ratings yet
- Registers and StatementsDocument7 pagesRegisters and StatementsspiceshivNo ratings yet
- Assignment 1Document3 pagesAssignment 1Hafez MohammedNo ratings yet
- Jadual Alimah 2021.V3Document6 pagesJadual Alimah 2021.V3maryam cookNo ratings yet
- Microsoft Word - Muffovan-DatasheetEN - 16 - v2Document2 pagesMicrosoft Word - Muffovan-DatasheetEN - 16 - v2Uswatul HasanahNo ratings yet
- Asd Wei Gang Tuo 10 PDFDocument2 pagesAsd Wei Gang Tuo 10 PDFEagle EyeNo ratings yet
- WLC UpgradeDocument13 pagesWLC Upgradeapi-3703368No ratings yet
- Geronimo StiltonDocument2 pagesGeronimo StiltonRajeshNo ratings yet
- PRM AnswerDocument28 pagesPRM AnswerMinh TrangNo ratings yet
- Vocabulary + Grammar Unit 3 Test ADocument3 pagesVocabulary + Grammar Unit 3 Test AJoana FernandesNo ratings yet
- The Crucial Difference Between Creativity and InnovationDocument14 pagesThe Crucial Difference Between Creativity and InnovationTamara KlicekNo ratings yet
- Signed Off Understanding Culture11 q1 m2 Defining Culture and Politics v3 RemovedDocument24 pagesSigned Off Understanding Culture11 q1 m2 Defining Culture and Politics v3 Removedrhaybien vinluanNo ratings yet
- (Lesson2) Cultural, Social, and Political Institutions: Kinship, Marriage, and The HouseholdDocument5 pages(Lesson2) Cultural, Social, and Political Institutions: Kinship, Marriage, and The HouseholdPlat JusticeNo ratings yet
- Concerto in C Minor - Johann Christian Bach - CelloDocument24 pagesConcerto in C Minor - Johann Christian Bach - CellojosianeNo ratings yet
- Step 7 Err Code125936644Document37 pagesStep 7 Err Code125936644mohammadNo ratings yet
- Managerial EconomicsDocument15 pagesManagerial EconomicsAditi WaliaNo ratings yet
- Leadership Styles For 5 StagesDocument18 pagesLeadership Styles For 5 Stagesbimal.greenroadNo ratings yet
- Thou Shall Not StealDocument4 pagesThou Shall Not StealGiselle MarNo ratings yet
- Crowdfunding For Research: A Case Study in Research Management Centre in MalaysiaDocument8 pagesCrowdfunding For Research: A Case Study in Research Management Centre in MalaysiaCk WongNo ratings yet
- The Passion of Jesus Christ: BY Saint Alphonsus de LiguoriDocument67 pagesThe Passion of Jesus Christ: BY Saint Alphonsus de Liguorisatya0988No ratings yet
- Sustainable Project ManagementDocument4 pagesSustainable Project ManagementafirulNo ratings yet
- CFX-Intro 17.0 Lecture07 MovingZonesDocument41 pagesCFX-Intro 17.0 Lecture07 MovingZonesFabiano LebkuchenNo ratings yet
- Chakra Stones Cheat SheetDocument1 pageChakra Stones Cheat SheetamjohnpeterNo ratings yet