Professional Documents
Culture Documents
Volume 22 Issue 1 Editorial 1
Volume 22 Issue 1 Editorial 1
Uploaded by
Renu SrivastavaCopyright:
Available Formats
You might also like
- Current Status Trends and Challenges of CHNDocument41 pagesCurrent Status Trends and Challenges of CHNangayarkanni98% (46)
- Dr. Patrick J. Bryant Pharm.D. FSCIP, Dr. Heather A. Pace Pharm.D. - The Pharmacist's Guide To Evidence-Based Medicine For Clinical Decision Making-ASHP (2008) PDFDocument209 pagesDr. Patrick J. Bryant Pharm.D. FSCIP, Dr. Heather A. Pace Pharm.D. - The Pharmacist's Guide To Evidence-Based Medicine For Clinical Decision Making-ASHP (2008) PDFRaju Niraula100% (1)
- The Doh Nutrition ProgramDocument10 pagesThe Doh Nutrition ProgramDianne Mae100% (1)
- 109-124 Factors Influencing Routine Immunization Uptake Among NursingDocument16 pages109-124 Factors Influencing Routine Immunization Uptake Among Nursingclement johnNo ratings yet
- Vacccine in IndiaDocument9 pagesVacccine in IndiaBijoy AVNo ratings yet
- My ProjectDocument38 pagesMy ProjectfaizamuhammadaligmlNo ratings yet
- Pulse Polio Immunization IndiaDocument31 pagesPulse Polio Immunization IndiaBhumika RathoreNo ratings yet
- Extent of Compliance To Immunization Reasons For Non Continuity and Its Consequences PDFDocument26 pagesExtent of Compliance To Immunization Reasons For Non Continuity and Its Consequences PDFAPRIL LYNNo ratings yet
- Piis0022347613003089 PDFDocument13 pagesPiis0022347613003089 PDFMuhammad ThohirNo ratings yet
- Health&Clinical ManagementDocument125 pagesHealth&Clinical ManagementAnjum100% (1)
- Clinical Epidemiology Assignment Ii: Vaccine Policy of IndiaDocument6 pagesClinical Epidemiology Assignment Ii: Vaccine Policy of IndiaElegant WriangNo ratings yet
- 2019 - JSTMU - Polio EditorialDocument2 pages2019 - JSTMU - Polio EditorialDr. Sajida NaseemNo ratings yet
- Tele-Leprology: A Literature Review of Applications of Telemedicine and Tele-Education To LeprosyDocument12 pagesTele-Leprology: A Literature Review of Applications of Telemedicine and Tele-Education To Leprosyسلوى بوشبيرقةNo ratings yet
- Literature Review On Neonatal DeathDocument6 pagesLiterature Review On Neonatal Deathafdtovmhb100% (1)
- Position Paper On Japanese Encephalitis Vaccines v2Document3 pagesPosition Paper On Japanese Encephalitis Vaccines v22140916No ratings yet
- Health Care Challenges in IndiaDocument8 pagesHealth Care Challenges in IndiaKailash NagarNo ratings yet
- Factors Influencing Utilization of Immunisation Services by Mothers With Children Aged Below 5years at Nyimbwa Health Center Iv in Luweero DistrictDocument2 pagesFactors Influencing Utilization of Immunisation Services by Mothers With Children Aged Below 5years at Nyimbwa Health Center Iv in Luweero DistrictMubiru IbrahimNo ratings yet
- Immunization Coverage of 12 - 23 Months Old Children and Associated Factors in Jigjiga District, Somali National Regional State, EthiopiaDocument9 pagesImmunization Coverage of 12 - 23 Months Old Children and Associated Factors in Jigjiga District, Somali National Regional State, EthiopiaAMANUEL TEREFENo ratings yet
- Age Declaration FormDocument13 pagesAge Declaration FormSrimoy MundNo ratings yet
- The World Health OrganizationDocument4 pagesThe World Health Organizationampal100% (1)
- National Health ProgrammesDocument52 pagesNational Health ProgrammesZaina AkramNo ratings yet
- Immunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument24 pagesImmunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaEugene YeboahNo ratings yet
- Feasibility of Implementation of Simplified ManageDocument20 pagesFeasibility of Implementation of Simplified Manageرجاء خاطرNo ratings yet
- Hes 409, Week 1-3Document9 pagesHes 409, Week 1-3sodiqajayi2018No ratings yet
- Hehe-Ari Na Kay Pat SoweDocument7 pagesHehe-Ari Na Kay Pat SowePtwicia ArgusNo ratings yet
- Identifying The Determinants of Childhood Immunization in The PhilippinesDocument7 pagesIdentifying The Determinants of Childhood Immunization in The PhilippinesCarlo Joseph Intal LlacerNo ratings yet
- IdrvDocument39 pagesIdrvMyk MacalintalNo ratings yet
- Child Survival StrategyDocument78 pagesChild Survival Strategygeag20% (1)
- Acute Respiratory Infection and Pneumonia in IndiaDocument28 pagesAcute Respiratory Infection and Pneumonia in IndiaAnonymous so6ZnlKywNo ratings yet
- Article 1667458231Document9 pagesArticle 1667458231bharathNo ratings yet
- NHP NotesDocument21 pagesNHP Noteskedararadhya2k20No ratings yet
- Deraco, AS Family Health Care ResearchDocument2 pagesDeraco, AS Family Health Care ResearchAdrea DeracoNo ratings yet
- CONTEM - W - Group 4 (SDG 3)Document10 pagesCONTEM - W - Group 4 (SDG 3)Pompeyo Barroga Jr.No ratings yet
- Crack Ias PDFDocument136 pagesCrack Ias PDFShreshth MudgilNo ratings yet
- DtifoDocument11 pagesDtifoDwi atikaNo ratings yet
- Health System Quality and COVID-19 Vaccination. A Cross-Sectional Analysis in 14 CountriesDocument10 pagesHealth System Quality and COVID-19 Vaccination. A Cross-Sectional Analysis in 14 Countriesluis sanchezNo ratings yet
- Department of Health - Expanded Program On Immunization - 2012-05-16Document7 pagesDepartment of Health - Expanded Program On Immunization - 2012-05-16MasterclassNo ratings yet
- Jurnal 4Document8 pagesJurnal 4eka darmayanti putri siregarNo ratings yet
- The Problem: (Insert Citation)Document52 pagesThe Problem: (Insert Citation)Trisha100% (1)
- Research Proposal EdittedDocument47 pagesResearch Proposal EdittedSkyNo ratings yet
- Research Paper 2Document4 pagesResearch Paper 2jumiche0123No ratings yet
- Global Health Challenges 2.editedDocument12 pagesGlobal Health Challenges 2.editedfraz afzalNo ratings yet
- 7 - Health Seeking Behaviour and Perception of Quality of CareDocument6 pages7 - Health Seeking Behaviour and Perception of Quality of CareSunday AyamolowoNo ratings yet
- Respiratory in PakDocument10 pagesRespiratory in PakEman ShNo ratings yet
- Vaccinations For Pregnant Women: Clinical Expert SeriesDocument16 pagesVaccinations For Pregnant Women: Clinical Expert SeriesIzzatul YazidahNo ratings yet
- Expanded Program On ImmunizationDocument6 pagesExpanded Program On ImmunizationAiza Oronce100% (1)
- Influenza Remains A Critical Disease: Name: Tia Nur Istianah NIM/Class: 1001050152/DDocument13 pagesInfluenza Remains A Critical Disease: Name: Tia Nur Istianah NIM/Class: 1001050152/DTia Nur IstianahNo ratings yet
- Discontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisDocument20 pagesDiscontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisMamanya Fadhil HaniNo ratings yet
- Factors Influencing Utilization of Prevention of Mother To Child Transmission (PMTCT) Services Among Pregnant Women Attending Ante-Natal ClinicDocument6 pagesFactors Influencing Utilization of Prevention of Mother To Child Transmission (PMTCT) Services Among Pregnant Women Attending Ante-Natal ClinicIPROJECCT100% (1)
- Level of Awareness of Childbearing Mothers On Immunization of Children 0-5 Years in Maiha Local Government Area, Adamawa State NigeriaDocument8 pagesLevel of Awareness of Childbearing Mothers On Immunization of Children 0-5 Years in Maiha Local Government Area, Adamawa State NigeriaIJMSRTNo ratings yet
- An Investigation Into Factors Hindering Effective Uptake of Vaccine Among Children Who Are Below Five (5) in Akinyele Local Government Area Ibadan Oyo State, NigeriaDocument14 pagesAn Investigation Into Factors Hindering Effective Uptake of Vaccine Among Children Who Are Below Five (5) in Akinyele Local Government Area Ibadan Oyo State, NigeriaCentral Asian StudiesNo ratings yet
- Hadiya Azhar - 23110125 - Policy BriefDocument7 pagesHadiya Azhar - 23110125 - Policy BriefHadiya AzharNo ratings yet
- Stability and Ocular In-Vivo Pharmacodynamic Study of Ion Activated Brimonidine Tartarate Insitu GelDocument10 pagesStability and Ocular In-Vivo Pharmacodynamic Study of Ion Activated Brimonidine Tartarate Insitu GeliajpsNo ratings yet
- Journal of Vaccination For ChildrenDocument26 pagesJournal of Vaccination For ChildrenNurul SyafiqahNo ratings yet
- 2150 With Cover Page v2Document12 pages2150 With Cover Page v2RodsNo ratings yet
- Why Vaccines Matter Understanding The Broader Health Economic and Child Development Benefits of Routine VaccinationDocument6 pagesWhy Vaccines Matter Understanding The Broader Health Economic and Child Development Benefits of Routine VaccinationadeolamiraclealaoNo ratings yet
- Paper 1Document25 pagesPaper 1DrAqeel AshrafNo ratings yet
- NCD Assingment EditedDocument23 pagesNCD Assingment EditedAbass DavidNo ratings yet
- Pulse Polio ProgramDocument3 pagesPulse Polio ProgramRandeep KaurNo ratings yet
- Pneu Case Based Assignment PT 1 and 2Document4 pagesPneu Case Based Assignment PT 1 and 2api-659065431No ratings yet
- Episcleritis and Scleritis: BackgroundDocument7 pagesEpiscleritis and Scleritis: BackgroundElrach CorpNo ratings yet
- Treatment and Prevention. Springer-Verlag Berlin Heidelberg: Sehat: Anatomi Dan Fisiologi. Yogyakarta: UGMDocument2 pagesTreatment and Prevention. Springer-Verlag Berlin Heidelberg: Sehat: Anatomi Dan Fisiologi. Yogyakarta: UGMJontor KotlNo ratings yet
- Guía de Neuroimagen en Primer EpisodioDocument24 pagesGuía de Neuroimagen en Primer EpisodiokarlunchoNo ratings yet
- Manasika Roga ChikitsaDocument4 pagesManasika Roga ChikitsaReshma rajNo ratings yet
- Anticancer Drugs PDFDocument28 pagesAnticancer Drugs PDFHamza Mylo Senni100% (3)
- Case Report ASDDocument34 pagesCase Report ASDIrwansyah Ghenjy0% (1)
- Implants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitDocument5 pagesImplants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitNIMMY ANTONo ratings yet
- Classification of Chronic HepatitisDocument4 pagesClassification of Chronic HepatitisVardan KocharNo ratings yet
- Range of Motion PresentationDocument27 pagesRange of Motion Presentationsathish100% (1)
- Nursing InformaticsDocument2 pagesNursing Informaticsapi-469041523No ratings yet
- Impaired Tissue Integrity - Nursing Diagnosis & Care Plan PDFDocument15 pagesImpaired Tissue Integrity - Nursing Diagnosis & Care Plan PDFManar AbdallahNo ratings yet
- NCP For Impaired Physical MobilityDocument2 pagesNCP For Impaired Physical MobilityPrincess Averin Navarro50% (2)
- Cs 19 SolvedDocument4 pagesCs 19 SolvedgogoNo ratings yet
- Hemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?Document4 pagesHemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?asclepiuspdfsNo ratings yet
- Clothes Drag Technique: University of Baguio School of Criminal Justice and Public Safety Gen. Luna Road, Baguio CityDocument4 pagesClothes Drag Technique: University of Baguio School of Criminal Justice and Public Safety Gen. Luna Road, Baguio CityMarieRoseGuzmanSubdiNo ratings yet
- Endocrine System: Capillary Glucose MonitoringDocument34 pagesEndocrine System: Capillary Glucose Monitoringjoel david knda mj100% (1)
- Test Your Knowledge About Covid-19Document15 pagesTest Your Knowledge About Covid-19Ranz PanganibanNo ratings yet
- Cardio: Prometric Exam 5/4/2015 Internal MedicineDocument14 pagesCardio: Prometric Exam 5/4/2015 Internal MedicineWalid SakrNo ratings yet
- Induction of LabourDocument45 pagesInduction of LabourVidya RamanathanNo ratings yet
- AbstractBookAbstracts501 1000Document155 pagesAbstractBookAbstracts501 1000Jose Oscar TarazonaNo ratings yet
- Takaful Health2Document34 pagesTakaful Health2yusofprubsnNo ratings yet
- Bawaseer (Hemorrhoids)Document22 pagesBawaseer (Hemorrhoids)drmshiffaNo ratings yet
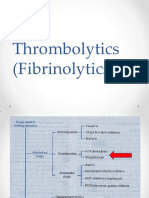
- Thrombolytics (Fibrinolytics)Document14 pagesThrombolytics (Fibrinolytics)J lodhiNo ratings yet
- NPF Focus1Document12 pagesNPF Focus1ramuNo ratings yet
- A Case Study On Abruptio PlacentaeDocument22 pagesA Case Study On Abruptio Placentaeporskol2No ratings yet
- Dr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiDocument35 pagesDr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiNailahRahmahNo ratings yet
- Febrile Neutropenia Topic DiscussionDocument42 pagesFebrile Neutropenia Topic Discussionapi-647904873No ratings yet
- Orthopedic MCQ (Group 5)Document4 pagesOrthopedic MCQ (Group 5)Law YouNo ratings yet
Volume 22 Issue 1 Editorial 1
Volume 22 Issue 1 Editorial 1
Uploaded by
Renu SrivastavaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Volume 22 Issue 1 Editorial 1
Volume 22 Issue 1 Editorial 1
Uploaded by
Renu SrivastavaCopyright:
Available Formats
4
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 22 , NO. 1, 2009
12 Howe SJ, Mansour MR, Schwarzwaelder K, Bartholomae C, Hubank M, Kempski H, et al. Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J Clin Invest 2008;118:31439. 13 Bushman FD. Retroviral integration and human gene therapy. J Clin Invest 2007;117:20836. 14 Aiuti A, Cattaneo F, Galimberti S, Benninghoff U, Cassani B, Callegaro L, et al. Gene therapy for immunodeficiency due to adenosine deaminase deficiency. N Engl J Med 2009;360:44758. 15 Kohn DB, Candotti F. Gene therapy fulfilling its promise. N Engl J Med 2009;360:51821. 16 Aiuti A, Cassani B, Andolfi G, Mirolo M, Biasco L, Recchia A, et al. Multilineage hematopoietic reconstitution without clonal selection in ADASCID patients treated with stem cell gene therapy. J Clin Invest 2007;117: 223340. 17 Felice B, Cattoglio C, Cittaro D, Testa A, Miccio A, Ferrari G, et al. Transcription factor binding sites are genetic determinants of retroviral integration in the human genome. PLoS ONE 2009;4:e4571. doi:10.1371/ journal.pone.0004571. Available at www.plosone.org 18 Raper SE, Chirmule N, Lee FS, Wivel NA, Bagg A, Gao GP, et al. Fatal systemic inflammatory response syndrome in a ornithine transcarbamylase deficient patient following adenoviral gene transfer. Mol Genet Metab 2003;80: 14858. 19 Evans CH, Ghivizzani AC, Robbins PD. Arthritis gene therapys first death. Arthritis Res Ther 2008;10:110 (doi:10.1186/ar2411). Available at http://arthritis-research.com/content/10/3/110 20 Cavazzana-Calvo M, Fischer A. Gene therapy for severe combined immunodeficiency: Are we there yet? J Clin Invest 2007;117:145665. 21 Peng Z. Current status of gendicine in China: Recombinant human Ad-p53 agent for treatment of cancers. Hum Gene Ther 2005;16:101627. 22 Guo G, Xin H. Chinese gene therapy: Splicing out the West? Science 2006;314:12325. 23 Guinn BA, Mulherkar R. International progress in cancer gene therapy. Cancer Gene Ther 2008;15:76575. 24 Chen L, Woo SLC. Complete and persistent phenotypic correction of phenylketonuria in mice by site-specific genome integration of murine phenylalanine hydroxylase cDNA. Proc Natl Acad Sci USA 2005;102:155816.
S. S. AGARWAL
Formerly Department of Genetics Sanjay Gandhi Post Graduate Institute of Medical Sciences Lucknow Uttar Pradesh agarwal_ss2000@yahoo.com
Lessons from the Challenges of Polio Eradication in India
In 1988, India resolved to eliminate the transmission of wild polioviruses (WPVs) by the year 2000, but failed; in 2002, the target was revised to 2005.1 However, the endemic transmission of WPV types 1 and 3 continues even in 2009.2 Indias problems on the polio eradication front are symptomatic of the defects in her health system.3 The only other countries with uninterrupted endemic transmission of WPVs are Pakistan, Afghanistan and Nigeria, all with weak health systems. Readers may recall the debate on the proposed health system reforms between two rival political party candidates in the recent election for President of the USA. In India, the political party that wins a majority forms the government, which implements the partys policy on health system. I am unaware whether any political party addresses issues related to the maladies (and the possible remedies) of our health system. So, there is no reform to implement though, in my opinion, reform is urgently required in the health sector. The inordinate delay in polio eradication suggests systemic deficiencies in our health infrastructure, especially regarding the organization of the health system and the sharing of responsibilities between the Centre and the states.3
The health system in the context of polio eradication
Indias health system should consist of two arms: medical carefocusing on individuals, particularly after they fall ill, for restoration to health; and public healthfocusing on the community and the environment for breaking the chains of transmission of infections to control endemic diseases and outbreaks. Medical care for rural communities is predominantly in the public sector but remains minimalist in spite
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 22, NO. 1, 2009
of the National Rural Health Mission. While medical care deficiencies in the public sector in urban communities have to a certain extent been mitigated by the private sector, both sectors are guilty of not ensuring quality and equity.4 Polio eradication is a global public health programme; Indias responsibility is polio elimination within the country. However, there is no Department of Public Health either at the Centre or in the states (with the exception of Tamil Nadu). Thus, many essential functions of public health in India are unmet. Instead of establishing public health infrastructure with a broad agenda of controlling all infectious diseases, we have special vehicles for targeted vertical control of tuberculosis, malaria, leprosy, AIDS, kala azar and lymphatic filariasis (under the Department of Health Services) and of childhood cluster of 6 diseases (Universal Immunization Programme [UIP] under the Department of Family Welfare).1 Indias official representative at the 1988 World Health Assembly committed to the elimination of WPVs by 2000 and we expected that UIP would achieve it on time.5 In 1995, when it became clear that this was unlikely to happen, the WHO stepped in and created a new special vehicle called the National Polio Surveillance Project (NPSP) and polio was placed under epidemiological monitoring through detection and virological investigation of all cases of acute flaccid paralysis.2 No other childhood disease targeted for control under UIP is being epidemiologically monitored.6 In 1978, India set out to reach 85% vaccination coverage of infants, but has reached <50% in 30 years.7 Inter-state disparities are unacceptably widesome with >95% but others with <30% coverage with 3 doses of DPT (diphtheriapertussistetanus) vaccine and trivalent OPV (tOPV) during infancy. The vaccination coverage in Uttar Pradesh and Bihar is among the lowest, contributing to barriers in interrupting the transmission of WPVs.3,7 During the 1970s and 1980s, studies had shown that tOPV had low vaccine efficacy (VE) in India and incomplete safety globally.8,9 On the other hand, inactivated poliovirus vaccine (IPV) had a superior VE in India and complete safety globally.9,10 However, on account of a health system flaw, a restrictive policy of the exclusive use of tOPV was continued and the government declined to license IPV.3 This official stand was mistaken by some global public health agencies to mean that Indian studies on VE of tOPV were not credible. Thus, a cycle was created in which the WHO and the government reinforced each others flawed policy of exclusive use of tOPV. Escape from this cycle was not easy then and it is not easy even today. The lesson to be learned here is that health-related policies should be supported by evidence, for which technical leadership should be strengthened at the Central and state levels. When in-country studies showed anomalous results, the government should have verified the results by independent investigation, for which a functional public health department with laboratory support was necessary, but not available. The Indian Council of Medical Research did undertake such an investigation and confirmed the low VE, but that was also ignored.11 In the absence of case-based disease surveillance, which is an integral function of a public health department, vaccine-failure polio was missed for decades.3,8,10,11 This shortcoming was recognized by the NPSP only after attempts at elimination of WPVs failed beyond 2004. In 2005, the NPSP conducted independent verification of VE using field epidemiology, for the first time, and re-discovered that 3 doses of tOPV provided protection to no more than 30% of children against WPV types 1 and 3.12 In 1982, WHO had warned all countries using OPV to keep vaccine-associated paralytic polio (VAPP) under surveillance.9 In the absence of disease surveillance and laboratory support services, this WHO recommendation could not be complied with. In summary, the major factor that led to Indias failure with polio elimination is the lack of an overarching Department of Public Health and the lack of technical leadership at the highest levels of policy-making. As in the case of similar departments in other fields, the Department of Public Health must also be headed by a technically qualified professional.
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 22 , NO. 1, 2009
In 1999, India took a leading role in a conference on Public health in South East Asia in the Twenty-first century convened in Calcutta (now Kolkata).13 The outcome was embodied in the Calcutta Declaration in which the importance of public health as a discipline and as a framework for employing public health-trained personnel with a clear career track (in other words a public health department, as in Tamil Nadu) was highlighted.13 This recommendation needs to be acted upon.
The current situation of polio
Though by definition, India is still endemic for WPV, the burden of disease has been drastically curtailed by a long, arduous and expensive intervention meant for total elimination. In the 1980s, the mean daily number of cases of polio was 5001000.8 In 2006, 2007 and 2008 the mean number was 1.9, 2.4 and 1.5, respectively.2 The drastic reduction was both numerical and geographical. During the past 5 years, WPVs have continued to circulate only in Uttar Pradesh and Bihar,2 but, a chain is as strong only as its weakest link. These 2 states together have a population of about 250 million (2001 Census), i.e. over 20% of the national total. Moreover, in recent years WPV types 1 or 3 from Uttar Pradesh and Bihar have spread to nearby areas (e.g. Delhi and Haryana) and faraway states (e.g. Orissa and Maharashtra) and neighbouring countries (e.g. Nepal and Bangladesh) and faraway countries (e.g. Lebanon and Angola).14 It is imperative that Uttar Pradesh and Bihar succeed soon so that India achieves success, without which global eradication of polio will remain unrealized. In 2006, there was an outbreak of WPV type 1, predominantly in Uttar Pradesh.2 An outbreak of WPV type 3 began in 2007 and continued into 2008, predominantly in Bihar.2 In response, unprecedented vaccine pressure is being applied. Presently, following the outbreaks when transmission efficiency and burden of WPVs are low, there is an opportunity for interrupting WPV types 1 and 3 in 200910, which should not be missed. Of the three serotypes of WPVs, type 2 was eliminated from India in 1999, providing proof that the type 2 component in tOPV performed more efficiently than the types 1 or 3 components. The wide differential in type-specific VE of tOPV were recognized and confirmed by several studies in India.8,10,11 VE against type 2 is the highest and against 1 the lowest.8,10,11 The interruption of type 2 WPV showed that adequate coverage of vaccination had been reached through multiple annual tOPV campaigns, but VE was inadequate against WPV types 1 and 3. It took 6 more years for this interpretation to be accepted, highlighting the gaps in epidemiology; since 2005, monovalent OPV types 1 and 3 (mOPV-1, mOPV-3) are being used since they have significantly higher type-specific efficacy.12 Taking a cue from the interruption of type 2, the current tactic is to focus on eliminating type 1 and, after ensuring success, to aim for eliminating type 3.2 As the issue of incomplete safety of OPV became global news, the government allowed the entry of IPV in India and licensed it in May 2006, but without evolving a policy on its use. The government and NPSP are in the process of developing an evidence-based policy on its use to complete and conclude polio elimination, re-defined as zero incidence of poliovirus infection (i.e. not only wild but also vaccine-derived).3
Possible solutions: The way forward
We can either somehow achieve polio eradication and leave the system as it is; or introduce systemic changes while eradicating polio. The former option may seem expedient, but the latter is in our long term interest. A third option is to accept the current status of polio as control and to discontinue the intensified efforts to interrupt WPV transmission, as has been proposed in a paper in this issue of the Journal.15 The authors advocate conservation of resources and suggest that those resources should be put to better useto improve the delivery of healthcare in the public sector.15 They point out that the polio elimination programme has been exorbitantly expensive.15 When one wages war (on polio) but disallows the use of the more powerful weapon (i.e. IPV) in favour of the
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 22, NO. 1, 2009
less efficient (OPV), consequent delays and cost-escalations will invariably follow. For controlling polio at the present level, resources will need to be provided perpetually, i.e. resources will not be conserved. Thus, the better option is to complete the operation, eliminate WPVs and thereafter eliminate vaccine polioviruses. This sequence will necessarily be expensive as the elimination of vaccine viruses will require the inclusion of IPV in the UIP.3 Had IPV been introduced earlier the comparative merits of both vaccines could have been evaluated. Thus, much time and money would have been saved for the elimination of WPVs. As OPV could have been withdrawn earlier, continued seeding of the community with vaccine viruses could have been stopped in time.3 In my opinion, the best way forward for us is to complete the task of polio elimination and also take early steps to reform our health system. Indias health system must be redesigned to be comprehensive, professional, efficient, responsive to peoples needs and oriented to quality and equity. The first step should be to establish a National Commission on Health Systems to assess the lessons learnt from Indias problems with elimination of polio and to apply remedies holistically. Appropriate tools of public health must be applied to control the many neglected infectious diseases including cholera, enteric fevers, shigellosis, leptospirosis, rabies and scrub typhus. India needs to graduate and acquire the skills of modern public health to address the new epidemics of diabetes, hypertension, cardiovascular and neurovascular diseases and obesity. The current spending on health, 0.91% of GDP, is woefully inadequate for a self-declared welfare state. India must drastically increase the budget also for appropriate healthcare with equity and quality. The Central and state governments should establish Departments of Public Health, with avenues for training in epidemiology and public health and career tracks for trained officers. Without Departments of Public Health increased fund allocations are unlikely to be absorbed or utilized or to succeed in disease control and health promotion.
Conclusion
As the prevalence of WPVs decline vaccine viruses show the tendency to fill the niche by evolving into circulating vaccine-derived polioviruses that are wild-like.3 Thus, true polio eradication requires the elimination of both WPVs as well as vaccine viruses.3 Therefore, IPV will have to be introduced for the safe withdrawal of OPV, at the earliest opportunity in the future. The original argument that elimination of WPV using the cheaper vaccine (OPV) would be more economical than by using the more expensive IPV was faulty; but as now as it was then, the question was not primarily one of economics but of science guiding policy. Way back in 1981 it was suggested that IPV would be the vaccine of the future and the use of OPV should be considered only as an interim measure.16 REFERENCES
1 Available at http://www.mohfw.nic.in/ (accessed on 6 April 2009). 2 National Polio Surveillance Project. AFP and polio data. Available at http://www.npspindia.org/bulletin.pdf (accessed on 6 April 2009). 3 Polio Eradication Committee, Indian Academy of Pediatrics. Universal Immunization Programme and polio eradication in India. Indian Pediatr 2008;45:80713. 4 Voluntary Health Association of India. Health services in rural and urban areas. Chapter 8. In: Mukhopadhyay A (ed). Report of the Independent Commission on Health in India. New Delhi:Voluntary Health Association of India; 1997:7595. 5 World Health Assembly. Global eradication of poliomyelitis by the year 2000. (Resolution WHA 41.28). World Health Organization, Geneva. 1988 6 John TJ. Resurgence of diphtheria in India in the 21st century. Indian J Med Res 2008;128:66970. 7 National Family Health Survey, India. NFHS-3 Fact sheets. Available at http://www.nfhsindia.org (accessed on 6 April 2009). 8 John TJ. Poliomyelitis in India. Prospects and problems of control. Rev Infect Dis 1984;6 (Suppl 2):S438S441. 9 World Health Organization Consultative Group. The relation between acute persisting spinal paralysis and poliomyelitis vaccine. Results of a ten-year enquiry. Bull World Health Organ 1982;60:23142. 10 John TJ. Immunization against polioviruses in developing countries. Rev Med Virol 1993;3:14960. 11 Pangi NS, Master JM, Dave KH. Efficacy of oral polio vaccine in infancy. Indian Pediatr 1977;14:5238. 12 Grassly NC, Fraser C, Wenger J, Deshpande JM, Sutter RW, Heymann DL, et al. New strategies for the elimination of polio from India. Science 2006;314:11503. 13 Anonymous. Calcutta declaration on public health. J Health Popul Dev Countries 2000;3:5. 14 Anonymous. Progress towards interrupting wild poliovirus transmission, January 2006May 2007. Wkly Epidemiol Rec 2007;82:24551.
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 22 , NO. 1, 2009
15 Yadav K, Rai SK, Vidushi A, Pandav CS. Intensified pulse polio immunization: Time spent and cost incurred at a primary healthcare centre. Natl Med J India 2009;22:1317. 16 John TJ. Towards a national policy on poliomyelitis. Indian Pediatr 1981;18:5036.
T. JACOB JOHN
439 Civil Supplies Godown Lane Kamalakshipuram Vellore Tamil Nadu tjacobjohn@yahoo.co.in
The National Medical Journal of India is indexed in Current Contents: Clinical Medicine and Science Citation Index. Editor
You might also like
- Current Status Trends and Challenges of CHNDocument41 pagesCurrent Status Trends and Challenges of CHNangayarkanni98% (46)
- Dr. Patrick J. Bryant Pharm.D. FSCIP, Dr. Heather A. Pace Pharm.D. - The Pharmacist's Guide To Evidence-Based Medicine For Clinical Decision Making-ASHP (2008) PDFDocument209 pagesDr. Patrick J. Bryant Pharm.D. FSCIP, Dr. Heather A. Pace Pharm.D. - The Pharmacist's Guide To Evidence-Based Medicine For Clinical Decision Making-ASHP (2008) PDFRaju Niraula100% (1)
- The Doh Nutrition ProgramDocument10 pagesThe Doh Nutrition ProgramDianne Mae100% (1)
- 109-124 Factors Influencing Routine Immunization Uptake Among NursingDocument16 pages109-124 Factors Influencing Routine Immunization Uptake Among Nursingclement johnNo ratings yet
- Vacccine in IndiaDocument9 pagesVacccine in IndiaBijoy AVNo ratings yet
- My ProjectDocument38 pagesMy ProjectfaizamuhammadaligmlNo ratings yet
- Pulse Polio Immunization IndiaDocument31 pagesPulse Polio Immunization IndiaBhumika RathoreNo ratings yet
- Extent of Compliance To Immunization Reasons For Non Continuity and Its Consequences PDFDocument26 pagesExtent of Compliance To Immunization Reasons For Non Continuity and Its Consequences PDFAPRIL LYNNo ratings yet
- Piis0022347613003089 PDFDocument13 pagesPiis0022347613003089 PDFMuhammad ThohirNo ratings yet
- Health&Clinical ManagementDocument125 pagesHealth&Clinical ManagementAnjum100% (1)
- Clinical Epidemiology Assignment Ii: Vaccine Policy of IndiaDocument6 pagesClinical Epidemiology Assignment Ii: Vaccine Policy of IndiaElegant WriangNo ratings yet
- 2019 - JSTMU - Polio EditorialDocument2 pages2019 - JSTMU - Polio EditorialDr. Sajida NaseemNo ratings yet
- Tele-Leprology: A Literature Review of Applications of Telemedicine and Tele-Education To LeprosyDocument12 pagesTele-Leprology: A Literature Review of Applications of Telemedicine and Tele-Education To Leprosyسلوى بوشبيرقةNo ratings yet
- Literature Review On Neonatal DeathDocument6 pagesLiterature Review On Neonatal Deathafdtovmhb100% (1)
- Position Paper On Japanese Encephalitis Vaccines v2Document3 pagesPosition Paper On Japanese Encephalitis Vaccines v22140916No ratings yet
- Health Care Challenges in IndiaDocument8 pagesHealth Care Challenges in IndiaKailash NagarNo ratings yet
- Factors Influencing Utilization of Immunisation Services by Mothers With Children Aged Below 5years at Nyimbwa Health Center Iv in Luweero DistrictDocument2 pagesFactors Influencing Utilization of Immunisation Services by Mothers With Children Aged Below 5years at Nyimbwa Health Center Iv in Luweero DistrictMubiru IbrahimNo ratings yet
- Immunization Coverage of 12 - 23 Months Old Children and Associated Factors in Jigjiga District, Somali National Regional State, EthiopiaDocument9 pagesImmunization Coverage of 12 - 23 Months Old Children and Associated Factors in Jigjiga District, Somali National Regional State, EthiopiaAMANUEL TEREFENo ratings yet
- Age Declaration FormDocument13 pagesAge Declaration FormSrimoy MundNo ratings yet
- The World Health OrganizationDocument4 pagesThe World Health Organizationampal100% (1)
- National Health ProgrammesDocument52 pagesNational Health ProgrammesZaina AkramNo ratings yet
- Immunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument24 pagesImmunization Programs For Infants, Children, Adolescents, and Adults: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaEugene YeboahNo ratings yet
- Feasibility of Implementation of Simplified ManageDocument20 pagesFeasibility of Implementation of Simplified Manageرجاء خاطرNo ratings yet
- Hes 409, Week 1-3Document9 pagesHes 409, Week 1-3sodiqajayi2018No ratings yet
- Hehe-Ari Na Kay Pat SoweDocument7 pagesHehe-Ari Na Kay Pat SowePtwicia ArgusNo ratings yet
- Identifying The Determinants of Childhood Immunization in The PhilippinesDocument7 pagesIdentifying The Determinants of Childhood Immunization in The PhilippinesCarlo Joseph Intal LlacerNo ratings yet
- IdrvDocument39 pagesIdrvMyk MacalintalNo ratings yet
- Child Survival StrategyDocument78 pagesChild Survival Strategygeag20% (1)
- Acute Respiratory Infection and Pneumonia in IndiaDocument28 pagesAcute Respiratory Infection and Pneumonia in IndiaAnonymous so6ZnlKywNo ratings yet
- Article 1667458231Document9 pagesArticle 1667458231bharathNo ratings yet
- NHP NotesDocument21 pagesNHP Noteskedararadhya2k20No ratings yet
- Deraco, AS Family Health Care ResearchDocument2 pagesDeraco, AS Family Health Care ResearchAdrea DeracoNo ratings yet
- CONTEM - W - Group 4 (SDG 3)Document10 pagesCONTEM - W - Group 4 (SDG 3)Pompeyo Barroga Jr.No ratings yet
- Crack Ias PDFDocument136 pagesCrack Ias PDFShreshth MudgilNo ratings yet
- DtifoDocument11 pagesDtifoDwi atikaNo ratings yet
- Health System Quality and COVID-19 Vaccination. A Cross-Sectional Analysis in 14 CountriesDocument10 pagesHealth System Quality and COVID-19 Vaccination. A Cross-Sectional Analysis in 14 Countriesluis sanchezNo ratings yet
- Department of Health - Expanded Program On Immunization - 2012-05-16Document7 pagesDepartment of Health - Expanded Program On Immunization - 2012-05-16MasterclassNo ratings yet
- Jurnal 4Document8 pagesJurnal 4eka darmayanti putri siregarNo ratings yet
- The Problem: (Insert Citation)Document52 pagesThe Problem: (Insert Citation)Trisha100% (1)
- Research Proposal EdittedDocument47 pagesResearch Proposal EdittedSkyNo ratings yet
- Research Paper 2Document4 pagesResearch Paper 2jumiche0123No ratings yet
- Global Health Challenges 2.editedDocument12 pagesGlobal Health Challenges 2.editedfraz afzalNo ratings yet
- 7 - Health Seeking Behaviour and Perception of Quality of CareDocument6 pages7 - Health Seeking Behaviour and Perception of Quality of CareSunday AyamolowoNo ratings yet
- Respiratory in PakDocument10 pagesRespiratory in PakEman ShNo ratings yet
- Vaccinations For Pregnant Women: Clinical Expert SeriesDocument16 pagesVaccinations For Pregnant Women: Clinical Expert SeriesIzzatul YazidahNo ratings yet
- Expanded Program On ImmunizationDocument6 pagesExpanded Program On ImmunizationAiza Oronce100% (1)
- Influenza Remains A Critical Disease: Name: Tia Nur Istianah NIM/Class: 1001050152/DDocument13 pagesInfluenza Remains A Critical Disease: Name: Tia Nur Istianah NIM/Class: 1001050152/DTia Nur IstianahNo ratings yet
- Discontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisDocument20 pagesDiscontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisMamanya Fadhil HaniNo ratings yet
- Factors Influencing Utilization of Prevention of Mother To Child Transmission (PMTCT) Services Among Pregnant Women Attending Ante-Natal ClinicDocument6 pagesFactors Influencing Utilization of Prevention of Mother To Child Transmission (PMTCT) Services Among Pregnant Women Attending Ante-Natal ClinicIPROJECCT100% (1)
- Level of Awareness of Childbearing Mothers On Immunization of Children 0-5 Years in Maiha Local Government Area, Adamawa State NigeriaDocument8 pagesLevel of Awareness of Childbearing Mothers On Immunization of Children 0-5 Years in Maiha Local Government Area, Adamawa State NigeriaIJMSRTNo ratings yet
- An Investigation Into Factors Hindering Effective Uptake of Vaccine Among Children Who Are Below Five (5) in Akinyele Local Government Area Ibadan Oyo State, NigeriaDocument14 pagesAn Investigation Into Factors Hindering Effective Uptake of Vaccine Among Children Who Are Below Five (5) in Akinyele Local Government Area Ibadan Oyo State, NigeriaCentral Asian StudiesNo ratings yet
- Hadiya Azhar - 23110125 - Policy BriefDocument7 pagesHadiya Azhar - 23110125 - Policy BriefHadiya AzharNo ratings yet
- Stability and Ocular In-Vivo Pharmacodynamic Study of Ion Activated Brimonidine Tartarate Insitu GelDocument10 pagesStability and Ocular In-Vivo Pharmacodynamic Study of Ion Activated Brimonidine Tartarate Insitu GeliajpsNo ratings yet
- Journal of Vaccination For ChildrenDocument26 pagesJournal of Vaccination For ChildrenNurul SyafiqahNo ratings yet
- 2150 With Cover Page v2Document12 pages2150 With Cover Page v2RodsNo ratings yet
- Why Vaccines Matter Understanding The Broader Health Economic and Child Development Benefits of Routine VaccinationDocument6 pagesWhy Vaccines Matter Understanding The Broader Health Economic and Child Development Benefits of Routine VaccinationadeolamiraclealaoNo ratings yet
- Paper 1Document25 pagesPaper 1DrAqeel AshrafNo ratings yet
- NCD Assingment EditedDocument23 pagesNCD Assingment EditedAbass DavidNo ratings yet
- Pulse Polio ProgramDocument3 pagesPulse Polio ProgramRandeep KaurNo ratings yet
- Pneu Case Based Assignment PT 1 and 2Document4 pagesPneu Case Based Assignment PT 1 and 2api-659065431No ratings yet
- Episcleritis and Scleritis: BackgroundDocument7 pagesEpiscleritis and Scleritis: BackgroundElrach CorpNo ratings yet
- Treatment and Prevention. Springer-Verlag Berlin Heidelberg: Sehat: Anatomi Dan Fisiologi. Yogyakarta: UGMDocument2 pagesTreatment and Prevention. Springer-Verlag Berlin Heidelberg: Sehat: Anatomi Dan Fisiologi. Yogyakarta: UGMJontor KotlNo ratings yet
- Guía de Neuroimagen en Primer EpisodioDocument24 pagesGuía de Neuroimagen en Primer EpisodiokarlunchoNo ratings yet
- Manasika Roga ChikitsaDocument4 pagesManasika Roga ChikitsaReshma rajNo ratings yet
- Anticancer Drugs PDFDocument28 pagesAnticancer Drugs PDFHamza Mylo Senni100% (3)
- Case Report ASDDocument34 pagesCase Report ASDIrwansyah Ghenjy0% (1)
- Implants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitDocument5 pagesImplants in Narrow Ridge Situations: A Piezo-Surgical Approach For Alveolar Ridge SplitNIMMY ANTONo ratings yet
- Classification of Chronic HepatitisDocument4 pagesClassification of Chronic HepatitisVardan KocharNo ratings yet
- Range of Motion PresentationDocument27 pagesRange of Motion Presentationsathish100% (1)
- Nursing InformaticsDocument2 pagesNursing Informaticsapi-469041523No ratings yet
- Impaired Tissue Integrity - Nursing Diagnosis & Care Plan PDFDocument15 pagesImpaired Tissue Integrity - Nursing Diagnosis & Care Plan PDFManar AbdallahNo ratings yet
- NCP For Impaired Physical MobilityDocument2 pagesNCP For Impaired Physical MobilityPrincess Averin Navarro50% (2)
- Cs 19 SolvedDocument4 pagesCs 19 SolvedgogoNo ratings yet
- Hemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?Document4 pagesHemodynamically Stable Left Ventricular Pseudoaneurysm: Who Should Manage - Surgeon or Cardiologist?asclepiuspdfsNo ratings yet
- Clothes Drag Technique: University of Baguio School of Criminal Justice and Public Safety Gen. Luna Road, Baguio CityDocument4 pagesClothes Drag Technique: University of Baguio School of Criminal Justice and Public Safety Gen. Luna Road, Baguio CityMarieRoseGuzmanSubdiNo ratings yet
- Endocrine System: Capillary Glucose MonitoringDocument34 pagesEndocrine System: Capillary Glucose Monitoringjoel david knda mj100% (1)
- Test Your Knowledge About Covid-19Document15 pagesTest Your Knowledge About Covid-19Ranz PanganibanNo ratings yet
- Cardio: Prometric Exam 5/4/2015 Internal MedicineDocument14 pagesCardio: Prometric Exam 5/4/2015 Internal MedicineWalid SakrNo ratings yet
- Induction of LabourDocument45 pagesInduction of LabourVidya RamanathanNo ratings yet
- AbstractBookAbstracts501 1000Document155 pagesAbstractBookAbstracts501 1000Jose Oscar TarazonaNo ratings yet
- Takaful Health2Document34 pagesTakaful Health2yusofprubsnNo ratings yet
- Bawaseer (Hemorrhoids)Document22 pagesBawaseer (Hemorrhoids)drmshiffaNo ratings yet
- Thrombolytics (Fibrinolytics)Document14 pagesThrombolytics (Fibrinolytics)J lodhiNo ratings yet
- NPF Focus1Document12 pagesNPF Focus1ramuNo ratings yet
- A Case Study On Abruptio PlacentaeDocument22 pagesA Case Study On Abruptio Placentaeporskol2No ratings yet
- Dr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiDocument35 pagesDr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiNailahRahmahNo ratings yet
- Febrile Neutropenia Topic DiscussionDocument42 pagesFebrile Neutropenia Topic Discussionapi-647904873No ratings yet
- Orthopedic MCQ (Group 5)Document4 pagesOrthopedic MCQ (Group 5)Law YouNo ratings yet