Professional Documents
Culture Documents
9Tx Epo Policy 3
9Tx Epo Policy 3
Uploaded by
damondouglas0 ratings0% found this document useful (0 votes)
47 views5 pagesAdmissions based on pancreas and / or kidney organ transplantation (STO only) will include a full iron study workup. Sodium ferric gluconate (Ferrlecit(r)) will be administered as 125mg / 100mL every other day.
Original Description:
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAdmissions based on pancreas and / or kidney organ transplantation (STO only) will include a full iron study workup. Sodium ferric gluconate (Ferrlecit(r)) will be administered as 125mg / 100mL every other day.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
Download as doc, pdf, or txt
0 ratings0% found this document useful (0 votes)
47 views5 pages9Tx Epo Policy 3
9Tx Epo Policy 3
Uploaded by
damondouglasAdmissions based on pancreas and / or kidney organ transplantation (STO only) will include a full iron study workup. Sodium ferric gluconate (Ferrlecit(r)) will be administered as 125mg / 100mL every other day.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
Download as doc, pdf, or txt
You are on page 1of 5
Recombinant Erythropoietin Use Protocol for the Solid Organ
Transplantation Service (STO and MTS)
April 20, 2004
1. Admissions based on pancreas and/or kidney organ transplantation (STO only)
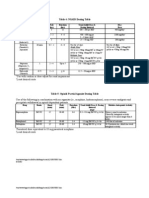
a. Admission labs (pre-transplant) will include a full iron study workup
i. Serum iron
ii. Serum ferritin
iii. Percent iron saturation
1. Transferrin must be ordered for calculation
2. Percent iron saturation = Serum iron / Total iron binding
capacity (TIBC)
3. TIBC = Transferrin / 0.7
b. Iron deficiency
i. Serum ferritin < 100ng/mL
ii. Serum ferritin < 800ng/mL and percent iron saturation < 20%
iii. IV iron administration contraindicated with serum ferritin >
800ng/mL
c. Patients defined as “iron deficient”
i. Starting POD #1, sodium ferric gluconate (Ferrlecit®) will be
administered as 125mg/100mL every other day over 2 hours until
discharge
1. First dose will require test dose 25mg over one hour. If
vitals are stable one hour post-infusion, the remaining
100mg will be administered over 1 hour
a. Reactions could include hypotension, itching, and
rash
b. Not required if patient has already received
2. Total Ferrlecit® will not exceed 1 gram (8 doses)
a. Ferrlecit® dosing can be repeated if:
i. Iron studies repeated every month during
admission indicate iron deficiency
ii. Ferrlecit® dosing within one month does not
exceed 1 gram
3. Discharge of “iron deficient” patients
a. Intolerant of IV iron
i. Started on oral iron supplementation
immediately following failed IV iron
therapy
ii. Ferrous sulfate 325mg tid
b. Received IV iron while inpatient
i. Start on oral iron supplementation upon
discharge if patient did not get total of 1gm
Ferrlecit®
1. Ferrous sulfate 325mg tid
2. Patient must be instructed to take
iron supplementation 2-4 hours
before or after:
a. Mycophenolate mofetil
(Cellcept®)
b. Gatifloxacin (Tequin®)
c. Ciprofloxacin (Cipro®)
ii. Do not start on oral iron supplementation if
patient received total of 1gm Ferrlecit®
ii. Surgical attending, and/or transplant nephrologist may override
protocol Ferrlecit® dosing if patient has concurrent infection
1. Should be documented in daily note
iii. Patient should complete full course if discharged and readmitted
within same month
1. Do not repeat iron studies within one month of previous
iron studies
d. Recombinant human erythropoietin EPO (Epogen® or Procrit®)
i. No patient will receive EPO within 7 days of organ transplantation
ii. Reserved for patients in delayed graft function (DGF) and anemic
1. The designation of “a patient in DGF”, with the respect to
the administration of EPO, will be reserved to:
a. Transplant nephrologist (STO)
b. Transplant surgical attending
2. Anemia is defined as hematocrit < 30 (on 3 blood draws)
iii. Surgical attending, and/or transplant nephrologist may alter
minimum hematocrit if patient has history coronary artery disease
(CAD)
1. Should be documented in daily note
iv. Initial dose
1. All patients initial dose = 10,000 units subcutaneous
weekly (150 units/kilogram per week for ideal body
weights 50 – 87 kg, 5 feet – 6 feet 4 inches)
v. Titration of EPO
1. Within two weeks of initiating EPO
a. Hematocrit increase > 8% of baseline
i. Decrease EPO dose by 25%
b. Hematocrit increase <2% of baseline
i. Increase EPO dose by 50%
2. Hematocrit > 36% for two consecutive weeks
a. Decrease EPO dose by 50%
b. Continue downward titration to discontinuation of
EPO
3. Increments of titration
a. Doses will be increased or decreased using the
following manufacturer designed vials
i. 2000, 3000, 4000, 10000, 20000, 40000
units
4. Goal of therapy
a. Hematocrit > 33 and < 36
2. Admissions based on complications post-transplantation (STO or MTS)
a. Admission labs will include a full iron study workup if:
i. Patient currently on EPO
ii. Serum creatinine > 2.0
1. Iron studies should not be reviewed if most recent
admission (within 30 days) included iron studies
b. Iron study labs
i. Serum iron
ii. Serum ferritin
iii. Percent iron saturation
1. Transferrin must be ordered for calculation
2. Percent iron saturation = Serum iron / Total iron binding
capacity (TIBC)
3. TIBC = Transferrin / 0.7
c. Iron deficiency
i. Serum ferritin < 100ng/mL
ii. Serum ferritin < 800ng/mL and percent iron saturation < 20%
iii. IV iron administration contraindicated with serum ferritin >
800ng/mL
d. Patients defined as “iron deficient”
i. Sodium ferric gluconate (Ferrlecit®) will be administered as
125mg/100mL over 2 hours every other day until discharge
1. First dose will require test dose 25mg over one hour. If
vitals are stable one hour post-infusion, the remaining
100mg will be administered over 1 hour
a. Reactions could include hypotension, itching, and
rash
b. Not required if patient has already received
2. Total Ferrlecit® will not exceed 1 gram
a. Ferrlecit® dosing can be repeated if:
i. Iron studies repeated every month during
admission indicate iron deficiency
ii. Ferrlecit® dosing within one month does not
exceed 1 gram (8 doses)
3. Discharge of “iron deficient” patients
a. The Transplant Infusion Center will utilized to
complete 1 gram of therapy
b. If patient unable to complete full Ferrlecit® course,
patient will be started on oral iron supplementation
i. Patient must be instructed to take iron
supplementation 2-4 hours before or after:
1. Mycophenolate mofetil (Cellcept®)
2. Gatifloxacin (Tequin®)
3. Ciprofloxacin (Cipro®)
c. If patient completed full Ferrlecit® course (8
doses), do not discharge on oral iron
supplementation
ii. MTS attending, MTS nurse practitioner, surgical attending, and/or
transplant nephrologist may override protocol Ferrlecit® dosing if
patient has concurrent infection
1. Should be documented in daily note
iii. Patient should complete full course if discharged and readmitted
1. Do not repeat iron studies within one month of previous
iron studies
e. Recombinant human erythropoietin EPO (Epogen® or Procrit®)
i. Patients admitted receiving EPO will continue their current dose
ii. Patients admitted not currently receiving EPO, can only be
initiated on EPO if all the following are met:
1. Hematocrit < 30
2. Complete iron studies reviewed
3. Stool sent to check for occult blood
4. Reticulocyte count sent (absolute count and percentage)
5. MTS attending, MTS nurse practitioner, surgical attending,
and/or transplant nephrologist has ruled out the following
as causes of decreased hematocrit:
a. Hemolysis
b. Acute hemorrhage
c. Malignancy
d. Medication-induced
i. Only those that will be stopped soon, and
are not chronic medications
1. Included, but not limited to
Thymoglobulin®
iii. MTS attending, MTS nurse practitioner, surgical attending, and/or
transplant nephrologist may alter minimum hematocrit if patient
has history coronary artery disease (CAD)
1. Should be documented in daily note
iv. Initial dose for those patients not currently receiving EPO
1. All patients initial dose = 10,000 units subcutaneous
weekly (150 units/kilogram per week for ideal body
weights 50 – 87 kg, 5 feet – 6 feet 4 inches)
v. Titration of EPO (for patients admitted on EPO or initiated on EPO
in hospital)
1. Within two weeks of initiating EPO or admission
a. Hematocrit increase > 8% of baseline
i. Decrease EPO dose by 25%
b. Hematocrit increase <2% of baseline
i. Increase EPO dose by 50%
2. Hematocrit > 36% for two consecutive weeks
a. Decrease EPO dose by 50%
b. Continue downward titration to discontinuation of
EPO
3. Increments of titration
a. Doses will be increased or decreased using the
following manufacturer designed vials
i. 2000, 3000, 4000, 10000, 20000, 40000
units
4. Goal of therapy
a. Hematocrit > 33 and < 36
3. SMARhT study
a. The patients are excluded from the proceeding protocol
4. Patients admitted with failed renal grafts
a. Follow protocol for “Admissions based on complications post-
transplantation (STO or MTS)”
5. Access or Vascular patients
a. Follow protocol for “Admissions based on complications post-
transplantation (STO or MTS)”
You might also like
- Ferosac InjDocument2 pagesFerosac InjMohamed Taleb75% (4)
- Pharmacology 2 Final Exam 2021-NkDocument16 pagesPharmacology 2 Final Exam 2021-NkT'amo HanashNo ratings yet
- ASSIGNMENT ON DRUGS AND PROCEDURES PERMITTED TO BE USED BY NURSE MIDWIVES BY GoIDocument5 pagesASSIGNMENT ON DRUGS AND PROCEDURES PERMITTED TO BE USED BY NURSE MIDWIVES BY GoIannu panchal100% (1)
- Metabolic Stress Case StudyDocument10 pagesMetabolic Stress Case StudydakotaNo ratings yet
- Psych Clinic Intake & Report OutlineDocument4 pagesPsych Clinic Intake & Report OutlineJulie Anne DeeNo ratings yet
- IVIron IGDocument12 pagesIVIron IGLorenz Joey RicarteNo ratings yet
- Nutrition in Pregnancy & AnaemiaDocument60 pagesNutrition in Pregnancy & AnaemiamohamadehabNo ratings yet
- MATERI 6 Mek. Toksisitas (Overdose)Document7 pagesMATERI 6 Mek. Toksisitas (Overdose)PERMATASARI BKUNo ratings yet
- Problems With The Thyroid GlandDocument10 pagesProblems With The Thyroid GlandElla Marie CruzadaNo ratings yet
- Curative Treatment of IDADocument40 pagesCurative Treatment of IDARakshita JainNo ratings yet
- Drug Guideline For Iron Polymaltose InjectionDocument7 pagesDrug Guideline For Iron Polymaltose Injectionmirza_baig_46No ratings yet
- Ferrous Sulfate Fer-In-SolDocument2 pagesFerrous Sulfate Fer-In-SolMilagrosMariaLlanosMamaniNo ratings yet
- Hematinics-Reading MaterialsDocument3 pagesHematinics-Reading MaterialsbNo ratings yet
- Hypothyroidism TestDocument6 pagesHypothyroidism TestVrushaliNo ratings yet
- Low Molecular Weight Heparins (LMWH) : I. Mechanism of ActionDocument7 pagesLow Molecular Weight Heparins (LMWH) : I. Mechanism of ActionIniya RajendranNo ratings yet
- Ferrous Sulphate NeomedDocument3 pagesFerrous Sulphate NeomedShuaib KauchaliNo ratings yet
- Oral and Parenteral Iron Preparations in PregnancyDocument45 pagesOral and Parenteral Iron Preparations in PregnancyArun George100% (3)
- Assessment TAsk PharmacodynamicsDocument2 pagesAssessment TAsk PharmacodynamicsMelvin Lazaro CabusoNo ratings yet
- Daunorubicin Hydrochloride IV Over 6 Hours On Days 1, 3, and 5, and Etoposide IV Over 4Document4 pagesDaunorubicin Hydrochloride IV Over 6 Hours On Days 1, 3, and 5, and Etoposide IV Over 4Mohammed HaiderNo ratings yet
- Management of Anaemia in PregnancyDocument8 pagesManagement of Anaemia in PregnancyAnonymous 9dVZCnTXSNo ratings yet
- Mastery Test 2 On MS 1Document17 pagesMastery Test 2 On MS 1Rika MaeNo ratings yet
- Extended Infusion Beta-Lactams ProtocolDocument9 pagesExtended Infusion Beta-Lactams ProtocolKanaga6432No ratings yet
- 9.2016. Parenteral Iron Therapy For Ida in PregnancyDocument2 pages9.2016. Parenteral Iron Therapy For Ida in PregnancynaquibroslanNo ratings yet
- Preparations of Intravenous IronDocument5 pagesPreparations of Intravenous IronSri Siti KhadijahElfNo ratings yet
- 2 - Canine and Feline Anesthesia GuidelinesDocument14 pages2 - Canine and Feline Anesthesia Guidelinesunknowen 22No ratings yet
- Amphotericin B Infusion ProtocolDocument1 pageAmphotericin B Infusion ProtocolNatasha MunapNo ratings yet
- Daunorubicin Hydrochloride IV Over 6 Hours On Days 1, 3, and 5, and Etoposide IV Over 4Document3 pagesDaunorubicin Hydrochloride IV Over 6 Hours On Days 1, 3, and 5, and Etoposide IV Over 4Mohammed HaiderNo ratings yet
- Pharmacology Adrenal GlandsDocument3 pagesPharmacology Adrenal GlandsMarc FosterNo ratings yet
- Administration of FerinjectDocument5 pagesAdministration of FerinjectSalma Al nemriNo ratings yet
- Ob ReviewerDocument6 pagesOb Reviewerjanelle tapiruNo ratings yet
- DesferalDocument11 pagesDesferalFalisha Belvia KairinNo ratings yet
- Long Quiz Drugs For Endocrinologic DisordersDocument4 pagesLong Quiz Drugs For Endocrinologic Disorderspay tinapayNo ratings yet
- Understanding Medical Surgical Nursing - 0845-0845Document1 pageUnderstanding Medical Surgical Nursing - 0845-0845Anas TasyaNo ratings yet
- Iron Supplement - During Pregnancy, Requirements For Iron IncreaseDocument1 pageIron Supplement - During Pregnancy, Requirements For Iron Increasegeorgeloto12No ratings yet
- FCM InsertDocument1 pageFCM InsertFida MarvatNo ratings yet
- DISP-CalculationsWorksheetLab LecDocument4 pagesDISP-CalculationsWorksheetLab LecRafaelaNo ratings yet
- Imidocarb Summary Report 2 Committee Veterinary Medicinal Products enDocument6 pagesImidocarb Summary Report 2 Committee Veterinary Medicinal Products enGilsson FigueroaNo ratings yet
- Thyroid & Antithyroid Drugs - 2020Document7 pagesThyroid & Antithyroid Drugs - 2020ireneNo ratings yet
- ObsNGyn - Medical Disorders in Pregnancy AtfDocument15 pagesObsNGyn - Medical Disorders in Pregnancy Atfosman nurNo ratings yet
- SMILE (Etoposide, Ifosfamide, Methotrexate and Dexamethasone)Document7 pagesSMILE (Etoposide, Ifosfamide, Methotrexate and Dexamethasone)SolikinNo ratings yet
- PharmacoDocument4 pagesPharmacoRouie Björn ABrianNo ratings yet
- Cuarta ParteDocument15 pagesCuarta ParterrhhNo ratings yet
- CancerDocument14 pagesCancerClara De Guzman83% (6)
- BloodDocument27 pagesBloodPATRICK ROSHAN ANo ratings yet
- Tutorial 2 - KGDocument4 pagesTutorial 2 - KGAbdurRahmanShafiNo ratings yet
- I. See Also: MyocardiumDocument4 pagesI. See Also: MyocardiumGiorgi NanetashviliNo ratings yet
- Ati Pharmacology Proctored ExamDocument4 pagesAti Pharmacology Proctored Examkinyuaboris990No ratings yet
- Human Albumin Prescription - AdministrationDocument4 pagesHuman Albumin Prescription - AdministrationKarissa MagaruNo ratings yet
- SQC ABx Guidelines 2-21-2011 PDFDocument2 pagesSQC ABx Guidelines 2-21-2011 PDFMinh SteveNo ratings yet
- Amoxicillin 125 MG 250 MG 5 ML Oral SuspensionDocument16 pagesAmoxicillin 125 MG 250 MG 5 ML Oral SuspensionAshrafNo ratings yet
- Boston Medical Center Maternity Care Guideline Guideline: Iron Defficiency Anemia Accepted: Updated: 04/2015Document4 pagesBoston Medical Center Maternity Care Guideline Guideline: Iron Defficiency Anemia Accepted: Updated: 04/2015Fernando Cardenas AriasNo ratings yet
- 35 Items Saunders Fluids and ElectrolytesDocument4 pages35 Items Saunders Fluids and ElectrolytesKrystelle Jade LabineNo ratings yet
- Pre Exam Answers I FoundDocument73 pagesPre Exam Answers I FoundDuy LuuNo ratings yet
- Ferrous Sulfate Syrup InsertDocument6 pagesFerrous Sulfate Syrup InsertPrincess TiongsonNo ratings yet
- Iron Deficiency Anemia in Pregnant Woman (RAD)Document24 pagesIron Deficiency Anemia in Pregnant Woman (RAD)Radziah Abd malekNo ratings yet
- Anemia in Pregnancy by MahreeDocument53 pagesAnemia in Pregnancy by MahreesherzadmahreeNo ratings yet
- Pharmacy & Medical Store Procedure.Document22 pagesPharmacy & Medical Store Procedure.Google BdNo ratings yet
- Iron Isomaltoside Monofer Final April 2011 Amended 030511 For WebsiteDocument8 pagesIron Isomaltoside Monofer Final April 2011 Amended 030511 For WebsiteUmaima faizNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- PIs Drug InteractionDocument1 pagePIs Drug InteractiondamondouglasNo ratings yet
- IV PO Conversion P&P.V2Document3 pagesIV PO Conversion P&P.V2damondouglasNo ratings yet
- University of Maryland Medical Center Fluconazole (Diflucan®)Document6 pagesUniversity of Maryland Medical Center Fluconazole (Diflucan®)damondouglasNo ratings yet
- Restricted AntimicrobialsDocument1 pageRestricted AntimicrobialsdamondouglasNo ratings yet
- Antimicrobial Renal DosingDocument5 pagesAntimicrobial Renal DosingdamondouglasNo ratings yet
- CAP Guidelines For UseDocument11 pagesCAP Guidelines For Usedamondouglas100% (1)
- CAP AlgorithmDocument1 pageCAP AlgorithmdamondouglasNo ratings yet
- 3.E.2-Caspofungin Guideline 2003Document3 pages3.E.2-Caspofungin Guideline 2003damondouglasNo ratings yet
- Sedation Pain AlgorithmDocument1 pageSedation Pain Algorithmdamondouglas100% (2)
- Perioperative Antibiotics For Surgical ProphylaxisDocument1 pagePerioperative Antibiotics For Surgical ProphylaxisdamondouglasNo ratings yet
- Sodium Content of Inject Able AntibioticsDocument1 pageSodium Content of Inject Able AntibioticsdamondouglasNo ratings yet
- Antibiogram 07Document1 pageAntibiogram 07damondouglas100% (1)
- CAP Guidelines For UseDocument11 pagesCAP Guidelines For Usedamondouglas100% (1)
- PONV GuidelinesDocument3 pagesPONV GuidelinesdamondouglasNo ratings yet
- IV Insulin - FinalDocument18 pagesIV Insulin - Finaldamondouglas100% (2)
- Opioid Equianalgesic ChartDocument1 pageOpioid Equianalgesic Chartdamondouglas100% (7)
- Hypertensive Urgency EmergencyDocument5 pagesHypertensive Urgency Emergencydamondouglas100% (3)
- NSAID Agonist Antagonist TableDocument1 pageNSAID Agonist Antagonist TabledamondouglasNo ratings yet
- IV PO ConversionsDocument1 pageIV PO Conversionsdamondouglas100% (1)
- GCC Anti Emetic Guidelines 2003Document2 pagesGCC Anti Emetic Guidelines 2003damondouglasNo ratings yet
- Practice Guidelines: Enteral Nutrition Delivery For The Adult PatientDocument15 pagesPractice Guidelines: Enteral Nutrition Delivery For The Adult Patientdamondouglas100% (1)
- HIT ProtocolDocument1 pageHIT ProtocoldamondouglasNo ratings yet
- IV PO Conversion CAPDocument3 pagesIV PO Conversion CAPdamondouglasNo ratings yet
- Hyperglycemia Algorithm 2Document1 pageHyperglycemia Algorithm 2damondouglasNo ratings yet
- Antifungal GuidelineDocument2 pagesAntifungal GuidelinedamondouglasNo ratings yet
- Clostridium Difficile Guideline - UMMCDocument5 pagesClostridium Difficile Guideline - UMMCdamondouglas100% (3)
- Calcium Gluconate Infusion Guideline For Use in CVVHDDocument1 pageCalcium Gluconate Infusion Guideline For Use in CVVHDdamondouglas100% (1)
- Calcium Dosing For PediatricsDocument1 pageCalcium Dosing For PediatricsdamondouglasNo ratings yet
- Antibiotic Dosing ESRDDocument6 pagesAntibiotic Dosing ESRDdamondouglas100% (3)
- RhabdovirusDocument74 pagesRhabdovirustummalapalli venkateswara raoNo ratings yet
- So You Want To Be A Urologist?: The First StepDocument2 pagesSo You Want To Be A Urologist?: The First StepDrThamma ShahiNo ratings yet
- Steroid Hyperglycemia: Prevalence, Early Detection and Therapeutic Recommendations: A Narrative ReviewDocument10 pagesSteroid Hyperglycemia: Prevalence, Early Detection and Therapeutic Recommendations: A Narrative ReviewMade Dedy KusnawanNo ratings yet
- 2011 Primary (Arabic Board)Document25 pages2011 Primary (Arabic Board)Mustafa Ismael NayyefNo ratings yet
- Dissociative Identity Disorder (DID) : Presented By: Joseph Rafael B. MasingDocument15 pagesDissociative Identity Disorder (DID) : Presented By: Joseph Rafael B. MasingIan Francis RojasNo ratings yet
- AIPGMEE 2006 Question PaperDocument96 pagesAIPGMEE 2006 Question PaperpavaniNo ratings yet
- Grade 3 Sense Organs, Nose Tongue and SkinDocument3 pagesGrade 3 Sense Organs, Nose Tongue and SkinPhen OrenNo ratings yet
- DR Nalli R GopinathDocument16 pagesDR Nalli R GopinathBabu RamakrishnanNo ratings yet
- Price ALL Z-VentDocument9 pagesPrice ALL Z-VentPanco NanaNo ratings yet
- Burning Mouth SyndromeDocument3 pagesBurning Mouth SyndromeYohana RebeccaNo ratings yet
- Gintex DSDocument1 pageGintex DSRaihanulKabirNo ratings yet
- Epidemiology of Covid-19 in A Long-Term Care Facility in King County, WashingtonDocument9 pagesEpidemiology of Covid-19 in A Long-Term Care Facility in King County, WashingtonZelgi PutraNo ratings yet
- Pharmacology of Silymarin: F. Fraschini, G. Demartini and D. EspostiDocument15 pagesPharmacology of Silymarin: F. Fraschini, G. Demartini and D. EspostiVennyNo ratings yet
- Year Book 2018-19 (21-08-20) - 1Document365 pagesYear Book 2018-19 (21-08-20) - 1Tabib Afzaal Ahmad VirkNo ratings yet
- Important Questions For Esic Staff Nurse Recruitment ExamDocument4 pagesImportant Questions For Esic Staff Nurse Recruitment ExamSuchitaNo ratings yet
- AOGD Bulletin December 2019Document68 pagesAOGD Bulletin December 2019Abhilekh SrivastavaNo ratings yet
- Neck Anatomy: Lymph NodesDocument5 pagesNeck Anatomy: Lymph NodesKiara GovenderNo ratings yet
- First AidDocument72 pagesFirst AidNaushad AliNo ratings yet
- ECG (Rythm Interpretation)Document39 pagesECG (Rythm Interpretation)RatnaSuryati100% (1)
- Menopause KDocument36 pagesMenopause Kkarendelarosa06100% (2)
- COMLEX Level 3 Time Grid and Self AssessmentDocument19 pagesCOMLEX Level 3 Time Grid and Self AssessmentR KidderNo ratings yet
- 06ectropion & EntropionDocument17 pages06ectropion & EntropionShari' Si Wahyu100% (1)
- High-Efficiency and High-Flux Hemodialysis: Sivasankaran Ambalavanan Gary Rabetoy Alfred K. CheungDocument10 pagesHigh-Efficiency and High-Flux Hemodialysis: Sivasankaran Ambalavanan Gary Rabetoy Alfred K. CheungveiaNo ratings yet
- Immunofluorescence Analyzer: Lifotronic FA-160Document2 pagesImmunofluorescence Analyzer: Lifotronic FA-160Bodega PromalabNo ratings yet
- Internet AddictionDocument23 pagesInternet AddictionAdam Bullock100% (1)
- Amandeep Kaur Nursing Demonstrator Ionurc, Goindwal Sahib, PunjabDocument20 pagesAmandeep Kaur Nursing Demonstrator Ionurc, Goindwal Sahib, PunjabSanjay Kumar SanjuNo ratings yet
- Department of Education: Individual Workweek Plan August 2021Document5 pagesDepartment of Education: Individual Workweek Plan August 2021Jeffren P. MiguelNo ratings yet
- ResearchDocument3 pagesResearchDr Sreeja KSNo ratings yet
- A Psychobiological Perspective On The Personality Disorders: LarryDocument12 pagesA Psychobiological Perspective On The Personality Disorders: LarryDrobota MirunaNo ratings yet