Professional Documents
Culture Documents
Loryang Casecon
Loryang Casecon
Uploaded by
Richard AbucayCopyright:
Available Formats
You might also like
- Dentist JurisprudenceDocument8 pagesDentist JurisprudenceSANDEEP100% (1)
- Tata Projects Offer Letter For Rayudu Sai Chandra Sekhar PDFDocument14 pagesTata Projects Offer Letter For Rayudu Sai Chandra Sekhar PDFAnonymous TX8oMMr280% (5)
- NURS FPX 6218 Assessment 1 Proposing Evidence-Based ChangeDocument6 pagesNURS FPX 6218 Assessment 1 Proposing Evidence-Based ChangeEmma WatsonNo ratings yet
- Nursing Upper Gi BleedingDocument23 pagesNursing Upper Gi BleedingLord Pozak Miller100% (3)
- Case Study - FractureDocument35 pagesCase Study - FractureJo-anne Cordero100% (4)
- Case Study On MalariaDocument18 pagesCase Study On MalariaBie WeNna100% (4)
- Gastroenteritis Care StudyDocument13 pagesGastroenteritis Care StudyÄxxö Ahkö Hinoguin50% (2)
- GAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolFrom EverandGAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolRating: 5 out of 5 stars5/5 (1)
- Case (Ovarian New Growth) (Gyne)Document5 pagesCase (Ovarian New Growth) (Gyne)Rona PieNo ratings yet
- Case Study On BurnsDocument16 pagesCase Study On BurnsRoanne Lagua100% (2)
- Pedia With LeukemiaDocument14 pagesPedia With LeukemiaAlynna ValbuenaNo ratings yet
- 52 Teen Boy Problems & How To Solve ThemDocument99 pages52 Teen Boy Problems & How To Solve ThemCristiano RochaNo ratings yet
- PT2012b PDFDocument59 pagesPT2012b PDFPhạm Thủy Cương100% (1)
- Comprehensive Nursing Care Plan: San Lazaro HospitalDocument37 pagesComprehensive Nursing Care Plan: San Lazaro HospitalKim AntonetteNo ratings yet
- 3rd Year Precept Pedia Case 4 HydroceleDocument4 pages3rd Year Precept Pedia Case 4 Hydrocelekristel_nicole18yaho100% (1)
- 28099453C Case Study 3Document27 pages28099453C Case Study 3Alice HuiiNo ratings yet
- 13 Areas DutyDocument3 pages13 Areas DutyAndrei MarcosNo ratings yet
- Client'S Profile: A. Demographic DataDocument11 pagesClient'S Profile: A. Demographic DataLincoln Cullen Tumulak SumayloNo ratings yet
- A Case Study of Hyperthermia Related To Infection As Evidenced by 38.9 C and Foul Smelling Post-Operative WoundDocument10 pagesA Case Study of Hyperthermia Related To Infection As Evidenced by 38.9 C and Foul Smelling Post-Operative WoundCleo Joyce C. CristalNo ratings yet
- Asuhan Keperawatan: Name: Ny. Sumini Age: Sex: Nationality: Company: Education:: Address: Date MRS: DiagnoseDocument5 pagesAsuhan Keperawatan: Name: Ny. Sumini Age: Sex: Nationality: Company: Education:: Address: Date MRS: DiagnosebennyarekakperNo ratings yet
- 13 AREAS of ASSESSMENTDocument2 pages13 AREAS of ASSESSMENTCrystal Queen MarquezNo ratings yet
- Cerebrovascular Disease (Bleed)Document25 pagesCerebrovascular Disease (Bleed)Margaret Jenaw JenawNo ratings yet
- Matt 2Document3 pagesMatt 2Matthew CalaraNo ratings yet
- Case Pres Cerebrovascular DiseaseDocument34 pagesCase Pres Cerebrovascular DiseaseADRIATICO JAROSLUVNo ratings yet
- Case Study 3Document27 pagesCase Study 3jazmae100% (2)
- Case StudyDocument57 pagesCase StudyJoy-Rena Sabinay OchondraNo ratings yet
- 13 Areas of Assessment I. Psychological StatusDocument3 pages13 Areas of Assessment I. Psychological StatusjoharaqohNo ratings yet
- Case Study Abdominal Blunt InjuryDocument10 pagesCase Study Abdominal Blunt InjuryHomework PingNo ratings yet
- Case Study On NSVDDocument50 pagesCase Study On NSVDNyj Quiño100% (2)
- 13 AREAS of ASSESSMENT (Geriatrict Ward)Document2 pages13 AREAS of ASSESSMENT (Geriatrict Ward)Crystal Queen Marquez100% (1)
- Ii. Chief ComplaintsDocument4 pagesIi. Chief ComplaintsArianne_Danglo_2118No ratings yet
- ADocument20 pagesADivinity Ü NicaNo ratings yet
- (Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)Document20 pages(Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)MikaCasimiroBalunanNo ratings yet
- Patient Health HistoryDocument8 pagesPatient Health HistoryRafi LabNo ratings yet
- HEALTH HISTORY WPS Office - Docx 1Document7 pagesHEALTH HISTORY WPS Office - Docx 1Cy PilapilNo ratings yet
- Case Presentation FinalDocument22 pagesCase Presentation Finalmafi0914No ratings yet
- Alyssa MaprideDocument2 pagesAlyssa MaprideMatthew CalaraNo ratings yet
- Case Study On Scarlet Fever12Document36 pagesCase Study On Scarlet Fever12Mark Sherwin LazoNo ratings yet
- Assessment and ClientDocument4 pagesAssessment and ClientEddie Lou GuzmanNo ratings yet
- CockDocument43 pagesCockAkuoko EricaNo ratings yet
- BPHDocument15 pagesBPH'mYk FavilaNo ratings yet
- FInal PowerpointDocument77 pagesFInal PowerpointJacky ChanNo ratings yet
- GoutDocument75 pagesGoutVan Talawec100% (2)
- Case English 1 - NDI Edit 220419Document24 pagesCase English 1 - NDI Edit 220419syongebobNo ratings yet
- AreasDocument2 pagesAreasKyre LandinginNo ratings yet
- April LeDocument21 pagesApril LeAprille Anne SagmitNo ratings yet
- Pattern Writing ExampleDocument14 pagesPattern Writing ExampleScribdTranslationsNo ratings yet
- Ent Case StudyDocument18 pagesEnt Case StudyKristian Karl Bautista Kiw-isNo ratings yet
- Case Study-Gastric CancerDocument19 pagesCase Study-Gastric Cancerbhelskie100% (2)
- Ob AssessmentDocument2 pagesOb AssessmentNathalie kate petallarNo ratings yet
- Final Case (Postpartum)Document14 pagesFinal Case (Postpartum)KimJohnSanchoManeroNo ratings yet
- A Case Study On Graves DiseaseDocument46 pagesA Case Study On Graves DiseaseRenie SerranoNo ratings yet
- A. Background of The StudyDocument14 pagesA. Background of The StudyronkathNo ratings yet
- Case Presentation: Group 9Document141 pagesCase Presentation: Group 9marialourdes2489No ratings yet
- Chronic Calculous CholecystitisDocument63 pagesChronic Calculous CholecystitisAYTONA, JAMAICA F.No ratings yet
- Learning Materials and Students WorksheetDocument5 pagesLearning Materials and Students WorksheetRatu Rini NurhayatiNo ratings yet
- Preterm Labor Case StudyDocument26 pagesPreterm Labor Case StudyKirk Espanol Bigstone82% (11)
- 13 Areas of AssessmentDocument2 pages13 Areas of AssessmentCrystal Queen MarquezNo ratings yet
- Hypokalemia Periodic ParalysisDocument14 pagesHypokalemia Periodic ParalysisJennirose JingNo ratings yet
- MattDocument3 pagesMattMatthew CalaraNo ratings yet
- NCP Heart FailureDocument11 pagesNCP Heart FailureaZhermAine100% (1)
- College of Nursing: Panpacific University North PhilippinesDocument20 pagesCollege of Nursing: Panpacific University North PhilippinesMar OrdanzaNo ratings yet
- Mindanao State University Iligan Institute of Technology College of Nursing Resource UnitDocument33 pagesMindanao State University Iligan Institute of Technology College of Nursing Resource UnitDanielle Faye ClerigoNo ratings yet
- Carpe Diem Ruiz Protcol Grand Rounds 4Document9 pagesCarpe Diem Ruiz Protcol Grand Rounds 4John Christopher RuizNo ratings yet
- Makita DUR369AZDocument160 pagesMakita DUR369AZAnonymous 4fOfUqNo ratings yet
- Bulletin of The United States Army MedicDocument3 pagesBulletin of The United States Army Medicbaladewa75No ratings yet
- Sandy-Hook SHAC Doc 2015.02.13 Draft Version of Final ReportDocument256 pagesSandy-Hook SHAC Doc 2015.02.13 Draft Version of Final ReportHelen BennettNo ratings yet
- "A Complete Health App": Designed by New HaircutDocument16 pages"A Complete Health App": Designed by New Haircutmonika sharmaNo ratings yet
- ABYIPDocument5 pagesABYIPJayson Guerrero100% (4)
- Pfizer Inc.: United States Securities and Exchange CommissionDocument246 pagesPfizer Inc.: United States Securities and Exchange CommissionDipanshu NagarNo ratings yet
- SDS Conductivity Standard 15 μScm MSDS USDocument6 pagesSDS Conductivity Standard 15 μScm MSDS USMd. Firozur RahmanNo ratings yet
- Psychology of Sport and Exercise: P. Wylleman, C.G. Harwood, A.-M. Elbe, A. Reints, D. de CaluweDocument12 pagesPsychology of Sport and Exercise: P. Wylleman, C.G. Harwood, A.-M. Elbe, A. Reints, D. de CaluweAraya ThimlamomNo ratings yet
- Sumber Data SIKDocument34 pagesSumber Data SIKandy azizNo ratings yet
- Wingila Mpamila Worksheet 8Document2 pagesWingila Mpamila Worksheet 8welcome martinNo ratings yet
- Candice Gorremans - Wellness Consultant ResumeDocument2 pagesCandice Gorremans - Wellness Consultant Resumeapi-289209614No ratings yet
- Pharmacology of Disopyramide: Yosephine A. H. 020100058Document20 pagesPharmacology of Disopyramide: Yosephine A. H. 020100058zulfantri1983No ratings yet
- Position Paper On Child PovertyDocument10 pagesPosition Paper On Child PovertyJr YansonNo ratings yet
- Peningkatan Dukungan Sosial Orang Tua Dengan Anak Skizofrenia Melalui Solution Focused TherapyDocument12 pagesPeningkatan Dukungan Sosial Orang Tua Dengan Anak Skizofrenia Melalui Solution Focused TherapyziraNo ratings yet
- PNS For MilkfishDocument11 pagesPNS For MilkfishJohn Christopher NolialNo ratings yet
- Time Blocking PDFDocument65 pagesTime Blocking PDFlynn_y95% (20)
- Universal Crescent Power P LTD EIA Report Part IDocument66 pagesUniversal Crescent Power P LTD EIA Report Part ImanishxlriNo ratings yet
- NUR 111 Session 22 SAS SemillaDocument2 pagesNUR 111 Session 22 SAS SemillaCyrille Jhane A GalvezNo ratings yet
- Research ProjectsDocument2 pagesResearch Projectsapi-143464694No ratings yet
- Vox Bikol Vol. 28 Issue No. 27Document8 pagesVox Bikol Vol. 28 Issue No. 27andyvgimpayaNo ratings yet
- Good Laboratory PracticesDocument5 pagesGood Laboratory PracticesRajendra ChaudharyNo ratings yet
- Mica Flake MSDSDocument2 pagesMica Flake MSDSMayank RajgarhiaNo ratings yet
- Sample WHS ManualDocument16 pagesSample WHS Manualzahidahmed42100% (1)
- CÁC BÀI ĐỌC ĐIỀN - SGK 12 (OLD)Document17 pagesCÁC BÀI ĐỌC ĐIỀN - SGK 12 (OLD)linhvu.youthplusNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet
Loryang Casecon
Loryang Casecon
Uploaded by
Richard AbucayOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Loryang Casecon
Loryang Casecon
Uploaded by
Richard AbucayCopyright:
Available Formats
DATA BASE AND HISTORY
Patient Z, 81 years old, widowed, Filipino, a Roman Catholic from Ibabao, Agus, Lapu-Lapu City was admitted for the first time in VSMMC last January 31, 2011 at around 12:30 pm due to an inflamed wound at Right maxillary area of her face. Three months PTA, the patient had a small wart on her Right cheek as reported by patients S.O. but was not taken care of. The wart increased in size due to skin irritation such as scratching resulted to further infection.Two months PTA, the S.O. encouraged the patient to have a check-up on the nearest health center because of the increase of the size of the wart forming a mass but was then advised to go to the district hospital but the patient refused to do so. A month PTA, the S.O noticed a moist drainage from the mass. Two weeks PTA, the drainage became more purulent without reporting it to her S.O. The patient continues to rub the mass because of pruritic sensation. Two days PTA, the S.O. noticed a bloody discharge from the mass prompted them to seek medical attention at Lapu-Lapu City District Hospital later was referred to VSMMC for further medical management. The patient was then diagnosed with Squamous Cell carcinoma with the following Vital Signs upon admission of TEMP:37.1 C; PULSE:81bpm RESPIRATORY: 25cpm; BP: 140/90 mmHg. The patient has not received any blood transfusion before and has no known allergies to food and drugs. The patient was accompanied by her daughter-in-law. Her mother and father died by age, 12th rank in the family out of 18 siblings. She has 6 children and owns a Sari-Sari store. She lived in a concrete house which she owns with 3 rooms with her grandchildren and daughter-in-law. She usually awakens at night at around 11-12 oclock in the midnight to urinate and six times all in all in one day. And preferred to be in side-lying position when sleeping. Usually defecates every other day, as reported by the patient at around 8 oclock in the morning with a semi-formed stool, mode of human waste is water-sealed. The patient usually takes her breakfast at around 7 oclock in the morning with coffee and bread and lunch usually around 12 oclock in the afternoon and dinner around 6 in the evening. Likes to eat fish and utan. Takes a nap at 1-4 oclock in the afternoon and usually have snacks in between meals. Takes a bath once a day, shampoo her hair once a week and do handwashing as necessary and gargles with salt. There water source is artesian well for daily use and Distilled water for drinking and stores it in a dispenser and pitcher. Usually likes to watch t.v. and sleeps. The patient has no heredofamilial disease of Asthma, Diabetes Mellitus and Cancer but has Hypertension. Menarche of patient when she
was 14 years old, onset every second week of the month duration of 3-7 days, 30-day cycle with scanty bleeding and dysmenorrhea rarely occurs. She does not experience any difficulty encountered during her pregnancy with an obstetrical record of G-6,P-6, A-O. And the patient menopause at the age of 54 years old. The patient has no previous illness or surgery. And the patients present illness is Squamous Cell Carcinoma at Right maxillary area, a malignant proliferation arising from the epidermis.
SUBJECTIVE COMMUNICATION Comments Dili kayo siya makadungog day pero wala man siya maggamit ug eyeglass as verbalized by the pt. S.O. OXYGENATION Comments Naa na siyay ubo day magduha na ka semana as verbalized by the S.O. of the patient.
OBJECTIVE
The pupil size is 3mm on both Right and Left eyes. REACTION is Pupil Equally Round Reactive to Light Accommodation. Needs repetition of words before she could comprehend it. The respiratory rate of the patient is 16cpm with symmetrical chest expansion, nonproductive cough noted, wheezes heard upon auscultation, use of accessory muscle upon inhalation and expiration CIRCULATION The pulse of the patient is Comments Kung mulingkod 80bpm upon assessment. ko kay akong ipapatong ang Numbness of lower extremities akong tiil as verbalized by the reported by the patient. No pt. ankle edema noted. NUTRITION Comments Ginagmay ra jud na siya mukaon day pero mukaon man jud siya as verbalized by the S.O. ELIMINATION Date of Last Bowel Movement was on February 2, 2012 (date of assessment is February 4, 2012. Urinary frequency of 6-7 times MGT. OF HEALTH & ILLNESS LMP Pt. has menopause at age 55 years old. No history of alcohol intake reported. Patient has no difficulty in swallowing and recent change in appetite reported. The patient has no dentures but has partial teeth in both upper and lower palate. 10 borborygmous sounds heard upon auscultation per minute. Abdominal distention noted. Urine is light yellow in color with aromatic smell. Due to patients age, she cannot follow the treatment regimen but the S.O. of the patient is compliant to any treatment advised.
SUBJECTIVE
OBJECTIVE
SKIN INTEGRITY Comments Uga na jud ang pamanit sa tigulang day pero katol kaayo kaning dapit sa akong samad as verbalized by the patient. ACTIVITY/SAFETY Comments Manggunit siya kung mulakaw siya day niya usahay kay amo nalang siya palingkuron sa wheelchair para dili siya matumba as verbalized by S.O. of the patient. COMFORT/SLEEP/AWAKE Comments Maglisud ko ug katulog diri sa ospital day mong matulog nalang ko ug buntag, udto as verbalized by the S.O. of the patient. COPING The patient owns a sari-sari store near her house but depends on the financial support of her children. Her grandson is the most supportive member of her household
The skin is dry, warm to touch. A small erythema noted located at the right thigh of the patient. Patient is seen touching the mass and reported pruritic sensation on the area. The mass is covered with clean OS and changed every day. Limited motion of joint and when ambulating and changing position. Patient needs assistance in changing clothes but can feed herself. Patient is conscious, awake and responds some of the questions asked. There is pain on the maxillary area, pt. verbalized having sleeping difficulties. Patient seen taking naps in the afternoon. Siderails are raised to prevent fall and any other forms of injury. Patient does answer some of the questions asked but most of the time the S.O. do the answering but they are very cooperative and open to any questions asked.
IV. MEDICAL-SURGICAL MANAGEMENT
IDEAL LABORATORY EXAMINATIONS SCC Antigen released when SCCA is present PHARMACOLOGIC ERBITUX- epidermal growth factor receptor inhibitor -slow down/stop cell growth BLENOXANE- Bleomycin, antibiotic, antineoplasptic DIET High LYCOPENE High Vitamin E and C Low fiber TREATMENT EXCISION (SIMPLE)P- the doctor will cut out the cancerous tissue surrounding margin of healthy skin CURRETAGE and ELECTRODESICATIONscraping away cancer cells and using the electricity to kill any that any that remains JOHNS Surgery- removing the layer of skin and looking at it immediately under a microscopy then removing many layer of skin until there is no sign of cancer cells CHEMOTHERAPY-antineoplastic agents are used in attempt to destroy tumor cells by interfering cellular functions and reproduction SURGERY CRYOSURGERY-destroy tumor by deep freezing the tissue ELECTROSURGERYdestruction/ removal of tissue by electrical energy(heat) MOHs Micrographic Surgerytechnique that is most accurate and that best conserves the normal tissue. LASER THERAPY- intense beam of light vaporize the growth usually ACTUAL CBC U/A CxR ENALAPRIL MALEATE- antihypertensive Vitamin B-compexsupplement Ferrous Sulfate-Iron preparation Azithromycin- antibiotic CIPROFLOXACIN- anti-infective DAT Limit fluids to 1,200L/ day
INCISION BIOPSY- impending results BLOOD TRANSFUSION- to correct anemia - Last February 2&3, 2012 - O+
For schedule operation after anemia is corrected CP clearance-cleared
with little damage to surrounding tissue and with a reduced risk of bleeding, swelling and scarring.
Reference: Medical-Surgical Nursing Volume 2 10th edition
DISCHARGE SUMMARY
NAME of PATIENT: FAUSTINA AMORES_______________
MEDICATIONS
EXERCISE
TREATMENT
HEALTH-TEACHING
OUT-PATIENT
DIET
SPIRITUAL
Educated the patient and S.O. about the importance of drugs being prescribed, dosage and treatment regimen must be completed especially if the patient is prescribed with antibiotic to prevent microorganism-resistance. Sunscreens are also part of medication if there is any being prescribed by the doctor. Considering the age of the patient, exercise is limited to patient. Encouraging patient and S.O. to do active and passive ROM to avoid joint stiffness. Encouraged patient accompanied by her S.O. ambulatep as much as possible to increase gastric motility and avoiding sun exposure during 10AM-2PM. Encouraged S.O. of the patient for the continuation of Blood transfusion. The patient received to bags of PRBC lacking 2 and 1 bag standby for operation. Adviced the S.O. and the patient to comply all medications prescribed. Antibiotic creams are also applied to the site to prevent opportunistic infection. Instructed S.O. the importance of handwashing before and after handling the wound or whenever in contact with it. See to it that the dressing is intact, clean and if possible dry. Apply emollient cream, not powder, unto the surrounding area of the site to prevent dryness and further injury. Note that powder can be an irritant to the open wound. Instructed the S.O. and the patient to avoid unnecessary sun exposure (between 10am-2pm). Advise patient to wear protective clothing whenever going out. The wound is usually covered with a dressing to protect site from physical trauma and irritants, the patient is reminded with a note when will the patient be back for dressing change or if possible the S.O. is taught how to do wound dressing if in case it is on a daily basis. Discussed the importance of daily and proper wound dressing. Encouraged S.O. to watch signs of excessive bleeding and report to nearest hospital if possible. Advised the S.O. of the patient to prepare foods that are rich in lycopene like tomato,Vitamin E and C because they have antioxidant properties that help fight against cancer by slowing/ preventing the growth of cancerous cells. Also, advised patient to eat fruits and vegetables that promote wound healing and tissue repair( greenleafy). Increased fluid intake to flush out toxins in the body as tolerated by the patient and as remedy to constipation as well. Encouraged patient to continue have faith in God. Patient is a vocal, religious Roman Catholic. Encourage S.O. and patient to pray together.
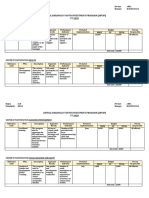
DATE ORDER ED 2/3/201 2
DIAGNOSTIC/ LABORATORY EXAMINATIONS
NORMAL VALUES
UNIT
RESULT
INTERPRETATION
2/1/201 2
Urinalysis Color Transparen cy Specific Gravity pH Protein Glucose RBC WBC Hematology(C BC) WBC HgB HcT MCV MCH RBC MCHC RDW MPV Platelet Differential Neutrophil Lymphocyte Monocyte Eosinophil Basophil Hematology (CBC) HgB
Yellow Cloudy 1.015 7.5 (---) (---) 0-2 10-25
4.8-10.8 120-160 0.37-0.47 81-99 27-31 4.2-5.4 330-370 11-16 7-11.1 150-400 40-74 19-48 3-9 0-7 0-2
10^g/ L g/L L/L fl pg 10^1 2/L g/L fl fl 10^g/ L % % % % %
13.30 68 0.22 100.00 31.60 2.16 316 11.70 7.20 151.00 83.50 9.80 5.30 1.30 0.10
1/31/12
You might also like
- Dentist JurisprudenceDocument8 pagesDentist JurisprudenceSANDEEP100% (1)
- Tata Projects Offer Letter For Rayudu Sai Chandra Sekhar PDFDocument14 pagesTata Projects Offer Letter For Rayudu Sai Chandra Sekhar PDFAnonymous TX8oMMr280% (5)
- NURS FPX 6218 Assessment 1 Proposing Evidence-Based ChangeDocument6 pagesNURS FPX 6218 Assessment 1 Proposing Evidence-Based ChangeEmma WatsonNo ratings yet
- Nursing Upper Gi BleedingDocument23 pagesNursing Upper Gi BleedingLord Pozak Miller100% (3)
- Case Study - FractureDocument35 pagesCase Study - FractureJo-anne Cordero100% (4)
- Case Study On MalariaDocument18 pagesCase Study On MalariaBie WeNna100% (4)
- Gastroenteritis Care StudyDocument13 pagesGastroenteritis Care StudyÄxxö Ahkö Hinoguin50% (2)
- GAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolFrom EverandGAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolRating: 5 out of 5 stars5/5 (1)
- Case (Ovarian New Growth) (Gyne)Document5 pagesCase (Ovarian New Growth) (Gyne)Rona PieNo ratings yet
- Case Study On BurnsDocument16 pagesCase Study On BurnsRoanne Lagua100% (2)
- Pedia With LeukemiaDocument14 pagesPedia With LeukemiaAlynna ValbuenaNo ratings yet
- 52 Teen Boy Problems & How To Solve ThemDocument99 pages52 Teen Boy Problems & How To Solve ThemCristiano RochaNo ratings yet
- PT2012b PDFDocument59 pagesPT2012b PDFPhạm Thủy Cương100% (1)
- Comprehensive Nursing Care Plan: San Lazaro HospitalDocument37 pagesComprehensive Nursing Care Plan: San Lazaro HospitalKim AntonetteNo ratings yet
- 3rd Year Precept Pedia Case 4 HydroceleDocument4 pages3rd Year Precept Pedia Case 4 Hydrocelekristel_nicole18yaho100% (1)
- 28099453C Case Study 3Document27 pages28099453C Case Study 3Alice HuiiNo ratings yet
- 13 Areas DutyDocument3 pages13 Areas DutyAndrei MarcosNo ratings yet
- Client'S Profile: A. Demographic DataDocument11 pagesClient'S Profile: A. Demographic DataLincoln Cullen Tumulak SumayloNo ratings yet
- A Case Study of Hyperthermia Related To Infection As Evidenced by 38.9 C and Foul Smelling Post-Operative WoundDocument10 pagesA Case Study of Hyperthermia Related To Infection As Evidenced by 38.9 C and Foul Smelling Post-Operative WoundCleo Joyce C. CristalNo ratings yet
- Asuhan Keperawatan: Name: Ny. Sumini Age: Sex: Nationality: Company: Education:: Address: Date MRS: DiagnoseDocument5 pagesAsuhan Keperawatan: Name: Ny. Sumini Age: Sex: Nationality: Company: Education:: Address: Date MRS: DiagnosebennyarekakperNo ratings yet
- 13 AREAS of ASSESSMENTDocument2 pages13 AREAS of ASSESSMENTCrystal Queen MarquezNo ratings yet
- Cerebrovascular Disease (Bleed)Document25 pagesCerebrovascular Disease (Bleed)Margaret Jenaw JenawNo ratings yet
- Matt 2Document3 pagesMatt 2Matthew CalaraNo ratings yet
- Case Pres Cerebrovascular DiseaseDocument34 pagesCase Pres Cerebrovascular DiseaseADRIATICO JAROSLUVNo ratings yet
- Case Study 3Document27 pagesCase Study 3jazmae100% (2)
- Case StudyDocument57 pagesCase StudyJoy-Rena Sabinay OchondraNo ratings yet
- 13 Areas of Assessment I. Psychological StatusDocument3 pages13 Areas of Assessment I. Psychological StatusjoharaqohNo ratings yet
- Case Study Abdominal Blunt InjuryDocument10 pagesCase Study Abdominal Blunt InjuryHomework PingNo ratings yet
- Case Study On NSVDDocument50 pagesCase Study On NSVDNyj Quiño100% (2)
- 13 AREAS of ASSESSMENT (Geriatrict Ward)Document2 pages13 AREAS of ASSESSMENT (Geriatrict Ward)Crystal Queen Marquez100% (1)
- Ii. Chief ComplaintsDocument4 pagesIi. Chief ComplaintsArianne_Danglo_2118No ratings yet
- ADocument20 pagesADivinity Ü NicaNo ratings yet
- (Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)Document20 pages(Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)MikaCasimiroBalunanNo ratings yet
- Patient Health HistoryDocument8 pagesPatient Health HistoryRafi LabNo ratings yet
- HEALTH HISTORY WPS Office - Docx 1Document7 pagesHEALTH HISTORY WPS Office - Docx 1Cy PilapilNo ratings yet
- Case Presentation FinalDocument22 pagesCase Presentation Finalmafi0914No ratings yet
- Alyssa MaprideDocument2 pagesAlyssa MaprideMatthew CalaraNo ratings yet
- Case Study On Scarlet Fever12Document36 pagesCase Study On Scarlet Fever12Mark Sherwin LazoNo ratings yet
- Assessment and ClientDocument4 pagesAssessment and ClientEddie Lou GuzmanNo ratings yet
- CockDocument43 pagesCockAkuoko EricaNo ratings yet
- BPHDocument15 pagesBPH'mYk FavilaNo ratings yet
- FInal PowerpointDocument77 pagesFInal PowerpointJacky ChanNo ratings yet
- GoutDocument75 pagesGoutVan Talawec100% (2)
- Case English 1 - NDI Edit 220419Document24 pagesCase English 1 - NDI Edit 220419syongebobNo ratings yet
- AreasDocument2 pagesAreasKyre LandinginNo ratings yet
- April LeDocument21 pagesApril LeAprille Anne SagmitNo ratings yet
- Pattern Writing ExampleDocument14 pagesPattern Writing ExampleScribdTranslationsNo ratings yet
- Ent Case StudyDocument18 pagesEnt Case StudyKristian Karl Bautista Kiw-isNo ratings yet
- Case Study-Gastric CancerDocument19 pagesCase Study-Gastric Cancerbhelskie100% (2)
- Ob AssessmentDocument2 pagesOb AssessmentNathalie kate petallarNo ratings yet
- Final Case (Postpartum)Document14 pagesFinal Case (Postpartum)KimJohnSanchoManeroNo ratings yet
- A Case Study On Graves DiseaseDocument46 pagesA Case Study On Graves DiseaseRenie SerranoNo ratings yet
- A. Background of The StudyDocument14 pagesA. Background of The StudyronkathNo ratings yet
- Case Presentation: Group 9Document141 pagesCase Presentation: Group 9marialourdes2489No ratings yet
- Chronic Calculous CholecystitisDocument63 pagesChronic Calculous CholecystitisAYTONA, JAMAICA F.No ratings yet
- Learning Materials and Students WorksheetDocument5 pagesLearning Materials and Students WorksheetRatu Rini NurhayatiNo ratings yet
- Preterm Labor Case StudyDocument26 pagesPreterm Labor Case StudyKirk Espanol Bigstone82% (11)
- 13 Areas of AssessmentDocument2 pages13 Areas of AssessmentCrystal Queen MarquezNo ratings yet
- Hypokalemia Periodic ParalysisDocument14 pagesHypokalemia Periodic ParalysisJennirose JingNo ratings yet
- MattDocument3 pagesMattMatthew CalaraNo ratings yet
- NCP Heart FailureDocument11 pagesNCP Heart FailureaZhermAine100% (1)
- College of Nursing: Panpacific University North PhilippinesDocument20 pagesCollege of Nursing: Panpacific University North PhilippinesMar OrdanzaNo ratings yet
- Mindanao State University Iligan Institute of Technology College of Nursing Resource UnitDocument33 pagesMindanao State University Iligan Institute of Technology College of Nursing Resource UnitDanielle Faye ClerigoNo ratings yet
- Carpe Diem Ruiz Protcol Grand Rounds 4Document9 pagesCarpe Diem Ruiz Protcol Grand Rounds 4John Christopher RuizNo ratings yet
- Makita DUR369AZDocument160 pagesMakita DUR369AZAnonymous 4fOfUqNo ratings yet
- Bulletin of The United States Army MedicDocument3 pagesBulletin of The United States Army Medicbaladewa75No ratings yet
- Sandy-Hook SHAC Doc 2015.02.13 Draft Version of Final ReportDocument256 pagesSandy-Hook SHAC Doc 2015.02.13 Draft Version of Final ReportHelen BennettNo ratings yet
- "A Complete Health App": Designed by New HaircutDocument16 pages"A Complete Health App": Designed by New Haircutmonika sharmaNo ratings yet
- ABYIPDocument5 pagesABYIPJayson Guerrero100% (4)
- Pfizer Inc.: United States Securities and Exchange CommissionDocument246 pagesPfizer Inc.: United States Securities and Exchange CommissionDipanshu NagarNo ratings yet
- SDS Conductivity Standard 15 μScm MSDS USDocument6 pagesSDS Conductivity Standard 15 μScm MSDS USMd. Firozur RahmanNo ratings yet
- Psychology of Sport and Exercise: P. Wylleman, C.G. Harwood, A.-M. Elbe, A. Reints, D. de CaluweDocument12 pagesPsychology of Sport and Exercise: P. Wylleman, C.G. Harwood, A.-M. Elbe, A. Reints, D. de CaluweAraya ThimlamomNo ratings yet
- Sumber Data SIKDocument34 pagesSumber Data SIKandy azizNo ratings yet
- Wingila Mpamila Worksheet 8Document2 pagesWingila Mpamila Worksheet 8welcome martinNo ratings yet
- Candice Gorremans - Wellness Consultant ResumeDocument2 pagesCandice Gorremans - Wellness Consultant Resumeapi-289209614No ratings yet
- Pharmacology of Disopyramide: Yosephine A. H. 020100058Document20 pagesPharmacology of Disopyramide: Yosephine A. H. 020100058zulfantri1983No ratings yet
- Position Paper On Child PovertyDocument10 pagesPosition Paper On Child PovertyJr YansonNo ratings yet
- Peningkatan Dukungan Sosial Orang Tua Dengan Anak Skizofrenia Melalui Solution Focused TherapyDocument12 pagesPeningkatan Dukungan Sosial Orang Tua Dengan Anak Skizofrenia Melalui Solution Focused TherapyziraNo ratings yet
- PNS For MilkfishDocument11 pagesPNS For MilkfishJohn Christopher NolialNo ratings yet
- Time Blocking PDFDocument65 pagesTime Blocking PDFlynn_y95% (20)
- Universal Crescent Power P LTD EIA Report Part IDocument66 pagesUniversal Crescent Power P LTD EIA Report Part ImanishxlriNo ratings yet
- NUR 111 Session 22 SAS SemillaDocument2 pagesNUR 111 Session 22 SAS SemillaCyrille Jhane A GalvezNo ratings yet
- Research ProjectsDocument2 pagesResearch Projectsapi-143464694No ratings yet
- Vox Bikol Vol. 28 Issue No. 27Document8 pagesVox Bikol Vol. 28 Issue No. 27andyvgimpayaNo ratings yet
- Good Laboratory PracticesDocument5 pagesGood Laboratory PracticesRajendra ChaudharyNo ratings yet
- Mica Flake MSDSDocument2 pagesMica Flake MSDSMayank RajgarhiaNo ratings yet
- Sample WHS ManualDocument16 pagesSample WHS Manualzahidahmed42100% (1)
- CÁC BÀI ĐỌC ĐIỀN - SGK 12 (OLD)Document17 pagesCÁC BÀI ĐỌC ĐIỀN - SGK 12 (OLD)linhvu.youthplusNo ratings yet
- CorrosivesDocument25 pagesCorrosivesahmed.farag.ali2020No ratings yet