Professional Documents
Culture Documents
02 Immunization
02 Immunization
Uploaded by
Isha BhattCopyright:
Available Formats
You might also like
- ANA Recognized Terminologies and Data Element SetsDocument5 pagesANA Recognized Terminologies and Data Element SetsBlair WoodsenNo ratings yet
- Pediatric Rheumatology CarteDocument628 pagesPediatric Rheumatology CarteCrischentian BrinzaNo ratings yet
- VaccinesDocument39 pagesVaccinesritu9456No ratings yet
- ImmunizationDocument36 pagesImmunizationshahbaz100% (8)
- IMMUNIZATIONDocument5 pagesIMMUNIZATIONbaker samuelNo ratings yet
- Immunizatuon ChissDocument51 pagesImmunizatuon ChissMariam AntonyNo ratings yet
- IMMUNIZATIO1 LatestDocument30 pagesIMMUNIZATIO1 LatestAkshay H.No ratings yet
- Immunisation NotesDocument11 pagesImmunisation NotesCynthia WilsonNo ratings yet
- 099 - VaccinesDocument4 pages099 - VaccinesArjan LallNo ratings yet
- Rakib L3 VaccinesDocument23 pagesRakib L3 VaccinesSadia Afrin OshinNo ratings yet
- Vaccination 130Document8 pagesVaccination 130wajid aliNo ratings yet
- IMMUNIZATIONDocument35 pagesIMMUNIZATIONAkshay H.No ratings yet
- Immunization, Expanded Program On Immunization /universal Immunization Program ImmunizationDocument21 pagesImmunization, Expanded Program On Immunization /universal Immunization Program ImmunizationHUSSAINA BANONo ratings yet
- Immunisation: Lorem Ipsum DolorDocument60 pagesImmunisation: Lorem Ipsum DolorDr. Ajeta GuptaNo ratings yet
- Pediatrics Finaleeee-205-218Document14 pagesPediatrics Finaleeee-205-218ahmedNo ratings yet
- CHN Immunization NotesDocument9 pagesCHN Immunization NotesJustin AncogNo ratings yet
- ImmunizationDocument12 pagesImmunizationOke AdasenNo ratings yet
- Virology Lecture 6 ImmunityDocument14 pagesVirology Lecture 6 Immunityao868598No ratings yet
- Vaccines & Its Types: Ms Saajida Sultaana MahusookDocument16 pagesVaccines & Its Types: Ms Saajida Sultaana MahusookGayathri deviNo ratings yet
- Vaccination Chart: National Immunization Schedule For New BornDocument20 pagesVaccination Chart: National Immunization Schedule For New BornsmilealwplzNo ratings yet
- The Immune SystemDocument4 pagesThe Immune SystemSseguya Lubega YaqubNo ratings yet
- Converted 4Document61 pagesConverted 4miss peppa pigNo ratings yet
- 9-3-23 Immunity, Epi, Disease Control, Delivered Lec by DR Shumaila Humayun, 09-03-23Document65 pages9-3-23 Immunity, Epi, Disease Control, Delivered Lec by DR Shumaila Humayun, 09-03-23Dr Sarah Bakhsh - Resident FCPS Community MedicineNo ratings yet
- Vaccin OlogyDocument79 pagesVaccin Ologyhamzabinamjad987No ratings yet
- What Are VaccinesDocument9 pagesWhat Are VaccinesfaizanmuslimNo ratings yet
- Different Types of Vaccines: Preparation of Measles VaccineDocument8 pagesDifferent Types of Vaccines: Preparation of Measles VaccineEkta ManglaniNo ratings yet
- Active and Passive ImmunizationDocument11 pagesActive and Passive ImmunizationNgakanNo ratings yet
- l2.1 Immunization Cold ChainDocument53 pagesl2.1 Immunization Cold Chainsinuaish syaNo ratings yet
- l3 Immunization & Cold ChainDocument53 pagesl3 Immunization & Cold ChainNur AinaaNo ratings yet
- Anti-Viral ChemotherapyDocument39 pagesAnti-Viral Chemotherapyjolan.freedomNo ratings yet
- VACCINESDocument8 pagesVACCINESJoyNo ratings yet
- Practical Applications of Immunology Written ReportDocument9 pagesPractical Applications of Immunology Written ReportVincent Drystan AdronNo ratings yet
- Chap 16 Part 1Document4 pagesChap 16 Part 1clrssNo ratings yet
- VaccinesDocument8 pagesVaccinesRaul MuresanNo ratings yet
- Immunization Part 1Document12 pagesImmunization Part 1Marleen ShehadaNo ratings yet
- Vaccines - Definition, Principle, Types, Examples, Side EffectsDocument26 pagesVaccines - Definition, Principle, Types, Examples, Side Effectssattyadev95No ratings yet
- Imunisasi: Bambang MulyawanDocument60 pagesImunisasi: Bambang Mulyawanmentarimen19No ratings yet
- VaccineDocument16 pagesVaccineTharinish KGNo ratings yet
- BTE722 - 2aDocument65 pagesBTE722 - 2aRakesh bhukyaNo ratings yet
- Vaccines in Swine ProductionDocument22 pagesVaccines in Swine ProductionRemelyn Rodrigo100% (1)
- Vaccines: Properties of Ideal VaccineDocument5 pagesVaccines: Properties of Ideal VaccinelujihaneNo ratings yet
- Immunitization and VaccinationDocument46 pagesImmunitization and VaccinationMazhar RehmanNo ratings yet
- Immunization 2Document24 pagesImmunization 2TemiNo ratings yet
- ImmunisationDocument42 pagesImmunisationDr. Ajeta GuptaNo ratings yet
- Immunization DR T V RaoDocument68 pagesImmunization DR T V Raotummalapalli venkateswara rao100% (1)
- POC 304 Inflammation Fourth ClassDocument22 pagesPOC 304 Inflammation Fourth ClassPrecious EmmanuelNo ratings yet
- HBB 2306 Notes IIIDocument5 pagesHBB 2306 Notes IIIALEXNo ratings yet
- Imunisasi: Bambang MulyawanDocument72 pagesImunisasi: Bambang MulyawanAnonymous MxxkdtMt6uNo ratings yet
- Vaccination: Passive ImmunityDocument12 pagesVaccination: Passive ImmunityuouoNo ratings yet
- Bacterial VacciensDocument18 pagesBacterial VacciensSamNo ratings yet
- Immunological ProductsDocument35 pagesImmunological ProductsUMME SADEA RAHMANNo ratings yet
- Immunization 1Document30 pagesImmunization 1kundamargret69No ratings yet
- Prevention and TreatmentDocument7 pagesPrevention and TreatmentAlexander EnnesNo ratings yet
- 13 ImmunizationDocument18 pages13 ImmunizationMunazzaNo ratings yet
- Active Immunization Long DOCPDFDocument31 pagesActive Immunization Long DOCPDFEnder IzaguirreNo ratings yet
- Immunity and Immunization, Vaccines and Their Role in Prevention of DiseaseDocument14 pagesImmunity and Immunization, Vaccines and Their Role in Prevention of Diseaseshivani.priyaNo ratings yet
- CHAPTER 16 MicroparaDocument46 pagesCHAPTER 16 MicroparaKathlyn LopeñaNo ratings yet
- VACCINE123Document18 pagesVACCINE123Mudit MisraNo ratings yet
- Prof. Dr. Payman A.Hamaseed: VaccinationDocument19 pagesProf. Dr. Payman A.Hamaseed: Vaccinationasia groupNo ratings yet
- 5.14 Immunoprophylaxis ImmunotherapyDocument60 pages5.14 Immunoprophylaxis ImmunotherapyAlberto MayorgaNo ratings yet
- MODULE 2: Types of Vaccine and Adverse ReactionsDocument29 pagesMODULE 2: Types of Vaccine and Adverse ReactionsnandaNo ratings yet
- Vaccination: How Millions of Lives Have Been Saved - Perhaps YoursFrom EverandVaccination: How Millions of Lives Have Been Saved - Perhaps YoursNo ratings yet
- PBHL 625 Longitudinal Data Analysis - Fall 2014Document3 pagesPBHL 625 Longitudinal Data Analysis - Fall 2014Isha BhattNo ratings yet
- Sasrtf For LDADocument6 pagesSasrtf For LDAIsha BhattNo ratings yet
- Clostridium Difficile EpidemiologyDocument36 pagesClostridium Difficile EpidemiologyIsha BhattNo ratings yet
- Final Exam 2013 Sample Epidemiology of Infectious DiseasesDocument7 pagesFinal Exam 2013 Sample Epidemiology of Infectious DiseasesIsha Bhatt100% (1)
- Special Report: Solutions For Joint and Arthritic Pain: by Jon Benson Author, Fit Over 40Document21 pagesSpecial Report: Solutions For Joint and Arthritic Pain: by Jon Benson Author, Fit Over 40tobyNo ratings yet
- PSATDocument578 pagesPSATDubey Deepak100% (1)
- Hubungan Response Time Seksio Sesarea Emergensi Kategori 1 Dengan Luaran Perinatal Di Rsup Dr. SardjitoDocument12 pagesHubungan Response Time Seksio Sesarea Emergensi Kategori 1 Dengan Luaran Perinatal Di Rsup Dr. Sardjitoilham rangkutiNo ratings yet
- Evaluation of The Child Oral Health Promotion MaliMali' Programme Based On Schools in The Kingdom of TongaDocument9 pagesEvaluation of The Child Oral Health Promotion MaliMali' Programme Based On Schools in The Kingdom of TongaAishwarya AntalaNo ratings yet
- RC msn2Document204 pagesRC msn2Amit Pasi100% (1)
- LHOC Transition 02.21.24 Patient Letter V5Document1 pageLHOC Transition 02.21.24 Patient Letter V5Pat ThomasNo ratings yet
- DoHS Annual Report 2072 73 PDFDocument566 pagesDoHS Annual Report 2072 73 PDFSubash KarkiNo ratings yet
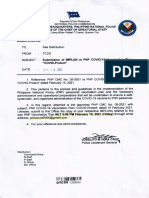
- CMC No. 05 2021 DTD Feb 15 2021Document13 pagesCMC No. 05 2021 DTD Feb 15 2021PSSg Junie Grebialde BotabaraNo ratings yet
- ¡Medicina1 2,000 Libros!1.2Document96 pages¡Medicina1 2,000 Libros!1.2jonathanguzman15No ratings yet
- HLTH 5465 3.0, Winter 2014: We Will Begin OurDocument12 pagesHLTH 5465 3.0, Winter 2014: We Will Begin Ourመሰረት ሀብቴNo ratings yet
- An Overview of Medical Acupuncture: Selected PaperDocument11 pagesAn Overview of Medical Acupuncture: Selected PaperHakim MacambiraNo ratings yet
- TATHLGP21248V022021Document16 pagesTATHLGP21248V022021vsharma0091No ratings yet
- NPI and Health TeachingDocument4 pagesNPI and Health TeachingJanelle Cabida SupnadNo ratings yet
- RecordingDocument36 pagesRecordingKripa SusanNo ratings yet
- KDOQI Clinical Practice Guideline Hemodialysis Update - Public Review Draft FINAL - 20150204 PDFDocument78 pagesKDOQI Clinical Practice Guideline Hemodialysis Update - Public Review Draft FINAL - 20150204 PDFศักดิ์ชัย พูนศรีเจริญกุลNo ratings yet
- Celiac Disease With Balanced TranslocationDocument3 pagesCeliac Disease With Balanced TranslocationAdvanced Research PublicationsNo ratings yet
- 2023 RestorativesDocument10 pages2023 Restorativesadel abdelmageedNo ratings yet
- The Budget Process-Cabilangan Crispin JayDocument3 pagesThe Budget Process-Cabilangan Crispin JayJerico ManaloNo ratings yet
- Rapid AdviceDocument44 pagesRapid AdviceJuhu NakaNo ratings yet
- Medical Diagnosis and Pathophysiology: (Be Sure To List Signs and Symptoms) - Please Indicate Your Source of InformationDocument3 pagesMedical Diagnosis and Pathophysiology: (Be Sure To List Signs and Symptoms) - Please Indicate Your Source of InformationKenneth Smith IINo ratings yet
- Jurnal HIVDocument9 pagesJurnal HIVRestu RahmanNo ratings yet
- H1N1 Influenza Vaccine Consent FormDocument1 pageH1N1 Influenza Vaccine Consent FormwigrenNo ratings yet
- Energy Medicine: The Scientific Basis - James L. Oschman PHDDocument6 pagesEnergy Medicine: The Scientific Basis - James L. Oschman PHDliryfuna50% (2)
- Case Study MM-2Document40 pagesCase Study MM-2Aya Sayed100% (1)
- Understanding Your Blood Tests For Blood CancerDocument9 pagesUnderstanding Your Blood Tests For Blood CancerSuhail KhanNo ratings yet
- Say Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541Document2 pagesSay Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541anon_734894635No ratings yet
- Gannan Medical UniversityDocument5 pagesGannan Medical Universityonepoint4No ratings yet
- Consent LcarnitineDocument2 pagesConsent LcarnitineZen AlkaffNo ratings yet
02 Immunization
02 Immunization
Uploaded by
Isha BhattOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
02 Immunization
02 Immunization
Uploaded by
Isha BhattCopyright:
Available Formats
Immunization Abdul Ghaffar (Phone: 733-3279; e-mail: ghaffar@med.sc.edu) MBIM 650/720 Medical Microbiology TEACHING OBJECTIVES: 1. 2. 3. 4. 5.
READING: Roitt, Brostoff and Male: Immunology. 6th ed., chapter 17 Know the distinction between passive and active immunization and their examples Distinguish between artificial and natural means of immunization Know the applications and problems of artificial passive immunization Know the applications and problems of artificial active immunization Know the modern approaches to immunization Lecture: 14
Immunization is the means of providing specific protection against most common and damaging pathogens. Specific immunity can be acquired either by passive or by active immunization and both modes of immunization can occur by natural or artificial means (Figure 1). Passive Immunity: Immunity can be acquired, without the immune system being challenged with an antigen, by transfer of serum or gamma globulins from an immune donor to a non immune individual. Alternatively, immune cells from an immunized individual may be used to transfer immunity. Passive immunity may be acquired naturally or artificially. Naturally acquired passive immunity: Immunity is transferred from mother to fetus through placental transfer of IgG or colostral transfer of IgA.
Immunity
Innate
Acquired
Artificially acquired passive immunity: Immunity is often artificially transferred by Active Passive injection with gamma globulins from other individuals or gamma globulin from an immune animal. Passive transfer of immunity with immune Artificial Natural Artificial Natural globulins or gamma globulins is practiced in numerous acute situations of infections (diphtheria, tetanus, measles, rabies, etc.), poisoning (insects, Figure 1. Different modes of acquiring of immunity reptiles, botulism), and as a prophylactic measure (hypogammaglobulinemia). In these situations, gamma globulins of human origin are preferable although specific antibodies raised in other species are effective and used in some cases (poisoning, diphtheria, tetanus, gas gangrene, botulism). While this form of immunization has the advantage of providing immediate protection, heterologous gamma globulins are effective for only a short duration and often result in pathological complications (serum sickness) and anaphylaxis. Homologous immunoglobulins carry the risk of transmitting hepatitis and HIV.
Passive transfer of cell-mediated immunity can also be accomplished in certain diseases (cancer, immunodeficiency). However, it is difficult to find histocompatible (matched) donors and there is severe risk of graft versus host disease.
1
Active Immunity: This refers to immunity produced by the body following exposure to antigens. Naturally acquired active immunity: Exposure to different pathogens leads to sub clinical or clinical infections, which result in a protective immune response against these pathogens. Artificially acquired active immunity: Immunization may be achieved by administering live or dead pathogens or their components. Vaccines used for active immunization consist of live (attenuated) organism, killed whole organism, microbial components or secreted toxins (detoxified). Live vaccines: Live organisms are used for immunization against a number of viral infections. Live vaccines for measles, mumps, rubella and chicken pox (varicella) are routinely used in this country. A live bacterial vaccine consisting of a strain of Mycobacterium bovis, Bacillus Calmet Geurin (BCG) is used against tuberculosis in many European and Asian countries. However, it is not used in this country. While many studies have shown the efficacy of this vaccine, a number of studies have cast doubt on its benefits. Live vaccines normally produce self-limiting non-clinical infections and lead to subsequent immunity, both humoral and cell-mediated, the latter being essential for intracellular pathogens. However, they carry a serious risk of causing overt disease in immunocompromised individuals. Furthermore, since live vaccines are often attenuated (made less pathogenic) by passage in animal, they can revert to their pathogenic form and cause serious illness. It is for this reason, polio live (Sabin) vaccine, which was used for many years, has been replaced by the inactivated (Salk) vaccine. Killed vaccines: These consist of whole organisms inactivated by heat, chemicals or UV irradiation treatment. Many killed viral and bacterial vaccines are available. Some of these are used to immunize people at risks (e.g. influenza, hepatitis A, etc.) while others are used to immunize travelers to different countries (e.g. yellow fever, cholera, typhoid etc.). Pertussis (whooping cough) whole bacterial vaccine was used routinely until a few years ago, but due to it serious side effect, it has been replaced by a formulation of acellular components. Sub-unit vaccines: Some vaccines consist of subcomponents of the pathogenic organisms, usually proteins or polysaccharides. Since polysaccharides are relatively weak T-independent antigens, and produce only IgM responses without immunologic memory, they are made more immunogenic and T-dependent by conjugation with proteins (e.g., haemophilus, pertussis, meningococcus, pneumococcus, etc.). Hepatitis-B, rabies vaccines consist of antigenic proteins cloned into a suitable vector (e.g., yeast). These subunit vaccines are designed to reduce the problems of toxicity and risk of infection. When the pathogenic mechanism of an agent involves a toxin, a modified form of the toxin (toxoid) is used as vaccine (e.g., diphtheria, tetanus, cholera). Toxoid, while remains immunogenic, loses its toxicity. Other novel vaccines: A number of novel approaches to active immunization are in the investigative stage and are used only experimentally. These include anti-idiotype antibodies, DNA vaccines and immunodominant peptides (recognized by the MHC molecules) and may be available in the future. Anti-idiotype antibodies against polysaccharide antibody produce long lasting immune responses with immunologic memory. Viral genes cloned into vectors, when injected transfect host cells and consequently produce a response similar to that produced against live-attenuated viruses (both cell-mediated and humoral). Immunodominant peptides are simple and easy to prepare and can provoke both humoral and cell mediated responses. Adjuvants: Weaker antigens may be rendered more immunogenic by the addition of other chemicals. Such chemicals are known as adjuvants. There are many biological and chemical substances that have been used in experimental conditions. However, only Aluminum salts (alum) are approved for clinical human use and it is incorporated in DTP vaccine. Adjuvants used experimentally include mixtures of oil and detergents, with or without certain bacteria, most often BCG, or their components. Newer adjuvant formulations include synthetic polymers. Adjuvants normally function by either creating an antigen depot and/or by stimulating mononuclear phagocytes.
The protective immunity conferred by a vaccine may be life-long (measles, mumps, rubella, small pox, tuberculosis, yellow fever, etc.) or may last as little as a few months (cholera). The primary immunization may be given at the age of 2-3 months (diphtheria, pertussis, tetanus, polio), or 13-15 months (mumps, measles, rubella). The currently recommended schedule of routine immunization (recommended by CDC and AIP; reproduced from MMWR, volume 5102, 2002) is summarized in Figure 2. A number of other vaccines are licensed for use in the US and are recommended for travelers or groups at risk.
Figure 2. Schedule for Routine Active Immunization of Normal Children Adverse effects of immunization: Active immunization may cause fever, malaise and discomfort. Some vaccine may also cause joint pains or arthritis (rubella), convulsions, sometimes fatal (pertussis), or neurological disorders (influenza). Allergies to egg may develop as a consequence of viral vaccines produced in egg (measles, mumps, influenza, yellow fever). Booster shots result in more pronounced inflammatory effects than the primary immunization. The noticeable and serious side effects documented have been those following the DTP vaccine (Table 2). Most of these were attributable to the whole pertussis component of the vaccine and have been eliminated since the use of the acellular pertussis preparation.
Table 2. Approximate rates of adverse event occurring within 48 hours DTP vaccination Event Local: redness, swelling, pain Mild/moderate systemic: fever, drowsiness, fretfulness vomiting, anorexia More serious systemic: persistent crying, fever collapse, convulsions acute encephalopathy permanent neurological deficit 1 in 2-3 doses 1 in 2-3 doses 1 in 5-15 doses 1 in 100-300 doses 1 in 1750 doses 1 in 100,000 doses 1 in 300,000 doses Frequency
You have learned:
Different modes of acquiring immunity You know which mode is used or applicable in what situation Advantages and disadvantages of different modes of immunization Rationale for vaccine design Risk and benefits of vaccination
You might also like
- ANA Recognized Terminologies and Data Element SetsDocument5 pagesANA Recognized Terminologies and Data Element SetsBlair WoodsenNo ratings yet
- Pediatric Rheumatology CarteDocument628 pagesPediatric Rheumatology CarteCrischentian BrinzaNo ratings yet
- VaccinesDocument39 pagesVaccinesritu9456No ratings yet
- ImmunizationDocument36 pagesImmunizationshahbaz100% (8)
- IMMUNIZATIONDocument5 pagesIMMUNIZATIONbaker samuelNo ratings yet
- Immunizatuon ChissDocument51 pagesImmunizatuon ChissMariam AntonyNo ratings yet
- IMMUNIZATIO1 LatestDocument30 pagesIMMUNIZATIO1 LatestAkshay H.No ratings yet
- Immunisation NotesDocument11 pagesImmunisation NotesCynthia WilsonNo ratings yet
- 099 - VaccinesDocument4 pages099 - VaccinesArjan LallNo ratings yet
- Rakib L3 VaccinesDocument23 pagesRakib L3 VaccinesSadia Afrin OshinNo ratings yet
- Vaccination 130Document8 pagesVaccination 130wajid aliNo ratings yet
- IMMUNIZATIONDocument35 pagesIMMUNIZATIONAkshay H.No ratings yet
- Immunization, Expanded Program On Immunization /universal Immunization Program ImmunizationDocument21 pagesImmunization, Expanded Program On Immunization /universal Immunization Program ImmunizationHUSSAINA BANONo ratings yet
- Immunisation: Lorem Ipsum DolorDocument60 pagesImmunisation: Lorem Ipsum DolorDr. Ajeta GuptaNo ratings yet
- Pediatrics Finaleeee-205-218Document14 pagesPediatrics Finaleeee-205-218ahmedNo ratings yet
- CHN Immunization NotesDocument9 pagesCHN Immunization NotesJustin AncogNo ratings yet
- ImmunizationDocument12 pagesImmunizationOke AdasenNo ratings yet
- Virology Lecture 6 ImmunityDocument14 pagesVirology Lecture 6 Immunityao868598No ratings yet
- Vaccines & Its Types: Ms Saajida Sultaana MahusookDocument16 pagesVaccines & Its Types: Ms Saajida Sultaana MahusookGayathri deviNo ratings yet
- Vaccination Chart: National Immunization Schedule For New BornDocument20 pagesVaccination Chart: National Immunization Schedule For New BornsmilealwplzNo ratings yet
- The Immune SystemDocument4 pagesThe Immune SystemSseguya Lubega YaqubNo ratings yet
- Converted 4Document61 pagesConverted 4miss peppa pigNo ratings yet
- 9-3-23 Immunity, Epi, Disease Control, Delivered Lec by DR Shumaila Humayun, 09-03-23Document65 pages9-3-23 Immunity, Epi, Disease Control, Delivered Lec by DR Shumaila Humayun, 09-03-23Dr Sarah Bakhsh - Resident FCPS Community MedicineNo ratings yet
- Vaccin OlogyDocument79 pagesVaccin Ologyhamzabinamjad987No ratings yet
- What Are VaccinesDocument9 pagesWhat Are VaccinesfaizanmuslimNo ratings yet
- Different Types of Vaccines: Preparation of Measles VaccineDocument8 pagesDifferent Types of Vaccines: Preparation of Measles VaccineEkta ManglaniNo ratings yet
- Active and Passive ImmunizationDocument11 pagesActive and Passive ImmunizationNgakanNo ratings yet
- l2.1 Immunization Cold ChainDocument53 pagesl2.1 Immunization Cold Chainsinuaish syaNo ratings yet
- l3 Immunization & Cold ChainDocument53 pagesl3 Immunization & Cold ChainNur AinaaNo ratings yet
- Anti-Viral ChemotherapyDocument39 pagesAnti-Viral Chemotherapyjolan.freedomNo ratings yet
- VACCINESDocument8 pagesVACCINESJoyNo ratings yet
- Practical Applications of Immunology Written ReportDocument9 pagesPractical Applications of Immunology Written ReportVincent Drystan AdronNo ratings yet
- Chap 16 Part 1Document4 pagesChap 16 Part 1clrssNo ratings yet
- VaccinesDocument8 pagesVaccinesRaul MuresanNo ratings yet
- Immunization Part 1Document12 pagesImmunization Part 1Marleen ShehadaNo ratings yet
- Vaccines - Definition, Principle, Types, Examples, Side EffectsDocument26 pagesVaccines - Definition, Principle, Types, Examples, Side Effectssattyadev95No ratings yet
- Imunisasi: Bambang MulyawanDocument60 pagesImunisasi: Bambang Mulyawanmentarimen19No ratings yet
- VaccineDocument16 pagesVaccineTharinish KGNo ratings yet
- BTE722 - 2aDocument65 pagesBTE722 - 2aRakesh bhukyaNo ratings yet
- Vaccines in Swine ProductionDocument22 pagesVaccines in Swine ProductionRemelyn Rodrigo100% (1)
- Vaccines: Properties of Ideal VaccineDocument5 pagesVaccines: Properties of Ideal VaccinelujihaneNo ratings yet
- Immunitization and VaccinationDocument46 pagesImmunitization and VaccinationMazhar RehmanNo ratings yet
- Immunization 2Document24 pagesImmunization 2TemiNo ratings yet
- ImmunisationDocument42 pagesImmunisationDr. Ajeta GuptaNo ratings yet
- Immunization DR T V RaoDocument68 pagesImmunization DR T V Raotummalapalli venkateswara rao100% (1)
- POC 304 Inflammation Fourth ClassDocument22 pagesPOC 304 Inflammation Fourth ClassPrecious EmmanuelNo ratings yet
- HBB 2306 Notes IIIDocument5 pagesHBB 2306 Notes IIIALEXNo ratings yet
- Imunisasi: Bambang MulyawanDocument72 pagesImunisasi: Bambang MulyawanAnonymous MxxkdtMt6uNo ratings yet
- Vaccination: Passive ImmunityDocument12 pagesVaccination: Passive ImmunityuouoNo ratings yet
- Bacterial VacciensDocument18 pagesBacterial VacciensSamNo ratings yet
- Immunological ProductsDocument35 pagesImmunological ProductsUMME SADEA RAHMANNo ratings yet
- Immunization 1Document30 pagesImmunization 1kundamargret69No ratings yet
- Prevention and TreatmentDocument7 pagesPrevention and TreatmentAlexander EnnesNo ratings yet
- 13 ImmunizationDocument18 pages13 ImmunizationMunazzaNo ratings yet
- Active Immunization Long DOCPDFDocument31 pagesActive Immunization Long DOCPDFEnder IzaguirreNo ratings yet
- Immunity and Immunization, Vaccines and Their Role in Prevention of DiseaseDocument14 pagesImmunity and Immunization, Vaccines and Their Role in Prevention of Diseaseshivani.priyaNo ratings yet
- CHAPTER 16 MicroparaDocument46 pagesCHAPTER 16 MicroparaKathlyn LopeñaNo ratings yet
- VACCINE123Document18 pagesVACCINE123Mudit MisraNo ratings yet
- Prof. Dr. Payman A.Hamaseed: VaccinationDocument19 pagesProf. Dr. Payman A.Hamaseed: Vaccinationasia groupNo ratings yet
- 5.14 Immunoprophylaxis ImmunotherapyDocument60 pages5.14 Immunoprophylaxis ImmunotherapyAlberto MayorgaNo ratings yet
- MODULE 2: Types of Vaccine and Adverse ReactionsDocument29 pagesMODULE 2: Types of Vaccine and Adverse ReactionsnandaNo ratings yet
- Vaccination: How Millions of Lives Have Been Saved - Perhaps YoursFrom EverandVaccination: How Millions of Lives Have Been Saved - Perhaps YoursNo ratings yet
- PBHL 625 Longitudinal Data Analysis - Fall 2014Document3 pagesPBHL 625 Longitudinal Data Analysis - Fall 2014Isha BhattNo ratings yet
- Sasrtf For LDADocument6 pagesSasrtf For LDAIsha BhattNo ratings yet
- Clostridium Difficile EpidemiologyDocument36 pagesClostridium Difficile EpidemiologyIsha BhattNo ratings yet
- Final Exam 2013 Sample Epidemiology of Infectious DiseasesDocument7 pagesFinal Exam 2013 Sample Epidemiology of Infectious DiseasesIsha Bhatt100% (1)
- Special Report: Solutions For Joint and Arthritic Pain: by Jon Benson Author, Fit Over 40Document21 pagesSpecial Report: Solutions For Joint and Arthritic Pain: by Jon Benson Author, Fit Over 40tobyNo ratings yet
- PSATDocument578 pagesPSATDubey Deepak100% (1)
- Hubungan Response Time Seksio Sesarea Emergensi Kategori 1 Dengan Luaran Perinatal Di Rsup Dr. SardjitoDocument12 pagesHubungan Response Time Seksio Sesarea Emergensi Kategori 1 Dengan Luaran Perinatal Di Rsup Dr. Sardjitoilham rangkutiNo ratings yet
- Evaluation of The Child Oral Health Promotion MaliMali' Programme Based On Schools in The Kingdom of TongaDocument9 pagesEvaluation of The Child Oral Health Promotion MaliMali' Programme Based On Schools in The Kingdom of TongaAishwarya AntalaNo ratings yet
- RC msn2Document204 pagesRC msn2Amit Pasi100% (1)
- LHOC Transition 02.21.24 Patient Letter V5Document1 pageLHOC Transition 02.21.24 Patient Letter V5Pat ThomasNo ratings yet
- DoHS Annual Report 2072 73 PDFDocument566 pagesDoHS Annual Report 2072 73 PDFSubash KarkiNo ratings yet
- CMC No. 05 2021 DTD Feb 15 2021Document13 pagesCMC No. 05 2021 DTD Feb 15 2021PSSg Junie Grebialde BotabaraNo ratings yet
- ¡Medicina1 2,000 Libros!1.2Document96 pages¡Medicina1 2,000 Libros!1.2jonathanguzman15No ratings yet
- HLTH 5465 3.0, Winter 2014: We Will Begin OurDocument12 pagesHLTH 5465 3.0, Winter 2014: We Will Begin Ourመሰረት ሀብቴNo ratings yet
- An Overview of Medical Acupuncture: Selected PaperDocument11 pagesAn Overview of Medical Acupuncture: Selected PaperHakim MacambiraNo ratings yet
- TATHLGP21248V022021Document16 pagesTATHLGP21248V022021vsharma0091No ratings yet
- NPI and Health TeachingDocument4 pagesNPI and Health TeachingJanelle Cabida SupnadNo ratings yet
- RecordingDocument36 pagesRecordingKripa SusanNo ratings yet
- KDOQI Clinical Practice Guideline Hemodialysis Update - Public Review Draft FINAL - 20150204 PDFDocument78 pagesKDOQI Clinical Practice Guideline Hemodialysis Update - Public Review Draft FINAL - 20150204 PDFศักดิ์ชัย พูนศรีเจริญกุลNo ratings yet
- Celiac Disease With Balanced TranslocationDocument3 pagesCeliac Disease With Balanced TranslocationAdvanced Research PublicationsNo ratings yet
- 2023 RestorativesDocument10 pages2023 Restorativesadel abdelmageedNo ratings yet
- The Budget Process-Cabilangan Crispin JayDocument3 pagesThe Budget Process-Cabilangan Crispin JayJerico ManaloNo ratings yet
- Rapid AdviceDocument44 pagesRapid AdviceJuhu NakaNo ratings yet
- Medical Diagnosis and Pathophysiology: (Be Sure To List Signs and Symptoms) - Please Indicate Your Source of InformationDocument3 pagesMedical Diagnosis and Pathophysiology: (Be Sure To List Signs and Symptoms) - Please Indicate Your Source of InformationKenneth Smith IINo ratings yet
- Jurnal HIVDocument9 pagesJurnal HIVRestu RahmanNo ratings yet
- H1N1 Influenza Vaccine Consent FormDocument1 pageH1N1 Influenza Vaccine Consent FormwigrenNo ratings yet
- Energy Medicine: The Scientific Basis - James L. Oschman PHDDocument6 pagesEnergy Medicine: The Scientific Basis - James L. Oschman PHDliryfuna50% (2)
- Case Study MM-2Document40 pagesCase Study MM-2Aya Sayed100% (1)
- Understanding Your Blood Tests For Blood CancerDocument9 pagesUnderstanding Your Blood Tests For Blood CancerSuhail KhanNo ratings yet
- Say Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541Document2 pagesSay Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541anon_734894635No ratings yet
- Gannan Medical UniversityDocument5 pagesGannan Medical Universityonepoint4No ratings yet
- Consent LcarnitineDocument2 pagesConsent LcarnitineZen AlkaffNo ratings yet