Professional Documents
Culture Documents
Vitiligo The White Leprosy
Vitiligo The White Leprosy
Uploaded by
9730218936Copyright:
Available Formats
You might also like
- Vitiligo and Leukoderma in Children: Maria Isabel Herane, MDDocument13 pagesVitiligo and Leukoderma in Children: Maria Isabel Herane, MDBimo Aryo TejoNo ratings yet
- Melasma Insights and PerspectivesDocument6 pagesMelasma Insights and PerspectivesTatianaNo ratings yet
- Vitiligo: Refer ATDocument18 pagesVitiligo: Refer ATAndhika FrabesNo ratings yet
- Artikel Kelainan Kulit - Vitiligo DLLDocument13 pagesArtikel Kelainan Kulit - Vitiligo DLLRosa SeptianaNo ratings yet
- Skin Pigmentation + Hari DisorderDocument113 pagesSkin Pigmentation + Hari DisorderAfiqah So JasmiNo ratings yet
- Laporan Kasus Aiman KamilaDocument16 pagesLaporan Kasus Aiman KamilazzooooeeeeeeNo ratings yet
- An Overview On Melasma 2376 0427 1000216Document18 pagesAn Overview On Melasma 2376 0427 1000216dhilaidrisNo ratings yet
- A Review On Common Dermatologic ConditionsDocument8 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- A Review On Common Dermatologic ConditionsDocument10 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- Acquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateDocument53 pagesAcquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateBaoz PingNo ratings yet
- Skin PDFDocument3 pagesSkin PDFPerry SinNo ratings yet
- MelasmDocument22 pagesMelasmLeonardo Alves F AlmeidaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014machiiNo ratings yet
- A Review On Common Dermatologic ConditionsDocument16 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- Vitiligo: An Update: Published: 17 January 2011Document21 pagesVitiligo: An Update: Published: 17 January 2011Narayanan RajendranNo ratings yet
- TranslateDocument67 pagesTranslatesriwahyuniNo ratings yet
- 32Document21 pages32gamhaelNo ratings yet
- Liken Planus & Lichen Sclerosus Et Atropichus, Granuloma AnulareDocument29 pagesLiken Planus & Lichen Sclerosus Et Atropichus, Granuloma AnulareroserosannaNo ratings yet
- Kuliahskin Pigmentation + Hair Disorder-Power Pointedit-2 - 26april11Document113 pagesKuliahskin Pigmentation + Hair Disorder-Power Pointedit-2 - 26april11Andersen ChenNo ratings yet
- The Lichens in Vulvovaginal Disease 2015Document20 pagesThe Lichens in Vulvovaginal Disease 2015Vidini Kusuma AjiNo ratings yet
- Amyloidosis SkinDocument6 pagesAmyloidosis SkinGoran MaliNo ratings yet
- Stevens Johnson Syndrome CASEDocument53 pagesStevens Johnson Syndrome CASEKathrina CraveNo ratings yet
- Manila Central UniversityDocument5 pagesManila Central UniversityRajan ChaudharyNo ratings yet
- Tratment Melasma PDFDocument18 pagesTratment Melasma PDFGheavita Chandra DewiNo ratings yet
- SGD Ein 2 Kelompok 5Document27 pagesSGD Ein 2 Kelompok 5Rahmadanti Nur FadillaNo ratings yet
- Meds CapeDocument14 pagesMeds CapeMeta SakinaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014Erlangga DayudNo ratings yet
- Pityrosporum FolliculitisDocument3 pagesPityrosporum Folliculitisshivam18No ratings yet
- LentigoDocument15 pagesLentigoaditya ratna utariNo ratings yet
- Cytokine: E.S. Robinson, V.P. WerthDocument9 pagesCytokine: E.S. Robinson, V.P. WerthArthurAkkNo ratings yet
- Stevens-Johnson Syndrome CASEDocument38 pagesStevens-Johnson Syndrome CASEChristy Rose AgrisNo ratings yet
- Melasma and Post Inflammatory Hyperpigmentation Management Update and Expert OpinionDocument19 pagesMelasma and Post Inflammatory Hyperpigmentation Management Update and Expert OpinionLutfi MKNo ratings yet
- Cutaneous amylo-WPS OfficeDocument6 pagesCutaneous amylo-WPS Officesveeram3No ratings yet
- Skin PigmentatDocument110 pagesSkin Pigmentatsteven saputra0% (1)
- PigmentationDocument28 pagesPigmentationCabdiladif Ahmed McrfNo ratings yet
- Jadotte Pityriasis AlbaDocument8 pagesJadotte Pityriasis Albapene asoyNo ratings yet
- Jurnal Keperluan PentingDocument4 pagesJurnal Keperluan PentingmhdtaufikkNo ratings yet
- Urticaria and AngioedemaDocument40 pagesUrticaria and AngioedemaDea LeeteukNo ratings yet
- The Evolution of Biochemical Indices After Basal Cell Epithelioma Removal - Case ReportDocument6 pagesThe Evolution of Biochemical Indices After Basal Cell Epithelioma Removal - Case ReportGurgas LeonardNo ratings yet
- DERMATOLOGY Notes From Uworld, DR-KYDocument22 pagesDERMATOLOGY Notes From Uworld, DR-KYLayan Mohammad100% (1)
- Toxic Responses of The SkinDocument25 pagesToxic Responses of The SkinfianceeleeNo ratings yet
- Exfoliative DermatitisDocument7 pagesExfoliative DermatitisRidyah Ning TyasNo ratings yet
- Lupus ErythematosusDocument3 pagesLupus ErythematosusAMOS MELINo ratings yet
- 157-Article Text-621-1-10-20120514Document7 pages157-Article Text-621-1-10-20120514loNo ratings yet
- UWorld Notes - Mark ChaskesDocument36 pagesUWorld Notes - Mark Chaskesise7No ratings yet
- Ghafourian Et Al 2014 Vitiligo Symptoms Pathogenesis and TreatmentDocument5 pagesGhafourian Et Al 2014 Vitiligo Symptoms Pathogenesis and Treatmentnramrattan475No ratings yet
- Vitiligo 1-09-220vitiligoDocument11 pagesVitiligo 1-09-220vitiligomulyadiansyahNo ratings yet
- Natural Options For Management of MelasmaDocument17 pagesNatural Options For Management of Melasmapuji lestari100% (1)
- Health and Wellness Integumentary System: by DR M Umer IqbalDocument25 pagesHealth and Wellness Integumentary System: by DR M Umer IqbalShimmering MoonNo ratings yet
- A HoyDocument17 pagesA HoyMadelaine MoncayoNo ratings yet
- Dermatomyositis Case7Document15 pagesDermatomyositis Case7Hanina Macataman MetmugNo ratings yet
- Alopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DDocument7 pagesAlopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DSistaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014cjristinNo ratings yet
- Melasma: An Up-to-Date Comprehensive Review: Oluwatobi A. Ogbechie-Godec Nada ElbulukDocument14 pagesMelasma: An Up-to-Date Comprehensive Review: Oluwatobi A. Ogbechie-Godec Nada ElbulukDra Natalia Maria ZuluagaNo ratings yet
- Leishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Comprehensive Insights into Acute Cutaneous Lupus: Unraveling Pathways, Implications, and InterventionsFrom EverandComprehensive Insights into Acute Cutaneous Lupus: Unraveling Pathways, Implications, and InterventionsNo ratings yet
- Surviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsFrom EverandSurviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsNo ratings yet
- Understanding Skin Problems: Acne, Eczema, Psoriasis and Related ConditionsFrom EverandUnderstanding Skin Problems: Acne, Eczema, Psoriasis and Related ConditionsNo ratings yet
- Steroids PDFDocument35 pagesSteroids PDFPratyusha VallamNo ratings yet
- JURDING (Corticosteroids Therapy in Combination With Antibiotics For Erysipelas)Document21 pagesJURDING (Corticosteroids Therapy in Combination With Antibiotics For Erysipelas)Alif Putri YustikaNo ratings yet
- What Are The Therapeutic Classes of DrugsDocument3 pagesWhat Are The Therapeutic Classes of DrugsFrank GomesNo ratings yet
- Clobetasol CreamDocument9 pagesClobetasol CreamGiulianospharmacyNo ratings yet
- Chapter 37: Drugs Used To Treat Thyroid DiseaseDocument40 pagesChapter 37: Drugs Used To Treat Thyroid DiseaseAziil LiizaNo ratings yet
- ACE Group Guidelines SARS CoV 2Document6 pagesACE Group Guidelines SARS CoV 2Dr. Hilder HernandezNo ratings yet
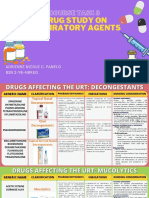
- Course Task 8 Drug Study On Respiratory AgentsDocument23 pagesCourse Task 8 Drug Study On Respiratory AgentsAdrienne Nicole PaneloNo ratings yet
- Adrenocorticosteroids & Adrenocortical AntagonistsDocument20 pagesAdrenocorticosteroids & Adrenocortical Antagonistsapi-3859918No ratings yet
- Traumatic Optic NeuropathyDocument5 pagesTraumatic Optic NeuropathyMiftahurrahmah GmsNo ratings yet
- Pharmacologic: Systemic Administration AssessmentDocument3 pagesPharmacologic: Systemic Administration Assessmentitsmeaya100% (1)
- Management of Acute Respiratory Diseases PDFDocument21 pagesManagement of Acute Respiratory Diseases PDFFernandoXavierNo ratings yet
- Necrobiosis Lipoidica Dia..-GhjuytDocument7 pagesNecrobiosis Lipoidica Dia..-GhjuytAshesForTearsNo ratings yet
- Clinical Pharmacy Questions and AnswersDocument8 pagesClinical Pharmacy Questions and AnswersMelavNo ratings yet
- CIRCI Guidelines 2015Document6 pagesCIRCI Guidelines 2015Wissam SleimanNo ratings yet
- SNAP Comparison of Topical SteroidsDocument12 pagesSNAP Comparison of Topical SteroidsRany100% (1)
- Deflazacort - GluticordDocument25 pagesDeflazacort - GluticordChintan ChavdaNo ratings yet
- Mometasone FuroatDocument8 pagesMometasone FuroatAnonymous ZrLxxRUr9zNo ratings yet
- Pharmacology For The Interventional Pain Physician: Magdalena Anitescu Honorio T. Benzon Renata VariakojisDocument1 pagePharmacology For The Interventional Pain Physician: Magdalena Anitescu Honorio T. Benzon Renata VariakojisFaith Acu CureNo ratings yet
- DS Norepinephrine HydrocortisoneDocument4 pagesDS Norepinephrine HydrocortisoneReign RaineNo ratings yet
- Fucicort CreamDocument4 pagesFucicort Creamcupcake xNo ratings yet
- Beclomethasone DipropionateDocument3 pagesBeclomethasone Dipropionateapi-3797941No ratings yet
- Pharmacology NotebookDocument31 pagesPharmacology Notebookapi-284057899No ratings yet
- Steroid Injection Costs. Cheap Anabolic Steroids #Rjhy8NurDocument2 pagesSteroid Injection Costs. Cheap Anabolic Steroids #Rjhy8NurMarielaNo ratings yet
- Clobetasol Anuth8ngDocument7 pagesClobetasol Anuth8ngWhiel Kurt Arzaga SaragconNo ratings yet
- FENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialDocument23 pagesFENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialYadvir GargNo ratings yet
- лекц10Document41 pagesлекц10A A D H INo ratings yet
- Conference Reports and Expert Panel: DOI 10.1007/s00134-017-4919-5Document13 pagesConference Reports and Expert Panel: DOI 10.1007/s00134-017-4919-5Mari ArcenganNo ratings yet
- Farmakologi Obat Pada Reaksi HipersensitivitasDocument59 pagesFarmakologi Obat Pada Reaksi HipersensitivitasTitip Elia GustamiNo ratings yet
- A Seminar On Adrenal Cortex Hormones: Presented By: Jignesh Patel 1 Year M. Pharm A.B.M.R.C.P Banglore-90Document14 pagesA Seminar On Adrenal Cortex Hormones: Presented By: Jignesh Patel 1 Year M. Pharm A.B.M.R.C.P Banglore-90Amit GhoshNo ratings yet
- 2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDDocument58 pages2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDKishan SethNo ratings yet
Vitiligo The White Leprosy
Vitiligo The White Leprosy
Uploaded by
9730218936Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vitiligo The White Leprosy
Vitiligo The White Leprosy
Uploaded by
9730218936Copyright:
Available Formats
VITILIGO THE WHITE LEPROSY
Introduction The skin is the largest and most visible organ of the human body. Hence any blemish on the skin visibly affects the onlooker and thus the person affected profoundly. A healthy normal skin is essential for a person's physical and mental well being. It is an important aspect of their sexual attractiveness,a sense of well being and a sense of self confidence. Variations in the color of human skin are because of pigment called melanin, which is produced by special types of cells known as melanocytes. The intensity of pigmentation may vary in human skin because of numerous reasons like race, environmental condition and disease. Any change in the pigmental level of the skin always generates concern, because it can have serious health as well as cosmetic implications. An increase in the pigmental level of skin known as hyperpigmentation can result from excessive tanning, pregnancy, addissons disease and hyperpigmentation of sacrs. A lack or loss of pigment known as hypopigmentation can result from albinism, vitiligo, leprosy, hypopigmented scars and many other. Of all the acquired hypopigmentary disorders vitiligo is probably the most common. Vitiligo is an acquired depigmentation disorder of great concern affecting 14% of the world population. Since ancient times patients with vitiligo suffered the same mental abuses as lepers. In actual fact vitiligo was referred as Sweta Kustha meaning "White leprosy". In India vitiligo is commonly known as leucoderma. Leucoderma(Vitiligo) is a Latin word, meaning white skin' is caused by the destruction of melanocytes, the cells responsible for skin color. In Ayurvedic classical literature, such as the Charaka Samhita , leucoderma is called svitra or kilasa. The disorder is said to affect all races and genders equally and in 95% of cases, leucoderma manifests before age 40. [4] As for a possible hereditary link, approximately one third of cases report a family history. The most commonly affected areas of the body are the sun-exposed tops of hands and faces, and hyperpigmented areas of the body, such as the groin, nipples, genitalia and axilla, which includes face(24.5%), neck( 18.8%) ,scalp(11.2%). The disorder is not infectious, nor does it cause pathological harm. However, leucoderma does leave the skin aesthetically disfigured, often causing psychological and emotional stress
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
CLASSIFICATION OF VITILIGO Classification system is important because of special significance assigned by some authorities to each type of vitiligo. Vitiligo can be classified in two ways, Clinical classification of vitiligo according to Nordlund: Nordlund established a clinical classification based on distribution and extension of lesions (3). Localized: a. Focal: One or more macules with casual distribution i.e. non segmental pattern b. Segmental/Unilateral: One or more macules are localized in a unilateral body region,with a
dermatomeric distribution; a typical feature is an abrupt stop of the lesions at the midline. c. Mucosal: Unique involvement of mucous membranes Generalized: a. Vulgaris: it is the most common variety with a symmetrical distribution of lesions in typical zones, Presence of scattered stains extensively disseminated b. Acrofacialis: Patches are localized on distal extremities and face. c. Mixed: Co-existence of acrofacialis and vulgaris forms. Universalis: Universal vitiligo involves more than 80% of the body. Depigmented lesion formed almost completely the skin surface.
Vitiligo classification by Koga : This is a more recent classification subdividing vitiligo into two clinical types: a. Vitiligo segmentalis (type A) and b. Vitiligo non segmentalis(type B).
Type A Type A is more common, has a potential lifelong evolution and is associated with Koebner phenomenon and frequently with autoimmune diseases, such as Sutton nevus, thyroid disorders, juvenile diabetes mellitus, pernicious anemia and Addisons disease. In Segmental vitiligo unilateral
2
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
depigmented macules that do not cross the midline and follow Blaschko lines.
Type B Type B is rarer and has a dermatomal distribution, after rapid onset and evolution it usually exhibits a stable course. The natural course of the disease is generally unpredictable, but it is often progressive, some degree of spontaneous repigmentation occurs in 10-20% of patients, but it is rarely cosmetically acceptable (5), often occurring in a perifollicular pattern. In Nonsegmental vitiligo bilateral and symmetrical distribution of depigmented macules occurs.
MELANIN PRODUCTION Melanin is a photoprotective to skin cells, protecting them from light and UV radiation and the greater its density in the epidermis, the more protection is given to the layers of skin below. It does this by absorbing, reflecting and refracting light and preventing it from penetrating to the nucleus of keratinocytes or to lower levels of the skin. Melanin is also believed to play a role in scavenging free radicals, which can injure skin cells, and in facilitating UV induced apoptosis (programmed cell death), which removes damaged cells. Thus, melanins protective role goes beyond providing a physical barrier. It has been suggested that the 2-3 fold melanin levels seen in darker skin types, compared to lighter skintypes, convey up to 100-fold difference in sensitivity to ultraviolet radiation due to these protective functions. To produce me,lanin naturally, the MC1R pathway must be activated by the ligand alpha-Melanocyte Stimulating Hormone (-MSH) binding to the MC1R on the outside surface of the melanocyte. Approximately 1000 of these receptors exist on each healthy melanocyte. In the skin -MSH is expressed by keratinocytes and, less commonly, melanocytes and Langerhans cells as a protective response to damage caused by ultraviolet radiation (UVR, see below). -MSH molecules then bind with the MC1R on the melanocyte to activate the MC1R pathway and produce
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 3
VITILIGO THE WHITE LEPROSY
melanin. Following this process, melanin granules are deposited in packages called melanosomes which are then transported to the ends of the melanocyte projections, called dendrites. The tips of these dendrites are then enveloped by nearby keratinocytes into which the melanin granules are released. These spread out to form a pigmented, protective barrier over the keratinocytes nucleus (See Figure).
In addition to activating melanin, -MSH is known to have several other roles in the skin. Recent research has shown that -MSH reduces the generation of free radicals particularly hydrogen peroxide following UVR impact. However, -MSH must be able to bind to the MC1R to achieve this function. In some fairer skin types, and individuals with mutations or damage to the MC1R , the normal response when -MSH binds to the MC1R is significantly impaired or completely absent, reducing the protective response of these individuals. Alpha-MSH is also known to play a role in inhibiting both the expression and activity of pro-inflammatory molecules (cytokines) in skin, meaning that it acts in an anti-inflammatory capacity.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
Etiology and pathogenesis Etiology is still unknown, but some evidence based pathogenetic hypotheses have been proposed to explain the loss of melanocytes in epidermis, discussed as follows:
Genetic hypothesis Melanocytes have an inherent abnormality that impedes their growth and differentiation in conditions that support normal melanocytes. Family clustering of cases is common, since about 20% of patients have at least one affected firstdegree relative, with a non-Mendelian pattern suggestive of multifactorial, polygenic inheritance (14), segregation analyses suggest the involvement of multiple interacting genes in different populations (15). Several genes and chromosomal regions have been implicated in susceptibility to vitiligo, but none has been confirmed so far (16). In addition, several Human Leucocyte Antigen (HLA) abnormalities have been associated with vitiligo. A very recent and large epidemiological study supports the involvement of both genetic and non genetic factors in the pathogenesis of the disease and suggests that some genetic factors may be shared with other autoimmune diseases (16).
Autoimmune hypothesis This hypothesis proposes that an immune system disorder results in destruction of melanocytes. It is first supported by the frequent observation that several autoimmune disorders (thyroid diseases, Sutton nevi, juvenile diabetes mellitus, pernicious anemia and Addisons disease) are associated with vitiligo. A significant association of vitiligo was demonstrated with thyroid dysfuntion and/or thyroid antibodies in particular (18). It is likely that both humoral and cellular immunity co-operate in the destruction of melanocytes. Concerning humoral immunity, antibodies to surface and cytoplasmic antigens of melanocytes have been found in vitiligo patients, mainly belonging to the IgG class. The autoantigens most frequently identified are antigens related to HLA class I molecules, tyrosinase, tyrosinase-related protein (TRP)-1 and TRP-2 (the last three are melanocytespecific antigens) (19). However, the pathogenetic role of antimelanocyte antibodies remains unclear. The serum levels of antibodies to melanocyte antigens seem to correlate with activity and extent of the disease and with the presence of other immune disorders, and to decrease in vitiligo patients responding to therapy (19).
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
Concerning cellular immunity, an important role has been given to the infiltrate underlying the pigmented lesional skin, where CD4 and CD8 positive T cells were detected, also expressing activation molecules. A substantial number of infiltrating T cells express the cutaneous lymphocyte antigen (CLA) typical of skin homing cells (20), and a recent study found CLA positive cytotoxic T cells in apposition to disappearing melanocytes in the perilesional skin (21). In vitiligo patients, high frequencies of Melan-A/Mart1 (a melanosomal antigen) specific CD8 positive T cells were detected in peripheral blood (1). Interestingly, Melan-A/Mart1 specific CD8 positive T lymphocytes were identified in inflammatory lesions of melanocyte destruction following infusion of Melan-A/Mart1 specific CD8 positive T-cell clones in melanoma patients (22): this finding gives direct evidence of T-cell mediated vitiligo.
http://www.bio.davidson.edu/Courses/Immunology/Students/Spring2003/Leese/Vitiligo.htm
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
Neuronal hypothesis This hypothesis suggests that some neurochemical mediators, possibly secreted from contiguous nerve endings, are cytotoxic for pigment cells. This theory is supported by the existence of segmental variant of vitiligo that affects a dermatome, by the occurrence of vitiligo after a period of severe emotional stress, and by the onset of disease in patients with neurological disorders or with peripheral nerve injury (23, 24). Abnormalities of neuropeptides have been observed in perilesional skin and in blood of vitiligo patients (25). In addition, increased catecholamine discharge or synthesis has been associated with disease activity, suggesting a role of catecholamines in the depigmentation process (26). Important support to this theory has been given by the demonstration of morphological and functional communication between epidermal melanocytes and nervous system (27).
Autocytotoxic/metabolic hypothesis: This theory suggests an intermediate or metabolic product of melanin synthesis causes melanocyte destruction. Oxidative stress has been suggested to be the initial pathogenetic event in melanocyte degeneration (28, 29) with H2O2 accumulation in the epidermis of patients with active disease (12). Defective recycling of tetrahydrobiopterin has been reported in vitiligo epidermis, associated to the intracellular production of H2O2 (28, 12). In addition, an alteration in the antioxidant pattern, with a significant reduction of catalase activity, has been demonstrated in both lesional and non lesional epidermis of patients (30), as well as in melanocytes (29). However, the antioxidant imbalance was confirmed in peripheral blood mononuclear cells of active vitiligo patients, and was correlated to an increased intracellular production
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 7
VITILIGO THE WHITE LEPROSY
of reactive oxygen species and appeared to be due to a mitochondrial impairment (31). These findings support the concept of a possible systemic oxidative stress in vitiligo.
Novel microenvironment-related hypothesis Cytokine imbalance in the epidermal microenvironment has been demonstrated in lesional skin in active vitiligo. A decrease in cytokines stimulating melanocyte impairs normal life and activity of melanocytes, and an increase in cytokines inhibiting melanocytes were detected in depigmented lesions (32). According to this hypothesis, a central role is assigned to cutaneous microenvironment.
Convergence/ Mixed theory The description of many credible contributory factors to the pathogenesis of vitiligo led to this theory, in which different causal elements may act synergistically or independently to provoke disappearance of melanocytes. Genetic factors, oxidative stress, autoimmunity, mutations, altered cellular environment can all contribute to the disease (33).
Symptoms Vitiligo symptoms include depigmentation of the skin on the external body parts. This appearance of light colored patches in the skin is the most crucial symptom that may differ in shade from one patient to another as well as from one patch to the other. These patches are commonly found on the areas of the body that are more exposed to sun, including the lips, face, arms, feet and hands. Other body areas where white patches appear are the following: rectum, genitals, navel, nostrils and eyes, around the mouth, and armpits and groin. The most obvious sign of vitiligo is loss of pigment on the flat skin, resulting in creating milky-white, irregularly shaped patches on it.The skin cells do not produce enough melanin. For some people this can happen quickly, while for others the patches may stay the same for months or years.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
The first white patch usually develops where the skin has been exposed to the sun. About 12% vitiligo patients, experience intense itching at the site of area that exposed to sunlight, but normally it does not cause itching or any physical discomfort to the skin. If the white patches appear symmetrically on more than one part of body, then such condition may progress quite slowly, but if you have white patches on only one area of your body, then this condition may progress more rapidly. Less common signs include loss of hairs colour pigment or graying of hair on scalp, eyebrows, eyelashes or other affected areas. The loss of pigment may also experience on the tissues that line inside the mouth (mucous membranes) and the retina of the eye in vitiligo patients The white spots are usually more common over bony areas. Sometime, these white spots or patches produce a mirror image effect by occurring in the same areas on both sides of the body.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
VITILIGO THE WHITE LEPROSY
Diagnosis The diagnosis of vitiligo is made based on a physical examination, medical history, and laboratory tests. A doctor will likely suspect vitiligo if the physical examination reveals white patches of skin on the body-particularly on sun-exposed areas, including the hands, feet, arms, face, and lips. If vitiligo is suspected, the doctor asks about patients medical history. Important factors in the diagnosis include a family history of vitiligo, a rash, sunburn, or other skin trauma that occurred at the site of vitiligo 2 to 3 months before depigmentation started, stress or physical illness, and premature graying of the hair (before age 35). In addition, the doctor asks whether patient or anyone in patients family has had any autoimmune diseases and whether patient is very sensitive to the sun. To help confirm the diagnosis, the doctor may take a small sample (biopsy) of the affected skin to examine under a microscope. In vitiligo, the skin sample will usually show a complete absence of pigment-producing melanocytes. On the other hand, the presence of inflamed cells in the sample may suggest that another condition is responsible for the loss of pigmentation. As vitiligo may be associated with pernicious anemia or hyperthyroidism , the doctor may also take a blood sample to check the blood-cell count and thyroid function. Vitiligo is diagnosed by means of inspection with WOODs lamp. Woods lamp is a hand- held ultraviolet (UV) irradiation device that emits UVA. It has been used to identify the areas of depigmentation that may not be visible to the naked eye especially in pale skin.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
10
VITILIGO THE WHITE LEPROSY
For some patients, the doctor may recommend an eye examination to check for uveitis (inflammation of part of the eye), which sometimes occurs with vitiligo. A blood test to look for the presence of antinuclear antibodies (a type of autoantibody) may also be done. This test helps determine if the patient has another autoimmune disease.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
11
VITILIGO THE WHITE LEPROSY
Treatments Vitiligo cannot be cured, but many treatments help to restore lost skin color. Now a days vitiligo can be managed using wide range of traditional, new, experimental therapeutic methods, each one of which has different indications. Treatment can be divided in to 3 main types; repigmentation, depigmentation, cosmetics Prescription medicine: Steroids: Corticosteroids are broad group of drugs that are widely used in various dermatological and non dermatological conditions. Corticosteroids both topical and systemic have been used in vitiligo for over four decades with some concern about its efficacies well as its known or expected side effects. Corticosteroids helps in returning of color to skin (repigmenting), particularly if they are started early in the disease. These drugs which include cortisone are similar to the hormones produced by your adrenal glands. Mechanism of action of corticosteroids in vitiligo Corticosteroids suppress autoantibody formation and likely induce apoptosis of cytotoxic T cells. The autoimmune hypothesis still prevails in the pathogenesis of non-segmental vitiligo, and the autoimmune process is not limited to the skin. In progressive disease, there is continuous assault on melanocytes. Topical corticosteroids suppress autoimmune dysfunction at the site of a vitiligo lesion, but these do not have any effect on the disease process. Systemic corticosteroids act not only on lesional immune activity, but also on the T cells in peripheral circulation. Besides modulating cellmediated immunity, corticosteroids also suppress autoantibody formation. The serum of actively spreading vitiligo patients who received oral corticosteroids and showed improvement had a decrease in complement-mediated cytotoxicity by melanocyte autoantibodies and a reduced antibody titer to the melanocyte surface antigen.
Systemic corticosteroids Structure and classification
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 12
VITILIGO THE WHITE LEPROSY
The structure of corticosteroids consists of three hexane rings and one pentane ring known as the cyclopentanoperhydrophenathrene nucleus. The different systemic corticosteroids are variations of this basic structure. Systemic corticosteroids are classified according to their half-lives. Short Acting Cortisone Hydrocortisone Deflazacort Intermediate Acting Prednisone Prednisolone Methylprednisolone Triamcinolone Long Acting Dexamethasone Betamethasone Topical corticosteroid A mild topical corticosteroid cream or ointment is prescribed for children younger than 10 years old or a stronger form for adults. Patients need to apply the cream or ointment to the white patches on skin for at least three months before any results. This treatment is simple and safe, but your doctor will monitor closely for side effects, such as skin shrinkage and streaks or lines on your skin. Topical steroids have revolutionized the practice of dermatology since they were introduced in the late 1950s. Topical steroids can be divided up into four groups according to their strength. As a rule, use the weakest possible steroid that will do the job. However, sometimes it is appropriate to use a potent preparation for a short time to make sure the skin condition clears completely. Class 1 Very potent (up to 600 times as potent as hydrocortisone) Class 2 Potent (I50-100 times as potent as hydrocortisone)
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 13
Clobetasol propionate (Cream/Ointment) Betamethasone dipropionate (Cream/Ointment)
VITILIGO THE WHITE LEPROSY
Class 3
17-butyrate (Cream/Topical Emulsion/ Lipocream /Ointment/Scalp Lotion) Betamethasone valerate (Cream/Ointment/Scalp Application/ Lotion) Betamethasone dipropionate (Cream/Ointment) Diflucortolone valerate (Cream/Fatty Ointment/Ointment) Hydrocortisone Mometasone furoate ( Cream/Lotion/Ointment) Methylprednisolone aceponate (Cream/Ointment)
Moderate (2-25 times as potent as hydrocortisone) Class 4 Mild Hydrocortisone 0.5-2.5% (Cream/Soft Cream, Lotion-HC 1%,Fatty Cream HC, Ointment) Clobetasone butyrate (Cream) Triamcinolone acetonide (Cream/Ointment)
Topical steroids are also available in combination with salicylic acid to enhance penetration, and with antibacterial and antifungal agents. Skin absorption of topical steroids Steroids are absorbed at different rates from different parts of the body. A steroid that works on the face may not work on the palm. But a potent steroid may cause side effects on the face. For example: Forearm absorbs 1% Armpit absorbs 4% Face absorbs 7% Eyelids and genitals absorb 30% Palm absorbs 0.1% Sole absorbs 0.05%
Like all medications, corticosteroids are associated with potential adverse effects (side effects) especially if they are used incorrectly.
Side effects of topical steroids Internal side effects If more than 50g of clobetasol propionate, or 500g of hydrocortisone is used per week,
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 14
VITILIGO THE WHITE LEPROSY
sufficient steroid may be absorbed through the skin to result in adrenal gland suppression and/or eventually Cushing's syndrome. Adrenal Gland Suppression. Topical steroids can suppress the production of natural steroids, which are essential for healthy living. Stopping the steroids suddenly may then result in illness. Cushing's Syndrome If large amounts of steroid are absorbed through the skin, fluid retention, raised blood pressure, diabetes etc. may result. Skin side effects Local side effects of topical steroids include: Skin thinning (atrophy) and stretch marks (striae). Easy bruising and tearing of the skin. Perioral dermatitis (rash around the mouth). Enlarged blood vessels (telangiectasia). Susceptibility to skin infections. Disguising infection e.g. tinea incognito. Allergy to the steroid cream. The risk of these side effects depends on the strength of the steroid, the length of application, the site treated, and the nature of the skin problem. If you use a potent steroid cream on your face as a moisturiser, you will develop the side effects within a few weeks. If you use 1% hydrocortisone cream on your hands for 25 years, you will have done no harm. Bruising Skin thinning Prominent capillaries Stretch marks
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
15
VITILIGO THE WHITE LEPROSY
Topical steroids are very effective medications. They work by reducing inflammation, and when used correctly are very safe.
Surgical Therapy In the last years, surgical therapies consist the use of autologous skin grafts have been proposed. It is mandatory to treat only patients showing stability in their vitiligo lesions: hypopigmented patches should be stable from at least 2 years before surgical therapy and is warmly recommended to subject the patient to a minigrafting test before performing the definitive graft, in order to evaluate the positive response and the inauspicious occurrence of Koebners phenomenon at the donor site after 23 months follow-up. The surgical response is higher in segmental or focal vitiligo than in generalized vitiligo. Moreover, better surgical results are obtained in patients younger than 20 years, but skin graft is not recommended for patients with a tendency to form keloids or develop hyperpigmentation after minimal trauma Autologous skin grafts
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
16
VITILIGO THE WHITE LEPROSY
The pigment containing skin from one area of the body is surgically shifted to an area where there is no pigment. The success is usually not predictable and the result may be more un-acceptable than the base-line. When the cost, the hassle and the risk of surgical complications like scarring and infection are added, it becomes a fairly risky option to go for vitiligo treatment. Skin grafts using blisters It is a variation in the technique of skin grafting, in which blisters on the pigment containing skin are artificially created and then cut out to be transplanted at the required site. The risk of scaring is less than the standard technique, but success in the form of re-pigmentation is not very encouraging. Autologous melanocyte transplants The pigment containing skin from one area of the body is surgically shifted to an area where there is no pigment. The procedure has shown some promise, but is not widely available, because it is still in its experimental stages. Tattooing Tattooing is not a traditional vitiligo treatment but used as a camouflage technique, it is done with artificial pigments which are deposited into the skin, with the help of traditional tattooing needles or by surgical techniques in present scientific era. The accuracy of color match shall depend upon the skill of the person doing it. It will work best for darker skins, and the color may become lighter with the passage of time. There are risks of serious infections spreading with tattooing through traditional methods. Tattooing should only be carried out by certified and licensed professionals
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
17
VITILIGO THE WHITE LEPROSY
Photo therapy UV light, or phototherapy vitiligo treatment can help create repigmentation. This process is slow, working from the outer edges of each patch inward, so regular phototherapy vitiligo treatment is prescribed. Phototherapy vitiligo treatment may continue twice a week for a year or more. Phototherapy equipment has been well-studied and has been proven to be an effective treatment for vitiligo. (nmiv) Photochemotherapy and phototherapy stimulate melanocytes to cause repigmentation and have minimal immunomodulatory action on T-lymphocytes, but may not halt the rapid destruction of melanocytes. PUVA (photochemotherapy) is a type of ultraviolet radiation treatment (phototherapy) used for severe skin diseases. PUVA is a combination treatment which consists of Psoralens (P) and then exposing the skin to long wave ultraviolet radiation (UVA). It has been available in its present form since 1976. Psoralens are compounds found in many plants which make the skin temporarily sensitive to UVA. The ancient Egyptians were the first to use psoralens for the treatment of skin diseases thousands of years ago. Methoxsalen capsules are taken two hours before exposure to UVA. Bulbs emitting different wavelengths are used for UVB (short wavelength radiation). Those patients requiring treatment to small areas only may be treated using the smaller hand and foot unit. 'Bathwater' PUVA may be suitable. In this case the hands and/or feet are soaked in a dilute solution of methoxsalen for 30 minutes, then immediately exposed to UVA. A few patients may be treated with topical Tripsor PUVA - a lotion is painted on the affected areas 10 minutes before UVA exposure. PUVA is useful for patients with various skin disorders, including psoriasis, dermatitis, polymorphic light eruption and mycosis fungoides. The number and the frequency of PUVA treatments will depend on the condition being treated and individual factors. Side Effects Burning An overdose of PUVA results in a sunburn-like reaction called phototoxic erythema. It is more likely in fair skinned patients who sunburn easily. A burn is most likely 48 to 72 hours after the first two or three treatments. Sensitive areas such as breasts and buttocks may need to be covered for all or part of the treatment. Avoid photosensitizers such as certain medications, perfumed cosmetics and coal coal tar. If the treated skin becomes pink the dose of UVA will not be increased. One or more treatments
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar 18
VITILIGO THE WHITE LEPROSY
may be missed. Unfortunately phototoxic erythema can persist for longer than sunburn from natural sunlight. Moisturizers and painkillers can reduce the discomfort. Itching Temporary mild pricking or itching of the skin is common after treatment. The skin is often rather dry. Apply moisturizing cream or lotion frequently. Antihistamine tablets may help. Nausea Nausea occurs in a quarter of those treated with psoralens. If it occurs, tell your phototherapy nurse or doctor. Nausea is less if the methoxsalen capsules are taken with food, or the dose is reduced. Antiemetic tablets can be prescribed. Tanning PUVA usually leads to tanning which lasts several months. Although the skin appears brown it may still burn easily on sun exposure. Eye damage If the eyes are not protected from UV radiation, keratitis may occur. This results in red sore gritty eyes. Damage to the lens in the eye leading to cacoal taracts is another possible risk. Skin aging and skin cancer Extensive PUVA treatment results in premature aging changes in the skin (i.e. increased dryness, freckling and wrinkling) and can increase the chance of skin cancer. Fair skinned individuals or those with previous sun or radiation damage are most at risk. This is not a concern for most patients, who receive PUVA therapy for two or three months only. Patients on long term maintenance therapy should have their skin checked by the specialist at least every 6 months. Bring any new moles or freckles, sores which are slow to heal, or growing lumps to the doctor's attention. It should be remembered that usually, but not always, skin cancers are readily curable. When ageing changes are evident or skin cancers occur, it becomes unwise to continue this form of treatment. Pregnancy There is no evidence to suggest that PUVA will damage a developing baby. However, should a patient become pregnant, or suspect she is pregnant, during a course of treatment, we advise our patients to stop PUVA treatment immediately. Narrow-band ultraviolet B (NBUVB) therapy. In recent years, NBUVB, a special form of ultraviolet B light, has been used as an alternative to PUVA. This type of therapy can be administered like PUVA and given up to three times a week. However, no
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
19
VITILIGO THE WHITE LEPROSY
pre-application of psoralen is required, thus simplifying the treatment process. NBUVB may be a safer long-term alternative to PUVA. However, more research is needed.
Home Remedies Majority of the patients will try a home remedy as vitiligo treatment, at least once in their lifetime. They range from simple dietary modifications to the ingestion of psoralens. The benefits are as variable as the nature of remedies. The most effective of all home remedies of course is the use of psoralens, but an unsupervised use of these potent herbs can lead to very unpleasant side effects, which may preclude their further continuation.
1.
Take about 25 grams of radish seeds and ground them into a powdery substance. Add 2 tsp vinegar and make a fine paste. Apply this paste on the affected area and wash off when dry.
2.
In about eight liters of water, soak 500 gm turmeric. Boil the concoction until only a liter of it is left. Strain this liquid and add liter mustard oil to it. Apply this on the patchy areas two times a day, for at least 2-3 months.
3.
Soak psoralea seeds in ginger juice for 3 days. Thereafter, dry them and grind to make a fine powder. Have 1 gram of this powder, with a glass of milk, for about a month. You can also apply this powder on white patches.
4.
Another method would be to soak psoralea and tamarind seeds in water for 3-4 days. Dry them well and grind to form a paste. Apply this paste on the affected area on a daily basis.
5.
Goosefoot vegetable is effective in treating leucoderma. Apply the juice of this vegetable on the affected area, once a day. Continue it for 2 months.
6. 7.
Mix red clay and ginger in equal parts. Apply this on the affected area and wash off when dry. Fill a copper vessel with drinking water and leave it overnight. Have this water, on an empty stomach, every morning. This is effective in healing leucoderma.
8.
Combine 100 gm each of alfalfa and cucumber juice. Consume this mixture two times a day i.e. in the morning and evening. This is a useful home remedy for treating leucoderma.
9.
Take a handful of dry pomegranate leaves and grind them into a fine powder. Have about 8 grams of this powder every morning and evening, with a glass of water.
10. 11.
Neem is very effective in treating leucoderma. Try to drink a glass of neem juice everyday. Grind black gram and add water, to form a paste. Apply this paste on the affected area, washing off after it dries, for about 4 to 5 months. It is an effective remedy for treating leucoderma.
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
20
VITILIGO THE WHITE LEPROSY 12.
Holy basil leaves prove to be beneficial in treating white patches. Consume raw basil leaves or make a decoction out of Holy basil's leaves and stem, along with water.
13.
Make a poultice of ginger leaves and apply it on the white patches. It is quite effective in treating leucoderma.
14.
Increase the consumption of walnuts and figs. While walnuts purify blood, figs have healing properties to cure leucoderma. http://www.iloveindia.com/home-remedies/leucoderma.html
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
21
VITILIGO THE WHITE LEPROSY
Dr. L. H. Hiranandani College of Pharmacy, Ulhasnagar
22
You might also like
- Vitiligo and Leukoderma in Children: Maria Isabel Herane, MDDocument13 pagesVitiligo and Leukoderma in Children: Maria Isabel Herane, MDBimo Aryo TejoNo ratings yet
- Melasma Insights and PerspectivesDocument6 pagesMelasma Insights and PerspectivesTatianaNo ratings yet
- Vitiligo: Refer ATDocument18 pagesVitiligo: Refer ATAndhika FrabesNo ratings yet
- Artikel Kelainan Kulit - Vitiligo DLLDocument13 pagesArtikel Kelainan Kulit - Vitiligo DLLRosa SeptianaNo ratings yet
- Skin Pigmentation + Hari DisorderDocument113 pagesSkin Pigmentation + Hari DisorderAfiqah So JasmiNo ratings yet
- Laporan Kasus Aiman KamilaDocument16 pagesLaporan Kasus Aiman KamilazzooooeeeeeeNo ratings yet
- An Overview On Melasma 2376 0427 1000216Document18 pagesAn Overview On Melasma 2376 0427 1000216dhilaidrisNo ratings yet
- A Review On Common Dermatologic ConditionsDocument8 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- A Review On Common Dermatologic ConditionsDocument10 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- Acquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateDocument53 pagesAcquired Hypopigmentation Disorders Other Than Vitiligo - UpToDateBaoz PingNo ratings yet
- Skin PDFDocument3 pagesSkin PDFPerry SinNo ratings yet
- MelasmDocument22 pagesMelasmLeonardo Alves F AlmeidaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014machiiNo ratings yet
- A Review On Common Dermatologic ConditionsDocument16 pagesA Review On Common Dermatologic ConditionsQuality TimbersNo ratings yet
- Vitiligo: An Update: Published: 17 January 2011Document21 pagesVitiligo: An Update: Published: 17 January 2011Narayanan RajendranNo ratings yet
- TranslateDocument67 pagesTranslatesriwahyuniNo ratings yet
- 32Document21 pages32gamhaelNo ratings yet
- Liken Planus & Lichen Sclerosus Et Atropichus, Granuloma AnulareDocument29 pagesLiken Planus & Lichen Sclerosus Et Atropichus, Granuloma AnulareroserosannaNo ratings yet
- Kuliahskin Pigmentation + Hair Disorder-Power Pointedit-2 - 26april11Document113 pagesKuliahskin Pigmentation + Hair Disorder-Power Pointedit-2 - 26april11Andersen ChenNo ratings yet
- The Lichens in Vulvovaginal Disease 2015Document20 pagesThe Lichens in Vulvovaginal Disease 2015Vidini Kusuma AjiNo ratings yet
- Amyloidosis SkinDocument6 pagesAmyloidosis SkinGoran MaliNo ratings yet
- Stevens Johnson Syndrome CASEDocument53 pagesStevens Johnson Syndrome CASEKathrina CraveNo ratings yet
- Manila Central UniversityDocument5 pagesManila Central UniversityRajan ChaudharyNo ratings yet
- Tratment Melasma PDFDocument18 pagesTratment Melasma PDFGheavita Chandra DewiNo ratings yet
- SGD Ein 2 Kelompok 5Document27 pagesSGD Ein 2 Kelompok 5Rahmadanti Nur FadillaNo ratings yet
- Meds CapeDocument14 pagesMeds CapeMeta SakinaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014Erlangga DayudNo ratings yet
- Pityrosporum FolliculitisDocument3 pagesPityrosporum Folliculitisshivam18No ratings yet
- LentigoDocument15 pagesLentigoaditya ratna utariNo ratings yet
- Cytokine: E.S. Robinson, V.P. WerthDocument9 pagesCytokine: E.S. Robinson, V.P. WerthArthurAkkNo ratings yet
- Stevens-Johnson Syndrome CASEDocument38 pagesStevens-Johnson Syndrome CASEChristy Rose AgrisNo ratings yet
- Melasma and Post Inflammatory Hyperpigmentation Management Update and Expert OpinionDocument19 pagesMelasma and Post Inflammatory Hyperpigmentation Management Update and Expert OpinionLutfi MKNo ratings yet
- Cutaneous amylo-WPS OfficeDocument6 pagesCutaneous amylo-WPS Officesveeram3No ratings yet
- Skin PigmentatDocument110 pagesSkin Pigmentatsteven saputra0% (1)
- PigmentationDocument28 pagesPigmentationCabdiladif Ahmed McrfNo ratings yet
- Jadotte Pityriasis AlbaDocument8 pagesJadotte Pityriasis Albapene asoyNo ratings yet
- Jurnal Keperluan PentingDocument4 pagesJurnal Keperluan PentingmhdtaufikkNo ratings yet
- Urticaria and AngioedemaDocument40 pagesUrticaria and AngioedemaDea LeeteukNo ratings yet
- The Evolution of Biochemical Indices After Basal Cell Epithelioma Removal - Case ReportDocument6 pagesThe Evolution of Biochemical Indices After Basal Cell Epithelioma Removal - Case ReportGurgas LeonardNo ratings yet
- DERMATOLOGY Notes From Uworld, DR-KYDocument22 pagesDERMATOLOGY Notes From Uworld, DR-KYLayan Mohammad100% (1)
- Toxic Responses of The SkinDocument25 pagesToxic Responses of The SkinfianceeleeNo ratings yet
- Exfoliative DermatitisDocument7 pagesExfoliative DermatitisRidyah Ning TyasNo ratings yet
- Lupus ErythematosusDocument3 pagesLupus ErythematosusAMOS MELINo ratings yet
- 157-Article Text-621-1-10-20120514Document7 pages157-Article Text-621-1-10-20120514loNo ratings yet
- UWorld Notes - Mark ChaskesDocument36 pagesUWorld Notes - Mark Chaskesise7No ratings yet
- Ghafourian Et Al 2014 Vitiligo Symptoms Pathogenesis and TreatmentDocument5 pagesGhafourian Et Al 2014 Vitiligo Symptoms Pathogenesis and Treatmentnramrattan475No ratings yet
- Vitiligo 1-09-220vitiligoDocument11 pagesVitiligo 1-09-220vitiligomulyadiansyahNo ratings yet
- Natural Options For Management of MelasmaDocument17 pagesNatural Options For Management of Melasmapuji lestari100% (1)
- Health and Wellness Integumentary System: by DR M Umer IqbalDocument25 pagesHealth and Wellness Integumentary System: by DR M Umer IqbalShimmering MoonNo ratings yet
- A HoyDocument17 pagesA HoyMadelaine MoncayoNo ratings yet
- Dermatomyositis Case7Document15 pagesDermatomyositis Case7Hanina Macataman MetmugNo ratings yet
- Alopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DDocument7 pagesAlopecia Areata: Amos Gilhar, M.D., Amos Etzioni, M.D., and Ralf Paus, M.DSistaNo ratings yet
- Vitiligo and Clinical: September 2014Document11 pagesVitiligo and Clinical: September 2014cjristinNo ratings yet
- Melasma: An Up-to-Date Comprehensive Review: Oluwatobi A. Ogbechie-Godec Nada ElbulukDocument14 pagesMelasma: An Up-to-Date Comprehensive Review: Oluwatobi A. Ogbechie-Godec Nada ElbulukDra Natalia Maria ZuluagaNo ratings yet
- Leishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeishmaniasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Comprehensive Insights into Acute Cutaneous Lupus: Unraveling Pathways, Implications, and InterventionsFrom EverandComprehensive Insights into Acute Cutaneous Lupus: Unraveling Pathways, Implications, and InterventionsNo ratings yet
- Surviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsFrom EverandSurviving Leukemia and Hodgkin's Lymphoma: An Overview Of Effective Treatment MethodsNo ratings yet
- Understanding Skin Problems: Acne, Eczema, Psoriasis and Related ConditionsFrom EverandUnderstanding Skin Problems: Acne, Eczema, Psoriasis and Related ConditionsNo ratings yet
- Steroids PDFDocument35 pagesSteroids PDFPratyusha VallamNo ratings yet
- JURDING (Corticosteroids Therapy in Combination With Antibiotics For Erysipelas)Document21 pagesJURDING (Corticosteroids Therapy in Combination With Antibiotics For Erysipelas)Alif Putri YustikaNo ratings yet
- What Are The Therapeutic Classes of DrugsDocument3 pagesWhat Are The Therapeutic Classes of DrugsFrank GomesNo ratings yet
- Clobetasol CreamDocument9 pagesClobetasol CreamGiulianospharmacyNo ratings yet
- Chapter 37: Drugs Used To Treat Thyroid DiseaseDocument40 pagesChapter 37: Drugs Used To Treat Thyroid DiseaseAziil LiizaNo ratings yet
- ACE Group Guidelines SARS CoV 2Document6 pagesACE Group Guidelines SARS CoV 2Dr. Hilder HernandezNo ratings yet
- Course Task 8 Drug Study On Respiratory AgentsDocument23 pagesCourse Task 8 Drug Study On Respiratory AgentsAdrienne Nicole PaneloNo ratings yet
- Adrenocorticosteroids & Adrenocortical AntagonistsDocument20 pagesAdrenocorticosteroids & Adrenocortical Antagonistsapi-3859918No ratings yet
- Traumatic Optic NeuropathyDocument5 pagesTraumatic Optic NeuropathyMiftahurrahmah GmsNo ratings yet
- Pharmacologic: Systemic Administration AssessmentDocument3 pagesPharmacologic: Systemic Administration Assessmentitsmeaya100% (1)
- Management of Acute Respiratory Diseases PDFDocument21 pagesManagement of Acute Respiratory Diseases PDFFernandoXavierNo ratings yet
- Necrobiosis Lipoidica Dia..-GhjuytDocument7 pagesNecrobiosis Lipoidica Dia..-GhjuytAshesForTearsNo ratings yet
- Clinical Pharmacy Questions and AnswersDocument8 pagesClinical Pharmacy Questions and AnswersMelavNo ratings yet
- CIRCI Guidelines 2015Document6 pagesCIRCI Guidelines 2015Wissam SleimanNo ratings yet
- SNAP Comparison of Topical SteroidsDocument12 pagesSNAP Comparison of Topical SteroidsRany100% (1)
- Deflazacort - GluticordDocument25 pagesDeflazacort - GluticordChintan ChavdaNo ratings yet
- Mometasone FuroatDocument8 pagesMometasone FuroatAnonymous ZrLxxRUr9zNo ratings yet
- Pharmacology For The Interventional Pain Physician: Magdalena Anitescu Honorio T. Benzon Renata VariakojisDocument1 pagePharmacology For The Interventional Pain Physician: Magdalena Anitescu Honorio T. Benzon Renata VariakojisFaith Acu CureNo ratings yet
- DS Norepinephrine HydrocortisoneDocument4 pagesDS Norepinephrine HydrocortisoneReign RaineNo ratings yet
- Fucicort CreamDocument4 pagesFucicort Creamcupcake xNo ratings yet
- Beclomethasone DipropionateDocument3 pagesBeclomethasone Dipropionateapi-3797941No ratings yet
- Pharmacology NotebookDocument31 pagesPharmacology Notebookapi-284057899No ratings yet
- Steroid Injection Costs. Cheap Anabolic Steroids #Rjhy8NurDocument2 pagesSteroid Injection Costs. Cheap Anabolic Steroids #Rjhy8NurMarielaNo ratings yet
- Clobetasol Anuth8ngDocument7 pagesClobetasol Anuth8ngWhiel Kurt Arzaga SaragconNo ratings yet
- FENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialDocument23 pagesFENO As Monitoring Tool in Bronchial Asthma A Randomised Control TrialYadvir GargNo ratings yet
- лекц10Document41 pagesлекц10A A D H INo ratings yet
- Conference Reports and Expert Panel: DOI 10.1007/s00134-017-4919-5Document13 pagesConference Reports and Expert Panel: DOI 10.1007/s00134-017-4919-5Mari ArcenganNo ratings yet
- Farmakologi Obat Pada Reaksi HipersensitivitasDocument59 pagesFarmakologi Obat Pada Reaksi HipersensitivitasTitip Elia GustamiNo ratings yet
- A Seminar On Adrenal Cortex Hormones: Presented By: Jignesh Patel 1 Year M. Pharm A.B.M.R.C.P Banglore-90Document14 pagesA Seminar On Adrenal Cortex Hormones: Presented By: Jignesh Patel 1 Year M. Pharm A.B.M.R.C.P Banglore-90Amit GhoshNo ratings yet
- 2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDDocument58 pages2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDKishan SethNo ratings yet