Professional Documents
Culture Documents
PPPP
PPPP
Uploaded by
Christy Ada IjeomaCopyright:
Available Formats
You might also like
- TheQuestforTheCures 7EpisodeTranscriptsEbookDocument250 pagesTheQuestforTheCures 7EpisodeTranscriptsEbookciprian72100% (1)
- Nelson JaundiceDocument7 pagesNelson JaundiceJesly CharliesNo ratings yet
- Virginia Environmental Literacy Plan TemplateDocument8 pagesVirginia Environmental Literacy Plan TemplateVirginia Association for Environmental EducationNo ratings yet
- Biology Comparison of The Major Animal Phyla ChartDocument2 pagesBiology Comparison of The Major Animal Phyla Chart09temp100% (3)
- Bac GroundDocument6 pagesBac GroundRitu Ayu PutriNo ratings yet
- Neonatal JaundiceDocument30 pagesNeonatal JaundiceAnonymous Y3fqBduNo ratings yet
- Jaundice EnglishDocument5 pagesJaundice EnglishArinaManaSikanaNo ratings yet
- Neonatal JaundiceDocument4 pagesNeonatal JaundiceChristian Eduard de DiosNo ratings yet
- Overview#showall: March 04 2016Document32 pagesOverview#showall: March 04 2016viyolaazzahraNo ratings yet
- Referrence:: Glucose-6-Phosphatase Dehydrogenase (G-6-PD) DeficiencyDocument2 pagesReferrence:: Glucose-6-Phosphatase Dehydrogenase (G-6-PD) DeficiencyKim DeyNo ratings yet
- Causes: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekDocument7 pagesCauses: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekIzzah100% (1)
- Pathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornDocument45 pagesPathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornJaner BanosNo ratings yet
- Consequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsDocument3 pagesConsequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsAradhanaRamchandaniNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceGiska T PutriNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceAlya Afifa100% (1)
- Neonatal HandbookDocument11 pagesNeonatal HandbookJanua NavaretteNo ratings yet
- Neonatal JaundiceDocument48 pagesNeonatal JaundiceRemy MartinsNo ratings yet
- Neonatal JaundiceDocument18 pagesNeonatal JaundiceArinaManaSikanaNo ratings yet
- Breastmilk JaundiceDocument13 pagesBreastmilk JaundicenadiancupNo ratings yet
- 1 Core Concepts Bilirubin MetabolismDocument9 pages1 Core Concepts Bilirubin Metabolismlink0105No ratings yet
- Core Concepts Bilirrubin MetabolismDocument9 pagesCore Concepts Bilirrubin MetabolismAngelina ChunNo ratings yet
- Presentation and Duration of Neonatal JaundiceDocument5 pagesPresentation and Duration of Neonatal JaundiceRizki DaulayNo ratings yet
- Core Concepts:: Bilirubin MetabolismDocument9 pagesCore Concepts:: Bilirubin MetabolismManasye AlanNo ratings yet
- 17 - Neonatal Jaundice MCH 410 2012Document32 pages17 - Neonatal Jaundice MCH 410 2012frederickmwansa22No ratings yet
- IctericiaDocument19 pagesIctericiadavid pinedaNo ratings yet
- Jurnal NHDocument14 pagesJurnal NHShintya DewiNo ratings yet
- Icterus, HiperbilirubinemiaDocument3 pagesIcterus, HiperbilirubinemiameidyNo ratings yet
- Difference Between Physiologic Jaundice and Pathologic JaundiceDocument2 pagesDifference Between Physiologic Jaundice and Pathologic JaundiceNurulAqilahZulkifli100% (4)
- Hiperbilirrubinemia DirectaDocument9 pagesHiperbilirrubinemia DirectaRonal Cadillo MedinaNo ratings yet
- Neonatal Jaundice DR - MaslianiDocument58 pagesNeonatal Jaundice DR - MaslianiHengky HanggaraNo ratings yet
- Ikterus NeonatorumDocument10 pagesIkterus NeonatorumHerryanto AgustriadiNo ratings yet
- Neonatal Jaundice: AuthorsDocument9 pagesNeonatal Jaundice: AuthorsRam Kumar ShresthaNo ratings yet
- Neonatal Hyperbilirubinemia and JaundiceDocument8 pagesNeonatal Hyperbilirubinemia and JaundiceAndreea GeorgianaNo ratings yet
- HyperbilirubinemiaDocument48 pagesHyperbilirubinemiaEdrik Luke Pialago100% (2)
- ) Jaundice PDFDocument4 pages) Jaundice PDFAzzNo ratings yet
- Neonatal JaundiceDocument10 pagesNeonatal JaundiceLGK maoreNo ratings yet
- Neonatal Jaundice - StatPearls - NCBI BookshelfDocument14 pagesNeonatal Jaundice - StatPearls - NCBI BookshelfDhany karubuyNo ratings yet
- Pediatrics in Review33 (7) 291Document14 pagesPediatrics in Review33 (7) 291Barbara Helen Stanley100% (1)
- Neonatal JaundiceDocument77 pagesNeonatal Jaundiceodhiambovictor2424No ratings yet
- Neonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsDocument41 pagesNeonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsBegashawNo ratings yet
- Disease JaundiceDocument19 pagesDisease JaundiceMeena KoushalNo ratings yet
- Neonatal JaundiceDocument2 pagesNeonatal JaundiceyahyuNo ratings yet
- Neonatal Jaundice Assignment BCH 806Document11 pagesNeonatal Jaundice Assignment BCH 806ukosam10No ratings yet
- NIH Public Access: Author ManuscriptDocument10 pagesNIH Public Access: Author ManuscriptNofiyanty NicolasNo ratings yet
- UNIT HyperbilirubinemiaDocument17 pagesUNIT Hyperbilirubinemiaurmila dewanNo ratings yet
- Neonatal JaundiceDocument2 pagesNeonatal JaundiceyahyuNo ratings yet
- HyperbiliruminemiaDocument36 pagesHyperbiliruminemiamurugesh69No ratings yet
- Refer atDocument28 pagesRefer atAngga NuralamNo ratings yet
- Jaundice Clinical Manifestation and Pathophysiology A Review ArticleDocument3 pagesJaundice Clinical Manifestation and Pathophysiology A Review ArticleHany ZutanNo ratings yet
- Neonatal Jaundice NotesDocument5 pagesNeonatal Jaundice NotesEros CuestaNo ratings yet
- Jaundice: Newborn To Age 2 Months: Education GapDocument14 pagesJaundice: Newborn To Age 2 Months: Education GapRaul VillacresNo ratings yet
- Breast Milk Jaundice - JPG 2Document13 pagesBreast Milk Jaundice - JPG 2asmaaNo ratings yet
- Jaundice Newborn - 2Document15 pagesJaundice Newborn - 2Miratunnisa AzzahrahNo ratings yet
- Maternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyDocument6 pagesMaternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyEditor IJTSRDNo ratings yet
- Introduction (Hyperbilirubinemia)Document5 pagesIntroduction (Hyperbilirubinemia)bluewipesNo ratings yet
- 2 Jaundice in The NBDocument33 pages2 Jaundice in The NBCheru DugaseNo ratings yet
- Neonatal JaundiceDocument24 pagesNeonatal JaundiceChetan SekhriNo ratings yet
- Approach To Neonatal JaundiceDocument36 pagesApproach To Neonatal JaundiceDrMubashir ShaikhNo ratings yet
- HyperbilirubinemiaDocument11 pagesHyperbilirubinemianursereview100% (12)
- Crs Hiperbilirubinemia EricDocument30 pagesCrs Hiperbilirubinemia Ericerix firmando100% (1)
- Neonatal JaundiceDocument46 pagesNeonatal JaundiceEricson KipronoNo ratings yet
- Von Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVon Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Agriculture Technology: Importance of Agricultural TechnologyDocument5 pagesAgriculture Technology: Importance of Agricultural TechnologyEnixam ZulevtNo ratings yet
- Covid-19 Test Result Summary: Sars-Cov-2 Viral Rna - Not DetectedDocument1 pageCovid-19 Test Result Summary: Sars-Cov-2 Viral Rna - Not Detectedpogito ramosNo ratings yet
- Respiratory System Questions and Answers BiosDocument4 pagesRespiratory System Questions and Answers BiosChrispin MsofeNo ratings yet
- CBSE Class 12 Biotechnology WorksheetDocument3 pagesCBSE Class 12 Biotechnology WorksheetMia WulansaniNo ratings yet
- Physiology of Flowering Plant Molecular LevelDocument59 pagesPhysiology of Flowering Plant Molecular LevelDrRuby Ranjan SharmaNo ratings yet
- Epigenetics: Doug Brutlag Professor Emeritus of Biochemistry & Medicine Stanford University School of MedicineDocument54 pagesEpigenetics: Doug Brutlag Professor Emeritus of Biochemistry & Medicine Stanford University School of MedicineSathish KumarNo ratings yet
- Introduction of Natural ImmunityDocument4 pagesIntroduction of Natural ImmunitySamanthaNo ratings yet
- Resistance of The Body To Infection: Ii. Immunity and AllergyDocument25 pagesResistance of The Body To Infection: Ii. Immunity and AllergyVergel John ErciaNo ratings yet
- Full Download PDF of Kuby Immunology 8th Edition by Jenni Punt (Ebook PDF) All ChapterDocument43 pagesFull Download PDF of Kuby Immunology 8th Edition by Jenni Punt (Ebook PDF) All Chapteralhakosajie100% (17)
- Chapter 8Document53 pagesChapter 8contactrafiakhuramNo ratings yet
- Physics Answer+key 01jpa,+02jpaDocument5 pagesPhysics Answer+key 01jpa,+02jpaHardik TiwariNo ratings yet
- QP - Class IX - Science - Mid-Term - Assessment - 2021 - 22 - Oct - 21Document6 pagesQP - Class IX - Science - Mid-Term - Assessment - 2021 - 22 - Oct - 21Ashish GambhirNo ratings yet
- Definition.: The Human Digestive SystemDocument32 pagesDefinition.: The Human Digestive SystemEmma Joel OtaiNo ratings yet
- A Lead CompoundDocument2 pagesA Lead CompoundfikrifazNo ratings yet
- Chapter 43 ImmunologyDocument13 pagesChapter 43 Immunologyflux23No ratings yet
- Use of The PTXD Gene As A Portable Selectable Marker For Chloroplast Transformation in Chlamydomonas ReinhardtiiDocument9 pagesUse of The PTXD Gene As A Portable Selectable Marker For Chloroplast Transformation in Chlamydomonas ReinhardtiiJavier RodriguezNo ratings yet
- 8465 1F QP Synergy SpecimenSet 2 v1.0 PDFDocument34 pages8465 1F QP Synergy SpecimenSet 2 v1.0 PDFK's Gaming0% (1)
- Names For Trace Fossils A Uniform Approa PDFDocument22 pagesNames For Trace Fossils A Uniform Approa PDFcatfoulkrodNo ratings yet
- Journal Critique Technical MethodsDocument4 pagesJournal Critique Technical MethodsJam SalazarNo ratings yet
- Tertiary Protein StructuresDocument12 pagesTertiary Protein StructuresAbhi VermaNo ratings yet
- Mic 221 Slides and LessonDocument48 pagesMic 221 Slides and LessonNosibusiso KhaliphaNo ratings yet
- Mapping by Somatic Cell Hybrids Jan 28 2021Document22 pagesMapping by Somatic Cell Hybrids Jan 28 2021MuskanNo ratings yet
- Drug Approval System in IndonesiaDocument31 pagesDrug Approval System in IndonesiaYolanda XiaoNo ratings yet
- Advantages and Disadvantages of Prime Editing Compared With Wild Type CRISPRDocument3 pagesAdvantages and Disadvantages of Prime Editing Compared With Wild Type CRISPRCarlos Julio Nova LopezNo ratings yet
- Histology: The Study of TissuesDocument37 pagesHistology: The Study of TissuesHans Even Dela Cruz100% (1)
- Plant Water Relations - Absorption Transport and Control MechanismsDocument29 pagesPlant Water Relations - Absorption Transport and Control MechanismsJacoSkinfieldNo ratings yet
- Detailed Notes - Topic 8 Exchange and Transport in Animals - Edexcel Biology GCSEDocument10 pagesDetailed Notes - Topic 8 Exchange and Transport in Animals - Edexcel Biology GCSELei LavinaNo ratings yet
PPPP
PPPP
Uploaded by
Christy Ada IjeomaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PPPP
PPPP
Uploaded by
Christy Ada IjeomaCopyright:
Available Formats
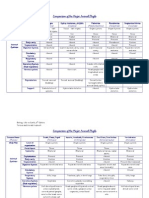
Neonatal Jaundice
Neonatal jaundice occurs when a baby has high levels of bilirubin in the blood. Bilirubin is a yellow substance that the body creates when it replaces old red blood cells. It is a very common condition worldwide occurring in up to 60% of term and 80% of preterm newborns in the first week of life (Slusher et al., 2004; Haque and Rahman, 2000). Jaundice is the most common condition that requires medical attention in newborns. The yellow coloration of the skin and sclera in newborns with jaundice is the result of accumulation of unconjugated bilirubin. In most infants, unconjugated hyperbilirubinemia reflects a normal transitional phenomenon. However, in some infants, serum bilirubin levels may excessively rise, which can be cause for concern because unconjugated bilirubin is neurotoxic and can cause death in newborns and lifelong neurologic sequelae in infants who survive (kernicterus). For these reasons, the presence of neonatal jaundice frequently results in diagnostic evaluation (Maisels & Gifford1986)
Neonatal physiologic jaundice results from simultaneous occurrence of the following 2 phenomena:
Bilirubin production is elevated because of increased breakdown of fetal erythrocytes. This is the result of the shortened lifespan of fetal erythrocytes and the higher erythrocyte mass in neonates.
Hepatic excretory capacity is low both because of low concentrations of the binding protein ligandin in the hepatocytes and because of low activity of glucuronyl transferase,
the enzyme responsible for binding bilirubin to glucuronic acid, thus making bilirubin water soluble (conjugation).
Bilirubin is produced in the reticuloendothelial system as the end product of heme catabolism and is formed through oxidation-reduction reactions. Approximately 75% of bilirubin is derived from hemoglobin, but degradation of myoglobin, cytochromes, and catalase also contributes. In the first oxidation step, biliverdin is formed from heme through the action of heme oxygenase, the rate-limiting step in the process, releasing iron and carbon monoxide. The iron is conserved for reuse, whereas carbon monoxide is excreted through the lungs and can be measured in the patient's breath to quantify bilirubin production.
Next, water-soluble biliverdin is reduced to bilirubin, which, because of the intramolecular hydrogen bonds, is almost insoluble in water in its most common isomeric form (bilirubin IX Z,Z). Because of its hydrophobic nature, unconjugated bilirubin is transported in the plasma tightly bound to albumin. Binding to other proteins and erythrocytes also occurs, but the physiologic role is probably limited. Binding of bilirubin to albumin increases postnatally with age and is reduced in infants who are ill.
The presence of endogenous and exogenous binding competitors, such as certain drugs, also decreases the binding affinity of albumin for bilirubin. A minute fraction of unconjugated bilirubin in serum is not bound to albumin. This free bilirubin is able to cross lipid-containing membranes, including the blood-brain barrier, leading to neurotoxicity. In fetal life, free bilirubin crosses the placenta, apparently by passive diffusion, and excretion of bilirubin from the fetus occurs primarily through the maternal organism.
When it reaches the liver, bilirubin is transported into liver cells, where it binds to ligandin. Uptake of bilirubin into hepatocytes increases with increasing ligandin concentrations. Ligandin concentrations are low at birth but rapidly increase over the first few weeks of life. Ligandin concentrations may be increased by the administration of pharmacologic agents such as phenobarbital.
Bilirubin is bound to glucuronic acid (conjugated) in the hepatocyte endoplasmic reticulum in a reaction catalyzed by uridine diphosphoglucuronyltransferase (UDPGT). Monoconjugates are formed first and predominate in the newborn. Diconjugates appear to be formed at the cell membrane and may require the presence of the UDPGT tetramer.
Bilirubin conjugation is biologically critical because it transforms a water-insoluble bilirubin molecule into a water-soluble molecule. Water-solubility allows conjugated bilirubin to be excreted into bile. UDPGT activity is low at birth but increases to adult values by age 4-8 weeks. In addition, certain drugs (phenobarbital, dexamethasone, clofibrate) can be administered to increase UDPGT activity.
Infants who have Gilbert syndrome or who are compound heterozygotes for the Gilbert promoter and structural mutations of the UDPGT1A1 coding region are at an increased risk of significant hyperbilirubinemia. Interactions between the Gilbert genotype and hemolytic anemias such as glucose-6-phosphatase dehydrogenase (G-6-PD) deficiency, hereditary spherocytosis, or ABO hemolytic disease also appear to increase the risk of severe neonatal jaundice.
Further, the observation of jaundice in some infants with hypertrophic pyloric stenosis may also be related to a Gilbert-type variant. Genetic polymorphism for the organic anion transporter
protein OATP-2 correlates with a 3-fold increased risk for developing marked neonatal jaundice. Combination of the OATP-2 gene polymorphism with a variant UDPGT1A1 gene further increases this risk to 22-fold. Studies also suggest that polymorphisms in the gene for glutathione-S-transferase (ligandin) may contribute to higher levels of total serum bilirubin.
Thus, some interindividual variations in the course and severity of neonatal jaundice may be explained genetically. As the impact of these genetic variants is more fully understood, development of a genetic test panel for risk of severe and/or prolonged neonatal jaundice may become feasible.
Once excreted into bile and transferred to the intestines, bilirubin is eventually reduced to colorless tetrapyrroles by microbes in the colon. However, some deconjugation occurs in the proximal small intestine through the action of B-glucuronidases located in the brush border. This unconjugated bilirubin can be reabsorbed into the circulation, increasing the total plasma bilirubin pool. This cycle of uptake, conjugation, excretion, deconjugation, and reabsorption is termed 'enterohepatic circulation'. The process may be extensive in the neonate, partly because nutrient intake is limited in the first days of life, prolonging the intestinal transit time.
In mother-infant dyads who are experiencing difficulties with the establishment of breast feeding, inadequate fluid and nutrient intake often leads to significant postnatal weight loss in the infant. Such infants have an increased risk of developing jaundice through increased enterohepatic circulation, as described above. This phenomenon is often referred to as breastfeeding jaundice and is different from the breast milk jaundice described below.
Certain factors present in the breast milk of some mothers may also contribute to increased enterohepatic circulation of bilirubin (breast milk jaundice). -glucuronidase may play a role by uncoupling bilirubin from its binding to glucuronic acid, thus making it available for reabsorption. Data suggest that the risk of breast milk jaundice is significantly increased in infants who have genetic polymorphisms in the coding sequences of the UDPGT1A1 or OATP2 genes. Although the mechanism that causes this phenomenon is not yet agreed on, evidence suggests that supplementation with certain breast milk substitutes may reduce the degree of breast milk jaundice (see Other therapies).
Neonatal jaundice, although a normal transitional phenomenon in most infants, can occasionally become more pronounced. Blood group incompatibilities (eg, Rh, ABO) may increase bilirubin production through increased hemolysis. Historically, Rh isoimmunization was an important cause of severe jaundice, often resulting in the development of kernicterus. Although this condition has become relatively rare in industrialized countries following the use of Rh prophylaxis in Rh-negative women, Rh isoimmunization remains common in developing countries.
Nonimmune hemolytic disorders (spherocytosis, G-6-PD deficiency) may also cause increased jaundice, and increased hemolysis appears to have been present in some of the infants reported to have developed kernicterus in the United States in the past 10-15 years. The possible interaction between such conditions and genetic variants of the Gilbert and UDPGT1A1 genes, as well as genetic variants of several other proteins and enzymes involved in bilirubin metabolism, is discussed above.
These discoveries also highlight the challenges involved in the common use of the terms physiologic jaundice and pathologic jaundice. Although physiologic jaundice is a helpful concept from a didactic perspective, applying it to an actual neonate with jaundice is more difficult.
Consider the following metaphor: Think of total serum bilirubin in neonatal jaundice as a mountain covered by a glacier. If a measurement of the height of the mountain is taken when standing on the summit, the amount of rock and the amount of ice that comprise this measurement is unclear. The same is true for many total serum bilirubin values obtained in neonatal jaundice. An underpinning of physiologic processes and pathological process (eg, Rhesus incompatibility) may clearly contribute to the measurement. However, how much of the measured total value comes from each of these components is unclear. Also, because genetic variants in bilirubin metabolism are only exceptionally pursued in the diagnostic work-up of infants with jaundice, their possible contribution to the measured total serum bilirubin is usually unknown.
You might also like
- TheQuestforTheCures 7EpisodeTranscriptsEbookDocument250 pagesTheQuestforTheCures 7EpisodeTranscriptsEbookciprian72100% (1)
- Nelson JaundiceDocument7 pagesNelson JaundiceJesly CharliesNo ratings yet
- Virginia Environmental Literacy Plan TemplateDocument8 pagesVirginia Environmental Literacy Plan TemplateVirginia Association for Environmental EducationNo ratings yet
- Biology Comparison of The Major Animal Phyla ChartDocument2 pagesBiology Comparison of The Major Animal Phyla Chart09temp100% (3)
- Bac GroundDocument6 pagesBac GroundRitu Ayu PutriNo ratings yet
- Neonatal JaundiceDocument30 pagesNeonatal JaundiceAnonymous Y3fqBduNo ratings yet
- Jaundice EnglishDocument5 pagesJaundice EnglishArinaManaSikanaNo ratings yet
- Neonatal JaundiceDocument4 pagesNeonatal JaundiceChristian Eduard de DiosNo ratings yet
- Overview#showall: March 04 2016Document32 pagesOverview#showall: March 04 2016viyolaazzahraNo ratings yet
- Referrence:: Glucose-6-Phosphatase Dehydrogenase (G-6-PD) DeficiencyDocument2 pagesReferrence:: Glucose-6-Phosphatase Dehydrogenase (G-6-PD) DeficiencyKim DeyNo ratings yet
- Causes: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekDocument7 pagesCauses: Neonatal Jaundice or Neonatal Hyperbilirubinemia, or Neonatal Icterus (From The GreekIzzah100% (1)
- Pathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornDocument45 pagesPathogenesis and Etiology of Unconjugated Hyperbilirubinemia in The NewbornJaner BanosNo ratings yet
- Consequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsDocument3 pagesConsequences of Hyperbilirubinemia:: Kernicterus Is The Major Consequence of Neonatal Hyperbilirubinemia. Although It IsAradhanaRamchandaniNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceGiska T PutriNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceAlya Afifa100% (1)
- Neonatal HandbookDocument11 pagesNeonatal HandbookJanua NavaretteNo ratings yet
- Neonatal JaundiceDocument48 pagesNeonatal JaundiceRemy MartinsNo ratings yet
- Neonatal JaundiceDocument18 pagesNeonatal JaundiceArinaManaSikanaNo ratings yet
- Breastmilk JaundiceDocument13 pagesBreastmilk JaundicenadiancupNo ratings yet
- 1 Core Concepts Bilirubin MetabolismDocument9 pages1 Core Concepts Bilirubin Metabolismlink0105No ratings yet
- Core Concepts Bilirrubin MetabolismDocument9 pagesCore Concepts Bilirrubin MetabolismAngelina ChunNo ratings yet
- Presentation and Duration of Neonatal JaundiceDocument5 pagesPresentation and Duration of Neonatal JaundiceRizki DaulayNo ratings yet
- Core Concepts:: Bilirubin MetabolismDocument9 pagesCore Concepts:: Bilirubin MetabolismManasye AlanNo ratings yet
- 17 - Neonatal Jaundice MCH 410 2012Document32 pages17 - Neonatal Jaundice MCH 410 2012frederickmwansa22No ratings yet
- IctericiaDocument19 pagesIctericiadavid pinedaNo ratings yet
- Jurnal NHDocument14 pagesJurnal NHShintya DewiNo ratings yet
- Icterus, HiperbilirubinemiaDocument3 pagesIcterus, HiperbilirubinemiameidyNo ratings yet
- Difference Between Physiologic Jaundice and Pathologic JaundiceDocument2 pagesDifference Between Physiologic Jaundice and Pathologic JaundiceNurulAqilahZulkifli100% (4)
- Hiperbilirrubinemia DirectaDocument9 pagesHiperbilirrubinemia DirectaRonal Cadillo MedinaNo ratings yet
- Neonatal Jaundice DR - MaslianiDocument58 pagesNeonatal Jaundice DR - MaslianiHengky HanggaraNo ratings yet
- Ikterus NeonatorumDocument10 pagesIkterus NeonatorumHerryanto AgustriadiNo ratings yet
- Neonatal Jaundice: AuthorsDocument9 pagesNeonatal Jaundice: AuthorsRam Kumar ShresthaNo ratings yet
- Neonatal Hyperbilirubinemia and JaundiceDocument8 pagesNeonatal Hyperbilirubinemia and JaundiceAndreea GeorgianaNo ratings yet
- HyperbilirubinemiaDocument48 pagesHyperbilirubinemiaEdrik Luke Pialago100% (2)
- ) Jaundice PDFDocument4 pages) Jaundice PDFAzzNo ratings yet
- Neonatal JaundiceDocument10 pagesNeonatal JaundiceLGK maoreNo ratings yet
- Neonatal Jaundice - StatPearls - NCBI BookshelfDocument14 pagesNeonatal Jaundice - StatPearls - NCBI BookshelfDhany karubuyNo ratings yet
- Pediatrics in Review33 (7) 291Document14 pagesPediatrics in Review33 (7) 291Barbara Helen Stanley100% (1)
- Neonatal JaundiceDocument77 pagesNeonatal Jaundiceodhiambovictor2424No ratings yet
- Neonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsDocument41 pagesNeonatal Hyperbilirubinemia: Mahlet Abayneh Assistant Professor of PediatricsBegashawNo ratings yet
- Disease JaundiceDocument19 pagesDisease JaundiceMeena KoushalNo ratings yet
- Neonatal JaundiceDocument2 pagesNeonatal JaundiceyahyuNo ratings yet
- Neonatal Jaundice Assignment BCH 806Document11 pagesNeonatal Jaundice Assignment BCH 806ukosam10No ratings yet
- NIH Public Access: Author ManuscriptDocument10 pagesNIH Public Access: Author ManuscriptNofiyanty NicolasNo ratings yet
- UNIT HyperbilirubinemiaDocument17 pagesUNIT Hyperbilirubinemiaurmila dewanNo ratings yet
- Neonatal JaundiceDocument2 pagesNeonatal JaundiceyahyuNo ratings yet
- HyperbiliruminemiaDocument36 pagesHyperbiliruminemiamurugesh69No ratings yet
- Refer atDocument28 pagesRefer atAngga NuralamNo ratings yet
- Jaundice Clinical Manifestation and Pathophysiology A Review ArticleDocument3 pagesJaundice Clinical Manifestation and Pathophysiology A Review ArticleHany ZutanNo ratings yet
- Neonatal Jaundice NotesDocument5 pagesNeonatal Jaundice NotesEros CuestaNo ratings yet
- Jaundice: Newborn To Age 2 Months: Education GapDocument14 pagesJaundice: Newborn To Age 2 Months: Education GapRaul VillacresNo ratings yet
- Breast Milk Jaundice - JPG 2Document13 pagesBreast Milk Jaundice - JPG 2asmaaNo ratings yet
- Jaundice Newborn - 2Document15 pagesJaundice Newborn - 2Miratunnisa AzzahrahNo ratings yet
- Maternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyDocument6 pagesMaternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyEditor IJTSRDNo ratings yet
- Introduction (Hyperbilirubinemia)Document5 pagesIntroduction (Hyperbilirubinemia)bluewipesNo ratings yet
- 2 Jaundice in The NBDocument33 pages2 Jaundice in The NBCheru DugaseNo ratings yet
- Neonatal JaundiceDocument24 pagesNeonatal JaundiceChetan SekhriNo ratings yet
- Approach To Neonatal JaundiceDocument36 pagesApproach To Neonatal JaundiceDrMubashir ShaikhNo ratings yet
- HyperbilirubinemiaDocument11 pagesHyperbilirubinemianursereview100% (12)
- Crs Hiperbilirubinemia EricDocument30 pagesCrs Hiperbilirubinemia Ericerix firmando100% (1)
- Neonatal JaundiceDocument46 pagesNeonatal JaundiceEricson KipronoNo ratings yet
- Von Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandVon Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Agriculture Technology: Importance of Agricultural TechnologyDocument5 pagesAgriculture Technology: Importance of Agricultural TechnologyEnixam ZulevtNo ratings yet
- Covid-19 Test Result Summary: Sars-Cov-2 Viral Rna - Not DetectedDocument1 pageCovid-19 Test Result Summary: Sars-Cov-2 Viral Rna - Not Detectedpogito ramosNo ratings yet
- Respiratory System Questions and Answers BiosDocument4 pagesRespiratory System Questions and Answers BiosChrispin MsofeNo ratings yet
- CBSE Class 12 Biotechnology WorksheetDocument3 pagesCBSE Class 12 Biotechnology WorksheetMia WulansaniNo ratings yet
- Physiology of Flowering Plant Molecular LevelDocument59 pagesPhysiology of Flowering Plant Molecular LevelDrRuby Ranjan SharmaNo ratings yet
- Epigenetics: Doug Brutlag Professor Emeritus of Biochemistry & Medicine Stanford University School of MedicineDocument54 pagesEpigenetics: Doug Brutlag Professor Emeritus of Biochemistry & Medicine Stanford University School of MedicineSathish KumarNo ratings yet
- Introduction of Natural ImmunityDocument4 pagesIntroduction of Natural ImmunitySamanthaNo ratings yet
- Resistance of The Body To Infection: Ii. Immunity and AllergyDocument25 pagesResistance of The Body To Infection: Ii. Immunity and AllergyVergel John ErciaNo ratings yet
- Full Download PDF of Kuby Immunology 8th Edition by Jenni Punt (Ebook PDF) All ChapterDocument43 pagesFull Download PDF of Kuby Immunology 8th Edition by Jenni Punt (Ebook PDF) All Chapteralhakosajie100% (17)
- Chapter 8Document53 pagesChapter 8contactrafiakhuramNo ratings yet
- Physics Answer+key 01jpa,+02jpaDocument5 pagesPhysics Answer+key 01jpa,+02jpaHardik TiwariNo ratings yet
- QP - Class IX - Science - Mid-Term - Assessment - 2021 - 22 - Oct - 21Document6 pagesQP - Class IX - Science - Mid-Term - Assessment - 2021 - 22 - Oct - 21Ashish GambhirNo ratings yet
- Definition.: The Human Digestive SystemDocument32 pagesDefinition.: The Human Digestive SystemEmma Joel OtaiNo ratings yet
- A Lead CompoundDocument2 pagesA Lead CompoundfikrifazNo ratings yet
- Chapter 43 ImmunologyDocument13 pagesChapter 43 Immunologyflux23No ratings yet
- Use of The PTXD Gene As A Portable Selectable Marker For Chloroplast Transformation in Chlamydomonas ReinhardtiiDocument9 pagesUse of The PTXD Gene As A Portable Selectable Marker For Chloroplast Transformation in Chlamydomonas ReinhardtiiJavier RodriguezNo ratings yet
- 8465 1F QP Synergy SpecimenSet 2 v1.0 PDFDocument34 pages8465 1F QP Synergy SpecimenSet 2 v1.0 PDFK's Gaming0% (1)
- Names For Trace Fossils A Uniform Approa PDFDocument22 pagesNames For Trace Fossils A Uniform Approa PDFcatfoulkrodNo ratings yet
- Journal Critique Technical MethodsDocument4 pagesJournal Critique Technical MethodsJam SalazarNo ratings yet
- Tertiary Protein StructuresDocument12 pagesTertiary Protein StructuresAbhi VermaNo ratings yet
- Mic 221 Slides and LessonDocument48 pagesMic 221 Slides and LessonNosibusiso KhaliphaNo ratings yet
- Mapping by Somatic Cell Hybrids Jan 28 2021Document22 pagesMapping by Somatic Cell Hybrids Jan 28 2021MuskanNo ratings yet
- Drug Approval System in IndonesiaDocument31 pagesDrug Approval System in IndonesiaYolanda XiaoNo ratings yet
- Advantages and Disadvantages of Prime Editing Compared With Wild Type CRISPRDocument3 pagesAdvantages and Disadvantages of Prime Editing Compared With Wild Type CRISPRCarlos Julio Nova LopezNo ratings yet
- Histology: The Study of TissuesDocument37 pagesHistology: The Study of TissuesHans Even Dela Cruz100% (1)
- Plant Water Relations - Absorption Transport and Control MechanismsDocument29 pagesPlant Water Relations - Absorption Transport and Control MechanismsJacoSkinfieldNo ratings yet
- Detailed Notes - Topic 8 Exchange and Transport in Animals - Edexcel Biology GCSEDocument10 pagesDetailed Notes - Topic 8 Exchange and Transport in Animals - Edexcel Biology GCSELei LavinaNo ratings yet