Professional Documents
Culture Documents
An Update On Cancer-And Chemotherapy - Related Cognitive Dysfunction: Current Status
An Update On Cancer-And Chemotherapy - Related Cognitive Dysfunction: Current Status
Uploaded by
gorklanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An Update On Cancer-And Chemotherapy - Related Cognitive Dysfunction: Current Status
An Update On Cancer-And Chemotherapy - Related Cognitive Dysfunction: Current Status
Uploaded by
gorklanCopyright:
Available Formats
An Update on Cancer- and ChemotherapyRelated Cognitive Dysfunction: Current Status
Michelle C. Janelsins,a Sadhna Kohli,b Supriya G. Mohile,c Kenneth Usuki,a Tim A. Ahles,d and Gary R. Morrowa,e
The purpose of this review is to summarize the current literature on the effects of cancer treatmentrelated cognitive difculties, with a focus on the effects of chemotherapy. Numerous patients have cognitive difculties during and after cancer treatments and, for some, these effects last years after treatment. We do not yet fully understand which factors increase susceptibility to cognitive difculties during treatment and which cause persistent problems. We review possible contributors, including genetic and biological factors. Mostly we focus is on cognitive effects of adjuvant chemotherapy for breast cancer; however, cognitive effects of chemotherapy on the elderly and brain tumor patients are also discussed. Semin Oncol 38:431-438 2011 Elsevier Inc. All rights reserved.
STATE OF THE FIELD
p to 75% of cancer patients experience cognitive impairment (eg, problems with memory, executive functioning, and attention) during or after treatment of their cancer. For many (up to 35%), this persists for months or years following treatment.1 6 With more than 11 million cancer survivors in the United States,7 up to 3.9 million individuals may be living with long-lasting cognitive difculties from cancer and cancer treatments. This is an important area of concern, because these effects could inuence adherence to treatments and lead to long-term impairment. Cognitive decits that occur from cancer or its treatment vary and may be subtle or dramatic, temporary or permanent, and stable or progressive.8 We highlight
recent work in cancer- and chemotherapy-related cognitive difculties and explore possible mechanisms.
SUMMARY OF CLINICAL RESEARCH LITERATURE
Some cognitive problems in those who receive chemotherapy are more severe than in those who only receive locoregional therapy (eg, radiation, surgery).9,10 Cognitive problems with chemotherapy can negatively impact activities of daily living such as (1) work performance,5 (2) access to medical and other health services, and (3) caring for and socially interacting with family members.11 Systematic research to understand cognitive difculties with chemotherapy was rst reported during the mid 1990s to early 2000s2 4,12; early studies often did not include pretreatment assessment data and/or were cross-sectional in design. The lack of pretreatment data was most likely due to difculty obtaining such information from newly diagnosed patients. Studies over the past decade have incorporated pretreatment assessments of cognitive function. The importance of a pretreatment baseline was evidenced in a study5 of the effects of 5-uorouracil, doxorubicin, and cyclophosphamide (FAC) chemotherapy on cognitive function in breast cancer. This was one of the rst prospective, longitudinal studies to assess cognitive function with pretreatment and post-treatment cognitive measures. There were no overall mean differences in cognitive function between patients and controls (normative data). Within-subject analyses showed that 61% had cognitive declines in learning, attention, and processing speed. If the pretreatment assessment had been 431
aDepartment
of Radiation Oncology, University of Rochester Medical Center, Rochester, NY. bDepartment of Oncology, Mayo Clinic, Rochester, MN. cDepartment of Medicine, University of Rochester Medical Center, Rochester, NY. dDepartment of Psychiatry and Behavioral Sciences, Memorial SloanKettering Cancer Center, New York, NY. eDepartment of Psychiatry, University of Rochester Medical Center, Rochester, NY. The authors do not have any nancial disclosures or conicts of interest. Partially supported by NCI R25CA10618. Address correspondence to Michelle C. Janelsins, PhD, Research Assistant Professor, University of Rochester Medical Center, James P. Wilmot Cancer Center, Department of Radiation Oncology, Rochester, NY 14642. E-mail: michelle_janelsins@urmc.rochester.edu 0270-9295/ - see front matter 2011 Elsevier Inc. All rights reserved. doi:10.1053/j.seminoncol.2011.03.014
Seminars in Oncology, Vol 38, No 3, June 2011, pp 431-438
432
M.C. Janlesins et al
unavailable, 46% would not have had detectable cognitive impairments (because their post-treatment assessment scores were normal). This is extremely important since cognitive dysfunction can be subtle. If a patient scores well on a cognitive test before chemotherapy and less well after treatment (but that score is still within the normal range), the decline may nevertheless represent a clinically signicant difference. Approximately 10 additional longitudinal studies have investigated cancer- and/or treatment-related cognitive difculties; many treatment studies assessed the effects of chemotherapy and used standard neuropsychological assessments.10,1323 In all, 12% to 82% of patients had cognitive difculties in the domains of executive function, memory, psychomotor speed, and attention. Not all studies revealed signicant changes in all domains; those in memory, executive function, processing speed, and attention appear most frequent. Additionally, many studies had small numbers and were not powered to test multiple cognitive domains. These studies used a variety of cognitive assessments and control groups, and most investigated patients on various treatment regimens. One recent study compared patients exposed to chemotherapy, those not exposed, and a healthy control group; those exposed to chemotherapy had the greatest decits.21 Several studies have shown cognitive decits in cancer patients before chemotherapy.5,22 For example, in one study 33% of patients had cognitive difculties in verbal learning and memory prior to chemotherapy.5 Another recent study revealed that 23% of women being treated for breast cancer had difculty before chemotherapy.22 These could be related to psychological variables related to cancer diagnosis (eg, stress, anxiety, depression) or to other factors (eg, cognitive reserve). More research is needed to explicitly understand factors that lead to cognitive difculties before and during treatment, and to understand those that contribute to long-lasting impairment. Most studies of chemotherapy-related cognitive difculties have focused on breast cancer. Longitudinal studies are needed in other disease groups to understand whether cognitive difculties are more or less severe in these conditions. For example, in a crosssectional study,3 breast and lymphoma patients showed long-term problems; however, no large prospective study in lymphoma has been conducted to conrm these results. More work is needed in well-powered long-term observational studies to understand the course and severity of cognitive difculties, and possible mechanisms of action.
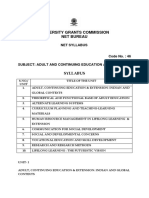
Figure 1. Possible contributors to cognitive difculties in cancer patients. Multiple factors can contribute to cognitive difculties in cancer patients. Physiological factors, such as the patients genetic make-up and hormone levels, and the inammatory response to cancer treatments, also may cause cognitive difculties. Some also can be psychological factors such as anxiety, depression, and stress, which increase vulnerability to development of cognitive difculties. Bolded topics are discussed within this review.
nisms have been proposed (Figure 1). Assessment of various biological factors (eg, inammatory markers, genetic markers, and brain imaging) may help identify high-risk groups for cognitive difculties or those at highest risk for persistent long-term effects. Although we currently have no treatments for cognitive difculties in cancer patients, identifying biological markers related to cognitive function would enable us to understand possible mechanisms and eventually develop successful interventions.
Brain Volume, Activity, and Metabolism
Subtle cognitive changes pose unique challenges to detection and management. First, the cause may not be apparent, and the impairments not evaluable with standard, objective neuropsychological measures. Second, subtle cognitive changes may be confounded by other problems commonly associated with cancer and its treatment, like depression, anxiety, and fatigue. To develop prophylactic interventions, we must understand the mechanisms behind the effects of treatment on cognition. We need to use every tool at our disposal, not only to document the extent of the cognitive changes via neuropsychological testing but also to probe changes in brain volume, metabolic status, and CNS activity following treatment. Documenting these changes is possible with neuroimaging techniques. These include computerized tomography (CT), single-photon emission-computed tomography (SPECT), positron emission tomography (PET), and magnetic resonance imaging (MRI). The latter two are particularly powerful because they allow one to assess metabolic activity (PET via radiolabeling and MRI via various spectroscopic techniques). MRI has particular value
MECHANISMS
We are far from understanding the underlying molecular mechanisms that contribute to cognitive difculties. Various biological and psychological mecha-
Cancer and chemotherapy-related cognitive dysfunction
433
because of the range of techniques available to probe brain anatomy and physiology. These include highresolution anatomical images, which allow accurate measurement of therapy-induced changes in gray and white matter volumes. Functional MRI measures areas of brain activation during stimuli such as a motor task or neuropsychological assessment. Diffusion MRI allows measurements of the diffusivity of water in the brain. Spectroscopic MRI provides information about the biochemical processes in the brain. Finally, because it does not use ionizing radiation, MRI can be repeated on the same individual to assess short- or long-term longitudinal changes. Although similar studies can be done with PET, they are limited by dose exposure guidelines and may not be possible at frequent intervals. The application of any of the neuroimaging techniques, but particularly the combination of MRI techniques, will prove useful in elucidating the structural, metabolic, and functional consequences of cancer and cancer therapies. Neuroimaging techniques have matured and are readily available in most clinical settings. Thus, future studies of the effects of cancer therapies on cognition should include neuroimaging, as well as conventional neuropsychological testing, to test hypotheses about the fundamental processes involved in the cognitive dysfunction following therapy. Preliminary work24 showed reductions in gray matter volume of frontal and temporal brain regions over the course of chemotherapy with partial recovery after treatment; these reductions were not seen in patients not exposed to chemotherapy or in healthy controls. These data temporally coincide with functional changes in neurocognitive assessment. Neuroimaging studies would also determine whether patients use compensatory mechanisms to enhance performance on neuropsychological testing even though they are aware that their function is worse than before treatment. Evidence for this hypothesis may be the lack of correlation between self-report and performance on neuropsychological testing.25 Preliminary imaging work has demonstrated by functional MRI that a patient diagnosed with breast cancer receiving chemotherapy had to work harder to complete a cognitive task than her twin sister who did not have cancer.26
for Hodgkins disease.33 In breast cancer patients receiving paclitaxel, levels of IL-6 increased 3 days after treatment compared to pretreatment but not in those who received a combination of uorouracil, cyclophosphamide, and methotrexate.34 Signicant changes in markers of endothelial and platelet activation were found in breast cancer on anthracycline-based treatment, further supporting the hypothesis that inammation occurs as a result of chemotherapy.35 Increased levels of IL-6 have been associated with poorer executive function, whereas higher levels of IL-8 were associated with better memory performance in patients with acute myelogenous leukemia and myelodysplastic syndrome prior to treatment.36 Another study found a trend between cytokine levels and cognitive performance in breast cancer.37 The investigators are currently assessing cytokine levels in relationship to cognitive function (via neuropsychological and computerized tests) in an ongoing observational study of cognitive function in colorectal cancer.38 Further clarication of the role of cytokines, chemokines, and other immune factors on cognitive function in cancer is needed. Large-scale observational studies that correlate changes in cytokines and chemokines with those in cognitive function should help clarify the association between inammation and cognitive function in cancer patients on different chemotherapy regimens.
Genetic Contributors
Only a subgroup of breast cancer survivors may experience long-term changes in cognitive ability. Several genome-wide association studies have identied single-nucleotide polymorphisms (SNPs) in genes in multiple signaling pathways (ie, inammation, dopamine, DNA repair, oxidative stress) perhaps related to cognitive decline in normal aging, Alzheimers disease and other syndromes with cognitive decline.39 41 Therefore, genetic variation related to cognitive function may be associated with increased risk for long-term cognitive changes.32 Two studies examined the association between apolipoprotein E (APOE) and catechol-o-methyltransferase (COMT) genotypes and cognitive function in cancer survivors.42,43 Apolipoprotein E (ApoE) is a complex glycolipoprotein that facilitates uptake, transport, and distribution of lipids. It appears to play an important role in neuronal repair and plasticity after injury.44 The human E4 allele has been associated with a variety of disorders with prominent cognitive dysfunction. These include otherwise normal patients with memory complaints, Alzheimers disease, and poor outcomes in stroke and traumatic brain injury.45 Cancer survivors with at least one E4 allele scored signicantly lower in the visual memory and spatial ability domains, with a trend to score lower in executive function compared to survivors who did not carry an E4 allele.42
Cytokines and Other Inammation Markers
Although increased inammatory markers are associated with cognitive difculties in numerous neurodegenerative diseases and cognitive disorders,2731 there is little information about the relationship of inammatory responses to cognitive function in cancer. Elevated peripheral levels of pro-inammatory cytokines may be related to cognitive problems.32 Chemotherapy has been associated with increased levels of pro-inammatory cytokines (eg, interleukin [IL]-1 ) in those treated
434
M.C. Janlesins et al
The COMT Val158Met SNP has been associated with dopamine levels in the prefrontal cortex. COMT-Val carriers metabolize dopamine more rapidly, with less availability of a neurotransmitter critical for cognitive function. COMT-Val carriers perform more poorly on tests of attention and executive function compared to COMT-Met carriers.45 Breast cancer survivors who were COMT-Val carriers and exposed to chemotherapy performed more poorly on tests of attention than healthy controls who were also carriers.43 These studies support the hypothesis that genetic factors increase vulnerability to cognitive changes with cancer treatments. Examination of other neural repair/ plasticity genes and neurotransmitter activity genes, and those associated chemotherapy-induced cognitive change such as DNA damage/repair (eg, recombination 11 homolog A46) or blood-brain barrier damage may reveal important associations with post-treatment cognitive function.32 Finally, increasing interest in epigenetics (changes in gene activity without any in DNA structure) and cognitive function may lead to examination of chemotherapy-induced epigenetic changes associated with cancer-treatment related cognitive impairment.47
The differential diagnosis of the type and extent of impairment is important in treatment planning and prognosis.53 Cognitive disorders such as dementia limit life expectancy and can affect whether patients should receive adjuvant therapy. Cognitive disorders interfere with medication compliance and consent to treatment and increase caregiver burden. Cognitively impaired persons receive less denitive cancer care than others.54 56 Cognitive disorders in older patients present prior to cancer treatment are often underdiagnosed without screening. Six percent to 10% of people age 65 years suffer from dementia. Prevalence approaches 50% in community-living populations older than 80 years.57 Cognitive impairment is associated with an increased risk for progression to dementia, with progression rates of 10% to 15% per year compared with 1% to 2.5% in the cognitively intact.58 60 One fth of geriatric cancer patients screen positively for cognitive disorders in an academic setting.61,62
Chemotherapy
Investigators have prospectively studied the impact of cancer treatment on cognitive function in older patients with breast cancer, following complaints of memory changes and impaired concentration. The data are still limited regarding the impact of cancer treatment on an older persons cognition. In one longitudinal prospective study of older patients with breast cancer, 51% of 45 evaluable patients perceived a decline in cognitive function after 6 months of chemotherapy.63 Other studies demonstrated no signicant change in Mini-Mental Status Exam (MMSE) scores after chemotherapy or hormonal therapy over a short time period.64,65 In one longitudinal study, 28 older women with breast cancer scheduled for adjuvant chemotherapy underwent neuropsychological testing and a comprehensive geriatric assessment (CGA) before therapy and 6 months after completion.14 Thirty-nine percent scored 2 standard deviations below normative data at 6 months compared to their baseline neuropsychological test scores.14 Exploratory analyses of longitudinal CGA results demonstrated no changes in functional status, comorbidity, or depression scores.66 At the same time, one population-based study suggests that women with breast cancer who receive chemotherapy have a higher likelihood of dementia after long-term follow-up.67 More large, prospective, long-term studies are necessary to denitively assess the impact of breast cancer treatment on the cognitive function of older patients.
Menopausal Status and Hormonal Therapies
Most evidence for cognitive difculties in cancer patients and survivors is attributed to chemotherapy. The literature on hormonal balance and cognition suggests that menopausal status and endocrine therapy can also inuence cognitive function in cancer. For example, the transition from pre- to post-menopausal status is associated with alterations in cytokines such as IL-648 and cognitive difculties in learning and memory.49 Case studies in cancer reveal that cognitive difculties can vary among patients who received the same course of chemotherapy; this could be related to menopausal status.50 Breast cancer patients who received chemotherapy and tamoxifen have greater difculty than those who received chemotherapy alone.25 Another cross-sectional study assessing tamoxifen in premenopausal breast cancer patients compared to healthy controls found greater difculty in visual and verbal memory and processing speed.51 One prospective study found deterioration in verbal memory and executive function in post-menopausal patients taking tamoxifen for 1 year (but not in those taking the aromatase inhibitor, exemestane, compared to healthy controls).52 Larger studies are needed to conrm these results and to address the combined effects of chemotherapy and endocrine therapy on cognitive function in cancer.
Hormonal Therapy TREATMENT-RELATED COGNITIVE IMPAIRMENT IN ELDERLY CANCER PATIENTS
Impaired cognitive function is a common complaint among older patients presenting for medical treatment. The cognitive effects of hormonal therapy with androgen deprivation therapy (ADT) in men with prostate cancer have conicting results due to small sample size, short observation time, or perhaps a heteroge-
Cancer and chemotherapy-related cognitive dysfunction
435
neous effect of ADT.68 Several studies have evaluated ADT on the cognition of men with prostate cancer but few have described the baseline prevalence of cognitive impairment. One study examined the cognitive function of 25 men, ages 49 to 75, following 12 months of androgen deprivation.69 They found improvements in visual and semantic memory. While not signicantly different, the range on the MMSE of the treatment group at baseline was 2129. This suggested that some had signicant cognitive impairment prior to treatment. A study of outcomes at 1 year found cognitive losses in those undergoing hormonal treatment compared to controls.70 They also noted that the community control group performed signicantly better than the prostate cancer group at baseline. This suggests that some may have cognitive impairment prior to treatment, which may impact overall results. In another study of 32 patients (median age, 71 years), 45% scored 1.5 standard deviations below the mean on 2 neuropsychological measures at baseline.71 Within exploratory analyses, those who scored below expectation at baseline displayed no change in cognition, while people with average or better scores at baseline displayed improvements in visuospatial planning and timed tests of phonemic uency. This again suggests that a subset have cognitive impairment before treatment that may impact overall results. Clinical suspicion of dementia is not as sensitive as available screening tools.72 A cognitive assessment tool (eg, Blessed Dementia Rating Scale,73 MMSE,74 MiniCog,75 and Short Portable Mental Status Questionnaire) for older cancer patients should screen for baseline impairment and follow effects of therapy on cognitive function. The purpose of screening is to assess cognitive capacity and stratify risk; abnormal scores should trigger a comprehensive work-up with cognitive specialists. Unfortunately, these tools have not yet demonstrated the ability to detect treatment-induced changes in cognition. A more detailed neuropsychological evaluation is needed to accomplish this goal.63
further understand the effects that chemotherapy and other treatments have on intact brain structures and cognitive function.
ANIMAL STUDIES
Animal models are especially important to the cancer and cognition eld. It is not easy to assess molecular changes in the human brain. While parallel ndings between animal and human experiments do not establish equivalence, animal models may inform hypotheses relating to the clinical condition. Experiments in animal models can usually be done much more quickly than parallel clinical studies and allow for many more aspects of a research question to be addressed. Furthermore, addressing a research question in an animal model is usually much less expensive than the same research question in a human study, assuming that study in a human is even technologically possible. Animal studies have found that chemotherapy agents can negatively affect memory behavior in mice,77 80 likely due to reductions in adult neurogenesis.80 83 Mice exposed to doxorubicin had increased cortical and hippocampal levels of tumor necrosis factor-alpha (TNF- ), hyperactivation of microglia, induction of oxidative stress and mitochondrial dysfunction, and increased neural cell death. This was despite the fact that doxorubicin was not detected in the brains of these mice.84,85 These studies suggest that chemotherapy causes neurotoxicity within the brain and that inammation may be a mediator of cognitive difculties by reducing neural transmission. Future work in animal models will provide more mechanistic insight and allow testing of interventions for cognitive impairment.
SUMMARY
Cancer- and chemotherapy-related cognitive impairment is an important clinical problem that negatively impacts quality of life for many individuals during treatment and post-treatment. We have reviewed various topics relevant to the cognition and cancer eld and highlighted important areas for future research. Understanding the factors that lead to cognitive impairments from chemotherapy and other cancer treatments will allow us to better understand how to educate patients about these difculties and ultimately how to treat them.
TREATMENT-RELATED COGNITIVE IMPAIRMENT IN BRAIN TUMOR PATIENTS
In addition to the neurological complications brain tumors themselves impose, the treatments are often associated with harmful effects on the CNS that can lead to cognitive impairments. These patients may experience a broad array of both acute and late toxicities, resulting both from direct toxic effects on the nervous system and indirect dysfunction (eg, metabolic dysregulation, cerebrovascular disorders). Toxicity from brain tumor therapy may range from focal neurological decits to generalized neurological syndromes. These frequently include fatigue and cognitive impairment, including decreased executive function.76 Since patients with brain tumors live longer, it is important to
REFERENCES
1. Janelsins M, Roscoe JA, Jean-Pierre P, Morrow GR. Cognitive functioning in breast cancer patients during and following chemotherapy [abstract]. Supplement to American Society of Clinical Oncology. 2009:47. 2. Brezden CB, Phillips KA, Abdolell M, Bunston T, Tannock IF. Cognitive function in breast cancer patients
436
M.C. Janlesins et al
3.
4.
5.
6.
7. 8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
receiving adjuvant chemotherapy. J Clin Oncol. 2000; 18:2695701. Ahles TA, Saykin AJ, Furstenberg CT, et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol. 2002;20:48593. van Dam FS, Schagen SB, Muller MJ, et al. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst. 1998;90: 210 8. Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100:22929. Yamada TH, Denburg NL, Beglinger LJ, Schultz SK. Neuropsychological outcomes of older breast cancer survivors: cognitive features ten or more years after chemotherapy. J Neuropsychiatry Clin Neurosci. 2010;22: 48-54. Cancer facts and gures. Atlanta, GA: American Cancer Society; 2009. Schagen SB, Hamburger HL, Muller MJ, Boogerd W, van Dam FS. Neurophysiological evaluation of late effects of adjuvant high-dose chemotherapy on cognitive function. J Neurooncol. 2001;51:159 65. Kohli S, Griggs JJ, Roscoe JA, et al. Self-reported cognitive impairments in patients with cancer. J Oncol Practice. 2007;3:54 9. Quesnel C, Savard J, Ivers H. Cognitive impairments associated with breast cancer treatments: results from a longitudinal study. Breast Cancer Res Treat. 2009;116: 11323. Reid-Arndt SA, Yee A, Perry MC, Hsieh C. Cognitive and psychological factors associated with early posttreatment functional outcomes in breast cancer survivors. J Psychosoc Oncol. 2009;27:41534. Wieneke MH, Dienst ER. Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psychooncology. 1995;4:61 6. Schagen SB, Muller MJ, Boogerd W, Mellenbergh GJ, van Dam FS. Change in cognitive function after chemotherapy: a prospective longitudinal study in breast cancer patients. J Natl Cancer Inst. 2006;98:17425. Hurria A, Rosen C, Hudis C. Cognitive function of older patients receiving adjuvant chemotherapy for breast cancer: a pilot prospective longitudinal study. J Am Geriatr Soc. 2006;54:92531. Collins B, Mackenzie J, Stewart A, Bielajew C, Verma S. Cognitive effects of chemotherapy in post-menopausal breast cancer patients 1 year after treatment. Psychooncology. 2009;18:134 43. Hermelink K, Untch M, Lux MP, et al. Cognitive function during neoadjuvant chemotherapy for breast cancer: results of a prospective, multicenter, longitudinal study. Cancer. 2007;109:190513. Jenkins V, Shilling V, Deutsch G, et al. A 3-year prospective study of the effects of adjuvant treatments on cognition in women with early stage breast cancer. Br J Cancer. 2006;94:828 34.
18. Ahles TA, Saykin AJ, McDonald BC, et al. Cognitive function in breast cancer patients prior to adjuvant treatment. Breast Cancer Res Treat. 2008;110:14352. 19. Stewart A, Collins B, Mackenzie J, Tomiak E, Verma S, Bielajew C. The cognitive effects of adjuvant chemotherapy in early stage breast cancer: a prospective study. Psychooncology. 2008;17:12230. 20. Ouimet LA, Stewart A, Collins B, Schindler D, Bielajew C. Measuring neuropsychological change following breast cancer treatment: an analysis of statistical models. J Clin Exp Neuropsychol. 2009;31:73 89. 21. Ahles TA, Saykin AJ, McDonald BC, et al. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol. 2010 Oct 10;28:4434 40. 22. Jansen CE, Cooper BA, Dodd MJ, Miaskowski CA. A prospective longitudinal study of chemotherapy-induced cognitive changes in breast cancer patients. Support Care Cancer. 2010 Sep 5. [Epub ahead of print] 23. Wefel JS, Saleeba AK, Buzdar AU, Meyers CA. Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer. 2010;116: 3348-56. 24. McDonald BC, Conroy SK, Ahles TA, West JD, Saykin AJ. Gray matter reduction associated with systemic chemotherapy for breast cancer: a prospective MRI study. Breast Cancer Res Treat. 2010;123:819 28. 25. Castellon SA, Ganz PA, Bower JE, Petersen L, Abraham L, Greendale GA. Neurocognitive performance in breast cancer survivors exposed to adjuvant chemotherapy and tamoxifen. J Clin Exp Neuropsychol. 2004;26:955 69. 26. Ferguson RJ, McDonald BC, Saykin AJ, Ahles TA. Brain structure and function differences in monozygotic twins: possible effects of breast cancer chemotherapy. J Clin Oncol. 2007;25:3866 70. 27. Galimberti D, Fenoglio C, Lovati C, et al. Serum MCP-1 levels are increased in mild cognitive impairment and mild Alzheimers disease. Neurobiol Aging. 2006;27: 1763 8. 28. Bermejo P, Martin-Aragon S, Benedi J, et al. Differences of peripheral inammatory markers between mild cognitive impairment and Alzheimers disease. Immunol Lett. 2008;117:198 202. 29. McNaull BB, Todd S, McGuinness B, Passmore AP. Inammation and anti-inammatory strategies for Alzheimers disease - a mini-review. Gerontology. 2009;56:314. 30. Smith PF. Inammation in Parkinsons disease: an update. Curr Opin Invest Drugs. 2008;9:478 84. 31. Roberts RO, Geda YE, Knopman DS, et al. Metabolic syndrome, inammation, and nonamnestic mild cognitive impairment in older persons: a population-based study. Alzheimer Dis Assoc Disord. 2010;24:11-8. 32. Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7:192201. 33. Villani F, Busia A, Villani M, Vismara C, Viviani S, Bonfante V. Serum cytokine in response to chemo-radiotherapy for Hodgkins disease. Tumori. 2008;94:803 8. 34. Pusztai L, Mendoza TR, Reuben JM, et al. Changes in plasma levels of inammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;25:94 102. 35. Mills PJ, Ancoli-Israel S, Parker B, et al. Predictors of
Cancer and chemotherapy-related cognitive dysfunction
437
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47. 48.
49.
50.
51.
inammation in response to anthracycline-based chemotherapy for breast cancer. Brain Behav Immun. 2008;22:98 104. Meyers CA, Albitar M, Estey E. Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer. 2005;104:788 93. Vardy JL, Booth C, Pond GR, et al. Cytokine levels in patients with colorectal cancer and breast cancer and their relationship to fatigue and cognitive function [abstract]. J Clin Oncol. 2007;18S:9070. Vardy J, Dhillon H, Xu W, et al. Cognitive function in colorectal cancer patients: interim analysis of a longitudinal prospective study [abstract]. Cognition and Cancer Meeting. March 8 9, 2010; Memorial-Sloan Kettering Cancer Center, New York, NY. Fiocco AJ, Lindquist K, Ferrell R, et al. COMT genotype and cognitive function: an 8-year longitudinal study in white and black elders. Neurology. 2010;74:1296-302. Collins JS, Perry RT, Watson B Jr, et al. Association of a haplotype for tumor necrosis factor in siblings with lateonset Alzheimer disease: the NIMH Alzheimer Disease Genetics Initiative. Am J Med Genet. 2000;96:82330. Bertram L, McQueen MB, Mullin K, Blacker D, Tanzi RE. Systematic meta-analyses of Alzheimer disease genetic association studies: the AlzGene database. Nat Genet. 2007;39:1723. Ahles TA, Saykin AJ, Noll WW, et al. The relationship of APOE genotype to neuropsychological performance in long-term cancer survivors treated with standard dose chemotherapy. Psychooncology. 2003;12:6129. Small BJ, Rawson KS, Walsh E, et al. Catechol-O-methyltransferase (COMT) genotype modulates cancer treatment-related cognitive decits in breast cancer survivors. Cancer. 2011;117:1369 76. Morley KI, Montgomery GW. The genetics of cognitive processes: candidate genes in humans and animals. Behav Genet. 2001;31:51131. McAllister TW, Ahles TA, Saykin AJ, et al. Cognitive effects of cytotoxic cancer chemotherapy: predisposing risk factors and potential treatments. Curr Psychiatry Rep. 2004;6:364 71. Ahles T, Saykin A, McDonald B, et al. Genetics of cognitive decline post cancer chemotherapy [abstract]. Cognition and Cancer Meeting. March 8 9, 2010; MemorialSloan Kettering Cancer Center, New York, NY. 2010. Miller G. Epigenetics. The seductive allure of behavioral epigenetics. Science. 2010;329:24-7. Pfeilschifter J, Koditz R, Pfohl M, Schatz H, et al. Changes in proinammatory cytokine activity after menopause. Endocr Rev. 2002;23:90 119. Greendale GA, Huang MH, Wight RG, et al. Effects of the menopause transition and hormone use on cognitive performance in midlife women. Neurology. 2009;72: 1850 7. Paraska K, Bender CM. Cognitive dysfunction following adjuvant chemotherapy for breast cancer: two case studies. Oncol Nurs Forum. 2003;30:473 8. Palmer JL, Trotter T, Joy AA, Carlson LE, et al. Cognitive effects of tamoxifen in pre-menopausal women with breast cancer compared to healthy controls. J Cancer Surviv. 2008;2:275 82.
52. Schilder CM, Seynaeve C, Beex LV, et al. Effects of tamoxifen and exemestane on cognitive functioning of postmenopausal patients with breast cancer: results from the neuropsychological side study of the tamoxifen and exemestane adjuvant multinational trial. J Clin Oncol. 2010;28:1294-300. 53. Klepin H, Mohile S, Hurria A. Geriatric assessment in older patients with breast cancer. J Natl Compr Cancer Netw. 2009;7:226 36. 54. Gorin SS, Heck JE, Albert S, Hershman D. Treatment for breast cancer in patients with Alzheimers disease. J Am Geriatr Soc. 2005;53:1897904. 55. Gupta SK, Lamont EB. Patterns of presentation, diagnosis, and treatment in older patients with colon cancer and comorbid dementia. J Am Geriatr Soc. 2004;52: 16817. 56. Goodwin JS, Samet JM, Hunt WC. Determinants of survival in older cancer patients. J Natl Cancer Inst. 1996; 88:1031 8. 57. Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29: 12532. 58. Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148:42734. 59. Kelley BJ, Petersen RC. Alzheimers disease and mild cognitive impairment. Neurol Clin. 2007;25:577 609. 60. Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:18394. 61. Extermann M, Aapro M. Assessment of the older cancer patient. Hematol Oncol Clin North Am. 2000;14;6377. 62. Rodin MB, Mohile SG. A practical approach to geriatric assessment in oncology. J Clin Oncol. 2007;25:1936 44. 63. Hurria A, Goldfarb S, Rosen C, et al. Effect of adjuvant breast cancer chemotherapy on cognitive function from the older patients perspective. Breast Cancer Res Treat. 2006;98:343 8. 64. Chen H, Cantor A, Meyer J, et al. Can older cancer patients tolerate chemotherapy? A prospective pilot study. Cancer. 2003;97:110714. 65. Extermann M, Meyer J, McGinnis M, et al. A comprehensive geriatric intervention detects multiple problems in older breast cancer patients. Crit Rev Oncol Hematol. 2004;49:69 75. 66. Hurria A, Zuckerman E, Panageas KS, et al. A prospective, longitudinal study of the functional status and quality of life of older patients with breast cancer receiving adjuvant chemotherapy. J Am Geriatr Soc. 2006;54: 1119 24. 67. Heck JE, Albert SM, Franco R, Gorin SS. Patterns of dementia diagnosis in Surveillance, Epidemiology, and End Results breast cancer survivors who use chemotherapy. J Am Geriatr Soc. 2008;56:168792. 68. Nelson CJ, Lee JS, Gamboa MC, Roth AJ, et al. Cognitive effects of hormone therapy in men with prostate cancer: a review. Cancer. 2008;113:1097106. 69. Salminen E, Portin R, Korpela J, et al. Androgen deprivation and cognition in prostate cancer. Br J Cancer. 2003;89:971 6. 70. Green HJ, Pakenham KI, Headley BC, et al. Quality of life compared during pharmacological treatments and clini-
438
M.C. Janlesins et al
71.
72.
73.
74.
75.
76.
77.
78.
cal monitoring for non-localized prostate cancer: a randomized controlled trial. BJU Int. 2004;93:9759. Mohile SG, Lacy M, Rodin M, et al. Cognitive effects of androgen deprivation therapy in an older cohort of men with prostate cancer. Crit Rev Oncol Hematol. 2010;75: 152-9. Chodosh J, Petitti DB, Elliott M, et al. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004;52:10519. Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797 811. Folstein MF, Folstein SE, McHugh PR. Mini-Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12: 189 98. Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51:1451 4. DeAngelis LM, Posner JB, eds. Neurologic complications of cancer. side effects of chemotherapy. New York: Oxford University Press; 2009. Winocur G, Vardy J, Binns MA, Kerr L, Tannock I. The effects of the anti-cancer drugs, methotrexate and 5-uorouracil, on cognitive function in mice. Pharmacol Biochem Behav. 2006;85:66 75. Konat GW, Kraszpulski M, James I, Zhang HT, Abraham J. Cognitive dysfunction induced by chronic ad-
79.
80.
81.
82.
83.
84.
85.
ministration of common cancer chemotherapeutics in rats. Metab Brain Dis. 2008;23:32533. Foley JJ, Raffa RB, Walker EA. Effects of chemotherapeutic agents 5-uorouracil and methotrexate alone and combined in a mouse model of learning and memory. Psychopharmacology (Berl). 2008;199:52738. Mustafa S, Walker A, Bennett G, Wigmore PM. 5-Fluorouracil chemotherapy affects spatial working memory and newborn neurons in the adult rat hippocampus. Eur J Neurosci. 2008;28:32330. Janelsins MC, Roscoe JA, Berg MJ, et al. IGF-1 partially restores chemotherapy-induced reductions in neural cell proliferation in adult C57BL/6 mice. Cancer Invest. 2010;28:2928. Dietrich J, Han R, Yang Y, Mayer-Proschel M, Noble M. CNS progenitor cells and oligodendrocytes are targets of chemotherapeutic agents in vitro and in vivo. J Biol. 2006;5:22. Han R, Yang YM, Dietrich J, Luebke A, Mayer-Proschel M, Noble M. Systemic 5-uorouracil treatment causes a syndrome of delayed myelin destruction in the central nervous system. J Biol. 2008;7:12. Tangpong J, Cole MP, Sultana R, et al. Adriamycin-induced, TNF-alpha-mediated central nervous system toxicity. Neurobiol Dis. 2006;23:12739. Joshi G, Aluise CD, Cole MP, et al. Alterations in brain antioxidant enzymes and redox proteomic identication of oxidized brain proteins induced by the anti-cancer drug Adriamycin: implications for oxidative stress-mediated chemobrain. Neuroscience. 2010;166:796 807.
You might also like
- Book and Instructions For Fortune Telling 32cardsDocument55 pagesBook and Instructions For Fortune Telling 32cardscat100% (8)
- Trauma Sequelae (Libro)Document537 pagesTrauma Sequelae (Libro)Andrea BautistaNo ratings yet
- Maths Quiz For Grade 2: StartDocument3 pagesMaths Quiz For Grade 2: StartGregory100% (2)
- Satanism and Occult-Related ViolenceDocument93 pagesSatanism and Occult-Related Violence4uk57cNo ratings yet
- On The Primacy of The Intellect - Gordon H. ClarkDocument15 pagesOn The Primacy of The Intellect - Gordon H. ClarkMarcelo Sánchez100% (1)
- Clinical Patterns and Biological Correlates of Cognitive Dysfunction Associated To Cancer TreatmentDocument12 pagesClinical Patterns and Biological Correlates of Cognitive Dysfunction Associated To Cancer TreatmentRodolfo BenavidesNo ratings yet
- Chemotherapy Related Cog. Dysf.Document9 pagesChemotherapy Related Cog. Dysf.Manuel Guerrero GómezNo ratings yet
- Adhere Nci ADocument18 pagesAdhere Nci AMade A-gNo ratings yet
- Research MethodsDocument2 pagesResearch MethodsMahrukh SiddiquiNo ratings yet
- Skaali 2010 CancerDocument8 pagesSkaali 2010 CancerNagy DaherNo ratings yet
- Chemobrain Study Breast CarcinomaDocument10 pagesChemobrain Study Breast CarcinomaRodolfo BenavidesNo ratings yet
- Función Neurocognitiva en El Paciente Con CáncerDocument22 pagesFunción Neurocognitiva en El Paciente Con CáncerMIGUEL MORENONo ratings yet
- Whittaker Et Al-2022-Scientific ReportsDocument22 pagesWhittaker Et Al-2022-Scientific ReportsAlex WhittakerNo ratings yet
- 10 1093@jncics@pkz074Document34 pages10 1093@jncics@pkz074Sybil LandrinNo ratings yet
- Research Paper On Dual DiagnosisDocument6 pagesResearch Paper On Dual Diagnosisyfwkdbaod100% (1)
- 2014 Article 5105Document26 pages2014 Article 5105Billy Ch SendukNo ratings yet
- Palliative Care and End-Of-Life Care in Adults With Malignant Brain TumorsDocument10 pagesPalliative Care and End-Of-Life Care in Adults With Malignant Brain TumorsLaras Adythia PratiwiNo ratings yet
- Patients With Cancer - Overview of The Clinical Features and Diagnosis of Psychiatric Disorders - UpToDateDocument36 pagesPatients With Cancer - Overview of The Clinical Features and Diagnosis of Psychiatric Disorders - UpToDatemayteveronica1000No ratings yet
- 2019 Cognitive Rehabilitation For Cancer Related Cognitive DisfunctionDocument27 pages2019 Cognitive Rehabilitation For Cancer Related Cognitive DisfunctionAlba Sueiro DominguezNo ratings yet
- Annett - Et - Al-2015-Pediatric - Blood - & - Cancer 2Document54 pagesAnnett - Et - Al-2015-Pediatric - Blood - & - Cancer 2KarolinaMaślakNo ratings yet
- A Missing Piece? Neuropsychiatric Functioning in Untreated Patients With Tumors Within The Cerebellopontine AngleDocument9 pagesA Missing Piece? Neuropsychiatric Functioning in Untreated Patients With Tumors Within The Cerebellopontine AnglejuandellibroNo ratings yet
- Chapter 134 - VanDocument18 pagesChapter 134 - VanVan John MagallanesNo ratings yet
- 1-S2.0-S0889159103000783-Main XXXDocument8 pages1-S2.0-S0889159103000783-Main XXXSaiber PanNo ratings yet
- Cognitive Impairment and Delirium in Patients With CancerDocument11 pagesCognitive Impairment and Delirium in Patients With Cancerrichard phoNo ratings yet
- SCIENDIRESCTSDocument12 pagesSCIENDIRESCTSMasita Rezky Sari masita RezkyNo ratings yet
- Prevalence of Depression, Anxiety, and Adjustment Disorder in Oncological, Haematological, and Palliative-Care Settings: A Meta-Analysis of 94 Interview-Based StudiesDocument16 pagesPrevalence of Depression, Anxiety, and Adjustment Disorder in Oncological, Haematological, and Palliative-Care Settings: A Meta-Analysis of 94 Interview-Based StudiesClaudia EvelineNo ratings yet
- Cancer Depre Anx 2º ArtículoDocument12 pagesCancer Depre Anx 2º Artículoalvarogmc02No ratings yet
- Doctor-Patient CommunicationDocument10 pagesDoctor-Patient CommunicationrhismaNo ratings yet
- Perspective: Systems Biology of Metabolism: A Driver For Developing Personalized and Precision MedicineDocument8 pagesPerspective: Systems Biology of Metabolism: A Driver For Developing Personalized and Precision MedicineMauricio RíosNo ratings yet
- 1 s2.0 S003331821070671X MainDocument12 pages1 s2.0 S003331821070671X MainchalistaNo ratings yet
- Chap 1 2 3 1Document23 pagesChap 1 2 3 1Alexa Nicole GayosoNo ratings yet
- Attitudes of US Medical Trainees Towards Neurology Education: "Neurophobia" - A Global IssueDocument7 pagesAttitudes of US Medical Trainees Towards Neurology Education: "Neurophobia" - A Global Issuealikhanomer5No ratings yet
- Acceptance and Commitment Therapy in Cancer: Review of Applications and FindingsDocument27 pagesAcceptance and Commitment Therapy in Cancer: Review of Applications and FindingsJuan Alberto GonzálezNo ratings yet
- Spiritual Well Being in AdultsDocument12 pagesSpiritual Well Being in AdultsFrancisco MartinezNo ratings yet
- Psychosomatics. 2010 MarDocument12 pagesPsychosomatics. 2010 MarMario Gabriel CarignaniNo ratings yet
- Psychiatric Outcomes After Temporal Lobe Surgery in Patients With Temporal Lobe Epilepsy and Comorbid Psychiatric IllnessDocument8 pagesPsychiatric Outcomes After Temporal Lobe Surgery in Patients With Temporal Lobe Epilepsy and Comorbid Psychiatric IllnessFrancisco Javier Fierro RestrepoNo ratings yet
- Cancer Volume 77 Issue 2 1996Document7 pagesCancer Volume 77 Issue 2 1996BiancaTCNo ratings yet
- Cancer&CognitionDocument14 pagesCancer&CognitionAlannNo ratings yet
- Diagnostic Misconceptions? A Closer Look at Clinical Research On Alzheimer's DiseaseDocument4 pagesDiagnostic Misconceptions? A Closer Look at Clinical Research On Alzheimer's DiseaseFuraya FuisaNo ratings yet
- m1 Patientspopulations Medicalgenetics Syllabus f08Document6 pagesm1 Patientspopulations Medicalgenetics Syllabus f08ירדן לויןNo ratings yet
- JurnlDocument7 pagesJurnlyuliaNo ratings yet
- Encyclopedia of Behavioral Medicine 9783030399016 303039901x 9783030399023 3030399028 - CompressDocument2,457 pagesEncyclopedia of Behavioral Medicine 9783030399016 303039901x 9783030399023 3030399028 - CompressHilda FadhilahNo ratings yet
- Nursing Proces NewDocument10 pagesNursing Proces NewBrandy SangurahNo ratings yet
- The Impact of Cancer On Children's Physical, Emotional, and Psychosocial Well-BeingDocument3 pagesThe Impact of Cancer On Children's Physical, Emotional, and Psychosocial Well-BeingRegina Masli PutriNo ratings yet
- Beaumont 2011 Patient Reported Outcomes in Phase III Study of Everolimus Vs PlaceboDocument11 pagesBeaumont 2011 Patient Reported Outcomes in Phase III Study of Everolimus Vs PlaceboIzaty HamidNo ratings yet
- Prevalen of DDocument8 pagesPrevalen of DĐỗ Văn ĐứcNo ratings yet
- Cognitive and Psychological Factors Associated With Early PostDocument18 pagesCognitive and Psychological Factors Associated With Early PostRodolfo BenavidesNo ratings yet
- The Effectiveness of Psychosocial Interventions For Psychological Outcomes in Pediatric Oncology: A Systematic ReviewDocument21 pagesThe Effectiveness of Psychosocial Interventions For Psychological Outcomes in Pediatric Oncology: A Systematic ReviewFirnawati MaspekeNo ratings yet
- Carter Obermeyer - Irr Final DraftDocument8 pagesCarter Obermeyer - Irr Final Draftapi-670586475No ratings yet
- Nursing ProcessDocument10 pagesNursing ProcessBrandy SangurahNo ratings yet
- Behavioral Medicine in CancerDocument25 pagesBehavioral Medicine in CancerOVIDIU-IULIAN BOBEINo ratings yet
- Users' Guides To The Medical Literature XIVDocument5 pagesUsers' Guides To The Medical Literature XIVFernandoFelixHernandezNo ratings yet
- Enseñanza AnestesioDocument14 pagesEnseñanza AnestesioRaúl MartínezNo ratings yet
- Cancer Rehabilitation AssessmentDocument21 pagesCancer Rehabilitation AssessmentLiliana Carolina Guzman RiosNo ratings yet
- Faktor-Faktor Yang Mempengaruhi Kecemasan Pasien Dalam Tindakan Kemoterapi Di Rumah Sakit DR - Moewardi SurakartaDocument11 pagesFaktor-Faktor Yang Mempengaruhi Kecemasan Pasien Dalam Tindakan Kemoterapi Di Rumah Sakit DR - Moewardi SurakartaPoni Neng GelisNo ratings yet
- Cognitive Problems in Patients On Androgen Deprivation Therapy: A Qualitative Pilot StudyDocument6 pagesCognitive Problems in Patients On Androgen Deprivation Therapy: A Qualitative Pilot StudyDr. Glauber LeitãoNo ratings yet
- Pi Is 0959804910000079Document7 pagesPi Is 0959804910000079khudher99No ratings yet
- Patient-Related Barriers To Fatigue Communication in Cancer Patients Receiving Active TreatmentDocument13 pagesPatient-Related Barriers To Fatigue Communication in Cancer Patients Receiving Active TreatmentkhkjhkkjhjbNo ratings yet
- The Effect of Progressive Muscle Relaxation On Cancer Patients' Self-EfficacyDocument8 pagesThe Effect of Progressive Muscle Relaxation On Cancer Patients' Self-EfficacySyahri FaziraNo ratings yet
- Supportive Care Needs of Patients With Head and Neck Cancer Referred To Palliative MedicineDocument8 pagesSupportive Care Needs of Patients With Head and Neck Cancer Referred To Palliative Medicinemadhumitha srinivasNo ratings yet
- The Case For PharmacyDocument32 pagesThe Case For PharmacyLunar EclipseNo ratings yet
- Oncotarget 08 36800Document12 pagesOncotarget 08 36800Anonymous wGAc8DYl3VNo ratings yet
- Bunemann (2020)Document10 pagesBunemann (2020)Nerea AlvarezNo ratings yet
- Thyroid CancerDocument7 pagesThyroid CancerEphNo ratings yet
- Principle-Based Stepped Care and Brief Psychotherapy for Integrated Care SettingsFrom EverandPrinciple-Based Stepped Care and Brief Psychotherapy for Integrated Care SettingsAlexandros MaragakisNo ratings yet
- Leadership Denise Stodola Comm. 101 Michael Martin February 24, 2010Document10 pagesLeadership Denise Stodola Comm. 101 Michael Martin February 24, 2010Michael MartinNo ratings yet
- Kinder Class Program S.Y. 2023 2024Document14 pagesKinder Class Program S.Y. 2023 2024Erikajane IgnacioNo ratings yet
- ACT ToolkitDocument54 pagesACT ToolkitWanda Vegara SimónNo ratings yet
- Section I (2-3 Minutes) : Oral Exam Rp06 Empower - Units 4-6Document3 pagesSection I (2-3 Minutes) : Oral Exam Rp06 Empower - Units 4-6Daniel Lagos IbáñezNo ratings yet
- Adult EducationDocument6 pagesAdult EducationMrs. Sweety DwivediNo ratings yet
- Structuredfield Experience Log Sum18itec7305Document3 pagesStructuredfield Experience Log Sum18itec7305api-370169875No ratings yet
- 1.1 Data, Information and Knowledge A Level ITDocument12 pages1.1 Data, Information and Knowledge A Level ITZoya AliNo ratings yet
- Group 3 - Program DetailsDocument3 pagesGroup 3 - Program DetailsDean MarcNo ratings yet
- Mba 4 Sem Marketing of Services RMB MK 04 2017 18Document2 pagesMba 4 Sem Marketing of Services RMB MK 04 2017 18Reema SinghNo ratings yet
- Psicopatology in The GenomeDocument254 pagesPsicopatology in The Genomeandrea-lassini-4280No ratings yet
- Parker Sauvageau - Final ResearchDocument18 pagesParker Sauvageau - Final Researchapi-356280513No ratings yet
- Assessor Feedback (Assessment Conducted)Document2 pagesAssessor Feedback (Assessment Conducted)priyanshiNo ratings yet
- Unit 17: Quality Management in BusinessDocument5 pagesUnit 17: Quality Management in Businesschandni0810No ratings yet
- Republic of The Philippines Department oDocument15 pagesRepublic of The Philippines Department oMaritesNo ratings yet
- 3) The Entrepreneurial ProcessDocument31 pages3) The Entrepreneurial ProcessAli El HajjNo ratings yet
- Physical Education and Health SyllabusDocument2 pagesPhysical Education and Health Syllabusapi-327370513100% (1)
- Mobile and Interactive Media Use by Young Children: The Good, The Bad, and The UnknownDocument5 pagesMobile and Interactive Media Use by Young Children: The Good, The Bad, and The Unknownvampirek91100% (1)
- Uts Module 1 - Unit 4Document5 pagesUts Module 1 - Unit 4Juwudy LeeNo ratings yet
- Person-Based Structures: Mcgraw-Hill/IrwinDocument36 pagesPerson-Based Structures: Mcgraw-Hill/IrwinraktimbeastNo ratings yet
- Mridul Kumar SinghDocument11 pagesMridul Kumar Singhjini4998No ratings yet
- PRACTICAL RESEARCH 1 ReviewerDocument2 pagesPRACTICAL RESEARCH 1 ReviewerAngel Loraine AguilarNo ratings yet
- Central Bicol State University of Agriculture: WWW - Cbsua.edu - PH Op@cbsua - Edu.phDocument4 pagesCentral Bicol State University of Agriculture: WWW - Cbsua.edu - PH Op@cbsua - Edu.phAl Grace DoblonNo ratings yet
- Thesis Statement About El SalvadorDocument5 pagesThesis Statement About El Salvadorafktgoaaeynepd100% (2)
- Marerial 1 Class 9 Congratulation Hopes and WishesDocument2 pagesMarerial 1 Class 9 Congratulation Hopes and Wishesnurhayati kanaya intaniaNo ratings yet
- Make em Don't Break emDocument9 pagesMake em Don't Break emBala UrmarNo ratings yet