Punto 6 Innovation
Uploaded by
antonella.ado47Topics covered
- Anxiety Management,
- Emotional Well-being,
- Material Reliability,
- Cardiac Resynchronization Ther…,
- Psychological Impact,
- Health Autonomy,
- Quality of Life Improvement,
- Patient Autonomy,
- Technological Advancements,
- Patient Testimony
Punto 6 Innovation
Uploaded by
antonella.ado47Topics covered
- Anxiety Management,
- Emotional Well-being,
- Material Reliability,
- Cardiac Resynchronization Ther…,
- Psychological Impact,
- Health Autonomy,
- Quality of Life Improvement,
- Patient Autonomy,
- Technological Advancements,
- Patient Testimony
Common questions
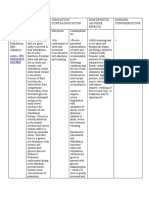
Powered by AIPacemaker implantation provides significant physical benefits by regulating heart rate, particularly for patients with bradycardia or atrioventricular block, leading to a regular heart rhythm and reduction of symptoms like syncope, fatigue, and dizziness . Psychologically, it increases confidence and autonomy by reducing the fear of sudden cardiac crises, fostering improved emotional well-being, and allowing more active participation in social life due to more stable health .
Miniaturization of pacemakers involves challenges such as balancing the compact size with sufficient battery life and ensuring device reliability and robustness. Despite size reductions, the battery must sustain long-term performance. Technologies like high-capacity batteries and miniaturized circuits are used, but these components need to resist internal stresses and impacts .
Pacemakers use biocompatible materials like silicone and polyurethane to mitigate degradation from chemical interactions with bodily fluids and withstand mechanical stress from heart movements. These materials are chosen for their durability and resistance to chemical damage, while special treatment can enhance corrosion resistance to extend the components' lifespan .
The 81-year-old female patient experienced improved heart function with an increased ejection fraction and reduced heart failure symptoms, such as shortness of breath and fatigue, post-pacemaker implantation. Psychologically, although initially anxious about the device, she gained confidence and improved her quality of life by regaining autonomy and engaging in activities previously avoided .
The younger patient typically shows quicker and more pronounced improvements in clinical and physical outcomes due to better initial health and faster device adaptation. In contrast, an elderly patient may experience a slower recovery with more psychological and device adjustment challenges, influenced by frailty and increased anxiety about the device .
The primary goals of CRT with a biventricular pacemaker are to restore synchrony between the left and right ventricles, improving the overall efficiency of the heart, reducing heart failure symptoms, and enhancing cardiac output, particularly in patients with ventricular dyssynchrony .
Modern pacemakers incorporate electromagnetic shielding systems to minimize interference from sources like MRI machines and electronic devices, which could otherwise disrupt pacemaker function. This protection is crucial to prevent malfunctions that could lead to serious health risks for patients .
The adaptation and management of pacemaker settings are crucial for optimal outcomes. This process involves regular adjustments to fine-tune the pacing mode and address evolving health needs. In elderly patients, this process may be more complex due to coexisting health conditions, necessitating careful monitoring to ensure the device effectively mitigates symptoms and improves heart function .
The selection of biocompatible materials in pacemakers is crucial for ensuring long-term functionality and safety. These materials must resist corrosion and degradation, particularly from bodily fluids, to maintain the integrity and performance of the device over time. Materials like titanium and specialized polymers help achieve these goals by withstanding chemical and mechanical stresses present in the body .
Patients often experience anxiety over device malfunctions and the need for future interventions. Healthcare professionals can support them through clear communication, regular monitoring, and psychological support, including counseling, to ease these concerns and help patients adapt to living with a medical device .