Professional Documents
Culture Documents
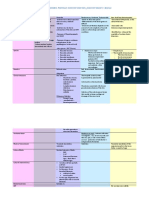
Chem Path
Chem Path
Uploaded by
Thodesia KazaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chem Path
Chem Path
Uploaded by
Thodesia KazaCopyright:
Available Formats
When a mosquito carrying dengue virus bites a person, the virus enters the skin together with the
mosquito's saliva. It binds to and enters white blood cells, and reproduces inside the cells while they move throughout the body. The white blood cells respond by producing a number of signaling proteins, such as interferon, which are responsible for many of the symptoms, such as the fever, the flu-like symptoms and the severe pains. In severe infection, the virus production inside the body is greatly increased, and many more organs (such as the liver and the bone marrow) can be affected, and fluid from the bloodstream leaks through the wall of small blood vessels into body cavities. As a result, less blood circulates in the blood vessels, and the blood pressure becomes so low that it cannot supply sufficient blood to vital organs. Furthermore, dysfunction of the bone marrow leads to reduced numbers of platelets, which are necessary for effective blood clotting; this increases the risk of bleeding, the other major complication of dengue fever. [22]
Viral replication
Once inside the skin, dengue virus binds to Langerhans cells (a population of dendritic cells in the skin that identifies pathogens).[22] The virus enters the cells through binding between viral proteins andmembrane proteins on the Langerhans cell, specifically the C-type lectins called DC-SIGN, mannose receptor and CLEC5A.[12] DC-SIGN, a non-specific receptor for foreign material on dendritic cells, seems to be the main point of entry. [13] The dendritic cell moves to the nearest lymph node. Meanwhile, the virus genome is replicated in membrane-bound vesicles on the cell's endoplasmic reticulum, where the cell's protein synthesis apparatus produces new viral proteins, and the viral RNA is copied. Immature virus particles are transported to the Golgi apparatus, the part of the cell where some of the proteins receive necessary sugar chains (glycoproteins). The now mature new viruses bud on the surface of the infected cell and are released by exocytosis. They are then able to enter other white blood cells, such as monocytes and macrophages.[12] The initial reaction of infected cells is to produce interferon, a cytokine that raises a number of defenses against viral infection through the innate immune system by augmenting the production of a large group of proteins mediated by the JAK-STAT pathway. Some serotypes of dengue virus appear to have mechanisms to slow down this process. Interferon also activates the adaptive immune system, which leads to the generation of antibodies against the virus as well as T cells that directly attack any cell infected with the virus.[12] Various antibodies are generated; some bind closely to the viral proteins and target them for phagocytosis (ingestion by specialized cells and destruction), but some bind the virus less well and appear instead to deliver the virus into a part of the phagocytes where it is not destroyed but is able to replicate further. [12]
Severe disease
Further information: Antibody-dependent enhancement It is not entirely clear why secondary infection with a different strain of dengue virus places people at risk of dengue hemorrhagic fever and dengue shock syndrome. The most widely accepted hypothesis is that of antibody-dependent enhancement (ADE). The exact mechanism behind ADE is unclear. It may be caused by poor binding of non-neutralizing antibodies and delivery into the wrong compartment of white blood cells that have ingested the virus for destruction. [12][13] There is a suspicion that ADE is not the only mechanism underlying severe dengue-related complications,[1] and various lines of research have implied a role for T cells and soluble factors such as cytokines and the complement system.[22] Severe disease is marked by two problems: dysfunction of endothelium (the cells that line blood vessels) and disordered blood clotting.[6] Endothelial dysfunction leads to the leakage of fluid from the blood vessels into the chest and abdominal cavities, while coagulation disorder is responsible for the bleeding complications. Higher viral load in the blood and involvement of other organs (such as thebone marrow and the liver) are associated with more severe disease. Cells in the affected organs die, leading to the release of cytokines and activation of both coagulation and fibrinolysis (the opposing systems of blood clotting and clot degradation). These alterations together lead to both endothelial dysfunction and coagulation disorder. [22]
Translate The WBC respond by producing a number of signaling proteins, such as interferon, which are responsible for many of the symptoms, such as the fever, the flu-like symptoms and the severe pains. (WBC bertindak balas dengan
menghasilkan beberapa protein isyarat, seperti interferon,yang bertanggungjawab bagi kebanyakan gejala, seperti demam, gejala-gejala seperti selesema dan sakit teruk. )
In severe infection, the virus production inside the body is greatly increased, and many more organs can be affected, and fluid from the bloodstream leaks through the wall of small blood vessels into body cavities. (Pada
jangkitan yang teruk, pengeluaran virus di dalam badan bertambah dengan banyaknya, dan lebih banyak organ boleh terjejas, dan cecair dari kebocoran saluran darah melalui dinding saluran darah kecil ke dalam rongga badan. )
As a result, less blood circulates in the blood vessels, and the blood pressure becomes so low that it cannot supply sufficient blood to vital organs. (Hasilnya, kurang darah beredar dalam saluran
darah, dan tekanan darah menjadi begiturendah bahawa ia tidak dapat membekalkan darah yang mencukupi kepada organ-organ penting. )
Future more, dysfunction of the bone marrow leads to reduced numbers of platelets, which are necessary for effective blood clotting. (Masa depan yang lebih, kegagalan fungsi sumsum
tulang membawa kepada nombordikurangkan platelet, yang perlu untuk pembekuan darah yang berkesan. )
You might also like
- DM TestsDocument23 pagesDM TestsMunaNo ratings yet
- Seegene HPV28 Manual en InglésDocument43 pagesSeegene HPV28 Manual en InglésPort0% (1)
- Dengue FeverDocument8 pagesDengue Feverramoli1988No ratings yet
- Amo PathologyDocument10 pagesAmo PathologyOtema JamesNo ratings yet
- Document 1Document3 pagesDocument 1Sidharth TripathiNo ratings yet
- What Is Dengue Fever?Document9 pagesWhat Is Dengue Fever?Sk RiazNo ratings yet
- Acute and Chronic InflammationDocument22 pagesAcute and Chronic InflammationRedhwan85No ratings yet
- Plasma Leakage Audio Narration - FinalDocument2 pagesPlasma Leakage Audio Narration - FinalRahmat Aji PramonoNo ratings yet
- Dengue Fever Is A MosquitoDocument4 pagesDengue Fever Is A MosquitoPartha Permana PutraNo ratings yet
- 2.4 2.5 Radang Akut Kronik Dan MorfologiDocument51 pages2.4 2.5 Radang Akut Kronik Dan MorfologimeNo ratings yet
- DENGUEDocument9 pagesDENGUERahul KhulbeyNo ratings yet
- Kelainan Hematologi Pada Demam Berdarah Dengue: J Peny Dalam, Volume 10 Nomor 3 September 2009Document10 pagesKelainan Hematologi Pada Demam Berdarah Dengue: J Peny Dalam, Volume 10 Nomor 3 September 2009almira dina mariskiNo ratings yet
- Dengue and Chikungunya Infections in ChildrenDocument9 pagesDengue and Chikungunya Infections in ChildrenAl-Harits OctaNo ratings yet
- 1 Acute InflammationDocument6 pages1 Acute InflammationNauzaina IjazNo ratings yet
- Dengue FeverDocument4 pagesDengue FeverAteng JeonNo ratings yet
- Understanding Emerging and ReDocument15 pagesUnderstanding Emerging and ReGWeezyNo ratings yet
- Acute InflammationDocument64 pagesAcute InflammationSuleiman KikulweNo ratings yet
- HIV ResearchDocument1 pageHIV ResearchGiuseppe Riccardo LongoNo ratings yet
- jcm-10-00877 InvestigaçãoDocument33 pagesjcm-10-00877 InvestigaçãoLucas Monteiro LopesNo ratings yet
- DENGUE CASE MANAGEMENT DiscussionDocument5 pagesDENGUE CASE MANAGEMENT DiscussionHanako AranillaNo ratings yet
- 10 1080@09537104 2020 1755031 PDFDocument4 pages10 1080@09537104 2020 1755031 PDFJuan Fernando BermúdezNo ratings yet
- Inflammation and RepairDocument34 pagesInflammation and Repairanshum guptaNo ratings yet
- Pathogenesis of Severe Dengue InfectionDocument4 pagesPathogenesis of Severe Dengue InfectionAhmed MawardiNo ratings yet
- T Cell Immunopathogenesis of Dengue Virus Infection: Lokesh Guglani and S.K. KabraDocument12 pagesT Cell Immunopathogenesis of Dengue Virus Infection: Lokesh Guglani and S.K. KabraayushintamahaputriNo ratings yet
- Acute and Chronic InflammationDocument121 pagesAcute and Chronic Inflammationbariq AlnawaisehNo ratings yet
- Inflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDocument26 pagesInflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDavid Cahyo WibisonoNo ratings yet
- LeukocytosisDocument2 pagesLeukocytosisNeoMedicaNo ratings yet
- Pathophysiology: The Aedes MosquitoDocument4 pagesPathophysiology: The Aedes MosquitoLlerym Onairda AzellebNo ratings yet
- Denguefinalpdf-170803082145 2Document74 pagesDenguefinalpdf-170803082145 2L. HusnaNo ratings yet
- Group No 3Document19 pagesGroup No 3محمد نعیم اقبالNo ratings yet
- 07 InflammationDocument69 pages07 InflammationSangameswaran B.BNo ratings yet
- Report Pathopysiology (Endocarditis) 12Document7 pagesReport Pathopysiology (Endocarditis) 12Ade Yulina Mursyidah Sa'adNo ratings yet
- Ws Dengue 1. Patogenesis DHFDocument22 pagesWs Dengue 1. Patogenesis DHFGheavita Chandra DewiNo ratings yet
- Ref Virology and ImmunologyDocument20 pagesRef Virology and ImmunologyYosuaNo ratings yet
- AIDS & Clinical: Symptoms of AIDS Related Opportunistic Infections and Their Effects On Human BodyDocument5 pagesAIDS & Clinical: Symptoms of AIDS Related Opportunistic Infections and Their Effects On Human BodyMarviane ThenNo ratings yet
- Vascularized Tissue To Injurious Agent A Protective ResponseDocument13 pagesVascularized Tissue To Injurious Agent A Protective ResponseBravan AliennNo ratings yet
- Kuliah Pakar Modul 3.1Document68 pagesKuliah Pakar Modul 3.1Pramesti DarojahNo ratings yet
- Pathogenesis of Hemorrhagic Due To Dengue Virus: Literature ReviewDocument5 pagesPathogenesis of Hemorrhagic Due To Dengue Virus: Literature Reviewfebyan yohanesNo ratings yet
- Multiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundDocument6 pagesMultiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundrahayuNo ratings yet
- dkp2 ReskyDocument4 pagesdkp2 ReskyKurnia pralisaNo ratings yet
- 2.acute & Chronic Inflammation, S1Document90 pages2.acute & Chronic Inflammation, S1LennyOctaviaNo ratings yet
- Study-Notes - Inflammation-And-Repair (1) 88Document17 pagesStudy-Notes - Inflammation-And-Repair (1) 88jjjkkNo ratings yet
- Patof HivDocument6 pagesPatof Hivsheyla salsabilaNo ratings yet
- HIV AND TB SummaryDocument5 pagesHIV AND TB SummaryTharanga HewabuhageNo ratings yet
- DengueDocument4 pagesDengueKathleen DimacaliNo ratings yet
- Chapter 4Document30 pagesChapter 4Noriani ZakariaNo ratings yet
- Rangkuman Week 3 (PBL) - RADocument27 pagesRangkuman Week 3 (PBL) - RAMaria Dini AdmiratiNo ratings yet
- Case ReportDocument29 pagesCase ReportFinda RedhizaNo ratings yet
- SHS 301 Lect-05Document44 pagesSHS 301 Lect-05AAZEEN ALINo ratings yet
- Case Presentation 1Document37 pagesCase Presentation 1Safoora RafeeqNo ratings yet
- The Blood Vessels and Immunity FinishedDocument64 pagesThe Blood Vessels and Immunity FinishedAlano WheatleyNo ratings yet
- Disease Process NarrativeDocument4 pagesDisease Process NarrativeFritz DecendarioNo ratings yet
- Pathogenic PropertiesDocument6 pagesPathogenic PropertiesRichard JacsNo ratings yet
- Modif Reactive GGLDocument4 pagesModif Reactive GGLCatalina BarbarosieNo ratings yet
- Dengue Hemorrhagic Fever Pathophysiology DiagramDocument4 pagesDengue Hemorrhagic Fever Pathophysiology DiagramAni MarlinaNo ratings yet
- ) PDF Recorded Class 7 The Immune and Lymphatic Systems - COVID-19Document25 pages) PDF Recorded Class 7 The Immune and Lymphatic Systems - COVID-19MedevemarNo ratings yet
- Immunology and HIV: Immune System's Response To HIVDocument4 pagesImmunology and HIV: Immune System's Response To HIVMel FranciscoNo ratings yet
- Disease With No CureDocument17 pagesDisease With No CureJulie Ann SaquilayanNo ratings yet
- ENDOCARDITISDocument16 pagesENDOCARDITISjustkatirinNo ratings yet
- Hasan2016 Review Article JISPCD-6-1Document6 pagesHasan2016 Review Article JISPCD-6-1ngu mahNo ratings yet
- Kawasaki DiseaseDocument9 pagesKawasaki DiseaseMery Rose GanitnitNo ratings yet
- Verticle and Horizontal ResistanceDocument10 pagesVerticle and Horizontal Resistanceankit2147No ratings yet
- Holes Human Anatomy and Physiology 12th Edition Shier Test BankDocument30 pagesHoles Human Anatomy and Physiology 12th Edition Shier Test BankKatherineBowenfojib100% (16)
- Bacterial Urinary Tract InfectionDocument17 pagesBacterial Urinary Tract InfectionROSANNA BUCAGNo ratings yet
- Chronic Suppurative Otitis MediaDocument14 pagesChronic Suppurative Otitis MediaIkhsan100% (1)
- English Model Paper 6 emDocument5 pagesEnglish Model Paper 6 emReddy GmdNo ratings yet
- Branching, Aerobic, Partially Acid Fast and Non-Acid Fast Gram (+) BacilliDocument2 pagesBranching, Aerobic, Partially Acid Fast and Non-Acid Fast Gram (+) BacilliJustine Marie RevillaNo ratings yet
- Gr. 8 - Genetically Modified Organisms (Gmo'S) Genetically Modified OrganismsDocument2 pagesGr. 8 - Genetically Modified Organisms (Gmo'S) Genetically Modified OrganismsBrian CastañedaNo ratings yet
- Activity 1 (Zamudio)Document3 pagesActivity 1 (Zamudio)Phobelyn ZamudioNo ratings yet
- I. Choose The Correct Answer: Do at ClassDocument9 pagesI. Choose The Correct Answer: Do at ClassNishali SamNo ratings yet
- 2014 CMI Supplement 3Document102 pages2014 CMI Supplement 3farmacologNo ratings yet
- 3 - Iabcr 20162 03 02 - 13 17Document6 pages3 - Iabcr 20162 03 02 - 13 17EMNo ratings yet
- Unit 10 - Mutagenesis PDFDocument5 pagesUnit 10 - Mutagenesis PDFvuivevuiveNo ratings yet
- A Seminar On The Topic TetanusDocument16 pagesA Seminar On The Topic TetanusRajat PadhanNo ratings yet
- Microbiology Exam II Fall 2001 Name: - Multiple Choice: Circle The Most Correct Answer For Each of The Following Questions. (2 Points Each)Document8 pagesMicrobiology Exam II Fall 2001 Name: - Multiple Choice: Circle The Most Correct Answer For Each of The Following Questions. (2 Points Each)Jini Luckie0% (1)
- اسئله باطني مدققه 740823Document42 pagesاسئله باطني مدققه 740823Ashraf AlbhlaNo ratings yet
- Update in Inflammatory Bowel Disease: Graham MorrisonDocument6 pagesUpdate in Inflammatory Bowel Disease: Graham MorrisonJesse Helmut Hansen-BartelNo ratings yet
- Terilization Scrubbing and Universal Precaution: Dr. Aimen Humayun House Officer Surgical Unit 2 AIMTH SialkotDocument28 pagesTerilization Scrubbing and Universal Precaution: Dr. Aimen Humayun House Officer Surgical Unit 2 AIMTH SialkotAhsan JamilNo ratings yet
- Digestive System AnatomyDocument32 pagesDigestive System AnatomyDerrick njugunaNo ratings yet
- CD Respi 30 ADocument3 pagesCD Respi 30 ANae OrdanozoNo ratings yet
- What Is Immunization?Document6 pagesWhat Is Immunization?Aulia RahmawatiNo ratings yet
- Human Blood: iGCSE Edexcel BiologyDocument38 pagesHuman Blood: iGCSE Edexcel BiologyMaryam NaeemNo ratings yet
- Basic Cardiovascular Physiology-Pasquale Pagliaro, Raffaella RastaldoDocument438 pagesBasic Cardiovascular Physiology-Pasquale Pagliaro, Raffaella RastaldoJihuhn YuNo ratings yet
- Role of Salivary BiomarkersDocument48 pagesRole of Salivary BiomarkersKevin FossNo ratings yet
- High-Yield Histopathology 2e PDFDocument346 pagesHigh-Yield Histopathology 2e PDFmary100% (1)
- Microbio PDFDocument17 pagesMicrobio PDFHernandez IanNo ratings yet
- Class IX Chapter 4 MCQ'sDocument2 pagesClass IX Chapter 4 MCQ'sAyesha KhanNo ratings yet
- Hodgkin's DiseaseDocument28 pagesHodgkin's DiseasebikeyNo ratings yet
- Revision+worksheet+gr7+.sem3 BiologyDocument4 pagesRevision+worksheet+gr7+.sem3 BiologyMawadda AljawadiNo ratings yet