Professional Documents
Culture Documents
Waardenburg Syndrome 2007
Waardenburg Syndrome 2007
Uploaded by
marikosvaCopyright:
Available Formats
You might also like
- Oet ReadingDocument15 pagesOet Readingnj0% (1)
- Syndromes Aarskog Syndrome (9p)Document10 pagesSyndromes Aarskog Syndrome (9p)M BeirutiNo ratings yet
- Syndromic Deafness - Variant of Waardenburg Syndrome: Dr. Basavaraj Belaldavar Dr. Vini BalakrishnanDocument5 pagesSyndromic Deafness - Variant of Waardenburg Syndrome: Dr. Basavaraj Belaldavar Dr. Vini BalakrishnaninventionjournalsNo ratings yet
- Rehab AnswerDocument8 pagesRehab AnswerFardeen RafiqueNo ratings yet
- Sdarticle PDFDocument9 pagesSdarticle PDFManjeev GuragainNo ratings yet
- An Example of The Utility of Genomic Analysis For Fast and Accurate Clinical Diagnosis of Complex Rare PhenotypesDocument8 pagesAn Example of The Utility of Genomic Analysis For Fast and Accurate Clinical Diagnosis of Complex Rare PhenotypesGlauce L TrevisanNo ratings yet
- Management of Spasticity and Cerebral Palsy: Yasser Awaad, Tamer Rizk and Emira ŠvrakaDocument26 pagesManagement of Spasticity and Cerebral Palsy: Yasser Awaad, Tamer Rizk and Emira ŠvrakaAgnimitra ChoudhuryNo ratings yet
- Genetic Causes of Syndromic and Non-Syndromic Autism PDFDocument9 pagesGenetic Causes of Syndromic and Non-Syndromic Autism PDFRaisa CoppolaNo ratings yet
- Nance - The Genetics of DeafnessDocument11 pagesNance - The Genetics of DeafnessPablo VasquezNo ratings yet
- Autism Spectrum Disorders: Dr.R.G.Enoch MD Psychiatry Ii Yr GMKMCH, SalemDocument100 pagesAutism Spectrum Disorders: Dr.R.G.Enoch MD Psychiatry Ii Yr GMKMCH, Salemام اسامة السيايدةNo ratings yet
- Human GeneticsDocument9 pagesHuman Geneticseli pascualNo ratings yet
- Shapiro 1997Document6 pagesShapiro 1997JohnnyNo ratings yet
- Genetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LossDocument12 pagesGenetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LosssherinNo ratings yet
- Williams Syndrome FinalDocument10 pagesWilliams Syndrome Finalkab5405No ratings yet
- Uk Fragile XDocument4 pagesUk Fragile XChristin Natalia KalembangNo ratings yet
- Wassink 2001Document8 pagesWassink 2001Marcelo ClaroNo ratings yet
- E472 FullDocument17 pagesE472 FullC_DanteNo ratings yet
- Waardenburg Syndrome in An Infant of Diabetic MotherDocument5 pagesWaardenburg Syndrome in An Infant of Diabetic Motherराजीव गुप्ताNo ratings yet
- Matsy CytoDocument7 pagesMatsy CytoDarem SoNo ratings yet
- SyndromesDocument19 pagesSyndromesapi-26826496No ratings yet
- Orphanet Journal of Rare Diseases: Walker-Warburg SyndromeDocument5 pagesOrphanet Journal of Rare Diseases: Walker-Warburg SyndromeLópez Ruelas Mónica AzenethNo ratings yet
- VACTERL-Hydrocephaly, DK-Phocomelia, and Cerebro-Cardio-Radio-Reno-Rectal CommunityDocument6 pagesVACTERL-Hydrocephaly, DK-Phocomelia, and Cerebro-Cardio-Radio-Reno-Rectal CommunitySarly FebrianaNo ratings yet
- Research Synthesis PaperDocument9 pagesResearch Synthesis PaperFiona De CastroNo ratings yet
- Numerical - 1: Structural - 2Document9 pagesNumerical - 1: Structural - 2Khaled Zeama100% (1)
- Trisomy 8 Mosaicism Syndrome: Case ReportDocument4 pagesTrisomy 8 Mosaicism Syndrome: Case ReportIoanna DivriotiNo ratings yet
- Sordera SindromicaDocument8 pagesSordera SindromicaFabian Camelo OtorrinoNo ratings yet
- Resarch Assignment PhysDocument6 pagesResarch Assignment Physapi-547006629No ratings yet
- Tay-Sachs Disease Is A: o o o o o o o oDocument7 pagesTay-Sachs Disease Is A: o o o o o o o oShuaib SiddiquiNo ratings yet
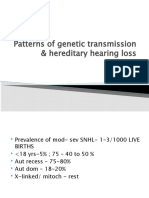
- Patterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyaDocument60 pagesPatterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyavipinNo ratings yet
- Klinefelter Syndrome and Associated Fragile-X Syndrome: Case II-5Document8 pagesKlinefelter Syndrome and Associated Fragile-X Syndrome: Case II-5صادقNo ratings yet
- 2 - Fragile X SyndromeDocument4 pages2 - Fragile X Syndromechenelyn_15No ratings yet
- Kabuki SyndomeDocument104 pagesKabuki SyndomeKim LianNo ratings yet
- Ajmg A 34257 PDFDocument3 pagesAjmg A 34257 PDFdtf1007No ratings yet
- Sudden Infant Death Syndrome: Case-Control Frequency Differences at Genes Pertinent To Early Autonomic Nervous System Embryologic DevelopmentDocument5 pagesSudden Infant Death Syndrome: Case-Control Frequency Differences at Genes Pertinent To Early Autonomic Nervous System Embryologic DevelopmentJailyn Carrasquel HerreraNo ratings yet
- Fragile X SyndromeDocument8 pagesFragile X SyndromeMay Pearl NuñalNo ratings yet
- A Case Study About Klinefelter SyndromeDocument7 pagesA Case Study About Klinefelter SyndromehoyNo ratings yet
- Genetic Disorder Research Assignment - SohrabDocument6 pagesGenetic Disorder Research Assignment - SohrabSohrab AliNo ratings yet
- Review and Update of Mutations Causing Waardenburg Syndrome: Human MutationDocument16 pagesReview and Update of Mutations Causing Waardenburg Syndrome: Human MutationIso MogoNo ratings yet
- Mendelian Disorders Class 12Document22 pagesMendelian Disorders Class 12Harith KumarNo ratings yet
- A Case Study About Klinefelter SyndromeDocument6 pagesA Case Study About Klinefelter Syndromehoy100% (1)
- Cognitive, Linguistic, and Motor Abilities in A Multigenerational Family With Childhood Apraxia of SpeechDocument20 pagesCognitive, Linguistic, and Motor Abilities in A Multigenerational Family With Childhood Apraxia of SpeechcamilaNo ratings yet
- Genetic Deafness in Pakistani PopulationDocument2 pagesGenetic Deafness in Pakistani PopulationZahid ShahNo ratings yet
- A Rare Case of Seven Siblings With Waardenburg Syndrome A Case Report. J Med Case Reports 12, 192 (2018) .Document5 pagesA Rare Case of Seven Siblings With Waardenburg Syndrome A Case Report. J Med Case Reports 12, 192 (2018) .Yu MinNo ratings yet
- Congenital MalformationsDocument9 pagesCongenital MalformationsibnuNo ratings yet
- Clinical Genetics - 2015 - Song - Hearing Loss in Waardenburg Syndrome A Systematic ReviewDocument10 pagesClinical Genetics - 2015 - Song - Hearing Loss in Waardenburg Syndrome A Systematic ReviewRawanNo ratings yet
- 9d7f PDFDocument4 pages9d7f PDFMubarak HazaziNo ratings yet
- Lecture 2 EnglishDocument24 pagesLecture 2 Englishmondalsawan96No ratings yet
- Kelainan GenetikDocument36 pagesKelainan GenetikImas Siti MNo ratings yet
- XYY SyndromeDocument4 pagesXYY SyndromesakuraleeshaoranNo ratings yet
- PROGERIADocument2 pagesPROGERIAeuchanNo ratings yet
- Genetic Disorders: U Me and SocietyDocument23 pagesGenetic Disorders: U Me and SocietyDeepansh GuptaNo ratings yet
- An Insight Into - Hemifacial MicrosomiaDocument6 pagesAn Insight Into - Hemifacial MicrosomiaIJAR JOURNALNo ratings yet
- Unit 3 Module 9 CombinedDocument14 pagesUnit 3 Module 9 Combinedapi-2930012170% (1)
- Unit 2 Classification of Language Abnormalities Based On EtiologyDocument33 pagesUnit 2 Classification of Language Abnormalities Based On Etiologyramandeep kaurNo ratings yet
- Menière's DiseaseDocument21 pagesMenière's DiseaseFelipeAsenjoÁlvarezNo ratings yet
- Fragile X Syndrome (Martin-Bell Syndrome)Document6 pagesFragile X Syndrome (Martin-Bell Syndrome)yudhi kurniawanNo ratings yet
- Genetic DiseaseDocument9 pagesGenetic DiseaseRAMAKRISHNANo ratings yet
- Lama 2 Gene Reviews Bookshelf - nbk97333Document25 pagesLama 2 Gene Reviews Bookshelf - nbk97333Didm S A MontNo ratings yet
- Fragile X Mental RetardationDocument8 pagesFragile X Mental RetardationFianirazhaPrimesaNo ratings yet
- Turner Syndrome Research PaperDocument7 pagesTurner Syndrome Research Paperapi-316370647100% (1)
- AP Biology Regulation Test ReviewDocument4 pagesAP Biology Regulation Test ReviewborntobewilderNo ratings yet
- Article Text 75576 1 10 20210527Document10 pagesArticle Text 75576 1 10 20210527Nimbus MultiversesNo ratings yet
- Cord Blood BankingDocument2 pagesCord Blood BankingKrystina ÜüNo ratings yet
- Congenital Fibrosis of The Extra-Ocular Muscles Syndrome Review ArticleDocument5 pagesCongenital Fibrosis of The Extra-Ocular Muscles Syndrome Review Articleanon_703701023No ratings yet
- Identi Fication of Pyridinium With Three Indole Moieties As An Antimicrobial AgentDocument5 pagesIdenti Fication of Pyridinium With Three Indole Moieties As An Antimicrobial AgentLuigi André Cabos ZavaletaNo ratings yet
- 5090 s04 QP 1Document20 pages5090 s04 QP 1mstudy123456No ratings yet
- SCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFDocument9 pagesSCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFlancetNo ratings yet
- Dapus 3 PDFDocument16 pagesDapus 3 PDFasengNo ratings yet
- Hnrs 199 Senior Capstone Project SQDocument24 pagesHnrs 199 Senior Capstone Project SQapi-618702342No ratings yet
- Unit 5 - Topic 4 PathologyDocument9 pagesUnit 5 - Topic 4 PathologyHùng Mạnh NguyễnNo ratings yet
- Lecture 1, Introduction To EndocrinologyDocument86 pagesLecture 1, Introduction To EndocrinologyAlexandru Ionut Popistaș100% (1)
- Alergi Susu SapiDocument2 pagesAlergi Susu SapiMaya FikriNo ratings yet
- BacteriaDocument1 pageBacteriaabdo aliNo ratings yet
- Iui Made Easy: Semen Analysis, Processing and PreservationDocument97 pagesIui Made Easy: Semen Analysis, Processing and PreservationSuryakant HayatnagarkarNo ratings yet
- Chapter 056Document42 pagesChapter 056Adistri KimNo ratings yet
- Guidelines RosaceaDocument14 pagesGuidelines Rosaceaika_anggrainiNo ratings yet
- BIOL 112 The Endocrine System PT 1..Document31 pagesBIOL 112 The Endocrine System PT 1..Khamron BridgewaterNo ratings yet
- Priority Value Tables by Testing DepartmentDocument8 pagesPriority Value Tables by Testing Departmentfreddy salcedoNo ratings yet
- WEEK 8 OTHER BLOOD GROUP SYSTEM PART 1 v2 PDFDocument6 pagesWEEK 8 OTHER BLOOD GROUP SYSTEM PART 1 v2 PDFjohn carlo cabanlitNo ratings yet
- 03 Intermediary MetabolismDocument10 pages03 Intermediary Metabolismhedayatinluv100% (1)
- Jof 07 00844 v2Document11 pagesJof 07 00844 v2Sonia HernándezNo ratings yet
- Mag Meet 2010 Abstract Booklet FinalDocument196 pagesMag Meet 2010 Abstract Booklet Finalabi_manyuNo ratings yet
- BME Chapter 17Document12 pagesBME Chapter 17nav4evrNo ratings yet
- Menopause Impacts Human Brain Structure, Connectivity, Energy Metabolism, and Amyloid-Beta DepositionDocument16 pagesMenopause Impacts Human Brain Structure, Connectivity, Energy Metabolism, and Amyloid-Beta Depositiondbozturk05No ratings yet
- Polymerase Chain Reaction & Types: Nandith P B Research ScholarDocument22 pagesPolymerase Chain Reaction & Types: Nandith P B Research ScholarNandit Banawalikar100% (1)
- Genome and StructureDocument1 pageGenome and Structuremanishkumar.allduniv4908No ratings yet
- Gene Technology Questions AQA OCR EdexcelDocument3 pagesGene Technology Questions AQA OCR EdexcelZainab AlziftawiNo ratings yet
- Antiviral Drugs Medical StudentsDocument59 pagesAntiviral Drugs Medical Studentstummalapalli venkateswara rao67% (3)
- JAKE GREEN - Lesson 14 Ihub Biology Unit1 Bend2Document15 pagesJAKE GREEN - Lesson 14 Ihub Biology Unit1 Bend2JAKE GREENNo ratings yet
Waardenburg Syndrome 2007
Waardenburg Syndrome 2007
Uploaded by
marikosvaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Waardenburg Syndrome 2007
Waardenburg Syndrome 2007
Uploaded by
marikosvaCopyright:
Available Formats
The British Journal of Developmental Disabilities Vol. 53, Part 1, JANUARY 2007, No. 104, pp.
53-62
CASE REPORT: ASSOCIATION OF WAARDENBURG SYNDROME WITH INTELLECTUAL DISABILITY, AUTISTIC SPECTRUM DISORDER AND UNPROVOKED AGGRESSIVE OUTBURSTS: A NEW BEHAVIOURAL PHENOTYPE?
Reza Kiani, Satheesh Kumar Gangadharan and Helen Miller
Introduction
Waardenburg syndrome (WS) is the most common inherited form of congenital deafness with a prevalence of about 1 in 42000 (Dourmishev and Janninger, 2005). Approximately 2-5% of congenital deafness is due to WS (Nayak and Isaacson, 2003). Deafness in this syndrome may be associated with changes in the eyes, hair or skin. The degree of hearing loss is almost always non-progressive but varies from mild to severe and may be unilateral or bilateral (Toriello et al., 1995). Four types of WS have been identified. The most common types of WS, type 1 (WS1) and 2 (WS2), are associated with more severe
hearing impairment. The prevalence of hearing impairment is higher in patients with WS2 than in those with WS1. Affected individuals may also have other congenital defects such as cleft palate /lip. The mortality rate, however, is similar to general population (Schwartz et al., 2006). In 1947, Dutch ophthalmologist, Petrus Johannes Waardenburg described the main features of WS as congenital sensory neural hearing loss, dystopia canthorum (lateral displacement of the inner corner of the eyes), hairy and hypo pigmented body, premature greying of hair with white forelock, synophrys (bushy eyebrows which join each other in the midline), blue eyes and pigmentary differences in the iris
*Reza Kiani, MD, MRCPsych Specialist Registrar/Honorary Lecturer in Psychiatry of Learning Disability, and Honorary Specialist Registrar, National Deaf Services. Leicester Frith Hospital, Leicester, UK Tel: 0116 225 5273 Fax: 0116 225 5272 email: drreki@yahoo.co.uk Satheesh Kumar Gangadharan, MD, MRCPsych Consultant in Psychiatry of Learning Disability, Leicester Frith Hospital, Leicester, UK Tel: 0116 225 5273 Fax: 0116 225 5272 email: satmini@yahoo.com Helen Miller, MRCPsych Consultant Psychiatrist, National Deaf Services, South West London and St Georges Mental Health Services, London, UK Tel: 020 8675 2100 Fax: 020 8675 2266 email: helen.miller@swlstg-tr.nhs.uk * For Correspondence
53
(heterochromia iridium), broad high nasal root and hypoplasia of the nasal septum (Waardenburg, 1951). This eventually became WS type 1 (WS1). Waardenburg syndrome type 2 (WS2) was defined by Arias in 1971. Patients with WS2 have all the features of WS1 except dystopia canthorum. Waardenburg syndrome type 3 (WS3), also known as Klein-Waardenburg syndrome has a similar phenotype to WS1 but with additional musculoskeletal characteristics, including Sprengel shoulder (congenital upward displacement of the shoulder blade), limb muscle hypoplasia, contractures, aplasia of the ribs, lack of differentiation of the small carpal bones and bilateral cutaneous syndactyly (webbing of the fingers) (Klein, 1983). Waardenburg syndrome type 4 (WS4), or Waardenburg-Shah syndrome, has features of WS2 combined with Hirschsprung disease (a congenital lack of the nerve supply of the intestinal wall, which leads to chronic constipation, vomiting and intestinal obstruction during infancy) (Dourmishev and Janninger, 2005). TABLE I shows the clinical features of the different types of WS.
Modes of inheritance in WS
The reason for the physical manifestation of WS is the absence of melanocytes in the inner ear (cochlea), skin, eyes and hair. Melanocytes are required in the vascular layer of the cochlea for hearing (Steel et al., 1989). While the first three types of WS have autosomal dominant inheritance (a child of one affected parent has a 50% risk of developing WS), WS4 has an autosomal recessive inheritance (a child of one
affected parent has a 25% risk of developing WS). WS may also be the product of de novo mutations (i.e. without having an affected mother or father). Several mutations in the PAX3 gene (located on chromosome band 2q35) have been noted in people with WS1 and WS2. The gene PAX3 helps in the activation of the MITF promoter (microphthalmiaassociated transcription factor). MITF has a role in the activation of the tyrosinase gene, which is involved in melanocyte differentiation. A mutation in the PAX3 gene therefore results in abnormalities of melanocyte differentiation (Watanabe et al., 1998). Abnormalities in melanocyte development in the skin, hair, eyes and inner ear lead to the physical manifestations. In some cases of WS2, mutations occur in the MITF gene itself (Jones, 1997). Mutations in other genes such as SNAI2 (Frith et al., 2005) and SLUG (Cryns and Van Camp, 2004) have also been reported. Genes affected in WS4 are either the Endothelin-3 (EDN3) or the EndothelinB receptor (EDNRB) genes (Edery et al., 1996). While homozygous mutation of these genes causes WS4, heterozygous mutation results in Hirschsprung disease alone (Schwartz et al., 2006). Mutation of the SOX10 gene has also been reported in individuals with WS4 (Pingault et al., 1998). TABLE II presents a summary of chromosomal and genetic abnormalities in WS.
Association of WS with intellectual disability
There is limited evidence for an association between WS and intellectual impairment. Some researchers have reported that WS does not affect intelligence (Smith et al., 1998). A study
54
evaluating the clinical features of 11 affected families (with a total of 52 individuals) found delayed milestones or poor school performance necessitating special schooling in 9 unrelated individuals with WS1 or WS2 patients (de Saxe, 1984). There is a case report of a 13-year-old boy where features of WS are associated with marked mental and motor retardation, severe gait disturbance, dystonia, muscular stiffness and peripheral neuropathy (Kawabata et al., 1987). Another case report describes a patient with WS3 who had microcephaly, mental retardation and severe skeletal abnormalities (Pasteris et al., 1993). Similarly, little is known about the prevalence of mental health problems or autistic spectrum disorder in people with WS. There is only one report in the literature about the association with psychiatric disorders (Siedlecka and
Smolenska, 1997). In this paper we describe two individuals with WS3 and profound bilateral deafness. We then explore the possibility of new behavioural phenotypes in this condition since both individuals present with moderate to severe intellectual disability, autistic spectrum disorder (ASD) and severe behavioural problems (TABLE III).
Case Histories
Case One
The first case, X, is a 36 year old south Asian male who has had profound hearing loss since birth. He appears to have WS3 as he has all the characteristics of WS1 associated with repeated dislocation of the
TABLE I Distinguishing features in different types of Waardenburg syndrome (WS)
WS1 WS2 WS3 WS4
Sensory neural hearing loss Dystopia canthorum Hirschsprung disease Musculoskeletal abnormalities
+/+ -
+/-
+/+ +
+/_ + -
TABLE II Genetic and chromosomal abnormalities in Waardenburg Syndrome
Type of WS Mode of inheritance Chromosomes (involved) Genes (involved)
WS1 & WS3 WS2
Autosomal dominant Autosomal dominant
2q35 3p12.3 - 14.1 1p21 - p13.3
PAX3 (Paired box gene 3) MITF (Microphthalmia-associated transcription factor) SNAI2 SLUG Endothelin-3 receptor (EDNR 3) Endothelin-B receptor (EDNRB)
WS4
Autosomal recessive
20q13.2 - q13.3 13q22
55
TABLE III Clinical characteristics of the reported patients with WS3
Case 1 Case 2
Facial features Broad high nasal root Synophrys or medial flaring of the eyebrows Hypoplastic alae nasi Dystopia canthrum Hypopigmentation Hypopigmentation of skin White forelock White body hair, eyebrows Eyes Heterochromia iridium Brilliant blue eyes Sensory neural hearing loss Unilateral/ bilateral Severity Musculoskeletal problems Sprengel shoulder Cleft lip or palate Hirschsprung disease Muscle contractures Limb muscle hypoplasia Other abnormalities Intellectual disability Medical problems Autistic spectrum disorder Severity of autistic traits Unpredicted violent outbursts Epilepsy Affected family member Medical conditions in the family
+ + + + + + + + bilateral profound + moderate + moderate + father and sisters diabetes mellitus hypothyroidism psoriasis keratoconus epilepsy
+ + + + + + + + bilateral profound + severe diabetes mellitus, psoriasis + severe + -
56
shoulder. He also has moderate intellectual disability and moderate autistic trait based on the Childhood Autism Rating Scale (CARS). Although there is a history of developmental delay, detailed information regarding his early development is not available. He is the second oldest child in a family of six. His father and two siblings also have features of WS1 but without any hearing impairment or intellectual disability. X has been profoundly deaf since childhood. He cannot hear or produce spoken language. Although he can understand and use basic British Sign Language and Makaton, his ability to sign is very limited. His level of understanding of sign language is higher than his expressive skills. He is physically fit and manages most daily living activities without assistance. He can write a few words and draw pictures to communicate. He has a longstanding history of severe aggressive behaviour. When he began special school at the age of 5, he was reported as having disturbed behaviour such as smashing windows, pulling hair and inappropriate urination. He subsequently attended a residential school for children with hearing impairments until he completed schooling. Although the majority of the incidents were aggression against objects such as smashing windows and destroying furniture, there were also documented episodes of very severe aggressive behaviour toward people, including stabbing a person with a kitchen knife, hitting another with a garden fork and pouring boiling water over a third person. He generally had a tendency to target the most vulnerable people such as the more disabled or female residents. Although X was prescribed various antipsychotic drugs for his aggressive outbursts, there is
no indication of any clear benefit from any medication. He recently required hospitalisation under Mental Health Act subsequent to breakdown of his long-term placement and a series of aggressive behaviour in a temporary placement. He displayed unprovoked violent episodes including throwing a coffee table aimed at a resident, pushing a female resident against the wall and smashing a plate on another residents head. In the hospital, with one-to-one support, a consistent approach, firm boundaries and a structured daily routine, he settled over a few weeks. He enjoys outdoor activities, watching television and doing puzzles. However, he continues to have occasional aggressive outbursts. Although most of these incidents appear to have been impulsive aggression without any obvious precipitating factors, a few incidents may have involved some premeditation. Often Xs facial expression is misleading, for example when he appears to be smiling and friendly just before an attack. Xs hearing impairment made assessment of any features of ASD difficult. However, the presence of ASD symptoms became clearer over time as his stereotyped communication patterns, rigid adherence to routine, ritualistic tidying and preoccupation with dates and events were recognised. He is very sensitive to changes in the environment and prefers to have his belongings arranged in order. He may become preoccupied with certain events that are important to him and repeatedly signs to confirm that they will happen. He has limited interest in other peoples activities. His social communication has always been difficult as he does not maintain a good eye contact and lacks concentration. Subsequent assessment by the professionals from the National Deaf
57
Services confirmed the presence of autistic traits. He was found to be using signs in a stereotyped manner. He tends to copy signs used by others (echolalia) and continually repeats some signs (perseveration). When writings, he always refer to himself by name rather than using I.
Case two
Y is a 29-year-old white male with WS3. He has profound bilateral deafness, crystal blue irises, dystopia cantrum, early greying of his hair and muscular dysplasia of his limbs (his arms and legs are very thin due to loss of muscle bulk). He has severe intellectual disability and severe traits of ASD based on CARS. He also suffers from psoriasis and diabetes mellitus (DM). He is long-sighted and has astigmatism. There is no family history of WS or associated psychiatric and medical disorders. Y was born in a normal delivery but showed delay in his developmental milestones. His hearing impairment was picked up in his second year of life after his family suspected that he was not reacting to others in a usual way. After attending a special needs school for a short period, he joined a deaf signing school. Reports from the school suggest that he was very settled there, with no report of challenging behaviour before he was 18. After leaving school, he stayed briefly in two residential homes, with his mother and in foster care. Around this time he developed challenging behaviour such as aggression towards others, destroying property and stealing food. After a twoyear stay in an assessment and treatment unit, he was moved to a residential place for deaf people. Although he settled down there initially, his challenging behaviour gradually began to re-emerge. He would
clean in a driven and repetitive manner and, if he was interrupted, he would become extremely upset and aggressive. Sometimes incidents happened out of the blue for no apparent reason. The violent outbursts tended to be towards the female staff and those who were significantly smaller than him. There was no evidence of depression. Although initially the presence of ritualistic and repetitive behaviours suggested a diagnosed of obsessive compulsive disorder, a detailed assessment by professionals from The National Deaf Services revealed that his ritualistic behaviours were part of autistic spectrum disorder. It was noticed that the challenging behaviours increased when he was uncertain about a situation and the boundaries were unclear. Y was also noted to be extremely tidy. He kept his personal belongings in a particular order. Any change in his room or routine led to him becoming distressed and aggressive. When he became anxious, he started cleaning his room. If he was interrupted, he would become extremely agitated and violent. According to his mother, he as a child, preferred his own company and to play alone. He preferred soft cuddly toys and would not play with other toys. Even now as an adult, he keeps a soft toy in his pocket and carries it everywhere he goes. From time to time, he needs to touch it and smell it. When he is anxious he moves the toy in front of his eyes in a flicking movement. He does not make good eye-to-eye contact. He also does not respect others personal space and often walks into other service users bedrooms inappropriately. He had been tried on different psychotropic drugs in the past without any clear benefit. These included carbamazepine (used as mood stabiliser), various selective serotonin reuptake
58
inhibitors and risperidone. The multidisciplinary team, therefore, decided to concentrate more on the behavioural management of his challenging behaviours. The medication was gradually tapered and stopped completely. Using picture books and involving staff who were fluent in British Sign Language improved Ys communication skills. It was also advised not to challenge him during the times that he was cleaning as it was thought that this gave him a sense of control. This was regarded as an important coping strategy for him. Limit setting was, however, used to minimise the impact of this behaviour on other activities. It was also noticed that Y used to sweat during some of the episodes. Aggression occurred on occasions when he wanted food but could not have it. The role of diabetes mellitus was also explored as a possible contributing factor to some of his unpredictable behaviours. In his management plan, he was encouraged to take regular snacks to avoid hypoglycaemic episodes. Y currently participates in various daily activities including swimming, bowling, working on the computer, doing puzzles and going out for lunch. His diabetes has been controlled by dietary restriction. The psychological strategies aimed at increasing his level of communication such as Treatment and Education of Autistic and related Communication Handicapped Children (TEACCH) and modifying his behaviour through firm boundaries, structured daily routine and positive response strategies have generally been successful.
Discussion
WS has been associated with cognitive delay and other neurological abnormalities
(de Saxe, 1984, Kawabata et al., 1987). Our case report highlights the presence of moderate to severe intellectual disability (ID), autistic spectrum disorder (ASD) and severe problem behaviours in two individuals with profound bilateral congenital deafness secondary to WS3. To the best of our knowledge, this association has not been reported elsewhere in the literature. We believe that there is a striking similarity in the presentation of these two individuals raising the possibility of a behavioural phenotype (the presence of ASD and impulsive aggression). ASD is described as a part of the behavioural phenotype of tuberous sclerosis, fragile-X syndrome, congenital rubella and herpes simplex encephalitis (Melville and Cameron, 2003). Impulse control disorder has also been described as being part of certain genetic syndromes such as tuberous sclerosis (Sadock and Sadock, 2003). Challenging behaviours are, however, common in people with ID, ASD or hearing impairment (Timehin and Timehin, 2004). In exploring the possible association of a behavioural phenotype of a genetic disorder with ID, the first issue to consider is whether the observed behaviour is a reflection of the severity of ID (OBrien, 2006). Therefore, it is possible that in our case reports, the apparent association between WS3 and ASD has arisen by chance, as people with ID have higher prevalence of ASD than the general population (Bhaumik et al., 1997). ASD occurs in about 10% of people with mild ID (IQ 50-69) (Gillberg, 1992), increasing to 27% in those with an IQ of less than 50 (Deb and Prasad, 1994). Equally, there is an association between ASD and hearing impairment (HI), as the rate of HI is higher in people with ASD than general population and vice versa. Rosenhall et al., (1999) reported a
59
prevalence rate of 3.5% for profound HI in 199 children with a diagnosis of ASD (quoted in Carvill, 2001). Furthermore, there are similarities between behaviours in children with a visual and HI and in those with ASD. Children with a profound hearing loss who have not had access to a good language model (i.e. sign language) may show delayed or impaired social and emotional development (e.g. theory of mind and understanding others verbal and non-verbal cues). Deaf children may also have to impose clear structure, predictable routines and restrictive behavioural patterns to their daily living activities to be able to make sense of the world around them and to feel safe and in control (Edwards, 2004). Given the above confounding factors, it is difficult to establish the presence of a behaviour phenotype based on a report of two individuals with striking similarities. Diagnosis of ASD was crucial to the effective management of behaviour problems in both the individuals. This report highlights the need for further research to estimate the prevalence of ASD in people with WS. We believe that it is possible that ASD is under-diagnosed in people with WS due to their hearing impairment. Jure et al (1991), reporting a prevalence of 4% ASD in a sample of 1150 children with HI, found that in substantial proportion of them, ASD was diagnosed with an average four years delay. Conversely, hearing impairment had been overlooked for up to six years in some of the children with ASD (quoted in Carvill, 2001). The above association is also of interest from a genetic point of view. A number of studies have ascertained associations of ASD traits with terminal 2q deletion (with the breakpoint within 2q37). Lukusa et al. (2004) describe a 12-year-old female patient with terminal 2q37.3 cryptic deletion and ASD behaviour. There is also another
report of a child with a cryptic deletion of 2q35 including part of the PAX3 gene and a balanced 2; 8 translocation. Although not qualified for a diagnosis of WS, the child had ASD and very mild dystopia canthorum (one of the characteristic features of WS1 and 2). They speculated that a gene or genes responsible for ASD may lie at 2q35 (PAX 3 gene) or at the sight of the translocation (Borg et al., 2002).
Conclusion
In both individuals reported in this paper, a diagnosis of ASD had been either missed or not given enough consideration until early adulthood. This had, over the years, led to the breakdown of their care packages due to the display of severe challenging behaviours. Although it is difficult to draw any conclusions from these associations found in just two individuals with WS3, we believe that it is worthwhile reporting these cases, both to ensure that additional diagnoses of ID and ASD are not missed in people with WS3 and, most importantly, to inform and pave the way for early and appropriate intervention. Whether WS in our patients per se has been the cause of ASD directly or has increased the chance of ASD by causing ID and HI is not clear and a matter of further investigation and research.
Summary
There is little information available on psychiatric aspects of Waardenburg Syndrome. The present paper highlights the possible association of Warrdenburg Syndrome type 3 in two individuals with
60
profound bilateral congenital deafness, intellectual disability, autistic spectrum disorder and severe aggressive behaviour. There is a striking resemblance in clinical presentation in both individuals. The paper gives an overview of the syndrome; focuses on the presence of intellectual disability, autistic spectrum disorder, aggressive outbursts and their complex relationship in the individuals; and explores the possibility of a new behavioural phenotype in Waardenburg syndrome type 3.
Dourmishev, L. A. and Janninger, C. K. (2005). Waardenburg Syndrome. emedicine (Online), instant access to the mind of medicine. Edery, P Attie, T., Amiel, J., Pelet, A., Eng, C., ., Hofetra, R. M. W., Martelli, H., Bidaud, C., Munnich, A. and Lyonnet, S. (1996). Mutation of the endothelin-3 gene in the Waardenburg-Hirschsprung disease (ShahWaardenburg syndrome). Nature Genetics, 12, 442 4. Edwards, L. (2004). Neurophysiological development of hearing impaired children. Deafness in mind. Whurr publishers, 138140. Frith, H., Hurst, J. and Hall, J. (2005). Severe deafness in early childhood. Oxford desk reference Clinical Genetics, Oxford University Press 91 2. Gillberg, C. (1992). The Emmanual Miller Lecture 1991. Autism and autistic-like conditions: subclasses among disorders of empathy. Journal of Child Psychology and Psychiatry, 32, 79-108. Jones, K. L. (1997). Waardenburg syndrome. Smiths recognizable pattern of human malformation. Saunders, 248 9. Jure, R., Rapin, I. and Tuchman, R. F. (1991). Hearing impaired autistic children. Developmental Medicine and Child Neurology, 33, 1062-72. Kawabata, E., Ohba, N., Nakamura, A., Izumo, S. and Osame, M. (1987). Waardenburg syndrome: A variant with neurological impairment. Ophthalmic Paediatric Genetics, 8, 165-70. Klein, D. (1983). Historical background and evidence for dominant inheritance of the Klein-Waardenburg syndrome (type III) American Journal of Medical Genetics, 14, 23139. Lukusa, T., Vermeesch, J. R., Holvoet, M., Fryns, J. P and Devriendt, K. (2004). Deletion . 2q37.3 and autism: molecular cytogenetic mapping of the candidate region for autistic disorder. Genetic Counselling, 15, 293-301. Melville, C. and Cameron, J. (2003). Autism, Seminars in the psychiatry of learning disabilities. Gaskell publication, 124. Nayak, C. S. and Isaacson, G. (2003). Worldwide distribution of Waardenburg Syndrome. The
References
Arias, S. (1971). Genetic heterogeneity in the Waardenburg syndrome. Birth Defects Original Article Series, 7, 87-101. Bhaumik, S., Branford, D., McGrother, C. and Thorp, C. (1997). Autistic traits in adults with learning disabilities. British Journal of Psychiatry, 170, 502 -6. Borg, I., Squire, M., Menzel, C., Stout, K., Morgan, D., Willatt, L., O, Brien, P C., . Ferguson-Smith, M. A., Ropers, H. H., Tommerup, N., Kalscheuer, V M. and . Sargan, D. R. (2002). A cryptic deletion of 2q35 including part of the PAX3gene detected by breakpoint mapping in a child with autism and a de novo2; 8 translocation. Journal of Medical Genetics, 39, 391 9. Carvill, S. (2001). Sensory impairment, intellectual disability and psychiatry. Journal of Intellectual Disability and Research, 45, 46783. Cryns, K. and van Camp, G. (2004). Deafness genes and their diagnostic applications. Audiology & Neurotology, 9, 2-15. Deb, S. and Prasad, K. B. (1994). The prevalence of autistic disorder among children with a learning disability. British Journal of Psychiatry, 165, 395 -9. de Saxe, M., Kromber, J. G. and Jenkins, T. (1984). Waardenburg syndrome in South Africa. Part 1. An evaluation of the clinical findings in 11 families. South African Medical Journal, 66, 256-61.
61
Annals of Otology, Rhinology and Laryngology, 112, 817 20. OBrian, G. (2006). Behavioural phenotypes: causes and clinical implications. Advances in Psychiatric Treatment, 12, 338-348. Pasteris, N. G., Trask, B J., Sheldon, S. and Gorskl, J. L. (1993). Discordant Phenotype of two overlapping deletions involving the PAX3 gene in chromosome 2q35. Human Molecular Genetics, 2 , 953 9. Pingault, V Bondurand, N., Kuhlbrodt, K., ., Goerich, D. E., Prhu, M. O., Puliti, A., Herbarth, B., Hermans-Borgmeyer, I., Legius, E., Matthijs, G., Amiel, J., Lyonnet, S., Ceccherini, I., Romeo, G., Clayton Smith, J., Read, A. P Wegner, M. and ., Goossens, M. (1998). SOX10 mutations in patients with Waardenburg- Hirschsprung disease. Nature Genetics, 18, 171 3. Rosenhall, U., Nordin, V Sandstrom, M., ., Ahlsen, G. and Gillberg, C. (1999). Autism and hearing loss. Journal of Autism and Developmental Disorder, 29, 349- 57. Sadock, B. J. and Sadock, V A. (2003). Mental . Retardation. Kaplan and Sadocks Synopsis of Psychiatry. Lippincot, Williams and Wilkins. 1171- 2. Schwartz, R. A., Jozwiak, S., Bason, L. and Krantz, I. (2006). Waardenburg Syndrome. emedicine (Online), Instant access to the mind of medicine. Siedlecka, H. and Smolenska, J. (1997). Waardenburg syndrome with coexisting psychiatric disorders. Developmental Brain Dysfunction, 10, 240-247. Smith, S., Klodziej, P and Olney, A. H. (1998). . Waardenburg syndrome. Ear, Nose and Throat Journal, 77, 257 258. Steel, K. P and Barkway, C. (1989). Another . role for melanocytes: their importance for normal stria vascularis development in the mammalian inner ear. Development, 107, 453 63. Timehin, C. and Timehin, E. (2004). Prevalence of hearing impairment in a community population of adults with Learning Disability. British Journal of Learning Disabilities, 32, 203. Toriello, H. V Reardon, W. and Gorlin, R. ., J. (2004). Hereditary hearing loss and its syndromes. Oxford University Press.
Waardenburg, P J. (1951). A new syndrome . combining developmental anomalies of the eyelids, eyebrows and nose root with pigmentary defects of the iris and head hair and with congenital deafness. American Journal of Human Genetics, 3, 195 253. Watanabe, A, Takeda, K., Ploplis, B. and Tashibana, M. (1998). Epistatic relationship between Waardenburg syndrome genes MITF and PAX3. Nature Genetics, 18, 283 6.
62
You might also like
- Oet ReadingDocument15 pagesOet Readingnj0% (1)
- Syndromes Aarskog Syndrome (9p)Document10 pagesSyndromes Aarskog Syndrome (9p)M BeirutiNo ratings yet
- Syndromic Deafness - Variant of Waardenburg Syndrome: Dr. Basavaraj Belaldavar Dr. Vini BalakrishnanDocument5 pagesSyndromic Deafness - Variant of Waardenburg Syndrome: Dr. Basavaraj Belaldavar Dr. Vini BalakrishnaninventionjournalsNo ratings yet
- Rehab AnswerDocument8 pagesRehab AnswerFardeen RafiqueNo ratings yet
- Sdarticle PDFDocument9 pagesSdarticle PDFManjeev GuragainNo ratings yet
- An Example of The Utility of Genomic Analysis For Fast and Accurate Clinical Diagnosis of Complex Rare PhenotypesDocument8 pagesAn Example of The Utility of Genomic Analysis For Fast and Accurate Clinical Diagnosis of Complex Rare PhenotypesGlauce L TrevisanNo ratings yet
- Management of Spasticity and Cerebral Palsy: Yasser Awaad, Tamer Rizk and Emira ŠvrakaDocument26 pagesManagement of Spasticity and Cerebral Palsy: Yasser Awaad, Tamer Rizk and Emira ŠvrakaAgnimitra ChoudhuryNo ratings yet
- Genetic Causes of Syndromic and Non-Syndromic Autism PDFDocument9 pagesGenetic Causes of Syndromic and Non-Syndromic Autism PDFRaisa CoppolaNo ratings yet
- Nance - The Genetics of DeafnessDocument11 pagesNance - The Genetics of DeafnessPablo VasquezNo ratings yet
- Autism Spectrum Disorders: Dr.R.G.Enoch MD Psychiatry Ii Yr GMKMCH, SalemDocument100 pagesAutism Spectrum Disorders: Dr.R.G.Enoch MD Psychiatry Ii Yr GMKMCH, Salemام اسامة السيايدةNo ratings yet
- Human GeneticsDocument9 pagesHuman Geneticseli pascualNo ratings yet
- Shapiro 1997Document6 pagesShapiro 1997JohnnyNo ratings yet
- Genetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LossDocument12 pagesGenetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LosssherinNo ratings yet
- Williams Syndrome FinalDocument10 pagesWilliams Syndrome Finalkab5405No ratings yet
- Uk Fragile XDocument4 pagesUk Fragile XChristin Natalia KalembangNo ratings yet
- Wassink 2001Document8 pagesWassink 2001Marcelo ClaroNo ratings yet
- E472 FullDocument17 pagesE472 FullC_DanteNo ratings yet
- Waardenburg Syndrome in An Infant of Diabetic MotherDocument5 pagesWaardenburg Syndrome in An Infant of Diabetic Motherराजीव गुप्ताNo ratings yet
- Matsy CytoDocument7 pagesMatsy CytoDarem SoNo ratings yet
- SyndromesDocument19 pagesSyndromesapi-26826496No ratings yet
- Orphanet Journal of Rare Diseases: Walker-Warburg SyndromeDocument5 pagesOrphanet Journal of Rare Diseases: Walker-Warburg SyndromeLópez Ruelas Mónica AzenethNo ratings yet
- VACTERL-Hydrocephaly, DK-Phocomelia, and Cerebro-Cardio-Radio-Reno-Rectal CommunityDocument6 pagesVACTERL-Hydrocephaly, DK-Phocomelia, and Cerebro-Cardio-Radio-Reno-Rectal CommunitySarly FebrianaNo ratings yet
- Research Synthesis PaperDocument9 pagesResearch Synthesis PaperFiona De CastroNo ratings yet
- Numerical - 1: Structural - 2Document9 pagesNumerical - 1: Structural - 2Khaled Zeama100% (1)
- Trisomy 8 Mosaicism Syndrome: Case ReportDocument4 pagesTrisomy 8 Mosaicism Syndrome: Case ReportIoanna DivriotiNo ratings yet
- Sordera SindromicaDocument8 pagesSordera SindromicaFabian Camelo OtorrinoNo ratings yet
- Resarch Assignment PhysDocument6 pagesResarch Assignment Physapi-547006629No ratings yet
- Tay-Sachs Disease Is A: o o o o o o o oDocument7 pagesTay-Sachs Disease Is A: o o o o o o o oShuaib SiddiquiNo ratings yet
- Patterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyaDocument60 pagesPatterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyavipinNo ratings yet
- Klinefelter Syndrome and Associated Fragile-X Syndrome: Case II-5Document8 pagesKlinefelter Syndrome and Associated Fragile-X Syndrome: Case II-5صادقNo ratings yet
- 2 - Fragile X SyndromeDocument4 pages2 - Fragile X Syndromechenelyn_15No ratings yet
- Kabuki SyndomeDocument104 pagesKabuki SyndomeKim LianNo ratings yet
- Ajmg A 34257 PDFDocument3 pagesAjmg A 34257 PDFdtf1007No ratings yet
- Sudden Infant Death Syndrome: Case-Control Frequency Differences at Genes Pertinent To Early Autonomic Nervous System Embryologic DevelopmentDocument5 pagesSudden Infant Death Syndrome: Case-Control Frequency Differences at Genes Pertinent To Early Autonomic Nervous System Embryologic DevelopmentJailyn Carrasquel HerreraNo ratings yet
- Fragile X SyndromeDocument8 pagesFragile X SyndromeMay Pearl NuñalNo ratings yet
- A Case Study About Klinefelter SyndromeDocument7 pagesA Case Study About Klinefelter SyndromehoyNo ratings yet
- Genetic Disorder Research Assignment - SohrabDocument6 pagesGenetic Disorder Research Assignment - SohrabSohrab AliNo ratings yet
- Review and Update of Mutations Causing Waardenburg Syndrome: Human MutationDocument16 pagesReview and Update of Mutations Causing Waardenburg Syndrome: Human MutationIso MogoNo ratings yet
- Mendelian Disorders Class 12Document22 pagesMendelian Disorders Class 12Harith KumarNo ratings yet
- A Case Study About Klinefelter SyndromeDocument6 pagesA Case Study About Klinefelter Syndromehoy100% (1)
- Cognitive, Linguistic, and Motor Abilities in A Multigenerational Family With Childhood Apraxia of SpeechDocument20 pagesCognitive, Linguistic, and Motor Abilities in A Multigenerational Family With Childhood Apraxia of SpeechcamilaNo ratings yet
- Genetic Deafness in Pakistani PopulationDocument2 pagesGenetic Deafness in Pakistani PopulationZahid ShahNo ratings yet
- A Rare Case of Seven Siblings With Waardenburg Syndrome A Case Report. J Med Case Reports 12, 192 (2018) .Document5 pagesA Rare Case of Seven Siblings With Waardenburg Syndrome A Case Report. J Med Case Reports 12, 192 (2018) .Yu MinNo ratings yet
- Congenital MalformationsDocument9 pagesCongenital MalformationsibnuNo ratings yet
- Clinical Genetics - 2015 - Song - Hearing Loss in Waardenburg Syndrome A Systematic ReviewDocument10 pagesClinical Genetics - 2015 - Song - Hearing Loss in Waardenburg Syndrome A Systematic ReviewRawanNo ratings yet
- 9d7f PDFDocument4 pages9d7f PDFMubarak HazaziNo ratings yet
- Lecture 2 EnglishDocument24 pagesLecture 2 Englishmondalsawan96No ratings yet
- Kelainan GenetikDocument36 pagesKelainan GenetikImas Siti MNo ratings yet
- XYY SyndromeDocument4 pagesXYY SyndromesakuraleeshaoranNo ratings yet
- PROGERIADocument2 pagesPROGERIAeuchanNo ratings yet
- Genetic Disorders: U Me and SocietyDocument23 pagesGenetic Disorders: U Me and SocietyDeepansh GuptaNo ratings yet
- An Insight Into - Hemifacial MicrosomiaDocument6 pagesAn Insight Into - Hemifacial MicrosomiaIJAR JOURNALNo ratings yet
- Unit 3 Module 9 CombinedDocument14 pagesUnit 3 Module 9 Combinedapi-2930012170% (1)
- Unit 2 Classification of Language Abnormalities Based On EtiologyDocument33 pagesUnit 2 Classification of Language Abnormalities Based On Etiologyramandeep kaurNo ratings yet
- Menière's DiseaseDocument21 pagesMenière's DiseaseFelipeAsenjoÁlvarezNo ratings yet
- Fragile X Syndrome (Martin-Bell Syndrome)Document6 pagesFragile X Syndrome (Martin-Bell Syndrome)yudhi kurniawanNo ratings yet
- Genetic DiseaseDocument9 pagesGenetic DiseaseRAMAKRISHNANo ratings yet
- Lama 2 Gene Reviews Bookshelf - nbk97333Document25 pagesLama 2 Gene Reviews Bookshelf - nbk97333Didm S A MontNo ratings yet
- Fragile X Mental RetardationDocument8 pagesFragile X Mental RetardationFianirazhaPrimesaNo ratings yet
- Turner Syndrome Research PaperDocument7 pagesTurner Syndrome Research Paperapi-316370647100% (1)
- AP Biology Regulation Test ReviewDocument4 pagesAP Biology Regulation Test ReviewborntobewilderNo ratings yet
- Article Text 75576 1 10 20210527Document10 pagesArticle Text 75576 1 10 20210527Nimbus MultiversesNo ratings yet
- Cord Blood BankingDocument2 pagesCord Blood BankingKrystina ÜüNo ratings yet
- Congenital Fibrosis of The Extra-Ocular Muscles Syndrome Review ArticleDocument5 pagesCongenital Fibrosis of The Extra-Ocular Muscles Syndrome Review Articleanon_703701023No ratings yet
- Identi Fication of Pyridinium With Three Indole Moieties As An Antimicrobial AgentDocument5 pagesIdenti Fication of Pyridinium With Three Indole Moieties As An Antimicrobial AgentLuigi André Cabos ZavaletaNo ratings yet
- 5090 s04 QP 1Document20 pages5090 s04 QP 1mstudy123456No ratings yet
- SCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFDocument9 pagesSCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFlancetNo ratings yet
- Dapus 3 PDFDocument16 pagesDapus 3 PDFasengNo ratings yet
- Hnrs 199 Senior Capstone Project SQDocument24 pagesHnrs 199 Senior Capstone Project SQapi-618702342No ratings yet
- Unit 5 - Topic 4 PathologyDocument9 pagesUnit 5 - Topic 4 PathologyHùng Mạnh NguyễnNo ratings yet
- Lecture 1, Introduction To EndocrinologyDocument86 pagesLecture 1, Introduction To EndocrinologyAlexandru Ionut Popistaș100% (1)
- Alergi Susu SapiDocument2 pagesAlergi Susu SapiMaya FikriNo ratings yet
- BacteriaDocument1 pageBacteriaabdo aliNo ratings yet
- Iui Made Easy: Semen Analysis, Processing and PreservationDocument97 pagesIui Made Easy: Semen Analysis, Processing and PreservationSuryakant HayatnagarkarNo ratings yet
- Chapter 056Document42 pagesChapter 056Adistri KimNo ratings yet
- Guidelines RosaceaDocument14 pagesGuidelines Rosaceaika_anggrainiNo ratings yet
- BIOL 112 The Endocrine System PT 1..Document31 pagesBIOL 112 The Endocrine System PT 1..Khamron BridgewaterNo ratings yet
- Priority Value Tables by Testing DepartmentDocument8 pagesPriority Value Tables by Testing Departmentfreddy salcedoNo ratings yet
- WEEK 8 OTHER BLOOD GROUP SYSTEM PART 1 v2 PDFDocument6 pagesWEEK 8 OTHER BLOOD GROUP SYSTEM PART 1 v2 PDFjohn carlo cabanlitNo ratings yet
- 03 Intermediary MetabolismDocument10 pages03 Intermediary Metabolismhedayatinluv100% (1)
- Jof 07 00844 v2Document11 pagesJof 07 00844 v2Sonia HernándezNo ratings yet
- Mag Meet 2010 Abstract Booklet FinalDocument196 pagesMag Meet 2010 Abstract Booklet Finalabi_manyuNo ratings yet
- BME Chapter 17Document12 pagesBME Chapter 17nav4evrNo ratings yet
- Menopause Impacts Human Brain Structure, Connectivity, Energy Metabolism, and Amyloid-Beta DepositionDocument16 pagesMenopause Impacts Human Brain Structure, Connectivity, Energy Metabolism, and Amyloid-Beta Depositiondbozturk05No ratings yet
- Polymerase Chain Reaction & Types: Nandith P B Research ScholarDocument22 pagesPolymerase Chain Reaction & Types: Nandith P B Research ScholarNandit Banawalikar100% (1)
- Genome and StructureDocument1 pageGenome and Structuremanishkumar.allduniv4908No ratings yet
- Gene Technology Questions AQA OCR EdexcelDocument3 pagesGene Technology Questions AQA OCR EdexcelZainab AlziftawiNo ratings yet
- Antiviral Drugs Medical StudentsDocument59 pagesAntiviral Drugs Medical Studentstummalapalli venkateswara rao67% (3)
- JAKE GREEN - Lesson 14 Ihub Biology Unit1 Bend2Document15 pagesJAKE GREEN - Lesson 14 Ihub Biology Unit1 Bend2JAKE GREENNo ratings yet