Professional Documents
Culture Documents
Typical Responses To Crisis
Typical Responses To Crisis
Uploaded by
Ahmadz Cha'emOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Typical Responses To Crisis
Typical Responses To Crisis
Uploaded by
Ahmadz Cha'emCopyright:
Available Formats
The degree of stress experienced in coping with the unexpected crisis will interact with the life cycle
stage and the social situation to influence the individual's coping ability.
Typical responses to crisis These behaviors may alert you to the fact that someone is experiencing a crisis (Hansel, 1976). The person shows a preoccupation with the crisis situation and talks about the event, not attending to other issues. She feels isolated, alone and distant and may be cut off from friends and relative.. This occurs because the person in crisis is fearful that she cannot live up to the rules and expectations about behavior in asocial interaction at this time. She is likely to cry at work or when out with friends or to withdraw or to be unable to think clearly. Nonetheless, the need for closeness is shown by the way the person uses touch and eye contact, standing near, disclosing deep information and using intimate language. She is looking for warmth and comfort from someone, particularly those she thinks might be able to help resolve the crisis. There is a loss of confidence, with a less sure feeling about herself and a heightened sensitivity to the judgments of others. It is important to help this person find the positive in herself and work with the person's strengths rather than reinforce her perception of weakness and lack of self, experienced at this time. A crisis often shows in random and unexpected behaviors that do not conform to role expectations. A person in crisis is open to trying. out new roles due to the disruption of clear identity. People in this crisis environment need to be very aware of this. This willingness to try new roles can be helpful and allow for change and growth as a result of crisis. It can be unhelpful if the roles suggested and taken on are restricting or even dysfunctional. Becoming mentally or physically ill, taking on the sick role, may or may not prove constructive. The significant people in the person's life may help or hinder the person in crisis. The resolution of the crisis will be affected by these close networks of people. They may be accepting and tolerant of distress, yet reinforce
effective behavior. If the person distances too far from them they may be hurt and reject the person in crisis. If the crisis continues and new behavior becomes entrenched which the significant other people disapprove of they may withdraw from the individual. Change is not necessarily encouraged. People in crisis feel uncertain and confused and find that memories of the past swirl about at random, interfering with attention to that moment. When it comes to decision-making trial and error is used, with random stabs in the dark. It is difficult to choose from different solutions let alone to formulate those solutions. You cannot see the wood for the trees. Signals of distress are sent out to others, clinging and embracing behavior occurs. The person wants to change but does not know how. Initially, significant other people will act as buffers and protect the person in crisis and may significantly influence the selection of solutions. If they are not able to cope with the distress, or disapprove of the way the person in crisis is acting they may withdraw. There are three major ways of understanding crisis (Bancroft, 1979).
The individual model (based on psychoanalytic theory) This model looks at why this particular person is overwhelmed. It is of interest to know what degree of self identity the person has and to what degree she can tolerate frustration. Have there been past crisis experiences and if so how were these handled? One factor which correlates with an ineffective response in crisis is parental over protection. A young person who is deprived of any opportunity to experience coping with frustration and failure has no basis on which to build crisis handling behaviour.
The behavioural model (based on normative understanding) Crisis experience is viewed as normal. The interest centers on what problemsolving skills the person has and on what actions she has taken which indicate success or failure in resolving the crisis. It is also of interest to know if the thoughts and actions which would normally be expected in the situation are occurring. If you have experienced a crisis you will know that it is comforting to
find, that while feeling out of control and acting that way in your view, others appear to cope with this and see it as normal under the circumstances.
The interactional model (based on systems theory) This view is interested to monitor the responses of significant others in the person'? life, Do they encourage the person to deal with and resolve the crisis or is the person encouraged to become helpless and dependent. The *mad' or 'bad' role may be encouraged, or the 'sick' role. Sometimes the family unit (the system) needs the person in a particular role known as the 'identified patient' so as to protect the other family members from chaos. The social network can inhibit change and growth. Within a system like the family the person is encouraged to remain her usual self, for better or worse, because that is what the family knows and that old 'self has a function for that family. The same idea can be transferred to the workplace. Does someone function as the scapegoat, the problem, the person in crisis who 'can't', thereby allowing everyone else to function? When understanding a person in crisis and the coping mechanisms they employ it is of value to look at all these aspects: the intrapersonal, the interpersonal and the social context - a systemic interactional perspective.
CAPLAN'S CRISIS CIRCLE To understand further what happens in a crisis, Caplan's circle (see Fig. 7.1) will now be explored, based on the definition presented earlier. The person is faced with an obstacle and the coping mechanisms normally used do not work effectively. Consequently an increase further reduction in anxiety and tension is experienced. The more the anxiety and tension increase the more difficult it is to see the wood for the trees. Consequently, loss of insight occurs. It becomes harder and harder to think of possible solutions; ways out of this chaotic experience. Problem-solving ability is reduced leaving the person feeling helpless, not knowing which way to go and where to turn; immobilized. A further increase in anxiety and tension may then occur with further loss of insight, reduction in
problem-solving and an even deeper helplessness and immobility. This vicious circle can go round and round until a threshold level is reached (sec Fig. 7.2); a level where the person draws on latent or new resources which can be physical, psychosocial, spiritual or all of these. Otherwise major disorganization will occur (including perhaps a psychotic episode).
Phases of the crisis circle There are four phases in this process towards resolution or major disorganization (Brandon, 1970). Phase 1 Phase one occurs as a result of the threat being perceived. Old memories are revived accompanied by emotional reaction. The impact of the crisis will be influenced by such factors as bodily state, influence of infection or exhaustion, and the availability of support systems and other external resources. Past experience and previously developed coping mechanisms will also influence behavior. As tension and anxiety increase usual problem-solving methods are tried. When unsuccessful the crisis state develops.
Phase 2 As the tension rises disorganization begins. Usual functioning is interfered with. The person is upset, anxious and feels insecure and helpless. Trial and error problem-solving occurs and feelings are discharged.
Phase3 Tension rises and there is a threshold level reached with a draining of internal and external resources. New problem-solving techniques are employed and solutions attempted. Often at this stage the problem is defined in a new way. The solution may resolve the crisis. Resolution normally occurs within 4-6 weeks when new coping mechanisms are found.
Phase 4 This occurs when the solution applied does not really solve the crisis. It may stop the discomfort and distress but in the longer term prove maladaptive. Major disorganization ensues including sometimes psychosis. However, it is important to realize that the majority of people reach threshold level and do find the necessary resources to adapt to the crisis and overcome the obstacle. Sometimes you can see a person struggling with an issue, going round in circles and making poor and unfruitful attempts to solve the problem. While the person does not want to recognize her need for help, all you can do is offer support and wait. When threshold level (Fig. 7.2) is reached the person will be willing to use the resources available. It can be very frustrating watching someone go round in circles but if you rush in and fix it for them they will not learn from experience and develop new coping mechanisms. Even when asked for help it is important to act as a supporter and confidante who can help the person in crisis gain some equilibrium and problem-solve, but wherever possible the most effective help still leaves the person in charge of her own decisions and life.
Where to intervene in a crisis Taking over responsibility Here you are helping at the 'inability to act' part of the circle. Sometimes the person is so overwhelmed or so ill that she becomes a' 'patient' to be taken care of. This means that the person's current responsibilities will have to be dealt with by others. The person is usually then removed from the environment provoking the stress. She may stay with friends or relatives or be admitted to a hospital. The person needs time spent with her and permission to talk, with acceptance and concern offered by the care givers. The person may be quite exhausted and require sleep. Medication has a place for helping sleep if really necessary and also to dampen high and distressing psychological arousal. If used, medication is viewed as a short term treatment only!
Taking over of responsibility is not usually necessary in the majority of crisis reactions and is the choice made only when the person is considerably swamped.
Helping people in crisis help themselves Here you are helping at the anxiety and tension, insight and problem-solving areas. This is the preferred choice. People are aware of the crisis and turmoil they are experiencing and ask for help. Often the first step is to define the actual problem. Towards this end it is useful to encourage the person to express emotion; anger, frustration, guilt, sadness; whatever the emotions are which have been elicited as a result of the crisis. It is usually of benefit to release and express these feelings. The person requires acceptance; the showing of warmth and empathy which will build trust. Emphasizing the positive aspects of the person and using and eliciting her strengths will build self-esteem and prevent the helper from also being overcome by the problem. Most importantly the person is encouraged and helped to problem-solve. Choices are presented. If there is only one choice there is really no choice at all. If there are two choices, they are often polarized; good or bad; right or wrong; black or white. The availability of two choices only, may leave a person stuck on the horns of a dilemma with no way of finding shades of grey and room to move. Wherever possible try to find at least three possible choices before deciding on a potential solution. As part of this process you may need to give information, make statements of reality, let a person know about incongruent messages, employ reflective listening, not provide answers and be comfortable with silence or with strong emotion. It is sometimes appropriate to give advice particularly of an expert kind such as medical, legal, monetary or contraceptive advice. Avoid advice-giving unless it is really necessary. The patient is best helped by finding her own solution which is right for her.
There are times when psychotropic drugs may be valuable such as to lower intense feeling, to make way for problem-solving behaviour, to help with sleep, or to improve mood in depression so that problem-solving behaviour can be initiated. Drugs are best kept until last and not used unless really necessary. Distressed behaviour with experience of emotion and feelings of chaos are normal during crisis. Out of chaos comes change. A crisis is certainly one for the person experiencing it, but as that person becomes very stressed those around her may also experience severe stress to the point of crisis. This is often the case in nursing when the stress load carried may be very great if dealing with many very ill people, death, and distressed and bereaved relatives. Many times health professionals also have a sense of grief sharpened by a tense of failure. It is a trap to emphasize curing sometimes to the detriment of caring. Dying is the final stage of living. To care and make comfortable while a person negotiates this final life stage is really what is needed. Curing is no longer relevant.
THE KUBLER-ROSS CRISIS MODEL The dying process is often avoided and not talked about partly because of the fear of death and the uncertainty about a future life; partly because the possible loss of someone dear is not faced early, and in hospitals partly because of the 'cure' injunction which contributes to the health professional's sense of failure when someone dies. Although people have often not been told their diagnosis or their prognosis they nonetheless know, and will be able to tell you this when they realize you are willing to let them talk about their realization, and the feelings and thoughts they are experiencing.
Stages in the dying process Denial This functions as a buffer while the person becomes ready to accept the diagnosis which heralds her death. It is a useful mechanism which allows time to adjust. The patient will let it go when ready as long as the staff are not giving non-verbal
messages which imply that the illness and feelings are not to be talked about. Some people die denying their illness; that is their right. Partial denial is also useful from time to time. The person may accept the diagnosis but will sometimes talk of a future which is clearly not possible. This can help the person continue to face life, when death becomes difficult to look at too closely.
Anger People often wonder why this should happen to them! 'Why me?' they will ask. There is no answer to this question. An answer is not being looked for, it is just a way of expressing frustration at the limits now placed on life plans. If the person is allowed to express her anger and it is realized there is no need to respond defensively or to prevent the expression of this emotion, in most people this anger will pass. Anger0 is often expressed towards the very people we love and trust the most. Somehow we believe they will still care and be there for us. Patients can be co-operative and friendly from a nurse's perspective and give particular relatives an awful time. The important thing is to recognize the anger for what it is: the person's expression of frustration and not a personal attack. Support needs to be provided for the person to whom the anger is addressed. The majority of people will lose their angry feelings eventually, particularly if accepted and supported. That means you acknowledge their anger, do not defend yourself, and treat them as people, not someone to be handled with kid gloves, or avoided. Confrontation, Imessages, reality statements and information will not do any harm accompanied by your listening skills where appropriate.
Bargaining People make bargains between themselves and their God. These are private and not usually shared. They sometimes make bargains like 'If I don't cat, I'll feel better.' A bargain is really trying to gain more time. Many patients will bargain for time 'Just to be at my daughter's
You might also like
- The Overthinking Cure: How to Stay in the Present, Shake Negativity, and Stop Your Stress and AnxietyFrom EverandThe Overthinking Cure: How to Stay in the Present, Shake Negativity, and Stop Your Stress and AnxietyRating: 4.5 out of 5 stars4.5/5 (17)
- Metal & Stone - 56 - 110 - Einleitung - ENDocument5 pagesMetal & Stone - 56 - 110 - Einleitung - ENlotus630No ratings yet
- 220 Unit For NVQ 2Document3 pages220 Unit For NVQ 2ChiriacAioana75% (4)
- Schemas and Schema Modes For Formulation and Treatment Planning (David Edwards)Document15 pagesSchemas and Schema Modes For Formulation and Treatment Planning (David Edwards)Milán Glasznik100% (1)
- Crisis ManagementDocument39 pagesCrisis ManagementbolutifeNo ratings yet
- Assessment 7: Crisis CounsellingDocument21 pagesAssessment 7: Crisis Counsellingsyeda maryem100% (1)
- Crisis & Its InterventionDocument13 pagesCrisis & Its InterventionAncy Varkey100% (1)
- A Client's Guide To Schema TherapyDocument13 pagesA Client's Guide To Schema Therapyvasilikiser100% (3)
- A Client's Guide To Schema TherapyDocument13 pagesA Client's Guide To Schema TherapyClaudia Delia Foltun100% (11)
- Ten Commandments For The Scrupulous (Revised)Document8 pagesTen Commandments For The Scrupulous (Revised)Mihaela FarauanuNo ratings yet
- ENG MPK20 Ormet REV2 Manual PDFDocument47 pagesENG MPK20 Ormet REV2 Manual PDFSandra Brizolla LuvisaNo ratings yet
- Those Who CareDocument9 pagesThose Who CareBulshu BeristainNo ratings yet
- Crisis Theory and Phases of DevelopmentDocument6 pagesCrisis Theory and Phases of DevelopmentNic Korapat100% (1)
- Res Lili EnceDocument2 pagesRes Lili EnceagaNo ratings yet
- What Is Crisis?: Development of A CrisisDocument24 pagesWhat Is Crisis?: Development of A CrisisVaness143No ratings yet
- Healing From Dissociation Some Steps - SvaliDocument6 pagesHealing From Dissociation Some Steps - SvaliclaireemeryhNo ratings yet
- Crisis InterventionDocument18 pagesCrisis InterventionKitoy AwomiNo ratings yet
- What Is Crisis?: Development of A CrisisDocument19 pagesWhat Is Crisis?: Development of A CrisisJosephine MarietaNo ratings yet
- Survival Chances TextDocument6 pagesSurvival Chances TextChristine CarreonNo ratings yet
- What Is Crisis?: Development of A CrisisDocument18 pagesWhat Is Crisis?: Development of A CrisisKATHY TRUONGNo ratings yet
- DBTDocument5 pagesDBTVidya Mohan Krithikanand100% (1)
- Crisis Intervention: Difference Between Stress & CrissisDocument14 pagesCrisis Intervention: Difference Between Stress & CrissisLahunWanniangNo ratings yet
- Resilience:: American Psychological AssociationDocument11 pagesResilience:: American Psychological AssociationDisha PradeepNo ratings yet
- How to Handle Tough Situations : Finding Inner Strength To Survive The Toughest Crisis And Life ChallengesFrom EverandHow to Handle Tough Situations : Finding Inner Strength To Survive The Toughest Crisis And Life ChallengesNo ratings yet
- Psyche Prefinal CrisisDocument5 pagesPsyche Prefinal CrisisAziil LiizaNo ratings yet
- Satir Theory Twenty Years After Her DeathDocument4 pagesSatir Theory Twenty Years After Her DeathgoshNo ratings yet
- Self EsteemDocument4 pagesSelf EsteemSharon BooNo ratings yet
- ACT For Interpersonal Problems: Using Mindfulness, Acceptance, and Schema Awareness To Change Interpersonal BehaviorsDocument9 pagesACT For Interpersonal Problems: Using Mindfulness, Acceptance, and Schema Awareness To Change Interpersonal BehaviorsNew Harbinger Publications48% (21)
- Caring For People With Challenging Behaviors, Second Edition ExcerptDocument6 pagesCaring For People With Challenging Behaviors, Second Edition ExcerptHealth Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.No ratings yet
- Stress and Coping Mechanisms: Manage your stress and live a happier lifeFrom EverandStress and Coping Mechanisms: Manage your stress and live a happier lifeNo ratings yet
- A Study OnDocument25 pagesA Study Onjayson cajateNo ratings yet
- Dialectical Behavior Therapy: Feeling Good Again by Overcoming Mood Swings, Gaining Emotional Control with the DBT TherapyFrom EverandDialectical Behavior Therapy: Feeling Good Again by Overcoming Mood Swings, Gaining Emotional Control with the DBT TherapyRating: 3 out of 5 stars3/5 (1)
- Crisis Intervention/Suicide Prevention: Relational Self Help SeriesFrom EverandCrisis Intervention/Suicide Prevention: Relational Self Help SeriesRating: 2 out of 5 stars2/5 (1)
- Crisis InterventionsDocument14 pagesCrisis InterventionsReet_paed100% (5)
- Crisis, Loss, Grief, ResponseDocument14 pagesCrisis, Loss, Grief, Responsef9fq4x8qvnNo ratings yet
- Bert Hellinger Family Systems TherapyDocument6 pagesBert Hellinger Family Systems TherapyHugomar100% (2)
- Positive Thinking & SpeakingDocument6 pagesPositive Thinking & SpeakingaitezazNo ratings yet
- Crisis InterventionDocument19 pagesCrisis InterventionKJ Bindu33% (3)
- Stress – The CommonSense Approach: How to Harness, Exploit and Control StressFrom EverandStress – The CommonSense Approach: How to Harness, Exploit and Control StressNo ratings yet
- Grief Work BlatnerDocument7 pagesGrief Work Blatnerbunnie02100% (1)
- Critical Incidents and Their Operational ImpactDocument6 pagesCritical Incidents and Their Operational ImpactIAHN NegotiatorNo ratings yet
- Rezilienta DefinitiitDocument7 pagesRezilienta DefinitiitLaura PârvulescuNo ratings yet
- Dora's Essentials - Examining Anxiety (What's Normal & What's Not?)From EverandDora's Essentials - Examining Anxiety (What's Normal & What's Not?)No ratings yet
- This Transcript Was Exported On Feb 17, 2020 - View Latest VersionDocument4 pagesThis Transcript Was Exported On Feb 17, 2020 - View Latest VersionfsdfsdfdsdsNo ratings yet
- A Joosr Guide to... How to Deal with Difficult People by Gill Hasson: Smart Tactics for Overcoming the Problem People in Your LifeFrom EverandA Joosr Guide to... How to Deal with Difficult People by Gill Hasson: Smart Tactics for Overcoming the Problem People in Your LifeNo ratings yet
- Inside the Mind of a Narcissistic Person and How to Counter Attack Their Behavior: Everything You Need to Know About Narcissistic PersonsFrom EverandInside the Mind of a Narcissistic Person and How to Counter Attack Their Behavior: Everything You Need to Know About Narcissistic PersonsRating: 3.5 out of 5 stars3.5/5 (2)
- The Road To ResilienceDocument7 pagesThe Road To ResilienceAnca IonNo ratings yet
- Navigating the Storm: A Roadmap for Coping with Panic and Social AnxietyFrom EverandNavigating the Storm: A Roadmap for Coping with Panic and Social AnxietyNo ratings yet
- 52 Proverbs to Fight Depression and Trauma: Irish Holistic WisdomFrom Everand52 Proverbs to Fight Depression and Trauma: Irish Holistic WisdomNo ratings yet
- Improving Your Resilience: How to bounce back after disappointmentFrom EverandImproving Your Resilience: How to bounce back after disappointmentNo ratings yet
- This Is How You Grow After Trauma Simple Strategies For Resilience, Confidence, Healing and Hope (Olivia Remes)Document154 pagesThis Is How You Grow After Trauma Simple Strategies For Resilience, Confidence, Healing and Hope (Olivia Remes)r jNo ratings yet
- Module 2: Reaction To CrisisDocument9 pagesModule 2: Reaction To CrisisTubocurareNo ratings yet
- Ab 5Document11 pagesAb 5boouananiNo ratings yet
- Covid EffectsDocument2 pagesCovid EffectsMuhammadSalmanButtNo ratings yet
- ResilienceDocument10 pagesResiliencecoclegendth14No ratings yet
- Psyc Essay Final 010420Document2 pagesPsyc Essay Final 010420Ali HajassdolahNo ratings yet
- Social Anxiety and Cognitive Behavioural TechniquesDocument14 pagesSocial Anxiety and Cognitive Behavioural TechniquesAura Mateiu100% (1)
- Easy Steps To Overcoming Challenges From Difficult People At WorkFrom EverandEasy Steps To Overcoming Challenges From Difficult People At WorkNo ratings yet
- Military Leadership C/ - Emalin Pilotos 0830H-0930H StrengthDocument21 pagesMilitary Leadership C/ - Emalin Pilotos 0830H-0930H StrengthAliyah CasinNo ratings yet
- Literature Review On Cocoyam PDFDocument5 pagesLiterature Review On Cocoyam PDFf0typiwydeb3100% (1)
- Preparation and Attempt in Accordance To IPCDocument11 pagesPreparation and Attempt in Accordance To IPCpratikminj100% (5)
- Astm C421 PDFDocument3 pagesAstm C421 PDFMirella FaresNo ratings yet
- Kartotrak v1.0 Features: 1. Gis-B Ased Interf AceDocument4 pagesKartotrak v1.0 Features: 1. Gis-B Ased Interf AceOurs2fNo ratings yet
- Eng4u Elements of Short Stories Literary Devices Test1Document2 pagesEng4u Elements of Short Stories Literary Devices Test1Αθηνουλα ΑθηναNo ratings yet
- Objective: To Obtain A Position As EnglishDocument6 pagesObjective: To Obtain A Position As EnglishThey Yawai AungNo ratings yet
- IcqDocument25 pagesIcqDankaNo ratings yet
- The Passport To Success 9 Module 1Document18 pagesThe Passport To Success 9 Module 1gina100% (1)
- How-To Build A Little Autonomous Robot With PIC 18F4520 PDFDocument22 pagesHow-To Build A Little Autonomous Robot With PIC 18F4520 PDFanselmoNo ratings yet
- IDP PULL DA DatasheetDocument2 pagesIDP PULL DA Datasheetjosuna2006No ratings yet
- Critical Analysis Essay - A Black Feminist StatementDocument2 pagesCritical Analysis Essay - A Black Feminist StatementAna Lucía Mosquera RosadoNo ratings yet
- Assessment Plan ShilohDocument2 pagesAssessment Plan Shilohapi-478596695No ratings yet
- COMMUNICATION DOCC - OdtDocument21 pagesCOMMUNICATION DOCC - OdtRama KrishnaNo ratings yet
- Mastering OpenStack - Sample ChapterDocument43 pagesMastering OpenStack - Sample ChapterPackt PublishingNo ratings yet
- Unit-9 Edmund Burke PDFDocument10 pagesUnit-9 Edmund Burke PDFAbhinav100% (1)
- Cti ListDocument6 pagesCti ListRana SaimNo ratings yet
- MCK Rhetoric Introduction (Backman)Document14 pagesMCK Rhetoric Introduction (Backman)Eduardo ÍndigoNo ratings yet
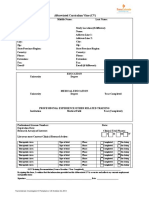
- TransCelerate Curriculum Vitae Form PDFDocument1 pageTransCelerate Curriculum Vitae Form PDFYuli JlsNo ratings yet
- MA1 Revision WorksheetDocument9 pagesMA1 Revision WorksheetSami100% (1)
- Fys EngelskDocument79 pagesFys EngelskGeorge ErdicNo ratings yet
- High Voltage Engineering LucasDocument204 pagesHigh Voltage Engineering LucasCarlos Vidal Solis VelizNo ratings yet
- Communication AssesmentDocument15 pagesCommunication AssesmentpwaingankarNo ratings yet
- Test Bahasa Inggris (Tbi)Document3 pagesTest Bahasa Inggris (Tbi)MARIANo ratings yet
- Columbia's Motion For JNOVDocument48 pagesColumbia's Motion For JNOVSarah BursteinNo ratings yet
- USSH Writing B1 Paragraph Writing RevisionDocument6 pagesUSSH Writing B1 Paragraph Writing RevisionVI NGUYỄN THỊ THẢONo ratings yet
- Jntuk BT 3 2 R16 TT 2019Document5 pagesJntuk BT 3 2 R16 TT 2019Vennela PriyaNo ratings yet
- Singular Value Decomposition in Image Noise Filtering and ReconstDocument68 pagesSingular Value Decomposition in Image Noise Filtering and ReconstarlysonNo ratings yet