Professional Documents
Culture Documents
The Perioperative Nurse's Duties and Responsibilities: Surgical Nursing Defined
The Perioperative Nurse's Duties and Responsibilities: Surgical Nursing Defined
Uploaded by
Siena Lou CeniaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Perioperative Nurse's Duties and Responsibilities: Surgical Nursing Defined
The Perioperative Nurse's Duties and Responsibilities: Surgical Nursing Defined
Uploaded by
Siena Lou CeniaCopyright:
Available Formats
The Perioperative Nurse's Duties and Responsibilities
Surgical Nursing Defined
The perioperative nurse is responsible and accountable for the major nursing activities occurring in the surgical suite. These include, but are not limited to the following: Assessing of the patient's physiological and psychological status before, during, and after surgery Identifying priorities and implementing care based on sound nursing judgment and individual patient needs Functioning as a role model of a professional perioperative nurse for students and colleagues Functioning as a patient advocate by protecting the patient from incompetent, unethical, or illegal practices during the perioperative period Coordinating all activities associated with the implementation of nursing care by other members of the health-care team Demonstrating a thorough knowledge of aseptic principles and techniques to maintain a safe and therapeutic surgical environment Directing or assisiting with the care and handling of all supplies, equipment, and instruments, to ensure their economic and efficient function for the patient and personnel under both normal and hazardous conditions Performing as a scrub or circulating nurse as needed, based on knowledge and expertise for a specific procedure Participating in continuing education programs directed toward personal and professional growth and development
Participating in professional organizational and research activities that support and enhance perioperative nursing practice
seconPerioperative Nurses Week: November 7, 2011
Operating Room Nursing Activities
Circulating Nurse
Perioperative nursing practice has one continuous goal: to provide a standard of excellence in the care of the patient before, during, and after surgery. As the only nonscrubbed member of the surgical team, besides anesthesia, the circulating nurse represents the coordinating link between the scrub team and all other departments and personnel associated with the surgical patient and the procedure. Other departments that may be involved in the patient's surgical experience include, but are not limited to, x-ray, pathology, blood bank, laboratory, blood gas lab, tissue banking, mammography, and radiation oncology. The Circulating nurse, by virtue of her professional educational preparation and specialized skill, is responsible for managing patient care activities in the operating suite, so his/her duties begin long before the patient arrives in the operating room and continues until the final dispensation of the patient, operating room records, and specimens is completed. The following list depicts some of the activities performed by the circulating nurse prior to induction of anesthesia, during the procedure, and upon conclusion of the procedure: Assisting and preparing the procedure room Supervising the transporting, moving, and lifting of the patient
Assisting anesthesia as requested during induction and reversal of anesthesia Positioning the patient for surgery Performing the surgical skin prep Conducting and maintaining accurate records of counts Maintaining accurate documentation of nursing activities during the procedure Dispensing supplies and medications to the surgical field Maintaining an aseptic and safe environment Estimating fluid and blood loss Handling special equipment, specimens, etc Communicating special postoperative needs to appropriate persons at the conclusion of the case Perioperative nursing represents a multifacedted challenge to today's operating room nurse. In this role, the nurse has an opportunity to: Prepare the patient and family for surgery Provide comfort and support to patients and their family Use sound nursing judgment and problem-solving techniques to assure a safe and effective surgical experience. Whether scrubbing, circulating, or supervising other team members, the perioperative nurse is always aware of the total environment, as well as the patient's reaction to the environment and the care given during all three phases of surgical intervention. The perioperative nurse is knowledgeable about aseptic technique, patient safety, legal aspects of nursing, and management of nursing activities associated with the specific surgical procedure being performed. OR nursing is unique: it provides a specialty service during the perioperative period that
stresses the need for continuity of care and respect for the individuality of the patient's needs.
Another Perioperative Nurse Role
Scrub Nurse
The perioperative nurse as a scrub nurse performs another essential role in the operating room. Her expertise includes knowledge of anatomy and physiology and the procedure to be performed, ability to recognize the instrumentation used in a particular surgery, and critical thinking skills to gather specialty items that may be needed during a procedure and in event of an emergency. The scrub nurse is a member of the sterile surgical team. His/her primary responsibility is maintenance of the sterile field. Other activities of the scrub nurse includes: Assisting and preparing the procedure room Gathering sterile supplies needed for the procedure and those that may be needed Setting up the sterile back table Dressing the surgeon and other members of the surgical team in their sterile attire Assisting in the placement of the sterile drapes Passing the instruments to the surgical team and assisting as needed to enhance the continuity of the procedure Constant surveillance of the surgical field thus maintaining sterility Anticipating the needs of the surgeon and asking for items before they are needed
Reporting to the circulating nurse the names of the specimens obtained during surgery Helps with the application of the sterile dressing at the end of the procedure Removal of bioburden from used instrumentation before sending it to be processed in Central processing. Assist in the cleaning of the procedure room to make ready for the next surgical procedure.
CNOR - Certified Nurse Operating Room
National Certification Exam
I passed the CNOR exam on September 8, 2009. I felt great accomplishment. I was so nervous when I went to take the exam. I've been out of school for 15 years and it's been over 14 years since I took my state board exam. I had studied well for this exam and I have a total of 27 years of OR experience between being a surgical tech and a RN. Just the thought of a "test" made my palms sweaty. The CNOR is a national certification exam for operating room nurses. The exam covers sterilization techniques, maintaining a sterile field, critical thinking skills in the operating room, dosage calculations, emergency situations like malignant hyperthermia and cardiac arrest, and more. The exam consists of 200 questions and 4 hours are allowed to complete the exam. I finished the exam in 2 hours and 45 minutes. I sat in front of the
computer staring at the screen and afraid to click the "submit" button for about another 15 minutes. I finally mustered the courage to click the button. I filled out the survey questions and when that was done a screen appeared that said "Congratulations! Our calculations indicate you have passed the CNOR certification exam". It was unofficial, but I had passed. What a relief! National certification examinations are an important part of a nurse's career. It increases the continuing education requirements beyond the state license requirements. To maintain the CNOR certification the nurse must obtain 150 continuing education units specific to the OR every 5 years. State continuing education requirements differ, but are a lesser amount and are general in nature. CAHO, aka Joint Commission, implemented new regulations in 2009. For the operating room these new regulations are referred to as Universal Protocol. Universal Protocol consists of three new expectations for the perioperative nurse: Conduct a pre-procedure verification process Marking the procedure site so the staff can identify without ambiguity the intended site for the procedure A time out is performed immediately prior to starting procedures
The pre-procedure verification is an ongoing process of information gathering and verification, beginning with the decision to perform a procedure, continuing through all settings involved in the pre-procedure preparation of the patient, up to
and including the time-out just before the start of the procedure. The purpose of the pre-procedure verification process is to make sure that all relevant documents and related information or equipment are available prior to the start of the procedure, correctly identified, labeled, and matched to the patient's identifiers, and reviewed and are consistent with the patient's expectations. Missing information or discrepancies are addressed before starting the procedure. Verification of the correct person, correct site, and correct procedure occurs at the time the procedure is scheduled, at the time of preadmission testing and assessment, at the time of admission or entry into the facility for a procedure (whether elective or emergent), before the patient leaves the preprocedure area or enters the procedure room, and anytime the responsibility for care of the patient is transferred to another member of the procedural care team (including anesthesia providers) at the time of, and during, the procedure. Preferrably, the patient will be involved, awake and aware, if at all possible. Items that need to be accurately matched to the patient and available include: Relevant documentation (i.e., history and physical, nursing assessment, and pre-anesthesia screen) Accurately completed, and signed, procedure consent form Correct diagnostic and radiology test results that are properly labeled Any required blood products, implants, devices and/or special equipment for the procedure.
Marking the procedure site is done for all procedures involving laterality (side), the surface (flexor or extensor), the level (spine), or specific digit or lesion to be treated. The procedure site is initially marked before the patient is moved to the operating room and takes place with the patient involved, awake and aware, if possible. The site is marked by a licensed independent contractor (MD, Nurse Practitioner, Physician Assistant) that will be directly involved in the procedure and will be present at the time the procedure is performed. The method of marking must be unambiguous and used consistently throughout the hospital. The mark is made at or near the incision site, includes the marking person's initials, is made with a marker that is sufficiently permanent to remain visible after completion of the skin prep and sterile draping, and is positioned to be visible after the patient's skin has been prepped, is placed in the final position, and sterile draping is completed. The time-out is conducted prior to starting the procedure and, ideally, prior to the introduction of the anesthesia process, unless contraindicated. The time-out has the following characteristics: It is standardized (as defined by the hospital). It is initiated by a designated member of the team, usually the circulating nurse. It involves the immediate members of the team including the surgeon, the anesthesia providers, the circulating nurse, the operating room technician or scrub nurse, and other active participants as appropriate for the procedure.
It involves interactive verbal communication between all team members, and any team member is able to express concerns about the procedure verification. It includes a defined process for reconciling differences in responses.
During the time-out, all other activities are suspended, to the extent possible without compromising patient safety, so all relevant members of the team are focused on the active confirmation of the correct patient, correct procedure, correct site, and other critical elements. The completed components of the Universal Protocol and time-out are clearly documented.
You might also like
- Princeton CARS Workbook PDFDocument272 pagesPrinceton CARS Workbook PDFanon_940563124100% (2)
- Unitor MsdsDocument5 pagesUnitor Msdsvakil50% (2)
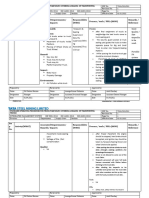
- I. Preoperative Assessment 1. Physical: Philippine Heart Center Perioperative Nursing RecordDocument2 pagesI. Preoperative Assessment 1. Physical: Philippine Heart Center Perioperative Nursing RecordERWINNo ratings yet
- Training Program For New Staff Nurses in IcuDocument4 pagesTraining Program For New Staff Nurses in IcuNick Alfaro100% (4)
- APP-KSMC-127 - (V4) - Crash Cart Checking & Maintenance Rev120314Document8 pagesAPP-KSMC-127 - (V4) - Crash Cart Checking & Maintenance Rev120314Kimberly Solis100% (2)
- Operating Room ProcedureDocument4 pagesOperating Room ProcedureROxanne S. RendonNo ratings yet
- Sample Form of Quality Assurance Nursing AuditDocument2 pagesSample Form of Quality Assurance Nursing Auditgandhialpit100% (1)
- Solomon Cb09 PPT 04Document34 pagesSolomon Cb09 PPT 04Spencer BrownNo ratings yet
- Backpod User Guide 2019Document36 pagesBackpod User Guide 2019Sean DrewNo ratings yet
- What Is Aseptic TechniqueDocument11 pagesWhat Is Aseptic TechniqueMarlchiel Nathan ArregladoNo ratings yet
- Operating Room Nurse Job DescriptionDocument1 pageOperating Room Nurse Job DescriptionKarla Fralala100% (1)
- OR Duty RLE RequirementsDocument5 pagesOR Duty RLE RequirementsSammy Jr FamilarNo ratings yet
- What Are The Functions of A Scrub NurseDocument24 pagesWhat Are The Functions of A Scrub NurseBrigette Jane Michelle Martil100% (1)
- Operating Room Personnel OrganizationDocument4 pagesOperating Room Personnel OrganizationantihistamiiineNo ratings yet
- Operating Room TeamDocument7 pagesOperating Room TeamFaruqueHossain100% (1)
- Scrub Nurse Circulating NurseDocument2 pagesScrub Nurse Circulating NurseLalaine Nadulpit100% (3)
- Surgery 1 - UCDocument101 pagesSurgery 1 - UCEsvinch EsvinchNo ratings yet
- The COAT & Review Approach: How to recognise and manage unwell patientsFrom EverandThe COAT & Review Approach: How to recognise and manage unwell patientsRating: 5 out of 5 stars5/5 (1)
- Surgical Handwashing Resource Material 2023-2024Document9 pagesSurgical Handwashing Resource Material 2023-2024Cherry Louise O. SanvictoresNo ratings yet
- Intra Op CombinedDocument62 pagesIntra Op CombinedJan Federick Bantay100% (1)
- GENERAL SAFETY CHECKLIST GuidelinesDocument10 pagesGENERAL SAFETY CHECKLIST GuidelinesTina AlteranNo ratings yet
- Clinical FocusDocument10 pagesClinical FocusRyan-Jay AbolenciaNo ratings yet
- Etiquette and PrinciplesDocument3 pagesEtiquette and PrinciplesHoney Bee S. PlatolonNo ratings yet
- Post Operative MGTDocument10 pagesPost Operative MGTNatukunda DianahNo ratings yet
- Endoscopy NurseDocument7 pagesEndoscopy NurseEden Paulette ConsadNo ratings yet
- Perioperative Nursing1Document141 pagesPerioperative Nursing1Jordan Bautista100% (1)
- Duties and Responsibilities of An RN: Lpns CnasDocument4 pagesDuties and Responsibilities of An RN: Lpns CnasSPTDNo ratings yet
- Operating NURSEDocument8 pagesOperating NURSEAlexis de los SantosNo ratings yet
- Operation Theater Policies and Procedures ManualDocument33 pagesOperation Theater Policies and Procedures Manualakinrav50% (2)
- ReportDocument4 pagesReportKinjal VasavaNo ratings yet
- Minor SurgeryDocument7 pagesMinor SurgeryBabylyn Purugganan100% (1)
- Scrub Nurse (Mastectomy)Document6 pagesScrub Nurse (Mastectomy)Jeroham R. CoNo ratings yet
- Operating Room Orientation Manual Goals &Document4 pagesOperating Room Orientation Manual Goals &bhuselleNo ratings yet
- ASSISTING IN A MAJOR OPERATION Circulating Nurse Performance EvaluationDocument2 pagesASSISTING IN A MAJOR OPERATION Circulating Nurse Performance EvaluationKrizzia Angela BacotocNo ratings yet
- Nurs 253 Preceptor Evaluation Forms-FinalDocument8 pagesNurs 253 Preceptor Evaluation Forms-Finalapi-284094534No ratings yet
- IntraoperativeDocument4 pagesIntraoperativeLynette Roldan RN100% (1)
- Nursing Skill RevisionDocument1 pageNursing Skill RevisionMichelle TseNo ratings yet
- Job Description - Nursing SuperintendentDocument4 pagesJob Description - Nursing SuperintendentSheen BelsylinNo ratings yet
- Responsibilities HNDocument7 pagesResponsibilities HNMitzi Basa DimainNo ratings yet
- Endorsement Clinical Handover/ EndorsementDocument4 pagesEndorsement Clinical Handover/ EndorsementGuiah RomaNo ratings yet
- 8 Decontamination Disinfection SterilizationDocument8 pages8 Decontamination Disinfection SterilizationJay VillasotoNo ratings yet
- Nursing Core Competency PresentationDocument92 pagesNursing Core Competency Presentationleyshan100% (1)
- Perioperative Nursing Management Ksu 0Document35 pagesPerioperative Nursing Management Ksu 0moath qadourah100% (1)
- Hourly Round ProjectDocument8 pagesHourly Round ProjectaustinisaacNo ratings yet
- Admission of PatientsDocument34 pagesAdmission of PatientsDavid OpokuNo ratings yet
- IPSGDocument4 pagesIPSGmohsinaNo ratings yet
- Care of Clients Requiring SurgeryDocument27 pagesCare of Clients Requiring SurgeryNokz M. Raki-inNo ratings yet
- Nursing EmpowermentDocument1 pageNursing Empowermentsudhakar pNo ratings yet
- Principles of Sterile TechniqueDocument3 pagesPrinciples of Sterile TechniqueMaria VisitacionNo ratings yet
- CsDocument7 pagesCsakosiMJcutie100% (1)
- Critical Care NursingDocument2 pagesCritical Care NursingJyoti KathNo ratings yet
- 001mission, Vision Values StatementDocument3 pages001mission, Vision Values StatementAeryll JasminNo ratings yet
- Pre Op ChecklistDocument1 pagePre Op ChecklistKoushik Reddy PodduturiNo ratings yet
- Head Nurse TopicsDocument24 pagesHead Nurse TopicsPaulo Tiangson MejiaNo ratings yet
- Duties or NurseDocument10 pagesDuties or NursehailleyannNo ratings yet
- Head Nurse - PrintDocument4 pagesHead Nurse - PrintMark Joseph Felicitas CuntapayNo ratings yet
- NABH Staff RatioDocument1 pageNABH Staff RatioRetteri KUMARANNo ratings yet
- Nursing Service MANUALDocument37 pagesNursing Service MANUALjoan olanteNo ratings yet
- Roles of Different Personnel in TheatreDocument13 pagesRoles of Different Personnel in TheatreVincent KoronjiNo ratings yet
- Perioperative Nursing Care ModuleDocument68 pagesPerioperative Nursing Care ModuleEnrico Sapitula Del Rosario100% (4)
- Circulating NurseDocument3 pagesCirculating NurseSoheil LimboNo ratings yet
- Teaching Plan (Endoscopy)Document7 pagesTeaching Plan (Endoscopy)Joseph TheThirdNo ratings yet
- Or JournalDocument4 pagesOr JournalbillyktoubattsNo ratings yet
- PrixDocument2 pagesPrixJoy Kristine PanganNo ratings yet
- Oster Scientific Literature ReviewDocument2 pagesOster Scientific Literature Reviewapi-548337885No ratings yet
- Nikaido 2018Document5 pagesNikaido 2018Carmen Iturriaga GuajardoNo ratings yet
- PHCT Lec Topic 1Document3 pagesPHCT Lec Topic 1armand bayoranNo ratings yet
- Transfusion Related Immunomodulation (Trim) : By/ Aymen OmerDocument14 pagesTransfusion Related Immunomodulation (Trim) : By/ Aymen OmeraymenNo ratings yet
- EAP 582.4 WasteWater Engineering Treatment Principles and Design - Session1Document31 pagesEAP 582.4 WasteWater Engineering Treatment Principles and Design - Session1Abu Ahmed Mokammel HaqueNo ratings yet
- Edited PPT HEALTH 4th (Autosaved)Document23 pagesEdited PPT HEALTH 4th (Autosaved)Chloe Belamare JaplitNo ratings yet
- Demirturkkocasarac 2016Document9 pagesDemirturkkocasarac 2016emanNo ratings yet
- Topics (Week 3)Document3 pagesTopics (Week 3)Jolina T. OrongNo ratings yet
- Case Proforma Final, SurgeryDocument37 pagesCase Proforma Final, SurgeryDiwakesh C B100% (4)
- Macro Perspective of Tourism and Hospitality 6Document22 pagesMacro Perspective of Tourism and Hospitality 6Crhystal Joy Reginio100% (3)
- The Preanalytical PhaseDocument24 pagesThe Preanalytical PhaseArturo Eduardo Huarcaya OntiverosNo ratings yet
- Government Medical College, Badaun-1Document2 pagesGovernment Medical College, Badaun-1Utkarsh VermaNo ratings yet
- Vestige E-Catalogue May 2021Document143 pagesVestige E-Catalogue May 2021Rameez FaroukNo ratings yet
- An Introduction To Performance Based Design in NFPA ... - WOBODocument48 pagesAn Introduction To Performance Based Design in NFPA ... - WOBOAgustín Rosas PérezNo ratings yet
- Patpat Foundations of Special and Inclusive Education ReviewerDocument27 pagesPatpat Foundations of Special and Inclusive Education ReviewerJoseph John Estobaña100% (2)
- What Is PayrollDocument3 pagesWhat Is PayrollAbraham Mayo MakakuaNo ratings yet
- Bactec 9000Document12 pagesBactec 9000PAbloNo ratings yet
- Psychoanalysis and Psychodynamic TherapiesDocument51 pagesPsychoanalysis and Psychodynamic Therapieskuro hanabusaNo ratings yet
- Five Gold KeysDocument32 pagesFive Gold Keyssiddy09No ratings yet
- Complementary Feeding: Prepared By: Vheralyn B. Diesta MW 2-1Document11 pagesComplementary Feeding: Prepared By: Vheralyn B. Diesta MW 2-1Merry RoseNo ratings yet
- SOP For Tarpaulin Sealing of Transportation Truck - 21Document5 pagesSOP For Tarpaulin Sealing of Transportation Truck - 21syed aquib100% (1)
- How The COVID-19 Epidemic Changed Working Conditions in FranceDocument4 pagesHow The COVID-19 Epidemic Changed Working Conditions in FranceRenata JapurNo ratings yet
- Fisioterapia Pós Covid em PortugalDocument2 pagesFisioterapia Pós Covid em PortugalMaria JoanaNo ratings yet
- Top 5 Healthcare AI Startups To Watch For in 2021Document6 pagesTop 5 Healthcare AI Startups To Watch For in 2021appengine.ai100% (2)
- Steps in Poultr-WPS OfficeDocument3 pagesSteps in Poultr-WPS OfficeMartin, Jestony N.No ratings yet
- Perspective Essay TopicsDocument4 pagesPerspective Essay Topicsb725c62j100% (2)