Professional Documents
Culture Documents
Supra Ventricular Tachycardia in Pregnancy
Supra Ventricular Tachycardia in Pregnancy
Uploaded by
lulzimkamberiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Supra Ventricular Tachycardia in Pregnancy
Supra Ventricular Tachycardia in Pregnancy
Uploaded by
lulzimkamberiCopyright:
Available Formats
Supraventricular tachycardia in Pregnancy
CaSe report
Supraventricular tachycardia in Pregnancy
Lulzim Kamberi1, Hajdin itaku1, Teuta Hoxha-Kamberi2 University Clinical Center of Kosova, Department of Cardiology, Prishtine, Kosovo1 University Clinical Center of Kosova, Department of Pediatric and Neonatology, Prishtine, Kosovo2
reatment of paroxysmal supraventricular tachycardia during pregnancy is necessary to protect both mother and the fetus. In case of hemodynamic deterioration, pharmacological treatment is the treatment of choice. There are limited reports for the safety and efficacy of verapamil use in pregnancy for treatment of paroxysmal supraventricular tachycardia. Numerous case reports and a retrospective study suggest that adenosine is safe and effective for these kinds of arrhythmias. Key words: Supraventricular tachycardia, pregnancy.
Corersponding author: lulzim Kamberi, lulzimkamberi@gmail.com
t
1.
introduCtion We present a 32-yr-old patient-physician; a Caucasian pregnant woman with SVT. Before pregnancy, verapamil had always terminated successfully her episodes of paroxysmal supraventricular tachycardia. During her first pregnancy, she suffered from an attack of paroxysmal supraventricular tachycardia. Verapamil was given without success and her condition was destabilized even more. Adenosine was effective in converting her arrhythmias.
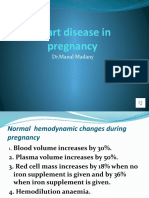
2. CaSe PreSentation Verapamil is not effective and it even worsens symptoms and impairs hemodynamics. Adenosine proved to be safe and effective in treatment of paroxysmal supraventricular tachycardia in pregnancy. Introduction In women of reproductive age, the most common arrhythmia is PSVT. In pregnancy it is defined as any tachyarrhythmia with a heart rate greater than 120 beats/ min, requiring atrial or atrioventricular junctional tissue for its initiation and maintenance. The diagnosis is confirmed by ECG (1). PSVT causes or ex-
acerbates symptoms which more than half of pregnant women already have (such as dispnea, palpitations, dizziness, presyncope, and syncope) (2). Treatment of PSVT in pregnancy may also affect the fetus. For this reason, non-pharmacological treatments are chosen, including vagal maneuvers such as carotid massage, Valsalva maneuver and facial ice immersion. These are well tolerated and aid in diagnosis. Pharmacological treatment is best reserved for those with hemodynamic changes, severe symptoms, or sustained arrhythmias. Adenosine, a naturally occurring purine nucleotide, transiently depresses sinus node activity and slows atrioventricular conduction, and is also effective in terminating PSVT. It is rapidly metabolized with an elimination half-life of less than 10 seconds. In addition, adenosine does not cross the placenta, making it suitable for use in pregnancy. Numerous case reports, and one retrospective study, suggest that adenosine is safe and effective (3,4). The first case describing the use of adenosine in human pregnancy appeared in 1991 (5). Verapamil, a calcium
channel-blocking agent, is as effective as adenosine in converting an PSVT to sinus rhythm, in the general population (6). Peripheral vasodilation and negative inotropy are unwanted sideeffects causing or xacerbating systemic hypotension, congestive heart failure, bradyarrhythmias, and ventricular fibrillation. In addition, verapamil readily crosses the placenta and has been shown to cause fetal bradycardia, heart block, and when used in higher doses, fetal toxicity. There are limited reports of its safety and efficacy for use in pregnancy for treatment of PSVT (7,8).
3. diSCuSSion A 32-yr-old caucasian woman, physician, with a BMI of 23.67 (height 1.67 m and weight 66 kg at term) without past history of heart disease, except PSVT from childhood. No history of smoking or alcohol abuse. She took verapamil as needed for her PSVT episodes and this proved successful. At 38 weeks of gestation during her first pregnancy, in the morning, she suffered from an attack of PSVT. She was seen by her family physician and her PSVT was confirmed by ECG; with heart rate 219 beats/min(fig.1)Fig. 1. Shows ECG during the attack of PSVT in the pregnant woman He recommended for her to take verapamil orally (40 mg), since it always reverted her arrhythmia to a normal sinus rhythm. However, this time PSVT was not converted to a normal sinus rhythm even after 8 hours, at which point she was referred to the nearest Emergency Center where she was given
305
MED ARH 2010; 64(5) CaSe rePort
Supraventricular tachycardia in Pregnancy
figure 1. ECG. shows ECG of attack of paroxysmal supraventricular tachycardia in the pregnant woman
figure 2. ECG. Shows ECG changes after adenosine administration with bursts of ventricular tachycardia and cardiac pauses
figure 3. ECG. Shows ECG conversion into normal sinusal rhythm
verapamil intravenously, with no effect. Since, she was not hemodynamically stable (BP=80/40 mmHg) and her symptoms worsened she was sent to our Emergency Center at 11:35 PM. Because verapamil was ineffective, we decided to terminate PSVT with adenosine, 6 mg rapidly intravenously. The PSVT was successfully terminated after a short burst of VT (Figure 1) and cardiac cycle pauses (Figure 2), followed by sinus rhythm (Figure 3). The PSVT had lasted for more than 15 hours. She was discharged and returned at 40 weeks in labour, which developed spontaneously. Delivery of a healthy baby occurred shortly afterwards. The consequent echocardiography did not show any pathology. Paroxysmal supraventricular tachycardia is seen somewhat frequently in the emergency department but less frequently during pregnancy. However, it is the commonest sustained arrhythmia in pregnant women. Definition and pathoanatomy of PSVT is well known. Diagnosis is confirmed by ECG. Paroxysmal supraventricular tachycardia, per se, and pharmacological treatment of PSVT in pregnancy may affect both mother and fetus. For this reason, nonpharmacological treatment (vagal maneuvers, Valsalva maneuver and facial 306
ice immersion), is treatment of choice to terminate PSVT and to avoid side effects of medications. Pharmacological treatment is best reserved for those with haemodynamic changes, severe symptoms or sustained arrhythmias. Verapamil has been the most commonly used agent for the treatment of PSVT with a narrow QRS complex. Potential side effects of verapamil including systemic hypotension, acute heart failure, bradyarrhythmia, and heart block may occur in pregnant women. After placental transfer bradycardia, heart block, depression of contractility, ventricular fibrillation and hypotension may be induced in the fetus. In addition, verapamil readily crosses the placenta and has been shown to cause fetal bradycardia, heart block and in higher doses, fetal toxicity. There are limited reports of its safety and efficacy for use in pregnancy for treatment of PSVT (8,9). Adenosine is rapidly metabolized with an elimination half-life of less than 10 s; it transiently depresses sinus node activity and slows atrioventricular conduction, and is very effective in terminating PSVT even in the cases of hypotension and other unstable conditions. In addition adenosine does not cross the placenta, making it suitable for use in pregnancy. After its first use in
1991 (7) numerous case reports (3) and a retrospective study (4), suggest that adenosine is safe and effective. Safety and effectiveness has been reported when verapamil was ineffective (9). We report on the case of 32-yr-old physician, suffering PSVT, that orally used verapamil after 2 hours of PSVT onset, was ineffective. Verapamil was used intravenously approximately 6 hours after oral use and caused the unwanted side effects of hypotension and acute congestive heart failure. In this unstable condition she was admitted in our centre after approximately 15 hours of PSVT. After taking ECG, SPO2, respiration rate and blood pressure monitoring, she was given adenosine intravenously. After a very short burst of VT and pauses she was converted to sinus rhythm. During the time of attack, it was referred that she had palpitations and pulse rate at always approximately 220 beats/min. The symptoms dramatically worsened after intravenous verapamil use.
4. ConCluSion PSVT in pregnancy may occur without any detectable reasons. Use of verapamil in our case was not effective, furthermore it deteriorated the condition and impaired hemodynamics Adenosine proved as safe and effective in treatment of PSVT in pregnancy. referenCeS
1. 2. 3. Nelson-Piercy C. Handbook of Obstetric Medicine, 2nd edn. London: Martin Dunitz, 2002; 22-3 Oakley C. Heart Disease in Pregnancy, 1st edn. London: British Medical Association, 1997; 248-9 Harrison JK, Greenfeld RA, Wharton JM. Acute termination of supraventricular tachycardia by adenosine during pregnancy. Am Heart J, 1992; 5: 1386-8. Elkayam U, Goodwin TM. Adenosine therapy for supraventricular tachycardia during pregnancy. Am J Cardiol, 1995; 75: 521-3. Podolsky SM, Varon J. Adenosine use during pregnancy. Ann Emerg Med, 1991;20:10278. Garratt C, Linker N, Griffith M, Ward D, Camm AJ. Comparison of adenosine and verapamil for termination of paroxysmal junctional tachycardia. Am J Cardiol, 1989; 64: 1310-16. Bryerly WG, Hartmann A, Foster DE, Tannenbaum AK. Verapamil in the treatment of maternal paroxysmal supraventricular tachycardia. Ann Emerg Med, 1991; 20:552-4. Mason BA, Ricci-Goodman J, Koos BJ. Adenosine in the treatment of maternal paroxysmal supraventricular tachycardia. Obstet Gynecol, 1992 Sep;80(3 Pt 2):478-80. Hsl P, Rust M, Johannigmann J, Schmidt G. Paroxysmal supraventricular tachycardia in pregnancy. Value of adenosine and other anti-arrhythmia agents. Geburtshilfe Frauenheilkd, 1996 Jun;56(6):313-6.
4. 5. 6.
7.
8.
9.
MED ARH 2010; 64(5) CaSe rePort
You might also like
- Money Tooth BookDocument41 pagesMoney Tooth BookVizi Adrian0% (2)
- Case Analysis and Prescribing Techniques Robin Murphy.01213 1contentsDocument3 pagesCase Analysis and Prescribing Techniques Robin Murphy.01213 1contentsTanveer HussainNo ratings yet
- Wellness MarketDocument104 pagesWellness MarketsnehakopadeNo ratings yet
- Short Answer Questions AnaesthesiaDocument91 pagesShort Answer Questions AnaesthesiaMeena Ct100% (12)
- ArticuloDocument8 pagesArticuloveliaisabelvelazquezNo ratings yet
- Anesthetic Challenges and Successful Management of Uncorrected Tetralogy of Fallot (Tof) in PregnancyDocument3 pagesAnesthetic Challenges and Successful Management of Uncorrected Tetralogy of Fallot (Tof) in PregnancyIJAR JOURNALNo ratings yet
- Eclampsia Precedes Pre-EclampsiaDocument3 pagesEclampsia Precedes Pre-EclampsiaIOSRjournalNo ratings yet
- Heart Diseases in PregnancyDocument70 pagesHeart Diseases in PregnancySergiu HelciugNo ratings yet
- 2015 319 TJOG RefractoryVTinpregnancyDocument3 pages2015 319 TJOG RefractoryVTinpregnancyIsmul 'D' SadlyNo ratings yet
- Epidural Anesthesia For Cesarean Section For Pregnant Women With Rheumatic Heart Disease and Mitral StenosisDocument6 pagesEpidural Anesthesia For Cesarean Section For Pregnant Women With Rheumatic Heart Disease and Mitral StenosisNengLukmanNo ratings yet
- MX Postpartum HPTDocument6 pagesMX Postpartum HPTPavani NallaluthanNo ratings yet
- Anesthesia For High Risk PatientDocument5 pagesAnesthesia For High Risk PatientAfrida SahestinaNo ratings yet
- Arrhythmiasinpreg 140820163522 Phpapp01Document24 pagesArrhythmiasinpreg 140820163522 Phpapp01fajaroktavianNo ratings yet
- Heart Disease in Pregnancy VoiceoverDocument30 pagesHeart Disease in Pregnancy VoiceoverMohammed AbdNo ratings yet
- Case Reflection Pregnant Woman With Mitral Valve Prolapse: William Ray Cassidy 08/268114/KU/12814Document7 pagesCase Reflection Pregnant Woman With Mitral Valve Prolapse: William Ray Cassidy 08/268114/KU/12814WilliamRayCassidyNo ratings yet
- ContentServer 2Document5 pagesContentServer 2Ni Wayan Ana PsNo ratings yet
- Guideline For The Management of Hypertensive Disorders of PregnancyDocument51 pagesGuideline For The Management of Hypertensive Disorders of PregnancyAhmad JokhadarNo ratings yet
- Anesthetic ComplicationsDocument28 pagesAnesthetic ComplicationsSamuel RealesNo ratings yet
- Regional Anesthesia in Patients With Pregnancy Induced HypertensionDocument10 pagesRegional Anesthesia in Patients With Pregnancy Induced HypertensionEdo GeradNo ratings yet
- Atrio-Ventricular Septal Defect in Pregnant Women, How To Deal With It: A Case StudyDocument6 pagesAtrio-Ventricular Septal Defect in Pregnant Women, How To Deal With It: A Case StudyDara Dasawulansari SyamsuriNo ratings yet
- Anestesi Spinal Pada Seksio Sesaria Wanita Dengan Tetralogy Fallot Tidak TerkoreksiDocument6 pagesAnestesi Spinal Pada Seksio Sesaria Wanita Dengan Tetralogy Fallot Tidak TerkoreksimarinarizkyutamiNo ratings yet
- Pentalogy of Fallot Review NotesDocument11 pagesPentalogy of Fallot Review NotesMutivanya Inez MaharaniNo ratings yet
- Anaesthetic of Choice During Pregnancy and LactationDocument5 pagesAnaesthetic of Choice During Pregnancy and LactationDegefu TadesseNo ratings yet
- Ghid Esc Din 2018Document6 pagesGhid Esc Din 2018Flavius Ion NicolaeNo ratings yet
- Thromboembolism & ThromboprophylaxisDocument48 pagesThromboembolism & Thromboprophylaxisazida90No ratings yet
- Cardiac Arrhythmias in The Pregnant Woman and The Foetus: Arrhythmia ManagementDocument5 pagesCardiac Arrhythmias in The Pregnant Woman and The Foetus: Arrhythmia ManagementRendyNo ratings yet
- Regional Anesthesia in Patients With Pregnancy Induced HypertensionDocument10 pagesRegional Anesthesia in Patients With Pregnancy Induced Hypertensionwindy patadunganNo ratings yet
- Acog HtaDocument7 pagesAcog HtaLaura María Salamanca TerneraNo ratings yet
- Anesthesia For Cesarean SectionDocument84 pagesAnesthesia For Cesarean SectionCharlene Serino JavierNo ratings yet
- Pre-Eclampsia: A Lifelong Disorder: 1974 (CWLTH) Both Need Further ExaminationDocument3 pagesPre-Eclampsia: A Lifelong Disorder: 1974 (CWLTH) Both Need Further ExaminationCarloxs1No ratings yet
- Pre Eclampsia and Eclampsia: A Review and Recent UpdatesDocument38 pagesPre Eclampsia and Eclampsia: A Review and Recent UpdatesHan OWNo ratings yet
- Oajtmr 02 00054Document3 pagesOajtmr 02 00054MorindaNo ratings yet
- Anesthesia For Cesarean SectionDocument84 pagesAnesthesia For Cesarean SectionNunung HasanahNo ratings yet
- Assessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaDocument6 pagesAssessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaprabuNo ratings yet
- Pengaruh Anestesi Regional Dan General Pada Sectio Cesaria Pada Ibu Dengan Pre Eklampsia Berat Terhadap Apgar ScoreDocument11 pagesPengaruh Anestesi Regional Dan General Pada Sectio Cesaria Pada Ibu Dengan Pre Eklampsia Berat Terhadap Apgar ScoreJessica TobingNo ratings yet
- Case Report: Perioperative Management of A Patient With Secreting Paraganglioma Undergoing Cesarean SectionDocument3 pagesCase Report: Perioperative Management of A Patient With Secreting Paraganglioma Undergoing Cesarean SectionYolanda FitrianiNo ratings yet
- Pathophysiology and Medical Management of Systemic Hypertension in PregnancyDocument11 pagesPathophysiology and Medical Management of Systemic Hypertension in Pregnancydr faathirNo ratings yet
- Management of Anesthesia in A Pregnant Patient With An Unmodified Congenital Heart DiseaseDocument5 pagesManagement of Anesthesia in A Pregnant Patient With An Unmodified Congenital Heart DiseaseZakia DrajatNo ratings yet
- Classification of Hypertension in Pregnancy: 10 Tables11 And2,2 10 11 12 13Document3 pagesClassification of Hypertension in Pregnancy: 10 Tables11 And2,2 10 11 12 13Melinda KusumadewiNo ratings yet
- Complications of Pregnancy: Clinical Guidelines O MDocument23 pagesComplications of Pregnancy: Clinical Guidelines O MTiong NeeNo ratings yet
- Cardiac Disease and Pregnancy: Clinical GuidelinesDocument9 pagesCardiac Disease and Pregnancy: Clinical GuidelinesBagus Wanda Habibullah100% (1)
- 1 s2.0 S2666668521001324 MainDocument5 pages1 s2.0 S2666668521001324 Mainmchojnacki81No ratings yet
- Management Postpartum HipertensionDocument6 pagesManagement Postpartum HipertensionRegina MeliaNo ratings yet
- Abstrak Makalah Bebas MedanDocument11 pagesAbstrak Makalah Bebas Medandr.raziNo ratings yet
- Antepartum and Postpartum Uterine ArteryDocument7 pagesAntepartum and Postpartum Uterine ArterypaolabriglimNo ratings yet
- BJOG P 380Document2 pagesBJOG P 380Amanqui Alex DerlyNo ratings yet
- Emergency Cesarean in A Patient With Atrial Septal DefectDocument3 pagesEmergency Cesarean in A Patient With Atrial Septal DefectDara Dasawulansari SyamsuriNo ratings yet
- Case Based Discussion KB PH, MSDocument8 pagesCase Based Discussion KB PH, MSRaziNo ratings yet
- Progression of Diabetic Retinopathy During Pregnancy in Women With Type 2 DiabetesDocument8 pagesProgression of Diabetic Retinopathy During Pregnancy in Women With Type 2 DiabetesEstela Beatríz Mora GarcíaNo ratings yet
- Anesthesia For Cesarean SectionDocument84 pagesAnesthesia For Cesarean SectionssamaddNo ratings yet
- Is The Prophylactic Administration of Magnesium Sulphate in Women With Pre-Eclampsia Indicated Prior To Labour?Document6 pagesIs The Prophylactic Administration of Magnesium Sulphate in Women With Pre-Eclampsia Indicated Prior To Labour?Jananuraga MaharddhikaNo ratings yet
- Jurnal AdeDocument5 pagesJurnal AdeSuryanti SultanNo ratings yet
- PR Refkas - Peripartum CardiomyopathyDocument16 pagesPR Refkas - Peripartum CardiomyopathyakmilNo ratings yet
- Case ReportDocument4 pagesCase ReportStella RNo ratings yet
- International Journal of Scientific Research: AnesthesiologyDocument2 pagesInternational Journal of Scientific Research: AnesthesiologyALfuNo ratings yet
- 1 PBDocument4 pages1 PBkadek sanggingNo ratings yet
- Obestritic Anesthesia DNB Q & ADocument162 pagesObestritic Anesthesia DNB Q & Ahiwotbetesfa2123No ratings yet
- 2.2.1 Medical Management T C: 2 Complications of PregnancyDocument19 pages2.2.1 Medical Management T C: 2 Complications of PregnancyMohamad Rizki DwikaneNo ratings yet
- Transient Severe Isolated Right Ventricular Hypertrophy in Neonates. Hayrullah Alp Et Al. 2014Document3 pagesTransient Severe Isolated Right Ventricular Hypertrophy in Neonates. Hayrullah Alp Et Al. 2014EgorSazhaevNo ratings yet
- 4810cr10 PDFDocument2 pages4810cr10 PDFdr.putra888No ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- BurnvictimcasestudyDocument55 pagesBurnvictimcasestudyapi-289388577No ratings yet
- Neral PractitionersDocument216 pagesNeral PractitionersSudhir Tyagi100% (1)
- Pds UpdatedDocument2 pagesPds Updatedapi-609488951No ratings yet
- Musculoskeletal Imaging - The Basics: Laurie Lomasney, MD Department of Radiology Loyola University Medical CenterDocument45 pagesMusculoskeletal Imaging - The Basics: Laurie Lomasney, MD Department of Radiology Loyola University Medical CenterJohnny CordayNo ratings yet
- Nephrotoxic Drugs - Ready ReckonersDocument14 pagesNephrotoxic Drugs - Ready ReckonerskrgduraiNo ratings yet
- How The Strategy of The 12 Magic Points Makes A Tiger With A Pair of Wings 1294072199Document3 pagesHow The Strategy of The 12 Magic Points Makes A Tiger With A Pair of Wings 1294072199kahuna_ronbo3313100% (1)
- MRI BasicsDocument129 pagesMRI BasicsAnmol Agrawal100% (1)
- Option Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsDocument7 pagesOption Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsJig GamoloNo ratings yet
- Carl Rogers - Person-Centered Theory PDFDocument21 pagesCarl Rogers - Person-Centered Theory PDFAiden Lee50% (2)
- FentanylDocument1 pageFentanylAndreas MedicNo ratings yet
- AcromegalyDocument15 pagesAcromegalyHernandez LennieNo ratings yet
- Revised Rate ListDocument127 pagesRevised Rate ListBarnali Majumder100% (1)
- Scabies Management: Community Control of ScabiesDocument3 pagesScabies Management: Community Control of Scabiespet_trinNo ratings yet
- PDF My English Lab Top Notch 3Document15 pagesPDF My English Lab Top Notch 3Jorge Rhenals100% (2)
- Changing Face of Homoeopathic Pharmacy: Lecture by Dr. P. N. VarmaDocument44 pagesChanging Face of Homoeopathic Pharmacy: Lecture by Dr. P. N. VarmawasiuddinNo ratings yet
- Contact Lenses Sss 2013Document33 pagesContact Lenses Sss 2013Peter HoNo ratings yet
- Wrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Document63 pagesWrist Anatomy: Bones Quiz - What Bones Comprise The Wrist? Joints Quiz - What Joints Comprise The Wrist?Mnn SaabNo ratings yet
- Labiaplasty: A Guide For WomenDocument3 pagesLabiaplasty: A Guide For WomenBudi Iman SantosoNo ratings yet
- Soalan Pathology 2Document347 pagesSoalan Pathology 2muhammadridhwanNo ratings yet
- PET - CT Raditherapy Planning PDFDocument121 pagesPET - CT Raditherapy Planning PDFPatricia MeloNo ratings yet
- AnencephalyDocument10 pagesAnencephalyRm LavariasNo ratings yet
- Revascularizacion CardiacaDocument100 pagesRevascularizacion CardiacaDaniel PradenasNo ratings yet
- Ophthalmology Revision LectureDocument80 pagesOphthalmology Revision LectureCarla LaniganNo ratings yet
- Act 586 Private Healthcare Facilities and Services Act 1998 PDFDocument84 pagesAct 586 Private Healthcare Facilities and Services Act 1998 PDFAdam Haida & Co100% (1)
- Croup SyndromeDocument3 pagesCroup SyndromeMabesNo ratings yet
- Health Assessment (Pain and Nutritional Assessment)Document5 pagesHealth Assessment (Pain and Nutritional Assessment)Lc VillahermosaNo ratings yet
- NeuroblastomaDocument9 pagesNeuroblastomasamantha mccoyNo ratings yet