Professional Documents
Culture Documents
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Uploaded by
Kunal YadavCopyright:
Available Formats
You might also like
- Richard M. Rosenfeld, Charles D. Bluestone - Evidence-Based Otitis Media (2003, PMPH-USA)Document546 pagesRichard M. Rosenfeld, Charles D. Bluestone - Evidence-Based Otitis Media (2003, PMPH-USA)Carmen-BadeaNo ratings yet
- IDSP P&L FormsDocument2 pagesIDSP P&L FormsKunal YadavNo ratings yet
- Research Paper: Alzheimer's DiseaseDocument13 pagesResearch Paper: Alzheimer's DiseaseABC Four CornersNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiapriiiiiiilllNo ratings yet
- Comparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphineDocument7 pagesComparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphinenatamkpNo ratings yet
- Baby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn InfantsDocument6 pagesBaby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn Infantsgladeva yugi antariNo ratings yet
- Comparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDocument8 pagesComparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDendy AgusNo ratings yet
- BjorlDocument6 pagesBjorlaaNo ratings yet
- Dr. - Nataraj - EJCM 132 1888 1893 2023Document7 pagesDr. - Nataraj - EJCM 132 1888 1893 2023vithz kNo ratings yet
- Ojog20120300033 78059405 PDFDocument5 pagesOjog20120300033 78059405 PDFPalwasha MalikNo ratings yet
- Midazolam Prevent AgitationDocument13 pagesMidazolam Prevent AgitationUzZySusFabregasNo ratings yet
- Comparison of Caudal Morphine and Tramadol For Postoperative Pain Control in Children Undergoing Inguinal HerniorrhaphyDocument6 pagesComparison of Caudal Morphine and Tramadol For Postoperative Pain Control in Children Undergoing Inguinal Herniorrhaphymanoj9980No ratings yet
- 1 s2.0 S0007091217366175 MainDocument5 pages1 s2.0 S0007091217366175 MainMeutia LaksaniNo ratings yet
- Heel Stick ThailandDocument9 pagesHeel Stick ThailandStaporn KasemsripitakNo ratings yet
- 334 EnglishDocument7 pages334 EnglishkhalidNo ratings yet
- Articulo 2Document7 pagesArticulo 2Christian Yzaguirre AbantoNo ratings yet
- Penggunaan Sedasi Pada Anak Dengan VentilatorDocument5 pagesPenggunaan Sedasi Pada Anak Dengan VentilatorCalvin AffendyNo ratings yet
- A Comparison of Three Induction Agents in Paediatric Anaesthesia-Cardiovascular Effects and RecoveryDocument11 pagesA Comparison of Three Induction Agents in Paediatric Anaesthesia-Cardiovascular Effects and RecoveryAlibai Guiapal SalakobNo ratings yet
- CA Novi AnestesiDocument7 pagesCA Novi AnestesiearlynkNo ratings yet
- Anaesthetic Consideration For Neonatal Surgical Emergencies: Review ArticleDocument7 pagesAnaesthetic Consideration For Neonatal Surgical Emergencies: Review ArticleArun JoseNo ratings yet
- Wa0001Document10 pagesWa0001rini sundariNo ratings yet
- Successful Implementation of A Pediatric Sedation Protocol For Mechanically Ventilated PatientsDocument6 pagesSuccessful Implementation of A Pediatric Sedation Protocol For Mechanically Ventilated PatientsSantosa TandiNo ratings yet
- The Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUDocument11 pagesThe Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comparison Between Epidural and IV Tramadol For Painless Labor and Effect On Perinatal OutcomeDocument10 pagesA Comparison Between Epidural and IV Tramadol For Painless Labor and Effect On Perinatal OutcomeLibay Villamor IsmaelNo ratings yet
- Prevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus KetamineDocument17 pagesPrevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus Ketamineandi ananNo ratings yet
- Research ArticleDocument7 pagesResearch Articlenaljnaby9No ratings yet
- Anaesthetic Consideration For Neonatal Surgical emDocument7 pagesAnaesthetic Consideration For Neonatal Surgical emLong LongNo ratings yet
- Complementary Therapies in Medicine: SciencedirectDocument6 pagesComplementary Therapies in Medicine: SciencedirectSurya Puji KusumaNo ratings yet
- A Follow-Up KAISA 2013Document6 pagesA Follow-Up KAISA 2013Daniela LucenaNo ratings yet
- Journal 3Document9 pagesJournal 3Suryanti SultanNo ratings yet
- Musa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim NasseriDocument6 pagesMusa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim Nasseridebby claudiNo ratings yet
- Handling ComparingDocument13 pagesHandling ComparingNunik KhoirunnisaNo ratings yet
- Tramadol en NiñosDocument5 pagesTramadol en NiñosElias Vera RojasNo ratings yet
- Anesthetic Management of A Newborn With A Cervical Meningomyelocele S. P, A. U, S M J M. RDocument4 pagesAnesthetic Management of A Newborn With A Cervical Meningomyelocele S. P, A. U, S M J M. RAnis Eka SukmadadariNo ratings yet
- 0256-4947 2015 58 PDFDocument7 pages0256-4947 2015 58 PDFUlfani DewiNo ratings yet
- Addition of Low-Dose Ketamine To Midazolam-fentanyl-propofol-Based Sedation For Colonoscopy A Randomized, Double-Blind, Controlled TrialDocument6 pagesAddition of Low-Dose Ketamine To Midazolam-fentanyl-propofol-Based Sedation For Colonoscopy A Randomized, Double-Blind, Controlled TrialRoderick Samuel PrenticeNo ratings yet
- 0 Aet484Document7 pages0 Aet484UsbahNo ratings yet
- The Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenDocument7 pagesThe Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenNi Komang Suryani DewiNo ratings yet
- DR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaDocument9 pagesDR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaIOSRjournalNo ratings yet
- Paracetamol vs. Dexketoprofen PDFDocument5 pagesParacetamol vs. Dexketoprofen PDFMikeNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- Ect in PregncyDocument13 pagesEct in PregncySasi KumarNo ratings yet
- Pediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineDocument7 pagesPediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineFatty MaulidiraNo ratings yet
- Annex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)Document7 pagesAnnex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)KHAIRULNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument6 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- The Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFDocument6 pagesThe Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFUmmu Qonitah AfnidawatiNo ratings yet
- 100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Document11 pages100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Haymanot AnimutNo ratings yet
- Ondan Hipo 2Document6 pagesOndan Hipo 2putri maharani andesNo ratings yet
- Cag La Oz Bak Isak Kurt 2009Document7 pagesCag La Oz Bak Isak Kurt 2009Arturo AlcantaraNo ratings yet
- Pediatrics DNB Q & ADocument132 pagesPediatrics DNB Q & Ahiwotbetesfa2123No ratings yet
- Pain MX 2nd Stage of Labour NoDocument19 pagesPain MX 2nd Stage of Labour NoMd NohNo ratings yet
- Paediatric Sedation: Michael R. J. Sury FRCADocument5 pagesPaediatric Sedation: Michael R. J. Sury FRCAZazzZaffaNo ratings yet
- Jtgga 4 2 110 165Document56 pagesJtgga 4 2 110 165drklftNo ratings yet
- Evaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryDocument8 pagesEvaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryAudra Firthi Dea NoorafiattyNo ratings yet
- Pain Relief During Labor and Delivery: A Brief 2013 UpdateDocument5 pagesPain Relief During Labor and Delivery: A Brief 2013 UpdateJheiczhietoot KibasNo ratings yet
- Paediatric Anaesthesia PDFDocument33 pagesPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriNo ratings yet
- Advantages of Tonsillectomy Done Under Local Word PDFDocument6 pagesAdvantages of Tonsillectomy Done Under Local Word PDFAgus KarsetiyonoNo ratings yet
- AnesthEssaysRes83324-3429942 093139Document6 pagesAnesthEssaysRes83324-3429942 093139burhanNo ratings yet
- 343-Article Text-653-1-10-20190607Document5 pages343-Article Text-653-1-10-20190607Zulkifli FachriyanNo ratings yet
- Preoperative Stabilisation in Congenital Diaphragmatic HerniaDocument3 pagesPreoperative Stabilisation in Congenital Diaphragmatic HerniaAgus PrimaNo ratings yet
- Rocuronium Versus Succinylcholine Are They.9Document4 pagesRocuronium Versus Succinylcholine Are They.9Kian PrakashNo ratings yet
- Pediatric Regional AnesthesiaDocument6 pagesPediatric Regional Anesthesiatq9prx5s5qNo ratings yet
- Uterus TransplantationFrom EverandUterus TransplantationMats BrännströmNo ratings yet
- Drugs For SNCUDocument2 pagesDrugs For SNCUKunal YadavNo ratings yet
- Strategic Alliances The Role of Civil Society in HealthDocument12 pagesStrategic Alliances The Role of Civil Society in HealthKunal YadavNo ratings yet
- Nutritional Rehabilitation CenterDocument12 pagesNutritional Rehabilitation CenterKunal Yadav0% (1)
- July, 2023 Nursing and Training Report.Document20 pagesJuly, 2023 Nursing and Training Report.Tosi AboloNo ratings yet
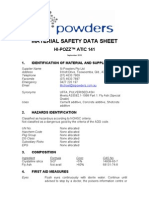
- Msds Hi PozzDocument6 pagesMsds Hi Pozzpenis1493No ratings yet
- Annotated BibliographyDocument8 pagesAnnotated Bibliographyapi-538355468No ratings yet
- Ssi Rabu, 29 Juni 2022Document49 pagesSsi Rabu, 29 Juni 2022Dhamar SetiaNo ratings yet
- Statewise HospitalsDocument426 pagesStatewise HospitalsdevNo ratings yet
- PharmacokineticsDocument10 pagesPharmacokineticsbrian3442No ratings yet
- Ferenczi - Confusion of The TonguesDocument5 pagesFerenczi - Confusion of The TonguessticataNo ratings yet
- ChokingDocument2 pagesChokingdrfidelenriqueNo ratings yet
- Common Breast DiseasesDocument64 pagesCommon Breast Diseasesamirahmei100% (1)
- Railway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Document8 pagesRailway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Latest Laws TeamNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharDocument97 pagesNonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharTarek NasrallahNo ratings yet
- OG Informing Abortion Debate DR Christine BaileyDocument2 pagesOG Informing Abortion Debate DR Christine BaileyYwagar YwagarNo ratings yet
- Nursing Care in ECTDocument3 pagesNursing Care in ECTRawan KhateebNo ratings yet
- 4 Relining TechniquesDocument9 pages4 Relining TechniquesvinnycoolbuddyNo ratings yet
- Occupational English Test: Writing Subtest: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Subtest: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesHarold MedranoNo ratings yet
- Case Analysis: American WellDocument2 pagesCase Analysis: American WellTatsat PandeyNo ratings yet
- Curriculum Vitae Mladen Boban, M.D., Ph.D. Personal InformationDocument2 pagesCurriculum Vitae Mladen Boban, M.D., Ph.D. Personal InformationGoran MaliNo ratings yet
- Common Errors in Xray Interpretation 2Document49 pagesCommon Errors in Xray Interpretation 2Shri RamaNo ratings yet
- Leukorrhea Panel PDFDocument8 pagesLeukorrhea Panel PDFahmadNo ratings yet
- Review Factors Contributing To Medication Errors: A Literature ReviewDocument9 pagesReview Factors Contributing To Medication Errors: A Literature Reviewsoul_0602No ratings yet
- FTC Vs HCG Diet Direct, Clint EthingtonDocument40 pagesFTC Vs HCG Diet Direct, Clint Ethingtontheskeptic21No ratings yet
- Removable Partial Denture Framework Try-InDocument13 pagesRemovable Partial Denture Framework Try-InAnye PutriNo ratings yet
- Oral Systemic ConnectionDocument37 pagesOral Systemic Connectionchrisdina puspita sari100% (1)
- Hon 2005Document5 pagesHon 2005lenirizkiNo ratings yet
- Bum Run GradDocument10 pagesBum Run GradsabyasachiNo ratings yet
- Investigatory Project On Malaria: Name: M.Bhavya Class: XI C' Year: 2018 - 2019Document18 pagesInvestigatory Project On Malaria: Name: M.Bhavya Class: XI C' Year: 2018 - 2019Muramsetty Bhavya0% (1)
- All About Nails - CosmetologyDocument6 pagesAll About Nails - CosmetologySheryline BonillaNo ratings yet
- PSGDocument57 pagesPSGsg1964No ratings yet
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Uploaded by
Kunal YadavOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Uploaded by
Kunal YadavCopyright:
Available Formats
Tr. J.
of Medical Sciences 29 (1999) 467-470 TBTAK
Binnur SARIHASAN Sibel BARI Fadime YELTA Ayla TR Haydar AHNOLU Emre STN Fuat GLDOU Deniz KARAKAYA Zeynep KAYHAN
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
Received: January 12, 1998
Abstract: This study was designed to investigate the anxiolytic effects as well as acceptance of spinal anesthesia after rectally administered midazolam, ketamine and atropine for postoperative sedation in children. Spinal anesthesia is an easy and safe method in the pediatric age group especially for outpatients. Spinal anesthesia was administered to 20 patients, aged between 2 months and 2 years, premedicated with 0.5 mg/kg midazolam + 5 mg/kg ketamine + 0.02 mg/kg atropine rectally. During vein puncture 14 children were asleep, 5 children were
anxious and 1 child was crying and during spinal anesthesia 7 children were asleep, 10 children were anxious and 3 children were crying. Motor and sensorial blockade was observed in 17 childern. 12 of them were asleep, but 5 children were anxious during surgery. We found that rectal premedication with midazolam, ketamine and atropine increases tolerance to vein puncture and spinal anesthesia. Key Words: Spinal anesthesia, rectal premedication, midazolam, ketamine, atropine.
Department of Anesthesiology Faculty of Medicine, Ondokuzmays University SamsunTurkey
Introduction The goal of pediatric premedication is to decrease anxiety and promote cooperation without depressing physiological functions. Sedation is recommended only in infants older than 6 to 8 weeks, during induction of anesthesia, vein puncture or spinal anesthesia. Rectal administration is an easy, painless and reliable way of premedication. Midazolam is anxyolitic, and produces amnesia, with a rapid onset and short halflife. It can be administered in several ways, including rectally with fast absorption (1). Ketamine is hypnotic and analgesic, and provides excellent cardiovascular and respitaroy stability. Ketamine may also be administered rectally (24). General anesthesia especially in infants is associated with significant risk. Spinal anesthesia in the high risk infant and child is simple, safe and effective. The hazard of apnea in premature infants is reduced. It has been confirmed that spinal anesthesia can indeed be a safe alternative to general anesthesia in the pediatric age group (5). This article summarises our experience with spinal anesthesia in 20 patients between 2 months and 2 years of age, who were given rectal premedication.
Materials and Methods Following approval from the Ethics Committee, twently healthy children (ASA1), aged 2 months2 years, scheduled for elective lower abdominal surgery, with a body weight ranging form 4 to 14 kg, were studied. In the operating room after electrocardiographic monitorization, all children were rectally premedicated with a mixture of 0.5 mg/kg midazolam, 5 mg/kg ketamine, 0.02 mg/kg atropine with saline (total volume 10 ml). All children received this solution 34 cm proximal to the anal sphincter by means of a disposable applicator and syringe. The buttocks were held together for 12 minutes after the administration. Vein puncture and spinal anesthesia were applied approximately 10 and 2025 minutes after the premedication, respectively. The children were placed in the lateral decubitus position for spinal anesthesia, and the back was cleansed with an iodophore solution. Lumbar puncture was performed in the lowest most easily palpable interspace below the third lumbar vertebra using a 22 gauge 3.5 cm disposable spinal needle. Skin analgesia was not used. When a free flow of cerebrospinal fluid (CSF) was obtained, 1 mg/kg articaine with 10% dextrose (total 467
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
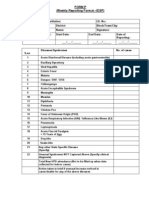
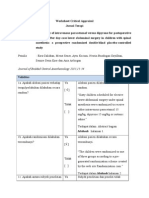
volume 0.15 ml/kg) was administered. CSF was not aspirated before or after the injection in order to prevent significant dilution of the small volume of local anesthetic. After removal of the spinal needle, the children were placed in the supine position. The legs were observed for signs of paralysis. The level of sensorial block was assessed using the pinprick method. The time from spinal anesthesia to motor block, the level of sensorial block and the time of motor block were noted. The degree of sedation (sleeping, awake but calm, anxious and very anxious or crying) was obtained preoperatively, on the 5th and 10th minutes after the premedication, during vein puncture and spinal anesthesia and the beginning of the surgery. The heart rate was obtained at the same times, and complications were noted. All children were monitored and observed postoperatively until they moved their legs. The Wilcoxon rank sum test was employed for the statistical analysis. Results Table 1 shows the demographic and clinical variables of the children. Preoperative diagnosis of the patients are presented in Table 2. Heart rates are presented as meanSD in Figure 1. Mean time from premedication to vein puncture was 12.054.36, mean time from premedication to spinal anesthesia was 23.555.61, mean time from spinal anesthesia to motor block was 4.332.72, mean duration of motor block was 28.4712.01 and mean duration of surgery was 37.03.9. In 40% of the patients the level of sensorial block was T8, in 60% T10.
Table 1. Demographic and clinical variables of the children (n=20).
Before premedication, 3 children (15%) were awake but calm, 17 children (85%) were crying. Five minutes after the rectal premedication, 1 child (0.5%) was asleep, 18 children (90%) were awake but calm, 1 child (0.5%) was anxious. Ten minutes after the rectal premedication, 11 children (55%) were asleep, 9 children (45%) were awake but calm. During vein puncture 14 children (70%) were asleep, 5 children (25%) were anxious, 1 child (0.5%) was crying and during spinal anesthesia 7 children (35%) were asleep, 10 children (50%) were anxious and 3 children (15%) were crying. All 10 patients who were anxious during spinal anesthesia calmed down after the skin was punctured and thereafter remained calm during the procedure. In the 3 children who were crying during spinal anesthesia 0.05 mg/kg midazolam was administered by the intravenous route, and the patients calmed down (Figure 2). Motor and sensorial block was observed in 17 children (85%). And of these 12 children (70.5%) were asleep, but 5 children (25%) were anxious during surgery. Spinal anethesia was unsuccessful in 3 children (35%). The duration of motor block was sufficient for surgery in 6 children (27.5%), but 11 children (51%) with longer surgical time, 0.05 mg/kg iv midazolam or general anesthesia by mask was necessary. The side effects (nystagmus hiccough and premature ventricular contractions) are documented in Table 3. Discussion In our study, we found that rectal premedication with 0.5 mg/kg midazolam plus ketamine and atropine increases acceptance of vein puncture and spinal anesthesia. The reason for using midazolam, a water soluble benzodiazepine, as premedication for outpatient anesthesia was its shorter action in order to avoid heavily sedated children and subsequent risk of aspiration during the postoperative period. Midazolam is an anxiolytic agent, which produces amnesia, but acts as a hypnotic in high doses (1). Amnesia and drowsiness increase significantly when ketamine is added to midazolam and
Table 3. Side effects.
Mean SD Age (months) Weight (g) Sex 12.4 1.94 9185 696 18 male/2 female
Table 2.
Diagnosis of the children (n=20).
Preoperative diagnosis Inguinal hernia Hydrocele Circumcision Umbilical cyst
Number of patients 15 (bilateral in 2 children) 2 2 1
Side effects Nystagmus and hiccough Hiccough Premature ventricular contraction
Number of children (%) 8 (40%) 1 (0.05%) 1 (0.05%)
468
B. SARIHASAN, S. BARI et al.
100 Sleeping 90 80 70 60 50 40 30 20 10 0 T1
Figure 1. Awake Anxious Crying
Degree of sedation of children. T1: Before the premedication, T2: Five minutes after the premedication, T3: Ten minutes after the premedication, T4: During vein puncture, T5: During spinal anesthesia, T6: Surgical preface.
T2
T3
T4
T5
T6
bpm 127 126 125 124 123 122 121 120 119 118 T1 Heart rate
Figure 2.
Heart rate of the children (meanSD). T1: Before the premedication, T2: Five minutes after the premedication, T3: Ten minutes after the premedication, T4: During vein puncture, T5: During spinal anesthesia, T6: Surgical preface.
T2
T3
T4
T5
T6
after rectal administration of the two drugs (4). As salivation may be a problem, the antisialogogue effect of atropine is desirable as an additive to midazolam and ketamine (4). The dose of midazolam for rectal premedication is recommended as 0.15 to 0.5 mg/kg (6). Anderson et al. found that children receiving 0.4 or 0.5 mg/kg of midazolam showed an increase in the level of anxiolysis (8). In this study, 0.5 mg/kg midazolam was used in order to obtain anxiolytic effect during spinal anesthesia and operation. Midazolam and ketamine were used by Lokken et al. in 24 children receiving dental therapy and a significant decrease in anxiety and amnesia was observed (8). In another study, sufficient amnesia and sedation in 83 children were obtained by rectal premedication with midazolam (9). Shane et al. compared 0.45 mg/kg midazolam and observed that the sedation degree was
good in 87% of children (10). Beebe used 0.5 mg/kg midazolam+3 mg/kg atropine in four groups in different combinations (Group 1: midazolam + ketamine + atropine, Group 2: midazolam + atropine, Group 3: ketamine + atropine, Group 4: just atropine) (11). In the first group, none of the children were crying or anxious and 40% of the children were asleep. In the study of Piotrowski, 66.7% of children accepted the vein puncture very well, and 24% well (12). Similarly, we found that acceptance of vein puncture was very good in 70% and that spinal anesthesia was well tolerated in 35% of the children. This difference is probably caused by the fact that spinal anesthesia is a more painful and difficult procedure than vein puncture. Inguinal operations in childhood are routinely performed in the outpatient setting. The child is returned to the family after the operation and the emotional stress of hospitalisation is avoided. The advantages of spinal
469
Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and Atropine
anesthesia in infants and children have been described since 1909 (13). Abajian et al. in 1984 sparked an interest in the use of spinal anesthesia in high riskinfants (14). Subsequent articles have confirmed that spinal anesthesia is effective in this population. Most experience indicates that a minumum volume of 0.2 ml is necessary in the preterm or newborn infant. Any smaller volume results in frequent failures or inadequate anesthesia (15, 16). In our study, the dose of articaine
administered depended on the childrens weight. We observed that spinal anesthesia with articaine is indicated in short lower abdominal surgical procedures (duration less than 30 minutes) because of its short duration of action. It is concluded that rectal premedication with midazolam+ketamine and atropine increased tolerance to vein puncture and spinal anesthesia in children.
References
1. Allonen H, Anttila V, Klotz U. Efectkinetics of midazolam. A new hypnotic benzodiazepine derivative. Naunyn. Schmiedebergs Arch. Pharmacol. 316 (suppl.): R. 74, 1981. Schultetus RR, Paulus DA, Spohr GK. Haemodynamic effects of ketamine and thiopentone during anaesthetic induction caeserean section. Can. Anaesth. Soc. J. 32: 592, 1985. Cartwright PD, Pingel SM. Midazolam and diazepam in ketamine anaesthesia. Anaesthesia 38; 439, 1984. De Jang PC, Verburg MP. Comparison of rectal to intramuscular administration of midazolam and atropine for premedication of children. Acta Anaesthesiologica Scandinavica, 32 (6); 4859, 1988. Blaise G, Roy WL. Spinal anesthesia in children. Anesth. Analg. (Cleve), 63; 1139, 1984. Lokken P, Bakstad OJ, Fonnelop E. Consesious sedation by rectal administration of midazolam or plus ketamin as alternatives to general anesthesia for dental treatment of uncooperative children. Scandinavian Journal of Dental Research, 102 (5); 27478, 1994. 7. SaintMaurice C, Esteve C, Holzer J. Gaudiche O, Lauture D, Hetzel W. Bessere Akzeptanz Massnahmen zur Einletiung einer narkose nach rektaler pramedikation mit midazolam bei kindern. Anaesthesist 1987; 36: 62933. 8. Andersen G, Pedersen NA, Johansson G, Stjernholm, Reinstrup P. Rectal midazolam as premedicant in children: a dose response study. Paed Anaesth 1994; 4: 36570. Krafft TC, Kramer N, Kunzelmann KH, Hickel R. Experience with midazolam as sedative in the dental treatment of uncooperative children. ASDC Journal of Dentistry for children, 60 (45); 2959, 1993. Shane SA, Fuchs SM, Khine. Efficacy of rectal midazolam for the sedation of prescholl children undergoing laceration repair. Annals of Emergency Medicine, 24 (6); 106573, 1994. 11. Beebe DS, Belani KG, Chang RN. Effectiveness of preperative sedation with rectal midazolam, ketamine or their combinatin in young children. Anesth. Analg., 75 (6); 8804, 1992. Piotrowski R, Petrow N. Anaesthesia induction in children: propofol in comparison ith thiopental following premedication with midazolam. Anaesthetist, 39 (8); 398405, 1990. Gray HT. A study of spinal anesthesia in infants and children. Lancet, 3; 913, 1909. Abajian C, Paul Mellish RW, Browne AF. Spinal anesthesia for surgery in the highrisk infant. Anesth. Analg., 63; 35962, 1984. Broadman LM. Reigonal anaesthesia in paediatric practice. Can. J. Anaesth., 34; S 43, 1987. Collins VJ. Principles of anesthesiology, Vol 2, Lea Pebiger Philedelphia, 3rd Edition 1993, p 1535.
2.
12.
3.
13.
9.
4.
14.
15. 10.
5.
16.
6.
470
You might also like
- Richard M. Rosenfeld, Charles D. Bluestone - Evidence-Based Otitis Media (2003, PMPH-USA)Document546 pagesRichard M. Rosenfeld, Charles D. Bluestone - Evidence-Based Otitis Media (2003, PMPH-USA)Carmen-BadeaNo ratings yet
- IDSP P&L FormsDocument2 pagesIDSP P&L FormsKunal YadavNo ratings yet
- Research Paper: Alzheimer's DiseaseDocument13 pagesResearch Paper: Alzheimer's DiseaseABC Four CornersNo ratings yet
- Jurnal AnestesiDocument8 pagesJurnal AnestesiapriiiiiiilllNo ratings yet
- Comparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphineDocument7 pagesComparison of Preventive Analgesia Techniques in Circumcision Cases Dorsal Penile Nerve Block, Caudal Block, or Subcutaneous MorphinenatamkpNo ratings yet
- Baby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn InfantsDocument6 pagesBaby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn Infantsgladeva yugi antariNo ratings yet
- Comparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDocument8 pagesComparison of Ketamine-Midazolam-Propofol Combination and Fentanyl-Midazolam-Propofol Combination For Sedation in ColonosDendy AgusNo ratings yet
- BjorlDocument6 pagesBjorlaaNo ratings yet
- Dr. - Nataraj - EJCM 132 1888 1893 2023Document7 pagesDr. - Nataraj - EJCM 132 1888 1893 2023vithz kNo ratings yet
- Ojog20120300033 78059405 PDFDocument5 pagesOjog20120300033 78059405 PDFPalwasha MalikNo ratings yet
- Midazolam Prevent AgitationDocument13 pagesMidazolam Prevent AgitationUzZySusFabregasNo ratings yet
- Comparison of Caudal Morphine and Tramadol For Postoperative Pain Control in Children Undergoing Inguinal HerniorrhaphyDocument6 pagesComparison of Caudal Morphine and Tramadol For Postoperative Pain Control in Children Undergoing Inguinal Herniorrhaphymanoj9980No ratings yet
- 1 s2.0 S0007091217366175 MainDocument5 pages1 s2.0 S0007091217366175 MainMeutia LaksaniNo ratings yet
- Heel Stick ThailandDocument9 pagesHeel Stick ThailandStaporn KasemsripitakNo ratings yet
- 334 EnglishDocument7 pages334 EnglishkhalidNo ratings yet
- Articulo 2Document7 pagesArticulo 2Christian Yzaguirre AbantoNo ratings yet
- Penggunaan Sedasi Pada Anak Dengan VentilatorDocument5 pagesPenggunaan Sedasi Pada Anak Dengan VentilatorCalvin AffendyNo ratings yet
- A Comparison of Three Induction Agents in Paediatric Anaesthesia-Cardiovascular Effects and RecoveryDocument11 pagesA Comparison of Three Induction Agents in Paediatric Anaesthesia-Cardiovascular Effects and RecoveryAlibai Guiapal SalakobNo ratings yet
- CA Novi AnestesiDocument7 pagesCA Novi AnestesiearlynkNo ratings yet
- Anaesthetic Consideration For Neonatal Surgical Emergencies: Review ArticleDocument7 pagesAnaesthetic Consideration For Neonatal Surgical Emergencies: Review ArticleArun JoseNo ratings yet
- Wa0001Document10 pagesWa0001rini sundariNo ratings yet
- Successful Implementation of A Pediatric Sedation Protocol For Mechanically Ventilated PatientsDocument6 pagesSuccessful Implementation of A Pediatric Sedation Protocol For Mechanically Ventilated PatientsSantosa TandiNo ratings yet
- The Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUDocument11 pagesThe Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comparison Between Epidural and IV Tramadol For Painless Labor and Effect On Perinatal OutcomeDocument10 pagesA Comparison Between Epidural and IV Tramadol For Painless Labor and Effect On Perinatal OutcomeLibay Villamor IsmaelNo ratings yet
- Prevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus KetamineDocument17 pagesPrevention of Shivering During Regional Anaesthesia - Comparison of Midazolam, Midazolam Plus Ketamine, Tramadol, and Tramadol Plus Ketamineandi ananNo ratings yet
- Research ArticleDocument7 pagesResearch Articlenaljnaby9No ratings yet
- Anaesthetic Consideration For Neonatal Surgical emDocument7 pagesAnaesthetic Consideration For Neonatal Surgical emLong LongNo ratings yet
- Complementary Therapies in Medicine: SciencedirectDocument6 pagesComplementary Therapies in Medicine: SciencedirectSurya Puji KusumaNo ratings yet
- A Follow-Up KAISA 2013Document6 pagesA Follow-Up KAISA 2013Daniela LucenaNo ratings yet
- Journal 3Document9 pagesJournal 3Suryanti SultanNo ratings yet
- Musa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim NasseriDocument6 pagesMusa Shirmohammadie, Alireza Ebrahim Soltani, Shahriar Arbabi, Karim Nasseridebby claudiNo ratings yet
- Handling ComparingDocument13 pagesHandling ComparingNunik KhoirunnisaNo ratings yet
- Tramadol en NiñosDocument5 pagesTramadol en NiñosElias Vera RojasNo ratings yet
- Anesthetic Management of A Newborn With A Cervical Meningomyelocele S. P, A. U, S M J M. RDocument4 pagesAnesthetic Management of A Newborn With A Cervical Meningomyelocele S. P, A. U, S M J M. RAnis Eka SukmadadariNo ratings yet
- 0256-4947 2015 58 PDFDocument7 pages0256-4947 2015 58 PDFUlfani DewiNo ratings yet
- Addition of Low-Dose Ketamine To Midazolam-fentanyl-propofol-Based Sedation For Colonoscopy A Randomized, Double-Blind, Controlled TrialDocument6 pagesAddition of Low-Dose Ketamine To Midazolam-fentanyl-propofol-Based Sedation For Colonoscopy A Randomized, Double-Blind, Controlled TrialRoderick Samuel PrenticeNo ratings yet
- 0 Aet484Document7 pages0 Aet484UsbahNo ratings yet
- The Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenDocument7 pagesThe Prophylactic Effect of Rectal Diclofenac Versus Intravenous Pethidine On Postoperative Pain After Tonsillectomy in ChildrenNi Komang Suryani DewiNo ratings yet
- DR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaDocument9 pagesDR T. Suryasree, DR K. Indira Priya Darshini, DR PratikshaIOSRjournalNo ratings yet
- Paracetamol vs. Dexketoprofen PDFDocument5 pagesParacetamol vs. Dexketoprofen PDFMikeNo ratings yet
- 1 ChestDocument5 pages1 ChestZakiyah Nur HaqqiNo ratings yet
- Ect in PregncyDocument13 pagesEct in PregncySasi KumarNo ratings yet
- Pediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineDocument7 pagesPediatric Premedication: A Double-Blind Randomized Trial of Dexmedetomidine or Ketamine Alone Versus A Combination of Dexmedetomidine and KetamineFatty MaulidiraNo ratings yet
- Annex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)Document7 pagesAnnex 8a Translation Le Tohic-Venous Insufficiency 2008 (Pasien Hamil)KHAIRULNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument6 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- The Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFDocument6 pagesThe Analgesic Efficacy of Tramadol As A Pre-Emptive Analgesic in Pediatric Appendectomy Patients PDFUmmu Qonitah AfnidawatiNo ratings yet
- 100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Document11 pages100 Case Studies in Pathophysiology-532hlm (Warna Hanya Cover)Haymanot AnimutNo ratings yet
- Ondan Hipo 2Document6 pagesOndan Hipo 2putri maharani andesNo ratings yet
- Cag La Oz Bak Isak Kurt 2009Document7 pagesCag La Oz Bak Isak Kurt 2009Arturo AlcantaraNo ratings yet
- Pediatrics DNB Q & ADocument132 pagesPediatrics DNB Q & Ahiwotbetesfa2123No ratings yet
- Pain MX 2nd Stage of Labour NoDocument19 pagesPain MX 2nd Stage of Labour NoMd NohNo ratings yet
- Paediatric Sedation: Michael R. J. Sury FRCADocument5 pagesPaediatric Sedation: Michael R. J. Sury FRCAZazzZaffaNo ratings yet
- Jtgga 4 2 110 165Document56 pagesJtgga 4 2 110 165drklftNo ratings yet
- Evaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryDocument8 pagesEvaluation of Sodium Nitroprusside For Controlled Hypotension in Children During SurgeryAudra Firthi Dea NoorafiattyNo ratings yet
- Pain Relief During Labor and Delivery: A Brief 2013 UpdateDocument5 pagesPain Relief During Labor and Delivery: A Brief 2013 UpdateJheiczhietoot KibasNo ratings yet
- Paediatric Anaesthesia PDFDocument33 pagesPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriNo ratings yet
- Advantages of Tonsillectomy Done Under Local Word PDFDocument6 pagesAdvantages of Tonsillectomy Done Under Local Word PDFAgus KarsetiyonoNo ratings yet
- AnesthEssaysRes83324-3429942 093139Document6 pagesAnesthEssaysRes83324-3429942 093139burhanNo ratings yet
- 343-Article Text-653-1-10-20190607Document5 pages343-Article Text-653-1-10-20190607Zulkifli FachriyanNo ratings yet
- Preoperative Stabilisation in Congenital Diaphragmatic HerniaDocument3 pagesPreoperative Stabilisation in Congenital Diaphragmatic HerniaAgus PrimaNo ratings yet
- Rocuronium Versus Succinylcholine Are They.9Document4 pagesRocuronium Versus Succinylcholine Are They.9Kian PrakashNo ratings yet
- Pediatric Regional AnesthesiaDocument6 pagesPediatric Regional Anesthesiatq9prx5s5qNo ratings yet
- Uterus TransplantationFrom EverandUterus TransplantationMats BrännströmNo ratings yet
- Drugs For SNCUDocument2 pagesDrugs For SNCUKunal YadavNo ratings yet
- Strategic Alliances The Role of Civil Society in HealthDocument12 pagesStrategic Alliances The Role of Civil Society in HealthKunal YadavNo ratings yet
- Nutritional Rehabilitation CenterDocument12 pagesNutritional Rehabilitation CenterKunal Yadav0% (1)
- July, 2023 Nursing and Training Report.Document20 pagesJuly, 2023 Nursing and Training Report.Tosi AboloNo ratings yet
- Msds Hi PozzDocument6 pagesMsds Hi Pozzpenis1493No ratings yet
- Annotated BibliographyDocument8 pagesAnnotated Bibliographyapi-538355468No ratings yet
- Ssi Rabu, 29 Juni 2022Document49 pagesSsi Rabu, 29 Juni 2022Dhamar SetiaNo ratings yet
- Statewise HospitalsDocument426 pagesStatewise HospitalsdevNo ratings yet
- PharmacokineticsDocument10 pagesPharmacokineticsbrian3442No ratings yet
- Ferenczi - Confusion of The TonguesDocument5 pagesFerenczi - Confusion of The TonguessticataNo ratings yet
- ChokingDocument2 pagesChokingdrfidelenriqueNo ratings yet
- Common Breast DiseasesDocument64 pagesCommon Breast Diseasesamirahmei100% (1)
- Railway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Document8 pagesRailway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Latest Laws TeamNo ratings yet
- Nonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharDocument97 pagesNonsteroidal Anti-Inflammatory Drugs: DR Tarek M Nasrallah Al - AzharTarek NasrallahNo ratings yet
- OG Informing Abortion Debate DR Christine BaileyDocument2 pagesOG Informing Abortion Debate DR Christine BaileyYwagar YwagarNo ratings yet
- Nursing Care in ECTDocument3 pagesNursing Care in ECTRawan KhateebNo ratings yet
- 4 Relining TechniquesDocument9 pages4 Relining TechniquesvinnycoolbuddyNo ratings yet
- Occupational English Test: Writing Subtest: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Subtest: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesHarold MedranoNo ratings yet
- Case Analysis: American WellDocument2 pagesCase Analysis: American WellTatsat PandeyNo ratings yet
- Curriculum Vitae Mladen Boban, M.D., Ph.D. Personal InformationDocument2 pagesCurriculum Vitae Mladen Boban, M.D., Ph.D. Personal InformationGoran MaliNo ratings yet
- Common Errors in Xray Interpretation 2Document49 pagesCommon Errors in Xray Interpretation 2Shri RamaNo ratings yet
- Leukorrhea Panel PDFDocument8 pagesLeukorrhea Panel PDFahmadNo ratings yet
- Review Factors Contributing To Medication Errors: A Literature ReviewDocument9 pagesReview Factors Contributing To Medication Errors: A Literature Reviewsoul_0602No ratings yet
- FTC Vs HCG Diet Direct, Clint EthingtonDocument40 pagesFTC Vs HCG Diet Direct, Clint Ethingtontheskeptic21No ratings yet
- Removable Partial Denture Framework Try-InDocument13 pagesRemovable Partial Denture Framework Try-InAnye PutriNo ratings yet
- Oral Systemic ConnectionDocument37 pagesOral Systemic Connectionchrisdina puspita sari100% (1)
- Hon 2005Document5 pagesHon 2005lenirizkiNo ratings yet
- Bum Run GradDocument10 pagesBum Run GradsabyasachiNo ratings yet
- Investigatory Project On Malaria: Name: M.Bhavya Class: XI C' Year: 2018 - 2019Document18 pagesInvestigatory Project On Malaria: Name: M.Bhavya Class: XI C' Year: 2018 - 2019Muramsetty Bhavya0% (1)
- All About Nails - CosmetologyDocument6 pagesAll About Nails - CosmetologySheryline BonillaNo ratings yet
- PSGDocument57 pagesPSGsg1964No ratings yet