Professional Documents
Culture Documents
Blockxiv Neoplasms Lymphoid 2006
Blockxiv Neoplasms Lymphoid 2006
Uploaded by
Ryo RyozCopyright:
Available Formats
You might also like
- PATHO LEC WBC Lymph Nodes Spleen Thymus Part1 CompressedDocument84 pagesPATHO LEC WBC Lymph Nodes Spleen Thymus Part1 CompressedAngelo HinonNo ratings yet
- WBC BasicsDocument70 pagesWBC BasicsZoe ZillaNo ratings yet
- MicrobiologyDocument52 pagesMicrobiologyhema100% (1)
- Medical Biotechnology - Bernard R. Glick Et Al. (American Society For Microbiology, 2014) PDFDocument758 pagesMedical Biotechnology - Bernard R. Glick Et Al. (American Society For Microbiology, 2014) PDFFriendlyGoodGirl100% (1)
- Lymphoid NeoplasmsDocument52 pagesLymphoid NeoplasmsAmalia Riska GNo ratings yet
- 4b TUMOR JAR RetikuloendotelialAAADocument98 pages4b TUMOR JAR RetikuloendotelialAAARyo RyozNo ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- Week 15-Mature-Lymphoid-Neoplasms-SCDocument65 pagesWeek 15-Mature-Lymphoid-Neoplasms-SCKyle CollladoNo ratings yet
- Lymphoma: Pro - Dr.Ahmed EisaDocument45 pagesLymphoma: Pro - Dr.Ahmed EisaOmar Mohammed100% (1)
- Diseases and Tumors of Lymphoid SystemDocument97 pagesDiseases and Tumors of Lymphoid SystemamyNo ratings yet
- Pathology of NHL, Part 1 For 2nd Year Medical StudentDocument28 pagesPathology of NHL, Part 1 For 2nd Year Medical Studentmina mounirNo ratings yet
- Lymphoreticular FinalDocument42 pagesLymphoreticular FinalNafis Fuad SheikhNo ratings yet
- Lymphoma (Ean's) - 2Document29 pagesLymphoma (Ean's) - 2eanfital11No ratings yet
- LHYMPHOMADocument24 pagesLHYMPHOMACryptic LadyNo ratings yet
- Hodgkein and Nonhodgkein LymphomaDocument57 pagesHodgkein and Nonhodgkein Lymphomasamar yousif mohamedNo ratings yet
- Pathology of NHL, Part 2 For 2nd Year Medical StudentDocument19 pagesPathology of NHL, Part 2 For 2nd Year Medical Studentmina mounirNo ratings yet
- Non - Hodgkin LymphomaDocument25 pagesNon - Hodgkin LymphomaRo RyNo ratings yet
- Non Hodgkin Lymphoma by Dr. AnumDocument43 pagesNon Hodgkin Lymphoma by Dr. AnumHumar HaiderNo ratings yet
- LymphomaDocument53 pagesLymphomaRobert ChristevenNo ratings yet
- Malignant Lymphomas: DR Nilukshi PereraDocument48 pagesMalignant Lymphomas: DR Nilukshi PereraThaveeshaLindsayWhiteNo ratings yet
- LymphomaDocument69 pagesLymphomaDawit g/kidanNo ratings yet
- Opeyemi IdaeworDocument66 pagesOpeyemi IdaeworOpeyemi IdaeworNo ratings yet
- Ashok NHLDocument112 pagesAshok NHLDr MurariNo ratings yet
- Advances in Management of NHLDocument34 pagesAdvances in Management of NHLMohammed Abd ElfattahNo ratings yet
- Non-Hodgkins Lymphoma (Report)Document50 pagesNon-Hodgkins Lymphoma (Report)Dayledaniel SorvetoNo ratings yet
- 11 Hematological MalignanciesDocument34 pages11 Hematological MalignanciesalitahawarbarintNo ratings yet
- Lymphoid NeoplasmsDocument39 pagesLymphoid NeoplasmsMoshe GiftNo ratings yet
- Lymphomas: Dr. Y.A. AdelabuDocument28 pagesLymphomas: Dr. Y.A. Adelabuadamu mohammadNo ratings yet
- NHL Nandu CopasDocument95 pagesNHL Nandu CopaswihelminaNo ratings yet
- LNs HNDocument190 pagesLNs HNNinna Isabel VictorioNo ratings yet
- C6.1clasificare LimfoameDocument10 pagesC6.1clasificare LimfoameRădulescu AndreeaNo ratings yet
- Overview of LymphomasDocument44 pagesOverview of LymphomasHarsha MaheshwariNo ratings yet
- Lymph Node CytologyDocument39 pagesLymph Node Cytologykamranghani641No ratings yet
- Non-Hodgkins LymphomaDocument22 pagesNon-Hodgkins LymphomaNyoman TapayanaNo ratings yet
- Limfoma (Kuliah 3a Ipd III)Document30 pagesLimfoma (Kuliah 3a Ipd III)Rianda Dwi PutraNo ratings yet
- NHL Arshad KhanDocument30 pagesNHL Arshad KhanArshad khanNo ratings yet
- Medicine Seminar Combined-1Document30 pagesMedicine Seminar Combined-1Deepanshu KumarNo ratings yet
- Haematology LeukaemiaDocument28 pagesHaematology LeukaemiaFrolian MichaelNo ratings yet
- Overview of LymphomaDocument42 pagesOverview of Lymphomaadamu mohammadNo ratings yet
- Non-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!Document48 pagesNon-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!francis00090No ratings yet
- Pathology of Lymph Nodes: Norman Levy, MDDocument92 pagesPathology of Lymph Nodes: Norman Levy, MDAdi ParamarthaNo ratings yet
- Non Hodgkin's LymphomaDocument31 pagesNon Hodgkin's LymphomaJeo Thomas100% (1)
- 3 Final Lymphoma and MyelomaDocument16 pages3 Final Lymphoma and MyelomaRumela Chakraborty100% (1)
- Acute Leukemia: Thirunavukkarasu MurugappanDocument22 pagesAcute Leukemia: Thirunavukkarasu MurugappanFelix Allen100% (1)
- Non-Hodgkin's LymphomasDocument23 pagesNon-Hodgkin's LymphomasshevmyrNo ratings yet
- Lymphoid Lekemia: DR Budi Enoch SPPDDocument32 pagesLymphoid Lekemia: DR Budi Enoch SPPDLia pramitaNo ratings yet
- Bethy Suryawathy, Dr.,Sppa.,Phd. Bagian Patologi Anatomi Fakultas Kedokteran UnpadDocument31 pagesBethy Suryawathy, Dr.,Sppa.,Phd. Bagian Patologi Anatomi Fakultas Kedokteran UnpadDhika ArdiansyahNo ratings yet
- LymphomaDocument20 pagesLymphomaChairul Adilla Ardy100% (1)
- DR Opeyemi IdaeworDocument69 pagesDR Opeyemi IdaeworOpeyemi IdaeworNo ratings yet
- WBC DisordersDocument45 pagesWBC DisordersyalahopaNo ratings yet
- 2 - Lymphoma Lecture by Dr. M T - PresentationDocument40 pages2 - Lymphoma Lecture by Dr. M T - Presentationsohilaw210No ratings yet
- A7Document4 pagesA7Saman SadeghiNo ratings yet
- 牙三實驗 HematopathologyDocument57 pages牙三實驗 Hematopathology6zpv64hbthNo ratings yet
- Lymphoma: David Lee MD, FRCPCDocument36 pagesLymphoma: David Lee MD, FRCPCQasim AliNo ratings yet
- Hodgkin'S Disease AND Non-Hodgkin'S LymphomaDocument42 pagesHodgkin'S Disease AND Non-Hodgkin'S LymphomaRayya TriandaNo ratings yet
- NHL 1Document13 pagesNHL 1kushalNo ratings yet
- Hodgkin-Lymphoma. Plasma Cell NeoplasiasDocument2 pagesHodgkin-Lymphoma. Plasma Cell NeoplasiasSaman SadeghiNo ratings yet
- Genevieve Crane - Approach To Lymph Node-Path Cast Lymph Node Pathology Eve CraneDocument75 pagesGenevieve Crane - Approach To Lymph Node-Path Cast Lymph Node Pathology Eve CraneJose SirittNo ratings yet
- Hodgkin's Lymphoma (Patho Lec 2)Document37 pagesHodgkin's Lymphoma (Patho Lec 2)mina mounirNo ratings yet
- Hodgkin's DiseaseDocument58 pagesHodgkin's Diseasealibayaty1No ratings yet
- 1 - Lymphomas - Gelinde NarekineDocument64 pages1 - Lymphomas - Gelinde NarekineAntna SinekNo ratings yet
- NHLDocument35 pagesNHLnn zelaNo ratings yet
- Chronic Lymphocytic LeukemiaFrom EverandChronic Lymphocytic LeukemiaMichael HallekNo ratings yet
- InflamasiDocument63 pagesInflamasiRyo RyozNo ratings yet
- 4b TUMOR JAR RetikuloendotelialAAADocument98 pages4b TUMOR JAR RetikuloendotelialAAARyo RyozNo ratings yet
- InflamasiDocument63 pagesInflamasiRyo RyozNo ratings yet
- 7 Tumor KulitDocument102 pages7 Tumor KulitRyo RyozNo ratings yet
- Jurnal Tatalaksana KAD Pada AnakDocument18 pagesJurnal Tatalaksana KAD Pada AnakAfkaraHusnaFirdanisaNo ratings yet
- Using Insulin: What Is Insulin? Types of InsulinDocument4 pagesUsing Insulin: What Is Insulin? Types of InsulinRyo RyozNo ratings yet
- Anti-Stress Cem - Tech by MichaelDocument30 pagesAnti-Stress Cem - Tech by MichaelTulhina AndreiNo ratings yet
- Pathogenesis of Graft-Versus-Host Disease (GVHD) - UpToDateDocument12 pagesPathogenesis of Graft-Versus-Host Disease (GVHD) - UpToDatemihaela popescuNo ratings yet
- Vetscan ObjectivesDocument395 pagesVetscan ObjectivesDeep PatelNo ratings yet
- ImmunoSero Immunology Overview NotesDocument4 pagesImmunoSero Immunology Overview NotesAndrienne Valen de BelenNo ratings yet
- Acquired ImmunityDocument16 pagesAcquired ImmunityMohammed Hashem100% (1)
- Immunology Overview: Armond S. Goldman Bellur S. PrabhakarDocument45 pagesImmunology Overview: Armond S. Goldman Bellur S. PrabhakarIoana AsziaNo ratings yet
- Human Health and Disease-1Document12 pagesHuman Health and Disease-1Ananya MoniNo ratings yet
- Stevens (Science) Med TechDocument31 pagesStevens (Science) Med TechnotsoninjaninjaNo ratings yet
- Parasitic Infections: Pathogenesis and Immunity: J. StewartDocument7 pagesParasitic Infections: Pathogenesis and Immunity: J. Stewartnour achkarNo ratings yet
- General Biology 2 (4 Quarter) : Animal and Plant ReproductionDocument23 pagesGeneral Biology 2 (4 Quarter) : Animal and Plant Reproductionamethyst grande100% (1)
- Lymphatic CaseDocument6 pagesLymphatic CaseGlenn Arjay BataraoNo ratings yet
- Cancer Immune TherapyDocument452 pagesCancer Immune TherapyatyNo ratings yet
- Immunity All NotesDocument112 pagesImmunity All NotesJonathan Carlisle CheungNo ratings yet
- Immuno Modulator yDocument377 pagesImmuno Modulator ysaman7752No ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- Leukemia Infographic PDFDocument1 pageLeukemia Infographic PDFPriyanka KhuranaNo ratings yet
- Part C-35 MCQS/ 7 PP: MCQ PaediatricsDocument6 pagesPart C-35 MCQS/ 7 PP: MCQ Paediatricswindows3123100% (1)
- Immuno and InfectiousDocument17 pagesImmuno and Infectiousgreen_archerNo ratings yet
- Metapopulation ModellingDocument25 pagesMetapopulation Modellingjolamo1122916No ratings yet
- Study Guide: Cytokines Associated With Innate ImmunityDocument12 pagesStudy Guide: Cytokines Associated With Innate ImmunityxxxxxxxNo ratings yet
- Acute Lymphocytic Leukaemia Diagnosis and Treatment A Review PDFDocument7 pagesAcute Lymphocytic Leukaemia Diagnosis and Treatment A Review PDFJunita Nelly Esther JosephNo ratings yet
- Incorrectly: CorrectlyDocument25 pagesIncorrectly: CorrectlypikachuNo ratings yet
- Lymph Drainage Therapy PDFDocument7 pagesLymph Drainage Therapy PDFDiego Mamani Mullisaca100% (2)
- (Advances in Space Biology and Medicine 6) Sjoerd L. Bonting (Eds.) - Elsevier Science (1997)Document318 pages(Advances in Space Biology and Medicine 6) Sjoerd L. Bonting (Eds.) - Elsevier Science (1997)Sohnit KumarNo ratings yet
- Perfect Score Module 2017 Form 5 Answer SchemeDocument24 pagesPerfect Score Module 2017 Form 5 Answer SchemeChen ShyanNo ratings yet
- Hematological Anatomy, Physiology and Assessment: This Course Has Been Awarded One (1.0) Contact Hour. July 30, 2019Document19 pagesHematological Anatomy, Physiology and Assessment: This Course Has Been Awarded One (1.0) Contact Hour. July 30, 2019Mill Jan CruzNo ratings yet
- Basic ImmunologyDocument29 pagesBasic ImmunologyHema Duddukuri0% (1)
Blockxiv Neoplasms Lymphoid 2006
Blockxiv Neoplasms Lymphoid 2006
Uploaded by
Ryo RyozOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blockxiv Neoplasms Lymphoid 2006
Blockxiv Neoplasms Lymphoid 2006
Uploaded by
Ryo RyozCopyright:
Available Formats
neoplasms of the
Lymphoid System
T. Utoro
Department of Pathology GMUSM
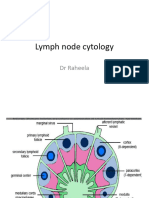
Structure of Normal Lymphnode
Lymphoid Neoplasms
Certain relevant principles must be
emphasized
Can be suspected from the clinical features, but
histological examination of lymph nodes and
other involved tissue is required for diagnosis
The vast majority of lymphoid neoplasm (80% -
85%) are of B-cell origin; most of the remainder
being T-cell tumors; only rarely are tumors of NK
origin encountered
Two basic forms of B-cell lymphoma: follicular &
diffuse type
Lymphoid Neoplasms
close to immune regulatory system
Lymphoid neoplasm are tumors of the immune
system disrupt normal immune regulatory
mechanisms (evidences: susceptibility to
infection, autoimmune diseases)
Patients with inherited or acquired immunodefi-
ciency are at high risk of developing certain
lymphoid neoplasm, particularly these associated
with EBV infection
Lymphoid Neoplasms
All lymphoid neoplasms are derived from single
transformed cell monoclonal
Divided into 2 big groups: NHLs and HLs
NHLs often present as involvement of a particular tissue
site, but sensitive molecular assay usually show that the
tumor is widely disseminated at the time of diagnosis
only systemic therapy are curative
HLs are often presents at a single site spreads
methodically to contiguous lymph nodes group early
course tumors may be cured with local therapy alone
Lymphoid Neoplasms
HL spreads in orderly fashion, and as a result
staging is of importance in determining therapy
In contrast, the spread of NHL is less predictable
most patients are assumed to have systemic
disease at the time of diagnosis staging in
particular NHL provides useful prognosis
information, but generally not important in guiding
therapy
E T I O L O G Y
Chromosomal translocation: CML, Burkitt lymphoma
Inherited genetic factors: Bloom syndrome, Fanconi
anemia, ataxia telangiectasia, Down syndrome
Viruses: HTLV-1, EBV, KSHV, HHV-8
Environmental agents: Helicobacter pylorii (gastric B-cell
lymphoma), gluten-sensitive enteropathy (T-cell lymphoma),
HIV (B-cell lymphoma)
Iatrogenic factors: radiotherapy & chemotherapy
mutagenic effect
The WHO Classification of the
Lymphoid Neoplasms
I. Precursor B-cell Neoplasms: neoplasms of
immature B-cells
II. Peripheral B-cell Neoplasms: neoplasms of
mature B-cells
III. Precursor T-cell Neoplasms: neoplasms of
immature T-cells
IV. Peripheral T-cell and NK-cell Neoplasms:
neoplasms of mature T-cell and NK-cell
V. Hodgkin Lymphoma: neoplasms of Reed-
Sternberg cells and variants
Origin of Lymphoid Neoplasms
CLP: common lymphoid precursor; BLB: pre-B lymphoblast;
NBC: naive B-cell; MC: mantle B-cell; GC: germinal center B-cell;
MZ: marginal zone B-cell; DN: CD4/CD8 double negative pre-T cell;
DP: CD4/CD8 double positive pre-T cell; PTC: peripheral T-cell
The WHO Classification of the Lymphoid Neoplasms
I. Precursor B-cell Neoplasms
ALL
The WHO Classification of the Lymphoid Neoplasms
III. Precursor T-cell Neoplasms
Acute lymphoblastic leukemia / lymphoma
-Originate from B-cell or T-cell, mostly from T-cell
-Can be differed by B-cell marker CD22
-The nuclear chromatin is delicate and finely stippled,
and nucleoli are either absent or inconspicuous
The WHO Classification of the Lymphoid Neoplasms
II. Peripheral B-cell Neoplasms
CLL / small lymphocytic lymphoma
B-cell prolymphocytic leukemia
Lymphoplasmacytic lymphoma
Splenic and nodal marginal zone lymphoma
Extranodal marginal zone lymphoma
Mantel cell lymphoma
Follicular lymphoma
Marginal zone lymphoma
Hairy cell leukemia
Plasmacytoma / plasma cell myeloma
Diffuse large B-cell lymphoma
Burkitt lymphoma
II. Peripheral B-cell Neoplasms
Small Lymphocytic Leukemia
Small Lymphocytic Lymphoma
The two indistinguishable disorders: morphologically,
phenotypically, and genotypically; differing only in the
degree of peripheral blood lymphocytosis
Proliferation center: loose aggregates of pro-lymphocyte
pathognomonic
Tumor cells usually infiltrate the splenic white and red
pulp, and the hepatic portal tract, although the extent of
involvement varies widely.
II. Peripheral B-cell Neoplasms
Small Lymphocytic Leukemia
Small Lymphocytic Lymphoma
Diffuse effacement of nodal architecture
The majority of the tumor cells are
small round lymphocytes.
Arrow: pro-lymphocyte
II. Peripheral B-cell Neoplasms
Follicular Lymphoma
The most common form of NHL in the USA
(45% of adult lymphomas)
Usually present in the middle age and afflicts
males and females equally
Less common in Europe, and rare in Asian
population
The tumor cells closely resemble normal
germinal center B-cells
II. Peripheral B-cell Neoplasms
Follicular Lymphoma
In most cases, at low magnification, a predominantly
nodular or nodular and diffuse growth pattern is
observed
Two principle cells are observed in varying proportion:
(1) small cell with irregular or cleaved nuclear contour
and scant cytoplasm centrocyte
(2) larger cells with open nuclear chromatin, several
nucleoli, and modest amount of cytoplasm centroblast
Involvement: bone marrow (85%), spleen, liver
Te overall median survival is 7 to 9 years, is not
improved by aggressive therapy
Follicular Lymphoma (spleen)
Prominent nodules represent white pulp follicles expanded by
follicular lymphoma cells
Follicular Lymphoma
Malignant lymph follicles are marked by Bcl-2 positive
Follicular Lymphoma
Small lymphoid cells with condensed chromatin and irregular or
cleaved nuclear outline (centrocyte), mixed with a population of
larger cells with nucleoli (centroblast)
Mantle cell lymphoma
Neoplastic lymphoid cells surround a small, atrophic
germinal center exhibiting mantle zone pattern of growth
Homogenous population of small lymphoid cells with somewhat irregular
nuclear outlines, condensed chromatin, and scant cytoplasm.
II. Peripheral B-cell Neoplasms
Diffuse large B-cell lymphoma
(DLBCL)
Slight male predominance
Age about 60 years
5% of childhood lymphoma
Clinically present with a rapidly enlarging,
often symptomatic mass, at a single nodal
or extranodal site
Diffuse large B-cell lymphoma
Spleen: typical isolated large mass
Diffuse large B-cell Lymphoma
Tumor cells show prominent nucleoli
Diffuse large B-cell lymphoma
Tumor cells with large nuclei, open chromatin,
and prominent nucleoli
II. Peripheral B-cell Neoplasms
Burkitt lymphoma
Categories: (1) African (endemic) Burkitt lymphoma,
(2) sporadic (non-endemic), (3) a subset of aggressive
lymphoma occuring in individual with HIV infection
Responds well to short-term, high dose chemotherapy
(children & young adults)
Clinical feature
Both endemic & non-endemic are found largely in
children and young adults (30%)
Most tumor manifests at extra-nodal sites
Burkitt lymphoma
Low power: many tingible body
macrophages Starry sky appearance
Monotonous appearance, tumor cells
with multiple small nucleoli and high
mitotic index (typical)
Burkitt Lymphoma
Several starry sky macrophages was shown (arrows)
II. Peripheral B-cell Neoplasms
Multiple myeloma of the skull
The sharply punched-out bone lesions are
most obvious in the calvarium
Multiple myeloma (bone aspirate)
Normal marrow cells are replaced by plasma cells
Lymphoplasmacytic lymphoma
Bone marrow biopsy:
various degrees of plasma cell differentiation
Mast cell
The WHO Classification of the Lymphoid Neoplasms
IV. Peripheral T&NK-cell Neoplasms
T-cell prolymhocytic leukemia
Large granular lymhocytic leukemia
Mycosis fungoides / Sezary syndrome
Peripheral T-cell lymphoma, unspecified
Anaplastic large cell lymphoma
Angioimmunoblastic T-cell lymphoma
Enteropathy-associated T-cell lymphoma
Panniculitis-like T-cell lymphoma
Hepatosplenic T-cell lymphoma
Adult T-cell leukemia/Lymphoma
NK/T-cell lymphoma, nasal type
NK-cell leukemia
Peripheral T&NK-cell Lymphoma
Peripheral T-cell lymphoma
T-cell lymphoma without specific defining features fall
collectively into the category of unspecified
Account for approximately half of all T-cell lymphoma in
the western world
As a group they are aggressive malignant with low 5-yrs
They may be nodal or extra nodal
Variable expression most nodal expressing CD4+
They may be associated with eosinophilia
Peripheral T&NK-cell Lymphoma
Peripheral T-cell lymphoma
A spectrum of small, intermediate, and large lymphoid cells,
many with irregular nuclear contours.
Peripheral T&NK-cell Lymphoma
Anaplastic large cell lymphoma
mitosis
Anaplastic large cell lymphoma
Hallmark cells with horseshoe-like or embryo like nuclei
and abundant cytoplasma lie near the center of the field.
IHC: ALK protein
The WHO Classification of the Lymphoid Neoplasms
V. Hodgkin Lymphoma
Classical subtype
Nodular sclerosis
Mixed cellularity
Lymphocyte-rich
Lymphocyte depletion
Lymphocyte pre-dominance
V. Hodgkin
Lymphoma
Lymphocyte predo-
minant.
Mixed cellularity
Lymphocyte rich
Lymphocyte depleted
Nodular sclerosis
V. Hodgkin Lymphoma
Reed-Sternberg cell, positive for CD30
V. Hodgkin Lymphoma
Reed-Sternberg cell
Mirror-image nuclei contain large eosinophilic nucleoli
Reed-Sternberg cells and variants
A. Diagnostic RS-cells with 2 nuclear lobes, large inclusion-
like nucleoli, and abundant cytoplasm
B. Mononuclear variant.
C. Lacunar variant, characteristic of the nodular sclerosis
subtype. It has a folded or multilobated nucleus lying
within a clear space created by disruption of its
cytoplasm during processing
D. Lymphohistiocytic (L&H) variant, complex nuclear
irregularities, small nucleoli, fine chromatin, and abundant
pale cytoplasm.
Hodgkin lymphoma
(Reed-Sternberg cells and variants)
A B
C D
Hodgkin lymphoma:
nodular sclerosis type
Well-defined bands of pink, acellular collagen that subdivided
the tumor cells and associated reactive infiltrate into nodules
Hodgkin lymphoma:
mixed cellularity type
Numerous mature-looking lymphocytes surround scattered,
large pale-staining L&H variants (popcorn cells)
Hodgkin lymphoma
lymphocytic predominance type
Reed-Sternberg cells is surrounded by reactive cells, including eosinophils
Ann Arbor Staging System
Stage I
A/B
a
I
IE
Involvement of a single lymph node region
or
A single extra lymphatic organ or site
Stage II
A/B
II
IIE
Involvement of 2 or more lymph node regions on the same
side of the diaphragm, or
With localized contiguous involvement of an extra
lymphatic organ or site
Stage III
A/B
III
IIIE
IIIS
IIIES
Involvement of lymph node regions of both sites of the
diaphragm
Or, with localized contiguous involvement of an extra
lymphatic organ or site, or
With involvement of spleen, or
both extra lymphatic organ or site and spleen involvement
Stage IV
A/B
IV Diffuse or disseminated involvement of one or more extra
lymphatic organs with or without associated lymph node
involvement
References
Rubins Pathology. Clinical Foundations of
Medicine, 2005. Emanuel Rubin cs; Lippincott
Williams & Wilkins.
Robbins Pathologic Bases of Medicine, 2005.
Cotran, Kumar, Collins. Saunders
Pathology, 2
nd
ed. 2002. Arthur S. Schneider,
Philip A. Szanto; Lippinctt Williams & Wilkins
Mycosis Fungoides
Mycosis
Fungoides
A mature T-cell lymphoma presenting
in the skin with patches/plaques, and
characterized by epidermal and
dermal infiltration of small to medium
T-cells with cerebriform nuclei.
Mycosis Fungoides
Plaques lesion with infiltrates of
atypical, cerebriform lymphocytes
in the upper dermis
The epidermis is involved, mainly with
single cells
Mycosis Fungoides
Neoplastic cells with cerebriform nuclei form Pautrier microabscess within epidermis.
Mycosis
Fungoides
Tumor lesion with more massive
infiltrates involving both the
upper and deep dermis
Mycosis Fungoides
B. In the epidermis Pautrier abscess can be seen. C. The neoplastic cells show an
aberrant phenotype with expression of CD3, but no reaction for either CD4 (D) or
CD8 (E)
You might also like
- PATHO LEC WBC Lymph Nodes Spleen Thymus Part1 CompressedDocument84 pagesPATHO LEC WBC Lymph Nodes Spleen Thymus Part1 CompressedAngelo HinonNo ratings yet
- WBC BasicsDocument70 pagesWBC BasicsZoe ZillaNo ratings yet
- MicrobiologyDocument52 pagesMicrobiologyhema100% (1)
- Medical Biotechnology - Bernard R. Glick Et Al. (American Society For Microbiology, 2014) PDFDocument758 pagesMedical Biotechnology - Bernard R. Glick Et Al. (American Society For Microbiology, 2014) PDFFriendlyGoodGirl100% (1)
- Lymphoid NeoplasmsDocument52 pagesLymphoid NeoplasmsAmalia Riska GNo ratings yet
- 4b TUMOR JAR RetikuloendotelialAAADocument98 pages4b TUMOR JAR RetikuloendotelialAAARyo RyozNo ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- Week 15-Mature-Lymphoid-Neoplasms-SCDocument65 pagesWeek 15-Mature-Lymphoid-Neoplasms-SCKyle CollladoNo ratings yet
- Lymphoma: Pro - Dr.Ahmed EisaDocument45 pagesLymphoma: Pro - Dr.Ahmed EisaOmar Mohammed100% (1)
- Diseases and Tumors of Lymphoid SystemDocument97 pagesDiseases and Tumors of Lymphoid SystemamyNo ratings yet
- Pathology of NHL, Part 1 For 2nd Year Medical StudentDocument28 pagesPathology of NHL, Part 1 For 2nd Year Medical Studentmina mounirNo ratings yet
- Lymphoreticular FinalDocument42 pagesLymphoreticular FinalNafis Fuad SheikhNo ratings yet
- Lymphoma (Ean's) - 2Document29 pagesLymphoma (Ean's) - 2eanfital11No ratings yet
- LHYMPHOMADocument24 pagesLHYMPHOMACryptic LadyNo ratings yet
- Hodgkein and Nonhodgkein LymphomaDocument57 pagesHodgkein and Nonhodgkein Lymphomasamar yousif mohamedNo ratings yet
- Pathology of NHL, Part 2 For 2nd Year Medical StudentDocument19 pagesPathology of NHL, Part 2 For 2nd Year Medical Studentmina mounirNo ratings yet
- Non - Hodgkin LymphomaDocument25 pagesNon - Hodgkin LymphomaRo RyNo ratings yet
- Non Hodgkin Lymphoma by Dr. AnumDocument43 pagesNon Hodgkin Lymphoma by Dr. AnumHumar HaiderNo ratings yet
- LymphomaDocument53 pagesLymphomaRobert ChristevenNo ratings yet
- Malignant Lymphomas: DR Nilukshi PereraDocument48 pagesMalignant Lymphomas: DR Nilukshi PereraThaveeshaLindsayWhiteNo ratings yet
- LymphomaDocument69 pagesLymphomaDawit g/kidanNo ratings yet
- Opeyemi IdaeworDocument66 pagesOpeyemi IdaeworOpeyemi IdaeworNo ratings yet
- Ashok NHLDocument112 pagesAshok NHLDr MurariNo ratings yet
- Advances in Management of NHLDocument34 pagesAdvances in Management of NHLMohammed Abd ElfattahNo ratings yet
- Non-Hodgkins Lymphoma (Report)Document50 pagesNon-Hodgkins Lymphoma (Report)Dayledaniel SorvetoNo ratings yet
- 11 Hematological MalignanciesDocument34 pages11 Hematological MalignanciesalitahawarbarintNo ratings yet
- Lymphoid NeoplasmsDocument39 pagesLymphoid NeoplasmsMoshe GiftNo ratings yet
- Lymphomas: Dr. Y.A. AdelabuDocument28 pagesLymphomas: Dr. Y.A. Adelabuadamu mohammadNo ratings yet
- NHL Nandu CopasDocument95 pagesNHL Nandu CopaswihelminaNo ratings yet
- LNs HNDocument190 pagesLNs HNNinna Isabel VictorioNo ratings yet
- C6.1clasificare LimfoameDocument10 pagesC6.1clasificare LimfoameRădulescu AndreeaNo ratings yet
- Overview of LymphomasDocument44 pagesOverview of LymphomasHarsha MaheshwariNo ratings yet
- Lymph Node CytologyDocument39 pagesLymph Node Cytologykamranghani641No ratings yet
- Non-Hodgkins LymphomaDocument22 pagesNon-Hodgkins LymphomaNyoman TapayanaNo ratings yet
- Limfoma (Kuliah 3a Ipd III)Document30 pagesLimfoma (Kuliah 3a Ipd III)Rianda Dwi PutraNo ratings yet
- NHL Arshad KhanDocument30 pagesNHL Arshad KhanArshad khanNo ratings yet
- Medicine Seminar Combined-1Document30 pagesMedicine Seminar Combined-1Deepanshu KumarNo ratings yet
- Haematology LeukaemiaDocument28 pagesHaematology LeukaemiaFrolian MichaelNo ratings yet
- Overview of LymphomaDocument42 pagesOverview of Lymphomaadamu mohammadNo ratings yet
- Non-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!Document48 pagesNon-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!francis00090No ratings yet
- Pathology of Lymph Nodes: Norman Levy, MDDocument92 pagesPathology of Lymph Nodes: Norman Levy, MDAdi ParamarthaNo ratings yet
- Non Hodgkin's LymphomaDocument31 pagesNon Hodgkin's LymphomaJeo Thomas100% (1)
- 3 Final Lymphoma and MyelomaDocument16 pages3 Final Lymphoma and MyelomaRumela Chakraborty100% (1)
- Acute Leukemia: Thirunavukkarasu MurugappanDocument22 pagesAcute Leukemia: Thirunavukkarasu MurugappanFelix Allen100% (1)
- Non-Hodgkin's LymphomasDocument23 pagesNon-Hodgkin's LymphomasshevmyrNo ratings yet
- Lymphoid Lekemia: DR Budi Enoch SPPDDocument32 pagesLymphoid Lekemia: DR Budi Enoch SPPDLia pramitaNo ratings yet
- Bethy Suryawathy, Dr.,Sppa.,Phd. Bagian Patologi Anatomi Fakultas Kedokteran UnpadDocument31 pagesBethy Suryawathy, Dr.,Sppa.,Phd. Bagian Patologi Anatomi Fakultas Kedokteran UnpadDhika ArdiansyahNo ratings yet
- LymphomaDocument20 pagesLymphomaChairul Adilla Ardy100% (1)
- DR Opeyemi IdaeworDocument69 pagesDR Opeyemi IdaeworOpeyemi IdaeworNo ratings yet
- WBC DisordersDocument45 pagesWBC DisordersyalahopaNo ratings yet
- 2 - Lymphoma Lecture by Dr. M T - PresentationDocument40 pages2 - Lymphoma Lecture by Dr. M T - Presentationsohilaw210No ratings yet
- A7Document4 pagesA7Saman SadeghiNo ratings yet
- 牙三實驗 HematopathologyDocument57 pages牙三實驗 Hematopathology6zpv64hbthNo ratings yet
- Lymphoma: David Lee MD, FRCPCDocument36 pagesLymphoma: David Lee MD, FRCPCQasim AliNo ratings yet
- Hodgkin'S Disease AND Non-Hodgkin'S LymphomaDocument42 pagesHodgkin'S Disease AND Non-Hodgkin'S LymphomaRayya TriandaNo ratings yet
- NHL 1Document13 pagesNHL 1kushalNo ratings yet
- Hodgkin-Lymphoma. Plasma Cell NeoplasiasDocument2 pagesHodgkin-Lymphoma. Plasma Cell NeoplasiasSaman SadeghiNo ratings yet
- Genevieve Crane - Approach To Lymph Node-Path Cast Lymph Node Pathology Eve CraneDocument75 pagesGenevieve Crane - Approach To Lymph Node-Path Cast Lymph Node Pathology Eve CraneJose SirittNo ratings yet
- Hodgkin's Lymphoma (Patho Lec 2)Document37 pagesHodgkin's Lymphoma (Patho Lec 2)mina mounirNo ratings yet
- Hodgkin's DiseaseDocument58 pagesHodgkin's Diseasealibayaty1No ratings yet
- 1 - Lymphomas - Gelinde NarekineDocument64 pages1 - Lymphomas - Gelinde NarekineAntna SinekNo ratings yet
- NHLDocument35 pagesNHLnn zelaNo ratings yet
- Chronic Lymphocytic LeukemiaFrom EverandChronic Lymphocytic LeukemiaMichael HallekNo ratings yet
- InflamasiDocument63 pagesInflamasiRyo RyozNo ratings yet
- 4b TUMOR JAR RetikuloendotelialAAADocument98 pages4b TUMOR JAR RetikuloendotelialAAARyo RyozNo ratings yet
- InflamasiDocument63 pagesInflamasiRyo RyozNo ratings yet
- 7 Tumor KulitDocument102 pages7 Tumor KulitRyo RyozNo ratings yet
- Jurnal Tatalaksana KAD Pada AnakDocument18 pagesJurnal Tatalaksana KAD Pada AnakAfkaraHusnaFirdanisaNo ratings yet
- Using Insulin: What Is Insulin? Types of InsulinDocument4 pagesUsing Insulin: What Is Insulin? Types of InsulinRyo RyozNo ratings yet
- Anti-Stress Cem - Tech by MichaelDocument30 pagesAnti-Stress Cem - Tech by MichaelTulhina AndreiNo ratings yet
- Pathogenesis of Graft-Versus-Host Disease (GVHD) - UpToDateDocument12 pagesPathogenesis of Graft-Versus-Host Disease (GVHD) - UpToDatemihaela popescuNo ratings yet
- Vetscan ObjectivesDocument395 pagesVetscan ObjectivesDeep PatelNo ratings yet
- ImmunoSero Immunology Overview NotesDocument4 pagesImmunoSero Immunology Overview NotesAndrienne Valen de BelenNo ratings yet
- Acquired ImmunityDocument16 pagesAcquired ImmunityMohammed Hashem100% (1)
- Immunology Overview: Armond S. Goldman Bellur S. PrabhakarDocument45 pagesImmunology Overview: Armond S. Goldman Bellur S. PrabhakarIoana AsziaNo ratings yet
- Human Health and Disease-1Document12 pagesHuman Health and Disease-1Ananya MoniNo ratings yet
- Stevens (Science) Med TechDocument31 pagesStevens (Science) Med TechnotsoninjaninjaNo ratings yet
- Parasitic Infections: Pathogenesis and Immunity: J. StewartDocument7 pagesParasitic Infections: Pathogenesis and Immunity: J. Stewartnour achkarNo ratings yet
- General Biology 2 (4 Quarter) : Animal and Plant ReproductionDocument23 pagesGeneral Biology 2 (4 Quarter) : Animal and Plant Reproductionamethyst grande100% (1)
- Lymphatic CaseDocument6 pagesLymphatic CaseGlenn Arjay BataraoNo ratings yet
- Cancer Immune TherapyDocument452 pagesCancer Immune TherapyatyNo ratings yet
- Immunity All NotesDocument112 pagesImmunity All NotesJonathan Carlisle CheungNo ratings yet
- Immuno Modulator yDocument377 pagesImmuno Modulator ysaman7752No ratings yet
- Disorders of White Blood Cells and Lymphoid TissuesDocument30 pagesDisorders of White Blood Cells and Lymphoid Tissuesammar amerNo ratings yet
- Leukemia Infographic PDFDocument1 pageLeukemia Infographic PDFPriyanka KhuranaNo ratings yet
- Part C-35 MCQS/ 7 PP: MCQ PaediatricsDocument6 pagesPart C-35 MCQS/ 7 PP: MCQ Paediatricswindows3123100% (1)
- Immuno and InfectiousDocument17 pagesImmuno and Infectiousgreen_archerNo ratings yet
- Metapopulation ModellingDocument25 pagesMetapopulation Modellingjolamo1122916No ratings yet
- Study Guide: Cytokines Associated With Innate ImmunityDocument12 pagesStudy Guide: Cytokines Associated With Innate ImmunityxxxxxxxNo ratings yet
- Acute Lymphocytic Leukaemia Diagnosis and Treatment A Review PDFDocument7 pagesAcute Lymphocytic Leukaemia Diagnosis and Treatment A Review PDFJunita Nelly Esther JosephNo ratings yet
- Incorrectly: CorrectlyDocument25 pagesIncorrectly: CorrectlypikachuNo ratings yet
- Lymph Drainage Therapy PDFDocument7 pagesLymph Drainage Therapy PDFDiego Mamani Mullisaca100% (2)
- (Advances in Space Biology and Medicine 6) Sjoerd L. Bonting (Eds.) - Elsevier Science (1997)Document318 pages(Advances in Space Biology and Medicine 6) Sjoerd L. Bonting (Eds.) - Elsevier Science (1997)Sohnit KumarNo ratings yet
- Perfect Score Module 2017 Form 5 Answer SchemeDocument24 pagesPerfect Score Module 2017 Form 5 Answer SchemeChen ShyanNo ratings yet
- Hematological Anatomy, Physiology and Assessment: This Course Has Been Awarded One (1.0) Contact Hour. July 30, 2019Document19 pagesHematological Anatomy, Physiology and Assessment: This Course Has Been Awarded One (1.0) Contact Hour. July 30, 2019Mill Jan CruzNo ratings yet
- Basic ImmunologyDocument29 pagesBasic ImmunologyHema Duddukuri0% (1)