Professional Documents
Culture Documents
Grand Reports
Grand Reports
Uploaded by
filchibuffOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Grand Reports
Grand Reports
Uploaded by
filchibuffCopyright:
Available Formats
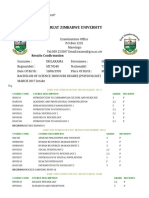
QUIRINO MEMORIAL MEDICAL CENTER
PROJ. 4, QUEZON CITY
DEPARTMENT OF PEDIATRICS
A CLINICAL CASE
PRESENTED BY:
ANDY M. MARTINEZ
JAMES B. TAMAYO
REGIL O. TORRES
IDENTIFYING DATA:
D. T.
6 years old
Female
Filipino
Roman Catholic
Right handed
San Roque, Quezon City
Birthday: April 5, 2006
QMMC: October 04, 2012 at around 8:40 pm
INFORMANT:
Patient herself and mother
CHIEF COMPLAINT:
Fever of 4 days duration
HISTORY OF PRESENT ILLNESS :
4 days PTC:
Fever (Tmax: 38.2 C)
Headache: unilateral, frontal in location, non radiating, 5/10,
pulsating
Poor appetite, weak-looking
No cough, colds, muscle pain, difficulty of breathing, chest pain
Paracetamol 250mg/5ml, 5ml syrup every 4 hours temporarily
relieved
No consult
2 days PTC:
Still with fever (Tmax: 38.7 C)
Headache: unilateral, frontal in location, non radiating, 7/10,
pulsating
Poor appetite, weak-looking
Non productive cough, no phlegm
Sore throat
1 episode of vomiting (undigested food)
Abdominal pain: 5/10, pricking, non radiating
Paracetamol 250mg/5ml, 5ml syrup every 4 hours temporarily
relieved
No consult
1 day PTC:
Persistence of the above symptoms
Consult admission
MATERNAL AND BIRTH HISTORY:
35 y/o G4P4 (4004) via NSD
Full termed and planned pregnancy
4x prenatal check up at QMMC
No tobacco, drugs and alcohol use
No fetomaternal illnesses during pregnancy. No vaginal
bleeding.
No infectious diseases such as fever, cough or colds contracted
during her pregnancy.
OBSTETRIC HISTORY: G4P4 (4004)
Year MOD Where Sex Complications
G1 1999 NSD QMMC Male None
G2 2003 NSD QMMC Male None
G3 2006 NSD QMMC Female None
G4 2008 NSD QMMC Female None
NEONATAL HISTORY :
Estimated weight of 8 lbs
No congenital anomalies
Pink color with a loud cry
No cyanosis
The child was breastfed
FEEDING HISTORY:
Infancy:
Breastfed until 6 months with good suck, no noted feeding
difficulties
Bottle-feeding started using Bona, approximately 6-8 bottles per
day
Introduction of solid foods at 6 months (mashed potatoes)
Childhood:
Eats 3 times a day
Present diet and appetite- likes eating chicken, hotdog and eggs
DEVELOPMENTAL HISTORY:
Smiles in response to voice at 2 months
Grasp objects at around 4 months
Crawl and sit at around 5 - 6 months
Follow command with gesture at 7 - 8 months
Roll over - 5 months
Speech- 6 months
Hold a bottle - 7 months
Reach out to objects - 9 months
Walk alone - 1 year
Jump - 2 years
Plays and watches TV with his mother everyday
IMMUNIZATIONS:
Immunizations complete
BCG 0.05ml ID at 1
st
month
Hepa B 0.5ml IM at birth, 1
st
, 6
th
months
Measles 0.5ml SC at 9
th
months
DPT 0.5ml IM at 2
nd
, 4
th
, 6
th
months
OPV 2-3 drops at 2
nd
, 4
th
, 6
th
months
No adverse reactions to the immunizations given
PAST MEDICAL HISTORY :
No history of asthma, TB, pneumonia, diabetes,
hypertension
No allergies to foods or medication
History of exposure to throat infection - brother, Sept. 30,
2012
No past hospitalization or surgeries
FAMILY HISTORY :
(-) Allergy
(-) Asthma
(-) DM
(-) PTB
(-) HTN
(-) Cancer
(-) CVD
(-) Thyroid disease
(-) Kidney disease
FAMILY GENOGRAM:
Dimpas, Family
As of October 4, 2012
San Roque, Quezon City
1995
Ron, 15
Susan,35 Susan,32 Jeffrey,29
Tricia,6 Rey, 10
Reynaldo, 38
Rachelle, 3
Legend:
Throat infection, September 30, 2012
index patient
Rey, 55 Rosaly, 56
SOCIAL HISTORY:
Lives with other 6 family members
Water source (NAWASA)
Garbage is collected twice a week
Good interpersonal relations with her brothers and sisters
Good living condition
REVIEW OF SYSTEM:
Skin:
(-) Itchiness
(-) Excessive dryness
(-) Pallor
Head:
(-) Dizziness
Eyes:
(-) Photophobia
(-) Excessive lacrimation
(-) Photophobia
(-) Diplopia
(-) Eye pain
(-) Loss of vision
(-) Double vision
Ears:
(-) Changes in hearing
(-) Tinnitus
(-) Discharge
(-) Otalgia
Nose:
(-) Changes in smell
(-) Epistaxis
(-) Obstruction
(-) Colds
Mouth and throat:
(-) Gum bleeding
(-) Tooth ache
(-) Changes in taste
Respiratory System:
(-) Sputum production
(-) Hemoptysis
(-) Difficulty of breathing
Cardiovascular System:
(-) Orthopnea
(-) PND
(-) Palpitations
(-) Syncope
(-) Easy fatigability
Gastrointestinal System:
(-) Diarrhea
(-) Hematemesis
(-) Constipation
(-) Melena
(-) Hematochezia
Genito-urinary Tract:
(-) Urinary frequency
(-) Incontinence
(-) Genital puritus
(-) Dysuria
(-) Hematuria
Endocrine:
(-) Polyuria
(-) Polyphagia
(-) Polydipsia
Hematologic:
(-) Easy bruisability
(-) Abnormal bleeding
Neuromuscular/Musculoskeletal:
(-) Seizure
(-) Weakness
PHYSICAL EXAMINATION UPON ADMISSION:
General Survey: awake, conscious, coherent, ambulatory, not
in cardio-respiratory distress
Vital signs:
BP: 90/60
CR: 100 bpm
RR: 24 b/m
Temp: 38. 3 C
Weight: 24 kgs
PHYSICAL EXAMINATION:
HEENT: Normocephalic, no head injuries, anicteric sclera,
pupils are reactive to light, nasal mucosa pink, no polyps,
septum is midline, oral mucosa is pink, hyperemic and
swollen tonsils, no pharyngeal exudates, tongue midline,
supple neck, no CLAD
Chest/Lungs: No masses or scars. Symmetric chest wall
expansion, no retractions, clear breath sounds
Cardiovascular: Adynamic precordium, PMI: 5
th
left ICS, regular
rate and rhythm, no murmurs, S1 > S2
Abdomen: Flat, no scars, masses or hyperpigmentations. No
enlarged or dilated veins, no visible pulsations or peristalsis.
NABS, tympanitic. No bruit, rigidity, masses, organomegaly,
mild tenderness. Spleen and kidneys not felt. No
costovertebral angle tenderness (CVAT).
Extremities: No scars or masses. Full equal pulses, no edema
and cyanosis
LABORATORY RESULTS:
Test Result Reference range
RBC 4.41 4.20 - 5.40
Hemoglobin 119 L 120 - 160
Hematocrit 0.36 0.36 - 0.47
MCV 82.2 80 - 96
MCH 26. 9 L 27 - 31
MCHC 32.80 32 - 36
RDW 13.7 11.6 - 14.6
Platelet Count 349 150 - 450
WBC 15.3 H 5.0 - 10.0
Neutrophils 0.835 H 0.500 - 0. 700
Lymphocytes 0.095 L 0.200 - 0.500
Monoctyes 0.068 0.020 - 0.090
Basophils 0.002 0.000 - 0. 020
URINALYSIS :
Color Yellow
Transparency Clear
PH 6.0
Specific Gravity 1.030
WBC 0-2/hpf
RBC 0- 3/ hpf
Albumin negative
Sugar negative
SEROLOGY :
Rapid Test Dengue IgG- negative
IgM-negative
Dengue Antigen Negative
COURSE IN THE WARD :
DAY S O A P
Hospital day 1:
8:45 pm
(+) fever x 4days
(+) sore throat
(+) epigastric pain
(+) headache
BP-90/60
RR: 24
PR: 100 bpm
Temp: 38.2 C
.
ATP r/o DHF I Please admit to
pedia ward.
Secure consent for
admission
management.
DAT + no dark
colored foods.
TPR+ BP Q4 ad
record.
PNSS 1L@ 28
gtts/min.
Labs:
CBC, APC, Dengue
blot, U/A.
Tx:Paracetamol 250
mg/ 5 ml, give 6.5
ml Q4 if fever >37.8
deg cel.
Ranitidine 25 mg
TIV q 8 hrs
DAY S O A P
3:00 am (+) febrile episodes
(+) abdominal pain
(+) hyperemic
tonsils
Fair intake
Full pulses
(-) cough and colds
Temp: 38.5 C
ATP r/o DHF
IVF : PNSS 1L x 30
gtts /ml.
Star Ranitidine
25mg TIV.
Ampicillin 500 mg
TID Q6.
Awaits lab results.
Hospital day 2: Febrile episodes
Comfortable
Good intake
(-) abdominal pain
Temp: 36.7 C
ATP, Non exudative IVF D5NM 1L cc x
25 gtts/min.
Meds: Amipicillin
d/c Ranitidine.
CBC w/ APC
Day S O A P
Hospital Day 3: Afebrile
Comfortable
Good intake
(-) vomiting
Full pulses
Temp-36.8 C
Neutro- 0.374
WBC-7.3
ATP, Non exudative
MGH after result of
CBC.
Hospital Day 4 : Afebrile
Comfortable
Good intake
(-) vomiting
(-) hyperemic
tonsils
Temp-36.7 Cel. ATP, Non exudative
MGH
OPD ff up after 1
week, 7am.
Meds:
Amoxicillin
250mg/5ml, 7.5 ml
TIDx 7 days.
Ascorbic acid ,
250mg/5ml, OD.
SALIENT FEATURES:
6 years old
Fever
Sore throat
Headache
Cough
Abdominal pain
Vomiting
History of exposure to throat infection
Hyperemic and swollen tonsils and pharynx
DIFFERENTIAL DIAGNOSIS:
Acute tonsillopharyngitis
Dengue
Leptospirosis
Diptheria
DENGUE FEVER :
Transmitted by the bite of an Aedes mosquito
Occurs in tropical and sub-tropical areas of the world
Symptoms appear 3-14 days after the infective bite
Symptoms: range from a mild fever, to incapacitating high
fever, with severe headache, pain behind the eyes,
muscle and joint pain, and rash
There are no specific antiviral medicines for dengue. It is
important to maintain hydration.
Dengue haemorrhagic fever (fever, abdominal pain,
vomiting, bleeding) is a potentially lethal complication,
affecting mainly children.
LEPTOSPIROSIS:
Infectious disease caused by a type of bacteria called a
spirochete.
Transmitted by many animals such as rats, skunks,
opossums, raccoons, foxes, and other vermin.
Mode of transmission:
contact with infected soil or water through broken skin
and mucous membrane
ingesting contaminated food or water
Most Common:
Dry cough
Fever
Headache
Muscle pain
Nausea, vomiting, and
diarrhea
Shaking chills
Less common:
Abdominal pain
Abnormal lung sounds
Bone pain
Conjunctivitis
Enlarged lymph glands
Enlarged spleen or liver
Joint aches
Muscle rigidity
Muscle tenderness
Skin rash
Sore throat
DIPTHERIA:
Acute infectious disease caused by the
bacteria Corynebacterium diphtheriae.
Diphtheria spreads through respiratory droplets (such as
those produced by a cough or sneeze) of an infected
person or someone who carries the bacteria but has no
symptoms.
Most commonly infects the nose and throat.
The throat infection causes a gray to black, tough, fiber-like
covering, which can block the airways.
In some cases, diphtheria may first infect the skin,
producing skin lesions.
Risk factors include crowded environments, poor hygiene,
and lack of immunization.
Fever
Chills
Fatigue
Bluish skin coloration
Sore throat
Hoarseness
Cough
Headache
Difficulty/Painful swallowing
Difficulty breathing
Rapid breathing
Foul-smelling bloodstained nasal discharge
Lymphadenopathy
PRIMARY WORKING IMPRESSION:
ACUTE TONSILLOPHARYNGITIS, NON EXUDATIVE
Swelling of the pharynx and the
tonsils.
The pharynx is the back of the
throat, including the back of the
tongue.
Both pharyngitis and
tonsillopharyngitis -- sore throat.
TYPES BASED ON ETIOLOGY:
Viral tonsillopharyngitis:
Inflammatory condition of the tonsils
Cause: respiratory viruses
oadenovirus, influenza, parainfluenza, and respiratory syncitial
virus.
Other viral agents
o include coxsackie, echoviruses, herpes simplex and Epstein Barr
Virus (EBV)
Bacterial tonsillopharyngitis:
Inflammatory condition of the pharynx and or tonsils
Cause:
o Group A beta-hemolytic streptococci (GABHS)
o Hemophilus influenza
o Moraxella catarrhalis
Features suggestive of bacterial etiology:
Sudden onset
Sore throat /Dysphagia
Fever
Petechiae
Headache
Nausea, vomiting, and abdominal pain
Inflammation of pharynx and tonsils
Patchy discrete exudates
Tender, enlarged anterior cervical nodes
Patients aged 5-15 years
History of exposure
Features suggestive of viral etiology:
Conjunctivitis
Coryza
Cough
Hoarseness
Diarrhea
****Highlighted features are adapted from the Centor Criteria****
DISCUSSION
Tonsillopharyngitis:
30% of patients
Group A -hemolytic streptococcus (GABHS) is most
common
But Staphylococcus aureus, Streptococcus
pneumoniae, Mycoplasma pneumoniae, andChlamydia
pneumoniae are sometimes involved
Rare causes:
Pertussis,Fusobacterium,Diphtheria,Syphilis,Gonorrhea
GABHS: occurs most commonly between ages 5 and 15 and
is uncommon before age 3.
Streptococcal tonsillopharyngitis:
Inflammatory condition of the pharynx caused by Group A
beta-hemolytic streptococci
Incubation period: 2 5 days
Most common in children: 5 - 12 years of age
Risk of acute rheumatic fever complicating untreated
streptococcal pharyngitis is 1%.
Assoc. complications: glomerulonephritis and RHD
RISK FACTORS :
Age: children and teens, and people aged 65 years or
older
Exposure: with a sore throat or any other infection
involving the throat, nose, or ears
Exposure: cigarette smoke, toxic fumes, industrial smoke,
and other air pollutants
Hay fever or other allergies and stress
Having other conditions that affect your immune system,
such as AIDS or cancer
SYMPTOMS:
Sore throat
Pain or difficulty when swallowing
Difficulty breathing
Fever
Enlarged lymph nodes in your neck
Hoarse voice
Red or irritated looking throat
Swollen tonsils
White patches on or near your tonsils
Runny nose or stuffy nose
Cough
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE AND
CHRONIC TONSILLOPHARYNGITIS
1. The diagnosis of acute tonsillopharyngitis may be made
clinically for both children and adults. It is important to
differentiate whether the infection is viral or bacterial in
etiology.
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE
AND CHRONIC TONSILLOPHARYNGITIS
2. The diagnosis of acute group A streptococcal infection
should be suspected on clinical grounds and may be
supported by performance of a laboratory test.
Grade B Recommendation:
Throat culture remains to be the gold standard for the
diagnosis of streptococcal pharyngitis with a sensitivity
of 90-95%.
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE
AND CHRONIC TONSILLOPHARYNGITIS
Grade B Recommendation:
A positive rapid antigen detection test (RADT) may be
considered definitive evidence for treatment of
streptococcal pharyngitis, with specificity of 95% and
sensitivity of 89.1%.
These values are similar to those of throat culture
which has a 99% specificity and 83.4% sensitivity.
RADT: not widely available locally and cannot be
considered part of routine diagnostic assessment.
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE
AND CHRONIC TONSILLOPHARYNGITIS
Grade C Recommendation
Either a positive throat culture or RADT provides adequate
confirmation of GABHS in the pharynx, but a negative
RADT result should be confirmed with a throat culture
whenever possible.
However, the value of early diagnosis in the minority of
cases when streptococcus is present should be weighed
against the higher cost incurred in testing the majority of
cases seen.
Selective use of diagnostic studies is suggested.
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE
AND CHRONIC TONSILLOPHARYNGITIS
3. The diagnosis of chronic tonsillitis can be made by a
history of medically documented episodes of acute
tonsillitis for at least 4 times a year.
Grade C Recommendation
There are four randomized controlled trials (RCT) on
tonsillectomy versus non-surgical intervention studies in
children but no RCT in adults.
More than 5 episodes and American Academy of
Otolaryngology-Head and Neck Surgery more than 3
episodes as indication for tonsillectomy.
RECOMMENDATIONS ON THE DIAGNOSIS OF ACUTE
AND CHRONIC TONSILLOPHARYNGITIS
4. The diagnosis of obstructive adenoidal hypertrophy should
be made on the basis of enlarged adenoids and a
persistent difficult in breathing and/or swallowing.
Grade C Recommendation:
The following may be used in the diagnosis of obstructive
adenoidal hypertrophy:
Anterior rhinoscopy
Posterior rhinoscopy
Intraoral palpation
Soft tissue lateral films of the nasopharynx may be used to
determine the adenoid enlargement but its low sensitivity and the
need for proper radiologic techniques is emphasized
DIAGNOSIS:
Clinical evaluation
GABHS ruled out by rapid antigen test, culture, or both
Blood count and differential count.
TREATMENT/MANAGEMENT:
Antibiotics for strep throat
Drugs to reduce sore throat pain; these drugs include:
Ibuprofen (Motrin, Advil)
Acetaminophen (Tylenol)
Aspirin
Note: Aspirin is not recommended for children or teens
with a current or recent viral infection. This is because of
the risk of Reye's syndrome.
Numbing throat spray
Decongestants and antihistamines
Throat lozenges
Corticosteroids
PROGNOSIS;
Good
COMPLICATIONS;
Rheumatic fever and subsequent rheumatic heart disease
Poststreptococcal glomerulonephritis
Peritonsillar abscess
Systemic infection
Otitis media
Mastoiditis
Septicemia or toxic shock syndrome
Rhinitis
Sinusitis
Pneumonia
HOME CARE :
Get plenty of rest
Drink plenty of water
Gargle with warm salt water several times a day
Drink warm liquids (tea or broth) or cool liquids
Avoid irritants that might affect your throat, such as smoke
from cigarettes, cigars, or pipes, and cold air
Avoid drinking alcohol
PREVENTION:
Wash hands frequently
If someone who had a sore throat, keep his eating utensils
and drinking glasses separate from those of other family
members
If a toddler with a sore throat has been sucking on toys, wash
the toys in soap and water.
If you have hay fever or another respiratory allergy, ask for
consult.
Avoid the substance that causes your allergy.
THANK YOU(,)
You might also like
- Anesthesia Care PlanDocument2 pagesAnesthesia Care PlanMedShare100% (11)
- Internal Medicine Study GuideDocument71 pagesInternal Medicine Study GuideMedicine4theMasses95% (19)
- Method Statement - Relocation of Water MeterDocument5 pagesMethod Statement - Relocation of Water MeterMG50% (2)
- PNEUMONIA Case 2 PDFDocument49 pagesPNEUMONIA Case 2 PDFRed OrangeNo ratings yet
- Fluid Management For The Pediatric Surgical Patient POWERPOINTDocument34 pagesFluid Management For The Pediatric Surgical Patient POWERPOINTDipta Anggara100% (2)
- Hirschsprung NCM 109 Case PresentationDocument10 pagesHirschsprung NCM 109 Case PresentationValerie LeddaNo ratings yet
- GBS Case StudyDocument5 pagesGBS Case StudyDelphy Varghese0% (1)
- Appraisal FormDocument5 pagesAppraisal FormRay Dan Aro CelerianNo ratings yet
- 2009 Parasitology MCQsDocument12 pages2009 Parasitology MCQsfilchibuff89% (9)
- All Questions PhysiologyDocument25 pagesAll Questions Physiologyfilchibuff100% (6)
- All Questions PhysiologyDocument25 pagesAll Questions Physiologyfilchibuff100% (6)
- Chemistry: 1.tietz Textbook of Clinical Chemistry and Molecular Diagnostics, Fourth Edition, Page 861Document1 pageChemistry: 1.tietz Textbook of Clinical Chemistry and Molecular Diagnostics, Fourth Edition, Page 861Tauqeer AbbasNo ratings yet
- Introduction To Artificial Intelligence AssignmentDocument48 pagesIntroduction To Artificial Intelligence AssignmentSreePrakashNo ratings yet
- Tiger Bio Filter - InformationDocument3 pagesTiger Bio Filter - InformationPRASHANT INGALENo ratings yet
- Pedia PPT1Document52 pagesPedia PPT1Jan Mikhail FrascoNo ratings yet
- Case Presentation: Paediatrics: by Tapan Jyoti Saikia 8 Sem Gauhati Medical CollegeDocument22 pagesCase Presentation: Paediatrics: by Tapan Jyoti Saikia 8 Sem Gauhati Medical CollegeArpit Mehta100% (1)
- SCHIZODocument25 pagesSCHIZOQuinonez Anna MarieNo ratings yet
- Name of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisDocument13 pagesName of The Hospital - Teaching Hospital, Karapitiya: Case 7 Puerperal PsychosisCharith Rukmal KodituwakkuNo ratings yet
- Background: Viral Mumps InfectionDocument5 pagesBackground: Viral Mumps InfectionAgustin UyNo ratings yet
- Toaz - Info Case Study Pneumonia PRDocument41 pagesToaz - Info Case Study Pneumonia PRTrixNo ratings yet
- Case Presentation On Copd: By, Thomas Eipe Pharm D InternDocument32 pagesCase Presentation On Copd: By, Thomas Eipe Pharm D InternThomas EipeNo ratings yet
- Epilepsy CaseDocument17 pagesEpilepsy CaseSuresh ThanneruNo ratings yet
- Definition:: EpilepsyDocument7 pagesDefinition:: EpilepsyNinia MNo ratings yet
- Pedia - DengueDocument10 pagesPedia - DengueJan Mikhail FrascoNo ratings yet
- Mental Health Case StudyDocument11 pagesMental Health Case Studyapi-453449063No ratings yet
- Case PresentationDocument5 pagesCase Presentationahmadhajjj100% (1)
- Seminar 2 (Paeds)Document31 pagesSeminar 2 (Paeds)Jonathan YeohNo ratings yet
- Clinical Case: Section A - Group 8Document68 pagesClinical Case: Section A - Group 8madison Deli100% (1)
- CASE STUDY TablesDocument9 pagesCASE STUDY TablesMicah MagallanoNo ratings yet
- Case 1 Doc GonsalvesDocument7 pagesCase 1 Doc GonsalvesMonique Angela Turingan GanganNo ratings yet
- A Case Presentation On Enteric FeverDocument15 pagesA Case Presentation On Enteric FeverJob GeorgeNo ratings yet
- College of Nursing: Panpacific University North PhilippinesDocument20 pagesCollege of Nursing: Panpacific University North PhilippinesMar OrdanzaNo ratings yet
- Client Profile With HypertensionDocument8 pagesClient Profile With HypertensionplokatzNo ratings yet
- Pediatric Case StudyDocument29 pagesPediatric Case Studyapi-296281683No ratings yet
- Case Presentation Meningitis 1Document17 pagesCase Presentation Meningitis 1chaudharitrushar007No ratings yet
- PEDIA - TachypneaDocument12 pagesPEDIA - TachypneaAlvin Germo PasuquinNo ratings yet
- Obstetrics Case PresentationDocument27 pagesObstetrics Case PresentationMahaprasad sahoo 77No ratings yet
- Refractive ErrorDocument6 pagesRefractive Errortri erdiansyahNo ratings yet
- History:: Chief Complaint: History of Present IllnessDocument4 pagesHistory:: Chief Complaint: History of Present IllnessIbrahem Y. NajjarNo ratings yet
- Cirrhosis Case For PrintingDocument12 pagesCirrhosis Case For PrintingSean Mercado100% (1)
- Case Presentation IM DDHDocument12 pagesCase Presentation IM DDHAishwarya BharathNo ratings yet
- Case Presentation On MalariaDocument13 pagesCase Presentation On Malarialavate amol bhimraoNo ratings yet
- Epilepsy in ChildhoodDocument20 pagesEpilepsy in ChildhoodRizky Indah SorayaNo ratings yet
- How Phototherapy WorksDocument4 pagesHow Phototherapy WorksmaramNo ratings yet
- Cough and Dyspnea Case StudyDocument4 pagesCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Care Plan-Otitis NewDocument33 pagesCare Plan-Otitis NewSUNIL KUMARNo ratings yet
- Case No 1 ClinicalDocument7 pagesCase No 1 ClinicalSarah Saqib AhmadNo ratings yet
- Final Hernioplasty Compilation RevisedDocument58 pagesFinal Hernioplasty Compilation RevisedRaidis PangilinanNo ratings yet
- Antepartum HemorrhageDocument6 pagesAntepartum HemorrhageNurul SyuhadaNo ratings yet
- Pediatric Case PresentationDocument12 pagesPediatric Case PresentationMohammed jouhra100% (1)
- Role of Food and Exercise in Polycystic Ovarian SyndromeDocument3 pagesRole of Food and Exercise in Polycystic Ovarian SyndromeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Case ReportDocument19 pagesCase ReportvivitaslimNo ratings yet
- BronchopnemoniaDocument23 pagesBronchopnemoniadg_tajudinNo ratings yet
- Neonatal Case Presentation-1Document16 pagesNeonatal Case Presentation-1Ananya SampathNo ratings yet
- DENGUEDocument21 pagesDENGUEHikari 光 ShidouNo ratings yet
- My Cwu OphthalDocument16 pagesMy Cwu OphthalSalsabila Al-BasheerNo ratings yet
- Management of Patient With Meningitis and Encephalitis: ModeratorDocument71 pagesManagement of Patient With Meningitis and Encephalitis: ModeratorSachin DwivediNo ratings yet
- Name: Wong Wai Kheong Matrix No: BMS12081154Document13 pagesName: Wong Wai Kheong Matrix No: BMS12081154myolie wuNo ratings yet
- Danger Signs in NewbornDocument22 pagesDanger Signs in NewbornAbhirup BoseNo ratings yet
- Cwe Nephrotic SnydromeDocument12 pagesCwe Nephrotic SnydromeFariezuan HamidNo ratings yet
- Case PresentationDocument11 pagesCase PresentationjassmileNo ratings yet
- Case HirschsprungDocument29 pagesCase HirschsprungPriscila StevanniNo ratings yet
- Peds Case 3Document5 pagesPeds Case 3Mohammed AhmedNo ratings yet
- Case Study - OTITIS MEDIADocument9 pagesCase Study - OTITIS MEDIAHasing Amado100% (1)
- 10 Aschool Health PRGRM DoneDocument166 pages10 Aschool Health PRGRM DoneHarshitha100% (1)
- Case Presentation - Visceral LeishmaniaDocument18 pagesCase Presentation - Visceral LeishmaniaAAANo ratings yet
- Nursing Care PlanDocument15 pagesNursing Care PlanJemina Rafanan RacadioNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Cholecystitis, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Cholecystitis, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Comprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)Document31 pagesComprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)filchibuffNo ratings yet
- Pedia MCUDocument65 pagesPedia MCUfilchibuffNo ratings yet
- Mary Johnston Hospital: Philhealth AccreditedDocument1 pageMary Johnston Hospital: Philhealth AccreditedfilchibuffNo ratings yet
- PDF Adult Directory2009Document48 pagesPDF Adult Directory2009filchibuffNo ratings yet
- Philippine College of Physicians Daily Census OPD Hospital: (M or F) (S or P)Document2 pagesPhilippine College of Physicians Daily Census OPD Hospital: (M or F) (S or P)filchibuffNo ratings yet
- Mary Johnston Hospital: Philhealth AccreditedDocument1 pageMary Johnston Hospital: Philhealth AccreditedfilchibuffNo ratings yet
- Img 20160912 0003Document1 pageImg 20160912 0003filchibuffNo ratings yet
- Anesthesiology Lecture Research Paper: Centro Escolar UniversityDocument1 pageAnesthesiology Lecture Research Paper: Centro Escolar UniversityfilchibuffNo ratings yet
- Microbiology - Basic Immunology RevisedDocument6 pagesMicrobiology - Basic Immunology RevisedfilchibuffNo ratings yet
- Ob - Gyne FinalddffDocument28 pagesOb - Gyne FinalddfffilchibuffNo ratings yet
- DirectoryDocument1 pageDirectoryfilchibuffNo ratings yet
- Airport Diagram: Field Elev 439Document1 pageAirport Diagram: Field Elev 439filchibuffNo ratings yet
- History Physical FormatDocument3 pagesHistory Physical FormatfilchibuffNo ratings yet
- PhysiologyDocument4 pagesPhysiologyAileen Castillo100% (1)
- (P) Physiology - CimDocument7 pages(P) Physiology - CimfilchibuffNo ratings yet
- Ob-Gyn Review Part 3Document101 pagesOb-Gyn Review Part 3filchibuffNo ratings yet
- Final FS Balachan DipDocument121 pagesFinal FS Balachan DipRosemarie VeluzNo ratings yet
- RESEARCH PaperDocument17 pagesRESEARCH PaperVhi-an DaudNo ratings yet
- Jaut 08 I 2 P 129Document4 pagesJaut 08 I 2 P 129fahmie halimNo ratings yet
- BCL-TA - (2 - 8a) - TECH - Manual - ENG - (DBQ100-EN Rev00) PDFDocument63 pagesBCL-TA - (2 - 8a) - TECH - Manual - ENG - (DBQ100-EN Rev00) PDFGhozy AnamNo ratings yet
- Transcript Hazvineyi M DhlakamaDocument2 pagesTranscript Hazvineyi M DhlakamaLiane ShamidoNo ratings yet
- Module 2Document7 pagesModule 2Sheryhan BayleNo ratings yet
- Entellus Medical Investor Presentation August 2017Document26 pagesEntellus Medical Investor Presentation August 2017medtechyNo ratings yet
- Lesson Plan SampleDocument2 pagesLesson Plan SampleClarin Guivencan CharlotteNo ratings yet
- Ophtalmology Record Corneal Ulcer: Anggi Lewis R P Aruan 1161050113Document7 pagesOphtalmology Record Corneal Ulcer: Anggi Lewis R P Aruan 1161050113LewishoppusNo ratings yet
- Basics of Binocular Single Vision and Strabismus: Acta Scientific Ophthalmology (ISSN: 2582-3191)Document3 pagesBasics of Binocular Single Vision and Strabismus: Acta Scientific Ophthalmology (ISSN: 2582-3191)Ramya SaisreeNo ratings yet
- Crestor (Rosuvastatin Calcium) : Abbreviations Abbrev Definitions Dictionary ICD9 Codes Equipment Hospitals Drugs More.Document2 pagesCrestor (Rosuvastatin Calcium) : Abbreviations Abbrev Definitions Dictionary ICD9 Codes Equipment Hospitals Drugs More.Aidi RahmanNo ratings yet
- Assignment 2Document8 pagesAssignment 2Nesha VincentNo ratings yet
- Menomonee Falls Express News 040613Document20 pagesMenomonee Falls Express News 040613Hometown Publications - Express NewsNo ratings yet
- Chapter 038Document51 pagesChapter 038Ako To100% (1)
- TCM Internal Medicine Simplified - HandoutDocument94 pagesTCM Internal Medicine Simplified - HandoutSam Gt100% (2)
- DAFTAR PUSTAKA ProposalDocument1 pageDAFTAR PUSTAKA ProposalHendra TampubolonNo ratings yet
- Kristine Fish: Health Promotion Programs. 26Document4 pagesKristine Fish: Health Promotion Programs. 26api-359759447No ratings yet
- Maha TUFSDocument10 pagesMaha TUFSVishal RathiNo ratings yet
- Vicks Vaporizer v100Document2 pagesVicks Vaporizer v100eddieyetNo ratings yet
- Relationship of Knowledge and Personal Hygiene With The Incidence of Leprosy in Tanjung Jabung TimurDocument5 pagesRelationship of Knowledge and Personal Hygiene With The Incidence of Leprosy in Tanjung Jabung TimurInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Holway & Spriet (2011) Sports NutritionDocument12 pagesHolway & Spriet (2011) Sports NutritionCallum BromleyNo ratings yet
- PFR Parental Authority and Custody CasesDocument134 pagesPFR Parental Authority and Custody CasesJun KwehNo ratings yet
- Research Schedule Winter Semester 2022-23Document40 pagesResearch Schedule Winter Semester 2022-23Rahil KodinariyaNo ratings yet
- Fosfomycin: Review and Use Criteria BackgroundDocument12 pagesFosfomycin: Review and Use Criteria BackgroundAbu Azzam Al-Hadi100% (1)